
Page 1 of 26
Title:
RAPID EVIDENCE SUMMARY:
VITAMIN D IN COVID-19
Author: CMO Office, Louise Hendrick
Organisation: Department of Health
Date: 27
th
January 2021
Action required:
☐ For noting
☐ For discussion
☒ For decision
Approved for future publication: YES
Version
1.0

Page 2 of 26
RAPID EVIDENCE SUMMARY: VITAMIN D IN COVID-19
24 JANUARY 2021
INTRODUCTION
▪ National Department of Health guidelines on vitamin D were updated in November
2020 and advise adults aged 65 and older to take a daily vitamin D supplement of 15
micrograms to support bone and muscle health.
▪ In the context of COVID-19, advice has previously issued recommending that
individuals that are self-isolating or unable to go outside should consider
supplementation.
▪ This rapid review was conducted to assess current evidence on the role of vitamin D in
the prevention and treatment of COVID-19 and additional considerations which may
impact decision-making.
▪ This review of the available research evidence up to January 2021 considers recent
rapid reviews, randomised controlled trial (RCT) evidence, observational studies and
laboratory studies.
o A recently updated rapid review conducted by the National Institute for
Health and Care Excellence (NICE) in the UK concluded that there is
currently a lack of evidence linking vitamin D and the incidence and severity
of COVID-19. The report recommends increasing awareness of existing
recommendations relating to vitamin D supplementation.
o Results from a randomised controlled trial (Entrenas Castillo, 2020)
reported reduced admission to ICU and reduced mortality in patients with
COVID-19 receiving standard care plus vitamin D compared to standard care
alone. However, this trial was noted to have significant methodological
limitations including low numbers (n=76) and serious risk of bias.
o Collectively, other evidence provides conflicting reports of an association
between vitamin D supplementation and a reduced risk of and poorer
outcomes with COVID-19 infection.
o A number of studies have suggested an association between low vitamin D
status and increased incidence and severity of COVID-19 infection.
However, causality has not been confirmed as many of the risk factors for
severe COVID-19 outcomes are the same as the risk factors for low vitamin
D status.
▪ Additional considerations outlined within the report include:
o Modest evidence to suggest that vitamin D may slightly reduce the risk of
acute respiratory illness.

Page 3 of 26
o Existing evidence of vitamin D deficiency in Ireland with TILDA results showing
that 13.1% of adults over 55 are deficient all year round, rising to 21.3% in
winter. Higher levels of deficiency have been reported in those aged 70+
(27.1%) and 85+ (46.6%) in winter, with 11.5% of those aged 70+ reported
taking a vitamin D supplementation. A cross-sectional study also reported
high levels of deficiency in Irish individuals of South Asian descent (66.7% had
vitamin D levels ≤30 nmol/L).
o International public health guidance typically recommends optimisation of
vitamin D status in the context of bone and muscle health. Several countries
have reiterated existing guidance given increased time spent indoors due to
COVID-19 restrictions (England, Scotland, Wales, Northern Ireland, Slovenia,
France).
o England and Scotland have recently launched an opt-in scheme offering a
free 4-month supply of vitamin D supplements for those listed as extremely
clinically vulnerable.
▪ There is insufficient high-quality evidence to support a change to existing guidance,
however this report makes the following recommendations:
o Increase awareness of existing guidance that adults age 65 and over should
take a 15 microgram daily supplement for bone and muscle health
o Adults spending increased time indoors or are housebound or in long-term
residential care or have dark skin are also recommended to take vitamin D
supplementation
o That ongoing developments, particularly RCTs, in this area be monitored
with guidance reviewed accordingly
BACKGROUND
This rapid review was conducted to assess the following question:
“What is the current evidence in relation to the role of vitamin D in prevention and
treatment of COVID-19?”
The potential role of vitamin D in the prevention and treatment of COVID-19 has been
proposed based on:
• Systematic reviews and meta-analyses showing a reduced risk of acute respiratory
tract illness with vitamin D supplementation.
• In vitro studies showing the role of vitamin D in induction of antimicrobial peptides in
response to both viral and bacterial stimuli,
1
2
and have demonstrated the
responsiveness of several hundred genes to vitamin D, including activated T cells, B
cells, dendritic cells and macrophages (immune cells).
3

Page 4 of 26
• A number of observational studies that have highlighted the relationship between UVB
exposure,
4
vitamin D supplementation,
5
6
vitamin D serum levels
7
and deficiency
8
and
COVID-19 incidence and outcomes.
Vitamin D is a group of fat-soluble seco-sterols. Vitamin D is obtained through synthesis in the
skin from 7-dehydrocholesterol under the influence of ultraviolet-B (UVB) light and through
the consumption of vitamin D-rich foods. Vitamin D is metabolised first to 25-hydroxyvitamin
D (25[OH]D), then to the bioactive form 1,25-dihydroxyvitamin D.
9
The classic function of
vitamin D is in the regulation of calcium absorption and homeostasis, supporting
musculoskeletal health. Deficiency which is typically defined as serum 25[OH]D levels
<25nmol/L, is associated with osteomalacia, low bone mass, fractures, muscle weakness,
increased risk of falls; and rickets in children.
10
11
12
Research suggests that vitamin D may also
play a role in immunity owing to the existence of vitamin D receptors on multiple different cell
types including immune cells, and studies showing an association between autoimmune
disease and vitamin D deficiency.
13
Ireland resides at the latitude band of 51–55°N resulting in a 5-month period from October to
February during which UVB-induced dermal synthesis of vitamin D does not occur and thus
supplementation is recommended in certain groups.
14
15
Characteristics, such as skin
pigmentation, age, clothing style, sunscreen use, outdoor activity and sun exposure behaviour
influence vitamin D status,
16
with deficiency more common in individuals that are
institutionalised, elderly, obese and with dark skin.
17
EXISTING GUIDELINES
Existing guidelines on vitamin D encompass recommendations for infants aged 0 to 12
months; children aged 1 to 4 years and adults aged 65 years and older.
Since 2010 the HSE has recommended a 5 microgram (5μg) daily vitamin D supplement in liquid
or drop form babies for babies from birth to 12 months.
18
The initial guidance followed a 2007
review by the FSAI’s Scientific Committee which highlighted the re-emergence of rickets in
infants in Ireland with 23 cases reported in the early 2000s at two Dublin-based paediatric
hospitals.
19
This guidance was updated in 2020 limiting this recommendation to babies that
are breastfed or taking less than 300mls of infant formula a day,
20
reflecting the European
Food Safety Authority’s approval of increased vitamin D levels in fortified infant formula
21
and
subsequent FSAI recommendation.
22
In October 2020 the Department of Health issued guidance recommending a 5 microgram
(5μg) vitamin D only supplement in liquid or drop form to be taken daily from Halloween (31st
October) to St Patrick’s Day (17th March) in children from one to four years (inclusive).
23

