Medicaid Suspension under Washington Apple Health FAQ
Individuals in the custody of the criminal justice system need seamless access to community treatment networks
and medical assistance upon release to prevent gaps in treatment and reduce barriers to accessing care. Beginning
July, 2017 due to the passage of Substitute Senate Bill (SSB) 6430, the Health Care Authority (HCA) will suspend,
rather than terminate, medical assistance benefits for individuals who are incarcerated or committed to a state
hospital. The intent is to provide continuity of care for individuals upon re-entry into the community. For more
information, visit www.hca.wa.gov/medicaid-suspension
About Medicaid Suspension
What is suspension of Medicaid?
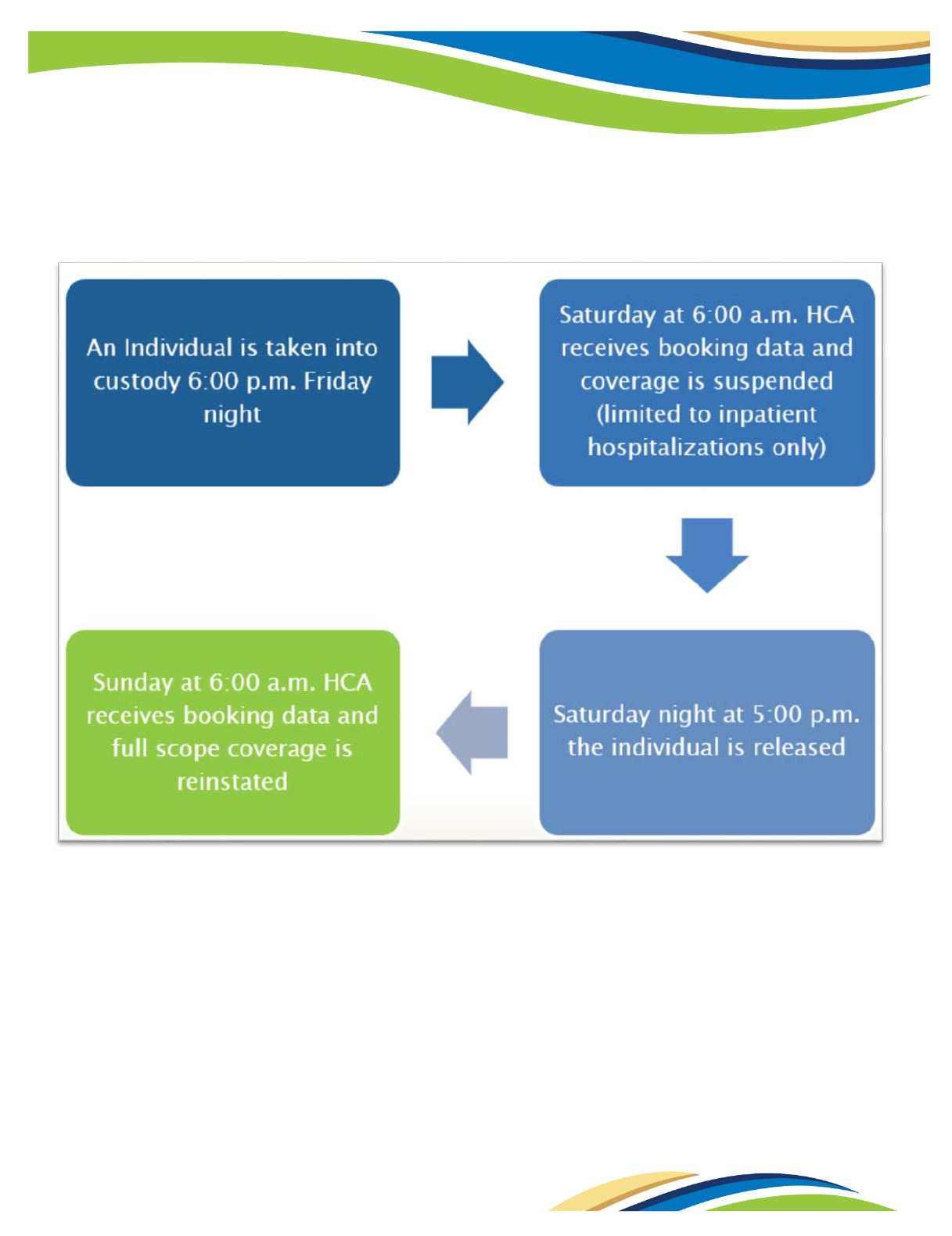
HCA promoted new system automation and policy in July 2017 regarding incarcerated individuals and their
Washington Apple Health (Medicaid) coverage. ProviderOne (P1) interfaces daily with the city/county Jail Booking
and Reporting System (JBRS) and incarcerated individuals will show in P1 with a new “SBP (suspended benefit
package) Institutionalized Dates” RAC (recipient aid category) and a new “Suspended – Inpatient Hospital Services
Only” service package. This means the individual’s coverage is in a suspended status and P1 will only pay inpatient
claims. Apple Health eligibility is not changed but the scope of coverage is reduced to inpatient services only (an
inpatient event is when an individual is formally admitted by doctor’s orders). When the individual is released, the
interface end-dates the SBP Institutionalized RAC and full scope coverage is restored without any action required
on the part of the individual. Please refer to the suspension process example provided in this document.
