
THE
MEASUREMENT
OF
PATIENT-REPORTED
OUTCOMES
OF
REFRACTIVE
SURGERY:
THE
REFRACTIVE
STATUS
AND
VISION
PROFILE*
BY
Oliver
D.
Schein,
MD,
MPH
ABSTRACT
Purpose:
To
develop
a
questionnaire,
the
Refractive
Status
and
Vision
Profile
(RSVP),
to
assess
health-related
quality
of
life
associated
with
refractive
error
and
its
correction.
Methocds:
The
published
literature
on
patient
report
of
visual
and
overall
function
was
reviewed,
and
the
RSVP
was
self-
administered
by
550
participants
with
refractive
error.
Cross-sectional
validation
was
performed
using
standard
psycho-
metric
techniques.
The
responsiveness
of
the
RSVP
to
surgical
intervention
was
assessed
prospectively
in
a
subset
of
176
patients.
The
principal
outcome
measures
were
scores
on
the
overall
RSVP
scale
(S)
and
on
8
RSVP
subscales
(func-
tioning,
driving,
concern,
expectations,
symptoms,
glare,
optical
problems,
problems
with
corrective
lenses).
Results:
The
RSVP
(S)
and
its
subscales
demonstrated
very
good
internal
consistency
(Cronbach's
alpha,
0.70-0.93).
S
and
several
subscale
scores
were
independently
associated
with
satisfaction
with
vision
and
were
more
correlated
with
sat-
isfaction
with
vision
than
with
either
visual
acuity
or
refractive
error.
Higher
refractive
error
was
associated
with
lower
scores
on
S
and
on
5
subscales.
In
the
prospective
surgical
cohort,
15%
of
patients
had
some
worsening
in
their
total
RSVP
score;
however,
substantial
variation
was
seen
in
the
individual
subscales
where
worsening
ranged
from
7%
(problems
with
corrective
lenses)
to
41%
(driving).
The
effect
size
(measure
of
responsiveness)
of
the
RSVP
and
most
of
its
subscales
was
very
high.
Approximately
14%
of
patients
had
significant
worsening
in
3
or
more
subscales,
and
this
outcome
was
found
to
be
independently
associated
with
being
dissatisfied
with
vision
following
surgery
(OR,
5.84;
95%
CI,
1.88,
8.13).
Conclusions:
The
RSVP
has
been
validated
as
a
questionnaire
that
measures
patient-reported
quality
of
life
related
to
refractive
error
and
its
correction.
It
is
responsive
to
surgical
intervention
and
provides
important
information
regard-
ing
patient
outcomes
not
available
from
standard
clinical
measurements.
Tr
Am
Ophth
Soc
2000;98:439-469
INTRODUCTION
In
1994,
I
attended
a
meeting
of
the
Advisory
Panel
of
the
Food
and
Drug
Administration
(FDA)
when
it
was
presented
its
first
completed
data
set
from
a
clinical
trial
of
an
excimer
laser
for
photorefractive
keratectomy
(PRK).
The
panel
was
under
tremendous
pressure,
since
this
was
the
first
time
it
had
been
asked
to
consider
approval
of
this
new
technology.
The
perceived
burden
of
responsibility
was
huge,
and
there
was
consensus,
since
validated,
that
once
approved,
the
technology
would
explode
in
popularity.
The
clinical
trial
presented
all
of
the
standard
information
required,
documenting
visual
acuity
in
numerous
ways
(eg,
uncorrected,
correct-
ed,
stratified
by
pupil
size,
with
and
without
glare
'From
the
Department
of
Ophthalmology,
The
Wilmer
Eye
Institute,
Johns
Hopkins
University
School of
Medicine,
Baltimore,
Maryland.
Supported
by
grant
L-K24
EY00395-01
from
the
National
Eye
Institute,
grant
EY07127
from
the
National
Research
Service
Award,
and
the
Burton
E.
Grossman
Program
for
Preventive
Ophthalmology.
sources)
as
well
as
residual
refractive
error
(eg,
with
and
without
cycloplegia,
spherical
and
cylindrical
change,
accuracy).
The
results
presented
were
quite
straightfor-
ward.
The
targets,
measured
by
these
traditional
clinical
assessments,
were
met
in
a
reasonably
high
proportion
of
cases.
However,
that
FDA
panel
meeting
lasted
over
12
hours
and
was
characterized
by
uncertainty
and
dispute
as
to
the
inferences
that
one
might
draw
from
the
clinical
data.
Specifically,
the
question
lingered
as
to
what
the
impact
of
PRK
was
(and
would
be)
on
patient
visual
and
overall
function.
Isn't
it
possible,
the
question
was
asked,
that
tolerance
of
risk
and
either
enjoyment
of
or
dissatis-
faction
with
the
outcomes
of
PRK
might
vary
according
to
the
specific
needs,
perception,
and
function
of
individual
patients?
The
Advisory
Panel
was
clearly
frustrated
that
the
data
presented
could
not
integrate
the
standard
clini-
cal
measurements
with
patient
perception
of
function
in
order
to
produce
a
composite
assessment
of
how
success-
ful
the
treatment
actually
was.
I
shared
that
frustration
and
concluded
that
additional
tools
needed
to
be
devel-
oped
to
address
this
gap.
Tr.
Am.
Ophth.
Soc.
Vol.
98,
2000
439

Schein
Over
the
intervening
years,
there
has,
indeed,
been
an
explosion
in
refractive
surgery
in
the
United
States.
There
are
a
number
of
competing
excimer
lasers,
each
with
variations
in
the
profiles
of
treatment
applied.
Also,
there
are
a
number
of
evolving
refractive
procedures
in
addition
to
PRK,
the
most
prominent
of
which
are
laser-
assisted
in
situ
keratomileusis
(LASIK),
intracorneal
rings,
and
intraocular
lenses
of
various
designs
designed
for
pha-
kic
patients.
There
are
now
approved
treatments
for
hyperopia
and
astigmatism
in
addition
to
those
approved
earlier
for
myopia.
A
variety
of
other
technologies
are
currently
under
development.
Most
strikingly,
the
popu-
lation
undergoing
refractive
surgery
has
increased
expo-
nentially
since
1996,
when
approximately
50,000
refrac-
tive
procedures
were
performed
in
the
United
States.
It
has
recently
been
estimated
that
over
1.5
million
refrac-
tive
surgical
procedures
were
performed
in
the
United
States
in
1999.
This
proliferation
of
the
technology,
its
continued
evolution,
and
the
array
of
competing
strategies
have
rendered
even
more
acute
the
need
for
assessments
that
incorporate
the
patient's
perspective
in
defining
the
outcomes
of
refractive
surgery
procedures.
The
underlying
hypotheses
of
the
research
presented
in
this
thesis
are
that
the
systematic
assessment
of
vision-
related
quality
of
life
in
patients
undergoing
or
consider-
ing
refractive
surgery
will
(1)
provide
important
informa-
tion
that
cannot
be
provided
by
traditional
clinical
meas-
urements
and
(2)
provide
a
tool
to
optimize
patient
selec-
tion
and
hence
outcome
of
surgery.
The
first
section
of
this
thesis
reviews
the
rationale
and
current
status
of
visual
function
questionnaires
in
ophthalmology,
emphasizing
their
application
to
assessing
the
outcomes
of
surgical
intervention.
This
section
also
indicates
why
already
validated
instruments
are
not
suit-
able
to
the
needs
of
refractive
surgery
assessment.
The
second
section
describes
the
development
and
psychome-
tric
validation
of
the
Refractive
Status
and
Vision
Profile
(RSVP)
questionnaire.
The
third,
and
most
important,
section
presents
RSVP
data
collected
prior
to
and
follow-
ing
refractive
surgery
on
a
cohort
of
patients.
These
data
indicate
the
responsiveness
of
the
questionnaire
to
the
surgical
intervention
and
confirm
that
such
nonconven-
tional
measurements
can
help
to
identify
those
patients
most
likely
to
be
satisfied
with
the
results
of
surgery
post-
operatively.
The
fourth
and
final
section
suggests
possible
ways
in
which
the
patient
perspective
on
refractive
error
and
its
correction
may
be
incorporated
into
future
research
and
practice.
SECTION
1
Although
physicians
have
always
tried
to
understand
and
be
responsive
to
the
impact
of
diseases
and
treatments
on
the
overall
function
of
patients,
it
has
become
increasing-
ly
recognized
that
the
assessment
of
health-related
quali-
ty
of
life
(HRQoL)
needs
to
have
a
significant
role
in
the
practice
of
medicine.
HRQoL
may
have
a
variety
of
dimensions,
including
function
(overall,
physical,
social,
psychological),
symptoms,
health
perceptions,
and
satis-
faction.
Ideally,
if
one
were
able
to
assess
these
dimen-
sions
for
illnesses
and
their
treatments
both
in
individual
patients
and
in
populations,
then
one
would
have
a
pow-
erful
method
to
optimize
recommendations
for
individual
patients,
set
policy
and
priorities
for
populations
(eg,
a
method
to
prioritize
resources),
and
compare
the
effec-
tiveness
of
alternative
treatments
based
on
their
perceived
impact
on
patients.
Unfortunately,
such
diverse
goals
can-
not
be
readily
achieved
by
using
off-the-shelf
validated
questionnaires.
Generic
Versus
Disease-Specific
Questionnaires
Depending
on
the
goals
of
the
evaluation
that
needs
to
be
made,
there
are
advantages
and
disadvantages
to
what
are
known
as
"generic"
and
"disease-specific"
measures.'
Generic
measures
tend
to
focus
on
overall
physical,
social,
and
emotional
function.
Perhaps
the
2
most
widely
used
generic
measures
of
HRQoL
for
the
assessment
of
the
impact
of
chronic
diseases
and
their
treatment
are
the
Sickness
Impact
Profile2
and
the
SF-36.3
These
indicators
of
overall
function
are
particularly
valuable
when
trying
to
achieve
a
metric
across
different
disease
states.
For
exam-
ple,
if
one
wanted
to
compare
the
overall
health
status
of
2
populations,
then
one
might
choose
a
generic
health
sta-
tus
measure
as
the
metric.
Alternatively,
if
one
were
interested
in
comparing
the
effectiveness
of
different
treatments
regarding
overall
patient
function
over
time
in
the
same
population
(eg,
medical
versus
surgical
treat-
ment
of
coronary
artery
disease),
then
such
generic
meas-
ures
would
be
very
helpful.
Ophthalmic
interventions
such
as
cataract
surgery
have
been
shown
to
have
a
beneficial
effect
on
overall
function
and
quality
of
life
as
measured
by
generic
instru-
ments.4-6
However,
such
generic
instruments
share
an
important
limitation.
They
are
relatively
insensitive
to
the
specific
benefits
of
a
treatment
or
to
the
nuances
of
pro-
gression
of
a
specific
disease.
This
is
not
surprising,
of
course,
since
the
content
of
generic
questionnaires
is
pur-
posely
general
in
nature,
while
the
content
of
a
disease-
specific
instrument
should
reflect
the
special
knowledge
of
patients
and
physicians
who
are
intimately
familiar
with
the
course
of
the
specific
disease.
Validated,
disease-spe-
cific
questionnaires
permit
the
assessment
of
the
severity
of
the
specific
disease,
the
relationship
of
the
disease
to
overall
function,
and
the
response
(or
lack
thereof)
of
the
440
VALIDATED
QUESTIONNAIRES
MEASURING
PATIENT-REPORTED
VISUAL
FUNCTION

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
condition
to
intervention.
Disease-specific
and
generic
assessments
may
also
be
combined
when
the
particular
research
or
policy
question
requires
information
from
both
perspectives.
Within
the
field
of
ophthalmology,
one
may
make
still
further
distinctions.
A
visual
function
instrument
may
be
considered
generic
in
that
it
is
said
to
relate
to
any
con-
dition
that
affects
vision-related
quality
of
life,
or
it
may
be
disease-specific
(eg,
cataract).
An
example
of
the
former
is
the
NEI-VFQ,7
which
was
developed
as
a
generic
visu-
al
function
instrument
to
be
used
for
a
wide
variety
of
dis-
orders.
Examples
of
the
latter
include
the
VF-144'5"
and
the
ADVS,6"
which
were
designed
specifically
for
cataract,
although
both
have
been
subsequently
shown
to
be
valid
measures
of
visual
function
in
patients
with
other
visual
disorders
as
well.'0-"2
The
following
discussion
is
designed
to
summarize
the
status
of
the
published
literature
on
visual
function
instruments
that
have
been
validated
in
a
rigorous
fashion,
including
the
assessment
of
surgical
out-
come.
However,
before
reviewing
the
published
ques-
tionnaires,
a
brief
discussion
of
the
term
"validation"
as
it
applies
to
questionnaires
is
in
order.
Assessing
the
Validity
of
a
Questionnaire
The
terminology
describing
the
behavior
and
perform-
ance
of
questionnaires
was
developed
in
the
psychometric
literature.'3
In
its
simplest
interpretation,
a
questionnaire
that
is
valid
measures
what
it
says
it
does.
Three
types
of
validity
are
commonly
described.
Criterion
validity
refers
to
a
comparison
(statistical
correlation)
of
the
question-
naire
with
an
accepted,
external
standard.
For
example,
one
would
expect
some
association
between
poor
function
as
measured
by
a
visual
function
instrument
and
reduced
Snellen
visual
acuity.
Content
validity
refers
to
whether
the
questionnaire
contains
sufficient
detail
to
describe
the
particular
function.
For
example,
one
might
expect
a
questionnaire
on
visual
function
to
contain
1
or
more
items
related
to
glare,
such
as
night
driving.
Construct
validity
is
a
form
of
"face"
validity
where
the
condition
studied
produces
an
expected,
reasonable
response
pat-
tern
in
the
questionnaire.
For
example,
persons
with
macular
degeneration
would
be
expected
to
report
more
difficulty
with
reading
small
print
than
those
without
the
condition.
Construct
validity
is
typically
assessed
by
com-
paring
the
distribution
of
scores
(eg,
means).
Finally,
dis-
criminant
and
convergent
validity
are
terms
used
to
describe
the
performance
of
measures
that
have
more
than
one
domain.
For
example,
a
questionnaire
might
contain
separate
domains
covering
the
areas
of
social
function,
psychological
well-being,
driving,
and
activities
of
recreation.
For
a
questionnaire
with
multiple
domains
to
exhibit
discriminant
validity,
each
item
within
the
domain
should
be
more
highly
correlated
with
a
summary
measure
of
that
domain
than
with
summary
measures
of
other
domains.
Convergent
validity
is
demonstrated
by
showing
a
strong
correlation
of
each
item
within
a
domain
with
its
summary
measure.
Discriminant
and
convergent
validity
may
be
assessed
by
a
technique
known
as
multi-
trait
analysis.'4
The
reliability
of
an
instrument
is
generally
assessed
by
its
ability
to
yield
similar
results
in
a
repeatable
manner
when
applied
more
than
once
to
the
same
subject
or
group
of
subjects.
Reproducibility
refers
to
the
ability
of
the
questionnaire
to
provide
similar
responses
when
applied
more
than
once
to
the
same
individuals
over
a
rel-
atively
short
time.
It
is
usually
measured
statistically
by
calculating
the
intraclasss
correlation
coefficient.
Reliability
may
also
be
demonstrable
across
administra-
tion
techniques
(eg,
reliable
or
not
for
both
telephone
and
in-person
interviews)
or
interviewers
(inter-interviewer
reliability).
Consistency
refers
to
the
degree
to
which
items
measuring
the
same
domain
or
aspect
of
function
are
internally
correlated.
This
is
usually
assessed
by
the
Cronbach's
alpha
coefficient,
where
as
values
approach
1,
they
approximate
perfect
internal
consistency,
and
as
they
approach
0,
they
demonstrate
no
internal
consistency.
The
reliability
and
validity
of
a
questionnaire
are
usu-
ally
assessed
cross-sectionally
(ie,
at
one
point
in
time)
in
a
cohort
of
patients
with
a
specific
condition.
However,
not
all
questionnaires
that
are
validated
in
such
a
way
are
responsive
to
interventions.
Responsiveness,
which
refers
to
the
sensitivity
of
the
questionnaire
to
change
(improve-
ment
or
worsening)
in
health
status,
is
the
most
important
form
of
validation
for
an
instrument
whose
intended
use
is
the
assessment
of
a
surgical
intervention.
The
respon-
siveness
of
a
questionnaire
may
be
assessed
in
a
variety
of
ways,
including
the
simple
comparison
of
scores
before
and
after
an
intervention
by
using
paired
analyses
or
by
calculating
an
effect
size."5'17
VALIDATED
VISUAL
FUNCTION
QUESTIONNAIRES
THAT
HAVE
BEEN
APPLIED
TO
SURGICAL
POPULATIONS
Bermth-Petersen,
in
Denmark,
was
perhaps
the
first
oph-
thalmologist
to
recognize
the
need
for
a
systematic
evalu-
ation
of
patient
function
related
to
cataract."8"21
His
Visual
Functioning
Index
(VFI)
consisted
of
11
items,
including
vision
at
different
distances
and
settings,
driving,
social
activities,
and
self-care
activities.
This
Danish
question-
naire
was
validated
both
cross-sectionally
and
prospec-
tively
in
small
cohorts
of
patients
undergoing
cataract
sur-
gery'o22
and
was
used
to
estimate
societal
costs
of
visual
disability
due
to
cataract
and
to
compare
outcomes
of
intraocular
lens
implantation
versus
aphakic
contact
lens
use.
The
reliability
of
the
instrument
was
not
assessed.
Subsequent
to
his
own
publications,
little
additional
441

