
REPORT
Evaluation of the Impact of the No
Surprises Act on Health Care Market
Outcomes:
Baseline Trends and Framework for
Analysis
First Annual Report
The First of Five Reports Required
by the Consolidated Appropriations Act, 2021
July 6, 2023
U.S. Department of Health and Human Services
Office of the Assistant Secretary for Planning and Evaluation

July 2023
REPORT TO CONGRESS
2
Office of the Assistant Secretary for Planning and Evaluation
The Assistant Secretary for Planning and Evaluation (ASPE) advises the Secretary of the U.S. Department
of Health and Human Services (HHS) on policy development in health, disability, human services, data,
and science; and provides advice and analysis on economic policy. ASPE leads special initiatives;
coordinates the Department's evaluation, research, and demonstration activities; and manages cross-
Department planning activities such as strategic planning, legislative planning, and review of regulations.
Integral to this role, ASPE conducts research and evaluation studies; develops policy analyses; and
estimates the cost and benefits of policy alternatives under consideration by the Department or Congress.
Office of Health Policy
The Office of Health Policy (HP) provides a cross-cutting policy perspective that bridges Departmental
programs, public and private sector activities, and the research community, in order to develop, analyze,
coordinate and provide leadership on health policy issues for the Secretary. HP carries out this mission by
conducting policy, economic and budget analyses, assisting in the development and review of regulations,
assisting in the development and formulation of budgets and legislation, and assisting in survey design
efforts, as well as conducting and coordinating research, evaluation, and information dissemination on
issues relating to health policy.
Suggested Citation
Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health & Human
Services. Evaluation of the Impact of the No Surprises Act on Health Care Market Outcomes: Baseline
Trends and Framework for Analysis – First Annual Report. July 2023.
Acknowledgements
Many people at ASPE contributed to this project. The lead authors are Joel Ruhter and Steve Sheingold.
Other contributors include Nancy De Lew, Ken Finegold, and Benjamin D. Sommers. ASPE also
acknowledges support from RAND staff. The statements expressed in this report do not necessarily reflect
the views of RAND.

July 2023
REPORT TO CONGRESS
3
Contents
Chapter 1. Introduction and Overview .........................................................................................8
Chapter 2. State Actions on Surprise Billing ................................................................................ 11
Chapter 3. Consolidation and Competition – Trends and Evidence of Effects in Healthcare ................ 15
Chapter 4. Descriptive Analysis of Trends in OON Billing – Baseline Before NSA Implementation......... 26
Chapter 5. A Conceptual Framework and Potential Methods ........................................................ 32
Chapter 6. Conclusion............................................................................................................. 36
References ........................................................................................................................... 37
Appendix A. Section 109 of the No Surprises Act ......................................................................... 41
Appendix B. Recent State Balance Billing Protections .................................................................. 42
Appendix C. Condensed Summary of Consolidation Effects on Health Care Prices, Spending, Quality,
Access, and Wages ................................................................................................................ 44

July 2023
REPORT TO CONGRESS
4
Executive Summary
The No Surprises Act (NSA)
1
was enacted on December 27, 2020, to address certain instances of surprise
billing – circumstances where individuals with private health plans and coverage
2
receive unexpectedly
high medical bills when they are unknowingly or unavoidably treated by an out-of-network (OON)
provider, facility, or provider of air ambulance services. Under the law, an OON provider
3
subject to
balance billing requirements generally may not charge more than the patient’s in-network cost sharing
requirement based on the Recognized Amount for non-air ambulance items and services.
4
The law also
creates a process for resolving disputes over payment rates between providers and plans and issuers
under certain circumstances. The enactment of NSA, as well as several previous state surprise billing laws,
was motivated by consumer concerns about the adverse financial impacts of surprise medical bills.
Section 109 of NSA requires the Secretary, in consultation with the Federal Trade Commission and
Attorney General, to produce five annual reports on the impact of NSA on patterns of vertical or horizontal
integration, overall health care costs, and access to health care items and services. This is the first of those
reports.
For several reasons, estimates of these impacts of NSA have some limitations. The surprise billing
provisions in the law went into effect on January 1, 2022, and it may take time to see the full impact of
the law on these outcomes. In addition, surprise bills are likely to be a relatively small proportion of total
health care claims for items and services. Furthermore, existing data suggest these bills, and therefore the
law’s impact, may be concentrated in a few services areas, such as emergency departments (EDs) and air
ambulance services. These service areas may see significant impacts, while the majority of items and
services in the health care sector may be less directly impacted by the law. Finally, the trends in NSA
impacts that are the subject of these reports are influenced by many factors over time including but not
limited to demographic changes, technology changes that affect health care delivery, economic
conditions, the COVID-19 pandemic, and health care policies that alter financial incentives. Distinguishing
NSA impacts from these other influences will be challenging methodologically.
This first report focuses largely on establishing a baseline and a framework for further evaluation. The
report details key trends in factors that will be important to evaluate NSA effects including: the
implementation and impacts of state surprise billing laws already in effect; trends in market consolidation
and concentration; the impact of market consolidation and concentration on prices, quality, and spending;
1
The No Surprises Act was included as part of the Consolidated Appropriations Act, 2021 (P.L. 116-260, 134 Stat.
1182, Division BB, Title I).
2
This report will use the term “private health plan and coverage” to refer to the products and “plans and issuers” to
refer to the entities offering the private health plans and coverage regulated by NSA. See page 8 for additional detail
on the private health plans and coverage regulated by NSA.
3
In this report, “provider” refers to providers, facilities, and providers of air ambulance services that are subject to
NSA requirements.
4
The Recognized Amount is the lesser of the amount billed by the provider or facility or the Qualifying Payment
Amount (QPA),if an applicable state law or All-Payer Model Agreement does not provide for a different out-of-
network rate. For air ambulance services provided by a nonparticipating provider, the cost-sharing requirement must
be based on the lesser of the QPA or the billed amount.

July 2023
REPORT TO CONGRESS
5
and trends in OON billing. This report also describes a conceptual framework for considering the health
care market effects of NSA, as well as describing potential methodologic approaches (and their limitations)
for estimating these effects. Subsequent reports will implement these approaches.
Estimating NSA Impacts: Baseline Factors
Estimating the effects of NSA requires distinguishing them from other factors already influencing trends
in health care market outcomes of interest and pre-existing trends in these outcomes. Three of these key
factors are: the effect of state surprise billing laws, existing trends in market consolidation, and pre-NSA
trends in OON billing.
State Surprise Billing Laws - Prior to the enactment of NSA on December 27, 2020, 33 states had enacted
surprise billing protections which vary in level of protection and scope. NSA fills a major gap in these state
laws by covering self-insured plans that are subject the Employee Retirement Income Security Act of 1974
(ERISA) rather than state regulation. Existing studies suggest that these preexisting state surprise billing
protections affect both in-network and OON prices as well as providers’ decisions to join networks. These
effects will need to be accounted for in evaluating NSA.
Market Consolidation and Concentration - There are two concepts relevant for describing and measuring
the degree of competition or market power: consolidation and concentration. Consolidation refers to
actions by participants – such as a merger, purchase, or acquisition – that ultimately modify market
structure and potentially increase their market power. Concentration refers to the relative size and
number of competitors in a market at any given time; concentration is “high” when sales (or purchases)
are made by a few competitors.
The number of hospital consolidations increased in 2010 relative to the previous decade and has followed
a fairly consistent pattern through 2020. As a result, by one measure, the number of hospital markets that
were of moderate or low concentration declined by nearly half during these years, from 23 percent of
markets in 2008 to 12 percent of markets in 2020 (see Chapter 3 for more detail on how these measures
were constructed). On the other hand, about one-third of commercial health insurance markets were of
moderate or low concentration in both 2008 and 2020. Physicians have been involved in a considerable
amount of consolidation activity during these years, both in terms of mergers between physician groups
and mergers with hospitals (vertical consolidation) as well as private equity acquisition of physician
practices.
Health care market consolidation and concentration may have independent impacts on outcomes of
interest such as price and quality. It will be important to account for these impacts in evaluating the effects
of NSA. An environmental scan conducted for this report examined evidence on impacts of consolidation
on price, quality, and access to health care in health care provider and health insurance markets. It found
strong evidence that horizontal consolidation of hospitals is associated with higher prices paid to providers
and some evidence that vertical consolidation of hospitals and physician practices leads to higher prices
paid to providers. It also found that horizontal consolidation of commercial insurers is associated with
lower prices paid to providers as insurers gain market power in negotiations with providers. However, the
lower prices paid to providers do not appear to be passed onto consumers, who face higher premiums

July 2023
REPORT TO CONGRESS
6
following insurer consolidation. Finally, the scan also assessed the evidence of the effects of consolidation
on quality of care and found that evidence on these effects was generally weak and mixed as to the
direction of the impact on quality measures.
In addition to the broader trends in health care consolidation described above, the health care system has
undergone dramatic changes since 2020 due to the COVID-19 pandemic, and researchers are still
examining the full scope of those changes – as well as what their long-term impacts will be on health care
markets. This creates additional challenges and uncertainty in identifying the effects of NSA surprise billing
protections that took effect in 2022.
OON Billing – In order to estimate the impacts of NSA, it is important to establish the overall trend in OON
billing and drill down to the items and services most likely to be affected. Providers, items and services,
and patients most commonly associated with surprise OON bills prior to NSA are likely to be those most
affected by the law. Overall, there was a downward trend in OON claims prior to NSA implementation –
the prevalence of professional claims that were OON decreased from 6.0 percent to 4.7 percent from
2012 to 2020. In addition, the share of total payments that were OON declined over this period from 9.2
percent in 2012 to 6.8 percent in 2020.
Most physicians have a very low prevalence of OON bills. Approximately 70 percent of physicians bill 2
percent or fewer of their claims OON. A small share of physicians account for a disproportionate share of
OON bills, with just over 5 percent of physicians who bill the majority of their claims OON. The specialties
with the highest rates of OON billing are psychiatry, emergency medicine, pathology, anesthesiology, and
pain medicine, each of which, on average, bill over 4 percent of their claims OON. Another factor in the
rate of OON bills is the place of service. Claims from EDs (13 percent) and ambulatory surgery centers
(ASCs) (8 percent) are more likely to be billed OON than claims from office visits (4 percent).
A Conceptual Framework for Estimating NSA Impacts
NSA requires the Secretary, in consultation with the Federal Trade Commission and Attorney General, to
provide an assessment of the impact of NSA on market consolidation, health care spending, and access to
health care. It is therefore useful to develop a conceptual framework that considers all of the pathways
by which NSA might affect health care market outcomes. A primary goal of NSA is to reduce the number
of surprise bills and the out-of-pocket spending associated with them. A potential downstream effect of
the reduced out-of-pocket liability is that medical debt may be reduced. However, there may be other
effects as well. Negotiations between providers and plans and insurers affect both in-network and OON
prices, as well as network participation by providers. To the extent that these dynamics, impacted by NSA,
lead to more market power for insurers, insurers may be able to negotiate lower in-network prices, reduce
premiums, or limit overall health spending. One possible response to the increase in insurer market power
is providers seeking to consolidate to increase their own market power and strengthen their bargaining
positions, which could lead to higher relative prices and increased spending.
Methods for Estimating Potential NSA Impacts

July 2023
REPORT TO CONGRESS
7
As described above, estimating the independent impacts of NSA on key outcomes such as prices,
spending, quality, access to health care, and market consolidation will be challenging. For future reports,
we will identify the most promising study designs and statistical methods to explore these questions as
data become available. In addition, we will hold discussions with interested parties and use qualitative
methods as appropriate to provide the most comprehensive picture of NSA impacts as possible.

