
Scientific Advisory Group
COVID-19 Scientific Advisory
Group Rapid Evidence Brief
Vitamin D in the Treatment and Prevention of COVID-19
January 7, 2021

2
Last revised: January 7, 2021
Table of contents
Lay Summary .................................................................................................................. 3
Authorship and Committee Members .............................................................................. 4
Topic ............................................................................................................................... 5
Context ............................................................................................................................ 5
Key Messages from the Evidence Summary ................................................................... 6
Recommendations .......................................................................................................... 6
Practical Considerations .................................................................................................. 7
Research Gaps ............................................................................................................... 8
Strength of Evidence ....................................................................................................... 8
Limitations of this review .............................................................................................. 8
Summary of Evidence ..................................................................................................... 9
Evidence from secondary and grey literature ........................................................... 9
Research Question 1 ................................................................................................... 9
Evidence from the primary literature ........................................................................ 9
Synthesis of the Information Relating to Question 1 .............................................. 11
Research Question 2 ................................................................................................. 12
Evidence from the primary literature ...................................................................... 12
Synthesis of the Information Relating to Question 2 .............................................. 12
Research Question 3 ................................................................................................. 12
Evidence from the primary literature ...................................................................... 12
Synthesis of the Information Relating to Question 3 .............................................. 17
Research Question 4 ................................................................................................. 18
Evidence from the primary literature ...................................................................... 18
Synthesis of the Information Relating to Question 4 .............................................. 18
Evolving Evidence ......................................................................................................... 18
Appendix ....................................................................................................................... 20
List of Abbreviations .................................................................................................. 20
Methods ..................................................................................................................... 20
Literature Search .................................................................................................... 20
Critical Evaluation of the Evidence ......................................................................... 21
Search Strategy ......................................................................................................... 25
References .................................................................................................................... 27

3
Last revised: January 7, 2021
Lay Summary
Background
• Vitamin D is important for bone and muscle health. It has also been hypothesized
that vitamin D may have a role in the body’s immune response to respiratory
viruses, including COVID-19.
• There is an overlap between groups at risk of vitamin D deficiency and groups at
high risk of severe COVID-19, with a complex relationship of lower
socioeconomic status and nutritional status. Low vitamin D levels may be a
marker of poor health so whether low vitamin D levels are a cause of COVID-19
or a reflection of health status is a point of debate.
• We examined current scientific evidence to evaluate if vitamin D is effective in
the treatment and prevention of COVID-19.
Findings
• There is no high quality evidence that suggests taking vitamin D supplements is
specifically effective in the prevention or treatment of COVID-19.
• For general health, it is important to have adequate vitamin D levels regardless of
the effects on COVID-19. The recommended daily intake for Canadians ranges
from 400-800 IU (10-20 mcg) daily depending on stage of life, with a tolerable
upper intake level of 1,000-4,000 IU (25-100 mcg) daily.
• Further research on vitamin D and COVID-19, with well-designed randomized
controlled trials and appropriate follow-up time is ongoing.

4
Last revised: January 7, 2021
Authorship and Committee Members
Name
Contribution
Marni Armstrong
Primary writer (evidence extraction, data synthesis, original
draft preparation)
Marla Palakkamanil
Primary writer (evidence extraction, data synthesis, original
draft preparation)
Nicole Loroff
Librarian (search strategy and eligibility screening)
Jeremy Slobodan
Primary scientific reviewer
Judy Seidel
Mary Modayil
Lynora Saxinger
Secondary scientific reviewers
Braden Manns
Lynora Saxinger
Scientific Advisory Group chairs (oversight and leadership
responsibility)
John Conly, Alexander
Doroshenko, Shelley
Duggan, Nelson Lee,
Elizabeth MacKay,
Andrew McRae,
Melissa Potestio,
Jeremy Slobodan,
James Talbot, Brandie
Walker, Nathan Zelyas
Scientific Advisory Group members (review and approval of
document)
© 2020, Alberta Health Services, COVID-19 Scientific Advisory Group
This copyright work is licensed under the
Creative Commons Attribution-NonCommercial-NoDerivative 4.0
International license. You are free to copy and distribute the work including in other media and formats for
non-commercial purposes, as long as you attribute the work to Alberta Health Services, do not adapt the
work, and abide by the other licence terms. To view a copy of this licence, see
https://creativecommons.org/licenses/by-nc-nd/4.0/. The licence does not apply to AHS trademarks, logos or content for which
Alberta Health Services is not the copyright owner. Disclaimer: This material is intended for general information only and is provided
on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health
Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness,
applicability or fitness for a particular purpose of such information. This material is not a substitute for the advice of a qualified health
professional. Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions,
demands or suits arising from such use.

5
Last revised: January 7, 2021
Topic: Vitamin D in the treatment and prevention of COVID-19
Key Research Questions
1. What is the effectiveness and safety of vitamin D supplementation for the
treatment of COVID-19?
2. What is the effectiveness and safety of vitamin D supplementation for the
prevention of COVID-19?
3. Is vitamin D status associated with susceptibility to COVID-19?
• Is there any evidence that low vitamin D levels are an independent risk for
COVID-19 infection or severe COVID-19 infection?
4. From the evidence selected, are there any subgroups of people who may benefit
from vitamin D supplementation more than the wider population of interest?
Context
• Vitamin D is important for bone and muscle health. It has also been hypothesized
that vitamin D may have a role in the body’s immune response to respiratory viruses.
• Research suggests that there is inadequate sunlight (UVB) during Alberta’s winters
for effective synthesis of vitamin D due to a significant impact of northern latitudes.
Edmonton, at 52 degrees N, has an ineffective winter period from October through
March
, Boston at 42.2 degrees N from November to February, but winter
photoconversion is effective south of 34 degrees N (Webb et al., 1988).
• Given the widespread interest in therapeutic potential of vitamin D, clinicians may be
increasingly asked about whether vitamin D deficiency is related to increased
susceptibility to or severity of COVID-19.
• Media reports are presenting vitamin D as promising in the prevention and treatment
of COVID-19.
• Some media and social media reports appear to recommend supplementation well
above the current vitamin D supplementation guidelines.
• This evidence summary examines the effectiveness and safety of vitamin D
supplementation for the treatment and prevention of COVID-19, and explores the
evidence regarding vitamin D as an independent risk factor for COVID-19 infection.
• This review summarizes and builds upon the evidence review
completed by the
National Institute for Health and Care Excellence (NICE) COVID-19 Rapid Guideline:
Vitamin D published December 17, 2020. This review comprises an updated
literature search through to December 8, 2020, compared to the NICE review where
the literature search ended October 27, 2020.
•
There is an overlap between groups at high risk of vitamin D deficiency and groups
at high risk of severe COVID-19. Examples include people with chronic disease,
older age, and people of Black and minority ethnic heritage, which makes
assessment of observed associations between low vitamin D and COVID-19
infection challenging. Vitamin D levels may be indicative of co-morbidities that may
themselves impact COVID-19 outcomes, so whether low vitamin D levels are a
cause of disease or consequence of health disparity has remained a point of debate.

6
Last revised: January 7, 2021
Key Messages from the Evidence Summary
• There is no high quality evidence to support taking vitamin D supplements to specifically
prevent or treat COVID-19. To date, there are three RCTs assessing different
formulations of vitamin D in patients hospitalized with COVID-19; however, the results
have been variable and concerns with small sample size, dosing regimen, and
inappropriate randomization limit the conclusions that can be drawn. The largest trial
(Murai et al, 2020; n = 240) showed no benefit.
• While there have been a number of observational studies evaluating the association of
vitamin D status and COVID-19, the evidence is very weak. Concerns with confounding
(see description of patient population at risk overlap above), sample size, selection bias,
and reverse causality limit the conclusions that can be drawn.
• Addressing vitamin D deficiency is important for general health, irrespective of the
effects on COVID-19. People should continue to follow the current practice guidelines on
daily vitamin D supplementation. The daily recommended intake for Canadians ranges
from 400-800 IU daily by age and can be found at:
https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/vitamins-
minerals/vitamin-calcium-updated-dietary-reference-intakes-nutrition.html#a10.
• There may be some benefit from daily, low-dose vitamin D supplementation (between
400 to 1,000 IU/day) in reducing the risk of acute respiratory tract infections, based on a
meta-analysis of randomized controlled clinical trials.
Recommendations
Recommendation 1: Vitamin D should not be offered as therapy for COVID-19 infection.
Rationale: To date, the clinical evidence is very weak with only a few small studies available.
There is insufficient evidence at this time to recommend treatment of COVID-19 with high
dose vitamin D supplementation, except as part of a clinical trial.
Recommendation 2: Vitamin D supplementation should not be recommended for the
purpose of preventing COVID-19.
Rationale: While a number of observational studies have demonstrated an association
between vitamin D status and COVID-19, the strength of the evidence remains very low and
there are no RCTs evaluating vitamin D as preventive therapy.
Recommendation 3: Health Care Providers and patients are encouraged to follow current
established guidelines by Health Canada
which suggest appropriate supplementation of
vitamin D, with all Albertans noted to be eligible for appropriate supplementation.
Rationale: Vitamin D deficiency has been established as an important risk factor for bone
health, and supplementation with vitamin D may reduce the risk of acute respiratory tract
infections. Testing of vitamin D levels is not required or routinely recommended prior to
vitamin D supplementation.

7
Last revised: January 7, 2021
Practical Considerations
• Given the current evidence, testing for vitamin D deficiency is not recommended in
routine screening or in the setting of COVID-19 – see the guidelines from Choosing
Wisely Canada (Pathology and Family Medicine) and the Alberta Medical Association
.
• Associations between vitamin D status and COVID-19 are not surprising as vitamin D
deficiency may represent a surrogate marker for a general micronutrient deficiency,
which in turn reflects the patient’s overall health status – many of the risk factors for
severe COVID‑19 outcomes are the same as the risk factors for low vitamin D status.
• Clinicians should encourage appropriate vitamin D supplementation (see the current
Health Canada
guidelines for Canadians) particularly in groups at higher risk of vitamin
D deficiency.
• While there is limited evidence for an association between vitamin D and the severity of
COVID-19, it is reasonable to counsel patients around appropriate vitamin D
requirements and recommended supplementation for general health. This would include
people at higher susceptibility for COVID-19 (e.g. those in long-term care centers) to
ensure that current vitamin D supplementation is in accordance with guidelines.
Current Recommendations on Vitamin D Supplementation
Vitamin D supplements are available in two forms: vitamin D
2
(ergocalciferol) and vitamin D
3
(cholecalciferol). Both vitamin D
2
and vitamin D
3
are metabolized by the liver to form 25-
hydroxycholecalciferol or 25(OH)D (calcifediol), which is then metabolized by the kidney to form
calcitriol (1,25-dihydroxycholecalciferol), the most biologically active form of vitamin D (Armas,
Hollis, & Heaney, 2004). Vitamin D
3
is the preferred supplementary form, with vitamin D
2
being
available for large-dose preparations.
Current recommendations are based on an Institute of Medicine report (IOM, 2011)
commissioned by Health Canada on the dietary reference intakes for vitamin D. The report
suggests that a 25(OH)D serum level of 50 nmol/L is sufficient for most of the population to
maintain bone and overall health and have based the recommended dietary allowances on this
serum level and the assumption that sun exposure is minimal. However, as vitamin D
supplementation for the general adult population is safe and necessary, supplements can be
recommended without testing for deficiency.
Table 1: Dietary Reference Intakes (DRIs) for Vitamin D (Health Canada, 2020)
Age
group
Recommended Dietary
Allowance (RDA) per day
Tolerable Upper Intake
Level (UL) per day
Infants 0-6 months
400 IU (10 mcg)*
1000 IU (25 mcg)
Infants 7-12 months
400 IU (10 mcg)*
1500 IU (38 mcg)
Children 1-3 years
600 IU (15 mcg)
2500 IU (63 mcg)
Children 4-8 years
600 IU (15 mcg)
3000 IU (75 mcg)
Children and Adults 9-70 years
600 IU (15 mcg)
4000 IU (100 mcg)
Adults > 70 years
800 IU (20 mcg)
4000 IU (100 mcg)
Pregnancy & Lactation
600 IU (15 mcg)
4000 IU (100 mcg)
*Adequate Intake rather than Recommended Dietary Allowance.