Schein
research
was
performed
with
the
VFI.
Later,
Brenner
and
colleagues23
compared
cataract
surgical
patients
to
controls,
asking
them
detailed
questions
about
visual
function.
Previously
validated
instruments
were
used
to
assess
social
functioning
and
mood,
but
these
were
not
integrated
with
the
questions
on
visual
function
for
which
no
validation
was
performed.
The
questionnaires
used
were
shown
to
be
responsive
to
the
intervention
of
cataract
surgery.
Mangione
and
colleagues9
developed
the
Activities
of
Daily
Vision
Scale
(ADVS),
which
was
first
validated
cross-sectionally
in
a
large
cohort
of
cataract
surgical
patients.
This
instrument
contains
separate
subscales
for
night
and
day
driving,
near
and
distance
vision,
and
glare.
It
was
shown
to
be
responsive
to
cataract
surgery,
with
the
total
and
all
subscales
improving
following
recovery
from
surgery.
Both
the
ADVS
and
the
SF-36
were
applied
to
the
same
cohort
of
cataract
surgical
patients.
Although
there
was
some
improvement
noted
in
the
generic
meas-
ure,
the
disease-specific
measure
was
far
more
sensitive
to
change
following
cataract
surgery.
The
ADVS
has
also
been
shown
to
be
useful
as
a
component
of
a
predictive
model
for
outcomes
of
cataract
surgery.24
It
has
subse-
quently
been
validated
in
patients
with
retinal
disease.'2
It
has
not
been
demonstrated
to
be
responsive
in
patients
with
refractive
error
undergoing
refractive
surgery.
The
VF-14'58
was
specifically
designed
to
measure
visual
function
related
to
cataract
and
outcomes
of
cataract
surgery.
It
is
a
14-item
questionnaire
without
subscales
that
includes
items
on
sports,
reading,
recre-
ation,
driving,
household
activities,
people
recognition,
and
seeing
steps.
It
was
first
validated
cross-sectionally
in
a
large
cohort
of
cataract
surgical
patients
who
were
also
asked
to
complete
the
Sickness
Impact
Profile
(SIP)2
questionnaire
as
well
as
answer
general
questions
about
trouble
and
satisfaction
with
vision.
A
visual
symptoms
index
consisting
of
6
questions
about
specific
visual
symp-
toms
was
also
asked.
The
VF-14
was
found
to
be
inter-
nally
consistent
and
to
correlate
more
closely
with
self-
report
of
satisfaction
with
vision
than
did
visual
acuity
in
either
eye
or
the
SIP.
Subsequently,
4-month
surgical
out-
comes
of
this
large
cohort
were
studied.
The
VF-14
was
found
to
improve
in
89%
of
patients
and
to
be
more
sen-
sitive
to
the
surgical
intervention
than
the
generic
meas-
ure,
the
SIP.
Change
in
rating
of
trouble
and
satisfaction
with
vision
were
more
closely
correlated
with
the
VF-14
than
with
change
in
acuity
in
the
operated
eye,
indicating
that
the
VF-14
is
probably
a
better
measure
of
the
bene-
fit
of
cataract
surgery
than
change
in
acuity.
Finally,
a
pre-
dictive
model
was
developed&
which
showed
that
the
pre-
operative
VF-14
and
cataract
symptom
score
were
not
only
independent
predictors
of
postoperative
outcome
but
were
as
strong
predictors
as
patient
age
and
ocular
comorbidity.
The
VF-14
was
also
used
to
evaluate
the
benefit
to
patients
of
undergoing
a
second
eye
cataract
surgery,
a
controversial
topic
among
some
health-care
payors.
The
VF-14
showed
conclusively
that
patient-
reported
function
improves
significantly
following
surgery
in
the
second
eye.25
The
VF-14
has
been
translated
and
used
in
Finnish,
Danish,
Catalan,
and
Canadian-French,
and
its
reliability
and
responsiveness
have
been
confirmed
in
these
translated
versions.4'26"
The
VF-14
has
subse-
quently
been
validated
in
patients
undergoing
comeal
transplantation.0,29
It
has
recently
been
validated
cross-
sectionally
in
patients
with
retinal
disease"
and
is
current-
ly
being
evaluated
for
its
responsiveness
in
a
retinal
inter-
vention
trial
by
the
same
investigators.
It
has
not
been
tested
in
patients
undergoing
refractive
surgery.
A
questionnaire
developed
in
Sweden,
the
Catquest
30,
has
also
been
validated
both
cross-sectionally
and
prospectively
but
is
not
in
active
use
in
English-speaking
settings.
A
visual
function
questionnaire
that
has
been
validated
in
one
setting
or
country
is
not
necessarily
valid
universally.
For
example,
to
assess
the
relative
benefits
in
India
of
intracapsular
cataract
extraction
with
aphakic
spectacles
versus
extracapsular
surgery
with
an
intraocular
lens,
a
new
visual
function
and
vision-related
quality-of-
life
instrument
had
to
be
developed
and
validated.3'
The
level
of
visual
disability
due
to
cataract
is
much
more
severe
in
rural
India
than
in
developed
countries,
and
the
activities
and
needs
of
patients
are
different.
The
Visual
Activities
Questionnaire
was
developed
for
this
purpose
and
fully
validated
in
India.
The
use
of
this
questionnaire
permitted
a
very
powerful
demonstration
of
the
visual
and
quality-of-life
benefits
of
extracapsular
cataract
surgery
in
this
setting.32'34
This
important
finding
would
not
have
been
apparent
from
the
traditional
comparisons
of
Snellen
visual
acuity
and
the
enumeration
of
operative
complications.
The
above
summary
indicates
that
several
visual
func-
tion
questionnaires
have
been
methodologically
validated
and
have
been
shown
to
be
responsive
to
the
intervention
of
cataract
surgery.
The
NEI-VFQ7
has
been
validated
cross-sectionally
and
is
now
in
use
in
a
variety
of
studies
(retinal
disease,
glaucoma)
where
longitudinal
and
postin-
tervention
data
are
being
collected.
It
is
therefore
antici-
pated
that
data
on
responsiveness
of
this
questionnaire
to
a
variety
of
interventions
will
be
forthcoming.
A
review
of
the
literature
on
validated
visual
function
questionnaires
indicates
several
common
denominators.
First,
in
those
settings
where
generic
function
and
quality-of-life
indica-
tors
were
simultaneously
employed,
the
disease-
or
vision-
specific
questionnaires
were
always
more
sensitive
to
both
baseline
visual
disability
and
change
after
the
intervention.
As
discussed
earlier,
this
is
exactly
what
one
would
predict,
and
this
finding
again
justifies
the
use
of
disease-specific
442

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
instruments
when
assessing
outcomes
of
the
effectiveness
of
specific
interventions.
A
second
unifying
finding
is
that
the
various
validated
visual
function
questionnaires,
although
correlated
with
traditional
measures
such
as
Snellen
acuity,
actually
provided
valuable
information
not
available
using
traditional
clinical
measures.
For
example,
the
VF-144
was
closely
associated
with
patients'
self-report
of
trouble
with
vision,
while
Snellen
acuity
(in
the
better
or
worse
eye)
was
not
correlated
at
all.
VISUAL
FUNCTION
QUESTIONNAIRES,
REFRACTIVE
ERROR,
AND
REFRACTIVE
SURGERY
Approximately
25%
of
the
world's
population
is
myopic.
The
rate
of
refractive
surgery
has
grown
exponentially
over
the
past
several
years.
In
addition
to
the
improved
technology
and
enormous
eligible
population,
an
underly-
ing
assumption
of
refractive
surgeons
and
their
patients
is
that
the
procedure
yields
an
improvement
in
patient-per-
ceived
quality
of
life
related
to
vision
and
its
correction.
Certainly,
industry-
and
physician-generated
marketing
would
lead
one
to
believe
that
these
issues
are
paramount.
However,
no
validated
methodology
for
assessing
patient
function
and
vision-related
quality
of
life
has
been
devel-
oped
for
this
population.
Why
not
use
1
or
more
of
the
questionnaires
discussed
above,
such
as
the
ADVS
or
the
VF-14?
The
principal
reason
is
that
these
questionnaires
focus
directly
on
issues
related
to
loss
of
central
or
periph-
eral
vision,
which
affect
one's
ability
to
perform
activities.
Therefore,
an
individual
with
corrected
refractive
error,
even
high
myopia,
would
be
likely
to
achieve
the
same
score
on
such
questionnaires
as
individuals
who
have
no
refractive
error
and
who
have
normal
vision.
Such
ques-
tionnaires
are
therefore
insensitive
to
the
limitations
(eg,
visual,
symptoms,
quality
of
life,
social)
that
are
experi-
enced
by
individuals
with
refractive
error
who
consider
refractive
surgery.
Consequently,
such
quiestionnaires
would
also
be
insensitive
to
possible
changes
(improve-
ment
or
worsening)
that
might
occur
following
an
inter-
vention.
Finally,
they
would
be
incapable
of
detecting
dif-
ferences
in
the
effectiveness
of
one
intervention
com-
pared
with
another
for
subjects
with
refractive
error.
This
is
the
underlying
rationale
for
the
development
of
a
vision-targeted
quality-of-life
questionnaire
for
individu-
als
with
refractive
error.
Although
no
single
validated
instrument
has
been
previously
developed
for
this
purpose,
relevant
research
exists,
the
most
prominent
of
which
is
that
by
Bourque
performed
in
the
context
of
the
Prospective
Evaluation
of
Radial
Keratotomy
Study
(PERK).5-3
In
this
work,
psy-
chological
and
role-functioning
attributes
were
stressed,
and
visual
function
was
assessed
with
only
2
questions
(reading
newsprint
and
seeing
a
friend
across
the
street
without
glasses).
Satisfaction
was
assessed
with
a
10-ques-
tion
index
that
included
questions
about
clarity
of
vision,
comparison
of
vision
with
others,
and
satisfaction
with
surgical
results.
Satisfaction
was
found
to
be
most
closely
correlated
with
not
needing
corrective
lenses
for
distance
and
lack
of
fluctuation
in
daily
vision.
When
the
psy-
chosocial
characteristics
of
radial
keratotomy
candidates
was
assessed,36
no
evidence
of
psychological
or
social
deviancy
was
observed.
However,
patients
did
express
a
fear
of
being
without
vision
and
impatience
with
current
spectacle
and
contact
lens
correction
as
their
chief
moti-
vation
for
requesting
surgery.
The
research
by
Bourque
highlighted
the
importance
of
the
patient
perspective
in
assessing
the
outcomes
of
refractive
surgery
but
did
not
result
in
a
unique
or
validated
instrument
to
do
so.
Other
limited
attempts
to
incorporate
the
patient
perspective
into
the
assessment
of
refractive
surgical
out-
comes
have
been
made.
These
largely
have
used
a
simple
4-
or
5-point
scale to rate
satisfaction
with
vision
or
to
rate
specific
symptoms
such
as
glare.'5"
Of
note,
in
the
origi-
nal
cohort
of
patients
undergoing
PRK
presented
to
the
FDA
for
approval,57
78%
of
patients
indicated
that
they
were
satisfied
or
very
satisfied
with
their
vision
at
2
years
following
PRK.
The
remaining
22%
indicated
that
they
were
less
satisfied.
As
with
radial
keratotomy,
satisfaction
was
correlated
with
final
uncorrected
acuity.
However,
the
correlation
was
not
strong,
indicating
that
there
must
be
other
factors
at
play.
No
independent
assessment
of
visual
function
from
the
patient
perspective
was
m-ade
in
these
studies.
Similarly,
visual
sym-ptoms
suclh
as
glare
and
halo
0'50,55,58
have
been
commonly
reported
after
excimer
laser
refractive
surgery,
and
these,
too,
have
been
associated
with
reduced
satisfaction
with
vision.
However,
such
symptoms
again
have
not
assessed
in
a
val-
idated
fashion
nor
correlated
with
overall
patient
percep-
tion
of
visual
function.
Two
studies
from
Europe
515t'
have
attemptedI
to
eval-
uate
the
psychosocial
outcomes
of
excimer
laser
surgery
using
standardized
questionnaires.
McGhee
and
col-
leagues59
found
that
freedoim
from
spectacles
and
difficul-
ty
with
contact
lenses
were
the
most
common
reasons
for
seeking
treatment.
Interestingly,
they
failed
to
show
an
association
between
poor
standar(d
cliniical
outcomnes
(eg,
uncorrected
Snellen
acuity)
and
satisfaction,
raising
the
possibility
that
variation
in
patient
expectations
and
needs
may
be
important
and
poorly
recognized
factors.
The
most
comprehensive
assessment
of
visual
and
overall
function
in
patients
undergoing
excimer
laser
surgery
was
performed
by
Freitas58
in
Portugal.
Using
a
variety
of
exist-
ing
questionnaires
from
the
medical
literature
which
were
translated
into
Portuguese,
she
assessed
visual
function,
overall
functional
status,
general
well-being,
mental
status,
and
satisfaction
with
surgery
and
found
improvements
in
443

Schein
each
of
the
measures
used
following
PRK.
The
study,
however,
was
performed
in
a
very
small
sample
of
only
45
patients
and
did
not
result
in
an
independent
assessment
tool.
The
standard
for
reporting
outcomes
of
refractive
surgery
is
to
indicate
the
proportion
of
patients
achieving
various
Snellen
acuity
thresholds
without
spectacle
cor-
rection
(eg,
percent
20/25
or
better)
and
the
proportion
who
achieve
accuracy
thresholds
in
final
refraction
(eg,
attempted
minus
achieved
spherical
equivalent).
Secondary
outcome
measures
that
have
become
standard
are
also
clinical
measurements,
such
as
glare
disability,
corneal
topographic
irregularity,
refractive
stability,
and
astigmatism.
These
are
the
assessments
by
which
current
and
evolving
techniques
are
evaluated
by
the
profession
and
the
FDA.
Additional
measurements,
derived
from
patient
perception
of
function,
are
clearly
needed.
SECTION
2
DEVELOPMENT
OF
A
QUESTIONNAIRE
TO
MEASURE
VISION-
RELATED
QUALITY
OF
LIFE
IN
PERSONS
WITH
REFRACTIVE
ERROR
Conceptual
Framework
and
Design
Underlying
the
development
of
a
quality-of-life
measure
related
to
refractive
error
is
a
broad
conceptual
model.
Figure
1
illustrates
such
a
model,
in
which
a
variety
of
potential
external
factors
(eg,
education,
preferences,
Condition
Refractive
error
Initial
RX
External
Socioeconomic
status
Spectacles
4
-
Education
Contact
lenses
Resources
Both
Preferences
Refractive
surgery
Personality
/~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Symptoms
of
refractive
error
and
correction
Socioeconomic
status
Education
Resources
Preferences
Personality
Function
Health
perception
Social
Satisfaction
with
health
Physical
*
xecaios
Rating
of
vision
Visual
Expectations
Psychologic
FIGURE
Conceptual
model
of
vision-related
quality
of
life
related
to
refractive
error.
symptoms)
impinge
on
the
choice
of
baseline
manage-
ment
of
refractive
error
(eg,
spectacles
versus
contact
lenses)
as
well
as
on
the
decision
to
pursue
refractive
sur-
gery.
In
turn,
the
outcomes
of
the
surgery
may
be
associ-
ated
with
specific
symptoms
(related
to
either
the
under-
lying
refractive
error
or
the
subsequent
treatment).
These
symptoms,
modified
by
patient
expectations
and
health
perceptions
(eg,
worry,
satisfaction),
converge
on
an
over-
all
sense
of
functional
performance
(eg,
social,
physical).
The
model,
of
course,
may
be
overly
simplistic,
yet
it
helps
to
guide
the
approach
to
questionnaire
develop-
ment.
Guyatt'5
has
clearly
outlined
the
steps
that
need
to
be
considered
in
the
development
of
a
disease-specific
quality-of-life
measure.
He
makes
a
distinction
between
a
"Rolls
Royce"
and
a
"Volkswagen"
model.
In
the
former,
each
step
is
methodologically
rigorous,
leading
to
a
valid,
clinically
relevant,
and
responsive
instrument;
in
the
lat-
ter,
the
questionnaire
is
created
de
novo
based
on
existing
literature
and
professional
judgment,
leading
to
a
ques-
tionnaire
whose
validity
and
applicability
remain
uncer-
tain.
The
plan
undertaken
for
the
creation
of
the
RSVP
reflects
the
Rolls
Royce
framework
as
outlined
by
Guyatt.
These
stages
include
a
rigorous
approach
to
the
following:
item
selection,
item
reduction,
questionnaire
format,
pretesting,
reproducibility,
and
validity.
Overview
of
Questionnaire
Development
Potential
items
for
the
questionnaire
were
generated
from
a
review
of
the
literature,
focus
groups
with
ophthalmolo-
gists
and
optometrists,
and
interviews
and
focus
groups
of
individuals
with
refractive
error.
The
content
of
the
focus
groups
was
transcribed
and
summarized,
and
the
specific
wording
of
items
was
retained
to
the
extent
possible.
An
initial
version
of
the
questionnaire
was
pilot-tested
in
a
group
of
306
individuals
with
refractive
error,
and
then
statistical
analysis
of
this
initial
version
was
performed
to
shorten
and
improve
it.
The
revised
questionnaire,
called
the
Refractive
Status
and
Vision
Profile
(RSVP),
was
then
tested
in
a
new
population
of
550
individuals
with
refrac-
tive
error,
and
the
validity
of
the
questionnaire
and
its
sub-
scales
was
assessed.
Selection
and
Wording
of
Items
A
review
of
the
relevant
published
literature
(Section
1)
and
the
conceptual
model
(Fig
1)
helped
to
guide
the
ini-
tial
structured
interviews
with
2
optometrists
and
2
oph-
thalmologists,
1
of
whom
was
a
practicing
refractive
sur-
geon.
These
professionals
were
asked
to
identify
areas
of
functional
difficulty
related
to
refractive
error
and
its
cor-
rection
that
patients
frequently
had
reported
to
them.
A
focus
group
of
individuals
with
refractive
error
was
then
conducted,
in
which
the
voluntary
participants
identified
issues
in
their
own
experience
and
in
their
own
language.
444
Consequences
of
treatments
Psychological
Mechanical
Inconvenience
Optical
Expense