July 2023
REPORT TO CONGRESS
8
Chapter 1. Introduction and Overview
NSA was enacted to help protect participants, beneficiaries, and enrollees in group health plans and group
and individual health insurance coverage from surprise medical bills in certain situations where surprise
billing commonly occurs. The law’s provisions providing protections against surprise billing took effect on
January 1, 2022.
These NSA requirements apply to items and services provided to most individuals enrolled in private
health plans and coverage, including:
• Employment-based group health plans, including both self-insured and fully insured plans, and
plans sponsored by private employers, unions, or state and local government employers
• Individual or group health insurance coverage on or outside the Federal or State-based Exchanges
• Federal Employee Health Benefit (FEHB) plans
• Certain church plans within IRS jurisdiction
• Student health insurance coverage
Surprise billing refers to situations where an individual unexpectedly receives an OON bill for the
difference between what the provider charges for an item or service and what the individual’s plan or
issuer will pay. Surprise medical bills from OON providers are often for emergency or ancillary services
when patients do not have a choice of provider. Typical examples include emergency care, anesthesiology,
or diagnostic testing. These situations occur at both OON facilities and in-network facilities where a
treating physician or other provider is OON. Often surprise medical bills are much higher than patients
had anticipated before receiving health care items and services. Patients may have had no way of knowing
that these providers were not in their health plan’s or issuer’s network and might receive bills from these
providers for items or services not fully covered by their plan or issuer. The NSA, as well as several
previously enacted state surprise billing laws, was designed to address these kinds of surprise medical bills
(ASPE, 2021).
Prior to the enactment of NSA, studies found OON bills were a common occurrence for patients treated
in emergency departments or who were admitted to the hospital, many of which would be considered
surprise bills. In 2016, patient OON responsibility for ED surprise bills averaged $628 and was $2,040 for
inpatient admissions (Sun et al., 2019). These unexpected costs represent significant financial distress for
many Americans, 63 percent of whom report not being able to cover a hypothetical $400 emergency
expense exclusively using cash or its equivalent (Board of Governors of the Federal Reserve System, 2023)
In a 2016 survey, 69 percent of those who had problems paying for medical care received from an OON
provider said they did not know that the provider was not in their plan’s network (Hamel et al., 2016). In
2018, among those reporting problems affording health care, the second most frequently cited reason for
those problems was unexpected medical bills, some of which may be surprise bills (Hamel, Muñana, and
Brodie, 2019). In 2020, nearly 20 percent of insured adults in the two years prior received a surprise bill
because the provider was OON and two-thirds of adults are worried about being able to afford unexpected
medical bills (Pollitz et al., 2020). While the precise contribution of surprise billing to medical debt cannot
July 2023
REPORT TO CONGRESS
9
be determined from available data sources, surprise bills likely play a role in medical debt and financial
stress for American families (ASPE, 2020).
Prior to NSA, patients frequently received OON items and services which may have resulted in a surprise
bill. For large employer plans, 18 percent of ED visits and 16 percent of in-network inpatient stays had at
least one OON charge in 2017 (Pollitz et al., 2020). Other studies have found that 22 percent of ED visits
at in-network facilities included care by OON physicians from 2014 to 2015 (Cooper and Scott Morton,
2016), and 20 percent of inpatient admissions from the ED, 14 percent of outpatient visits to the ED, and
9 percent of elective inpatient admissions involved an OON provider in 2014 (Garmon and Chartock,
2017).
NSA provisions require plans and issuers to cover certain OON bills with patient cost-sharing requirements
not greater than the requirements that would apply if the bill were in-network. Plans and issuers and
providers that are unable to agree on the OON rate payable to the provider after a 30-day open
negotiation period may enter the Federal independent dispute resolution (IDR) process
5
to arbitrate the
OON rate. The most common medical procedure codes initially reported among disputes in the Federal
IDR
6
system from April 15 to September 30, 2022 involving emergency or non-emergency items and
services were ED services (66 percent), radiology (9 percent), and anesthesia (7 percent) (The
Departments, 2022).
Section 109 of NSA directs the Secretary, in consultation with the Federal Trade Commission and Attorney
General, to conduct a study on the effects of certain provisions of NSA on market consolidation, overall
health care costs, and access to health care services (see Appendix A for details). Section 109 also directs
the Secretary, in consultation with the Secretary of Labor and the Secretary of the Treasury, to make
recommendations with respect to potential challenges to addressing anti-competitive consolidation of
health care providers, plans and issuers. The effects of NSA on prices paid to OON providers will likely
depend on how the Federal IDR process unfolds and expectations among disputing parties about how
arbitrators may adjudicate cases. If OON rates decrease in general, then providers’ alternative to being in
a plan’s or issuer’s network would become less favorable and their bargaining power relative to health
plans and issuers would decrease, which could in turn lead to changes in in-network prices. If OON rates
increase, then the opposite could happen. Any price changes may have impacts on total health care
spending, consumer spending, and health care market decisions that could affect health care
consolidation, patient access to health care, and quality of care. The price effects of NSA may extend
beyond OON items and services, as negotiations between providers and plans and issuers over in-network
rates likely consider anticipated OON prices as the alternative to entering a contract. Given NSA’s potential
5
Disputes are eligible for the Federal IDR process only if there is no All-Payer Model Agreement or specified state
law that applies to the item or service, provider, and plan and issuer involved.
6
If a provider and plan or issuer cannot reach an agreement on an OON payment dispute, then either party may
initiate the Federal IDR process. The IDR process is a baseball-style arbitration process under which the provider and
the plan or issuer each submit to a third-party arbitrator (i.e., certified IDR entity) their best and final offers. The
certified IDR entity must review both offers and make a determination. Some states have their own separate IDR
process.

July 2023
REPORT TO CONGRESS
10
effects on OON and in-network prices, the law may also affect provider decisions about contracting with
plans and issuers, resulting in changes to network structures and the prevalence of OON billing.
Changes in prices and other aspects of the law may in turn lead to changes in OON spending, medical
debt, total spending, and premiums. Financial protections and changes in prices would affect financial
barriers to care. Changes in prices may affect provider decisions regarding consolidation, provider supply
(e.g., staffing), and investments in quality improvement over the long term. Changes in the supply of
providers would in turn have implications for access to health care, and changes in consolidation could
influence prices, access to health care, and quality of care.
Section 109 of NSA requires this report and four additional annual reports continuing from 2024 through
2027. This first report presents broad context and baseline trends for assessing potential impacts in the
future reports. The report also summarizes NSA, with a particular focus on the patient financial
protections and dispute resolution process that are likely to affect outcomes in the health care sector.
Because the surprise billing protections in NSA went into effect on January 1, 2022, robust data needed
to estimate the effects of NSA on consolidation, overall health care costs, and access to health care items
and services are not yet available. As data become available, future reports will contain empirical analysis
of these outcomes.
Trends in consolidation, as well as trends in health care costs and access to health care, are also influenced
by numerous factors such as local health care market characteristics, technology changes, and other
policies of the federal and state governments. Estimating the independent effects of NSA requires data
and methods that can distinguish them from these other influences. The report provides a description of
the baseline factors needed to establish the existing trends in the outcomes of interest. It discusses state
actions on surprise billing and literature on the impacts of those actions with a discussion of how those
may be relevant to evaluating NSA (Chapter 2). Next, the report discusses the landscape and trends in
health care market consolidation and how consolidation – a potential response by providers and health
insurance issuers to NSA – has been found to impact health care costs, access to health care, and market
concentration (Chapter 3). The report describes the recent trends in OON and surprise billing to better
understand on which patients and providers NSA might have the most impact (Chapter 4). In Chapter 5,
we present a conceptual model that will guide how we estimate NSA impacts relative to these baseline
trends. Finally, in Chapter 6, the report concludes with the analyses that we aim to include in future
reports. Future reports will continue to follow trends in OON and surprise billing, noting the types of
patients, providers, and items and services where these trends appear to change following the
implementation of NSA. Future reports will also track other primary effects of NSA on prices for items and
services as found in analysis of claims data. We expect that future reports will include more thorough
analysis of air ambulance services as well.
We intend to gather feedback from discussions with interested parties on initial impacts of NSA and
anticipated impacts on consolidation, health care costs, and access to health care. These discussions may
also form the basis for recommendations for effective enforcement of provisions of NSA required by
section 109.

July 2023
REPORT TO CONGRESS
11
Chapter 2. State Actions on Surprise Billing
Prior to the enactment of NSA, some states had implemented their own laws limiting surprise billing.
According to an analysis from the Commonwealth Fund, 33 states (see Appendix B) had enacted surprise
billing protections as of February 2021 (Kona, 2021). This includes 18 states with comprehensive
protections that apply to both ED and in-network hospital settings; cover both health maintenance
organization (HMO) and preferred provider organization (PPO) plans; prohibit balance billing; restrict
patient cost sharing to in-network amounts; and establish a formula for determining how much an insurer
will pay a provider in surprise billing scenarios, provide a dispute resolution process for settling
disagreements over payments, or both (Kona, 2021). The structure of surprise billing protections varies
by state, but there are two broad exemptions from state laws. First, pursuant to the Employee Retirement
Income Security Act (ERISA), state surprise billing laws generally do not apply to self-insured employer
plans sponsored by private employers (representing about 64 percent of commercial health coverage
enrollment) (Rosso, Isserman, and Shen, 2021), though in certain states ERISA plans can opt in to state
surprising billing laws. Second, federal law prohibits states from regulating prices of air ambulance
services (Turrini et al., 2021). NSA addresses these gaps in protections for patients by creating federal
protections for certain situations in which the state cannot or chooses not to regulate.
NSA does not supplant state surprise billing laws. If a state has an All-Payer Model Agreement or another
state law that determines payment amounts to OON providers for a service, the All-Payer Model
Agreement or other state law will generally determine the cost-sharing amount and the OON payment
rate. However, if there is a dispute in cases when the state's process does not apply, but NSA does, the
parties can use the Federal IDR process to resolve the dispute.
One complication for evaluating the impacts of NSA is that state methods for addressing surprise bills vary
substantially by state, both in terms of the general approach (i.e., whether the state relies on an IDR
process, directly sets payment standards, or uses a hybrid approach) and in terms of the benchmark rates
that state arbitrators must take into account during the state’s arbitration process or the specified price
levels, as applicable (Kona, 2021) (Table 2-1 ). For example, California sets payment benchmark rates for
nonemergency services at the greater of 125 percent of Medicare rates or the average in-network rate
for a given plan and region, while New York has established an IDR process where the arbitrator is required
to consider the 80
th
percentile of charges in a given region as a benchmark. Some states with surprise
billing laws have modified prior policies to align more closely with NSA standards—which apply to self-
insured plans pursuant to NSA—in order to create a uniform approach and therefore simplify the
regulations for providers and health insurance issuers (Hoadley, O’Brien, and Lucia, 2022; Adler et al.,
2021). Other states may also consider aligning with NSA or addressing perceived gaps in the NSA
protections.