Who is a justice involved (JI) individual?
A justice involved (JI) individual is any individual who is incarcerated in a prison or jail setting or is under
supervision or being monitored by a correctional entity including work release. This “status” could also extend to
infrequent contacts by a community supervision or probation officer long after release from a formal jail setting.
The JI individual is a new term and not universally used but is considered a favorable descriptive title.
Who is an institutionalized individual?
In relation to Apple Health Medicaid suspension, the term institutionalized refers to incarcerated individuals or
those residing in Western or Eastern State Hospitals.
What is a correctional facility?
Correctional facility is a term used to refer to either a city/county jail or prison. Prisons are state facilities
administered by the Department of Corrections (DOC). Jails and detention centers are administered by local
municipalities. Individuals who receive sentences for longer than one year will serve their term in prison.
Sentences for less than one year are served in a city/county jail.
What institutionalized populations will have Medicaid coverage suspended and when?
• On July 7, 2017 suspension went live for DOC (prisons) and city/county jails.
• A process for suspension of benefits for other populations, (Eastern/Western State Hospitals, juvenile
rehabilitation facilities and tribal jails for example) will be established in the second phase of
implementation (2017/2018).
Continued
HCA 19-619 (10/17)

Under what circumstances can a JI individual be eligible for Apple Health?
Justice involved individuals must meet the same Apple Health eligibility criteria as any other
individuals: citizenship or satisfactory immigration status, social security number enumeration, and
income are the major eligibility factors. Incarceration does not affect Apple Health eligibility, but it does
impact the scope of coverage. While incarcerated, only inpatient hospitalizations lasting longer than 24
hours are a covered benefit. When there is a question regarding whether an individual’s incarceration
status or setting allows them to be eligible for full scope coverage, the Apple Health (Medicaid) manual
“Program Options for the Justice-Involved” matrix
provides clarity. For any other questions regarding a
JI individual’s eligibility, please contact the Medical Assistance Customer Service Center (MACSC) at 1-
800-562-3022.
Are there exceptions to the rule regarding institutionalized individuals?
Yes, the exception is inpatient hospitalizations that last longer than 24 hours. Medicaid can be billed for
inpatient medical services for incarcerated individuals who were in jail or prison but required inpatient
medical care. These rules differ for those under 22 years of age in an Institution for Mental Disease
(IMD). In 2018 the State hospitals will be included in the scope of suspension and more details will be
provided at that time.
Will Apple Health be billed for medical services provided while an individual is
incarcerated?
Per the Centers for Medicare and Medicaid Services (CMS) rules, only inpatient hospitalizations lasting
longer than 24 hours are a covered benefit for Apple Health clients while incarcerated. All other medical
care is the responsibility of the correctional facility.
Will HCA be able to recoup any managed care premiums?
If determined an individual was incarcerated for a full calendar month (not 30 day period) and the
managed care premium was paid for that period, the premium will be recouped.
What system is used to suspend coverage?
In ProviderOne, claims suspend when the JBRS/DOC interface makes a direct match to an individual.
Once coded as suspended, ProviderOne will only pay inpatient claims. For additional information,
please refer to the section entitled “The Suspension Process”.
Is federal approval needed to suspend Apple Health eligibility vs terminating it?
No, we do not need CMS approval. Suspension is a policy encouraged by CMS.
What is care coordination?
Care coordination for the justice involved includes a deliberate organization of patient care and may
include activities such as scheduling medical appointments, conducting assessments and arranging
transportation. The intent is to facilitate a successful reentry into the community with the goal of
reducing recidivism (the incidence of reoffending).
Are correctional facilities required to collaborate with Behavioral Health
Organizations (BHOs) and Managed Care Organizations (MCOs)?
Correctional facilities are encouraged to collaborate and most facilities believe care coordination will
result in a benefit to the individual, the community and lead to reduced recidivism.
Continued
How will HCA know someone has been incarcerated?