Page 5 of 26
In November 2020 the Department of Health issued guidance advising adults aged 65 and older
to take a daily vitamin D supplement of 15 micrograms (15μg), either as a multivitamin, a
vitamin D-calcium combination or as a vitamin D only supplement, to support bone and muscle
health.
24
The guidance also recommends a diet with regular intakes of natural sources of
vitamin D, such as oily fish, eggs, meats and vitamin D-fortified. This follows a 2020 FSAI report,
on vitamin D and older adults, recommending that healthy older adults living independently
and who get sunlight exposure during summer should take 10μg (400 IU) daily dose during the
extended winter months (end of October to March); and for those of darker-skinned ethnicity,
this should be taken throughout the full year. The report recommends a 15µg (600 IU) daily
dose for housebound older adults with minimal or no sunlight exposure taken throughout the
full year. The report notes that such dosing should be sufficient and safe for most older
people.
25
METHODOLOGY
This rapid review aimed to provide a high-level summary of the evidence on vitamin D and
COVID-19. A scoping methodology was used and considered research evidence on vitamin D
status and prevention of SARS-CoV-2 infection; vitamin D supplementation and COVID-19
outcomes; vitamin D status and prevention of acute respiratory illness, and public health
guidance and measures. The research evidence cited includes literature up to 22
nd
January
2021.
REVIEW OF EVIDENCE FOR THE EFFECTIVENESS OF THE USE OF VITAMIN D IN THE
PREVENTION OF COVID-19
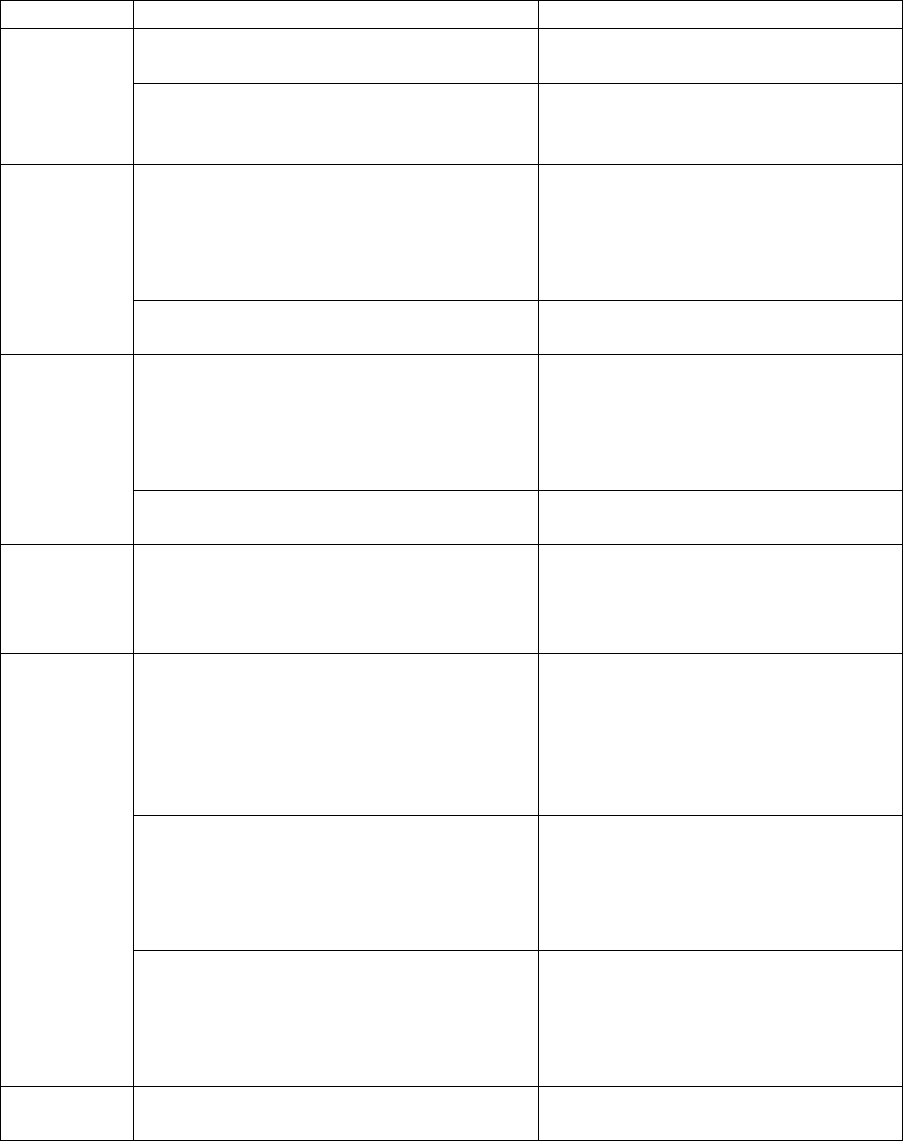
Search Results
Due to the limited time available for the completion of this rapid report, a scoping approach
was adopted to identify relevant studies published. The following table presents examples of
research studies identified, which are discussed under the relevant section.
Sample articles identified
Publication date
Rapid review
informing
national policy
NICE rapid review: Vitamin D for
COVID-19
26
December 2020
Systematic
Reviews
Yisak et al. Effects of Vitamin D on
COVID-19 Infection and Prognosis: A
Systematic Review
January 2021
Randomised
controlled trials
Entrenas Castillo et al. vitamin D
supplementation in the treatment of
COVID-19
October 2020

Page 6 of 26
Observational
studies
Hastie C et al. Vitamin D
concentrations and COVID-19 infection
in UK Biobank
April 2020
Laboratory
studies
McCarthy et al. Immuno-protection
against COVID-19
April 2020
National Institute for Health and Care Excellence (NICE) COVID-19 Rapid Guideline:
Vitamin D
The most up-to-date review of the evidence identified within this review comprises a rapid
review performed by the NICE in the UK, which was published on 17 December 2020. The
results of this rapid review are described below.
This review was performed to inform a policy recommendation based on three questions:
“What is the clinical effectiveness and safety of vitamin D supplementation for the
treatment of COVID-19 in adults, young people and children?”
“What is the clinical effectiveness and safety of vitamin D supplementation for the
prevention of SARS CoV2 infection (and subsequent COVID-19) in adults, young
people and children?”
“Is vitamin D status independently associated with susceptibility to developing COVID-
19, severity of COVID-19, and poorer outcomes from COVID-19 in adults, young
people and children?”
This review considered the following outcomes of interest:
▪ Incidence of COVID-19
▪ COVID-19-related ICU admission
▪ All-cause and COVID-19-related mortality
▪ Hospitalisation; ventilation; time to cure; complications; adverse effects and
tolerability
Overall, the categories of research incorporated in the review included: direct evidence
reporting multivariable models for outcomes of interest, systematic reviews and meta-
analyses of Randomised Control Trials (RCTs), observational studies and laboratory studies.
Pre-print research (not peer-reviewed) was included.
With respect to evidence for vitamin D supplementation in the treatment of COVID-19, one
RCT by Entrenas Castillo et al was included. This study reported a lower likelihood (OR 0.03,
95% CI 0.003-0.25) of admission to ICU in those receiving calcifediol treatment plus standard
care compared to those receiving standard care alone. However, the evidence quality was
deemed very low due to a very serious of bias and low number of participants (n=76).
27
Page 7 of 26
With respect to evidence for vitamin D supplementation in the prevention of COVID-19, no
articles were identified following review.
With respect to the evidence for an association between vitamin D status and COVID-19
susceptibility and severity 12 studies were included. Six studies explored the association
between vitamin D status and COVID-19 incidence. Results were mixed with one study
reporting a significant association between vitamin D concentration and risk of COVID-19
diagnosis (OR 0.984, 95% CI 0.983, 0.986, N=191,779)
28
; and two studies reporting no
association ((OR 1.00, 95% CI 0.998, 1.01, N=349,017)
29
and (OR 1.00, 95% CI 1.00, 1.00,
N=4,510)
30
) between vitamin D status and COVID-19 cases. The latter two studies utilised
serum vitamin D measurements from the UK biobank study which were collected between
2006 and 2010, which may differ from the populations included in the analysis.
Three studies assessed vitamin D deficiency and COVID-19 diagnosis. Two reported an
association with Meltzer et al reported an association between deficiency (˂25nmol/L) and
COVID-19 cases OR 1.77 (95% CI 1.12, 2.81)
31
and Merzon et al. reporting an association
between suboptimal levels (˂75nmol/L) and COVID cases OR 1.5 (95% CI 1.13 to 1.98)
32
. The
former did not adjust for demographic factors (e.g. sex, gender, ethnicity). An additional study
found no difference in COVID-19 cases between people above and below the thresholds,
˂25nmol/L OR 0.92 (95% CI 0.71, 1.21) and ˂ 50nmol/L OR 0.88 (95% CI 0.72, 1.08)²⁹. The
quality of all studies was graded as very low with criticism of methodological approach relating
to a failure to adjust for confounding variables (including sex, gender and ethnicity); use of UK
Biobank data (based on vitamin D measurements taken between 2006 and 2010); and lack of
power.
Seven studies assessed vitamin D status and an association with COVID-19 severity. Hernandez
et al. did not identify an association between vitamin D levels and ICU admission, need for
mechanical ventilation or in-hospital mortality OR 1.13 (95% CI 0.27, 4.77) n=197
33
. Macaya et
al. did not find an association between vitamin D levels (<50nmol/L) and death, ICU admission
or need for high-flow oxygen OR 3.2 (95% CI 0.99 to 11.4)
34
. A third study reported a significant
association between low vitamin D levels (<30nmol/L) and the composite outcome mechanical
ventilation and death, HR 6.12 (95% CI 2.79 to 13.42), n=185.
35
Ye et al. also reported an
association between vitamin D levels <50nmol/L and more severe COVID-19, OR 15.18 (95% CI
1.23, 187.45).
36
Annweiler et al. reported the results of two quasi-experimental studies, and found that
supplementation for a year was significantly negatively associated with the likelihood of severe