July 2023
REPORT TO CONGRESS
12
Table 2-1 Examples of Payment Determination Methods Under Surprise Billing Laws
Source
Payment Determination
Method
Details
California
Payment standard
• Emergency services: reasonable and customary amounts
• Nonemergency services: greater of 125% of Medicare or average in-
network rate for plan and region
Connecticut
Payment standard and IDR
hybrid
• Emergency services: greater of 80th percentile of charges in region,
in-network rate for plan, amount Medicare would reimburse for such
services
• Nonemergency services: in-network rate for plan unless another
amount is agreed on
New York
IDR
• Arbitrator is required to consider the 80th percentile of charges
Federal –
NSA
Federal IDR
•
Arbitrator is required to consider the Qualified Payment Amount,
generally the median in-network rate for region
•
IDR = independent dispute resolution
SOURCES: AHA, 2021; Corlette and Hoppe, 2019; Keith, Hoadley, and Lucia, 2021; and Kona, 2021.
These state laws represent important factors affecting baseline trends in OON billing and are therefore
important to estimating the independent impact of NSA. Because states generally do not regulate ERISA
plans with respect to surprise billing, many patients even in states that enacted surprise billing restrictions
were not protected by them prior to the implementation of NSA. Figure 2-1 provides an overview of
payment determination methods in NSA and a sample of states with various surprise billing laws enacted
prior to the passage of NSA.
Figure 2-1 – State Surprise Billing Protections Prior to NSA, 2021
Source: Kona, M. (2021) State Balance-Billing Protections. https://www.commonwealthfund.org/node/27021
Additional detail on author’s criteria for comprehensive versus partial protections available:
https://www.commonwealthfund.org/sites/default/files/2019-01/Criteria_for_Meeting_Standards_v2.pdf

July 2023
REPORT TO CONGRESS
13
The Impact of State Surprise Billing Actions: Existing Evidence
Several studies have evaluated the effect of state surprise billing laws on the prevalence of care provided
OON, and in-network and OON rates for health care item and services. This section provides a summary
of these studies. While state surprise billing laws were designed to decrease occurrences of surprise
billing, the potential impacts on in-network and OON prices are less clear. The emerging research suggests
the impacts can be influenced by the regulatory approach taken by the state.
The benchmark rate for payment can be an anchor for prices determined through an arbitration
process.
States varied in their approach to addressing surprise medical bills. In particular, states vary in whether
disputes are resolved through arbitration and what arbitrators should consider as “benchmark” rates for
the arbitration process. In New Jersey and in New York, where arbitrators are required to consider the
80th percentile of charges, average arbitration decisions have been 7–8 percent above the 80th percentile
of charges (Adler, 2019; Chartock et al., 2021). Further, the choice of a payment standard benchmark has
been associated with different trajectories in nonemergency charges after the enactment of surprise
billing protections as compared to states without surprise billing laws. In California, where the arbitration
standard was tied to in-network prices, nonemergency OON charges decreased by 25 percent. In New
York, where the arbitration standard is tied to billed charges, nonemergency OON charges increased by
24 percent (Gordon et al., 2022).
The evidence of the effects of state surprise billing laws on both in-network and OON prices appears
mixed. This may reflect varying state approaches for determining OON prices in scenarios generating
surprise bills. One study found that a state surprise billing law was associated with lower OON prices for
anesthesiologists in California—which stipulates relatively low rates for those services—while another
study found that a state surprise billing law was associated with higher OON prices for emergency services
in Connecticut, which sets relatively high rates for that care (Adler, Duffy, Ly, et al., 2021; La Forgia et al.,
2021). Two studies evaluating the same state (New York) and outcome (in-network prices for emergency
physician services) yielded conflicting results, which suggests the potential difficulty of evaluating these
laws (Adler, Duffy, Fiedler, et al., unpublished; Cooper, Scott Morton, and Shekita, 2020).
Researchers generally found that state surprise billing laws affect in-network prices for covered
services. While state laws regulating or restricting surprise bills most directly impact OON prices, there is
evidence that these laws can also impact in-network prices for health care items and services. In this way,
surprise billing laws can influence health care prices more generally. Among studies finding an association
between state surprise billing laws and in-network prices, two studies also evaluated OON prices and
found that the estimates for in-network and OON prices both decreased (Adler, Duffy, Fiedler, et al.,
unpublished; La Forgia et al., 2021). These results suggest that surprise billing laws can impact OON prices
and in-network prices as well.
Some studies show that state surprise billing laws were associated with an increase in the share of
medical bills that are for in-network care, while others show no significant change. The limited impact
found on in-network rates suggests that state surprise billing laws either increase or do not influence the

July 2023
REPORT TO CONGRESS
14
willingness of providers to join insurer networks. (Adler, 2019; Adler, Duffy, Fiedler, et al., unpublished;
Cooper, Scott Morton, and Shekita, 2020; Maryland Health Care Commission, 2015).
Numerous gaps remain in the understanding of the effects of state surprise billing laws. Evaluations of
state surprise billing laws have yielded varying results. Some of this variation likely stems from variation
in how states determine OON prices in surprise billing scenarios as well as other differences in state
regulation, state health care markets, and other state level variation. Additionally, many of these laws
were recently implemented and understanding the full impact may take some time. Further research is
needed to better understand the impacts of these laws.
To date, evaluations of state surprise billing laws have focused on primary outcomes like prices and rates
of OON claims and have not assessed the effect of these laws on out-of-pocket spending by consumers.
None of these state studies have evaluated downstream effects of the law, such as on total spending,
premiums, health care consolidation, access to health care, or the quality of care.
NSA is in the early stage of implementation and evaluations will evolve as data become available over the
coming years. As NSA is evaluated, it will be important to be cautious in making comparisons with
evaluations of state surprise billing laws which vary in their approach from the federal law. Furthermore,
because NSA was written to defer to some existing state surprise billing laws and limited the degree to
which NSA preempts state laws, many state surprise billing prohibitions continue. The fact that existing
trends likely differ depending on each state’s laws, and that some of these state law provisions will
continue along with NSA provisions, presents both opportunities and challenges as we develop methods
to estimate NSA’s impacts.

July 2023
REPORT TO CONGRESS
15
Chapter 3. Consolidation and Competition – Trends and Evidence of Effects in
Health Care Markets
NSA protections for consumers against surprise medical bills may have other effects on health care
markets. To the extent that NSA results in lower OON prices, providers may choose to move in-network
to increase patient volume if they no longer receive a significant price advantage by staying out of provider
networks. This may cause providers to lose some of their bargaining power with plans and issuers and
result in lower in-network prices (Cooper, Scott Morton, and Shekita, 2020). If these price changes do lead
to decreased bargaining power for providers at their existing levels of market power, they might, in turn,
look to consolidate to increase their market power to recoup some of their lost leverage in bargaining
with plans and issuers.
To the extent NSA creates further incentives for health care providers to increase their market power by
consolidating into larger groups, it is useful to review the literature on consolidation in health care to
anticipate potential impacts if consolidation were to continue, or accelerate, post-NSA.
Terminology – Competition, Concentration, Consolidation
In well-functioning markets, competition provides strong financial incentives for efficiency and value.
Informed consumers shop for the best value in products or services, and sellers compete on the price and
quality of those products or services. The financial incentives in this environment motivate sellers to
innovate to reduce costs and improve their products by adopting new technologies or new business
models. The consequences of not being innovative are that less efficient producers are driven from the
market by more aggressive and creative competitors. In theory, markets that function well to assure lower
prices and higher quality have several characteristics. In general, competition requires that there be a
sufficient number of buyers and sellers, that the buyers are well informed, and that there are relatively
low costs for market entry and exit. In general, competition and its favorable effects on price and quality
decreases with fewer providers offering products or services in a given market. When there are fewer
providers, participants gain market power which insulates them from the competitive forces that assure
the lowest prices and high-quality products.
There are two concepts relevant to describing and measuring the degree of competition or market power
that we focus on in this report: consolidation and concentration. Consolidation refers to actions by
participants that ultimately modify market structure and potentially increase their market power.
Concentration describes market structure as measured by the number and size of the competitors within
that market.
A consolidation event often refers to a merger, purchase, or acquisition of an entity. An entity exiting a
market can also increase the concentration of the remaining market. However, consolidation also
encompasses less formal joint arrangements between organizations. For example, there has been growth
in non-ownership arrangements and affiliations between organizations that allow for joint negotiations,
such as clinically integrated networks (CINs) and accountable care organizations (ACOs) in a form of “soft
consolidation” (Ridgely, Timbie, et al., 2020; Lyu, Chernew, and McWilliams, 2021). Consolidation that

July 2023
REPORT TO CONGRESS
16
eliminates or weakens competition often results in greater market power for the organization and the
potential for less competitive prices and quality. Conversely, a purported benefit of consolidation is that
greater integration will lead to increased efficiencies, coordination of care, and patient outcomes.
However, the achievement of these benefits is most closely tied to the ability of the consolidating
organizations to clinically integrate, which is not guaranteed simply because entities structurally integrate.
Concentration refers to the relative size and number of competitors in a market defined by product and
geography. Market concentration is typically represented by measures such as the Herfindahl-Hirschman
Index (HHI), which is described below. It is important to note that depending on existing market structure
and the size of a merger or acquisition, a given consolidation event may or may not have an appreciable
impact on concentration and market power.
Recent Trends in Health Care Consolidation
In this section, we summarize recent consolidation trends in both provider and insurance markets. More
detailed descriptions can be found in a recent study conducted by the RAND Corporation for ASPE to help
set the baseline for this series of reports to Congress (Liu et al., 2022). In future Reports to Congress, we
will assess how these trends change after the implementation of NSA. Hospital markets are becoming
more concentrated as a result of a steady stream of hospital consolidations. Physician practices have
grown more consolidated in the past decade, with more physicians belonging to larger practices and fewer
physicians in single or small practices (Capps, Dranove, and Ody, 2017; Muhlestein and Smith, 2016; Kane,
2021). Vertical consolidation between hospitals or health systems and physicians is increasing.
Trends in hospital consolidation began to increase in 2010 relative to prior years, though the number of
deals and the number of hospitals involved in the mergers are no higher than in the late 1990s (AHA,
2016; NICHM, 2020). Between 2010 and 2020, there were more than 1,000 announced hospital mergers
and acquisitions (Liu et al., 2022). As displayed in Figure 3-1, since 2017, the number of changes in hospital
ownership have fluctuated on a quarterly basis but do not seem to be subject to an increasing overall
trend. While many of these changes in ownership represent consolidation, some could be health care
systems divesting a hospital or a sale from a larger parent company to a smaller one; the latter two
changes of ownership could plausibly increase competition in a market.