Each night HCA receives jail data from the statewide JBRS and from DOC regarding incarcerated
individuals. State law requires prison and jail roster information be accessible to the public.
Do I need to report incarceration?
For Apple Health, HCA does not need this change reported due to receiving DOC and city/county jail
booking data. For any questions or updates, please contact the HCA Medical Assistance Customer
Service Center (MACSC) at 1-800-562-3022. Incarceration may need reporting, if receiving other state
benefits, such as cash or food assistance. Please report changes to DSHS at 1-877-501-2233.
Continued

Who can I contact if I have a question regarding an individual’s circumstances?
For any questions regarding an individual’s suspension status, please contact the Medical Assistance
Customer Service Center (MACSC) at 1-800-562-3022.
What if I think the suspension status in ProviderOne is incorrect?
When there is a question regarding an individual’s incarceration status, please contact the Medical
Assistance Customer Service Center (MACSC) at 1-800-562-3022.
How do you renew eligibility coverage for a suspended case?
Coverage for Apple Health for adults, pregnant women, children, and parents/caretakers is called
Modified Adjusted Gross Income (MAGI) Medicaid. MAGI households found reasonably compatible
(income verified below the Medicaid standard via an automated data-match) will auto-renew.
Households found not reasonably compatible (income reported under the Medicaid standard, but data
match verifies income over the Medicaid standard) and do not get renewed by a household member,
will close as they would today if no action was taken.
Apple Health coverage for individuals who are aged, blind, or disabled or in need of long-term care
(LTC) services and supports is called “Classic” Medicaid. Classic households will receive a renewal form
sent via mail to the last known address. If no response is received, coverage will terminate.
Apple Health coverage managed by DSHS’ Home & Community Services (HCS) are not automatically
suspended. If notification of incarceration is received for an LTC case, ProviderOne will generate a
Barcode tickler to DSHS. Future action taken by DSHS HCS staff is dependent upon HCS’ internal policy
and results of monitoring the case.
The grace period for completing a renewal continues to exist for cases that suspend, as referenced in
the Apple Health (Medicaid) eligibility manual
.
What if a client is enrolled in a managed care plan and becomes incarcerated?
An incarcerated individual remains enrolled in managed care even if they are incarcerated for all but
one day of the month. ProviderOne is programmed to dis-enroll from managed care plans when an
individual is incarcerated for the entirety of a month (not a 30 day period but a full calendar month
such as August 1st through August 31st).
Will the individual need to visit a DSHS Community Services Office (CSO)?
No, not in relation to suspension. Individuals may need to go to the CSO to apply for other services such
as cash and food assistance.
What will happen to the benefits of other family members in the same household?
In most cases the family coverage will remain the same. Occasionally, households will need to be
reconfigured when the future living arrangement will change significantly.
When an individual’s coverage is suspended, are they still being counted towards
the Medical Assistance Unit (MAU) of other household members?
Yes, only the incarcerated individual’s coverage is changed.
Continued

Suspension Changes in ProviderOne
How can incarcerated individuals be identified in ProviderOne?
In ProviderOne incarcerated individuals will have a SBP (suspended benefit package) Institutionalized
Dates Recipient Aid Category (RAC) of 8500 if residing in a city/county facility or an OHP (Offender
Health Plan) RAC of 8000 if residing in a DOC facility. The SBP and OHP RAC are not the true indicators
of suspension. Suspension dates can only be identified by the “Suspended – Inpatient Hospital Services
Only” service package. For further detail, please refer to the screen images that follow.
How can dates of suspension be identified in ProviderOne?
In the ProviderOne Benefit Inquiry screen, suspended cases will have a “Suspension – Inpatient Hospital
Services Only” service package listed. The dates provided are the dates of suspension.
Example of open Suspended Benefit Package (SBP) – Institutionalized Dates (8500 jail RAC) with open suspension
service package limiting coverage to inpatient hospitalizations only (see Appendix A).
Continued

This case is an example of a closed RAC 8000 Offender Health Plan (OHP) eligibility segment. The OHP RAC 8000
segment is utilized for DOC prison inmates. This example also shows a closed 8500 jail segment. In this scenario the
suspended service package limiting coverage to inpatient hospital services only is closed and the client has active
full scope Medicaid coverage. (see Appendix A)
Will HCA grant ProviderOne access to correctional facilities?
This subject is under review. Certified providers currently have access to look up clients in
ProviderOne. For those who do not have access to ProviderOne, HCA is researching other avenues for
correctional facilities to access client coverage information.
Suspension and Special Populations
Does being convicted or charged with a misdemeanor or felony affect Apple Health
suspension?