8
Last revised: January 7, 2021
• For adults over the age of 50 and at risk of osteoporosis, recommended
supplementation doses range from 800-2,000 IU.
• There are health risks associated with excessive or toxic amounts of vitamin D. The
upper limit suggested to be safe for most individuals is 4,000 IU per day, and toxic
levels of vitamin D usually require much higher consumption, up to 10,000 IU per
day. These risks include hypercalcemia, hypercalciuria, which can lead to nausea,
vomiting, muscle weakness, neuropsychiatric disturbances, pain, loss of appetite,
dehydration, polyuria, excessive thirst, and kidney stones. In extreme cases,
vitamin D toxicity can cause renal failure, calcification of soft tissues throughout the
body (including in coronary vessels and heart valves), cardiac arrhythmias, and
even death.
• There is no clinical benefit of testing vitamin D levels in the general population
regardless of common risks (such as low dietary intake and/or seasonal (sunlight)
variation), as vitamin D supplementation for the general population should be
recommended regardless of screening and monitoring.
• In patients with clinical conditions that may be predisposed to vitamin D deficiency
such as malabsorption syndromes, chronic renal or liver failure, unexplained bone
pain, unusual fractures, and other evidence of metabolic bone disorders, vitamin D
testing may be warranted
.
Research Gaps
As with all the COVID-19 literature, there is much we still do not know. This review and the
accompanying recommendations are limited by the fact that most studies in the area of vitamin
D and COVID-19 have many limitations, in particular, the potential for bias and insufficient
power. It is suggested that future RCTs completed have a minimum 8-week follow up and
examine all care settings (NICE, 2020, December). There should be a particular focus on
subgroup analyses including, but not limited to, age (such as over 75 years), ethnicity (for
example, Black, Asian and minority ethnic groups) and comorbidities (for example, obesity) that
are associated with poorer outcomes in people with COVID-19. Adequately powered RCTs of a
properly defined effective doses of vitamin D in prophylaxis and in therapy are needed to clarify
the role of vitamin D supplementation in COVID-19, and many trials are ongoing (71 trials are
registered at clinicaltrials.gov
). This brief therefore may be updated in the future.
Strength of Evidence
At this time, the evidence is not strong for the use of vitamin D supplementation in the
prevention or treatment of COVID-19. Much of the published evidence is observational and
examines retrospective associations making it subject to potential bias and confounding.
Association studies should be used to inform future research. Results from high quality,
appropriately powered randomized controlled trials are needed. We identified only three RCTs.
Two were small in size (n<80) with serious concerns with quality and confounding. The
remaining study was larger (n=240) and of a stronger methodological design; this study failed to
find any difference between the groups and has yet to be peer-reviewed.
Limitations of this review
Many of the populations examined here are patients who have been admitted to hospital or the
ICU. Clinical decisions made with respect to admission may vary greatly by country/jurisdiction

9
Last revised: January 7, 2021
and may change substantially over the course of the pandemic. This may limit the
generalizability of these findings to the Alberta context.
Rapid turnaround time limited the ability to perform an in-depth data extraction of effects and/or
meta-analysis. Databases were searched for English-language evidence published in 2020,
after the period covered by the NICE evidence review, thus, evidence from other jurisdictions
where English is not common has not been included in this review.
Summary of Evidence
This review summarizes and builds upon the evidence reviews
completed by the National
Institute for Health and Care Excellence (NICE, 2020, December) published December 17, 2020
for their
COVID-19 rapid guideline: Vitamin D. Their search was completed on October 27, 2020
and did not include preprints, whereas this current review had a search date of Dec 8, 2020 and
does include preprints.
Our search was adapted from the initial NICE evidence review Vitamin D for COVID-19, June
29, 2020 (NICE, 2020, June). For this review, we searched the literature in a database search
covering: OVID MEDLINE, LitCovid, PubMed, TRIP PRO, WHO COVID-19 Database, Centre
for Evidence Based Medicine (CEBM), CADTH COVID-19 Evidence Portal, COVID-Evidence
medRxiv, Cochrane Library and Google Scholar. Given the NICE systematic review, we
primarily limited our search to dates beyond their search date of June 5, 2020.
A total of two writers were involved in the screening and extraction. We identified 182 articles
that met our PICO criteria through title and abstract screen. The included studies were identified
through two screening stages. In the first stage, we screened articles based on our
inclusion/exclusion criteria (n=50). The majority of the studies excluded at this stage were
commentaries or reviews that were not systematic, as well as ecological studies that used
weather patterns (e.g. ultraviolet index) or geographical latitude of locations as a proxy for
vitamin D alone. The second stage of screening involved a preliminary quality appraisal screen
resulting in the inclusion of 16 key studies: 3 RCTs, 12 observational cohorts, and 1 systematic
review. It should be noted that given interventional studies are regarded as the highest level of
evidence, we did not exclude any interventional studies based on quality alone.
Evidence from secondary and grey literature
We found that any secondary and grey literature that was identified that addressed these
research questions primarily included citations to primary literature or original research. In turn,
this review limited its analysis and discussion to primary literature or original research (including
preprints) for all the research questions.
Research Question 1
What is the effectiveness and safety of vitamin D supplementation for the
treatment of COVID-19?
Evidence from the primary literature
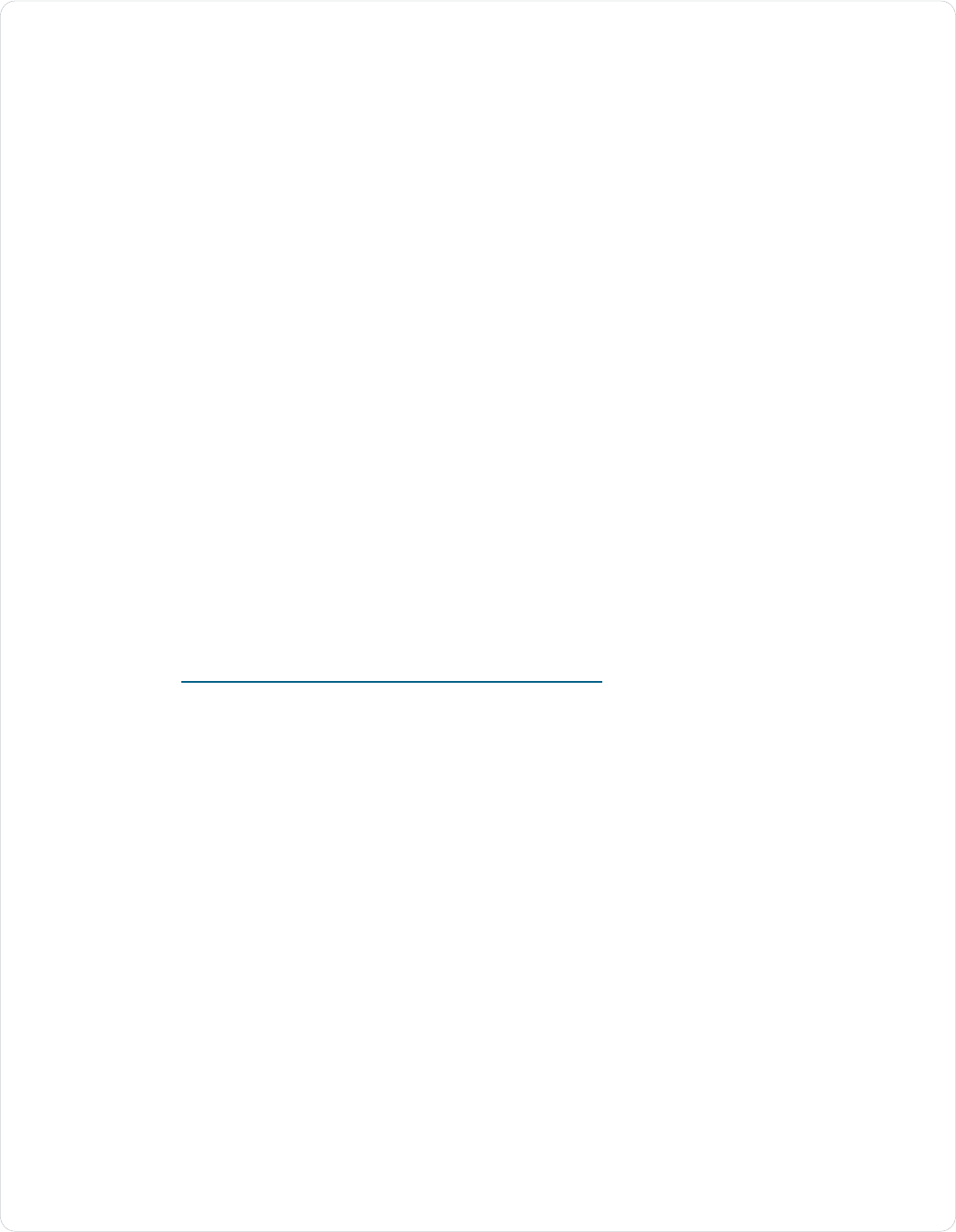
We identified three RCTs, details of the studies are summarized in Table 2.
A pilot randomized controlled trial (Entrenas Castillo et al., 2020) among patients (n=76)
hospitalised for COVID-19 infection evaluated the effectiveness of administering a high dose

10
Last revised: January 7, 2021
(0.532 mg / 21,280 IU) of oral 25-hydroxyvitamin D
3
(calcifediol) upon admission. Patients were
allocated at a 2:1 ratio for randomization and all patients received a combination of
hydroxychloroquine and azithromycin in combination with the vitamin D supplementation.
Outcomes included need for ICU admission and mortality. The study reported that among the
26 patients in the control group, 13 (50%) were admitted to ICU, and two died. In the
intervention group, only one out of 50 (2%) required ICU admission, and none died. Multivariate
risk estimate odds ratio for ICU admission after adjusting for hypertension and type 2 diabetes
mellitus was 0.03 (95% CI: 0.003-0.25). Weaknesses include small number of patients, ICU
admission as a subjective outcome, and the unusual dosing regimen.
A multicentre, double-blind, placebo-controlled RCT (Murai et al., 2020) in hospitalized patients
(n=240) with severe COVID-19 investigated the efficacy of a single dose of 200,000 IU of
vitamin D
3
. Outcomes included length of stay, admission to ICU, mechanical ventilation, and
mortality. The study found that length of stay was comparable between the two groups; there
was also no difference in mortality, admission to ICU and use of mechanical ventilation. Vitamin
D significantly increased serum 25(OH)D with no adverse reactions.
A placebo-controlled RCT (Rastogi et al., 2020) of hospitalized patients with COVID-19
examined whether a dose of 60,000 IU of vitamin D
3
for 7 days resulted in a difference in
negative SARS-CoV-2 RNA tests at 21 days. Ten (62.5%) participants in the intervention group
and 5 (20.8%) participants in the control arm (p<0.018) became SARS-CoV-2 RNA negative.
Table 2: Summary of identified randomized controlled trials
Study
Population
Intervention
group
Control group/
Comparator
Analysis
Outcome
Main Results
(Entrenas
Castillo et
al., 2020)
RCT
Spain
N=76 admitted
with confirmed
COVID-19
randomised in a
2:1 ratio into
intervention and
comparator
arms.
n=50 received
calcifediol (0.532
mg) on
admission, then
0.266 mg on days
3 and 7, then
weekly until
discharge, plus
standard care
n=26 received
standard care only
Univariate and
multivariable
logistic
regressions were
used to estimate
the probability of
admission to
intensive care
unit (ICU).
Mortality was
reported as
number of event
counts.
ICU
admission
COVID-19
mortality
Of the 26 patients
in the control
group, 13 (50%)
were admitted to
ICU, and two
died. In the
intervention
group, only one
out of 50 (2%)
required ICU
admission, and
none died.
Multivariate OR:
0.03 (95% CI:
0.003-0.25)
adjusted for
hypertension and
diabetes.
(Murai et
al., 2020)
RCT
Brazil
Preprint
N=240
hospitalized
patients with
severe COVID-
19 randomized
in a 1:1 ratio into
intervention and
comparator
arms.
n=120 received
single oral dose
of 200,000 IU of
vitamin D
3
dissolved in 10mL
of peanut oil
solution, plus
standard care
n=120 received
single oral dose of
10mL of peanut oil
solution, plus
standard care
Log-rank test was
used to compare
the Kaplan-Meier
estimate curves
for the number of
days for hospital
length of stay.
Hospital
length of stay
Mortality,
admission to
ICU,
mechanical
ventilation
requirement,
serum levels
of 25(OH)D,
creatinine,
calcium, C-
reactive
Hospital length of
stay was
comparable
between the
vitamin D
3
group
and the placebo
group (7.0 days
[95% CI: 6.1 to
7.9] and 7.0 days
[95% CI: 6.2 to
7.8 days], HR,
1.12, [95% CI: 0.9
to 1.5]; P = .379;
respectively). The