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
The
focus
group
discussion
was
recorded
and
subjected
to
a
content
analysis
in
which
items
were
grouped
by
domains
(eg,
symptoms,
concern).
Domains
identified
in
this
fashion
were
then
supplemented
by
the
input
of
the
literature
review
and
the
interviews
with
the
eye-care
pro-
fessionals.
Items
that
were
clearly
redundant
were
removed,
leaving
a
total
of
122
items
in
the
pilot
instru-
ment.
The
items
were
worded
in
short,
declarative
sen-
tences,
preserving
to
the
extent
possible
the
vernacular
of
the
patients
(eg,
"Because
of
my
vision,
I
have
trouble
watching
TV").
For
each
question,
the
subject
was
asked
to
indicate
how
frequently
the
problem
was
experienced
or
how
severe
it
was
perceived
to
be.
Additional
questions
accounted
for
corrective
lens
type
(ie,
spectacle
and/or
contact
lens
use).
The
domains
covered
included
psycho-
logical,
physical,
and
social
role
functioning;
symptoms;
dependency;
and
health
perceptions.
Pilot
Testing
Approval
for
the
pilot
study
was
obtained
from
the
University's
Joint
Committee
for
Clinical
Investigation.
The
pilot
questionnaire
was
completed
by
self-administra-
tion
by
306
individuals
with
refractive
error.
The
sample
size
chosen
for
questionnaire
development
and
validation
is
not
based
on
formal
hypothesis
testing
as,
for
example,
is
the
case
for
the
planning
of
a
clinical
trial.
The
goal
for
the
development
of
this
questionnaire
was
to
assemble
a
population
that
was
felt
to
be
representative
of
individuals
with
refractive
error
and
sufficiently
large
to
permit
analy-
ses
of
subgroups
(eg,
subjects
with
various
ranges
of
refractive
error).
On
the
basis
of
previous
experience
with
a
similar
questionnaire
related
to
visual
function,
the
VF-
14,
it
was
estimated
that
data
from
at
least
250
partici-
pants
would
be
necessary.
These
subjects
were
derived
from
2
optometric
practices,
1
general
ophthalmologic
practice,
and
1
refractive
surgery
practice.
The
practices
also
provided
data
on
visual
acuity
and
refractive
error.
Exploratory
analyses
of
these
pilot
data
were
performed
to
identify
items
that
were
rarely
experienced
or
rarely
caused
difficulty
for
patients
and
to
indicate
areas
that
were
redundant
or
were
nondiscriminatory
(ie,
could
not
distinguish
groups
of
subjects
from
each
other).
Factor
analysis
was
used
to
sort
item
groupings
(potential
sub-
scales)
into
the
general
categories
of
functioning,
symp-
toms,
and
health
perceptions.
The
factor
solutions
were
used60
to
exclude
certain
items
from
further
analyses
because
of
irrelevancy
(factor
loading
<0.1)
or
redundan-
cy
(factor
loading
>0.9).
These
analyses
yielded
a
revised
questionnaire,
the
Refractive
Status
and
Vision
Profile
(RSVP),
which
contained
42
items
covering
8
subscales.
Specific
global
items
were
added
in
which
subjects
were
asked
to
rate
their
satisfaction
(5-point
scale)
with
current
vision
(distance
and
near,
corrected
and
uncorrected)
and
to
rate
the
quality
of
their
vision
(10-point
scale,
again
for
corrected
and
uncorrected
vision).
To
assess
a
possible
relationship
to
overall
health
issues,
2
"global
health"
items
were
also
included:
concern
about
health
(10-point
scale)
and
general
rating
of
health
(5-point
scale).
Finally,
demographic
information
(eg,
age,
lens-wearing
history)
was
appended
to
the
questionnaire
to
provide
necessary
background
information
to
interpret
the
patient
responses.
PARTICIPANTS
IN
THE
EVALUATION
OF
THE
RSVP
The
study
was
approved
by
the
University's
Joint
Committee
for
Clinical
Investigation,
and
all
participants
gave
oral
consent
to
participate.
Study
coordinators
at
6
participating
sites,
5
refractive
surgery
practices,
and
1
optometric
practice
(see
Acknowledgments)
were
asked
to
give
the
RSVP
to
consecutive
patients
who
did
not
have
significant
ocular
conditions
unrelated
to
refractive
error
and
who
had
either
not
undergone
refractive
surgery
at
all
or
who
had
not
undergone
such
surgery
within
the
3
months
prior
to
participation.
All
patients
were
enrolled
between
May
and
December
1997.
The
questionnaire
was
self-administered,
taking,
on
average,
10
to
15
min-
utes
to
complete.
The
full
questionnaire
contained
the
42
items
of the
RSVP
plus
additional
questions
relating
to
satisfaction
with
and
rating
of
vision
and
demographic
fea-
tures
of
interest,
such
as
age,
sex,
and
lens-wearing
(spec-
tacle
and/or
contact
lens)
history.
Clinical
data
on
cor-
rected
and
uncorrected
acuity,
refractive
error,
and
ocular
medical
and
surgical
history
were
provided
by
the
coordi-
nators
on
standardized
forms.
A
copy
of
the
full
ques-
tionnaire
is
provided
in
the
Appendix.
Reproducibility
Test-retest
assessment
was
performed
on
a
subset
of
par-
ticipants
in
the
months
of
October
and
November
1997.
The
40
patients
who
did
not
have
intervening
refractive
surgery
were
asked
to
complete
the
RSVP
questionnaire
twice.
Twenty-nine
of
the
40
completed
a
second
RSVP
with
an
interval
of
2
days
to
3
weeks
between
completions
of
the
questionnaire.
The
interval
included
their
clinical
evaluation
for
refractive
surgery.
A
second
assessment
of
reproducibility
was
performed
in
a
convenience
sample
of
16
subjects
with
refractive
error
who
were
not
being
eval-
uated
for
refractive
surgery.
The
interval
between
com-
pletions
of
the
RSVP
questionnaire
in
this
group
ranged
from
1
day
to
1
week.
Scoring
of
the
Questionnaire
The
RSVP
responses
were
coded
to
values
of
1
through
5,
with
5
indicating
more
severe
trouble.
For
subscale
and
total
scale
scores,
the
mean
value
of
non-missing
respons-
es
was
calculated.
Subscales
for
which
all
the
items
had
445

Schein
missing
responses
were
coded
as
missing.
To
facilitate
interpretation
of
results,
the
mean
score
for
each
subscale
was
recalibrated
to
a
0
to
100
metric
by
subtracting
the
minimum
possible
mean
score
(1)
from
the
mean
score
for
the
scale,
dividing
this
difference
by
the
possible
range
of
the
mean
score
(5
mlinus
1),
and
multiplying
by
100.
The
total
score,
S,
was
calculated
by
taking
the
sum
for
all
42
iteims
incluided
in
all
the
subscales
of
the
RSVP
and
rescaling
to
a
0
to
100
scale.
related
to
physical/social
fuinctioning,
optical
problems,
driving,
ocular
symptoms,
concern,
glare,
expectations,
and
problems
with
glasses
and
contact
lenses.
These
sub-
scale
groupings
were
then
evaluated
with
multitrait
scal-
ing
methods,60
and
the
final
results
are
presented
in
Table
II.
Eight
subscales
composed
of
a
total
of
42
items
were
identified:
concern
(6
items),
driving
(3
items),
expecta-
tions
(2
items),
physical/social
functioning
(11
items),
symnptoms
(5
items),
optical
problems
(5
items),
glare
(3
items),
and
problems
with
corrective
lenses
(7
items).
RESULTS
PERFORMANCE
OF
THE
OVERALL
RSVP
Participants
A
total
of
550
subjects
coompleted
the
RSVP
question-
naire.
Table
I
illustrates
the
characteristics
of
the
partici-
pants.
The
mean
age
of
participants
was
37
years
(range,
18
to
71
years),
and
59%
were
female.
The
mean
refrac-
tive
error
was
-5.4
(range,
-18
to
+3.75),
and
96%
had
best
correcte(d
acuity
of
20/20
or
better
in
at
least
1
eye.
Approximnately
36%
wore
spectacles
only,
19%
wore
con-
tact
lenses
only,
and
43%
wore
both.
General
health
was
rated
very
good
or
excellent
by
88%
of
the
participants.
WVhile
the
mean
rating
of
vision
was
8.4
(0
to
10
scale,
with
10
represeniting
perfect
vision),
only
56%
indicated
that
they
were
satisfied
or
very
satisfied
with
their
vision.
Derivation
of
Subscale.s
The
factor
analysis
confirmed
the
subscale
structure
pre-
dicte(d
by
the
analyses
of
the
pilot
testing.
Factors
were
Individual
Measure
of
Validity
The
internal
consistency
of
the
overall
questionnaire
was
measured
by
Cronbach's
alpha.
An
alpha
of
0.7
(range,
0
to
1)
or
higher
is
considered
adequate
for
comparisons
of
subgroups.
The
Cronbach's
alpha
of
the
entire
question-
naire
(S)
was
0.92,
with
that
of
the
subscales
ranging
from
0.70
to
0.93.
Reproducibility,
as
assessed
by
the
intraclass
correlation
coefficient
(ICC),
differed
within
the
2
popu-
lations
studied.
In
the
group
that
underwent
a
refractive
surgery
evaluation
in
between
completions
of
the
ques-
tionnaire,
the
reproducibility
was
modest
(overall
ICC,
0.61).
In
the
group
not
undergoing
the
intervening
eval-
uation,
the
reproducibility
was
very
good
(overall
ICC,
0.88).
The
average
RSVP
score
(S)
was
26.6
(0
to
100
scale,
with
0
representing
no
impairment
on
any
item).
Criterion
validity
was
assessed
by
examining
the
TABLE
1:
CHARACTERISTICS
OF
PARTICIPANTS
(N=550)
Age
(miieanl
[SD],
ranige)
Spherical
equivalent,
wvorse
eNe
(imiean
[SD],
ranige)
Healtlh
coiicerni
(imieani
[SD],
ranige)
Rating
of
visionll
(mean
[SD],
ranige)
Genlder
(N,
%)
Souirce
(practice
type)
(N,
%)
Corrective
lenis
stattis
(N,%)
History
of
ref'ractive
surgery
(N,
%)
Best
correctedl
VA,
both
eves
(N,
%)
Healtlh
rating
(N,
%)
Satisfaction
\Nith
vision
Feemnale
Refractive
sturgery
Optomiietric
Glasses
only
Contact
lenses
only
Glasses
and
contact
lenses
No
lenses4
None
Oine
eye
Both
eyes
.20/20
OU
>20/20;
20/25
20/40
20/25
-
20/40
OU
Very
good
or
excellent
Satisfied
or
very
satisfied
37.2
(9.
7vy)
-5.4D
(3.5D)
1.6
(2.4)
8.4
(1.4)
325
508
42
196
105
234
13
466
71
13
472
52
22
480
304
18
-
7'1
-18.375
-+3.75D
0
-
10
0
-
10
59.1
92.4
7.6
35.6
19.1
42.5
2.4
84.7
12.9
2.4
86.4
9.5
4.0
87.9
56.2
*O=not
at
all
concerned;
10=verv
conicerned.
tO=completelv
blind;
10=perfect
vision.
4Twxo
additional
participanits
wore
glasses
for
reading
only.
446
CHARACTERISTICS
DESCRIPTION

The
Measu
rement
of
Patient-Reported
Outcomes
of
Refractive
Su
rgery
TABLE
II:
PROPERTIES
OF
THE
RSVP
AND
ITS
SUBSCALES
ICCt
NAME
NO.
ITEMS
%
CORRECTLY
cf
IcC4
(IN
STABLE
MEAN'
RANGE
SCALED
GROUP)§
Concern
6
100
0.83
0.77
(.88
44.0
0-
100
Driving
3
100
0.93
0.69
0.70
25.9
0
-
1((
Expectations
2
10(
0.70
0.42
0.91
58.7
0-
100
Physical/social
fuinctioning
11
96.1;
100
(.87
0.84
0.63
17.2
0
-
92.8
Symptoms
5
100
0.84
0.71
0.80
20.8
0-
100
Optical
problems
5
94.3;
100
0.82
0.68
0.91
12.8
0
-
95
Glare
3
90.5;
100
0.75
0.72
0.72
22.3
0-
100
Problems
with
corrective
lenses
7
100
0.82
0.76
0.78
34.0
0
-
100
S
(overall
scale)
42
97.6;
100
0.92
0.61
0.88
26.6
0.7
-
100
If
all
items
within
the
subscale
had
significanitly
higher
corrected
item-to-total
correlations
writh
their
own
soibscale
than
wNith
any
other
soibscale,
this
number
would
be
100%.
If
some
items
had
higher
(but
not
statistically
signiificantly
so)
corrected
item-to-total
correlations
wvith
their
owna
suibscale
than
with
any
other
subscale,
the
first
percentage
indicates
proportion
with
signiificantl)
higher
correlations
anid
the
second
percenitage
indicates
pro-
portion
with
higher
(wvhether
significantly
so
or
not)
correlations.
f
Cronbach's
alpha:
a
measure
of
internal
consistency.
Values
of
1.0
indicate
perfect
internal
consistency,;
values
0
in(licate
iso
internlal
consistency.
Values
of
.7
or
higher
are
considered
sufficient
for
comparing
subgroups
of
persons.
t
Intraclass
correlation
coefficient
to
measure
test-retest
reliability.
Measured
in
a
subgroup
of
29
participanits
who
repeated
the
RSVP
quiestioninaire
within
2
days
to
3
weeks
after
the
first
administration,
with
an
intervening
refractive
surgery
evaluation.
§
Intraclass
correlation
coefficient
to
measure
test-retest
reliability.
Measured
in
a
convenience
sanstple
of
16
persons
not
fromn
a
refractive
surgery
practice
who
repeated
the
RSVP
questionnaire
within
1
day
to
1
Nweek
after
the
first
admi-nistration.
1
All
subscale
scores
were
rescaled
to
0-100.
association
of
the
overall
RSVP
score
(S)
(Table
III)
with
the
traditional
clinical
assessments
(Snellen
acuity
and
refractive
error)
and
the
global
measures
(rating
of
vision,
satisfaction
with
vision,
general
health,
and
health
concern).
The
correlation
between
the
total
RSVP
score
(S)
and
both
satisfaction
with
vision
and
rating
of
vision
was
found
to
be
much
stronger
than
between
any
of
the
traditional
clinical
markers
and
these
same
measures.
Therefore,
the
RSVP
score
(S)
is
more
closely
related
to
an
individual's
reported
satisfaction
with
vision
or
rating
of
vision
than
are
any
of
the
traditional
clinical
measures,
including
refractive
error
(better
or
worse
eye)
and
Snellen
acuity
(corrected
or
uncorrected,
better
or
worse
eye).
Additionally,
the
RSVP
score
(S)
is
more
closely
associated
with
an
individual's
rating
of
general
health
and
health
concern
than
are
the
traditional
clinical
meas-
ures,
although
the
association
is
less
strong
than
with
sat-
isfaction
with
and
rating
of
vision.
Figure
2
illustrates
the
relationship
between
the
total
RSVP
score
(S)
and
various
clinical
and
demographic
vari-
ables.
Significantly
higher
scores
(more
perceived
disabil-
ity)
were
observed
in
patients
considering
refractive
TABLE
III:
ASSOCIATION*
BETWEEN
THE
RSVP
AND
DIFFERENT
MEASURES
OF
VISION
AND
HEALTH
STATUS
Sf
VISION
VISION
GENERAL
HEALTH
SATISFACTION'
RATING1
HEALTH
CONCERN'
VA,
uncorrected,
better
eye
-0.12*°
0.05
0.15"
-0.05
0.03
VA,
uncorrected,
worse
eye
-0.16**
0.05
0.14*0
-0.04
0.06
VA,
best
corrected,
better
eye
-0.05
0.090*
0.19*0
-0.06
0.02
VA,
best
corrected,
worse
eye
-0.100*
0.12*0
0.18"
-0.090*
-0.00
Spherical
equivalent,
better
eye
-0.19**
0.12*0
0.210*
-0.05
0.03
Spherical
equivalent,
worse
eye
-0.21**
0.15**
0.21*0
-0.06
0.05
S5
-0.41**
-0.42**
0.204
0.23
*
Vision
satisfaction
-0.1000
-0.08
Vision
rating
-0.15**
-0.08
*
As
measured
by
Spearman
correlation
coefficient.
f
Overall
scale.
t
1=very
dissatisfied;
10=very
satisfied.
§
0=completely
blind;
10=perfect
vision.
I
1=excellent;
5=poor.
¶
0=not
at
all
concerned;
10=very
concerned.
*
Correlation
coefficient
differs
significantly
from
0
(P<.05).
447