No, eligibility for Apple Health (and suspension) is not related to any crimes an individual may be
convicted of or charged with.
Continued

What happens to coverage in a suspended status for the aged, blind, or disabled
(non-MAGI) programs?
There is no difference under Apple Health suspension between “Classic”/non-MAGI and MAGI Medicaid.
Suspension will be applied to both “Classic”/non-MAGI and MAGI Medicaid with the same policies and
procedures. Renewals for MAGI will be based upon reasonable compatibility. Renewals for “Classic” will
follow the current policy and procedures for this population.
EXCEPTION: Coverage for individuals receiving aged, blind, or disabled coverage and receiving services
from DSHS HCS will not suspend and a tickler is sent to DSHS to manually review.
What about children who become incarcerated?
The Center for Medicare and Medicaid Services (CMS) rule which prohibits the use of federal dollars to
pay for care while an individual is institutionalized or incarcerated is applicable to adults and children.
The juvenile population is not included in Phase One of the suspension project and will be addressed in
late 2017 and 2018.
How will suspension affect a Supplemental Security Income (SSI) recipient?
An SSI recipient’s cash benefits will close if Social Security Administration (SSA) determines their stay
is more than temporary. This is an SSA process and will not change due to suspension. SSI-related
medical benefits will be suspended and reinstated upon release.
Does the coordination of care for individuals in Eastern or Western state hospital
apply only to MCOs in the fully integrated managed care regions?
All MCOs are required to provide care coordination for individuals being discharged from WSH or ESH,
regardless of the area they are discharged to. State hospitals are considered covered institutions under
SSB 6430.
What if the individual needing care is undocumented?
The process remains the same for undocumented individuals or individuals here less than 5 years; the
Alien Emergency Medical (AEM) program addresses inpatient hospitalization needs.
What if an individual is on an “immigration hold”?
An immigration hold or order implies they do not have a satisfactory immigration status that qualifies
them for Apple Health. This population is not included in the scope of suspension however they may be
eligible for AEM coverage.
If a client has met the five year bar during incarceration and is eligible for another
program, will the system transition them to the correct program?
Yes, the next time the system determines eligibility, the program will be switched to the correct one.
Are immigration detention centers included?
No, immigration detention centers are not considered institutions under SSB 6430.
Continued

What about a Washington state resident justice involved individual held in
another state?
Occasionally correctional entities rent space in other jails including other states. These individuals are
still the responsibility of the WA city/county facility or Department Of Corrections. If they have an
inpatient hospitalization in that other state, it is up to the WA facility to pay those costs or apply for
Medicaid to cover the costs. The address used should be in Washington. This does not include
individuals who are arrested in another state. In that situation Apple Health should be closed and the
arresting entity is responsible for any medical costs. ProviderOne only receives incarceration data for
Washington jails.
Are individuals in federal correctional facilities eligible for Apple Health?
No, individuals in federal correctional facilities are not considered WA residents; therefore, they are not
eligible. While in a federal facility an individual’s care is the responsibility of the federal government.
Additionally, federal facilities are not included in the scope of Medicaid suspension.
What will happen to American Indian/Alaska Native (AI/AN) coverage if
suspended?
For AI/AN individuals whose coverage was suspended, they will be enrolled back into the program they
were suspended from following the same process as all other incarcerated individuals. For example, an
individual enrolled in managed care will automatically be re-enrolled back into managed care, an
individual enrolled in fee for service (FFS), will go back onto FFS.
Why are work release participants in certain facilities eligible for Apple Health
(Medicaid) and others are not?
Some work release facilities allow “freedom of movement “which means participants can sign out to go
to the library, religious services, access medical care, etc. Other work release facilities do not allow this
“freedom of movement”. Primarily only DOC work release facilities allow this freedom of movement
however there are a few city/county jail facilities which qualify as well. The following is a list of specific
work release facilities where participants qualify for full scope (unsuspended) Apple Health coverage (if
all other eligibility factors are met).
• Ahtanum View – Yakima County
• Bellingham – Whatcom County
• Bishop House – King County
• Brownstone – Spokane County
• Clark County – Clark County
• Eleanor Chase House – Spokane County
• Helen B Ratcliff – King County
• Longview – Cowlitz County
• Olympia – Thurston County
• Peninsula – Kitsap County
• Progress House – Pierce County
• Reynolds – King County
• Tri-Cities – Benton County
Additionally, Thurston and Seattle/King County operate work release programs that allow “freedom of
movement” and thus participants can be eligible for unsuspended Apple Health the same as DOC work
release participants.
Note: The only DOC Facilities that are unapproved are: Lincoln and Rap Houses in Pierce County.