11
Last revised: January 7, 2021
protein, D-
dimer
rate of mortality,
admission to ICU,
and mechanical
ventilation
requirement did
not significantly
differ between
groups.
(Rastogi et
al., 2020)
RCT
India
N=40 admitted
with confirmed
COVID-19 were
randomized to
the intervention
arm or control
arm.
n=16 received
standard care
plus daily dose of
60,000 IU of
vitamin D
3
for 7
days with the aim
to achieve
25(OH)D level>50
ng/ml. 25(OH)D
levels assessed
at day-7, and
vitamin D
3
supplementation
continued for
those with
25(OH)D <50
ng/ml up until
day-14
n=24 received
standard care plus
daily dose of 5mL
of distilled water
for 7 days
Fischer Exact (2
by 2 tailed) test to
compare
proportion of
participants
achieving SARS-
CoV-2 RNA
negativity
Proportion of
participants
who turn
SARS-CoV-2
negative
(confirmed
twice at 24-
hour interval)
before week 3
and change in
inflammatory
markers
10 out of 16
patients could
achieve
25(OH)D>50
ng/ml by day-7
and another two
by day-14
(p<0.001) in
intervention
group. 10 (62.5%)
participants in the
intervention group
and 5 (20.8%)
participants in the
control arm
(p<0.018)
became SARS-
CoV-2 RNA
negative.
Synthesis of the Information Relating to Question 1
RCTs provide the strongest level of evidence as they are less susceptible to confounding.
Among the three RCTs identified, two (Entrenas Castillo et al., 2020; Rastogi et al., 2020)
reported results in support of vitamin D supplementation where one (Murai et al., 2020) reported
no difference between the intervention and control groups. However, issues with methodological
quality warrant caution when interpreting the results.
These studies are limited by their small sample sizes thereby decreasing their statistical power
and may be unrepresentative of the wider population of interest. The pilot RCT (Entrenas
Castillo et al., 2020) with 2:1 allocation was not placebo controlled and the blinding was
incomplete, leading to concerns with bias. In addition, patients assigned to calcifediol were
slightly older, whereas the control group had a higher percentage of hypertension and diabetes
mellitus. Finally, ICU admission is a somewhat subjective outcome measure which can be
affected by many variables. The randomized controlled trial (Murai et al., 2020) conducted in
Brazil had the largest sample size (n=240) of the 5 studies examined, and yet the sample size
could still have been underpowered to detect significant changes for the secondary outcomes.
As the patients had several coexisting diseases and were subjected to a diverse medication
regimen, the results could have been affected by the heterogeneity of the sample and its
treatment. The proportion of patients with 25-(OH)D deficiency in this study was considerably
lower than those reported in other cohorts, possibly as a consequence of differences in
geographic locations. The randomized controlled trial (Rastogi et al., 2020) conducted in India
only included mildly symptomatic and asymptomatic individuals, which limits the generalisability
of its results to symptomatic or severe cases of COVID-19. It is not clear whether the study was
blinded. The placebo used in the study was not exactly matched with regards to the taste and
consistency with the vitamin D
3
nano formulation leading to concerns of lack of concealment.
The use of SARS-COV2 RT-PCR negativity as an outcome is both nonclinical and of limited

12
Last revised: January 7, 2021
relevance given the wide variation in duration of RT-PCR positivity and lack of correlation with
clinical disease resolution (see an upcoming Scientific Advisory Group review on this topic).
Overall, there is limited and weak evidence from randomized controlled studies available at this
time. Of note, is that the larger study (Murai et al., 2020) with 240 patients and appropriate
randomization, failed to find any difference in outcomes with a single bolus supplementation of
vitamin D with COVID-19 diagnosis. Further research is needed in order to better evaluate if
vitamin D is effective in the treatment of COVID-19.
Research Question 2
What is the effectiveness and safety of vitamin D supplementation for the
prevention of COVID-19?
Evidence from the primary literature
No evidence relevant to the PICO protocol was found for this question.
Synthesis of the Information Relating to Question 2
At this time, there is no effectiveness or safety studies available on the efficacy nor the
effectiveness of vitamin D supplementation for the prevention of COVID-19. All available
evidence for prevention is limited to observational data as outlined below.
Note: Information and guidelines regarding the safety of vitamin D supplementation in general,
not specific to COVID-19, can be found at: Health Canada; Vitamin D and Calcium: Updated
Dietary Reference Intakes
Research Question 3
Is vitamin D status associated with susceptibility to COVID-19?
i. Is there any evidence that low vitamin D levels are an independent
risk factor for COVID-19 infection or severe COVID-19 infection?
Evidence from the primary literature
We identified 46 observational studies that reported on how vitamin D status is associated with
COVID-19 outcomes. Upon completing an initial quality appraisal, we identified 12 studies for
inclusion in this evidence review. The main reason for the exclusion of studies (n=34) was
based on quality and lack of appropriate adjustment for confounders. Among the 12 key studies
included, they examined associations of vitamin D with COVID-19 cases/infections, as well as
COVID-19 disease severity. Included in the severity outcomes were variables such as
hospitalization, admission to ICU, length of stay, mechanical ventilation, chest CT-scans,
pneumonia scoring and death. Table 3 outlines a summary of the observational studies.
Many of the studies reported on the prevalence of vitamin D deficiency in the identified COVID-
19 populations compared with controls. Although there was a range (55% to 97%), many of the
studies reported a statistically significant higher prevalence of vitamin D deficiency and lower
mean serum levels in those diagnosed with COVID-19 and in those with more severe disease
outcomes. Although several studies found no difference in vitamin D status among groups
(Butler-Laporte et al., 2020; Cereda, Bogliolo, Klersy, et al., 2020; Li et al., 2020), the majority of
included studies (n=7) did find a statistically significant difference with more vitamin D deficiency

13
Last revised: January 7, 2021
in the COVID-19 or more severe COVID-19 groups. The possibility of publication bias is not
excluded.
In evaluating the strength of the association between vitamin D status and COVID-19, the
results are less clear. While many studies reported a significant association, with odd ratios
ranging from 1.5 and as high as 3.87 in favor of vitamin D, some studies reported no association
and even reported an inverse association suggesting harm. Differing statistical approaches on
the adjustment/modeling for a variety of confounding variables further provided mixed results.
One systematic review and meta-analyses (Pereira, Dantas Damascena, Galvão Azevedo, de
Almeida Oliveira, & da Mota Santana, 2020) was identified with a search date ending Oct 9,
2020. This systematic review found that while vitamin D deficiency was not associated with a
higher chance of infection by COVID-19, they observed a positive association between vitamin
D deficiency and the severity of the disease. They reported that severe cases of COVID-19
were more likely to have vitamin D deficiency than mild cases with a modest odds ratio (OR
1.62%, 95% CI=1.06-2.58). However, concerns regarding the methodology and inappropriate
meta-analysis warrant caution when interpreting the results.
Table 3: Summary of observational studies included in the evidence review
Reference
N
Population
Comparisons
Outcomes
Summary of Key Results
(C. Annweiler et
al., 2020)
Retrospective
“quasi-
experimental”
study
France
66
Nursing home
residents
diagnosed with
COVID-19.
Residents
received chronic
vitamin D
3
supplementation
with regular
maintenance
boluses (single
oral dose of
80,000 IU
vitamin D
3
every
2 to 3 months).
When residents
last received
supplementation
dictated which
group they were
in:
n=57 received
vitamin D
3
bolus
within 1 month
of or a week
after COVID-19
diagnosis; n=9
did not receive
vitamin D
3
bolus
Associations between
predictor variables, such
as vitamin D
3
supplements, and the
likelihood of COVID-19
mortality at a specific
time.
Comparing time to death
between intervention and
comparator groups.
Associations between
bolus vitamin D
3
supplements and World
Health Organization
Ordinal Scale for Clinical
Improvement (OSCI)
score, taking into account
factors that may affect the
result.
COVID-19
mortality
World Health
Organization
Ordinal Scale
for Clinical
Improvement
(OSCI) score
for COVID-19
in acute phase
In the intervention group, 82.5%
(n=47) survived COVID-19,
compared to only 44.4% (n=4)
in the comparator group (P =
0.023). The adjusted model for
mortality according to vitamin
D
3
supplementation was HR =
0.11 [95% CI:0.03-0.48], P =
0.003.
(G. Annweiler et
al., 2020)
Retrospective
“quasi-
77
Patients
admitted to
hospital with
COVID-19.
Comparisons between
groups for the reported
outcomes.
Association between
each group and 14- day
14-day COVID-
19 mortality
In Group 1, 93% survived
compared to 81% in Group 2
(p=0.33) and 69% in Group 3
(p=0.02). Regular bolus vitamin
D
3
supplementation pre-
diagnosis was associated with

14
Last revised: January 7, 2021
experimental”
study
France
n=29 received
vitamin D
3
bolus
over the
preceding year
n=16 received a
vitamin D
3
supplement
after COVID-19
diagnosis
n=32 received
no vitamin D
3
supplement
mortality at a specific
time, adjusting for
confounders.
Comparison of survival
between the groups.
Association between
vitamin D status and
severe COVID- 19,
adjusted for confounding
variables.
OSCI score for
COVID-19 in
acute phase
less severe COVID-19 and
better survival rate in
hospitalized frail elderly.
Supplementation with 80,000 IU
vitamin D
3
after the diagnosis of
COVID-19 was not associated
with improved COVID-19
outcomes.
(Butler-Laporte
et al., 2020)
Cohort study
(Mendelian
Randomization)
Preprint
443,734
Genotype data
from UK
Biobank data
from people of
European
descent
Mendelian randomization
of genetic variants
strongly associated with
serum 25(OH)D from
genome-wide association
study (GWAS)
COVID-19 (risk
of infection,
hospitalization,
severity, death)
Genetically increased 25(OH)D
levels had no clear effect on
susceptibility but tended to
increase the odds ratio of
hospitalization (OR = 2.34; 95%
CI: 1.33, 4.11) and severe
disease (OR = 2.21; 95% CI:
0.87, 5.55). Sensitivity analyses
provided consistent estimates.
Findings do not support a
protective role of increased
25(OH)D levels on COVID-19
outcomes and may suggest
harm.
(Cereda et al.,
2020b)
Cohort study
129
Adults
hospitalized with
COVID-19
25(OH)D serum levels
assessed at hospital
admission and
categorized into: normal
(≥30 ng/mL), insufficient
(<30 - ≥20 ng/mL),
moderately deficient (<20
- ≥10 ng/mL), severely
deficient (<10 ng/mL)
Severe
pneumonia,
admission to
intensive care
units [ICU] and
in-hospital
mortality
77% of patients were vitamin D
deficient. Vitamin D deficiency
(<20 ng/mL) was not associated
with COVID-19 outcomes. A
significant positive association
between increasing vitamin D
levels and in-hospital mortality
(on a continuous logarithmic
scale, odds ratio = 1.73 [95%
CI: 1.11 to 2.69]; P = .016) was
observed.
(Chang et al.,
2020)
Case-control
study
Preprint
26,602
Individuals
tested by PCR
for SARS-CoV-
2; 992 were
COVID-19
positive; 72 with
severe outcome
25(OH)D level within past
year before PCR test.
Positive PCR
test
Vitamin D deficiency found to
be an independent risk factor
for COVID-19 (OR 1.8 [95% CI:
1.4–2.2], p=5.7 × 10−6)
(De Smet et al.,
2020)
Cohort study
186
Individuals
hospitalized with
severe SARS-
CoV-2 infection
25(OH)D measurement
on admission
Mortality
Of the patients with COVID-19,
59% were vitamin D deficient
on admission. Death rate was
15% (n=27). Vitamin D was
associated with mortality (odds
ratio [OR], 3.87; 95% CI: 1.30-
11.55), independent of age,
chronic lung disease, and
extent of lung damage
expressed by chest CT severity
score but not sex.