Page 8 of 26
COVID-19, OR 0.08 (95% CI 0.01, 0.81), but identified no difference if those only receiving a
bolus when diagnosed, OR 0.46 (95% CI 0.07, 2.85). These studies also reported on mortality
as a single outcome with one study reporting lower mortality risk in those receiving vitamin D3
bolus supplementation during COVID-19 or in the preceding month compared to those
receiving no treatment (Hazard ratio (HR) = 0.11 [95 %CI 0.03, 0.48], p = 0.003),⁶ and a second
study of 77 patients hospitalised with COVID-19 reported a higher risk of 14-day mortality in
those receiving no supplementation compared to those receiving supplementation in the
preceding year (HR = 0.07 (p = 0.017)) or those supplemented after a COVID-19 diagnosis (HR
= 0.37 (p = 0.28)).
37
Both studies had limitations including small sample size, lack of use of a
placebo, and use of estimations of vitamin D status based on supplementation which rely on
compliance and thus may be incorrect.
A further two studies reported on vitamin D status and mortality with Karahan et al. finding
that higher vitamin D levels were negatively associated with death OR 0.92 (95% CI 0.88, 0.98)²⁸
and Radujkovic et al. reporting higher mortality with serum vitamin D levels <30nmol/L (HR
14.73 (95% CI 4.16, 52.19)).³⁵
The review excluded numerous observational studies due to the use of unadjusted analysis
and a lack of relevant predictive values.
Taking into consideration all forms of evidence, the recommendations of this review were:
▪ A lack of evidence supporting the use of vitamin D in the treatment of COVID-19
▪ A lack of evidence supporting the use of vitamin D in the prevention of COVID-19
▪ A lack of evidence supporting an association between vitamin D status and the
incidence of COVID-19
▪ A call for urgent research into vitamin D supplementation and prevention of COVID-
19, particularly in Black African and Minority Ethnic (BAME) individuals, and people
categorised as overweight or obese.
Systematic Review
Yisak et al conducted a review of 9 articles and identified 7 studies that reported a correlation
between vitamin D status and COVID-19 infection, prognosis and mortality. 2 studies failed to
demonstrate an association. This review did not address the limitations of included studies
including unadjusted analysis and an absence of relevant predictive values.
38
Randomised Control Trials

Page 9 of 26
A pre-publication (not peer reviewed) Brazilian, multicentre, double-blind, RCT randomised
patients with 240 hospitalised patients with COVID-19 (1:1) to receive a single oral dose of
200,000 IU (5,000mcg) or placebo. 86.7% of patients in the supplementation arm achieved
vitamin D serum levels (≥30ng/mL) compared to 11% in the placebo group; however there was
no difference in hospital length of stay in vitamin D and placebo groups (7.0 days [95% CI 6.1,
7.9] and 7.0 days [95% CI 6.2, 7.8 days], HR 1.12, [95% CI 0.9, 1.5]; p = .379) respectively. There
was also no difference reported in secondary outcomes including mortality, admission to ICU
and requirement for ventilation. Study limitations include low power, and heterogeneity of the
patient sample and its treatment.
39
Rapid Review of evidence for use of vitamin D in the prevention of Acute Respiratory
Illness
Systematic Reviews and Meta-Analyses
Seven systematic reviews and meta-analyses were identified that assessed the role of vitamin
D in the prevention of acute respiratory illness. These suggest a modest reduced risk of acute
respiratory tract infection and asthma exacerbation due to respiratory tract infection with
vitamin D supplementation.
In a 2017 systematic review and meta-analysis of 25 RCTs, Martineau et al. identified patient
data for 10,933 (96.6%) of 11,321 participants aged 0 to 95 years.
40
Vitamin D supplementation
reduced the risk of acute respiratory tract infection among all participants (adjusted OR 0.88,
95% CI 0.81 to 0.96; P for heterogeneity <0.001). Protective effects were seen with daily or
weekly dosing between 20μg and 50μg (adjusted OR 0.81, 0.72 to 0.91) with stronger effects
in those with baseline deficiency defined as serum 25[OH]D levels<25 nmol/L (adjusted OR
0.30, 0.17 to 0.53). No effect was seen with bolus dosing and no reduction in adverse events
was observed.
A 2020 pre-publication, non-peer reviewed systematic review of 45 RCTs conducted by Joliffe
et al. reported patient data for 46,331 (98%) of 47,262 individuals in 42 trials (in total 73,384
patients were involved in 45 trials).
41
The study reported a reduced risk of acute respiratory
tract infection overall in those receiving vitamin d supplements vs placebo (OR 0.91, 95% CI
0.84, 0.99; P for heterogeneity 0.01). No statistically significant effect of vitamin D was seen
for any of the sub-groups defined by baseline 25[OH]D concentration. Protective effects were
seen in trials using daily dosing regimen (OR 0.75, 95% CI 0.61, 0.93) at daily dose equivalents
of 10 micrograms to 25 micrograms or 400 to 1000 IU, but not above (OR 0.70, 95% CI 0.55,
0.89); and for a duration of ≤12 months (OR 0.82, 95% CI 0.72, 0.94). There was no impact of
supplementation on adverse events. Limitations of this research included inconsistency
between study results, and differences between vitamin D supplementation doses and
regimens, durations, populations, settings and definition of outcomes, between studies.

Page 10 of 26
A 2021 systematic review and meta-analysis on micronutrient supplementation reported a
reduced the risk of ARI (risk ratio (RR)=0.97; 95% CI 0.94 to 1.00; p=0.028) based on 20 studies
and shortened the duration of symptoms (per cent difference: −6% (95% CI −9% to −2%;
p=0.003)), with an optimal dosing regimen proposed as daily dose ≥2000 IU (50mcg) vitamin D
and a <60000IU (1500mcg) loading dose.
42
A 2016 systematic review and meta-analysis of 15 RCTs reported patient data for 7,053
individuals and failed to demonstrate a statistically significant association between vitamin D
supplementation and risk of clinical respiratory tract infection (RR 0.94; 95% CI 0.88, 1.00).
43
Similarly, Wang et al. reported data for 2312 healthy participants aged 19 to 61 years in 8 RCTs
and reported no different between vitamin D and placebo groups in risk of self-reported cold,
cold duration and cold severity.
44
Additionally, included studies differed with respect to
population, baseline vitamin D levels and study length.
A 2015 systematic review of 7 RCTs in those aged 18 or younger found insufficient evidence
supporting vitamin D supplementation and reduction of acute respiratory illness (relative risk
(RR) 0·79, 95%CI 0·55, 1·13), all-cause mortality (RR 1·18, 95% CI 0·71, 1·94), or the rate of
hospital admission due to respiratory infection in healthy children (RR 0·95, 95% CI 0·72, 1·26),
however this study did identify a reduction in the risk of asthma exacerbation due to acute
respiratory illness with vitamin D supplementation (RR 0·26, 95% CI 0·11, 0·59).
45
A 2019
systematic review and meta-analysis incorporating patient data from 7 RCTs and 955
participants reported an overall reduction in the rate of asthma exacerbations requiring
treatment with systemic corticosteroids with vitamin D supplementation.
46
A systematic review on non-skeletal effects of Vitamin D found that those with low levels are
underrepresented in RCTs (inclusion criteria in 67 of 210 RCTs),
47
with a systematic review of
83 trials noting the poor quality of many meta-analyses.
48
Randomised Control Trials
Two randomised, double-blind, placebo-controlled clinical trials were identified that evaluated
the administration high dose vitamin D to critically ill patients with vitamin D deficiency (but
not COVID-19). A phase 3 trial of 1360 patients reported no difference in 90-day mortality in
those receiving early administration of high-dose enteral vitamin D (mortality difference, 2.9%;
95%CI, -2.1-7.9%; P = 0.26).
49
The VITdAL-ICU is the largest published ICU-based RCT on vitamin
D supplementation to date. This single-centre study was conducted from May 2010 through
September 2012 at 5 ICUs. 492 adult white patients with Vitamin D deficiency (≤20 ng/mL)
were randomised to receive high-dose vitamin D
3
or placebo over a 5-month period. The study
showed no reduction in hospital length of stay, hospital mortality, or 6-month mortality. Lower
hospital mortality was observed in a severely deficient subgroup and requires further study.
50
Multiple RCTs, included in the systematic reviews and meta-analysis discussed above, show
conflicting evidence on vitamin D and prevention of acute respiratory illness.
51
52
53