July 2023
REPORT TO CONGRESS
17
30
25
20
15
10
5
0
Figure 3-1 - Changes of Ownership, by Hospital per 1000, by Quarter (Annualized), 2016-2021
Source: W. Pete Welch et al. “Changes of Ownership of Hospital and Skilled Nursing Facilities: An Analysis of Newly Released CMS
Data.”. ASPE Data Point. April 20, 2022.
Physician Markets
Physician group mergers saw a major increase in 2021 (Figure 3-2). This increase occurred after a decline
in 2020 that was presumably related to uncertainty surrounding the COVID-19 pandemic. Whether this
increase is largely a function of mergers that might have otherwise happened in 2020 and were deferred
or whether it represents an accelerating pace of physician group mergers is still unclear.
Changes
in Ownership
(CHOWs)
by Hospital
per
1,000,
by Quarter,
Annualized

July 2023
REPORT TO CONGRESS
18
Figure 3-2 – Physician Medical Groups Mergers and Acquisitions, 2017 - 2021
Source: LevinPro HC, Levin Associates, December 2022 levinassociates.com
Over a longer timeframe, the period since 2017 has had a higher number of physician group mergers than
the years prior to 2017, other than the early partof 2020 when the COVID-19 pandemic initially developed
(Figure 3-3).
Figure 3-3 – Physician Group Mergers and Acquisitions by Month, 2012-2020
Source: LevinPro HC, Levin Associates, December 2022 levinassociates.com
The high number of mergers and acquisitions in 2021 was not focused in practice areas most associated
with surprise billing (i.e. ED, radiology, anesthesiology), though radiology was 11
th
highest among

July 2023
REPORT TO CONGRESS
19
physician specialties by deal volume (Figure 3-4). Again, however, we cannot distinguish here between
acquisitions that represent consolidation versus those that would be neutral or increase competition in a
given market.
Figure 3-4 – Physician Specialties by Merger and Acquisition Deal Volume, 2021
Source: LevinPro HC, Levin Associates, December 2022 levinassociates.com
Again, monitoring the composition of physician specialty mergers will be instructive for whether NSA is
having a major impact on provider consolidation.
Consolidation and Vertical Integration
In general, vertical consolidation or integration refers to a company acquiring or developing one or more
important parts of their production process or supply chain. In recent years, there has been an
acceleration of acquisitions combining traditionally independent elements of the health care supply chain.
Most prominent among these consolidations has been hospitals purchasing or contracting with
physicians’ practices. A recent report estimated that in 2021, nearly 50 percent of physicians were
employed by hospitals (Figure 3-5) (Avalere Health, 2021). Simultaneously, insurers and other corporate
entities also appear to be acquiring physicians’ practices and other health care providers. While the
number of practices employed by hospitals, insurers, and other corporate entities has been rising over
time, the uncertain revenue impacts of the COVID–19 pandemic during 2020 may have accelerated the
trend into 2021.

July 2023
REPORT TO CONGRESS
20
Figure 3-5 – Percent of Physicians Employed by Hospitals and Health Systems, 2019-2021
Source: COVID-19’s Impact On Acquisitions of Physician Practices and Physician Employment 2019-2020. June
2021. Physicians Advocacy Institute, prepared by Avalere Health.
http://www.physiciansadvocacyinstitute.org/Portals/0/assets/docs/Revised-6-8-21_PAI-Physician-Employment-Study-
2021-FINAL.pdf?ver=K6dyoekRSC_c59U8QD1V-A%3d%3d
The acquisition of physician practices by private equity firms has increased in recent years (Tan et al.,
2019; Patel et al., 2019). Private equity investment in anesthesia practices is associated with increased
prices paid to anesthesia practitioners (La Forgia et al., 2022). What role NSA may play in the ongoing
attractiveness of certain specialties to private equity investment is unclear.
Trends in Health Care Market Concentration
Health insurance, hospital, and physician organization markets have been characterized as highly
concentrated for years (Fulton, 2017). This section displays maps of a commonly-used measure of market
concentration in the academic literature and by antitrust agencies, the HHI,
7
for several health care
product markets at several levels of geography.
8
The HHI measures the relative sizes of firms in a market.
7
The Herfindahl–Hirschman Index (HHI) is calculated as the sum of the squared market shares of firms in a given
market and is scaled from 0 to 10,000.
8
Throughout this document, market definitions are not necessarily antitrust product markets nor was a full analysis
conducted in accordance with the U.S. Department of Justice and Federal Trade Commission Horizontal Merger
Guidelines § 5.3 (revised Aug. 19, 2010) that would establish any of these as an antitrust product or geographic
market.
There are multiple potential markets for health insurance and health care items and services. For example, in the
context of commercial health insurance, the DOJ has defined markets for individual, small group, large group, and

July 2023
REPORT TO CONGRESS
21
The measure approaches zero when a market has a large number of firms of equal size (i.e., “perfect
competition”) and reaches its maximum of 10,000 when the market is a monopoly. The Department of
Justice and Federal Trade Commission’s 2010 horizontal merger guidelines generally classify markets into
three types based on their HHI:
• Unconcentrated Markets: HHI below 1500
• Moderately Concentrated Markets: HHI between 1500 and 2500
• Highly Concentrated Markets: HHI above 2500.
9
HHI scores for hospital markets are calculated based on data from the American Hospital Association
Annual Survey. Adjusted hospital admissions
10
were used to measure the market share of each hospital
or hospital system. For these analyses, hospital markets are defined as the hospital referral region (HRR).
HRRs are regional health care markets designated by the Dartmouth Atlas Project (Wennberg and Cooper,
1999). HRRs reflect patterns in inpatient tertiary care referrals while core-based statistical areas (CBSAs)
11
reflect urban commuting patterns.
12
Federal antitrust agencies conduct relevant market analyses on a
case-by-case basis, meaning the relevant markets in antitrust enforcement actions may differ from the
methodology described here.
For at least the past three decades, hospital markets have become increasingly concentrated (Gaynor,
2020). The percentage of HRRs with an HHI <1,500 – meaning unconcentrated – decreased from 23
percent (71 of 306) in 2008 to 12 percent (36 of 306) in 2020 (Figure 3-6).
national accounts. With respect to national accounts, it is not necessarily clear that concentration in a single
geography is informative of overall competition for a given national account.
9
U.S. Department of Justice and Federal Trade Commission, Horizontal Merger Guidelines § 5.3 (2010).
https://www.justice.gov/atr/horizontal-merger-guidelines-08192010#5c
10
AHA’s adjusted admissions measure attempts to capture both inpatient admissions and outpatient volume by
scaling based on relative revenue. Adjusted Admissions = Admissions + (Admissions * (Outpatient Revenue/Inpatient
Revenue))
11
A core based statistical area (CBSA) is that of an area containing a large population center, or urban area, and
adjacent communities that have a high degree of integration with that population center.
12
The increase in remote work and telehealth due to the COVID-19 pandemic may also influence the construction
of relevant markets.

July 2023
REPORT TO CONGRESS
22
Figure 3-6 – Hospital Referral Region (HRR) Level Herfindahl-Hirschman Index (HHI) Scores For
Adjusted Admissions, 2008 and 2020
2008
2020
Source: ASPE Anaylsis of AHA Data
Below, in Figure 3-7, health insurance HHI scores are calculated using Clarivate Managed Market
Surveyor
13
data and are presented at the CBSA level. Markets for health insurance are also frequently
concentrated, but the distribution has not changed substantially in recent years. In 2008, 31 percent of
13
Clarivate Managed Market Surveyor captures enrollment of health lives and affiliations by payer and geography.

July 2023
REPORT TO CONGRESS
23
CBSAs had commercial health insurance HHI scores below 1,500 (120 of 384). In 2020, a similar 35 percent
of CBSAs had commercial health insurance HHI scores below 1,500 (134 of 384).
Figure 3-7 – Core-based Statistical Area (CBSA) Level Herfindahl-Hirschman Index (HHI) Scores for
Commercial Health Insurance Membership, 2008 and 2020
2008
2020
Source: ASPE Anaylsis of Clarivate|Clarivate Managed Market Surveyor

July 2023
REPORT TO CONGRESS
24
Impact of Consolidation and Concentration on Health Care Outcomes: Current Evidence
As part of an environmental scan of evidence on consolidation trends and the impacts of consolidation on
price, quality, and access to health care in health care provider and insurance markets conducted by the
RAND Corporation for ASPE, researchers reviewed 172 articles for evidence of the effects of consolidation
on these outcomes (Liu et al., 2022). They found strong evidence that hospital horizontal consolidation is
associated with higher prices paid to providers and some evidence of the same for vertical consolidation
of hospitals and physician practices. Few studies have directly examined total spending rather than prices
for items and services.
The report found that horizontal consolidation of commercial insurers is associated with lower prices paid
to providers as insurers gain market power in negotiations with providers. However, the lower prices paid
to providers do not appear to be passed onto consumers, who face higher premiums following insurer
consolidation.
The report also assessed the evidence of the effects of consolidation on quality of care. These assessments
of quality can be challenging to generalize as quality performance is complex and multifaced.
Furthermore, studies often examine a small number of quality measures that may not overlap with those
used in other studies. Studies often examine a specific instance of a merger rather than examine effects
nationally. These studies show mixed findings depending on the quality measures studied, setting, and
degree of integration. Several studies show no change in most quality measures following horizontal and
vertical consolidation. Other studies find mixed effects that vary with the degree of vertical integration.
There was insufficient evidence of the effects of horizontal or vertical consolidation on patient access to
health care, and low or insufficient evidence on the effects of consolidation on health care wages.
Despite increasing interest in the effects of consolidation in other care settings such as pharmacy and
telehealth provider markets as well as growing attention to private equity ownership and investment, the
report found insufficient or weak evidence on the effects of these changes in health care markets. Most
of the empirical studies included in the report on private equity investments focused on nursing homes,
and findings were either mixed or too limited to draw clear conclusions.
The report found moderate evidence that an expanding scope of practice is associated with, if anything,
a decrease in health care spending and increase in access to health care and quality of care, but the report
found insufficient evidence on the effects on health care prices and wages. The report also found
moderate evidence that certificate of need laws
14
are associated with no change or a decrease in health
care quality, but the evidence was low or insufficient for other outcomes.
The report found limited mixed evidence on the effects of hospital and physician consolidation on the
provision of charity care and insufficient evidence on its effects on medical debt burden and collection
14
Certificate of need (CON) laws requirehealthcare providers to obtain permission from a state (or state-authorized)
agency to construct new healthcare facilities, expand existing ones, or offer certain healthcare services.