15
Last revised: January 7, 2021
(Hernández et
al., 2020)
Case-control
study
413
Cases (n=216):
Individuals age
≥ 18 admitted to
hospital with
confirmed
COVID-19;
n=19 taking
vitamin D
supplements
Controls:
Individuals
recruited from
the Camargo
study cohort and
were sex-
matched with
non-vitamin D
supplemented
cases.
25(OH)D measurement
on hospital admission
(cases) or during
recruitment into study
(controls)
Composite
severity
endpoint:
Admission to
the ICU,
requirement for
mechanical
ventilation, or
in-hospital
mortality
Vitamin D deficiency was found
in 82.2% of COVID-19 cases
and 47.2% of population-based
controls (P < .0001). Vitamin D-
deficient COVID-19 patients
had a greater prevalence of
hypertension and
cardiovascular diseases, raised
serum ferritin and troponin
levels, as well as a longer
length of hospital stay than
those with serum 25OHD levels
≥20 ng/mL. No causal
relationship was found between
vitamin D deficiency and
COVID-19 severity as a
combined endpoint or as its
separate components.
(Kaufman et al.,
2020)
Cohort study
191,779
Participant data
collected from a
Quest
Diagnostics
database that
processed
SARS-CoV-2
tests and
matched it to
data held on
individual’s
vitamin D results
from the
preceding 12
months.
Patients stratified
according to their serum
25(OH)D level from
preceding 12 months: ≥75
nmol/L (optimal); 51-74
nmol/L (suboptimal);
<50 nmol/L(deficiency)
SARS-CoV2
infection
The association between lower
SARS-CoV-2 positivity rates
and higher circulating 25(OH)D
levels remained significant in a
multivariable logistic model
adjusting for all included
demographic factors (adjusted
odds ratio 0.984 per ng/mL
increment, 95% CI 0.983–
0.986; p<0.001). Other
significant factors in both the
adjusted and unadjusted
models were male sex,
northern and central latitudes,
predominately Black non-
Hispanic zip codes, and
predominately Hispanic zip
codes.
(Li et al., 2020)
Cohort study
(Mendelian
Randomization)
Preprint
495,780
Demographic
information and
genotype data
from UK
Biobank linked
to COVID-19
test results
provided by
Public Health
England
25(OH)D concentration
(status: deficient,
insufficient, sufficient),
ambient UVB, and
genetically predicted
25(OH)D concentrations
COVID-19 (risk
of infection,
hospitalisation
and death)
Significant inverse associations
were found between COVID-19
infection and 25(OH)D in
univariable models, but these
associations were non-
significant after adjustment for
confounders. Ambient UVB was
strongly and inversely
associated with hospitalization
and death. Although the main
Mendelian Randomization (MR)
analysis showed that
genetically predicted vitamin D
levels were not causally
associated with COVID-19 risk,
MR sensitivity analysis using
weighted mode method
indicated a potential causal
effect (p=0.041).
(Luo et al.,
2020)
895
COVID-19
positive patients
25(OH)D concentrations
between 2018-2019
COVID-19
incidence and
In the general linear model
adjusted for age, sex,

16
Last revised: January 7, 2021
Cross-sectional
study
hospitalized
(n=335) and an
age- and sex-
matched
population
(n=560)
disease
severity
comorbidities, and BMI, serum
25(OH)D concentrations were
significantly lower among
COVID-19 patients than the
2018–2019 controls.
Multivariable logistic regression
showed that male sex (OR:
2.26; 95% CI: 1.06, 4.82),
advanced age (≥65 y) (OR:
4.93; 95% CI: 1.44, 16.9), and
vitamin D deficiency
(<30 nmol/L) (OR: 2.72; 95%
CI: 1.23, 6.01) were
significantly associated with
COVID-19 severity
(all P < 0.05).
(Meltzer et al.,
2020)
Cohort study
4313
Patients tested
for SARS-CoV-2
infection at the
university.
25(OH)D or 1,25(OH)
2
D
measurement were from
the preceding 12 months.
To account for changes to
vitamin D status, status
was estimated by taking
into account changes to
supplements taken.
Participants were
grouped as follows: likely
deficient; likely sufficient;
last level deficient and
treatment increased; and
last level not deficient and
treatment decreased.
SARS-CoV-2
infection
The relative risk of testing
positive for COVID-19 was 1.77
times greater for patients with
likely deficient vitamin D status
compared with patients with
likely sufficient vitamin D status.
In multivariate analysis, testing
positive for COVID-19 was
associated with increasing age
up to age 50 years, non-White
race, and likely deficient vitamin
D status compared with
sufficient vitamin D status, a
difference that was statistically
significant.
(Merzon et al.,
2020)
Case-control
study
14,022
n=782,
COVID-19
positive;
n=7052,
COVID-19
negative
People of the
Leumit Health
Services who
were tested for
SARS-CoV-2.
25(OH)D levels for
COVID-19 positive and
COVID-19 negative
patient
SARS-CoV2
infection
Multivariate analysis, after
controlling for the demographic
variables, and psychiatric and
somatic disorders,
demonstrated an independent
and significant association
between low 25(OH)D levels
and the increased likelihood of
COVID-19 infection [adjusted
OR of 1.50 [(95% CI: 1.13–
1.98, P < 0.001)]. Age over 50
years, male gender, and low–
medium socioeconomic status
were also positively associated
with the risk of COVID-19
infection; age over 50 years
was positively associated with
the likelihood of hospitalization
due to COVID-19.
Vitamin D and COVID-19 in children
While we did not restrict our search by age, we only identified one study in our broader search
that examined the association of vitamin D status and COVID-19 infections in children (Yılmaz &
Şen, 2020). This study examined pediatric patients with COVID-19 and found significantly lower
17
Last revised: January 7, 2021
vitamin D levels 13.14 μg/L (4.19–69.28) in COVID-19 diagnosed children (n=40) than in
healthy controls (n=45) 34.81 μg/L (3.8–77.42) (p <.001). The symptom of fever was
significantly higher in COVID-19 patients who had deficient and insufficient vitamin D levels than
in patients who had sufficient vitamin D levels (p=.038). This study did not contain any predictive
values and it should be noted that the analysis was not adjusted for any confounders.
Evidence for Vitamin D and acute respiratory tract infections
Evidence regarding acute respiratory tract infections (ARTIs) may be applicable to COVID-19. A
systematic review and meta-analysis by Martineau et al. (2017), including 25 eligible RCTs
(11,321 participants), reported that daily or weekly vitamin D supplementation reduces the risk
of ARTIs, particularly among individuals with 25(OH)D concentrations <25 nmol/L but no effect
was seen in those receiving bolus doses (of 30,000 IU of more). However, study settings,
vitamin D supplemental doses, reporting and assessment of ARTIs, and trial results were very
heterogeneous. Many of the included studies were in populations with pre-existing respiratory
disease which may limit their applicability to the general population.
The same authors have now updated their meta-analysis (Jolliffe et al., 2020; preprint) with 20
more RCTs and reported an overall protective effect of vitamin D supplementation on ARTI risk
(OR 0.91, 95% CI: 0.84 to 0.99), with heterogeneity across trials (I
2
37.2%; p=0.014). The
update did not find a protective effect of vitamin D supplementation compared to placebo in
subgroups based on baseline serum 25(OH)D concentrations. The authors identified evidence
of publication bias and downgraded the quality of the evidence to ‘moderate’.
A recent evidence review on this topic concluded, overall, that there may be some benefit from
daily, low-dose vitamin D supplementation (between 10 and 25 µg/day; 400 to 1,000 IU/day) in
reducing risk of ARTIs. However, the size of any potential benefit of vitamin D in reducing ARTI
risk may be small. [For a more extensive overview of the evidence, please refer to the available
rapid review: Vitamin D and Acute Respiratory Tract Infections
from the Scientific Advisory
Committee on Nutrition (SACN, 2020) from the UK, published Dec 17, 2020].
Synthesis of the Information Relating to Question 3
In reviewing the evidence for the association of vitamin D status with COVID-19, there appears
to be support for low vitamin D status being associated with more severe outcomes from
COVID-19. However, this is not surprising as vitamin D deficiency may represent a surrogate
marker for a general micronutrient deficiency, which in turn reflects only the patient’s overall
health status. It is not possible to confirm causality because many of the risk factors for severe
COVID‑19 outcomes are the same as the risk factors for low vitamin D status. Furthermore,
vitamin D has been found to be a negative acute phase reactant (Waldron et al., 2013),
meaning its serum concentration falls during a systemic inflammatory response, which may
occur during severe COVID-19 illness. Therefore, it is difficult to know if low vitamin D status
causes poorer outcomes or vice versa.
Many authors have hypothesized a variety of mechanisms in which vitamin D could improve the
body’s immune response to COVID-19. It has been suggested that: a) vitamin D can normalize
mitochondrial dynamics, which would improve oxidative stress, pro-inflammatory state, and
cytokine production; b) vitamin D may prevent cytokine storms by decreasing the production of
inflammatory cytokines; and c) vitamin D reduces renin–angiotensin–aldosterone system
activation and, consequently, decreases reactive oxygen species generation and improves the
prognosis of COVID-19 infection. In contrast, one study (Cereda, Bogliolo, Klersy, et al., 2020)
that failed to find an association and even reported an association with potential harm,
hypothesized that the disease could also be an example of “reversed causality” –that severe
illnesses characterized by robust inflammatory responses, like COVID-19, may be responsible

18
Last revised: January 7, 2021
for a reduction in vitamin binding proteins (due to shorter half-life) and an increase in total body
water and volume distribution volume, which, in turn, could result in the dilution of solutes, thus
low serum concentrations.
Both non-randomized “quasi-experimental” studies (C. Annweiler et al., 2020; G. Annweiler et
al., 2020) were restricted to a limited number of nursing-home residents who might be
unrepresentative of all older adults. The timing of administration of vitamin D supplementation in
the “intervention” arms was quite broad. The studies were not able to control for residual
potential confounders such as baseline serum 25(OH)D levels. There are concerns of bias in
both studies with only 9 participants in the comparator group (C. Annweiler et al., 2020), and the
control group consisting of patients who refused supplementation (G. Annweiler et al., 2020).
These studies would support the need for additional research particularly around longer-term
supplementation as “prophylaxis” rather than therapy –that is, whether being vitamin D replete is
potentially protective against more severe outcomes in the event of COVID-19 infection.
Overall, many of the studies identified to date regarding vitamin D and COVID-19 are
retrospective association studies which inherently have significant limitations. These include
concerns with the accuracy and timeframe of vitamin D status measurements, the likelihood of
confounding, the general low quality of evidence, all which contribute to a high risk of bias and
in turn, a lack of generalizability to the Alberta population.
Research Question 4
From the evidence selected, are there any subgroups of people who may benefit
from vitamin D supplementation more than the wider population of interest?
Evidence from the primary literature
There is an overlap between groups at high risk of vitamin D deficiency and groups at high risk
of severe COVID-19. Examples include people with chronic disease, older age, and people of
Black and minority ethnic heritage. It has been suggested that the higher incidence of COVID-
19 infection in older people and ethnic minorities could be partly explained by lower serum
vitamin D, which is more common in these groups. However, infants and children are at risk of
vitamin D deficiency but are not considered high-risk for severe COVID-19. In our examination
of the current evidence, we did not find any studies of sufficient quality examining particular
subgroups of people.
Synthesis of the Information Relating to Question 4
Although there was limited evidence that directly answered this research question, Health
Canada (2020) notes that the following groups may be more at risk of vitamin D deficiency:
• Infants and children aged under four years old;
• Pregnant and breastfeeding women, particularly teenagers and young women;
• People over 65;
• People who have low or no exposure to the sun, for example those living in northern
latitudes (above the 35th parallel), those who cover their skin for cultural reasons, and
those who are housebound or confined indoors for long periods;
• People with darker skin, for example people of African, Caribbean, or South Asian family
origin
Evolving Evidence
19
Last revised: January 7, 2021
Research on COVID-19 is continually evolving and as such, the evidence will continue to be
assessed as new information is provided. There is a growing evidence base on vitamin D as an
independent risk for COVID-19 infection as researchers from the various jurisdictions publish
the findings from further along the COVID-19 trajectory. There will be a need to revisit the state
of the literature and understanding on the clinical effectiveness and safety of vitamin D
supplementation for the prevention and treatment of COVID-19. Of note, there are currently 71
registered trials at clinicaltrials.gov
related to vitamin D and COVID-19. Reassessment of the
evidence may be appropriate in 6 months from now and incorporate results released from
randomized controlled trials.