Schein
8
a
a
is
IB
a
a
a
8
i
a
a
8
a
a
is
8
a
lot
a
a
ja
8
a
8
Is
11-
FIGURE
2
Relationship
between
overall
RSVP
score
(S)
and
clinical
and
demo-
graphic
variables.
Distribution
of
scale
scores
are
expressed
using
box
plots.
Center
white
horizontal
line
represents
median.
Shaded
box
extends
from
25th
to
75th
percentiles.
Vertical
lines
extending
from
box
cover
extent
of
data
within
1.5
times
interquartile
range
(length
of
box).
Values
in
data
beyond
this
range
are
indicated
by
horizontal
solid
lines.
Indentations
in
box
centered
on
median,
in
lighter
shading,
represent
extent
of
95%
confidence
interval
for
median.
Width
of
each
box
is
pro-
portional
to
square
root
of
number
of
observations
for
that
box.
surgery
(compared
to
those
not
considering
it),
patients
wearing
both
contact
lenses
and
spectacles
(compared
to
wearing
just
1
or
the
other),
females,
and
those
with
greater
refractive
error.
No
significant
age
effect
on
the
total
RSVP
score
(S)
was
observed.
Using
multivariate
analysis
and
adjusting
for
age,
sex,
and
lens
usage,
RSVP
scores
remained
independently
associated
with
refractive
error
and
use
of
both
glasses
and
contact
lenses.
Associations
with
individual
subscales
are
also
shown
(Table
IV).
A
second
multivariate
analysis
was
performed
(Table
V),
which
confirmed
the
independent
association
of
the
total
RSVP
score
(S)
and
most
of the
subscales
with
satisfaction
with
vision
after
adjusting
for
age,
sex,
lens
usage,
and
refractive
error.
Finally,
an
analogous
analysis
was
performed
(Table
VI),
which
confirmed
an
independ-
ent
association
of
the
total
RSVP
score
(S)
with
patient
rating
of
vision.
PERFORMANCE
OF
THE
RSVP
SUBSCALES
The
Cronbach's
alpha
of
the
individual
subscales
(Table
II),
measuring
internal
consistency,
ranged
from
0.70
to
0.93
(median,
0.82).
Mean
subscale
scores
ranged
from
12.8
(optical
problems)
to
58.7
(physical/social
function-
ing).
Although
the
distribution
was
somewhat
skewed
toward
fewer
problems
for
some
of
the
subscales
(eg,
opti-
cal
problems),
it
was
judged
that
such
scales
might
still
be
potentially
valuable
for
evaluating
potential
adverse
effects
of
refractive
surgery
in
some
patients
and
they
were
there-
TABLE
IV:
MULTIVARIATE
ANALYSIS:
FACTORS
ASSOCIATED
WITH
RSVP
SCALE
SCORES*
REGRESSION
COEFFICIENT
(STANDARD
ERROR)
COVARIATE
CONCERN
EXPECTATIONS
PHYSICAL/SOCIAL
DRIVING
SYMPTOMS
OPTICAL
GLARE
PROBLEMS,
S
FUNCTIONING
PROBLEMS
CORRECTIVE
LENSES
Age
-1.34
0.51
-0.11
0.41
-1.34f
1.04
0.12
-0.15
-0.20
per
10
yr
(0.82)
(1.04)
(0.67)
(1.01)
(0.70)
(0.64)
(0.79)
(0.73)
(0.49)
Sex
1.64
5.18t
-1.73
8.80t
1.63
3.04t
5.71t
-4.19t
0.96
F
vs
M
(1.62)
(2.04)
(1.31)
(1.99)
(1.38)
(1.26)
(1.56)
(1.44)
(0.97)
Lens
type§
-1.62
0.17
-4.98t
-5.37t
11.50t
-2.72
0.45
-14.60t
-2.04
CL
only
(2.21)
(2.78)
(1.78)
(2.72)
(1.87)
(1.72)
(2.12)
(1.97)
(1.32)
GL/CL§
-0.27
0.79
7.16t
5.08t
18.96t
2.74t
5.924
-10.21t
4.67t
(1.81)
(2.29)
(1.46)
(2.24)
(1.54)
(1.42)
(1.75)
(1.62)
(1.09)
Spherical
-1.53t
-0.76t
-0.91+
-1.754
-0.01
-0.84t
-0.72t
0.32
-0.66t
equivalent
(0.25)
(0.31)
(0.20)
(0.31)
(0.21)
(0.20)
(0.24)
(0.22)
(0.15)
per
diopter
CL,
contact
lens;
GL,
glasses
Higher
subscale
scores
indicate
more
problems.
For
age,
a
positive
coefficient
means
that
as
age
increases,
reported
problems
increase.
For
s
pos-
itive
coefficient
means
that
females
report
more
trouble
than
males.
For
contact
lens
only,
a
negative
coefficient
means
fewer
problems
than
report-
ed
by
glasses
wearers
only.
For
glasses/contact
lenses,
a
positive
coefficient
means
more
problems
than
reported
by
glasses-only
wearers.
For
spher-
ical
equivalent,
a
negative
coefficient
means
those
with
a
greater
degree
of
myopia
(toward
the
negative
end
of
the
scale)
report
more
problems
than
those
with
a
lesser
degree
of
refractive
error.
fBorderline
significant
+
statistically
significant
§
Glasses
only
is
the
reference
category.
The
no-lens
group
was
too
small
to
allow
meaningful
conclusions
to
be
drawn.
448

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
TABLE
V:
MULTIVARIATE
ANALYSIS:
ASSOCIATION
OF
ADJUSTED
RSVP
SUBSCALE
SCORE
WITH
SATISFACTION
WITH
VISION11
REGRESSION
COEFFICIENT
(STANDARD
ERROR)
AGE
SEX
LENS
TYPEt
GIJCL
SPHERICAL
EQUIVALENT,
SUBSCALE
PER
10
YRS
F
VS
M
CL ONLY
WORSE
EYE
PER
1%
PER
DIOPTER
INCREASE
Overall
RSVP
score
(S)
-0.17
0.002
0.24
-0.31
0.03
-0.037
(0.05)t
(0.097)
(0.13)§
(0.11)1
(0.02)
(0.004)t
Subscales
-0.18
-0.012
0.29
-0.48
0.04
-0.012
Concern
(0.05)t
(0.101)
(0.11)t
(0.11)t
(0.02)t
(0.003)1
Expectations
0.17
0.003
0.30
-0.48
0.06
-0.004
(0.05)t
(0.103)
(0.14)t
(0.12)t
(0.02)1
(0.002)
Physical
social
function
-0.17
0.093
0.17
-0.29
0.04
-0.021
(0.05)t
(0.097)
(0.13)
(0.11)t
(0.02)t
(0.003)t
Driving
-0.17
0.098
0.21
-0.39
0.03
-0.017
(0.05)t
(0.099)
(0.13)
(0.11)t (0.02)§
(0.002)t
Symptoms
-0.18
-0.020
0.45
-0.24
0.06
-0.012
(0.05)t
(0.102)
(0.14)5
(0.13)t
(0.02)t
(0.003)t
Optical
-0.14
0.054
0.22
-0.40
0.04
-0.028
(0.05)t
(0.098)
(0.13)
(0.11)t
(0.02)t
(0.003)t
Glare
-0.16
0.022
0.31
-0.42
0.05
-0.012
(0.05)t
(0.103)
(0.14)t
(0.12)t
(0.02)t
(0.003)t
Problems
with
corrective
lenses
-0.17
-0.055
0.22
-0.54
0.06
-0.006
(0.05)
(0.103)
(0.15)
(0.12)t
(0.02)t
(0.003)§
CL,
contact
lens;
GL,
glasses.
°
Higher
values
indicate
more
satisfaction
with
vision.
A
negative
coefficient
indicates
that
those
who
report
more
problems
on
subscales
(or
are
older)
are
less
satisfied.
A
positive
coefficient
indicates
that
those
who
have
worse
refractive
error
are
less
satisfied.
For
lens
type,
a
positive
coefficient
means
those
who
wear
only
contact
lenses
are
more
satisfied
than
those
who
wear
only
glasses.
t
Only
glasses
is
the
reference
category.
t
Statistically
significant
(P<
.05)
§
Borderline
statistically
significant
(P<
.07)
11
Higher
values
indicate
vision
that
is
closer
to
perfect.
fore
retained.
The
discriminant
and
convergent
validities
of
the
subscales
were
strong
(Table
IV).
As
observed
with
the
total
RSVP
score
(S),
the
test-retest
reliability
was
stronger
in
the
stable
group
than
in
those
undergoing
an
intervening
refractive
surgery
evaluation.
Table
VII
illustrates
the
correlations
between
the
various
subscales.
The
correlations
are
logical,
thereby
adding
to
the
face
validity
of
the
scales.
For
example,
physical/social
func-
tioning
is
most
strongly
correlated
with
driving,
as
are
glare
and
optical
problems,
and
symptoms
were
most
cor-
related
with
glare
and
optical
problems.
As
for
the
overall
RSVP
score
(S),
criterion
validity
was
assessed
by
calculating
the
correlations
between
each
of
the
global
measures
and
each
subscale
and
comparing
those
correlations
to
those
of
the
traditional
clinical
mark-
ers
and
the
same
global
measures
(Table
VIII).
For
all
subscales
except
expectations
and
problems
with
correc-
tive
lenses,
the
correlation
of
the
subscales
with
satisfac-
tion
with
vision
was
greater
than
with
corrected
or
uncor-
rected
Snellen
acuity
or
refractive
error.
The
findings
were
similar
for
rating
of
vision,
except
that
1
additional
subscale,
concern,
was
not
more
correlated
with
this
out-
come
than
the
standard
clinical
measures.
Correlation
between
each
of
the
RSVP
subscales
and
health
concern
as
well
as
general
health
were
also
greater
than
between
these
global
health
measures
and
the
traditional
clinical
measures.
In
summary,
therefore,
the
subscales
were
found
to
be
more
correlated
with
external
global
meas-
ures
of
vision
and
general
health
than
Snellen
acuity
and
refractive
error.
Figures
3A
through
3H
illustrate
the
association
of
the
individual
subscales
with
practice
type
(refractive
sur-
gery
versus
general
practice),
corrective
lens
type
(glasses,
contact
lenses,
or
both),
age,
sex,
and
refractive
error.
Concern
was
greater
among
those
seen
at
refractive
surgi-
cal
practices
and
among
those
with
greater
refractive
error.
Females
had
lower
expectation
(greater
willingness
to
accept
less
than
perfect
vision)
scores
than
males,
as
were
scores
from
refractive
surgical
practices.
More
problems
with
physical/social
functioning
were
reported
in
persons
with
greater
refractive
error
and
in
persons
wearing
contact
lenses.
More
problems
with
driving
were
reported
among
those
with
greater
refractive
error,
females,
and
those
wearing
both
contact
lenses
and
glass-
es.
Symptoms
were
reported
more
frequently
by
younger
subjects,
females,
and
those
wearing
both
spectacles
and
contact
lenses.
Optical
problems
were
positively
associat-
ed
with
degree
of
refractive
error,
female
sex,
and
449

Schein
TABLE
VI:
FACTORS
ASSOCIATED
WITH
RATING
OF
VISION
REGRESSION
COEFFICIENT*
(STANDARD
ERROR)
AGE
SEX
LENS
TYPEf
SPHERICAL
EQUIVALENT,
SUBSCALE
PER
10
YRS
F
VS
M
CL
ONLY
GL/CL
WORSE
EYE
PER
1%
PER
DIOPTER
INCREASE
Overall
RSVP
score
(S)
-0.10
-0.10
0.20
-0.46
0.06
-0.038
(0.005)+
(0.11)
(0.15)
(0.12)§
(0.02)§
(0.005)§
Subscales
-0.10
-0.13
0.26
-0.63
0.071
-0.006
Concerni
(0.05)+
(0.11)
(0.15)
(0.13)§
(0.02)§
(0.003)t
Expectationis
-0.10
-0.12
0.26
-0.63
0.08
-0.004
(0.05)
(0.11)
(0.15)
(0.13)§
(0.02)§
(0.002)4
Physical
social
functioning
-0.10
-0.19
0.13
-0.43
0.06
-0.028
(0.05)4
(0.11)4
(0.15)
(0.12)§
(0.02)§
(0.004)§
Driving
-0.10
0.04
0.14
-0.53
0.04
-0.022
(0.05)4
(0.11)
(0.14)
(0.12)§
(0.02)§
(0.002)§
Symptoms
-0.12
-0.10
0.49
-0.28
0.08
-0.019
(0.05)§
(0.11)
(0.16)§
(0.14)+
(0.02)§
(0.003)§
Optical
problems
-0.06
-0.02
0.16
-0.55
0.06
-0.031
(0.05)
(0.10)
(0.14)
(0.12)§
(0.02)§
(0.003)§
Glare
-0.10
-0.05
0.27
-0.56
0.07
-0.014
(0.05)
(0.11)
(0.15)
(0.13)
§
(0.02)§
(0.003)§
Problems
with
corrective
lenises
-0.10
-0.17
0.22
-0.67
0.08
-0.002
(0.06)
(0.11)
(0.16)
(0.13)§
(0.02)§
(0.003)
CL,
contact
lens;
GL,
glasses.
*
Higher
values
indicate
vision
that
is
closer
to
perfect.
A
negative
coefficient
indicates
that
those
who
report
more
problems
on
subscales
(or
are
older)
rate
their
vision
less
highly.
A
positive
coefficient
indicates
that
those
who
have
worse
refractive
error
rate
their
vision
less
highly.
For
lens
type,
a
positive
coefficient
imieans
those
Nwho
wear
only
contact
lenses
rate
their
v,ision
more
highly
than
those
who
wear
only
glasses.
fOnily
glasses
is
the
referenice
category.
t
Statistically
significant
(P<
.05)
§
Borderline
statistically
signiificant
(P<
.07)
TABLE
VII:
ASSOCIATION
(CORRELATION
COEFFICIENTS)
OF
SUBSCALES
OF
THE
RSVP
SCALE
CONCERN
EXPECTATIONS
PHYSICAL/SOCIAL
DRINING
SYMPTOMS
OPTICAL
GLARE
PROBLEMS,
FUNCTIONING
PROBLEMS
CORRECTIVE
LENSES
Concern
1.0(
Expectationis
(.18
1.00
Physical/social
0.37a
0.13
1.00
functioniing
Driving
0.32
0.15
0.66
1.00
Symptoms
0.24
0.10
0.42
0.35
1.00
Optical
problems
0.31
0.10
0.55
0.61
0.43
1.0(
Glare
0.26
0.12
0.37
0.45
0.55
0.49
1.00
Problems
with
0.23
0.02
0.20
0.08
0.17
0.16
0.15
1.00
corrective
lenses
S°
0.62
0.26
0.82
0.72
0.63
0.71
0.61
0.47
*
Overall
scale
(all
items
combined)
increasing
age.
Glare
was
positively
associated
with
increasing
refractive
error,
female
sex,
and
persons
wearing
both
glasses
and
contact
lenses.
Finally,
problems
with
cor-
rective
lenses
were
associated
with
increasing
age,
patients
from
refractive
surgery
practices,
male
sex,
and
spectacle
use.
Multivariate
analyses
of
association
between
individ-
ual
subscales
and
clinical
and
demographic
measures
were
performed
in
an
analogous
fashion
to
those
per-
formed
for
the
overall
RSVP
score
(S).
The
findings
are
indicated
in
Table
IV
In
summary,
these
analyses
suggest
that
those
who
wear
both
contact
lenses
and
spectacles
report
more
trouble
with
physical/social
functioning,
driving,
symptoms,
glare,
and
problems
with
corrective
lenses
than
do
wearers
of
spectacles
only.
Those
wearing
contact
lenses
only
reported
more
trouble
with
symptoms
450