July 2023
REPORT TO CONGRESS
25
(not shown in Appendix C). The report found no studies examining the effects of insurer consolidation on
charity care and medical debt.
State surprise billing protections are relatively new. The report noted, that, to date, the effects of these
protections on prices have been heterogeneous depending on the various approaches taken and their
implementation. Few studies have examined outcomes other than prices.
The report also identified areas where there are gaps in evidence. Non-ownership forms of consolidation
that involve contractual arrangements or memorandum of understanding agreements between hospitals
or health systems and physicians are understudied and often difficult for researchers to measure. The
report noted that in addition to the limited evidence of the average effects of consolidation on quality of
care, there is very little evidence on the heterogeneity of these effects on quality for different care
settings, subpopulations, and extent of integration.
Table 3-1 Condensed Summary of Consolidation Effects on Health Care Prices, Spending, Quality,
Access, and Wages
Domain
Health Care
Prices
Health Care
Spending
Quality of
Care
Patient
Access
Health Care
Wages
Horizontal
Hospital
Increase
a
Increase
a
Mixed
depending
on measure
and setting
b
Possible
decrease
d
Decrease
a
Physician
Increase
a
Mixed
d
Mixed
d
No
evidence
d
No
evidence
d
Commercial
insurers
Decrease
c
Increase in
premiums
a
Possible
increase in
patient
experience
d
No direct
evidence,
might
decrease
with
premium
increase
d
Possible
decrease
d
Vertical
Hospitals and
physicians
Mixed:
increase or
no change
a
Increase
a
Mixed: small
increase or
no change
b
Possible
increase
d
Mixed
d
a
Cells shaded in red indicate effects that have sufficient SOE and are detrimental to consumers.
b
Cells shaded in yellow indicate effects that have sufficient SOE and are unclear for consumers.
c
Cells shaded in green indicate effects that have sufficient SOE and are beneficial to consumers.
d
Cells shaded in gray indicate effects that have insufficient SOE.
Appendix C summarizes the report’s assessment based on its environmental scan.

July 2023
REPORT TO CONGRESS
26
Chapter 4. Descriptive Analysis of Trends in OON Billing – Baseline Before
NSA Implementation
Recent Trends in OON and Surprise Bills
To anticipate potential impacts of NSA on the health care system, it is important to understand where its
provisions are most likely to have an impact. The providers, items and services, and patients most
associated with OON and surprise bills prior to NSA are likely to be the parties most affected by the law.
In addition, items and services with the largest differences between in-network and OON rates will be
most impacted by restrictions on balance billing and cost-sharing as well as the Federal IDR process which
change the dynamics of negotiation between payers and providers.
This section presents an analysis of Health Care Cost Institute (HCCI) data presenting descriptive statistics
of the trends and variation in OON billing in the United States in the period before NSA was enacted. The
HCCI 2.0 data contain claim and enrollment information for 55 million commercially insured individuals
per year between 2012 and 2020. The data are from three national insurers – Aetna, Humana, Kaiser
Permanente – and Blue Health Intelligence
15
. Together, the data constitute roughly one-third of enrollees
with employer-sponsored insurance in the United States, covering all 50 states. Below, in Figure 4-1, the
time trend of OON prevalence from 2012 to 2020 is shown. When presenting a snapshot of OON
prevalence by patient or provider characteristics for a given year, we show 2019 rather than 2020 data
due to possible effects from the COVID-19 pandemic
There are limitations to this analysis. It examines all types of OON billing, including OON bills incurred at
in-network and OON facilities, not surprise billing specifically. A recent study found the share of total
spending that occurred OON ranged from 6 to 8 percent in 2014 to 2017, which is similar to the results
presented here (Song et al., 2020). In contrast, studies focused on OON bills incurred at in-network
inpatient facilities from 2014 to 2016 found that about 15 percent of admissions had at least one
associated OON professional claim (Garmon and Chartock, 2017; Kennedy, Johnson, and Fuglesten Biniek,
2019). Additionally, while data on all states are included, the data may be less representative in states
where the largest commercial insurers are not included in the HCCI data.
OON prevalence is defined as the share of claims that were OON out of all professional claims. The HCCI
2.0 data include a network status flag that indicates whether the claim was paid in-network or OON. This
analysis focuses on professional claims since surprise billing often occurs for physician or other
professional services furnished by an OON provider at an in-network facility. While inpatient and
outpatient facility claims can be OON, the network status of facilities may be known for non-emergency
services, and therefore bills from OON inpatient and outpatient facilities may be less commonly
unexpected to the patient than professional claims. The network status for both facility and professional
claims for emergency services can be unknown to the patient at the time of care, but an OON facility claim
for an emergency service would typically be accompanied by OON professional claims as well.
15
Blue Health Intelligence is a data and analytics company that is a licensee of the Blue Cross Blue Shield Association
and that collects and maintains claims data from the 36 independent Blue Cross Blue Shield licensee insurance
companies.

July 2023
REPORT TO CONGRESS
27
Additionally, in some circumstances, a patient may affirmatively choose to receive services from an OON
provider, a decision that would not be captured by claims data if the patient chooses to finance the service
out-of-pocket.
Overall Trends in OON Billing
The overall prevalence of professional claims that were OON decreased from 6.0 percent to 4.7 percent
from 2012 to 2020 (Figure 4-1). Similarly, the share of payments that were OON out of total payments
also declined over this period from 9.2 percent in 2012 to 6.8 percent in 2020 (data not shown). These
declines seem to have been robust across insurance type, geography (urban vs. rural), age, and sex.
Figure 4-1 - OON Prevalence, 2012-2020
7%
6%
5%
4%
3%
2%
1%
0%
2012 2013 2014 2015 2016 2017 2018 2019 2020
Source: RAND analysis of OON trends using Health Care Cost Institute 2.0 data
Geographic Variation in OON prevalence
In 2019, 4.6 percent of professional claims were OON. However, there was substantial variation in the
rates of OON claims by state. Rates of OON claims were generally higher in the southwest and east than
in other regions of the country. Alaska (20.2 percent) had the highest rate of OON claims, and Nebraska
(1.8 percent) had the lowest.
OON Prevalence

July 2023
REPORT TO CONGRESS
28
Figure 4-2 - OON Prevalence by State, 2019
Source: Analysis of OON trends using Health Care Cost Institute 2.0 data
Figure 4-3 below shows rates of OON prevalence by urban vs. rural residence based on patient ZIP code.
Overall, among all professional claims, OON prevalence was slightly higher in urban areas than in rural
areas though the decline in OON prevalence has been similar for both in the period 2012 to 2020.
Figure 4-3 - OON Prevalence by Urban versus Rural Zip code of Residence
7%
6%
5%
4%
3%
2%
1%
0%
2012 2013 2014 2015 2016 2017 2018 2019 2020
Source: Analysis of OON trends using Health Care Cost Institute 2.0 data
Insurance Plan Type
The share of claims that are OON was highest among those with point of service (POS) insurance, with
health maintenance organizations (HMO) next, and preferred provider organizations ( PPO) the lowest.
The rate of OON claims jumped for HMO and PPO plans in 2020, but declined from 2012-2019 for all plan
Urban
Rural
OON Prevalence

July 2023
REPORT TO CONGRESS
29
types; the gap between the rates of OON claims in POS/HMO plans and PPO plans also shrank over this
time period.
Figure 4-4 - OON Prevalence by Insurance Plan Type
14%
12%
10%
8%
6%
4%
2%
0%
2012 2013 2014 2015 2016 2017 2018 2019 2020
Source: Analysis of OON trends using Health Care Cost Institute 2.0 data
Age
OON claims were most common among those aged 18-24 and least common for those aged 55-64. The
share of claims that are OON for all age groups has declined from 2012-2020.
Figure 4.5 - OON Prevalence by Patient Age
10%
8%
6%
4%
2%
0%
2012 2013 2014
2015 2016 2017 2018 2019 2020
Source: Analysis of OON trends using Health Care Cost Institute 2.0 data
Sex
The percentages of claims that are OON were consistently higher for men than for women, though both
have seen similar declines in the percentage of OON claims from 2012- 2020.
HMO
PPO
POS
0-17
25-34
45-54
18-24
35-44
55-64
OON Prevalence
OON Prevalence

July 2023
REPORT TO CONGRESS
30
Figure 4-6 - OON Prevalence by Gender
7%
6%
5%
4%
3%
2%
1%
0%
2012 2013 2014 2015 2016 2017 2018 2019 2020
Source: Analysis of OON trends using Health Care Cost Institute 2.0 data
OON Prevalence by Provider Characteristics
In Figure 4-7, physicians are grouped by the share of their total claims that were billed OON. The majority
of physicians had a very low prevalence of OON bills. Approximately 56 percent of physicians billed one
percent or less of their claims as OON and 70 percent of physicians billed 2 percent or fewer OON claims
(0-1 percent and 1-2 percent bars combined). Just over 5 percent of physicians billed the majority of their
claims OON.
Figure 4-7 - Share of Physician National Provider Identifiers (NPIs) by OON Billing Prevalence, 2019
60%
50%
40%
30%
20%
10%
0%
0-1% 1-2% 2-3% 3-4% 4-5% 5-10% 10-50% 50-100% 100%
OON Prevalence
Source: Analysis of 2019 OON prevalence using Health Care Cost Institute 2.0 data
The prevalence of physician OON billing varied by physician specialty. Some specialties show much higher
rates of OON billing than others. Psychiatry, emergency medicine, pathology, pain medicine, and
anesthesiology all billed greater than 4 percent of their claims OON on average.
Female
Male
Share
of Billing NPIs
OON Prevalence