20
Last revised: January 7, 2021
Appendix
List of Abbreviations
AHS: Alberta Health Services
COVID-19: Coronavirus Disease-2019
25(OH)D: serum concentrations of 25 hydroxyvitamin D
SARS-COV2 rRTPCR: severe acute respiratory syndrome coronavirus 2 real-time reverse
transcriptase–polymerase chain reaction
ICU: Intensive Care Unit
KRS: Knowledge Resource Services
SAG: Scientific Advisory Group
RCT: Randomized Controlled Trial
PICO: Population, Intervention, Comparator, Outcome (framework for literature searches)
Methods
Literature Search
A literature search was conducted by Nicole Loroff from Knowledge Resources Services (KRS) within the
Knowledge Management Department of Alberta Health Services. KRS searched databases for articles
published from June 1, 2020 until December 8, 2020 and included: OVID MEDLINE, LitCovid, PubMed,
TRIP PRO, WHO COVID-19 Database, Centre for Evidence Based Medicine (CEBM), CADTH COVID-19
Evidence Portal, COVID-Evidence medRxiv, Cochrane Library and Google Scholar. Briefly, the search
strategy involved combinations of keywords and subject headings including: vitamin d, vitamin d
deficiency ergocalciferol, calciferol, coronavirus, covid, covid 19, etc.
Articles identified by KRS in their search were initially screened by title against the identified PICO criteria
listed in Table 1 below. 182 articles were identified by KRS with references and abstracts provided for
further review. We excluded 132 articles from the review in accordance with the inclusion/exclusion
criteria stated below.
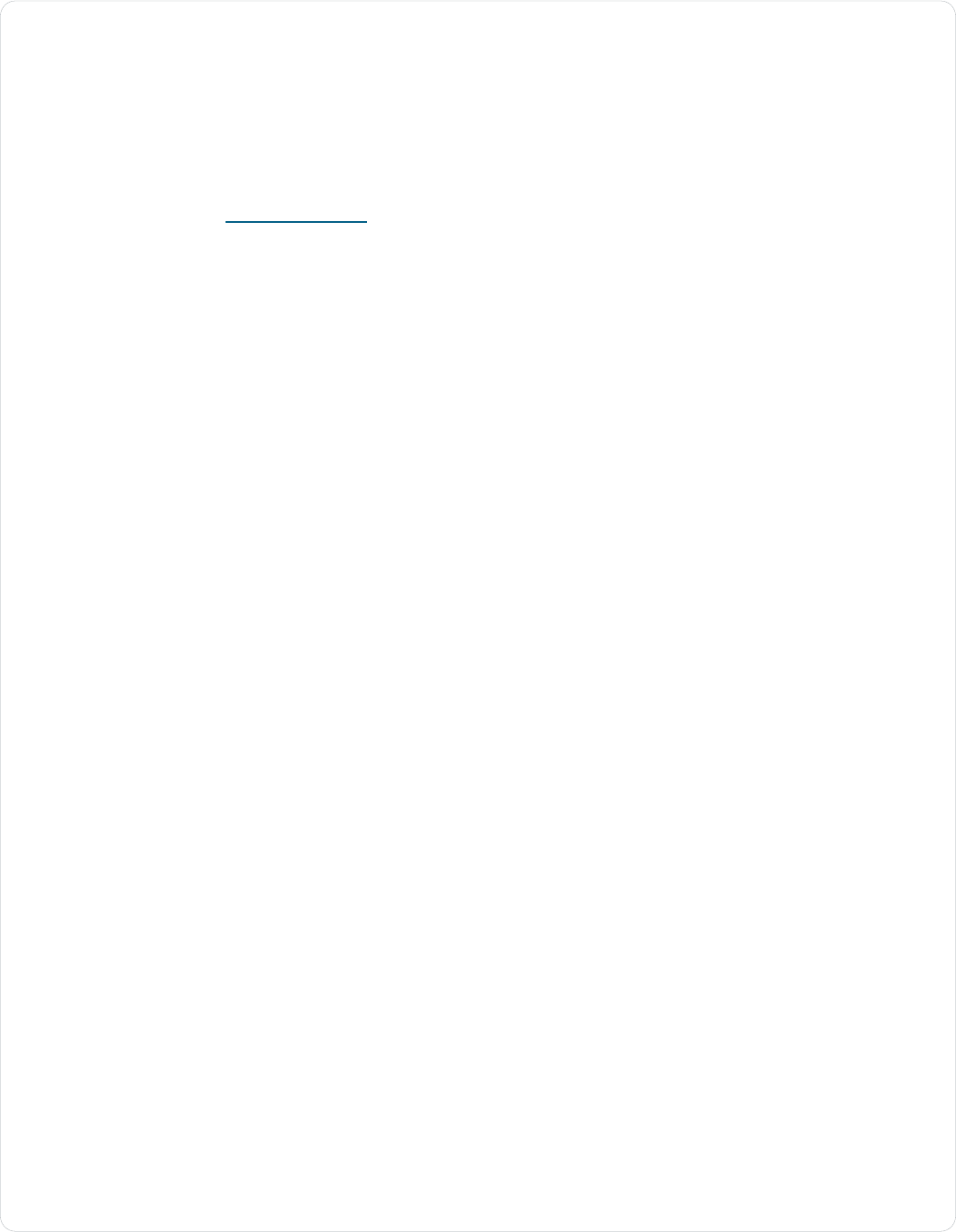
Table A1: PICO Table for Literature Review
Note: This table was adapted from National Institute for Health and Care Excellence (NICE) Vitamin D for
COVID-19 evidence review, (NICE, 2020, June).
Criteria
Details
P - Population and indication
Treatment or prevention of COVID-19, or the
susceptibility to COVID-19 infection in adults,
young people and children (or any population
subgroup)
For treatment: people with confirmed or suspected
COVID- 19 infection
For prevention: all people to prevent COVID-19
infection
21
Last revised: January 7, 2021
I – Intervention (exposure)
Vitamin D (all strengths, formulations and route of
administration) alone or in combination with other
treatments
Vitamin D status
C - Comparator(s)
Any other plausible strategy or comparator,
including placebo or no treatment
O - Outcomes
Treatment:
Critical outcomes: mortality
Important outcomes: hospitalization, ventilation,
complications, infection cure rates, time to clinical
cure, reduction in symptoms, rate of
complications, safety, tolerability and adverse
events
Prevention:
Critical outcomes: incidence of COVID-19
infection
Important outcomes: safety, tolerability,
adherence, morbidity
Table A2. Inclusion and exclusion criteria for results of the literature search
Inclusion Criteria
Exclusion Criteria
- English Language
- Human Studies Only
- All ages
- Patients with COVID-19 infection
- Systematic reviews
- Randomized controlled trials
- Interventional studies
- Controlled clinical trials
- Observational studies including case
series.
- Full-text only
- Preprints were included
- Ecological studies which used either
weather patterns (ultraviolet index) or
geographical latitude of locations as a
proxy for vitamin D alone (not measuring
vitamin D or supplementation) will not be
included
- Article is not from a credible source
- Article does not have a clear research
question or issue
- Presented data/evidence is not sufficient
to address the research questions
- Research question was unclear
- Commentary/ non-systematic reviews
Critical Evaluation of the Evidence
Exclusion criteria for study quality were adapted from the Mixed Methods Appraisal Tool (MMAT) (Hong
et al., 2018). Potential articles were evaluated on three criteria: 1) Peer reviewed or from a reputable
source; 2) Clear research question or issue; 3) Whether the presented data/evidence is appropriate to
address the research question. Preprints and non peer-reviewed literature (such as commentaries and
letters from credible journals) are not excluded out of hand due to the novelty of COVID-19 and the speed
with which new evidence is available.
Table 2 below is a narrative summary of the body of evidence included in this review. The categories,
format, and suggested information for inclusion were adapted from the Oxford Centre for Evidence-Based
Medicine, the Cochrane Library, and the AGREE Trust (Brouwers et al., 2010; Urwin, S., Gavinder, K.,
Graziadio, 2020; Viswanathan et al., 2008; Wynants et al., 2020).

22
Last revised: January 7, 2021
Table A3. Narrative overview of the literature included in this review.
Description
Volume
The literature search retrieved 182 articles from which key studies were identified
through two screening stages. The first stage involved screening the articles based
on inclusion/exclusion criteria above and narrowed the results down to 50 articles.
The second stage entailed evaluating the quality of these 50 studies based on the
Mixed Methods Appraisal Tool (Hong et al., 2018), and identifying 16 key studies
with appropriate methodological quality (3 RCTs and 12 observational) and 1
systematic review.
Among the articles identified with appropriate methodological quality, the articles
examined in this evidence review included 1 systematic review, 3 RCTs, 2
retrospective quasi-experimental studies, 2 retrospective case control study (1 was
pre-review), 4 retrospective cohort studies, 1 prospective cohort study, 1
retrospective cross-sectional study, and 2 cohort studies using Mendelian
Randomization (which were pre-review).
The jurisdictional distribution of the studies was as follows: USA (n=3), France (n=2),
and one each from Italy, Brazil, India, Israel, China, Belgium, UK, Spain, and an
International team.
No grey literature was included in this review.
Quality
The quality of the studies was assessed using the adapted MMAT (Hong et al.,
2018).
Two of the systematic reviews identified were excluded based on not being peer-
reviewed (preprints) and concerns with methodological quality. The one systematic
review (Pereira et al., 2020), was published in a peer-reviewed journal and was
higher in quality with a clear research question and appropriate methodology
following reporting guidelines. However, the meta-analysis was inappropriate with
heterogenous baseline characteristics, and the use of point estimates from studies
where some are adjusted (on different variables) and some are unadjusted
We identified 3 studies that applied vitamin D as an intervention in randomized
controlled trials. The quality of the studies warrants caution when interpreting the
results based on inappropriate randomization, lack of blinding, lack of placebo and
small sample sizes.
We identified 46 observational studies meeting our inclusion criteria. Among these,
12 were identified as key studies through our quality appraisal. Reasons for
exclusion from the final assessment were related to study quality such as lack of
statistical power (e.g. inception cohort of n <100 with very small # of events),
inappropriate or lack of adjustment for confounding, concerns with timing of exposure
measurement (i.e. vitamin D measured >10 years earlier), and lack of clarity on
methodology for vitamin D measurements. Identifying many studies of low
methodological quality is consistent with findings from the systematic review (Pereira
et al., 2020) where they reported that the methodological quality of the majority of the
included articles (74%) was identified as “high risk of bias”.
In our initial eligibility screen, we identified the majority of available studies to be
observational in design (e.g. retrospective cohort, case-control, cross-sectional, etc.)
using regression analyses to reveal relationships among variables while adjusting for
confounders. In the case of vitamin D, sicker people tend to have low vitamin D and
poorer COVID-19 outcomes. Regression analyses without any adjustments will not
infer whether vitamin D or some other variable(s) are associated with poorer COVID-
19 outcomes. Many other factors are associated both with COVID-19 outcomes and