Page 11 of 26
Laboratory Studies
Several laboratory-based simulation studies, or, mechanistic studies, have been published
which demonstrate a role for vitamin D in the induction of antimicrobial peptides in response
to both viral and bacterial stimuli. ¹ ²
54
A possible mechanism proposed to explain the
association between vitamin D deficiency and poor COVID-19 outcome is that correction of
vitamin D deficiency may suppress CD26, reducing adhesion of COVID‐19; in addition to
attenuation of interferon gamma and interleukin-6 inflammatory responses which are
predictors of poorer outcome in critically-ill ventilated patients including those with COVID‐
19.
55
It is important to note that vitamin D is a negative acute phase reactant i.e. serum levels fall in
response to acute stress response, therefore single sample 25-OHD levels during critical illness
may provide an inaccurate assessment of vitamin D status due to several confounders including
albumin levels, interstitial extravasation, decreased synthesis of binding proteins, and renal
wasting of 25-hydroxyvitamin D.
56
Conclusions on the evidence
• Significant limitations with existing research were identified:
o Systematic reviews and meta-analysis identified large heterogeneity and poor
study quality;
o Association studies included use of historic and inaccurate vitamin D status
measurements, lack of generalisability, high likelihood of confounding or
failure to adjust for confounders and general low quality of the evidence.
• There is no data from interventional trials showing that vitamin D supplementation may
prevent COVID‐19.
57
• Circumstantial evidence linking COVID-19 outcomes and Vitamin D status has led to
some supporting supplementation in vulnerable populations given safety profile and
low risk of harm
58
59
Evidence review: additional considerations
Several studies have estimated the prevalence of vitamin D deficiency in the Irish population.
The National Adult Nutrition Survey sampled of 1132 adults between October 2008 and April
2010. This representative survey found 35.7% of adults aged 50-64 years, and 44.0% of adults
aged 65-84 years had serum vitamin D levels less than 50nmol/l on a year-round basis, with
these figures increasing to 55.4% and 48.1% respectively in winter. This study also assessed
dietary intake of vitamin D and reported the mean daily intakes of vitamin D from diet and
supplements was 5.2μg for men and 8.5μg for women (≥65 years), and 27% of both men and
women regularly consumed a nutritional supplement containing vitamin D (males: 21%;
females: 32%). Mean daily intake of vitamin D from natural foods was 3.6μg and increased to

Page 12 of 26
4.7μg when the contribution of fortified foods was included. Fish, meats, eggs, and vitamin D-
fortified foods contributed 23%, 19%, 7% and 17%, respectively.
60
Results from the Irish Longitudinal Study on Ageing (TILDA) measured 25-hydroxyvitamin D
levels in 5,356 adults over 50 years of age. The prevalence of deficiency (25OHD < 30 nmol/L)
was 13.1% (95% CI: 12.1–14.2), with higher prevalence in winter, in smokers, in obese adults,
the physically inactive, those living alone, and in those over 80 years. Through extrapolation
they estimate that 1 in 8 (13%, 149,049) adults over 55 are deficient all year round;; 21.3%
(244,209) adults over 55 are deficient in winter; 27%.1 (115,536) of Irish adults over 70 that
were ‘cocooning’ in the springtime in 2020 are deficient and 46.6% (31,480) of all adults aged
>85 are deficient in winter. The report also identified that 9.4% (107,773) of those aged 55+
and 11.5% (49,028) of those aged 70+ reported taking a vitamin D supplement during winter.
61
62
A cross-sectional study of 186 individuals of South East Asian descent between 2013 and 2016
found that 66.7% had vitamin D levels ≤30 nmol/L (i.e. deficient) and 6.7% had levels ≥50
nmol/L (the 25(OH)D concentration defined by the EU as ‘sufficient’). Whilst average levels
were higher in females than males (25.0 vs. 18.0 nmol/L; p = 0.001) both groups had a
significant proportion with deficient status (56% and 76.8%, respectively).
63
A cross-sectional study assessed 24,302 eligible patient samples processed through University
Hospital Galway between January 2011 and December 2015. They reported vitamin D
deficiency was more common in nursing home residents compared to inpatients, outpatient
clinic patients or community-based patients (42% vs 37% vs 17% vs 13%; p < .001). Inpatients
with a LOS (≥3 days) had greater Vitamin D deficiency than those with LOS ≤2 days (p = .007).
Vitamin D deficiency was more common in Winter/Spring, in males, and in those aged ≥80
years.
64
Three Irish studies have demonstrated that daily 20µg vitamin D supplementation of
at least 10 weeks duration is sufficient to correct deficiency in nursing home residents
65
and
adults aged 50 and over.
66
67
A prospective cross-sectional study of healthy children attending the Children’s University
Hospital for elective surgery (26%), medical outpatients (62%), or the emergency department
(12%) for a minor complaint conducted from March 2010 to March 2011 found that of 252
children aged 1 to 17 years 21.9% had 25OHD levels <30 nmol/L, 32.7% were between 30 and
50 nmol/L, and 45.4% had levels >50 nmol/L. Higher levels were associated with younger age
(<4 years) and April-September sampling.
68
Recent review articles cited the high prevalence of
low vitamin D levels (25[OH]D<30nmol/L) in preterm infants and (25OHD<50nmol/L) in older
adults, hospital inpatients and nursing home residents, along with the potential anti-
inflammatory and immunomodulatory properties of Vitamin D as justification for ensuring
baseline Vitamin D sufficiency for potential enhancement of immune-protection against
CoVID-19.
69
70

Page 13 of 26
International Measures: England and Scotland
From January 2020 the Department of Health and Social Care in the UK are operating a 4-
month opt-in scheme for extremely clinically vulnerable people to receive a supply of daily
vitamin D supplements, this includes nursing home residents (Appendix A).
71
This follows a
Scottish initiative offering a free 4-month supply of daily vitamin D supplements to everyone
on the shielding list (Appendix B). Pregnant women, breastfeeding women and children under
12 months are already eligible for free supplements.
72
This followed the NICE rapid review
previously referred to which reported insufficient evidence supporting a benefit of vitamin D
supplementation in relation to COVID-19 prevention or response but advised supplementation
during winter due to increased time indoors and proven bone and muscle health benefits
(Appendix C). The NICE review recommended a 10μg (400 IU) dose per day or 25μg (1000IU)
if 10mcg unavailable. The review acknowledged that low vitamin D status was associated with
more severe outcomes from COVID-19, emphasising that this does not imply causality and
given Vitamin D levels fall during a systematic inflammatory response that it has not been
determined whether vitamin D status causes poorer outcomes or vice versa.
Conclusion
The role of vitamin D in bone and muscle health is well documented. Public health guidelines
support supplementation in older adults based on these benefits and the risk of deficiency in
older adults particularly those spending increased time indoors or in long-term nursing home
care. A possible immunomodulatory role has been suggested by in vitro studies and association
studies. There is currently insufficient evidence linking vitamin D use in the prevention and
treatment of COVID-19. Evidence reporting an association between low vitamin D status and
poorer outcomes in COVID-19 infection do not confirm causality and in most cases are of low
quality. Previous research shows a modest reduction in the risk of acute respiratory illness with
daily vitamin D3 supplementation over weeks to months. This evidence also has limitations,
including publication and reporting bias and heterogeneity in study populations, interventions,
and definitions of respiratory infections that include upper and lower respiratory tract
involvement.
Despite this, research has identified a high prevalence of low vitamin D levels in winter
months in Ireland, and given its role in bone and muscle health this report recommends the
following:
• Increase awareness of existing guidance that adults age 65 and over should take a 15
microgram daily supplement for bone and muscle health
• Adults spending increased time indoors or are housebound or in long-term residential
care or have dark skin pigmentation are also recommended to take vitamin D
supplementation
Page 14 of 26
• That ongoing developments, particularly RCTs, in this area be monitored with
guidance reviewed accordingly
Appendix
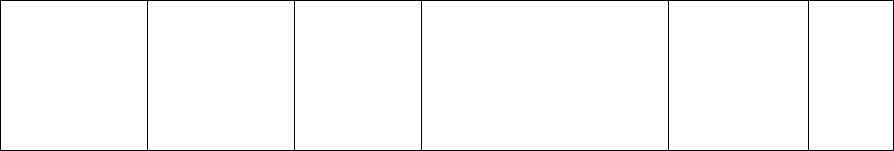
Appendix 1: Summary of COVID-19 Treatment Study
Study
Entrenas Castillo 2020 RCT Spain
Murai 2021 RCT Brazil (PRE-PRINT)
Population
N=76 patients admitted to hospital with
confirmed COVID-19
N=240 patients admitted to hospital
with confirmed COVID-19
Patients were randomised 2:1 into
intervention (n=50) and comparator arms
(n=26)
Patients were randomised 1:1 into
intervention (n=120) and comparator
arms (n=120)
Intervention
Patients in the intervention arm received
calcifediol treatment calcifediol (0.532 mg)
on admission, then 0.266 mg on days 3 and
7, then weekly until discharge, along with
standard care
Patients in the intervention arm
received a single oral dose of 200,000
IU (5,000mcg)
Patients in the comparator arm received
standard care only
Patients in the comparator arm
received a placebo
Analysis
Univariate and multivariable logistic
regressions were used to estimate the
probability of admission to intensive care
unit (ICU)
Univariate and multivariate regression
models for hospital length of stay,
admission to ICU and mechanical
ventilation requirement were adjusted
by potential confounders
Mortality was reported as number of
deaths
Mortality was reported as number of
deaths
Outcomes
1) ICU admission
2) COVID-19 mortality
1) Hospital length of stay
2) Mortality, admission to ICU and
requirement for ventilation
3) Vitamin D serum levels ≥30ng/mL
Results
Patients in the intervention arm were less
likely to be admitted to intensive care
versus those in the comparator group (OR
0.03 (95% CI 0.003, 0.25))
No difference in hospital length of
stay in vitamin D and placebo groups
(7.0 days [95% CI 6.1, 7.9] and 7.0
days [95% CI 6.2, 7.8 days], HR 1.12,
[95% CI 0.9, 1.5]; p = .379)
respectively
Patients in the intervention arm had lower
mortality versus those in the comparator
group (OR 0.097, 95%CI 0.004, 2.099)
No difference in the reported rate of
mortality (7.0% vs 5.1%; P = .59);
admission to ICU (15.8% vs 21.2%; P =
.314), and mechanical ventilation
requirement (7.0% vs 14.4%; P = .090)
86.7% of patients in the
supplementation arm achieved
vitamin D serum levels ≥30ng/mL
compared to 11% in the placebo
group
Limitations
Small sample size; serious risk of bias
Low power, and heterogeneity of the
patient sample and its treatment