July 2023
REPORT TO CONGRESS
31
Figure 4-8 - OON Prevalence for Selected Specialties, 2019
12%
10%
8%
6%
4%
2%
0%
Source: Analysis of 2019 OON prevalence using Health Care Cost Institute 2.0 data
Another factor in the rate of OON bills is the place of service. Claims from EDs (13 percent) and ASCs (8
percent) were more likely to be OON than office visits (4 percent).
Figure 4-9 - OON Prevalence by Place of Service, 2019
14%
12%
10%
8%
6%
4%
2%
0%
ED ASC Inpatient
Hospital
Independent
Laboratory
Office Outpatient
Hospital
Pharmacy
Source: Analysis of 2019 OON prevalence using Health Care Cost Institute 2.0 data
OON Prevalence
OON Prevalence

July 2023
REPORT TO CONGRESS
32
Chapter 5. A Conceptual Framework and Potential Methods
NSA requires the Secretary, in consultation with the Federal Trade Commission and Attorney General, to
study the effects of certain NSA provisions on consolidation, overall health care costs, and access to health
care items and services. The provisions of NSA may have several other potential effects on health care
markets and their outcomes including out-of-pocket spending, prices, and quality. In this chapter, we
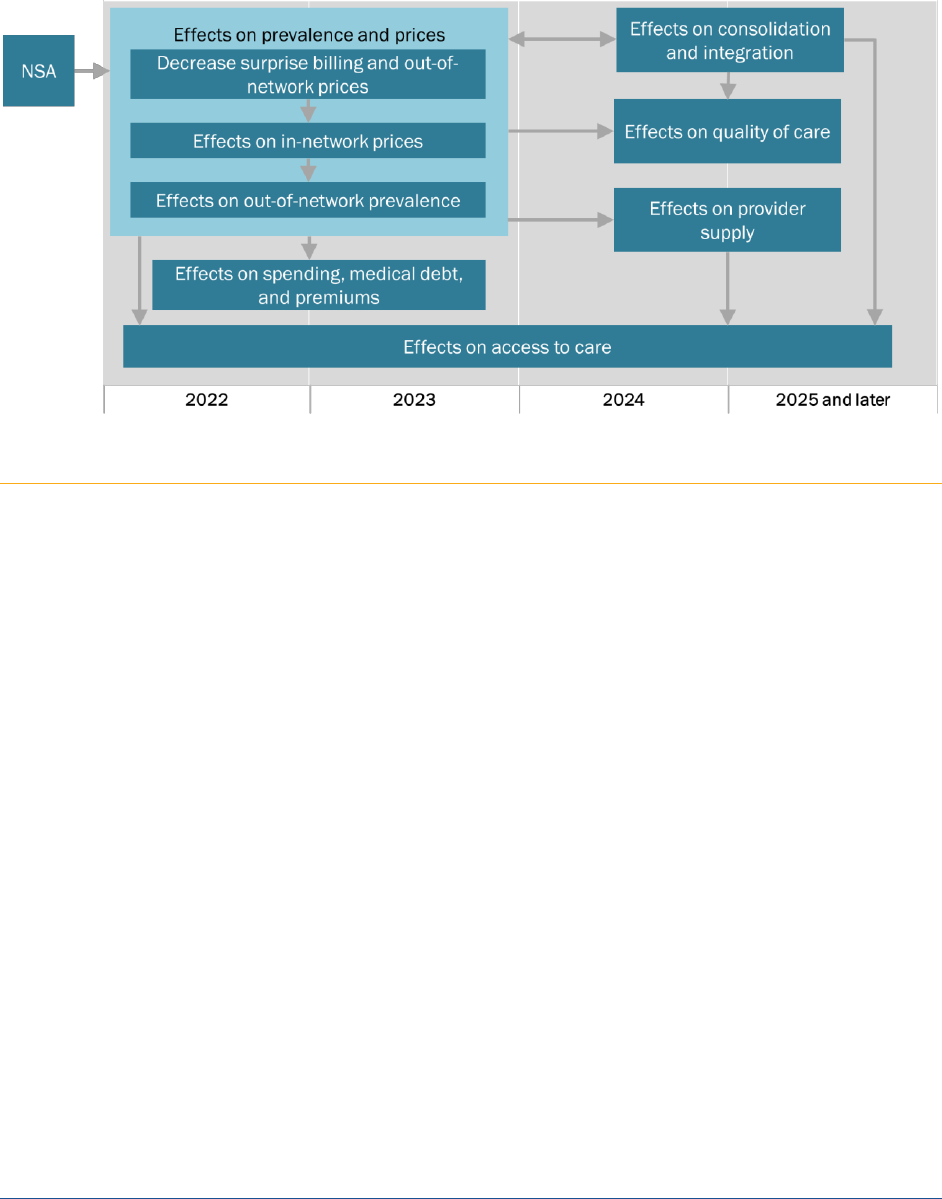
present a framework for understanding these effects and their interrelationships. Figure 5.1 summarizes
the potential effects NSA may have on health care market outcomes.
NSA creates financial protections for certain patients and establishes a process for determining OON
payment rates for certain surprise billing scenarios. Thus, a primary effect of NSA should be to reduce the
number of surprise bills and the out-of-pocket spending associated with them. A potential downstream
effect of the reduced out-of-pocket liability is that medical debt may be reduced.
These effects may extend beyond the financial protections afforded to patients for certain OON items and
services. To the extent that negotiations between providers and plans and issuers regarding payment
rates consider the rates providers would receive if they remain OON, there could be impacts on both in-
network rates and network participation by the providers. For example, in some areas, providers may see
attractive OON billing opportunities as an alternative to joining an issuer’s or plan’s network. By modifying
expectations about OON payments, the NSA may change the bargaining dynamic between plans and
issuers and providers and place more pressure on providers to join plan and issuer networks. The resulting
changes to network structures could further reduce the incidence of OON billing. Alternatively, providers
may believe that IDR process provides them with higher reimbursement than they would be able to
negotiate themselves, and making providers more willing to go out-of-network.
To the extent that these pressures provide more market power for issuers, they may be able to negotiate
lower in-network prices. Lower in-network prices could reduce growth in premiums and overall health
care spending, though as noted above, the evidence is not clear that such savings are consistently passed
on to consumers – particularly in the insurer market itself is highly concentrated.
Changes in prices may affect provider decisions regarding consolidation, provider supply (e.g., staffing),
and investments in quality improvement over the long term. Changes in the supply of providers would in
turn have implications for access to health care, and changes in consolidation could influence prices,
access to health care, and quality of care.
One possible response to this dynamic is providers seeking to strengthen their bargaining positions by
increasing their market power through consolidation. In turn, changes in market consolidation can
adversely affect prices and quality of care (see Chapter 3). Thus, as indicated in Figure 5-1, NSA may have
direct effects on these outcomes of interest as well as indirect effects on them through changes in market
consolidation.
July 2023
REPORT TO CONGRESS
33
Figure 5-1 - Potential Effects of NSA
Looking Forward: Planning for Future Research and Methods for Evaluating the Impact of NSA
Estimating the independent effects of NSA on the key outcomes in Figure 5-1 will be very challenging and
may require a variety of statistical methods and data sources. In this report, we include baseline
information on important trends – such as the prevalence of OON bills – that will be critical to conducting
these analyses. In this section, we describe the potential methodologies that could be applied in future
reports to analyze the impact of NSA on the key outcomes of interest. These methods include both
quantitative and qualitative analyses.
Interested-Party Discussions
Discussions with interested parties can generate information about the impact of NSA where there is a
lack of quantitative data or when evaluating NSA empirically would be difficult. These discussions can also
lead to uncovering important areas of impact not previously considered and suggesting other qualitative
(e.g., provider surveys) or quantitative analyses.
Interested-party discussions may be especially informative early in the implementation of NSA while key
sources of quantitative data are unavailable. Interested-party discussions and other qualitative methods
will continue to play an important role in later years, especially given the limitations of quantitative
approaches for assessing the nationwide implementation of NSA.

July 2023
REPORT TO CONGRESS
34
Descriptive Analysis
A descriptive analysis of quantitative data can show changes in outcomes following implementation of
NSA. In addition to evaluating changes in outcomes and trends, descriptive analysis can include outcomes
that would only be available after implementation of NSA (e.g., consumer complaints submitted via the
federal surprise billing complaints process). This report establishes some baseline trends in OON and
surprise billing (see Chapter 4) that we anticipate tracking in future reports.
In some instances, only descriptive analyses will be possible with the available data.
Quantitative Analyses
Estimating the independent impacts of NSA on key outcomes such as prices, spending, quality, access to
health care, and market consolidation will require the use of statistical modeling and leveraging multiple
research designs. Below we describe the potential methods that may be applied as the appropriate data
become available.
Interrupted Time Series (ITS) Methods
Interrupted Time Series (ITS) is a statistical analysis in which a period of time before an intervention is
compared to a period of time after an intervention, controlling for certain observable influences. The
difference between those trends – in rate and level – is one way to measure the effect of the interruption
or intervention. An ITS approach can evaluate a given outcome over time to assess whether the change
(e.g., an increase or decrease in prices for emergency services) occurred immediately following the
implementation of NSA.
As described above, many factors other than the implementation of NSA have likely affected trends in the
outcomes of interest. Therefore, ITS is not a strong method for attributing observed changes in these
trends fully or even partially to NSA. A stronger method is known as comparative interrupted time series
(CITS) in which changes in trends are analyzed and compared between a group subject to NSA and a similar
group not subject to NSA. One advantage of this approach is that it allows for the possibility that other
factors, such as the COVID-19 pandemic, may affect outcomes as long as that factor has the same effect
on both the treatment and comparator groups. While NSA will be implemented nationally, one approach
for this design might be to compare the trends for states that had strong surprise billing laws prior to NSA
with those that had no laws or weaker ones; alternatives could be to examine trends for service types or
providers in fields more likely to have sent surprise bills prior to NSA, compared to service types or
providers less likely to be impacted by the law. One disadvantage to CITS is that it requires the availability
of several data points both before and after implementation of NSA.
Difference-in-Difference Analysis
Difference-in-difference (DID) is a similar statistical technique to CITS in that it compares trends in
outcomes measured from a “treatment” group and a “comparison” group. After adjusting for some
observable differences between the groups, outcome differences that change more for the treatment

July 2023
REPORT TO CONGRESS
35
group than the control group are thought to be associated with the treatment. In contrast to CITS, DID
can use a single time point before and after the treatment, often an average calculated for those time
periods. Thus, fewer time periods of data are needed for DID than for CITS. A disadvantage to this
approach is that it assumes that the trends occurring prior to NSA would have continued similarly if not
for the law.
For the future reports, we will carefully examine relevant data as it becomes available and examine the
appropriate application of these methods to estimating changes in key outcomes.