23
Last revised: January 7, 2021
with vitamin D status, for example, obesity, ethnicity, diabetes, renal disease,
socioeconomic status, household crowding and urban place of residence. For this
reason, only studies that reported multivariable (adjusted) models for outcomes of
interest were included because at least some confounding variables are considered
in these models.
Furthermore, it is important to note that associations demonstrated in an adjusted
model do not imply that the relationships are causal. There are other factors that
could be influencing the association that were not adjusted for. Association should
not be confused with causality. This is especially important when many variables are
studied in a complex public health scenario. In this scenario, erroneous associations
can arise because the large number of factors makes it possible that an association
could be discovered by chance or collinearity. Studies on associations can be used
to form the basis for hypothesis testing for causality in randomized controlled trials.
Applicability
At the time of writing, there was no available evidence from populations in Alberta or
from the broader Canadian context. Given that different countries have had very
different levels of reported community transmission, this may influence the
associations or findings related to vitamin D. For example, there may be a higher
proportion of asymptomatic people in the comparator groups.
Many of the samples examined here are patients who have been admitted to hospital
or the ICU. Clinical decisions made with respect to admission may vary greatly by
country/jurisdiction and may change substantially over the course of the pandemic.
This may limit the generalizability of these findings to the context in hospitals in
Alberta.
It should also be reiterated that without high quality randomized controlled trial
evidence, no causal association between vitamin D deficiency and severity/outcome
of COVID-19 can be inferred.
Consistency
At this time, the available evidence is primarily observational in nature with only 3
RCTs available at this time. Two RCTS reported benefit, while one reported no
difference. More large-scale trials are needed to be able to draw conclusions.
Although many of the observational studies report an inverse association with
vitamin D deficiency and severity/complications of COVID-19, there were several
studies (Butler-Laporte et al., 2020; Cereda, Bogliolo, Klersy, et al., 2020) that found
the opposite and through their analysis, even found that higher vitamin D levels could
cause harm.
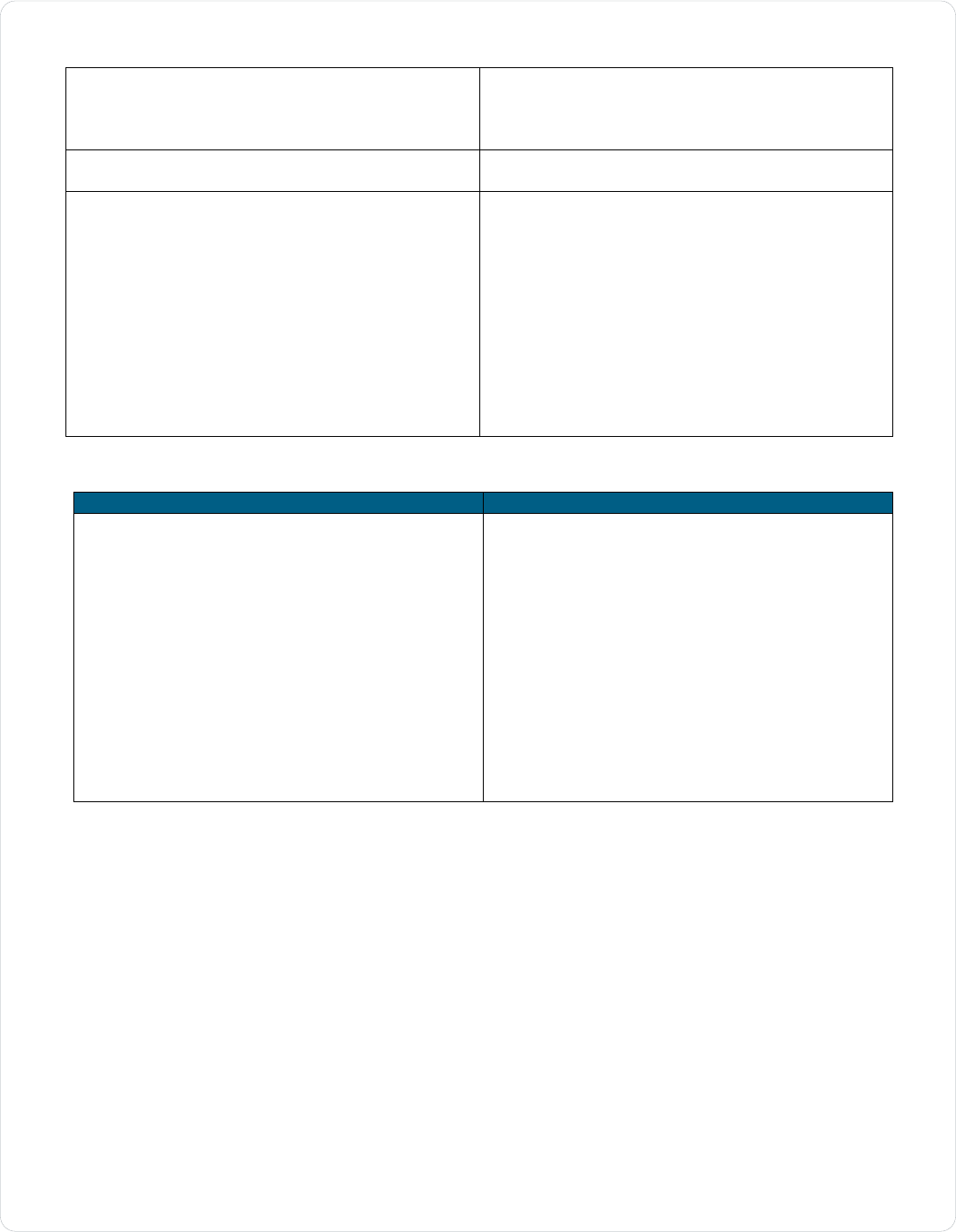
Table A4. Identified studies based on apriori inclusion/exclusion criteria (n=50)
Author
Study Design
Peer-reviewed?
(Abrishami et al., 2020)
Observational cohort
Peer-reviewed
(Arvinte, Singh, & Marik, 2020)
Observational cohort
Peer-reviewed
(Baktash et al., 2020)
Observational cohort
Peer-reviewed
(Blanch-Rubio et al., 2020)
Observational cross-sectional
Peer-reviewed
(Brenner, Holleczek, &
Schöttker, 2020)
Observational cohort
Peer-reviewed
(Butler-Laporte et al., 2020)
Cohort
(Mendelian randomization)
Preprint
(Carpagnano et al., 2020)
Observational cohort
Peer-reviewed
(Cereda, Bogliolo, Klersy, et al.,
2020)
Observational cohort
Peer-reviewed
(Cereda, Bogliolo, Lobascio, et
al., 2020)
Observational cohort
Peer-reviewed
(Chang et al., 2020)
Observational case-control
Preprint

24
Last revised: January 7, 2021
(D’avolio et al., 2020)
Observational cohort
Peer-reviewed
(Das et al., 2020)
Systematic review
Preprint
(De Smet, De Smet, Herroelen,
Gryspeerdt, & Martens, 2020)
Observational cohort
Peer-reviewed
(Faniyi et al., 2020)
Observational cohort
Preprint
(Fasano et al., 2020)
Observational cohort
Peer-reviewed
(Ferrari & Locatelli, 2020)
Observational cohort
Peer-reviewed
(Ghasemian et al., 2020)
Systematic review
Preprint
(Gonçalves et al., 2020)
Observational cross-sectional
Peer-reviewed
(Hars et al., 2020)
Observational cohort
Peer-reviewed
(Hastie et al., 2020)
Observational cohort
Peer-reviewed
(Hernández et al., 2020)
Observational case-control
Peer-reviewed
(Im et al., 2020)
Observational cohort
Peer-reviewed
(Israel et al., 2020)
Observational cohort
Preprint
(Jain et al., 2020)
Observational cohort
Peer-reviewed
(Karahan & Katkat, 2020)
Observational case-control
Peer-reviewed
(Kaufman, Niles, Kroll, Bi, &
Holick, 2020)
Observational cohort
Peer-reviewed
(Lau et al., 2020)
Observational cohort
Preprint
(Li et al., 2020)
Cohort
(Mendelian randomization)
Preprint
(Louca et al., 2020)
Observational cross-sectional
Preprint
(Luo, Liao, Shen, Li, & Cheng,
2020)
Observational cross-sectional
Peer-reviewed
(Macaya et al., 2020)
Observational case series
Peer-reviewed
(Maghbooli et al., 2020)
Observational cross-sectional
Peer-reviewed
*Note: journal has issued
expression of concern
(Mardani et al., 2020)
Observational case-control
Peer-reviewed
(Marik, Kory, & Varon, 2020)
Observational cohort
Peer-reviewed
(Meltzer et al., 2020)
Observational cohort
Peer-reviewed
(Mendy, Apewokin, Wells, &
Morrow, 2020)
Observational cohort
Preprint
(Merzon et al., 2020)
Observational case-control
Peer-reviewed
(Ohaegbulam, Swalih, Patel,
Smith, & Perrin, 2020)
Observational case series
Peer-reviewed
(Padhi, Suvankar, Panda, Pati,
& Panda, 2020)
Observational cohort
Peer-reviewed
(Panagiotou et al., 2020)
Observational cross-sectional
Peer-reviewed
(Pereira et al., 2020)
Systematic review
& meta-analysis
Peer-reviewed
(Pizzini et al., 2020)
Observational cohort
Peer-reviewed
(Pugach & Pugach, 2020)
Observational cohort
Preprint
(Radujkovic et al., 2020)
Observational cohort
Peer-reviewed
(Raharusun, Priambada,
Budiarti, Agung, & Budi, 2020)
Observational cohort
Peer-reviewed
(Raisi-Estabragh et al., 2020)
Observational cohort
Peer-reviewed
(Tomasa-Irriguible, Bielsa-
Berrocal, & Laguna, 2020)
Observational cohort
Preprint
(Tomisti et al., 2020)
Observational case-control
Preprint
(Ye et al., 2020)
Observational case-control
Peer-reviewed
(Yılmaz & Şen, 2020)
Observational cross-sectional
Peer-reviewed

25
Last revised: January 7, 2021
Search Strategy
Search strategy was partially adapted from the NICE Vitamin D for COVID-19 evidence summary, June
2020.
Citation tracking of key research was conducted in Google Scholar.
Ovid MEDLINE(R) and In-Process & Other Non-Indexed Citations and Daily 1946 to December 04,
2020
Date searched: December 7, 2020
Search strategy:
1. exp Vitamin D/ or exp Vitamin D Deficiency/ (71989)
2. ((vitamin* adj5 D*2) or vitaminD*2).tw,kf,kw. (81273)
3. (ergocalciferol* or calciferol* or vs041h42xc or dihydrotachysterol* or dihydrotachysterin* or
calcamine or 67-96-9 or r5lm3h112r or hydroxyvitamin D*2 or 25hydroxyvitamin D*2 or
hydroxyvitaminD*2 or 25hydroxyvitaminD*2 or hydroxycalciferol* or 25hydroxycalciferol* or
hydroxyergocalciferol* or 25hydroxyergocalciferol* or ercalcidiol or "25(OH)D" or 21343-40-8 or
alfacalcidol*).tw,kf,kw. (19975)
4. (cholecalciferol* or colecalciferol* or calciol or 67-97-0 or 1c6v77qf41 or hydroxycholecalciferol*
or hydroxycolecalciferol* or 25hydroxycholecalciferol* or 25hydroxycolecalciferol* or calcifediol*
or calcidiol* or "19356-17-3" or p6yz13c99q or t0wxw8f54e or dihydroxycholecalciferol* or
dihydroxycolecalciferol* or 25dihydroxycholecalciferol* or 25dihydroxycolecalciferol* or
dihydroxyvitamin D*2 or 25dihydroxyvitamin* or dihydroxyvitaminD*2 or calcitriol* or 32222-06-3
or 40013-87- 4 or 55721-11-4).tw,kf,kw. (21319)
5. or/1-4 (110112)
6. exp Coronavirus/ or exp Coronavirus Infections/ (54813)
7. (covid or coronaviru* or corona viru* or ncov* or n-cov* or novel cov* or COVID-19 or COVID19 or
COVID-2019 or COVID2019 or SARS-CoV-2 or SARSCoV-2 or SARSCoV2 or SARSCoV19 or
SARS-Cov-19 or SARSCov-19 or SARSCoV2019 or SARS-Cov-2019 or SARSCov-2019 or
"severe acute respiratory syndrome cov 2" or 2019 ncov or 2019ncov or post-covid).tw,kf,kw.
(69773)
8. or/6-7 (78492)
9. 5 and 8 (247)
10. limit 9 to english language (245)
11. limit 10 to dt=20200601-20211231 (192)
PubMed
Date searched: December 7, 2020
Search strategy:
1. "vitamin d"[MeSH Terms] or "vitamin d deficiency"[MeSH Terms] (71999)
2. "vitamin d*"[Title/Abstract] OR "vitamind*"[Title/Abstract] OR "vit d*"[Title/Abstract] (73723)
3. "ergocalciferol*"[Title/Abstract] OR "calciferol*"[Title/Abstract] OR
"dihydrotachysterol*"[Title/Abstract] OR "dihydrotachysterin*"[Title/Abstract] OR
"calcamine"[Title/Abstract] OR "hydroxyvitamin d*"[Title/Abstract] OR "25hydroxyvitamin
d*"[Title/Abstract] OR "hydroxyvitamind*"[Title/Abstract] OR "25hydroxyvitamind*"[Title/Abstract]
OR "hydroxycalciferol*"[Title/Abstract] OR "25hydroxycalciferol*"[Title/Abstract] OR
"hydroxyergocalciferol*"[Title/Abstract] OR "25hydroxyergocalciferol*"[Title/Abstract] OR
"ercalcidiol"[Title/Abstract] OR "25 oh d"[Title/Abstract] OR "alfacalcidol*"[Title/Abstract] (20479)
4. "cholecalciferol*"[Title/Abstract] OR "colecalciferol*"[Title/Abstract] OR "calciol"[Title/Abstract] OR
"hydroxycholecalciferol*"[Title/Abstract] OR "hydroxycolecalciferol*"[Title/Abstract] OR
"25hydroxycholecalciferol*"[Title/Abstract] OR "25hydroxycolecalciferol*"[Title/Abstract] OR
"calcifediol*"[Title/Abstract] OR "calcidiol*"[Title/Abstract] OR
"dihydroxycholecalciferol*"[Title/Abstract] OR "25dihydroxycholecalciferol*"[Title/Abstract] OR
"25dihydroxycolecalciferol*"[Title/Abstract] OR "25dihydroxyvitamin*"[Title/Abstract] OR
"dihydroxyvitamind*"[Title/Abstract] OR "calcitriol*"[Title/Abstract] (21123)
5. or/1-4 (102956)