The
Mleasuiremenit
of
Patietnt-Reported
Ouitcomes
of
Refractive
Sn
rgerij
cc
c
cc,
c
c
o o
c
oc
c
o
c
_-
-
-
C
C
D
C1
C
o
cc
6
-
cc
cc
~~~LD
Ci
cci
rc
izr=
p
r=
zzz)
COf-
ci
_ _
V-
5,
t_ t_
oc
cc
i-
C
_
_
_
_~~~~~~~~~~~~~~~~I.
-s
C:
-O
-
-
-i
_
_
-
C]
C>1
.,c
xc
c
_
c
o.
o
c
c.
oc
cc
ci
c
?c
°,
c,
o, o,
o
ci
cc
--
-sX
a
5
1-
C
1-
-Cc1
t-
o
-
o
i
Ci
o~~
-
C
_
-_
}
¢,
t~~~~~~~~~L
-
o
=
t
0-3
C N
-
cC
cC
C
O
O O 0
3~~~f7
-
DZrC
Iz
@_
C
F
= c: 2 c z X X :X 3 Xr9 ZAr 3 oe = d 5 ^° _o 3
-
4
.1.
=
;4
w
z
*4
'o,
g
=
W
i--o
z
0
z
0
-z
z
C
z
0
v:
D
<
F
=
:
<
W
=
:
z
z
_o
;t
5
No
v:
W
D
<
W
Z;
F
Z
W
=
v
v
:
:
Z
<
V:
W
;
X
m
D
n
F
Ct
=
;
=
E
Z
;
¢
;
;
v
oZ
v
!
O
U:
t
<
_..
5
W
;
;
;
C
C
4--
C)
.4
E
z
v
.R
R
VQ~r
cc
451

Schein
8
-
I
any
0
-2
9
3
-5.9
6
-
-99
-10
-20
Refractve
Eror
(sphericol
equabr.
wos.
eye,
dop9.s)
p-0001
FIG
3A
2
18-29
30-39
40(49
Age
(y--r)
p.7
2
any
+
O
-2.9
-3
5
9
4
-9.9
-10
-20
18-29
30-39
40-49
Refra000e
Eror
(sperical
equivalente,ww
eye.
dopters)
Ag
(years)
P=.1
FIG
3B
P=.
any
+
0
-2.9
4
-5.9
-6
-
-9.9
-10
-20
Ref,a
rt.
Errozr
(spho6cal
eqt*,aled,
*
orsey,
dioWes)
R02.oo(
Plo.
OoloqoO08089.091)
r_-
FIG
3c
any
+
0
-2.9
-3
-5.9
6
-9.9
-10
-2Z
Ret,acte
Errrx
(soherical
equivabnt
e
",
dioe
p=
2
FIG
3E
a01y
+
-2p9
-3
-
-5.9
{;
-9
9y
0
020
R.ftarcWhe
Errr,
(Sphaftl
eqwvalet
worsc
eye,
dbpter)
p.
02
FIG
3H
18-29
30-39
40-49
AVe
(years)
p=,4
t8-29
40(988
0-49
Age
(y-rS)
p-
02
I
e
I
I
.I
I
0
-
18-29
30-39
40(49
Age
(yeas)
p-
6
any
0
-2.9
-3
-S
9
-6
--.9
9
-10
-20
R8fnractve
Error
tsphr"
erivalent,
w
eye,
riopt0s)
p=.0001
.00y
+
0
-2,9
-3
-5.9
4
-909
-10
-20
Refacte
Error
(sph80cal
equ9va0
0,
,wO0.
y.o
dopt08s)
P=
0007
FIG
3D
FIG
3F
9.0.
0-P29
-3
-5p
6-9
4
-8909
*0
-20
Peirad
se
Error
(sphonabl
fLIVlt,m
wrecye,
riopters)
p-,6
FIG
3G
18-29
30-39
40-49
Age
(years)
p=5
18-29
30 39
404t9
Ag
(yearS)
p-.05
1t-29
30-39
40-49
09g
(y080)
p.02
FIGURE
3A
-
H
Relationship
between
individual
RSVP
subscales
and
clinical
and
demographic
variables.
Distribution
of
scale
scores are
expressed
using
box
plots.
Center
white
horizontal
line
represents
median.
Shaded
box
extends
from
25th
to
75th
percentiles.
Vertical
lines
extending
from
box
cover
extent
of
data
within
1.5
times
interquartile
range
(length
of
box).
Values
in
data
beyond
this
range
are
indicated
by
horizontal
solid
lines.
Indentations
in
box
centered
on
median,
in
lighter
shading,
represent
extent
of
95%
confidence
interval
for
median.
Width
of
each
box
is
proportional
to
square
root
of
number
of
observations
for
that
box.
452
8
I
_
_
rn
T
r
*
n
_
W _
r
_
.. ,
*
-
1
..
..
.I
.._
|
&
800
liii
=-
_
r
r_
r~~
li
;
I
>
T77
II
rh
iii
_2
-_
.00~~~~~
-
r
r
E~~~0-
_IIII
8
2
=
=
0
_
III
_
II
21
__r
-7.-
T~~~~
!
!
!
|
|i
.L
8-
-
':
III:'
9
r.
I
0
50+
8
I
50+
50+
50.
50+
50+
W0+
50.

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
but
significantly
less
trouble
with
physical/socialfunction-
ing,
driving,
and
problems
with
corrective
lenses
than
did
wearers
of
only
glasses.
All
subscales
were
significantly
associated
with
greater
degrees
of
refractive
error
except
for
symptoms
and
problems
with
corrective
lenses.
Females
reported
more
trouble
with
driving,
optical
problems,
and
glare
than
males
and
were
more
likely
to
accept
less
than
perfect
vision
(expectations).
Increasing
age
was
marginally
associated
with
reporting
of
more
symptoms.
Additional
multivariate
analyses
were
per-
formed
to
assess
the
association
of
the
RSVP
subscales
with
satisfaction
with
vision
(Table
V)
and
with
rating
of
vision
(Table
VI).
After
adjustment
for
age,
sex,
lens
usage,
and
refractive
error,
higher
(more
trouble)
scores
on
the
subscales
related
to
concern,
physical/socialfunc-
tioning,
driving,
symptoms,
optical
problems,
and
glare
were
all
significantly
and
independently
associated
with
less
satisfaction
with
vision.
A
borderline
association
was
observed
between
problems
with
corrective
lenses
and
less
satisfaction
with
vision.
Therefore,
the
RSVP
sub-
scales
yield
additional
information,
not
related
to
the
tra-
ditional
clinical
assessments,
that
are
related
to
patients'
satisfaction
with
vision.
When
comparable
analyses
were
performed
for
rating
of
vision
(Table
VI),
the
findings
were
similar.
After
adjustment
for
the
same
demograph-
ic
and
clinical
parameters,
all
of
the
subscales
except
for
problems
with
corrective
lenses
were
associated
with
rat-
ing
of
vision.
Therefore,
the
RSVP
subscales
yield
addi-
tional
information
related
to
patients'
rating
of
vision
not
contributed
by
the
standard
clinical
measures.
DISCUSSION
A
questionnaire
designed
to
measure
HRQoL
should
reflect
the
concerns
and
issues
most
important
to
the
rel-
evant
population
of
patients.
The
items
of
the
RSVP
were
selected
on
the
basis
of
a
cumulative
process,
which
included
review
of
the
published
literature
and
focused
discussions
with
experts
and
patients.
The
items
chosen
therefore
are
likely
to
reflect
the
principal
areas
of
con-
cern
for
patients
with
refractive
error.
The
validity
and
reliability
of
the
RSVP
and
its
subscales
were
extensively
evaluated
and
documented.
Both
the
overall
RSVP
score
(S)
and
most
of
the
subscales
were
independently
associ-
ated
with
satisfaction
with
vision
and
patient
rating
of
vision.
Moreover,
they
were
more
strongly
correlated
with
satisfaction
with
vision
and
rating
of
vision
than
were
either
refractive
error
or
Snellen
acuity,
even
in
multivari-
ate
analyses.
These
analyses
indicate
that
the
RSVP
and
its
subscales
provide
additional
information
about
patient
perception
of
visual
status
and
function
that
is
not
cap-
tured
by
traditional
clinical
measurements.
Interestingly,
test-retest
reliability
was
lower
in
a
group
of
patients
who
had
an
intervening
refractive
sur-
gery
evaluation
than
in
a
group
not
receiving
such
an
evaluation.
It
is
likely
that
the
evaluation
itself,
which
no
doubt
contained
an
appraisal
of
issues
related
to
visual
dif-
ficulties
and
a
discussion
of
the
risks
and
expectations
rel-
evant
to
refractive
surgery,
had
an
effect
on
the
responses
of
the
second
administration
of
the
RSVP.
This
hypothe-
sis
is
supported
by
the
fact
that
the
least
reproducible
sub-
scale
was
expectations,
the
area
one
might
anticipate
would
be
most
affected
by
an
intervening
surgical
evalua-
tion.
This
finding
suggests
that
the
timing
of
the
adminis-
tration
of
the
RSVP
(before
versus
after
surgical
evalua-
tion)
may
be
important
in
establishing
an
accurate
base-
line
for
estimating
function
and
vision-related
quality
of
life
for
individuals
considering
refractive
surgery.
There
are
several
potential
methodologic
limitations
to
the
development
of
any
functional
status
questionnaire,
which
also
may
apply
to
the
RSVP.
First,
1
or
more
items
of
concern
to
patients
may
have
been
overlooked.
As
mentioned
above,
the
use
of
a
multistage
process
to
iden-
tify
items
of
interest
at
least
limits
that
possibility.
A
sec-
ond
potential
limitation
is
that
the
population
in
which
the
instrument
was
developed
may
not
be
representative
of
those
in
which
the
instrument
will
likely
be
used.
The
pri-
mary
purpose
for
developing
the
RSVP
was
to
create
a
measure
that
would
be
useful
in
assessing
patient
out-
comes
of
refractive
surgery.
Therefore,
the
population
studied
was
largely
composed
of
individuals
considering
refractive
surgery.
A
small
proportion
of
individuals
who
had
refractive
error
but
who
were
not
considering
surgery
was
retained
to
improve
the
generalizability
of
the
find-
ings.
Of
course,
it
is
possible
that
the
refractive
surgery
candidates
who
participated
in
the
RSVP
development
might
differ
in
some
important
way
from
other
popula-
tions
of
patients
with
refractive
error
who
are
considering
refractive
surgery.
This
might
have
occurred
either
because
the
centers
patients
were
in
some
way
atypical
or
because
of
selection
bias
within
each
center.
Although
coordinators
were
asked
to
administer
the
RSVP
to
con-
secutive
eligible
patients,
this
was
not
possible
because
of
coordinator
time
and
other
restraints
in
each
practice.
The
design
and
resources
of
the
study
do
not
permit
a
rig-
orous
analysis
of
representativeness.
However,
the
possi-
bility
of
selection
and
related
biases
is
mitigated
by
includ-
ing
patients
from
multiple
sites
in
the
development
of
the
instrument.
In
fact,
subscale
scores
did
not
differ
signifi-
cantly
by
clinical
center,
suggesting
a
certain
homogeneity
of
patients
across
sites
and
that
variation
in
practice
pat-
terns
and
geographic
locale
may
not
present
a
significant
obstacle
to
the
development
of
a
visual
function
question-
naire
related
to
refractive
error
and
its
correction.
Finally,
only
a
small
percentage
of
participating
subjects
had
hyperopia.
Although
issues
related
to
hyperopia
were
453

Schein
specifically
addressed
in
the
selection
of
items
for
the
questionnaire,
it
is
possible
that
the
performance
of
the
RSVP
and
its
subscales
might
vary
depending
on
the
dis-
tribution
of
hyperopes
and
myopes
in
a
given
population.
In
conclusion,
the
RSVP
and
its
subscales
were
devel-
oped
in
a
methodologically
rigorous
manner
and
were
demonstrated
to
be
valid
and
reliable.
and
their
overall
health.
Clinical
and
demographic
data
were
provided
by
the
study
coordinators
at
each
center
and
included
information
on
baseline
and
postoperative
refractive
error
and
uncorrected
vision
as
well
as
date
and
type
of
operation
performed.
The
study
was
approved
by
the
Human
Studies
Committees
at
the
participating
sites,
and
each
patient
gave
verbal
consent
to
participate.
STATISTICAL
ANALYSIS
PROSPECTIVE
EVALUATION
OF
THE
RSVP
IN
PATIENTS
UNDERGOING
REFRACTIVE
SURGERY
The
previous
section
demonstrated
that
the
RSVP
and
its
subscales
exhibit
good
psychometric
validity
and
suggests
that
the
questionnaire
can
be
used
to
describe
the
HRQoL
related
to
vision
of
individuals
and
populations
with
refractive
error.
This
demonstration
was
performed
cross-sectionally.
In
other
words,
it
was
performed
at
a
single
moment
in
time
for
each
subject.
The
validation
did
not,
however,
provide
any
indication
as
to
whether
the
questionnaire
would
be
responsive
or
sensitive
to
change
in
visual
function
that
might
occur
following
refractive
surgery.'"
In
contrast,
it
is
possible
that
subscales
with
lim-
ited
utility
in
differentiating
subgroups
cross-sectionally
may
be
valuable
in
detecting
changes
that
follow
a
surgi-
cal
intervention.
Finally,
a
cross-sectional
validation
can-
not
provide
evidence
that
an
instrument
may
be
useful
as
a
preoperative
tool
to
help
predict
which
patients
will
have
the
best
outcomes
following
refractive
surgery.
To
address
these
important
issues,
a
prospective
assessment
of
the
RSVP,
administered
before
and
after
refractive
sur-
gery,
was
performed.
METHODOLOGY
Patients
and
Outcomiies
Patients
were
eligible
for
the
prospective
assessment
of
the
RSVP
if
they
completed
a
baseline
RSVP
and
under-
went
refractive
surgery
in
both
eyes.
Patients
were
recruited
from
the
same
5
centers
that
provided
patients
for
the
cross-sectional
validation
of
the
RSVP
and
were
recruited
between
May
and
December
1997.
Eligible
patients
received
a
copy
of
the
RSVP
questionnaire
to
complete
between
2
and
6
months
following
surgery
on
the
second
eye.
If
no
response
was
achieved,
a
second
questionnaire
was
sent.
If
there
was
still
no
response,
uip
to
5
attempts
were
made
by
telephone
to
contact
the
patient
to
request
participation.
In
addition
to
the
sub-
scales
of
the
RSVP,
patients
were
asked
to
rate
their
satis-
faction
with
vision
on
a
5-point
scale
(very
dissatisfied,
dis-
satisfied,
neither
satisfied
nor
dissatisfied,
satisfied,
or
very
satisfied)
and
to
rate
their
concern
about
their
vision
Responsiveniess
In
the
context
of
the
evaluation
of
a
functional
status
questionnaire
or
other
measurement
tool
(eg,
visual
acu-
ity),
responsiveness
refers
to
the
sensitivity
of
the
instru-
ment
to
change
following
an
intervention.
For
example,
as
discussed
previously,
1
of
the
advantages
of
disease-spe-
cific
questionnaires
(eg,
the
VF-14)
over
a
generic
health
status
questionnaire
(eg,
the
SIP)
is
that
it
is
much
more
likely
to
be
sensitive
to
the
relevant
intervention
(eg,
cataract
surgery).
The
standard
measure
of
the
respon-
siveness
of
a
questionnaire
is
to
calculate
its
effect
size.
This
can
be
most
simply
performed
by
incorporating
data
from
all
participating
patients
and
dividing
the
mean
change
in
a
measure
from
baseline
to
follow-up
by
the
standard
deviation
of
the
measure
at
baseline.17
This
sta-
tistic
was
calculated
for
the
RSVP
and
its
subscales.
A
second
technique
for
calculating
the
effect
size
is
known
as
the
responsiveness
statistic
of
Guyatt.'5
This
sta-
tistic
uses
the
same
numerator
as
in
effect
size,
but
its
denominator
is
the
standard
deviation
of
the
score
changes
of
patients
who
appear
stable
or
unchanged
over
time
on
the
basis
of
clinical
criteria.
This
technique
acknowledges
that
some
patients
may
have
improvement
or
worsening
in
certain
measurement
scores
even
though
they
may
be
clinically
unchanged.
With
this
technique,
the
responsiveness
of
an
instrument
is
predicated
on
the
notion
that
greater
change
should
be
seen
in
the
measure
for
improved
or
worsened
compared
with
stable
patients.
To
assess
effect
size
by
this
technique,
the
stable
group
was
defined
by
the
test-retest
performance
of
the
16
myopic
subjects
who
were
assessed
for
reproducibility
(see
Section
2).
In
addition
to
any
intrinsic
properties
of
the
meas-
urement
itself,
it
is
evident
that
responsiveness,
or
sensi-
tivity
to
change,
might
vary
depending
on
the
baseline
sta-
tus.
For
example,
responsiveness
might
vary
by
the
sever-
ity
of
disease
at
baseline.
Therefore,
responsiveness
was
also
evaluated
by
stratifying
the
patients
by
their
degree
of
preoperative
refractive
error.
One
of
the
subscales
derived
in
the
baseline
RSVP
was
expectations.
The
2
questions
in
this
subscale
relate
to
patients'
projected
tolerance
of
less
than
perfect
vision.
Since
it
does
not
make
sense
to
include
such
questions
454
SECTION
3
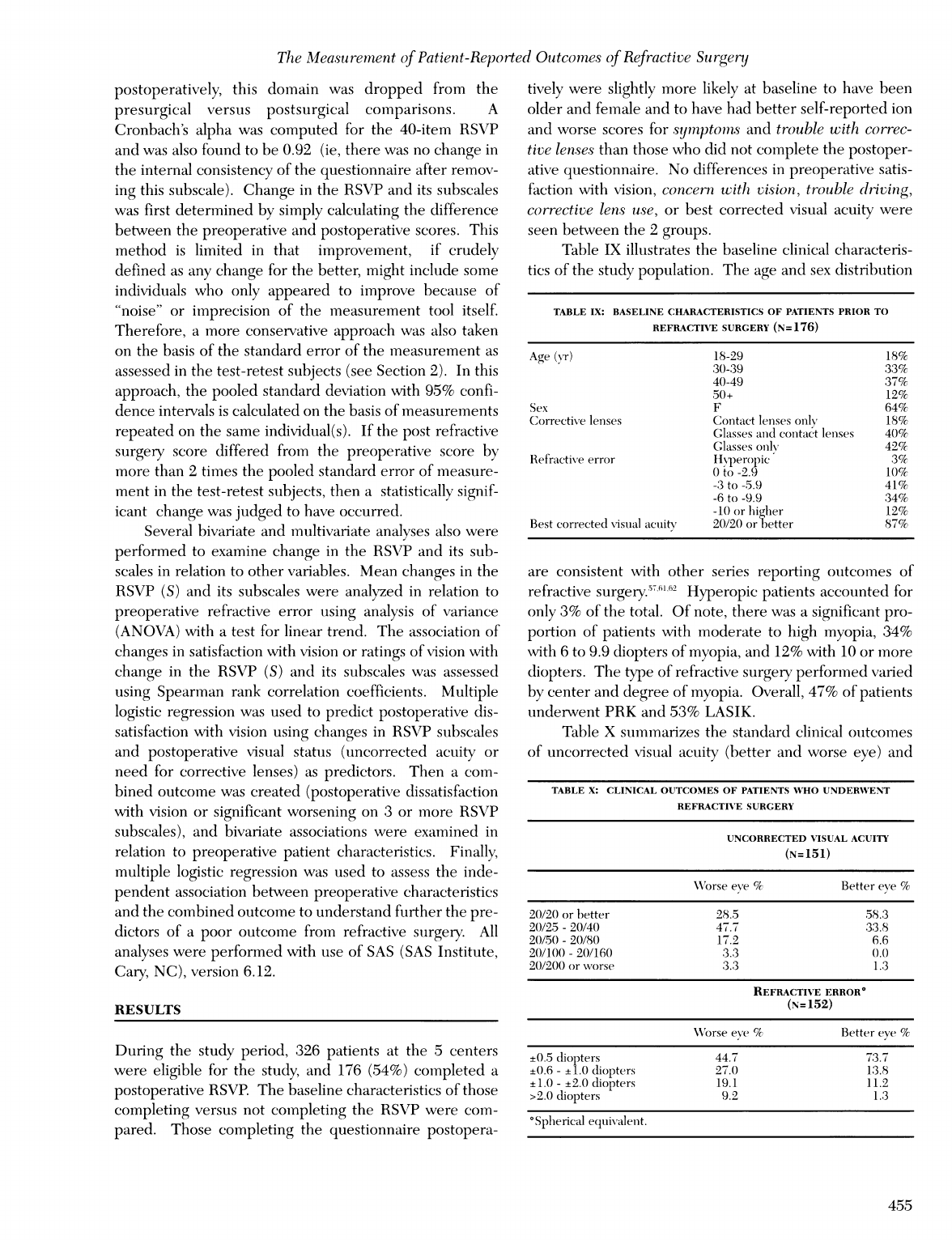
The
Measuremnent
of
Patient-Reported
Outcomes
of
Refractive
Sn
rgerij
postoperatively,
this
domain
was
dropped
from
the
presurgical
versus
postsurgical
comparisons.
A
Cronbach's
alpha
was
computed
for
the
40-item
RSVP
and
was
also
found
to
be
0.92
(ie,
there
was no
change
in
the
internal
consistency
of
the
questionnaire
after
remov-
ing
this
subscale).
Change
in
the
RSVP
and
its
subscales
was
first
determined
by
simply
calculating
the
difference
between
the
preoperative
and
postoperative
scores.
This
method
is
limited
in
that
improvement,
if
crudely
defined
as
any
change
for
the
better,
might
include
some
individuals
who
only
appeared
to
improve
because
of
"noise"
or
imprecision
of
the
measurement
tool
itself.
Therefore,
a
more
conservative
approach
was
also
taken
on
the
basis
of
the
standard
error
of
the
measurement
as
assessed
in
the
test-retest
subjects
(see
Section
2).
In
this
approach,
the
pooled
standard
deviation
with
95%
confi-
dence
intervals
is
calculated
on
the
basis
of
measurements
repeated
on
the
same
individual(s).
If
the
post
refractive
surgery
score
differed
from
the
preoperative
score
by
more
than
2
times
the
pooled
standard
error
of
measure-
ment
in
the
test-retest
subjects,
then
a
statistically
signif-
icant
change
was
judged
to
have
occurred.
Several
bivariate
and
multivariate
analyses
also
were
performed
to
examine
change
in
the
RSVP
and
its
sub-
scales
in
relation
to
other
variables.
Mean
changes
in
the
RSVP
(S)
and
its
subscales
were
analyzed
in
relation
to
preoperative
refractive
error
using
analysis
of
variance
(ANOVA)
with
a
test
for
linear
trend.
The
association
of
changes
in
satisfaction
with
vision
or
ratings
of
vision
with
change
in
the
RSVP
(S)
and
its
subscales
was
assessed
using
Spearman
rank
correlation
coefficients.
Multiple
logistic
regression
was
used
to
predict
postoperative
dis-
satisfaction
with
vision
using
changes
in
RSVP
subscales
and
postoperative
visual
status
(uncorrected
acuity
or
need
for
corrective
lenses)
as
predictors.
Then
a
com-
bined
outcome
was
created
(postoperative
dissatisfaction
with
vision
or
significant
worsening
on
3
or
more
RSVP
subscales),
and
bivariate
associations
were
examined
in
relation
to
preoperative
patient
characteristics.
Finally,
multiple
logistic
regression
was
used
to
assess
the
inde-
pendent
association
between
preoperative
characteristics
and
the
combined
outcome
to
understand
further
the
pre-
dictors
of
a
poor
outcome
from
refractive
surgery.
All
analyses
were
performed
with
use
of
SAS
(SAS
Institute,
Cary,
NC),
version
6.12.
RESULTS
During
the
study
period,
326
patients
at
the
5
centers
were
eligible
for
the
study,
and
176
(54%)
completed
a
postoperative
RSVP.
The
baseline
characteristics
of
those
completing
versus
not
completing
the
RSVP
were
com-
pared.
Those
completing
the
questionnaire
postopera-
tively
were
slightly
more
likely
at
baseline
to
have
been
older
and
female
and
to
have
had
better
self-reported
ion
and
worse
scores
for
symptomns
and
trouble
with
correc-
tive
lenses
than
those
who
did
not
complete
the
postoper-
ative
questionnaire.
No
differences
in
preoperative
satis-
faction
with
vision,
concern
with
vision,
trouble
driving,
corrective
lens
use,
or
best
corrected
visual
acuity
were
seen
between
the
2
groups.
Table
IX
illustrates
the
baseline
clinical
characteris-
tics
of
the
study
population.
The
age
and
sex
distribution
TABLE
IX:
BASELINE
CHARACTERISTICS
OF
PATIENTS
PRIOR
TO
REFRACTIVE
SURGERY
(N=176)
Age
(yr)
18-29
18%
30-39
33%
40-49
37%
50+
12%
Sex
F
64%
Corrective
lenses
Contact
lenses
only
18%
Glasses
and
cointact
lenses
40%
Glasses
ouivN
42%
Refractive
error
Hyperopic
3%
O
to
-2.9
10%
-3
to
-5.9
41%
-6
to
-9.9
34%
-10
or
higher
12%
Best
corrected
visual
acuity
20/20
or
better
87%
are
consistent
with
other
series
reporting
outcomes
of
refractive
surgery.
F76'2
Hyperopic
patients
accounted
for
only
3%
of
the
total.
Of
note,
there
was
a
significant
pro-
portion
of
patients
with
moderate
to
high
myopia,
34%
with
6
to
9.9
diopters
of
myopia,
and
12%
with
10
or
more
diopters.
The
type
of
refractive
surgery
performed
varied
by
center
and
degree
of
myopia.
Overall,
47%
of
patients
underwent
PRK
and
53%
LASIK.
Table
X
suimmarizes
the
standard
clinical
outcomes
of
uncorrected
visual
acuity
(better
and
worse
eye)
and
TABLE
X:
CLINICAL
OUTCOMES
OF
PATIENTS
WHO
UNDERWENT
REFRACTIVE
SURGERY
UNCORRECTED
VISUAL
ACUITY
(N=
151)
W\orse
eve
%
Better
eve
%
20/20
or
better
28.5 58.3
20/25
-
20/40
47.7
33.8
20/50
-
20/80
17.2
6.6
20/100
-
20/160
3.3
(.0
20/200
or
worse
3.3
1.3
REFRACTIVE
ERROR*
(N=
152)
WN'orse
eve
%
Better
eye
%
±0.5
diopters
44.7
73.7
±0.6
-
±1.0
diopters
27.0
13.8
±1.0
-
±2.0
diopters
19.1
11.2
>2.0
diopters
9.2
1.3
*Spherical
equivalent.
455
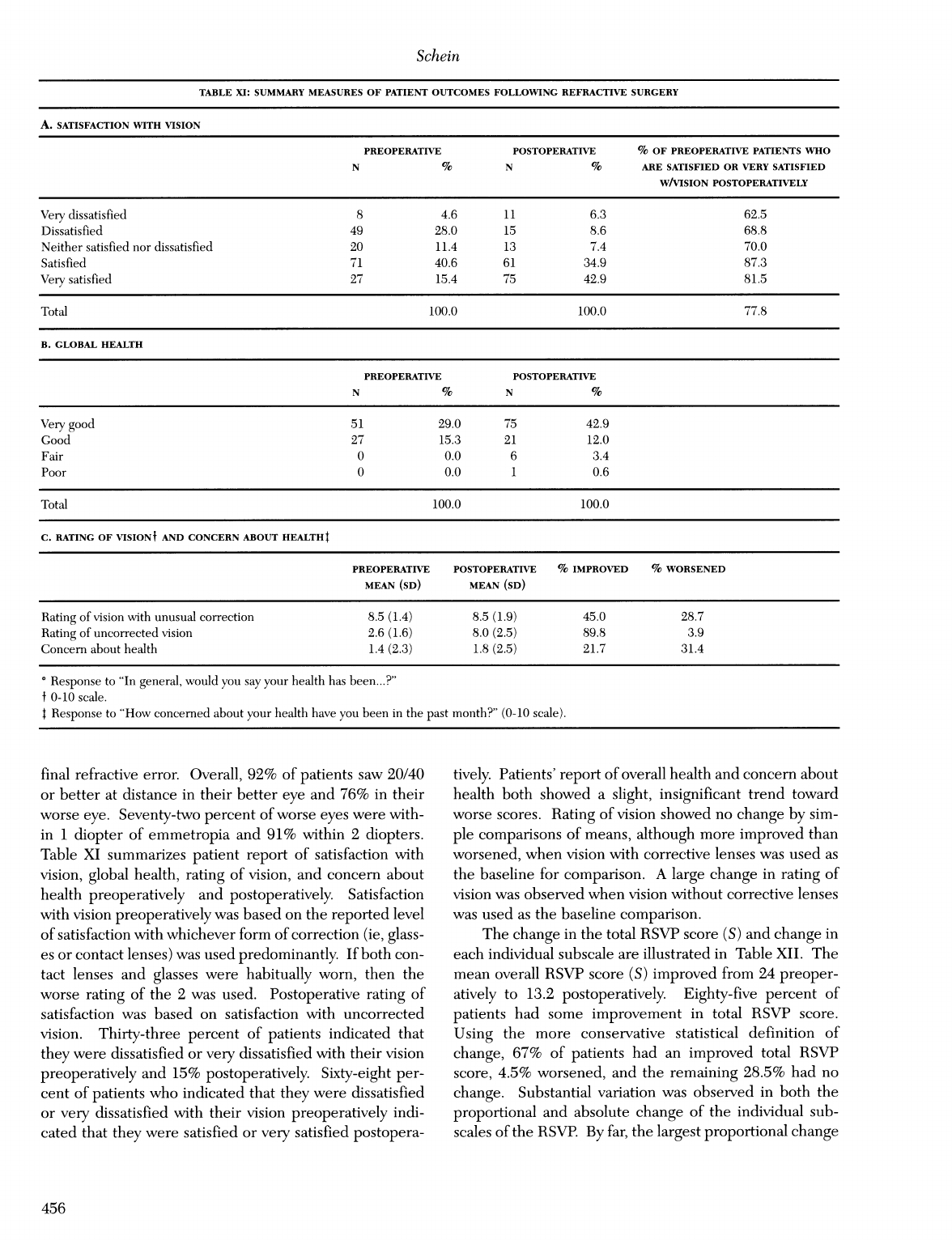
Schein
TABLE
XI:
SUMMARY
MEASURES
OF
PATIENT
OUTCOMES
FOLLOWING
REFRACTIVE
SURGERY
A.
SATISFACTION
WITH
VISION
PREOPERATIVE
POSTOPERATIVE
%
OF
PREOPERATIVE
PATIENTS
WHO
N
%
N
%
ARE
SATISFIED
OR
VERY
SATISFIED
W/VISION
POSTOPERATIVELY
Very
dissatisfied
8
4.6
11
6.3
62.5
Dissatisfied
49
28.0
15
8.6
68.8
Neither
satisfied
nor
dissatisfied
20
11.4
13
7.4
70.0
Satisfied
71
40.6
61
34.9
87.3
Very
satisfied
27
15.4
75
42.9
81.5
Total
100.0
100.0
77.8
B.
GLOBAL
HEALTH
PREOPERATIVE
POSTOPERATIVE
N
%
N
%
Very
good
51
29.0
75
42.9
Good
27
15.3
21
12.0
Fair
0
0.0
6
3.4
Poor
0
0.0
1
0.6
Total
100.0
100.0
C.
RATING
OF
VISIONt
AND
CONCERN
ABOUT
HEALTHt
PREOPERATIVE
POSTOPERATIVE
%
IMPROVED
%
WORSENED
MEAN
(SD)
MEAN
(SD)
Rating
of
vision
with
unusual
correction
8.5
(1.4)
8.5
(1.9)
45.0
28.7
Rating
of
uncorrected
vision
2.6
(1.6)
8.0
(2.5)
89.8
3.9
Concern
about
health
1.4
(2.3)
1.8
(2.5)
21.7
31.4
4
Response
to
"In
general,
would
you
say
your
health
has
been...?"
f
0-10
scale.
4
Response
to
"How
concerned
about
your
health
have
you
been
in
the
past
month?"
(0-10
scale).
final
refractive
error.
Overall,
92%
of
patients
saw
20/40
or
better
at
distance
in
their
better
eye
and
76%
in
their
worse
eye.
Seventy-two
percent
of
worse
eyes
were
with-
in
1
diopter
of
emmetropia
and
91%
within
2
diopters.
Table
XI
summarizes
patient
report
of
satisfaction
with
vision,
global
health,
rating
of
vision,
and
concern
about
health
preoperatively
and
postoperatively.
Satisfaction
with
vision
preoperatively
was
based
on
the
reported
level
of
satisfaction
with
whichever
form
of
correction
(ie,
glass-
es
or
contact
lenses)
was
used
predominantly.
If
both
con-
tact
lenses
and
glasses
were
habitually
worn,
then
the
worse
rating
of
the
2
was
used.
Postoperative
rating
of
satisfaction
was
based
on
satisfaction
with
uncorrected
vision.
Thirty-three
percent
of
patients
indicated
that
they
were
dissatisfied
or
very
dissatisfied
with
their
vision
preoperatively
and
15%
postoperatively.
Sixty-eight
per-
cent
of
patients
who
indicated
that
they
were
dissatisfied
or
very
dissatisfied
with
their
vision
preoperatively
indi-
cated
that
they
were
satisfied
or
very
satisfied
postopera-
tively.
Patients'
report
of
overall
health
and
concern
about
health
both
showed
a
slight,
insignificant
trend
toward
worse
scores.
Rating
of
vision
showed
no
change
by
sim-
ple
comparisons
of
means,
although
more
improved
than
worsened,
when
vision
with
corrective
lenses
was
used
as
the
baseline
for
comparison.
A
large
change
in
rating
of
vision
was
observed
when
vision
without
corrective
lenses
was
used
as
the
baseline
comparison.
The
change
in
the
total
RSVP
score
(S)
and
change
in
each
individual
subscale
are
illustrated
in
Table
XII.
The
mean
overall
RSVP
score
(S)
improved
from
24
preoper-
atively
to
13.2
postoperatively.
Eighty-five
percent
of
patients
had
some
improvement
in
total
RSVP
score.
Using
the
more
conservative
statistical
definition
of
change,
67%
of
patients
had
an
improved
total
RSVP
score,
4.5%
worsened,
and
the
remaining
28.5%
had
no
change.
Substantial
variation
was
observed
in
both
the
proportional
and
absolute
change
of
the
individual
sub-
scales
of
the
RSVP.
By
far,
the
largest
proportional
change
456

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
TABLE
XII:
RSVP
SUBSCALES
AND
OVERALL
S:
PREOPERATIVE,
POSTOPERATIVE,
AND
CHANGE
STATISTICS
RSVP
SUBSCALE
PREOP
PREOP
POSTOP
POSTOP
%
ANY
%
ANY
%
SIGNIFICANT
%
SIGNIFICANT
MEAN*
(SD)
RANGE
MEAN
(SD)
RANGE
IMPROVEMENT
WORSENING
IMPROVEMENTI
WORSENINGi
Concern
45.0
4.2-87.5
26.7
0-75
78.9
14.3
62.9
7.4
(18.1)
(16.8)
Functioning
15.9
0-65
7.4
0-86.4 70.4
19.5
40.2
5.9
(14.2)
(14.5)
Driving
24.3
0-100
23.7
0-100
38.0
41.5
28.3
29.5
(22.7)
(21.7)
Symptoms
19.6
0-75
10.8
0-75
59.0
27.1
44.6
12.7
(16.6)
(10.7)
Optical
problems
11.8
0-62.5
10.3
0-87.5
42.8
34.9
27.7
19.9
(13.6)
(13.5)
Glare
22.4
0-75
19.0
0-75
45.2
33.7
28.9
16.3
(17.3)
(16.1)
Trouble
w/corrective
35.0
7.1-81.3
7.4
0-75
86.5
7.0
73.7
2.3
lenses
(17.3)
(16.3)
Total
(S)
(40-item)
24.0
3.2-54.5
13.2
0-59.7
84.7
15.3
66.5
4.5
(10.6)
(10.5)
0
RSVP
and
subscale
scores
may
range
from
0-100.
Lower
scores
indicate
less
dysfunction.
f
Change
greater
than
2x
standard
error
of
measurement
(see
methods).
was
observed
for
trouble
with
corrective
lenses,
where
the
mean
fell
from
35
preoperatively
to
7.4
postoperatively.
Large
proportional
improvements
in
mean
scores
were
also
observed
for
concern
(45.0
preoperative
to
26.7
post-
operative),functioning
(15.9
preoperative
to
7.4
postoper-
ative),
and
symptoms
(19.6
preoperative
to
10.8
postoper-
ative).
Large
variation
was
also
seen
in
the
proportion
of
those
who
improved
significantly
(range,
27.7%
to
73.7%)
or
worsened
(2.3%
to
29.5%).
Of
note,
despite
the
good
outcomes
as
reflected
by
Snellen
acuity,
significant
wors-
ening
was
reported
in
the
subscale
concern
by
7.4%
of
patients,
functioning
by
5.9%,
driving
by
29.5%,
symp-
toms
by
12.7%,
optical
problems
by
19.9%,
and
glare
by
16.3%.
Only
2.3%
reported
more
trouble
with
corrective
lenses.
Figure
4
illustrates
the
preoperative
and
postop-
erative
distributions
of
the
RSVP
and
its
subscales.
P
t
40
C
c
Preoperative
Conlcern
score
a
.
'a.
c
g
I.
O
v
40
v
s
Prepraie
Dulving
score
!
I
E
S
a
a
.
a
.
I
.
.
a
..
.
.
.
X
.
..
O
40
a
so
100
Prooperati
Synmptom
cor
IU
i
.
.-1
.
..,-
II
.
-.a
.Po
ae
Optial
Problems
scor
Propat
Physical
Functioning
acor
*
........
G
s
Preoperative
Glare
score
I
I
I
a
a
.:..
0
.
.
..
.,
.
.
..
P
.
I.......
..
.
I
a
4
a
weI
Preo_per-ive
Probbms
wlthCorroaw
Lenaseoon
I:
40
U0
ProoperatveTotael
score
FIG
4
Preoperative
and
postoperative
distribution
of
RSVP
and
its
subscales
scores.
457
pi
lI.
S
.1
Ia
I-a
I
I.
a-
I
-
aO-
a.3
I
E
I.
'a'
I.
22
's.
I'
I
.
I
.
.
I
.
I
I
I
I.
.
-
-
.
6
.
I
d
:L
.1
'-,
I.
'.
..
J.
1.
."
.j
S..

Schein
TABLE
XIII:
PROPORTION
OF
PATIENTS
WORSENING
BY
NUMBER
OF
RSVP
SUBSCALES
NO.
SUBSCALES
WITH
SIGNIFICANT
WORSENING
%
PATIENTS
0
52.3
1
25.6
2
8.5
3
9.7
4
2.3
5
1.7
6
0.0
I
0.0
Chliaige
greater
than
2x
standard
error
of
measuirement
(see
methods)
Since
an
individual
may
have
improvement
or
wors-
ening
on
a
number
of
different
subscales,
the
proportion
of
individuals
reporting
up
to
7
subscales
with
significant
worsening
was
calculated,
and
this
information
is
present-
ed
in
Table
XIII.
Approximately
52%
of
patients
had
no
significant
worsening
in
any
of
the
subscales,
26%
had
worsening
in
1,
22%
in
2
or
more,
and
14.7%
of
patients
had
significant
worsening
in
3
or
more
subscales.
Figure
5
is
a
Venn
diagram
illustrating
the
relationship
between
3
different
measures
of
less
than
optimal
refrac-
tive
surgery
outcome:
the
traditional
outcomes
of
uncor-
rected
acuity,
dissatisfaction
with
vision,
and
a
new
pro-
Dissatisfied
or
er
\
20/40
in
eithere
dissatisfiedi
Nithl
%ision
/
/\
(n
=38)
NNithout
leiises
(nl=24)
;2
7
821
4
~4
>3
RSVP
stibscales
rth
\ \ s
_
X
~~~~~~~~~significaiit'
vorsenling
FIG
5
Venn
diagram
illustrating
minimal
overlap
between
3
different
measures
of
outcomes
following
refractive
surgery.
UCVA,
uncorrected
visual
acuity.
°
2x
SE
mean
variability
(see
Methods
section).
posed
measure,
a
worsening
of
3
or
more
of
the
RSVP
sub-
scales.
As
is
evident
from
this
diagram,
these
3
measures
are
assessing
different
outcome
domains.
Strikingly,
only
5
individuals
fell
into
the
intersection
of
the
3
measures.
The
relationship
between
preoperative
refractive
error
in
the
eye
with
less
refractive
error
and
change
in
the
RSVP
and
its
subscales
is
shown
in
Table
XIV.
(The
analysis
was
repeated
using
the
eye
with
greater
refractive
error,
and
the
results
were
nearly
identical.)
For
the
over-
TABLE
XIV:
ASSOCIATION
BETWEEN
PREOPERATIVE
REFRACTIVE
ERROR
AND
IMPROVEMENT
IN
RSVP
(S)
AND
SUBSCALES
FOLLOWING
REFRACTIVE
SURGERY
PREOPERATIVE
NO.
OF
Sf
%
PATIENTS
CONCERN4
%
PATIENTS
PHYSICAL
%
PATIENTS
DRIVINGII
%
PATIENTS
REFRACTIVE
PATIENTS*
IMPROVED
IMPROVED
FUNCTIONING§
IMPROVED
IMPROVED
ERROR
IN
IN
S
IN
CONCERN
IN
PHYSICAL
IN
DRIVING
BETTER
EYE
FUNCTIONING
I-lyperopic
7
5.5
(9.0)
85.7
7.9
(14.9)
57.1
-2.0
(6.2)
14.3
-11.9
(9.4)
0.00
0
to
-2.9
26
8.4
(12.9)
76.9
14.1
(20.1)
69.2
4.0
(21.1)
63.6
0.4
(23.0)
28.6
-3
to
-5.9
82
12.2
(13.2)
87.8
20.7
(19.8)
82.9
8.8
(21.9)
69.1
-0.6
(31.0)
42.5
-6
to
-9.9
48
11.2
(12.9)
83.3
19.7
(19.2)
83.0
10.1
(18.2)
80.4
1.6
(22.9)
39.1
-10
or
higher
13
8.9
(9.7)
84.6
12.4
(25.9)
69.2
9.0
(9.1)
84.6
9.0
(24.7)
41.7
PREOPERATIV'E
NO.
OF
SYMPTOMSS
%
PATIENTS
OPTICAL
%
PATIENTS
GLAREIf
%
PATIENTS
TROUBLE
%
PATIENTS
REFRACTIVE
PATIENTS*
IMPROVED
PROBLEMS"*
IMPROVED
IMPROVED
WITH
IMPROVED
ERROR
IN
IN
IN
OPTICAL
IN
GLARE
CORRECTIVE
IN
TROUBLE
BETIER
EYE
SYMfPTOMS
PROBLEMS
LENSEStt
W/LENSES
Hyperopic
7
13.2
(19.1)
85.7
1.3
(12.8)
28.6
5.4
(12.9)
57.1
23.3
(20.4)
85.7
0
to
-2.9
26
3.4
(17.3)
38.1
0.1
(21.1)
38.1
7.7
(18.4)
57.1
35.8
(25.8)
91.7
-3
to
-5.9
82
10.5
(16.9)
63.3
1.2
(17.8)
35.4
3.7
(18.4)
41.8 29.9
(19.5)
90.0
-6
to
-9.9
48
9.2
(22.5)
58.7
3.3
(16.0)
56.5
2.2
(16.3)
45.7
21.8
(21.9)
79.2
-10
or
higher
13
6.7
(17.7)
53.8
1.9
(9.7)
53.8
2.2
(21.3)
38.5
17.6
(15.7)
83.3
0
The
numher
of
patients
in
eaclh
category
varies
for
each
subscale
due
to
some
missing
data.
The
Ns
in
this
table
apply
to
the
total
S
score.
f
Analysis
of
variance
for
difference
in
meanis;
F=0.86;
P=.489;
Test
for
linlear
trend;
F=0.61;
P=.437.
Anialysis
of'sariance
for
difference
in
means;
F=1.39;
P=.241;
Test
for
linear
trend;
F=0.58;
P=.449.
§
Analysis
of
varianice
for
difference
in
means;
F=0.85;
P=.496;
Test
for
linear
trend;
F=2.16;
P=.144.
11
Analysis
of
variaioce
for
difference
in
means;
F=0.72;
P=.578;
Test
for linear
trend;
F=2.62;
P=.108.
¶
Aalysis
of
variance
for
differenice
in
means;
F=0.73;
P=.573;
Test
for
linear
trend;
F=0.15;
P=.698.
Anialvsis
of
variance
for
difference
in
means;
F=0.16;
P=.958;
Test
for
linear
trend;
F=0.07;
P=.789.
ff
Analysis
of
variance
for
differenice
in
means;
F=0.39;
P=.817;
Test
for
linear
trend;
F=0.46;
P=.500.
tt
Anialysis
of
variance
for
difference
in
means;
F=2.81;
P=.027;
Test
for
linear
trend;
F=1.51;
P=.220.
458