Page 15 of 26
Appendix 2: Summary of COVID-19 Association Studies²⁶
Study
Vitamin D
Measurement
N
Adjusted for
Association
Quality
Hastie 2020
Vitamin D
level (nmol/L)
Cases
n=449
Control
n=348,598
Ethnicity, sex, month of
assessment, Townsend
deprivation quintile,
household income, self-
reported health rating,
smoking status, BMI
category, age at
assessment, diabetes,
SBP, DBP, and
longstanding illness,
disability or infirmity
OR 1.00
(0.998 to
1.01)
Very
low
Vitamin D
level (nmol/L)
by ethnicity
OR 0.90
(0.66 to
1.23)
Very
low
Vitamin D
deficiency
OR 0.92
(0.71 to
1.21)
Very
low
Vitamin D
insufficiency
OR 0.88
(0.72 to
1.08)
Very
low
Hernandez
2020
Vitamin D
level (ng/ml)
Cases
n=197
Control
n=197
Age, smoking,
hypertension, diabetes
mellitus, history of
cardiovascular events,
immunosuppression,
body mass index (BMI),
serum corrected calcium,
glomerular filtration rate
and the month of
vitamin D determination
MD: -9.3;
p<0.001
Very
low
Kaufman
2020
Vitamin D
level (ng/ml)
Cohort
N=191,779
Gender, age, latitudes,
ethnicity
OR 0.984
(0.983 to
0.986)
Very
low
Meltzer 2020
Vitamin D
insufficiency
Positive
n=71
Negative
n=418
Hypertension, diabetes,
chronic pulmonary
disease, pulmonary
circulation disorders,
depression,
immunosuppression,
liver disease, and chronic
kidney disease.
OR 1.77
(1.12 to
2.81)
Very
low
Merzon 2020
Vitamin D
suboptimal
Cases
n=782
Control
n=7025
Age, gender, ethnicity,
smoking,
depression/anxiety,
schizophrenia, dementia,
diabetes, hypertension,
cardiovascular disease,
chronic lung disease,
obesity, BMI and
socioeconomic status
OR 1.45
(1.08‐1.95)
Very
low
Page 16 of 26
Raisi-
Esrabragh
2020
Vitamin D
level (nmol/L)
Cases
n=1326
Control
n=3184
Sex, age and ethnicity
OR 1 (1 to 1)
Very
low

Page 17 of 26
Appendix 3: Summary of Systematic Reviews and Meta-analyses of Vitamin D and Acute Respiratory Illness
73
Studies
Martineau et al (2017)
Jolliffe et al (2020)
Trials included
25 trials (11,321 participants) from 14 countries up to 31 December 2015
45 trials (73,384 participants) from 18 countries up to 1 May 2020
Individual patient
data
10,933 participants
46,331 participants (in 42 trials)
Study duration
7 weeks - 1.5 years
8 weeks - 5 years
Mean baseline
25(OH)D conc.
Reported in 19/25 trials: range 19 - 89 nmol/L
Reported in 34/42 trials: range 19-91 nmol/L
Population
10 (40%) in populations with pre-existing disease (including asthma,
chronic obstructive pulmonary disease, pneumonia)
13 (31%) in populations with pre-existing disease (including asthma, chronic
obstructive pulmonary disease, pneumonia)
1 (4%) in low birthweight infants
1 (2.4%) in low birthweight infants and 2 (4.8%) in preterm infants
1 (4%) in older care home residents with range of comorbidities (including
asthma, chronic obstructive pulmonary disease, congestive heart failure,
diabetes, dementia)
1 (2.4%) in older care home residents with range of comorbidities (including
asthma, chronic obstructive pulmonary disease, congestive heart failure,
diabetes, dementia)
Comparison
vitamin D vs placebo
vitamin D vs placebo
higher vs lower dose vitamin D
Vitamin D dosing
daily (12 RCTs; 7.5 to 100µg; 7 weeks to 13 months)
daily (21 trials; 7.5 to 100µg; 7 weeks to 2 years)
weekly (3 RCTs; 35 to 500 µg; 8 weeks to 6 months)
weekly (6 trials; 35 to 500 µg; 8 weeks 3 years)
bolus (10 RCTs; once, monthly, 2-monthly, 3-monthly; 750-5000µg; 3 to
18 months)
bolus (13 trials; once, monthly, 2- monthly, 3-monthly; 750-5000µg; 3 to 3
years)
bolus doses combined with daily vitamin D supplementation (3 studies)
bolus doses combined with daily vitamin D supplementation (2 studies
control group also received vitamin D (2 studies)
control group also received vitamin D (7 studies)
intervention group given vitamin D + calcium (1 study)
Subgroup analyses
Baseline 25(OH)D <25 nmol/l vs ≥25 nmol/l
Baseline 25(OH)D <25 vs 25-49.9 vs 50-74.9 vs ≥75nmol/l
Dosing regimen: daily or weekly without bolus vs ≥1 bolus of ≥750µg
Dosing regimen: daily vs weekly vs monthly or less frequent
Dose size daily equivalent: <20µg vs 20µg to <50µg vs ≥50µg
Dose size daily equivalent: <10µg vs 10-25µg vs > 25-50µg vs >50µg
Age: ≤1 year vs 1.1-15.9 years vs 16-65 years vs >65 years
Age: ≤1 year vs 1.1-15.9 years vs 16-64.9 years vs >65 years
Presence versus absence of asthma, COPD and previous influenza
vaccination
Presence of airway disease (asthma vs COPD) vs those without airway
disease