26
Last revised: January 7, 2021
6. "coronavirus"[MeSH Terms] OR "coronavirus infections"[MeSH Terms] (54793)
7. "covid"[Title/Abstract] OR "coronaviru*"[Title/Abstract] OR "corona viru*"[Title/Abstract] OR
"ncov*"[Title/Abstract] OR "n cov*"[Title/Abstract] OR "novel cov*"[Title/Abstract] OR "COVID-
19"[Title/Abstract] OR "COVID19"[Title/Abstract] OR "COVID-2019"[Title/Abstract] OR
"COVID2019"[Title/Abstract] OR "SARS-CoV-2"[Title/Abstract] OR "SARSCoV-2"[Title/Abstract]
OR "SARSCoV2"[Title/Abstract] OR "SARSCoV19"[Title/Abstract] OR "SARS-Cov-
19"[Title/Abstract] OR "SARSCoV2019"[Title/Abstract] OR "SARS-Cov-2019"[Title/Abstract] OR
"severe acute respiratory syndrome cov 2"[Title/Abstract] OR "2019 ncov"[Title/Abstract] OR
"2019ncov"[Title/Abstract] OR "post-covid"[Title/Abstract] (91535)
8. or/6-7 (100196)
9. 5 and 8 (336)
10. limit 9 to english language (334)
11. limit 10 from 2020/6/1-2021/21/31 (295)
Trip Pro
Date searched: December 7, 2020
(vitamin D* or vitaminD* or vit-D* or ergocalciferol* or cholecalciferol* or calciferol* or 25 hydroxyvitamin
D* or 25hydroxyvitamin D* or 25OHD) AND (covid or coronaviru* OR "corona virus" OR ncov* OR n cov*
OR COVID-19 OR COVID19 OR COVID-2019 OR COVID2019 OR SARS-COV-2 OR SARSCOV-2 OR
SARSCOV2 OR SARSCOV19 OR SARS-COV-19 OR SARSCOV-19 OR SARSCOV2019 OR SARS-
COV-2019 OR SARSCOV-2019 OR "severe acute respiratory syndrome cov 2" OR 2019 ncov OR
2019ncov OR Hcov* or post-covid) from:2020
LitCovid/WHO COVID-19 Research Database/Centre for Evidence Based Medicine (CEBM)/CADTH
COVID-19 Evidence Portal/COVID-Evidence
Date searched: December 7 & 8, 2020
vitamin D or vitaminD or vit-D or ergocalciferol* or cholecalciferol* or calciferol* or 25 hydroxyvitamin D* or
25hydroxyvitamin D* or 25OHD
medRxiv/Cochrane Library
Date searched: December 7 & 8, 2020
“covid-19 vitamin D”; “coronavirus vitamin D”

27
Last revised: January 7, 2021
References
Abrishami, A., Dalili, N., Mohammadi Torbati, P., Asgari, R., Arab-Ahmadi, M., Behnam, B., & Sanei-
Taheri, M. (2020). Possible association of vitamin D status with lung involvement and outcome in
patients with COVID-19: A retrospective study. European Journal of Nutrition, 1–9.
https://doi.org/10.1007/s00394-020-02411-0
Alberta Medication Association, Toward Optimized Practice (2014). Vitamin D testing and
supplementation (Clinical Practice Guideline). Retrieved from
https://actt.albertadoctors.org/CPGs/Pages/Vitamin-D.aspx
Annweiler, C., Hanotte, B., Grandin de l’Eprevier, C., Sabatier, J. M., Lafaie, L., & Célarier, T. (2020).
Vitamin D and survival in COVID-19 patients: A quasi-experimental study. Journal of Steroid
Biochemistry and Molecular Biology, Vol. 204. https://doi.org/10.1016/j.jsbmb.2020.105771
Annweiler, G., Corvaisier, M., Gautier, J., Dubée, V., Legrand, E., Sacco, G., & Annweiler, C. (2020,
November). Vitamin D supplementation associated to better survival in hospitalized frail elderly
covid-19 patients: The geria-covid quasi-experimental study. Nutrients, Vol. 12, pp. 1–12.
https://doi.org/10.3390/nu12113377
Armas, L. A. G., Hollis, B. W., & Heaney, R. P. (2004). Vitamin D2 is much less effective than vitamin D3
in humans. Journal of Clinical Endocrinology and Metabolism, 89(11), 5387–5391.
https://doi.org/10.1210/jc.2004-0360
Arvinte, C., Singh, M., & Marik, P. E. (2020). Serum levels of vitamin C and vitamin D in a cohort of
critically ill COVID-19 patients of a North American Community Hospital Intensive Care Unit in May
2020: A Pilot Study. Medicine in Drug Discovery, Vol. 8, p. 100064.
https://doi.org/10.1016/j.medidd.2020.100064
Baktash, V., Hosack, T., Patel, N., Shah, S., Kandiah, P., Van Den Abbeele, K., … Missouris, C. G.
(2020). Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgraduate
Medical Journal. https://doi.org/10.1136/postgradmedj-2020-138712
Blanch-Rubio, J., Soldevila-Domenech, N., Tio, L., Llorente-Onaindia, J., Ciria-Recasens, M., Polino, L.,
… Monfort, J. (2020). Influence of anti-osteoporosis treatments on the incidence of COVID-19 in
patients with non-inflammatory rheumatic conditions. Aging, 12(20), 19923–19937.
https://doi.org/10.18632/aging.104117
Brenner, H., Holleczek, B., & Schöttker, B. (2020, August). Vitamin D insufficiency and deficiency and
mortality from respiratory diseases in a cohort of older adults: Potential for limiting the death toll
during and beyond the COVID-19 pandemic? Nutrients, Vol. 12, pp. 1–11.
https://doi.org/10.3390/nu12082488
Brouwers, M. C., Kho BHSc, M. E., Browman, G. P., Burgers, J. S., Cluzeau, F., Feder, G., … McMaster
University Brouwers, F. (2010). Analysis AGREE II: Advancing guideline development, reporting and
evaluation in health care. CMAJ • DECEMBER, 14(18), 182. https://doi.org/10.1503/cmaj.090449
Butler-Laporte et al., G. (2020). Vitamin D and covid-19 susceptibility and severity: A mendelian
randomization study. MedRxiv. Retrieved from
https://www.medrxiv.org/content/medrxiv/early/2020/09/10/2020.09.08.20190975.1.full.pdf
Carpagnano, G. E., Di Lecce, V., Quaranta, V. N., Zito, A., Buonamico, E., Capozza, E., … Resta, O.
(2020). Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory
failure due to COVID-19. Journal of Endocrinological Investigation, 1–7.
https://doi.org/10.1007/s40618-020-01370-x
Cereda, E., Bogliolo, L., Klersy, C., Lobascio, F., Masi, S., Crotti, S., … Di Terlizzi, F. (2020). Vitamin D
25OH deficiency in COVID-19 patients admitted to a tertiary referral hospital. Clinical Nutrition.
https://doi.org/10.1016/j.clnu.2020.10.055
Cereda, E., Bogliolo, L., Lobascio, F., Barichella, M., Zecchinelli, A. L., Pezzoli, G., & Caccialanza, R.
(2020). Vitamin D supplementation and outcome in COVID-19 patients from the outbreak area of
Lombardy, Italy. Nutrition, 111055. https://doi.org/10.1016/j.nut.2020.111055
Chang, T., Ding, Y., Freund, M., Johnson, R., Schwarz, T., Yabu, J., … Pasaniuc, B. (2020). Prior
diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System. MedRxiv :
The Preprint Server for Health Sciences. https://doi.org/10.1101/2020.07.03.20145581
D’avolio, A., Avataneo, V., Manca, A., Cusato, J., De Nicolò, A., Lucchini, R., … Cantù, M. (2020). 25-
hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients,

28
Last revised: January 7, 2021
12(5), 1359. https://doi.org/10.3390/nu12051359
Das, P., Samad, N., Ahinkorah, B. O., Peprah, P., Mohammed, A., & Seidu, A.-A. (2020). Effect of vitamin
D deficiency on COVID-19 status: A systematic review. MedRxiv. Retrieved from
https://www.medrxiv.org/content/medrxiv/early/2020/12/03/2020.12.01.20242313.full.pdf
De Smet, D., De Smet, K., Herroelen, P., Gryspeerdt, S., & Martens, G. A. (2020). Serum 25(OH)D level
on hospital admission associated with COVID-19 stage and mortality. American Journal of Clinical
Pathology. https://doi.org/10.1093/ajcp/aqaa252
Entrenas Castillo, M., Entrenas Costa, L. M., Vaquero Barrios, J. M., Alcalá Díaz, J. F., López Miranda,
J., Bouillon, R., & Quesada Gomez, J. M. (2020). Effect of calcifediol treatment and best available
therapy versus best available therapy on intensive care unit admission and mortality among patients
hospitalized for COVID-19: A pilot randomized clinical study. Journal of Steroid Biochemistry and
Molecular Biology, Vol. 203. https://doi.org/10.1016/j.jsbmb.2020.105751
Faniyi, A. A., Lugg, S. T., Faustini, S. E., Webster, C., Duffy, J. E., Hewison, M., … Thickett, D. R. (2020).
Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for
COVID-19 like symptoms during the 2020 pandemic. MedRxiv, 2020.10.05.20206706-
2020.10.05.20206706. Retrieved from
https://www.medrxiv.org/content/medrxiv/early/2020/10/06/2020.10.05.20206706.full.pdf
Fasano, A., Cereda, E., Barichella, M., Cassani, E., Ferri, V., Zecchinelli, A. L., & Pezzoli, G. (2020).
COVID‑19 in parkinson’s disease patients living in Lombardy, Italy. Movement Disorders. Retrieved
from https://movementdisorders.onlinelibrary.wiley.com/doi/full/10.1002/mds.28176
Ferrari, D., & Locatelli, M. (2020). No significant association between vitamin D and COVID-19. A
retrospective study from a northern Italian hospital. Horgrefe Verlag. https://doi.org/10.1024/0300-
9831/a000687
Ghasemian, R., Shamshirian, A., Heydari, K., Malekan, M., Alizadeh-Navaei, R., Ebrahimzadeh, M. A., …
Shamshirian, D. (2020). The role of vitamin D in the Age of COVID-19: A systematic review and
meta-analysis. MedRxiv. https://doi.org/10.1101/2020.06.05.20123554
Gonçalves, T. J. M., Gonçalves, S. E. A. B., Guarnieri, A., Risegato, R. C., Guimarães, M. P., de Freitas,
D. C., … Parrillo, E. F. (2020). Prevalence of obesity and hypovitaminosis D in elderly with severe
acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clinical Nutrition ESPEN, Vol. 40, pp.
110–114. https://doi.org/10.1016/j.clnesp.2020.10.008
Hars, M., Mendes, A., Serratrice, C., Herrmann, F. R., Gold, G., Graf, C., … Trombetti, A. (2020). Sex-
specific association between vitamin D deficiency and COVID-19 mortality in older patients.
Osteoporosis International : A Journal Established as Result of Cooperation between the European
Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA.
https://doi.org/https://dx.doi.org/10.1007/s00198-020-05677-6
Hastie, C. E., Mackay, D. F., Ho, F., Celis-Morales, C. A., Katikireddi, S. V., Niedzwiedz, C. L., … Gray,
S. R. (2020). Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes &
Metabolic Syndrome: Clinical Research & Reviews. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7204679/
Health Canada. (2020). Vitamin D and calcium: updated dietary reference intakes - Canada.ca. Retrieved
December 20, 2020, from
https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-
eating/vitamins-minerals/vitamin-calcium-updated-dietary-reference-intakes-nutrition.html
Hernández, J. L., Nan, D., Fernandez-Ayala, M., García-Unzueta, M., Hernández-Hernández, M. A.,
López-Hoyos, M., … Martínez-Taboada, V. M. (2020). Vitamin D status in hospitalized patients with
SARS-CoV-2 infection. The Journal of Clinical Endocrinology & Metabolism.
https://doi.org/10.1210/clinem/dgaa733
Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., … Vedel, I. (2018). The
Mixed Methods Appraisal Tool (MMAT) Version 2018 for Information Professionals and
Researchers'. Retrieved from http://mixedmethodsappraisaltoolpublic.pbworks.com/
Im, J. H., Je, Y. S., Baek, J., Chung, M. H., Kwon, H. Y., & Lee, J. S. (2020). Nutritional status of patients
with COVID-19. International Journal of Infectious Diseases, 100, 390–393.
https://doi.org/10.1016/j.ijid.2020.08.018
Institute of Medicine (IOM). (2011). Dietary Reference Intakes for Calcium and Vitamin D. In Dietary
Reference Intakes for Calcium and Vitamin D. https://doi.org/10.17226/13050
Israel, A., Cicurel, A., Feldhamer, I., Yosef Dror, B., Giveon, S. M., … Gillis, D. (2020). The link between
vitamin D deficiency and Covid-19 in a large population. MedRxiv, 2020.09.04.20188268-