Th1e
Measu
renient
of
Patient-Reported
Outcomes
of
Refractive
Sn
rgery
all
RSVP
and
the
individual
subscales
(except,
perhaps,
for
trouble
with
lenses,
where
a
significant
difference
in
means
but
not
in
linear
trend
was
seen),
neither
the
mag-
nitude
of
change
nor
the
percent
of
patients
showing
improvement
varied
by
preoperative
refractive
error.
These
findings
indicate
that
the
degree
of
improvemient
reported
by
patients
in
these
various
domains
cannot
be
predicted
by
the
amount
of
refractive
error
preoperative-
ly.
Similarly
(Table
XV),
the
correlations
between
change
in
satisfaction
with
vision
or
change
in
rating
of
vision
and
the
RSVP
and
most
of
its
subscales
were
significant,
whereas
there
was
no
correlation
at
all
between
change
in
refractive
error
in
either
eye
and
change
in
satisfaction.
The
responsiveness
of
the
RSVP
and
its
subscales
was
calculated
using
2
statistical
methods
(effect
size
and
Guyatt's
responsive
statistic
[see
Methods
section])
and
using
3
different
external
measures
of
improvement.
These
external
measures
included
improved
satisfaction
with
vision,
having
an
uncorrected
visual
acuity
of
20/20
or
better
in
at
least
1
eye,
and
not
needing
spectacle
or
con-
tact
lens
correction
postoperatively.
Table
XVI
summa-
rizes
these
calculations.
According
to
Cohen,63
it
is
rea-
sonable
to
view
an
effect
size
of
0.2
as
"small,"
0.5
as
"medium,"
and
0.8
as
"large."
The
overall
RSVP
(S)
demonstrated
a
large
effect
size
in
all
the
comparisons.
As
measured
by
these
techniques,
the
responsiveness
of
the
individual
subscales
varied
substantially.
Driving
was
con-
sistently
the
least
responsive,
and
glare
and
optical
prob-
lemns
were
modestly
responsive.
The
subscales
concern
and
trouble
with
lenses
were
consistently
the
most
respon-
sive.
Finally,
Table
XVII
illustrates
the
responsiveness
of
the
RSVP
and
its
subscales,
stratified
by
preoperative
refractive
error.
The
responsiveness
of
the
questionnaire
subscales
did
not
vary
by
preoperative
refractive
error
with
the
exception
of
physical
functioning,
where
there
was
a
trend
toward
greater
responsiveness
for
greater
degrees
of
preoperative
myopia.
A
multivariate
analysis
was
performed
to
try
to
iden-
tify
factors
associated
with
patient
satisfaction
with
uncor-
rected
vision
postoperatively.
As
indicated
in
Section
1
of
this
thesis,
previous
research
has
indicated
that
the
strongest
predictors
of
dissatisfaction
after
refractive
sur-
gery
are
poor
uncorrected
distance
actiity
and
ongoing
need
for
spectacles
and/or
contact
lenses.
Since
these
variables
are
highly
correlated,
3
separate
analyses
were
done,
each
adjusting
for
age
and
sex
(
Table
XVIII),
where
the
first
model
included
uncorrected
visual
acuity;
the
second,
the
use
of
corrective
lenses
for
distance;
and
the
third,
the
use
of
lenses
for
distance
or
near.
In
all
3
mod-
els,
the
worsening
of
3
or
more
subscales
of
the
RSVP
was
independently
associated
with
dissatisfaction
with
vision
following
refractive
surgery.
In
each
mnodel,
worsening
on
3
or
more
subscales
was
associated
with
approximately
a
sixfold
excess
risk
of
reporting
dissatisfaction
with
vision
postoperatively.
Worsening
on
3
or
more
RSVP
subscales
was
found
to
be
a
stronger
factor
in
predicting
dissatisfac-
tion
than
the
traditional
clinical
assessments
of
uncorrect-
ed
visual
acuity
and
need
for
distance
or
reading
lenses.
Only
the
need
for
distance
lenses
was
a
stronger
predictor.
To
test
the
hypothesis
that
the
RSVP
or
1
or
more
of
its
components
administered
before
surgery
might
be
helpful
in
predicting
postoperative
outcomes,
a
final
TABLE
XV.:
SPEARMIAN
CORRELATIONS
BETWEEN
CHANGES
IN
DIFFERENT
OUTCOMIE
MIEASURES
(N)
CHANGE
IN
CHANGE
IN
CHANGE
IN
CHANGE
IN
CHANGE
IN
REFRACTIVE
REFRACTIVE
RSVT
(S)
CONCERN
PHYSICAL
ERROR
ERROR
FUNCTIONING
BETTER
EYE
WORSE
EYE
Chlange
in
satisfaction
with
vision
-0.104
-0.06f
0.59+
0.441
0.48+
(n=150)
(n=150)
(n=174)
(n=173)
(n=167)
Change
in
rating
of
vision
0.28
0.21
0.58
0.31
0.50
(n
=
109)
(n=
109)
(nI=
129)
(i=
128)
(n=
126)
CHANGE
IN
CHANGE
IN
CHANGE
IN
CHIANGE
IN
CHANGE
IN
DRIVING
SYNIPTONIS
OPTICAL
GLARE
TROUBLE
PROBLEMIS
W/CORRECTIVE
LENSES
Change
in
satisfaction
wNithi
vision
0.371
0.33+
0.33+
0.33+
0.251
(n=164)
(in=
164)
(n=164)
(n
=
164)
(n=169)
Change
in
rating
of
vision
0.52
0.44
0.52
0.31
-0.02
(n
=123)
(n=126)
(
4=126)
(
n=126)
n
n=126)
P
value
=
0.2:37
f
P
value
=
0.444
+
P
value
<
0.001
459