July 2023
REPORT TO CONGRESS
36
Chapter 6. Conclusion
NSA provides protections for patients against the financial consequences of many surprise bills in certain
circumstances. Surprise bills occur when individuals with a private health plan or coverage receive
unexpectedly high medical bills when they are unknowingly treated by an out-of-network (OON) provider.
For items and services furnished in certain situations, the law places requirements on both providers and
health plans and issuers to limit patients’ out-of-pocket consequences of surprise bills.
While the primary intended effect of NSA is to reduce the number of surprise bills and the associated
adverse financial consequences for patients, there are several potential health care market impacts that
may also occur. For this and subsequent reports, HHS, in consultation with the Federal Trade Commission
and the Attorney General, intend to examine the potential impacts on market consolidation, overall
health care costs, and access to health care items and services. This report presents a conceptual model
of how NSA may affect several related outcomes such as in-network and OON pricing, insurance and
health plan premiums, and quality of care. Health insurance and health plan claims data for items and
services furnished after the implementation of NSA should become available during 2023 and will be used
for the next report due January 2024.
There will be significant challenges for estimating these NSA effects relative to other important influences
on trends in the outcomes of interest. In beginning to address these challenges, we have provided baseline
information on OON billing, market consolidation and concentration, and current state surprise billing
laws already in effect. Subsequent reports will employ a variety of methodological approaches to examine
changes in these trends that may be attributable to the implementation of NSA.

July 2023
REPORT TO CONGRESS
37
References
Adler, Loren, Experience with New York’s Arbitration Process for Surprise Out-of-Network Bills, USC-
Brookings Schaeffer on Health Policy, October 24, 2019. https://www.brookings.edu/blog/usc-
brookings-schaeffer-on-health-policy/2019/10/24/experience-with-new-yorks-arbitration-process-for-
surprise-out-of-network-bills/
Adler, Loren, Erin Duffy, Matthew Fiedler, Paul Ginsburg, Bich Ly, and Erin Trish. The Impact of New
York’s Surprise Out-of-Network Billing Law on Payment Rates to Emergency Physicians, USC-Brookings
Schaeffer on Health Policy, unpublished.
Adler, Loren, Erin Duffy, Bich Ly, Conrad Milhaupt, and Erin Trish, Changes in Emergency Physician
Service Prices After Connecticut’s 2016 Surprise Billing Law, 2021.
https://www.brookings.edu/essay/changes-in-emergency-physician-service-prices-after-connecticuts-
2016-surprise-billing-law
American Hospital Association, “Hospital and Physician Groups File Lawsuit Over No Surprises
Act Final Rules That Jeopardize Patient Access to Care,” December 10, 2021. https://www.aha.org/legal-
documents/2021-12-10-hospital-and-physician-groups-filelawsuit-over-no-surprises-act-final
American Hospital Association. Announced Hospital Mergers and Acquisitions, 1998 – 2015. Trendwatch
Chartbook 2016. https://www.aha.org/system/files/research/reports/tw/chartbook/2016/chart2-9.pdf
ASPE “HHS Secretary’s Report on: Addressing Surprise Medical Billing.” A Report Required by Executive
Order 13877. Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health
and Human Services. July 2020. https://aspe.hhs.gov/reports/hhs-secretarys-report-addressing-surprise-
medical-billing
ASPE “Evidence on Surprise Billing: Protecting Consumers with the No Surprises Act.” Issue Brief No. HP-
2021-24. Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and
Human Services. November 2021. https://aspe.hhs.gov/reports/evidence-surprise-billing
Avalere Health. “COVID-19’s Impact On Acquisitions of Physician Practices and Physician Employment
2019-2020.” June 2021. http://www.physiciansadvocacyinstitute.org/Portals/0/assets/docs/Revised-6-
8-21_PAI-Physician-Employment-Study-2021-FINAL.pdf?ver=K6dyoekRSC_c59U8QD1V-A%3d%3d
Board of Governors of the Federal Reserve System. “Economic Well-Being of U.S. Households in 2022.”
May 2023. https://www.federalreserve.gov/publications/files/2022-report-economic-well-being-us-
households-202305.pdf
Capps, Cory, David Dranove, and Christopher Ody, “Physician Practice Consolidation Driven by Small
Acquisitions, So Antitrust Agencies Have Few Tools to Intervene,” Health Affairs, Vol. 36, No. 9,
September 2017, pp. 1556–1563.
Cooper, Zack, and Fiona Scott Morton. "Out-of-network emergency-physician bills—an unwelcome
surprise." New England Journal of Medicine. Vol. 375, No. 20. November 17 2016, pp. 1915-1918.

July 2023
REPORT TO CONGRESS
38
Cooper, Zack, Fiona Scott Morton, and Nathan Shekita, "Surprise! Out-of-Network Billing for Emergency
Care in the United States," Journal of Political Economy, Vol. 128, No. 9, September 1, 2020, pp. 3626-
3677.
Corlette, Sabrina, and Olivia Hoppe, “New York’s Law to Protect People from Surprise Balance Bills Is
Working as Intended, but Gaps Remain,” CHIRblog, May 13, 2019. http://chirblog.org/new-york-law-
surprise-balance-billing/
The Departments of Treasury, Labor, and Health and Human Services. "Initial Report on the Independent
Dispute Resolution (IDR) Process April 15 – September 30, 2022."
https://www.cms.gov/files/document/initial-report-idr-april-15-september-30-2022.pdf
Fulton, Brent D., “Health Care Market Concentration Trends in the United States: Evidence and
Policy Responses,” Health Affairs, Vol. 36, No. 9, September 2017, pp. 1530–1538.
Hoadley, Jack, Madeline O'Brien, and Keving Lucia, “No Surprises Act: A Federal-State Partnership to
Protect Consumers from Surprise Medical Bills,” Commonwealth Fund, October 2022.
https://www.commonwealthfund.org/publications/fund-reports/2022/oct/no-surprises-act-federal-
state-partnership-protect-consumers
Garmon, Christopher, and Benjamin Chartock, “One in Five Inpatient Emergency Department Cases May
Lead To Surprise Bills,” Health Affairs, Vol. 36, No. 1, January 2017, pp. 177–181.
Gaynor, Martin. "What to Do about Health‐ Care Markets? Policies to Make Health‐ Care Markets
Work." Hamilton Project Policy Proposal 2020-10, March 2020.
Goddard, Maria, “Competition in Healthcare: Good, Bad or Ugly?” International Journal of Health Policy
and Management, Vol. 4, No. 9, September 2015, pp. 567–569.
Gordon, Aliza S et al. “Provider Charges And State Surprise Billing Laws: Evidence From New York And
California.” Health Affairs Vol. 41, No. 9, September 2022, pp.1316-1323.
Hamel, Liz et al. "The Burden of Medica Debt: Results from the Kaiser Family Foundation/New York
Times Medical Bills Survey." Kaiser Family Foundation Report. January 2016. https://www.kff.org/wp-
content/uploads/2016/01/8806-the-burden-of-medical-debt-results-from-the-kaiser-family-foundation-
new-york-times-medical-bills-survey.pdf
Hamel, Liz, Caley Muñana, and Mollyann Brodie. "Kaiser Family Foundation/LA Times Survey Of Adults
With Employer-Sponsored Health Insurance." May 2019. https://files.kff.org/attachment/Report-KFF-
LA-Times-Survey-of-Adults-with-Employer-Sponsored-Health-Insurance
Kane, Carol K., Recent Changes in Physician Practice Arrangements: Private Practice Dropped to Less
Than 50 Percent of Physicians in 2020, Chicago, Ill.: American Medical Association, 2021.
Keith, Katie, Jack Hoadley, and Kevin Lucia, “Banning Surprise Bills: Biden Administration Issues First Rule
on the No Surprises Act,” Health Affairs Blog, July 6, 2021.
https://www.healthaffairs.org/do/10.1377/hblog20210706.903518/full/

July 2023
REPORT TO CONGRESS
39
Kona, Maanasa, “State Balance-Billing Protections,” Commonwealth Fund, webpage, February 5, 2021.
https://www.commonwealthfund.org/publications/maps-and-interactives/2021/feb/state-balance-
billing-protections
La Forgia, A., A. M. Bond, R. T. Braun, K. Kjaer, M. Zhang, and L. P. Casalino, "Association of Surprise-
Billing Legislation with Prices Paid to In-Network and Out-of-Network Anesthesiologists in California,
Florida, and New York: An Economic Analysis," JAMA Intern Med, Vol. 181, No. 10, Oct 1, 2021, pp.
1324-1331
La Forgia, A., et al. “Association of Physician Management Companies and Private Equity Investment
With Commercial Health Care Prices Paid to Anesthesia Practitioners.” JAMA Intern Med, Vol. 182, No.
4, February 22, 2022, pp. 396-404.
Liu, Jodi L., Zachary M. Levinson, Annetta Zhou, Xiaoxi Zhao, PhuongGiang Nguyen, and Nabeel Qureshi,
Environmental Scan on Consolidation Trends and Impacts in Health Care Markets, Office of the Assistant
Secretary for Planning and Evaluation. 2022.
Lyu, Peter F., Michael E. Chernew, and J. Michael McWilliams, “Soft Consolidation in Medicare ACOs:
Potential for Higher Prices Without Mergers or Acquisitions,” Health Affairs, Vol. 40, No. 6, June 2021,
pp. 979–988.
The Maryland Health Care Commissions. "Impact of the Assignment of Benefits Legislation, January 15,
2015. https://mhcc.maryland.gov/mhcc/pages/plr/plr/documents/LGSPT_AOB_rpt_20150115.pdf
Muhlestein, David B., and Nathan J. Smith, “Physician Consolidation: Rapid Movement from Small to
Large Group Practices, 2013–15,” Health Affairs, Vol. 35, No. 9, September 2016, pp. 1638–1642.
National Institute for Health Care Management Foundation. "Hospital Consolidation: Trends, Impacts
and Outlook." January 2020. https://nihcm.org/assets/articles/nihcm-consolidation-charts-updated-
010920.pdf.
Patel Shriji N., Sylvia Growth, Paul Sternberg Jr., “The Emergence of Private Equity in Ophthalmology,”
JAMA Ophthalmology, Vol. 137, No. 6, May 2, 2019, pp. 601-602.
Pollitz K, Lopes L, Kearney A, et al. US Statistics on Surprise Medical Billing. JAMA. 2020;323(6):498.
https://jamanetwork.com/journals/jama/fullarticle/2760721#:%7E:text=Overall%2C%20two%2Dthirds%
20of%20adults,but%20rates%20vary%20by%20state
Public Law 116-260, Consolidated Appropriations Act, Sec. 109, No Surprises Act, December 11, 2019.
Ridgely, M. Susan, Justin W. Timbie, Laura J. Wolf, Erin Lindsey Duffy, Christine Buttorff, Ashlyn Tom, and
Mary E. Vaiana, Consolidation by Any Other Name: The Emergence of Clinically Integrated Networks,
Santa Monica, Calif.: RAND Corporation, RR-A370-1, 2020.
https://www.rand.org/pubs/research_reports/RRA370-1.html
Ridgely, M. S., C. Buttorff, L. J. Wolf, E. L. Duffy, A. K. Tom, C. L. Damberg, D. P. Scanlon, and M. E.
Vaiana, "The Importance of Understanding and Measuring Health System Structural, Functional, and
Clinical Integration," Health Serv Res, Vol. 55 Suppl 3, No. Suppl 3, Dec, 2020, pp. 1049-1061.