Page 18 of 26
Results
Vitamin D supplementation reduced the risk of ARI among all participants
(adjusted odds ratio 0.88, 95% CI 0.81, 0.96: heterogeneity p < 0.001)
Vitamin D supplementation reduced the risk of ARI among all participants
(OR, 0.91; 95% CI, 0.84, 0.99; I 2=37.2% p for heterogeneity =0.014)
2 step IPD meta-analysis reported a reduced risk of ARI (OR, 0.80; 95% CI,
0.69, 0.93; p=0.004; I^2=53.3%, p= for heterogeneity 0.001)
No statistically significant difference of higher versus lower vitamin D dosing
(OR 0.87, 95% CI 0.73, 1.04 (I2 =0.0%, p for heterogeneity 0.496)
Sensitivity analyses
Excluding the 2 studies at unclear risk of bias: (OR, 0.82; 95% CI, 0.70,
0.95, p = 0.01; 10,744 participants).
Excluding the 4 studies at unclear risk of bias: (OR, 0.93; 95% CI, 0.86, 1.00)
Restricted to 14 trials where ARI a primary or coprimary outcome:
protective effects with vitamin D supplementation (OR, 0.82; 95% CI, 0.68,
1.00; p = 0.05, 5,739 participants)
Restricted to 18 trials with ARI as a primary or coprimary outcome: no
significant protective effect (OR, 0.89; 95% CI, 0.77, 1.03; 7,537
participants)
Subgroup analyses:
Dosing Frequency
Protective effect of vitamin D seen with daily or weekly vitamin D dosing
(OR, 0.81; 95% CI, 0.72, 0.91; p<0.001) but not bolus doses (OR, 0.97; 95%
CI, 0.86, 1.10; p=0.05)
Significant protective effect of vitamin D with daily dosing (OR 0.75, 95% CI
0.61, 0.93) but not weekly (OR 0.97, 95% CI 0.88, 1.06) or monthly to 3-
monthly (OR 0.98, 95% CI 0.93, 1.03)
Subgroup analyses:
Baselined 25(OH)D
concentration
Protective effect of vitamin D in those with levels <25 nmol/L (OR, 0.89;
95% CI, 0.77, 1.04; p=0.15; 19 RCTs; 3634 participants)
No significant effect in any of the subgroups

Page 19 of 26
Appendix 4: UK Definition of clinically extremely vulnerable groups: Summary of
Systematic Reviews and Meta-analyses of Vitamin D and Acute Respiratory Illness
74
People who are defined as clinically extremely vulnerable are at very high risk of severe
illness from coronavirus. Patients are identified as clinically extremely vulnerable either by
addition to the shielded patient list by a clinician or GP; or by having one or more of the
following:
• solid organ transplant recipients
• people with specific cancers:
• people with cancer who are undergoing active chemotherapy
• people with lung cancer who are undergoing radical radiotherapy
• people with cancers of the blood or bone marrow such as leukaemia,
lymphoma or myeloma who are at any stage of treatment
• people having immunotherapy or other continuing antibody treatments
for cancer
• people having other targeted cancer treatments that can affect the
immune system, such as protein kinase inhibitors or PARP inhibitors
• people who have had bone marrow or stem cell transplants in the last 6
months or who are still taking immunosuppression drugs
• people with severe respiratory conditions including all cystic fibrosis, severe
asthma and severe chronic obstructive pulmonary disease (COPD)
• people with rare diseases that significantly increase the risk of infections (such as
severe combined immunodeficiency (SCID), homozygous sickle cell disease)
• people on immunosuppression therapies sufficient to significantly increase risk of
infection
• problems with your spleen, for example splenectomy (having your spleen
removed)
• adults with Down’s syndrome
• adults on dialysis or with chronic kidney disease (stage 5)
• women who are pregnant with significant heart disease, congenital or acquired
• other people who have also been classed as clinically extremely vulnerable, based
on clinical judgement and an assessment of their needs. GPs and hospital clinicians
have been provided with guidance to support these decisions

Page 20 of 26
Appendix 5: Scottish Government Coronavirus (COVID-19): shielding list
75
Those recognised as being at the highest risk of severe illness from coronavirus will be notified
by post by the Chief Medical Officer. This includes the list below. Individuals in this list are
advised to contact their GP or specialist care provider if they have not received a letter.
Grouping
How would I know if I am in this group?
Solid organ
transplant
recipients
People who have had a transplant of heart, lung, stomach or other part of
intestine, liver and kidney. This is because of the medication taken to stop
rejection of the transplanted organ.
People with specific
cancers
• People with cancer who are undergoing active chemotherapy.
Or people who have had radical radiotherapy for lung cancer.
• People with cancers of the blood or bone marrow who are at
any stage of treatment. This includes cancers such as
leukaemia, lymphoma or myeloma.
• People with cancer who are having immunotherapy or other
continuing antibody treatments.
• People with cancer who are having specialised treatments
that can affect the immune system. This includes protein
kinase inhibitors or PARP inhibitors.
• People who have had bone marrow or stem cell transplants in
the last 6 months. Or people who are still taking
immunosuppression drugs.
People with severe
respiratory
conditions
• People with cystic fibrosis.
• People who are on home oxygen for a lung condition.
• People with severe asthma and on regular inhalers and long-
term steroid tablets. For example, Prednisolone or regular
injections to control your asthma.
• People with severe COPD. This usually means being on several
different inhaler medications in the last year. As well as a
steroid inhaler, this must include two long acting preventers.
For example, Long Acting Beta Agonists and Long Acting Anti-
Muscarinic Antagonists. Severe COPD means that:
o You are too breathless to walk 100 yards
o You have 2 or more lung infections a year or
o You need oxygen to help with your breathing
People with rare
diseases including
all forms of
This includes inborn errors of metabolism that significantly increase the risk
of infections. For example, SCID and homozygous sickle cell disease and
adults with Down's syndrome.

Page 21 of 26
Grouping
How would I know if I am in this group?
interstitial lung
disease /
sarcoidosis
There are many conditions classed as a rare disease. Not everyone with a
rare disease will be in the shielding group
People on
immunosuppression
therapies that
significantly
increase risk of
infection. Or people
who have had their
spleens removed
Immunosuppressive therapy helps to stop rejection of a bone marrow or
organ transplant. It can also treat conditions in which the immune system
is overactive. For example, autoimmune diseases and allergies.
In some cases these treatments may put people into the shielding group.
Your clinician can determine if your medications put you in this group.
• People on high dose corticosteroids (equal to Prednisolone
20mg or more) for 4 weeks or more.
• People on specific single therapies, e.g. Cyclophosphamide.
These medications are usually prescribed by specialists in
hospitals.
• People on lower dose of corticosteroids in combination with
other disease modifying medication.
• People on disease modifying medications who also have other
chronic medical conditions.
• People who take some medication and are otherwise healthy
may not need to be in the shielding group. This includes single
Disease Modifying medications (DMARD). It also includes
Biologic medications such as Methotrexate, Azathioprine,
Ciclosporin, Leflunomide plus others. Discuss this with your
specialist or GP if you are not sure.
People who are
pregnant with
significant heart
disease, congenital
or acquired
If you are being followed up by a specialist heart clinic during your
pregnancy.
People who are
receiving renal
dialysis
treatment and
people who have
chronic kidney
disease stage 5
People receiving or starting renal dialysis, and people who have chronic
kidney disease stage 5.

Page 22 of 26
Appendix 6: Pre-COVID NHS Vitamin D Recommendations
76
The NHS recommends that:
• breastfed babies and formula-fed babies consuming ≤500ml of infant formula per day
from birth to 1 year of age should be given a daily Vitamin D supplement containing 8.5
to 10 micrograms;
• children aged 1 to 4 years old should be given a daily supplement containing 10
micrograms;
• adults (including women who are pregnant or breastfeeding), young people and
children over 4 years should consider taking a daily supplement containing 10
micrograms (400IU) of vitamin D between October and early March;
• adults that are not often outdoors; are in an institution like a care home; usually wear
clothes that cover up most of their skin when outdoors; have dark skin (e.g. those from
an African, African-Caribbean or south Asian background) should consider taking a daily
supplement containing 10 micrograms of vitamin D throughout the year.
Caution should be taken in:
• those under the care of a renal, endocrinology or cancer specialist
• people with high vitamin D levels
• people with kidney stones (now or in the past)
• people with too much parathyroid hormone (hyperparathyroidism),
• people with cancer (some cancers can lead to high calcium levels)
• people with severe kidney disease
• people with a rare illness called sarcoidosis