29
Last revised: January 7, 2021
2020.09.04.20188268. Retrieved from
https://www.medrxiv.org/content/medrxiv/early/2020/09/07/2020.09.04.20188268.full.pdf
Jain, A., Chaurasia, R., Sengar, N. S., Singh, M., Mahor, S., & Narain, S. (2020). Analysis of vitamin D
level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory
markers. Scientific Reports, 10(1), 20191. https://doi.org/10.1038/s41598-020-77093-z
Jolliffe, D., Camargo, C. A., Sluyter, J., Aglipay, M., Aloia, J., Bergman, P., … Martineau, A. R. (2020,
November). Vitamin D supplementation to prevent acute respiratory infections: Systematic review
and meta-analysis of aggregate data from randomised controlled trials. MedRxiv, pp.
2020.07.14.20152728-2020.07.14.20152728.
https://doi.org/https://dx.doi.org/10.1101/2020.07.14.20152728
Karahan, S., & Katkat, F. (2020). Impact of Serum 25(OH) Vitamin D level on mortality in patients with
COVID-19 in Turkey. Journal of Nutrition, Health and Aging, 1–8. https://doi.org/10.1007/s12603-
020-1479-0
Kaufman, H. W., Niles, J. K., Kroll, M. H., Bi, C., & Holick, M. F. (2020). SARS-CoV-2 positivity rates
associated with circulating 25-hydroxyvitamin D levels. PLoS ONE, Vol. 15.
https://doi.org/10.1371/journal.pone.0239252
Lau, F., Majumder, R., Torabi, R., Saeg, F., Hoffman, R., Cirillo, J., & Greiffenstein, P. (2020). Vitamin D
insufficiency is prevalent in severe COVID-19. MedRxiv.
https://doi.org/10.1101/2020.04.24.20075838
Li, X., Geffen, J. van, Weele, M. van, Meng, X., ZHANG, X., He, Y., … Theodoratou, E. (2020).
Genetically-predicted vitamin D status, ambient UVB during the pandemic and COVID-19 risk in UK
Biobank: Mendelian randomisation study. MedRxiv, 2020.08.18.20177691-2020.08.18.20177691.
Retrieved from
https://www.medrxiv.org/content/medrxiv/early/2020/08/22/2020.08.18.20177691.full.pdf
Louca, P., Murray, B., Klaser, K., Graham, M. S., Mazidi, M., Leeming, E. R., … Menni, C. (2020). Dietary
supplements during the COVID-19 pandemic: insights from 1.4M users of the COVID Symptom
Study app - A longitudinal app-based community survey. MedRxiv, 2020.11.27.20239087-
2020.11.27.20239087. Retrieved from
http://medrxiv.org/content/early/2020/11/30/2020.11.27.20239087.abstract
Luo, X., Liao, Q., Shen, Y., Li, H., & Cheng, L. (2020). Vitamin D deficiency is inversely associated with
COVID-19 incidence and disease severity in Chinese people. The Journal of Nutrition.
https://doi.org/10.1093/jn/nxaa332
Macaya, F., Espejo, C., Valls, A., Fernández-Ortiz, A., González Del Castillo, J., Martín-Sánchez, F. J., …
Rubio, M. A. (2020, October). Interaction between age and vitamin d deficiency in severe covid-19
infection. Nutricion Hospitalaria, Vol. 37, pp. 1039–1042. https://doi.org/10.20960/nh.03193
Maghbooli, Z., Sahraian, M. A., Ebrahimi, M., Pazoki, M., Kafan, S., Tabriz, H. M., … Holick, M. F. (2020).
Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse
clinical outcomes in patients with COVID-19 infection. PLoS ONE, Vol. 15.
https://doi.org/10.1371/journal.pone.0239799
Mardani, R., Alamdary, A., Mousavi Nasab, S. D., Gholami, R., Ahmadi, N., & Gholami, A. (2020).
Association of vitamin D with the modulation of the disease severity in COVID-19. Virus Research,
Vol. 289. https://doi.org/10.1016/j.virusres.2020.198148
Marik, P. E., Kory, P., & Varon, J. (2020). Does vitamin D status impact mortality from SARS-CoV-2
infection? Medicine in Drug Discovery, Vol. 6, p. 100041.
https://doi.org/10.1016/j.medidd.2020.100041
Martineau, A. R., Jolliffe, D. A., Hooper, R. L., Greenberg, L., Aloia, J. F., Bergman, P., … Camargo, C. A.
(2017). Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review
and meta-analysis of individual participant data. British Medical Journal, 356.
https://doi.org/10.1136/bmj.i6583
Meltzer, D. O., Best, T. J., Zhang, H., Vokes, T., Arora, V., & Solway, J. (2020). Association of vitamin D
status and other clinical characteristics with COVID-19 test results. JAMA Network Open, 3(9),
e2019722–e2019722. https://doi.org/10.1001/jamanetworkopen.2020.19722
Mendy, A., Apewokin, S., Wells, A. A., & Morrow, A. L. (2020, June). Factors associated with
hospitalization and disease severity in a racially and ethnically diverse population of COVID-19
patients. MedRxiv : The Preprint Server for Health Sciences.
https://doi.org/10.1101/2020.06.25.20137323

30
Last revised: January 7, 2021
Merzon, E., Tworowski, D., Gorohovski, A., Vinker, S., Golan Cohen, A., Green, I., & Frenkel-
Morgenstern, M. (2020). Low plasma 25(OH) vitamin D level is associated with increased risk of
COVID-19 infection: An Israeli population-based study. FEBS Journal, 287(17), 3693–3702.
https://doi.org/10.1111/febs.15495
Murai, I. H., Fernandes, A. L., Sales, L. P., Pinto, A. J., Goessler, K. F., Duran, C. S. C., … Pereira, R. M.
R. (2020). Effect of vitamin D3 supplementation vs placebo on hospital length of stay in patients with
severe COVID-19: A multicenter, double-blind, randomized controlled trial. MedRxiv,
2020.11.16.20232397-2020.11.16.20232397. Retrieved from
http://medrxiv.org/content/early/2020/11/17/2020.11.16.20232397.abstract
National Institute for Health and Care Excellence (2020, December). Vitamin D for COVID-19 [A]
evidence reviews for the use of vitamin D supplementation as prevention and treatment of COVID-
19 (NICE guideline NG187). Retrieved from https://www.nice.org.uk/guidance/ng187/
National Institute for Health and Care Excellence (2020, June). Vitamin D for COVID-19 [A] evidence
reviews for the use of vitamin D supplementation as prevention and treatment of COVID-19 (NICE
guideline ES28).
Ohaegbulam, K. C., Swalih, M., Patel, P., Smith, M. A., & Perrin, R. (2020). Vitamin D supplementation in
COVID-19 patients: A clinical case series. American Journal of Therapeutics, Vol. 27, pp. e485–
e490. https://doi.org/10.1097/MJT.0000000000001222
Padhi, S., Suvankar, S., Panda, V. K., Pati, A., & Panda, A. K. (2020). Lower levels of vitamin D are
associated with SARS-CoV-2 infection and mortality in the Indian population: An observational
study. International Immunopharmacology, Vol. 88. https://doi.org/10.1016/j.intimp.2020.107001
Panagiotou, G., Tee, S. A., Ihsan, Y., Athar, W., Marchitelli, G., Kelly, D., … Quinton, R. (2020). Low
serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated
with greater disease severity. Clinical Endocrinology, Vol. 93, pp. 629–630.
https://doi.org/10.1111/cen.14310
Pereira, M., Dantas Damascena, A., Galvão Azevedo, L. M., de Almeida Oliveira, T., & da Mota Santana,
J. (2020). Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis. Critical
Reviews in Food Science and Nutrition, 1–9. https://doi.org/10.1080/10408398.2020.1841090
Pizzini, A., Aichner, M., Sahanic, S., Böhm, A., Egger, A., Hoermann, G., … Löffler-Ragg, J. (2020,
September). Impact of vitamin d deficiency on covid-19—A prospective analysis from the covild
registry. Nutrients, Vol. 12, pp. 1–9. https://doi.org/10.3390/nu12092775
Pugach, I., & Pugach, S. (2020). Strong correlation between prevalence of severe vitamin D deficiency
and population mortality rate from COVID-19 in Europe. MedRxiv.
https://doi.org/10.1101/2020.06.24.20138644
Radujkovic, A., Hippchen, T., Tiwari-Heckler, S., Dreher, S., Boxberger, M., & Merle, U. (2020). Vitamin D
deficiency and outcome of COVID-19 patients. Nutrients, 12(9), 1–13.
https://doi.org/10.3390/nu12092757
Raharusun, P., Priambada, S., Budiarti, C., Agung, E., & Budi, C. (2020). Patterns of COVID-19 mortality
and vitamin D: An Indonesian study. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3585561
Raisi-Estabragh, Z., McCracken, C., Bethell, M. S., Cooper, J., Cooper, C., Caulfield, M. J., … Petersen,
S. E. (2020). Greater risk of severe COVID-19 in black, asian and minority ethnic populations is not
explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status:
Study of 1326 cases from the UK biobank. Journal of Public Health (United Kingdom), Vol. 42, pp.
451–460. https://doi.org/10.1093/pubmed/fdaa095
Rastogi, A., Bhansali, A., Khare, N., Suri, V., Yaddanapudi, N., Sachdeva, N., … Malhotra, P. (2020).
Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-
controlled, study (SHADE study). Postgraduate Medical Journal. Retrieved from
https://pmj.bmj.com/content/early/2020/11/12/postgradmedj-2020-139065.full
Scientific Advisory Committee on Nutrition (2020). Update of rapid review: vitamin D and acute respiratory
tract infections. Retrieved from https://www.bmj.com/content/369/bmj.m1328.long
Tomasa-Irriguible, T.-M., Bielsa-Berrocal, L., & Laguna, L. B. (2020). Up to 40% of COVID-19 critically ill
patients have vitamin D deficiency. Retrieved from
https://www.preprints.org/manuscript/202009.0555/v1
Tomisti, L., Pulizzi, N., Pafundi, P. C., Macaro, D., Villari, L., Latorre, M., … Parri, G. (2020). Comparison
Of The 25oh-vitamin D levels between old patients hospitalized for Sars-cov-2 pneumonia and
patients with other acute illnesses: A retrospective case-control study. Retrieved from

31
Last revised: January 7, 2021
https://assets.researchsquare.com/files/rs-96491/v1_stamped.pdf
Urwin, S., Gavinder, K., Graziadio, S. (2020). What prognostic clinical risk prediction scores for COVID-19
are currently available for use in the community setting? Centre for Evidence-Based Medicine.
Viswanathan, M., Ansari, M. T., Berkman, N. D., Chang, S., Hartling, L., McPheeters, M., … Treadwell, J.
R. (2008). Assessing the risk of bias of individual studies in systematic reviews of health care
interventions. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Retrieved
from http://www.ncbi.nlm.nih.gov/pubmed/22479713
Waldron, J. L., Ashby, H. L., Cornes, M. P., Bechervaise, J., Razavi, C., Thomas, O. L., … Gama, R.
(2013). Vitamin D: A negative acute phase reactant. Journal of Clinical Pathology, 66(7), 620–622.
https://doi.org/10.1136/jclinpath-2012-201301
Webb, A.R., Kline, L., Holick, M.F. (1988). Influence of Season and Latitude on the Cutaneous Synthesis
of Vitamin D
3
: Exposure to Winter Sunlight in Boston and Edmonton Will Not Promote Vitamin
D
3
Synthesis in Human Skin, The Journal of Clinical Endocrinology & Metabolism, 67(2), 373–378.
Wynants, L., Van Calster, B., Collins, G. S., Riley, R. D., Heinze, G., Schuit, E., … Van Smeden, M.
(2020). Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical
appraisal. British Medical Journal, 7, 18. https://doi.org/10.1136/bmj.m1328
Ye, K., Tang, F., Liao, X., Shaw, B. A., Deng, M., Huang, G., … Yang, J. (2020). Does serum vitamin D
level affect COVID-19 infection and its severity?-A case-control study. Journal of the American
College of Nutrition, 1–8. https://doi.org/10.1080/07315724.2020.1826005
Yılmaz, K., & Şen, V. (2020). Is vitamin D deficiency a risk factor for COVID-19 in children? Pediatric
Pulmonology, Vol. 55, pp. 3595–3601. https://doi.org/10.1002/ppul.25106