July 2023
REPORT TO CONGRESS
40
Rosso, Ryan J., Noah D. Isserman, and Wen W. Shen, Surprise Billing in Private Health Insurance:
Overview of Federal Consumer Protections and Payment for Out-of-Network Services, Washington, D.C.:
Congressional Research Service, R46856, July 26, 2021.
Song, Zirui, William Johnson, Kevin Kennedy, Jean Fuglesten Biniek, and Jacob Wallace, "Out-of-Network
Spending Mostly Declined in Privately Insured Populations with a Few Notable Exceptions from 2008 to
2016," Health Affairs, Vol. 39, No. 6, 2020, pp. 1032-1041.
Sun, Eric C., Michelle M. Mello, Jasmin Moshfegh, and Laurence C. Baker. “Assessment of Out-of-
Network Billing for Privately Insured Patients Receiving Care in In-Network Hospitals,” JAMA Internal
Medicine, Vol. 179, No. 11, August 12, 2019, pp. 1543–1550.
Tan Sally, Kira Seiger, Peter Renehan, “Trends in private equity acquisition of dermatology practices in
the United States,” JAMA Dermatolology, Vol. 155, No. 9, July 24, 2019, pp. 1013-1021.
Turrini, Gina, Joel Ruhter, Andre R. Chappel, Nancy De Lew. “Air Ambulance Use and Surprise Billing.”
ASPE Issue Brief. September 10, 2021. https://aspe.hhs.gov/sites/default/files/2021-09/aspe-air-
ambulance-ib-09-10-2021.pdf.
Wennberg, John E., and Megan McAndrew Cooper. "The Quality of Medical Care in the United States: A
Report on the Medicare Program: The Dartmouth Atlas of Health Care 1999: The Center for the
Evaluative Clinical Sciences." (1999).

July 2023
REPORT TO CONGRESS
41
Appendix A. Section 109 of the No Surprises Act
SEC. 109. REPORTS.
(a) REPORTS IN CONSULTATION WITH FTC AND AG.—Not later than January 1, 2023, and annually
thereafter for each of the following 4 years, the Secretary of Health and Human Services, in consultation
with the Federal Trade Commission and the Attorney General, shall—
(1) conduct a study on the effects of the provisions of, including amendments made by, this Act
on—
(A) any patterns of vertical or horizontal integration of health care facilities, providers,
group health plans, or health insurance issuers offering group or individual health
insurance coverage;
(B) overall health care costs; and
(C) access to health care items and services, including specialty services, in rural areas and
health professional shortage areas, as defined in section 332 of the Public Health Service
Act (42 U.S.C. 254e);
(2) for purposes of the reports under paragraph (3), in consultation with the Secretary of Labor
and the Secretary of the Treasury, make recommendations for the effective enforcement of
subsections (a)(1)(C)(iv) and (b)(1)(C) of section 2799A–1 of the Public Health Service Act,
subsections (a)(1)(C)(iv) and (b)(1)(C) of section 716 of the Employee Retirement Income Security
Act of 1974, and subsections (a)(1)(C)(iv) and (b)(1)(C) of section 9816 of the Internal Revenue
Code of 1986, including with respect to potential challenges to addressing anti-competitive
consolidation of health care facilities, providers, group health plans, or health insurance issuers
offering group or individual health insurance coverage; and
(3) submit a report on such study and including such recommendations to the Committees on
Energy and Commerce; on Education and Labor; on Ways and Means; and on the Judiciary of the
House of Representatives and the Committees on Health, Education, Labor, and Pensions; on
Commerce, Science, and Transportation; on Finance; and on the Judiciary of the Senate.

July 2023
REPORT TO CONGRESS
42
Appendix B. Recent State Balance Billing Protections
STATUS OF BALANCE BILLING PROTECTION - OVER YEARS
States
By 2017
By 2019
By 2021
Alabama
NP
NP
NP
Alaska
NP
NP
NP
Arizona
NP
P
P
Arkansas
NP
NP
NP
California
C
C
C
Colorado
P
P
C
Connecticut
C
C
C
Delaware
P
P
P
District of Columbia
NP
NP
NP
Florida
C
C
C
Georgia
NP
NP
C
Hawaii
NP
NP
NP
Idaho
NP
NP
NP
Illinois
C
C
C
Indiana
P
P
P
Iowa
P
P
P
Kansas
NP
NP
NP
Kentucky
NP
NP
NP
Louisiana
NP
NP
NP
Maine
NP
P
C
Maryland
C
C
C
Massachusetts
P
P
P
Michigan
NP
NP
C
Minnesota
NP
P
P
Mississippi
P
P
P
Missouri
NP
NP
P
Montana
NP
NP
NP
Nebraska
NP
NP
P
Nevada
NP
NP
P
New Hampshire
P
C
C
New Jersey
P
C
C
New Mexico
P
P
C
New York
C
C
C
North Carolina
P
P
P
North Dakota
NP
NP
NP
Ohio
NP
NP
C
Oklahoma
NP
NP
NP
Oregon
NP
C
C
Pennsylvania
P
P
P

July 2023
REPORT TO CONGRESS
43
Rhode Island
P
P
P
South Carolina
NP
NP
NP
South Dakota
NP
NP
NP
Tennessee
NP
NP
NP
Texas
P
P
C
Utah
NP
NP
NP
Vermont
P
P
P
Virginia
NP
NP
C
Washington
NP
NP
C
West Virginia
P
P
P
Wisconsin
NP
NP
NP
Wyoming
NP
NP
NP
Key:
Comprehensive (C)
Partial (P)
No Protection (NP)
Sources:
1. Williams, L. H. (2017). Balance Billing by Health Care Providers: Assessing Consumer Protections
Across States.
https://www.commonwealthfund.org/publications/issue-briefs/2017/jun/balance-billing-health-care-
providers-assessing-consumer
2. Hoadley, J., Lucia, K., & Kona, M. (2019). State Efforts to Protect Consumers from Balance Billing.
https://www.commonwealthfund.org/blog/2019/state-efforts-protect-consumers-balance-billing
3. Kona, M. (2021) State Balance-Billing Protections
https://www.commonwealthfund.org/node/27021

July 2023
REPORT TO CONGRESS
44
Appendix C. Condensed Summary of the Effects of Consolidation on Health
Care Prices, Spending, Quality, Access, and Wages
Domain
Assessment
Health Care
Prices
Health Care
Spending
Quality of
Care
Patient
Access
Health Care
Wages
Horizontal
Hospital
Impact
Increase
a
Increase
a
Mixed
depending
on measure
and setting
b
Possible
decrease
d
Decrease
a
SOE
High
Moderate
Moderate
Insufficient
Low
Physician
Impact
Increase
a
Mixed
d
Mixed
d
No
evidence
d
No
evidence
d
SOE
Low
Insufficient
Insufficient
Insufficient
Insufficient
Commercial
insurers
Impact
Decrease
c
Increase in
premiums
a
Possible
increase in
patient
No direct
evidence,
might
Possible
decrease
d
experience
d
decrease
with
premium
increase
d
SOE
Low
Moderate
Insufficient
Insufficient
Insufficient
Medicare
Impact
No
Possible
No
Mixed for
No
Advantage
evidence
d
decrease in
premiums
d
evidence
d
plan
generosity
and ratings
d
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient
Medicaid
managed care
Impact
No
evidence
d
No
evidence
d
No
evidence
d
Possible
decrease in
plan choice
d
No
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient
Vertical
Hospitals and
physicians
Impact
Mixed:
increase or
no change
a
Increase
a
Mixed: small
increase or
no change
b
Possible
increase
d
Mixed
d
SOE
Moderate
High
Low
Insufficient
Insufficient
Providers and
insurers
Impact
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient
Other Markets
Pharmacy
Impact
Possible
decrease
d
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient
Telehealth
providers
Impact
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient
Private Equity
Nursing homes
Impact
No
evidence
d
Increase
a
Mixed
b
Possible
decrease
d
No
evidence
d
SOE
Insufficient
Low
Low
Insufficient
Insufficient
Hospitals
Impact
Possible
increase
b
No
evidence
d
Mixed
d
No
evidence
d
No
evidence
d
SOE
Low
Insufficient
Insufficient
Insufficient
Insufficient
Physician
practices
Impact
Possible
increase
d
Possibly no
change
d
Possible
increase
d
No
evidence
d
No
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient
Other Topics
Anticompetitive
practices
Impact
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
No
evidence
d
SOE
Insufficient
Insufficient
Insufficient
Insufficient
Insufficient

July 2023
REPORT TO CONGRESS
45
Domain
Assessment
Health Care
Prices
Health Care
Spending
Quality of
Care
Patient
Access
Health Care
Wages
Expanded scope
of practice
Impact
Possible
decrease
d
No change
or decrease
b
No change
or increase
b
No change
or increase
b
Mixed: no
change or
increase for
nurse
practitioners,
decrease for
physicians
d
SOE
Insufficient
Moderate
Moderate
Moderate
Insufficient
Certificate of
need laws
Impact
No change
or increase
d
No change
or increase
d
No change
or decrease
b
No change
or decrease
b
No
evidence
d
SOE
Insufficient
Insufficient
Moderate
Low
Insufficient
Surprise billing
policies
Impact
Mixed
b
No direct
evidence
d
No
evidence
d
Possible
increase or
no change
d
No direct
evidence
d
SOE
Low
Insufficient
Insufficient
Insufficient
Insufficient
NOTE: Health care prices refers to prices per service paid to providers. Health care spending includes premiums.
Quality of care reflects clinical quality and patient experience measures. No evidence refers to the lack of empirical
studies. Strength of evidence grades are high, moderate, low, and insufficient; evidence was graded based on the
number of studies, methodological quality, consistency, directness, and applicability.
a
Cells shaded in red indicate effects that have sufficient SOE and are detrimental to consumers.
b
Cells shaded in yellow indicate effects that have sufficient SOE and are unclear for consumers.
c
Cells shaded in green indicate effects that have sufficient SOE and are beneficial to consumers.
d
Cells shaded in gray indicate effects that have insufficient SOE.