Page 23 of 26
REFERENCES
1
Hansdottir S, Monick MM, Hunninghake GW et al. Respiratory epithelial cells convert inactive
vitamin D to its active form: potential effects on host defense. J Immunol 2008;356:7090-9
doi:10.4049/jimmunol.181.10.7090 pmid:18981129
2
Hewison M. Antibacterial effects of vitamin D. Nat Rev Endocrinol. 20117(6):337-45. doi:
10.1038/nrendo.2010.226. Epub 2011 Jan 25. Erratum in: Nat Rev Endocrinol. 2011 Aug;7(8):436.
PMID: 21263449
3
Hossein-nezhad A, Spira A, Holick MF. Influence of vitamin D status and vitamin D3 supplementation
on genome wide expression of white blood cells: a randomized double-blind clinical trial. PLoS ONE
2013;8, e58725. doi:10.1371/journal.pone.0058725
4
Moozhipurath RK, Kraft L, Skiera B. Evidence of protective role of Ultraviolet-B (UVB) radiation in
reducing COVID-19 deaths. Sci Rep. 2020;10(1):17705. doi: 10.1038/s41598-020-74825-z.
5
Grant,WB et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-
19 infections and deaths. Nutrients; 2020:12(4): 988
6
Annweiler C, Hanotte B, Celarier, T et al. Vitamin D and survival in COVID-19 patients: A quasi-
experimental study.; The Journal of steroid biochemistry and molecular biology; 2020; 105771
7
Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. Journal of
infection and public health;2020:13(10):1373-1380
8
Israel A, Cicurel AA, Lavie G et al. The link between vitamin D deficiency and Covid-19 in a large
population medRxiv 2020.09.04.20188268; doi: https://doi.org/10.1101/2020.09.04.20188268
9
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chemistry &
biology 2014;21(3): 319-29. doi:10.1016/j.chembiol.2013.12.016
10
Holick MF. Vitamin D deficiency. N Engl J Med 2020; 357: 266–81
11
Jones AN, Hansen KE. Recognizing the musculoskeletal manifestations of vitamin D deficiency. J
Musculoskelet Med. 2009;26(10):389-396
12
Scientific Advisory Committee on Nutrition. Vitamin D and health. 2016 Available online at:
https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report
13
Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881-886.
doi:10.2310/JIM.0b013e31821b8755
14
Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin
D
3
: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D
3
synthesis in
human skin. J Clin Endocrinol Metab 1988;67, 373–378
15
Webb AR, Engelsen O. Calculated ultraviolet exposure levels for a healthy vitamin D status.
Photochem Photobiol 2006; 82, 1697–1703
16
Cashman KD, Kiely M. Recommended dietary intakes for vitamin D: Where do they come from,
what do they achieve and how can we meet them? J Hum Nutr Diet. 2014; 27(5):434-42
17
Griffin G et al. Vitamin D and COVID-19: evidence and recommendations for
supplementation. Royal Society Open Science 2020; 7.12: 201912.
18
Health Service Executive. HSE Policy on Vitamin D Supplementation for Infants in Ireland (2010), 31
May 2010 https://pdf4pro.com/cdn/policy-on-vitamin-d-supplementation-for-infants-in-ireland-
595991.pdf
19
FSAI. FSAI Advises on National Policy for Vitamin D Supplementation for Infants. 16 May 2007
https://www.fsai.ie/details.aspx?id=6984
20
Health Service Executive. Vitamin D for babies 0 to 12 months. 2020
https://www2.hse.ie/wellbeing/child-health/vitamin-d-for-babies-0-12-months.html
21
European Food Safety Authority Scientific Opinion on the Essential Composition of Infant Formula.
2014 https://efsa.onlinelibrary.wiley.com/doi/10.2903/j.efsa.2014.3760

Page 24 of 26
22
FSAI Update to 2007 Scientific Committee Report: Recommendations for a National Policy on
Vitamin D Supplementation for Infants in Ireland 2020
https://www.fsai.ie/Recommendations_Update_VitaminD/
23
Department of Health. Vitamin D advice from the Department of Health for children from 1 to 4
years of age https://assets.gov.ie/93353/5b2c0185-e7c9-42df-9b19-05e1afe2882f.pdf
24
Department of Health. New advice on Vitamin D supplement for people aged 65 years and older. 24
Nov 2020 https://www.gov.ie/en/press-release/7d595-new-advice-on-vitamin-d-supplement-for-
people-aged-65-years-and-older/
25
FSAI Vitamin D Scientific Recommendations for Food-Based Dietary Guidelines for Older Adults in
Ireland 2020 https://www.fsai.ie/VitaminD_DietaryGuidelines_OlderAdults_Ireland
26
NICE. Covid-19 rapid guideline: vitamin D. 17 December 2020. www.nice.org.uk/guidance/ng187
27
Entrenas Castillo M et al. Effect of calcifediol treatment and best available therapy versus best
available therapy on intensive care unit admission and mortality among patients hospitalized for
COVID-19: A pilot randomized clinical study. The Journal of steroid biochemistry and molecular
biology 2020; 203): 105751. doi:10.1016/j.jsbmb.2020.105751
28
Kaufman HW, Niles JK, Kroll MH, Bi C, Holick MF (2020) SARS-CoV-2 positivity rates associated with
circulating 25-hydroxyvitamin D levels. PLOS ONE 15(9): e0239252.
https://doi.org/10.1371/journal.pone.0239252
29
Hastie CE, Mackay DF, Jill P et al. Vitamin D concentrations and COVID-19 infection in UK Biobank.;
Diabetes & metabolic syndrome; 2020;14 (4); 561-565
30
Raisi-Estabragh Z, McCracken C, Steffen E et al. Greater risk of severe COVID-19 in Black, Asian and
Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural
factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank.; Journal of public
health; 2020:42(3); 451-460
31
Meltzer DO, Best TJ, Solway J et al. Association of Vitamin D Status and Other Clinical Characteristics
With COVID-19 Test Results.; JAMA network open; 2020;3(9); e2019722
32
Merzon E, Tworowski D, Frenkel-Morgenstern M et al. Low plasma 25(OH) vitamin D level is
associated with increased risk of COVID-19 infection: an Israeli population-based study. The FEBS
journal; 2020
33
Hernandez JL, Nan D, Hernandez M et al. Vitamin D Status in Hospitalized Patients With SARS-CoV-2
Infection; The Journal of Clinical Endocrinology & Metabolism; 2020; dgaa733,
https://doi.org/10.1210/clinem/dgaa733
34
Macaya F, Espejo P, Miguel A et al. Interaction between age and vitamin D deficiency in severe
COVID-19 infection.; Nutricion hospitalaria; 2020;37(5); 1039-1042
35
Radujkovic A, Hippchen T, Merle U et al. Vitamin D Deficiency and Outcome of COVID-19 Patients.
Nutrients; 2020; 12(9)
36
Ye K, Tang F, Yang J et al. Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A
Case-Control Study.; Journal of the American College of Nutrition; 2020; 1-8
37
Annweiler G, Corvaisier M, Annweiler C et al. Vitamin D Supplementation Associated to Better
Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study.
Nutrients. 2020;12(11):3377. doi: 10.3390/nu12113377. PMID: 331478948
38
Yisak H, Ewunetei A, Kefale B, et al. Effects of Vitamin D on COVID-19 Infection and Prognosis: A
Systematic Review. Risk Manag Healthc Policy. 2021;14:31-38. Published 2021 Jan 7.
doi:10.2147/RMHP.S291584
39
Murai IH, Fernandes AL, Pereira RMR et al. Effect of Vitamin D3 Supplementation vs Placebo on
Hospital Length of Stay in Patients with Severe COVID-19: A Multicenter, Double-blind, Randomized
Controlled Trial
medRxiv 2020.11.16.20232397; doi: https://doi.org/10.1101/2020.11.16.20232397
40
Martineau AR, Jolliffe DA, Camargo CA Jr et al. Vitamin D supplementation to prevent acute
respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ.
2017 Feb 15;356:i6583. doi: 10.1136/bmj.i6583. PMID: 28202713; PMCID: PMC5310969