Schein
TABLE
XVI:
RESPONSIVENESS
OF
RSVP
(S)
AND
ITS
SUBSCALES
S
BY
DIFFERENT
DEFINMONS
OF
IMPROVED
OUTCOME
A.
USING
POSTOPERATIVE
SATISFACTION
WITH
VISION
AS
MEASURE
OF
OUTCOME
RSVP
SCALE
EFFECT
SIZE*f
GUYATT'S
RESPONSE
STATISTIC*4t
IMPROVED
SATISFACTION
IMPROVED
SATISFACTION
(N=91)
(N=91)
Concern
25.6/17.9=
1.43
25.6/6.7=3.82
Physical
functioning
13.5/13.9=0.97
13.5/7.2=1.88
Driving
7.4/21.7=0.34
7.4/8.3=0.89
Symptoms
14.0/18.0=0.78
14.0/5.8=2.41
Optical
problems
6.5/15.6=0.42
6.5/4.4=1.48
Glare
9.4/18.7=0.50
9.4/7.2=
1.31
Trouble
with
lenses
33.0/19.1=1.73
33.0/8.8=3.75
Total
S
16.4/11.1=
1.48
16.4/3.9=4.21
B.
USING
POSTOPERATIVE
VISUAL
ACUITY
AS
MEASURE OF
OUTCOME
RSVP
SCALE
EFFECT
SIZE§1I
GUYATT'S
RESPONSE
STATISTIC§t
1
EYE
20/20
OR
BETTER
1
EYE
20/20
OR
BETTER
(N=88)
(N=88)
Concern
19.2/18.4=1.04
19.2/67=2.87
Physical
functioning
9.5/16.0=0.59
9.5/7.2=1.32
Driving
1.7/25.2=0.07
1.7/8.3=0.20
Symptoms
9.6/17.9=0.54
9.6/5.8=
1.66
Optical
problems
1.8/13.8=0.13
1.8/4.4=0.41
Glare
4.3/18.4=0.23
4.3/7.2=0.60
Trouble
with
lenses
29.8/17.4=1.71
29.8/8.8=3.39
Total
S
11.9/11.8=1.01
11.9/3.9=3.05
C.
USING
POSTOPERATIVE
NEED
FOR
CORRECTIVE
LENSES
AS
MEASURE
OF
OUTCOME
RSVP
SCALE
EFFECT
SIZE*f
GUYATT'S
RESPONSE
STATISTIC*t
NO
DISTANCE
LENSES
NO
DISTANCE
LENSES
(N=153)
(N=153)
Concern
20.2/18.1
=
1.12
20.2/6.7=3.01
Physical
functioning
8.8/13.8=0.64
8.8/7.2=1.22
Driving
-0.7/21.2=-0.03
-0.7/8.3=-0.08
Symptoms
8.9/16.4=0.54
8.9/5.8=1.53
Optical
problems
1.8/13.7=0.13
1.8/4.4=0.41
Glare
4.1/17.0=0.24
4.1/7.2=0.57
Trouble
with
lenses
31.1/17.6=1.77
31.1/8.8=3.53
Total
(S)
12.1/10.4=1.16
12.1/3.9=3.10
°
Numerator
is
mean
change
in
subscale
score
(or
Total
S)
among
those
who
reported
any
improvement
in
satisfaction
with
vision
after
surgery.
t
Denominator
is
standard
deviation
of
preoperative
subscale
score
(or
Total
S)
among
those
who
reported
any
improvement
in
satisfaction
with
vision
after
surgery.
Denominator
is
standard
deviation
of
change
in
subscale
score
(or
Total
S)
among
stable
group
of
myopes
who
did
not
undergo
surgery.6
§
Numerator
is
mean
change
in
subscale
score
(or
totals)
among
those
who
had
at
least
1
eye
with
20/20
vision
after
surgery.
11
Denominator
is
standard
deviation
of
preoperative
subscale
score
(or
Total
S)
among
those
who
had
at
least
1
eye
with
20/20
vision
after
surgery.
analysis
was
performed.
In
this
analysis
(Table
XIX),
the
goal
was
to
look
for
predictors
of
poor
outcome
as
report-
ed
by
patients.
Poor
outcome
was
defined
as
a
postoper-
ative
report
of
being
dissatisfied
with
vision
or
having
a
significant
reduction
in
3
or
more
RSVP
subscales.
Age,
sex,
and
preoperative
refractive
error
were
not
predictive,
although
age
greater
than
45
was
consistently
associated
with
an
odds
ratio
of
approximately
1.5
(ie,
those
over
age
45
more
likely
to
be
dissatisfied).
Three
of
the
preopera-
tive
RSVP
subscales
(expectations,
physical
functioning,
and
symptoms)
were
associated
with
approximately
a
twofold
likelihood
of
poor
postoperative
outcome.
In
these
multivariate
analyses,
physicalfunctioning
reached
borderline
significance
(P=.06)
and
symptoms
was
statisti-
cally
significant
(P=.05)
as
a
predictor.
460

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
TABLE
XVII:
RESPONSIVENESS
OF
RSVP
SUBSCALES
AND
TOTAL
S
BY
PREOPERATIVE
REFRACTIVE
ERROR
IN
THE
BETTER
EYE
PREOPERATIVE
TOTAL
S
CONCERN
PHYSICAL
DRIVING
SYMPTOMS
OPTICAL
GLARE
TROUBLE
REFRACTIVE
FUNCTIONING
PROBLEMS
W/LENSES
ERROR
IN
THE
BETTER
EYE
(DIOPTERS)
Hyperopic
(N=7)
0.63
0.47
-0.30
-1.18
0.71
0.15
0.34
1.55
0.0
to
-2.9
(N=26)
0.75
0.71
0.33
0.02 0.19
0.01
0.41
1.88
-30.
to
-5.9
(N=82)
1.15
1.20
0.59
-0.03
0.67
0.09
0.21
1.81
-6.0
to
-9.9
(N=48
1.11
1.16
0.73
0.06
0.52
0.24
0.13
1.29
-10
or
worse
(N=13)
0.81
0.67
0.62
0.47
0.40
0.16
0.12
1.04
TABLE
XVIII:
PREDICTORS
OF
POSTOPERATIVE
DISSATISFACTION
WITH
VISION
MODEL
MODEL
2
MODEL
3
ODDS
RATIO
95%
CI
ODDS
RATIO
95%
CI
ODDS
RATIO
95%
CI
Age
.45
1.75
(0.59,
5.16)
1.52
(0.53,
4.37)
0.93
(0.30,
2.92)
Female
2.20
(0.69,
6.98)
1.89
(0.61,
5.86)
2.06
(0.72,
5.94)
Preoperative
refractive
1.02
(0.87,
1.19)
1.03
(0.87,
1.20)
1.00
(0.86,
1.16)
error'
.3
RSVP
subscales
5.84
(1.88,
18.13)+
6.96
(2.21,
21.87)t
6.20
(2.10,
18.26)t
w/significant
worseningf
Postoperative
uncorrected
3.54
(1.23,
10.19)§
acuity
worse
than
20/40
in
either
eye
Wear
distance
lenses
11.68
(3.72,
36.73)t
Wear
distance
or
4.86
(1.60,
14.80)t
reading
glasses
CI=confidence
interval.
*
Spherical
equivalent,
eye
with
less
refractive
error.
f
Change
greater
than
2x
standard
error
of
measurement
(see
Methods).
,
P<
.01.
§
0.01
<
P<
.05.
CONCLUSIONS
As
previously
discussed,
the
standard
indices
for
measuring
patient
outcomes
following
refractive
surgery
have
largely
been
limited
to
assessing
uncorrected
acuity
and
refractive
error.
Patient-reported
outcomes
either
have
not
been
reported
at
all
or
have
been
typically
limited
to
a
report
of
satisfaction
with
vision.
The
RSVP
and
its
subscales
have
been
shown
to
exhibit
a
variety
of
properties
that
recom-
mend
it
as
an
outcome
measure
which
should
be
comple-
mentary
to
the
traditional
clinical
assessments.
First,
the
RSVP
and
its
subscales
have
been
shown
to
be
highly
responsive
to
the
intervention
of
refractive
surgery.
Other
measures,
including
more
global
health
assessments,
were
not
responsive.
Second,
the
RSVP
and
its
subscales
have
been
shown
to
be
correlated
with
change
in
satisfaction
with
vision
postoperatively.
Change
in
refractive
error
was
not
correlated
at
all
with
this
outcome.
Third,
as
illustrated
in
the
Venn
diagram
(Fig
5),
the
use
of
uncorrected
Snellen
acuity,
self-report
of
satisfaction
with
vision,
and
the
RSVP
as
outcome
measures
do
not
identify
the
same
group
of
patients
as
successes
or
failures
of
the
surgical
intervention.
The
RSVP
clearly
provides
additional
information
about
patient
outcomes
that
is
not
captured
by
simply
assessing
patient
satisfaction
or
uncorrected
acuity.
Moreover,
as
shown
in
the
multivariate
analyses,
failure
to
improve
on
3
or
more
RSVP
subscales
was
independently
predictive
of
dissatisfaction
with
vision.
Fourth,
the
magnitude
of
improvement
in
the
RSVP
and
its
subscales
did
not
vary
significantly
in
relation
to
the
magnitude
of
the
initial
pre-
operative
refractive
error.
Although
this
might
appear
counterintuitive,
it
is
analogous
to
the
findings
reported
for
cataract
surgical
patients
when
the
VF-14
was
evaluated
as
one
of
multiple
outcome
measures
of
cataract
surgery.8
For
cataract
surgery,
it
was
found
that
the
magnitude
of
per-
ceived
functional
improvement
was
not
greater
for
those
with
worse
visual
acuity
preoperatively
(eg,
20/200
versus
20/50).
This
indicated
that
the
problems
with
visual
func-
tion
perceived
by
those
who
opted
for
cataract
surgery
were
not
reflected
by
Snellen
acuity
but
by
perceived
functional
461