Page 25 of 26
41
Jolliffe DA Camargo CA Jr, Martineau AR et al. Vitamin D supplementation to prevent acute
respiratory infections: systematic review and meta-analysis of aggregate data from randomised
controlled trials medRxiv 2020.07.14.20152728; doi: https://doi.org/10.1101/2020.07.14.20152728
42
Abioye AI, Bromage S, Fawzi W. Effect of micronutrient supplements on influenza and other
respiratory tract infections among adults: a systematic review and meta-analysis. BMJ Global
Health 2021;6:e003176.
43
Vuichard Gysin D, Dao D, Gysin CM, Lytvyn L, Loeb M. Effect of Vitamin D3 Supplementation on
Respiratory Tract Infections in Healthy Individuals: A Systematic Review and Meta-Analysis of
Randomized Controlled Trials. PLoSOne2016;356: e0162996.
doi:10.1371/journal.pone.0162996 pmid:27631625
44
Wang MX, Win SS, Pang J et al. Zinc supplementation reduces common cold duration among
healthy adults: A systematic review of randomized controlled trials with micronutrients
supplementation. Am J Trop Med Hyg. 2020;103(1):86-99. doi: 10.4269/ajtmh.19-0718.
45
Xiao L, Xing C, Yang Z, et al. Vitamin D supplementation for the prevention of childhood acute
respiratory infections: a systematic review of randomised controlled trials. Br J Nutr.
2015;114(7):1026–1034
46
Jolliffe, David A., et al. Vitamin D supplementation to prevent asthma exacerbations: a systematic
review and meta-analysis of individual participant data. The lancet Respiratory medicine 2017:5(11):
881-890.
47
Rejnmark L et al. “Non-skeletal health effects of vitamin D supplementation: A systematic review on
findings from meta-analyses summarizing trial data.” PloS one 2017; 12(7):e0180512
doi:10.1371/journal.pone.0180512
48
Autier P, Mullie P, Boniol M et al. Effect of vitamin D supplementation on non-skeletal disorders: a
systematic review of meta-analyses and randomised trials. Lancet Diabetes Endocrinol. 2017; 5: 986–
1004
49
National Heart Lung and Blood Institute PCTN, Ginde AA, et al. Early high-dose vitamin D3 for
critically ill, vitamin D-deficient patients. N Engl J Med. 2019;381(26):2529-2540.
50
Amrein K, Schnedl C, Holl A, et al. Effect of High-Dose Vitamin D
3
on Hospital Length of Stay in
Critically Ill Patients With Vitamin D Deficiency: The VITdAL-ICU Randomized Clinical
Trial. JAMA. 2014;312(15):1520–1530. doi:10.1001/jama.2014.13204
51
Bergman P, Norlin AC, Hansen S et al. Vitamin D3 supplementation in patients with frequent
respiratory tract infections: a randomised and double‐blind intervention study. BMJ Open 2012; 2:
e001663. https://doi.org/10.1136/bmjopen‐2012‐001663
52
Murdoch DR, Slow S, Chambers ST et al. Effect of vitamin D3 supplementation on upper respiratory
tract infections in healthy adults: the VIDARIS randomized controlled trial. JAMA 2012; 308: 1333–9.
53
Camargo CA Jr, Sluyter J, Scragg R et al. Effect of Monthly High-Dose Vitamin D Supplementation on
Acute Respiratory Infections in Older Adults: A Randomized Controlled Trial, Clinical Infectious
Diseases 2020 71(2); 311–317, https://doi.org/10.1093/cid/ciz801
54
Olliver M, Spelmink L, Bergman P et al. Immunomodulatory effects of vitamin D on innate and
adaptive immune responses to Streptococcus pneumoniae. J Infect Dis2013;356:1474-81.
doi:10.1093/infdis/jit355 pmid:23922371
55
McCartney DM, Byrne DG. Optimisation of Vitamin D Status for Enhanced Immuno-protection
Against Covid-19. Ir Med J. 2020;113(4):58. PMID: 32268051
56
Quraishi SA, Camargo CA Jr. Vitamin D in acute stress and critical illness. Curr Opin Clin Nutr Metab
Care. 2012 Nov;15(6):625-34. doi: 10.1097/MCO.0b013e328358fc2b. PMID: 23075939; PMCID:
PMC3751798.
57
Mitchell F. Vitamin-D and COVID-19: do deficient risk a poorer outcome? The Lancet Diabetes &
Endocrinology, 2020; 8(7): 570
58
Lancet Editorial Vitamin D and COVID-19: why the controversy? The Lancet Diabetes &
Endocrinology, Jan 11, 2021 DOI:https://doi.org/10.1016/S2213-8587(21)00003

Page 26 of 26
59
Laird E, Rhodes J, Kenny RA. Vitamin D and Inflammation: Potential Implications for Severity of
Covid-19. Ir Med J. 2020;113(5):81. PMID: 32603576.http://imj.ie/vitamin-d-and-inflammation-
potential-implications-for-severity-of-covid-19
60
Cashman KD, Muldowney S, Flynn A et al. Vitamin D status of Irish adults: findings from the National
Adult Nutrition Survey. Br J Nutr. 2013; 109:1248-56. doi: 10.1017/S0007114512003212.
61
Laird E, Kenny RA. Vitamin D deficiency in Ireland – implications for COVID-19. Results from the Irish
Longitudinal Study on Ageing (TILDA) 2020
https://tilda.tcd.ie/publications/reports/pdf/Report_Covid19VitaminD.pdf
62
Laird E, O’Halloran AM, Kenny RA et al. The prevalence of vitamin D deficiency and the
determinants of 25 (OH)D concentration in older Irish adults: Data from The Irish Longitudinal Study
on Ageing (TILDA). The Journals of Gerontology: Series A. 2018 ;3(4):519-525
https://academic.oup.com/biomedgerontology/ article/73/4/519/4103040
63
Laird E, Walsh JB, Healy M et al. A High Prevalence of Vitamin D Deficiency Observed in an Irish
South East Asian Population: A Cross-Sectional Observation Study. Nutrients. 2020;12(12):3674. doi:
10.3390/nu12123674. PMID: 33260572; PMCID: PMC7760119
64
Griffin TP, Wall D, O'Shea PM et al. Vitamin D status of adults in the community, in outpatient
clinics, in hospital and in nursing homes in the West of Ireland. J Gerontol A Biol Sci Med Sci. 2020;pii:
glaa010. doi: 10.1093/gerona/glaa010
65
McKenna MJ, Freaney R, Muldowney FP et al. Prevention of hypovitaminosis D in the
elderly. Calcified tissue international, 1985;37(2), 112-116.
66
Cashman KD, Hayes A, Seamans KM. Dietary calcium does not interact with vitamin D3 in terms of
determining the response and catabolism of serum 25-hydroxyvitamin D during winter in older
adults. The American Journal of Clinical Nutrition, 2014;99(6), 1414-1423
67
Cashman KD, Seamans KM, Hill TR et al. Relative effectiveness of oral 25-hydroxyvitamin D3 and
vitamin D3 in raising wintertime serum 25-hydroxyvitamin D in older adults. The American journal of
clinical nutrition, 2012;95(6), 1350-1356
68
Carroll A, Onwuneme C, Murphy NP et al. Vitamin D status in Irish children and adolescents: value
of fortification and supplementation. Clinical pediatrics, 2014;53(14), 1345-1351
69
Molloy EJ, Murphy N. Vitamin D, Covid-19 and Children. Ir Med J. 2020;113(4):64. PMID: 32268052.
70
McKenna MJ, Flynn MAT. Covid-19, Cocooning and Vitamin D Intake Requirements. Ir Med J.
2020;113(5):79. PMID: 32603573.
71
Department of Health and Social Care. Vitamin D and clinically extremely vulnerable (CEV) guidance
Jan 2021 https://www.gov.uk/government/publications/vitamin-d-for-vulnerable-groups/vitamin-d-
and-clinically-extremely-vulnerable-cev-guidance
72
NHS Inform Scotland Coronavirus (COVID-19): Shielding Jan 2021
https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/coronavirus-covid-
19/coronavirus-covid-19-shielding
73
Scientific Advisory Committee on Nutrition. Update of rapid review: Vitamin D and acute respiratory
tract infections Dec 2020
74
Department of Health and Social Care. Guidance on shielding and protecting people who are
clinically extremely vulnerable from COVID-19. 13 Jan 2021
https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-
vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-
persons-from-covid-19#cev
75
Scottish Government Coronavirus (COVID-19): shielding advice and support: highest risk group 25
Nov 2020 https://www.gov.scot/publications/covid-shielding/pages/highest-risk-classification/
76
NHS Vitamin D Recommendations 2020 https://www.nhs.uk/conditions/vitamins-and-
minerals/vitamin-d/