Schein
o
1-
o
c
ci
oZ
Lc
o
666=
'F
1-7
(6
z
ci
a
Z
Ic
co
cc
c1
Ci1
-
b
c
z
cnc
c
o
ccz
ccit
t-r~
z
0
c:
cc~~~~~
O
z
cc~~~~~~~~~~~~~~~~~~~
ci
0
ii-
~~~~~
z
Q
c
b.
IC
0
-
C
0
IC
0
C
C
0
0
O4
Q:
e
0
C
co
0
1-
ca
_-
o.
cc
o
cc
cii
o
-
o
cq
X
in
I'l
o
O'
cc
C.C
-1-
Z~
cc
cc
llc
666"-
c
I-
srcI
t
cq
cq~~~~~~~~~c
c-
cce
-
0
o
I.-
t
c,0
>
ci
cc
-
o
:
>~~~~~~~~~~~~~~~~~~~
o o
~~~bZ
-~~~~~~~~
0
.
u
>
1
o
o
o
-
~-
o0Oc
Q.
bocc
0
~~~~~~~~
.0~~~~~~~
b.C
0
0
0
1<
~~~~~~~~~~~~~
0-~~~~-0
~~~~
o~'
Q
s
_
z
0
0*
-o
0
0
CA
0-
cn
:;
0
z
0
u1:
;t
i*
CA
04
I'lc
0
0
cn
..
Eu
0
0.
12
0
0
e-
C
m
0
C
z
C~
o
0
'c
0-
C;
u:
C
0
cr
Q
CA
Q
ct
'C.
un
x
0
Q
ce
z
0
z
0
m
z
0
cc
cc
t-
C-
ci
H
4
0
C/N
6
11
cc
cc
cc
.N
0
11
462

Th
e
Measuremiwnt
of
Patient-Reported
Ouitcomes
of
Refractive
Surgery
need.
One
might
infer,
therefore,
that
the
magnitude
of
refractive
error
is
not
adequate
as
a
sole
measure
to
char-
acterize
patients'
functional
status
or
perceived
limitations
(eg,
symptoms,
difficulties
with
glasses
or
contact
lenses)
related
to
their
refractive
error.
Although
the
RSVP
produces
an
overall
composite
score,
the
use
of
this
total
score
may
not
be
optimal.
For
example,
it
is
possible
that
the
total
score
might
show
some
improvement
even
if
there
were
a
significant
(ie,
important
to
the
patient)
decrement
in
one
or
more
of
the
individual
subscales.
Therefore,
it
would
be
preferable
to
use
and
report
the
individual
subscales
in
any
characteri-
zation
of
patients
undergoing
refractive
surgery.
It
would
be
potentially
very
informative
to
learn,
for
example,
that
an
intervention
may
have
a
large
benefit
in
patient-report-
ed
function
but
a
worsening
in
symptoms
or
glare.
Retention
of
the
subscales
allows
this
possibility.
The
RSVP
and
a
number
of
its
subscales
were
shown
to
be
responsive
to
the
intervention
of
refractive
surgery
as
evi-
denced
by
the
large
effect
sizes
or
Guyatt's
responsiveness
statistics
found.
In
interpreting
the
data
on
effect
size,
the
overall
consistency
of
the
data
is
more
important
than
the
individual
effect
sizes
calculated.
Also,
the
finding
that
a
particular
subscale
has
a
small
effect
size
does
not
neces-
sarily
imply
that
the
subscale
provides
no
useful
informa-
tion
in
the
assessment
of
an
intervention.
For
example,
the
driving
subscale
consistently
was
shown
to
have
a
small
effect
size.
Yet,
as
shown
in
Table
XII,
an
equal
and
large
proportion
of
patients
reported
improvement
and
worsening
of
driving
ability
following
refractive
surgery.
Clearly,
one
would
not
want
to
delete
issues
related
to
driving
from
an
assessment
of
the
outcomes
of
refractive
surgery,
even
though
this
subscale
was
shown
to
have
a
low
effect
size.
From
the
perspective
of
surgeons
using
the
standard
clinical
outcomes
of
uncorrected
distance
acuity
and
achieved
refractive
error,
the
outcomes
of
this
cohort
of
refractive
surgical
patients
was
very
good,
especially
given
the
significant
number
of
individuals
who
had
moderate
to
high
myopia
preoperatively.
Yet,
as
demonstrated
by
the
RSVP
subscales,
worsening
was
reported
in
the
domains
related
to
driving,
symptoms,
optical
problems,
and
glare
by
13%
to
30%
of
patients.
From
the
patient
perspective,
therefore,
there
remains
significant
room
for
improvement.
The
findings
presented
do
not,
of
course,
represent
a
final
conclusion
regarding
patient
outcomes
of
refractive
surgery.
The
research
described
was
performed
to
develop
and
evaluate
the
RSVP
rather
than
to
compare
surgical
outcomes
by
technique
or
other
factors.
The
sur-
gery
performed
on
this
cohort
was
done
in
1997
in
5
cen-
ters.
It
is
possible
that
one
might
find
a
greater
benefit
(eg,
due
to
fewer
patient-perceived
limitations)
to
surgery
performed
in
the
year
2000
or
in
a
different
group
of
patients.
Yet,
it
is
likely
that
the
incorporation
of
the
patient's
perspective
on
HRQoL
associated
with
refractive
error
and
its
correction
will
provide
a
valuable
new
metric
to
assess
and
improve
patient
outcomes.
SECTION
4
FUTURE
RESEARCH
NEEDS
AND
PLANS
The
RSVP
and
its
subscales
have
been
validated
by
accepted
psychometric
standards
and
have
been
shown
to
be
responsive
to
the
intervention
of
refractive
surgery.
The
instrument
provides
useful
information
about
patients
and
their
outcomes
that
cannot
be
obtained
from
standard
measures.
However,
there
is
additional
work
to
be
done
to
maximize
its
value
as
a
research
tool
and
mod-
ifications
that
should
be
considered
to
render
it
feasible
and
useful
in
clinical
practice.
From
a
research
perspective,
it
would
first
be
valuable
to
administer
the
RSVP
preoperatively
and
postoperatively
to
a
larger
cohort
of
patients
with
a
wide
range
of
refractive
error
where
detailed
clinical
information
is
also
collected.
Although
the
items
of
the
RSVP
were
generated
through
a
process
that
included
the
concerns
of
patients
with
hyper-
opia
and
presbyopia,
the
instriment's
validity
and
respon-
siveness
were
assessed
in
a
population
that
was
largely
myopic.
The
development
of
a
larger
database
of
subjects
with
clinical
and
RSVP
data
would
also
allow
one
to
refine
the
predictive
models
further.
An
important
goal
of
this
research
is
to
define,
on
the
basis
of
information
collected
before
surgery,
subgroups
of
patients
who
have
a
greater
likelihood
of
worse
outcomes
after
surgery.
A
fundamental
assumption
of
this
research
program
is
that
standard
clinical
information
can
be
combined
with
insights
from
the
RSVP
(or
similar
questionnaires)
to
develop
predictive
models
that
are
significantly
more
accurate
than
could
be
obtained
using
either
the
clinical
information
or
the
questionnaire
data
alone.
The
data
collected
on
the
cohort
of
patients
present-
ed
in
this
thesis
suggest
that
data
derived
preoperatively
from
the
RSVP
subscales
symptoms,
physical
functioning,
and
perhaps
expectations
may
be
combined
with
age
and
sex
to
improve
one's
prediction
of
who
will
do
poorly
following
refractive
surgery.
However,
these
analyses
need
to
be
repeated
in
larger
cohorts
of
patients.
This
will
allow
not
only
an
opportunity
to
confirm
the
findings
presented
here
but
also
additional
statistical
power
that
would
enable
more
detailed
analyses
of
subgroups
of
patients.
A
second
aspect
that
I
recommend
for
a
research
agen-
da
on
patient
outcomes
of
refractive
surgery
is
the
incorpo-
ration
of
patient
"utilities"
into
the
assessment.
A
patient
"utility"
is
simply
the
preference
of
a
patient
for
one
partic-
ular
health
state
over
another.
There
are
a
variety
of
dif-
ferent
accepted
methodologies
for
assessing
patient
prefer-
463

Schein
ences64
66
that
reflect
different
strategies
to
elicit
patients
to
order
their
preferences
for
different
states
or
outcomes
on
a
scale.
For
example,
a
patient
might
be
asked
to
rate
hav-
ing
trouble
with
night
driving
on
a
scale,
anchored
at
one
end
by
"total
blindness"
and
the
other
by
"perfect
vision."
These
techniques
bear
on
the
important
issue
of
how
important
a
given
outcome
is
to
an
individual
patient.
Consider,
then,
2
imaginary
patients
who
have
20/20
uncor-
rected
acuity
following
refractive
surgery
for
the
same
degree
of
preoperative
myopia.
They
also
have
identical
RSVP
and
subscale
scores
that
include
significant
(and
identical)
worsening
on
the
glare
and
driving
subscales.
One
patient,
however,
has
rated
limitations
in
night
driving
near
the
"total
blindness"
end
of
the
preference
scale,
and
the
other
considers
such
a
limitation
no
more
than
a
minor
annoyance
having
rated
it,
as
an
isolated
symptom,
near
the
"perfect
vision"
end
of
the
scale.
Clearly,
these
2
patients
would
feel
that
they
had
experienced
very
different
out-
comes
of
refractive
surgery,
and
that
difference
may
not
have
been
captured
by
a
HRQoL
questionnaire
such
as
the
RSVP.
In
summary,
therefore,
it
would
be
useful
to
incor-
porate
a
measure
of
patient
preferences
to
help
to
interpret
the
results
of
the
RSVP
for
individual
patients.
Third,
it
would
be
valuable
to
learn
whether
the
RSVP
or
at
least
certain
of
its
subscales
would
be
able
to
distinguish
outcomes
of
competing
refractive
surgical
techniques.
Although
the
questionnaire
has
been
shown
to
be
very
responsive
to
the
intervention
of
refractive
sur-
gery,
it
does
not
necessarily
follow
that
it
would
be
suffi-
ciently
sensitive
to
distinguish
between
competing
tech-
niques,
such
as
LASIK
and
PRK
or other
evolving
tech-
niques.
Currently,
at
least
for
comparable
degrees
of
myopia,
the
standard
clinical
assessments
of
refractive
error
and
uncorrected
Snellen
acuity
have
not
been
able
to
distinguish
the
results
of
LASIK
and
PRK.67
However,
it
is
reasonable
to
consider
that
patient
perspectives
on
the
outcomes
of
these
various
approaches
will
be
helpful,
if
not
crucial,
in
their
assessment.
Ideally,
one
would
hope
that
a
research
tool
such
as
the
RSVP
might
inform
and
improve
clinical
practice.
However,
even
given
the
assumption
that
the
question-
naire
provides
insights
that
may
be
important
to
refractive
surgeons
and
their
patients,
it
will
not
be
used
routinely
in
a
clinical
setting
unless
a
variety
of
criteria
are
met.
The
administration
of
the
questionnaire
(1)
should
not
perturb
the
normal
flow
of
patients
in
an
efficient
practice,
(2)
should
expend
little
staff
time,
and
(3)
should
result
in
the
display
of
data
in
real
time
for
the
surgeon
and
patient
to
review.
As
it
currently
exists
as
a
research
tool,
the
RSVP
would
not
meet
these
criteria.
However,
current
efforts
are
now
being
devoted
to
programming
the
RSVP
onto
a
personal
computer
platform
in
a
manner
that
will
allow
patients
to
proceed
rapidly
through
the
questionnaire
without
supervision.
The
scoring
algorithms
will
be
embedded
within
this
program
so
that
the
patient's
total
and
subscale
scores
will
be
available
immediately
after
the
questionnaire
has
been
completed.
This
questionnaire
information
could
then
be
merged
with
the
standard
clin-
ical
markers
(eg,
age,
sex,
refractive
error)
on
the
same
patient
and
compared
with
a
large
existing
database
of
patients
who
had
previously
supplied
outcomes
data.
This
comparison
would
enable
the
surgeon
and
patient
to
use
the
predictive
model
in
real
time
to
inform
their
decisions
regarding
surgical
intervention.
ACKNOWLEDGEMENTS
I
would
like
especially
to
acknowledge
the
skills
and
assistance
of
Susan
Vitale,
PhD,
whose
exacting
attention
to
detail
underlies
the
statistical
work
of
this
thesis.
Further
statistical
consultation
was
expertly
provided
by
Sandra
Cassard,
ScD,
and
constructive
advice
and
criticism
by
Dr
Earl
P.
Steinberg.
It
is
only
through
the
support
of
the
par-
ticipating
clinical
directors
and
their
coordinators
that
this
project
could
be
completed:
Dr
Dimitri
Azar
(coordinator,
Mr
David
Rees),
Massachusetts
Eye
and
Ear
Infirmary,
Boston;
Dr
Howard
Gimbel
(coordinator,
Ms
Maria
Ferensowicz),
Gimbel
Eye
Center
and
the
Gimbel
Foundation,
Calgary,
Alberta,
Canada;
Dr
Peter
Hersh
(coordinator,
Ms
Bethann
Hibbert),
Cornea
and
Laser
Vision
Institute,
Teaneck,
New
Jersey;
Dr
Roy
Rubinfeld
(coordinator,
Ms
Kate
Kelly),
Washington
Eye
Physicians
and
Surgeons,
Chevy
Chase,
Maryland;
Drs
Terrence
O'Brien,
Nada
Jabbur,
and
Richard
Schoen
(coordinator,
Ms
Rebecca
Scarborough),
Wilmer
Eye
Institute,
Johns
Hopkins
Medical
Institutions,
Baltimore.
Finally,
I
would
like
to
acknowledge
Ms
Alice
Flumbaum,
whose
secretari-
al
and
organizational
support
are
unparalleled.
REFERENCES
1.
Patrick
DL,
Deyo
RA.
Generic
and
disease-specific
measures
in
assessing
health
status
and
quality
of
life.
Med
Care
1989;27:S217.
2.
Bergner
M,
Bobbitt
RA,
Carter
WB,
et
al.
The
Sickness
Impact
Profile:
Development
and
final
revision
of
a
health
status
measure.
Med
Care
1987;8:191-210.
3.
Ware
JE
Jr,
Sherboume
CD.
The
MOS
36-Item
Short-Form
Health
Survey
(SF-36):
I.
Conceptual
framework
and
item
selec-
tion.
Med
Care
1993;31:247-263.
4.
Steinberg
EP,
Tielsch
JM,
Schein
OD,
et
al.
National
study
of
cataract
surgery
outcomes:
Variation
in
4-month
postoperative
outcomes
as
reflected
in
multiple
outcome
measures.
Ophthalmology
1994;101:113-141.
5.
Schein
OD,
Steinberg
EP,
Cassard
SD,
et
al.
Predictors
of
out-
come
in
patients
who
underwent
cataract
surgery.
Ophthalmology
1995;102:817-823.
6.
Mangione
CM,
Phillips
RS,
Lawrence
MG,
et
al.
Improved
visual
function
and
attenuation
of
declines
in
health-related
quality
of
life
after
cataract
extraction.
Arch
Ophthalmol
1994;112:1419-1425.
464

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
7.
Mangione
CM,
Berrv
S,
Spritzer
K,
et
al.
Identifying
the
content
area
for
the
51-item
National
Eye
Institute
Visual
Function
Questionnaire:
Results
from
focus
groups
with
visually
impaired
persons.
Arch
Ophthalnwl
1998;116:227-233.
8.
Steinberg
EP,
Tielsch
J,
Schein
OD,
et
al.
The
VF-14.
An
index
of
functional
impairment
in
patients
with
cataracts.
Arch
Ophthalniwl
1994;
112:630-638.
9.
Mangione
CM,
Phillips
RS,
Seddon
JM,
et
al.
Development
of
the
Activities
of
Daily
Vision
Scale:
A
measure
of
visual
functional
sta-
tus.
Med
Care
1992;30:1111-1126.
10.
Boisjoly
H,
Gresset
J,
Fontaine
N,
et
al.
The
VrF-14
index
of
func-
tional
visual
impairment
in
candidates
for
a
cornea
graft.
Am
J
Ophthalmol
1999;128:33-44.
11.
Linder
M,
Chang
TS,
Scott
IU,
et
al.
Validity
of
the
Visual
Function
Index
(VF-14)
in
patients
w\ith
retinal
disease.
Arch
Ophthalmol
1999;1
17:1611-1616.
12.
Mangione
CM,
Gutierrez
PR,
Lowe
G,
et
al.
Influence
of
age-
related
maculopathy
on
visual
function
and
health-related
quality
of
life.
AmJ
Ophthalmol
1999;128:45-33.
13.
DeVellis
RF.
Scale
Development:
Theory
and
Applications.
Newbury
Park,
London,
New
Delhi:
SAGE
Publications,
Inc;
1991.
14.
Stewart
AL,
WVare
JE
Jr,
eds.
Measuring
Functiotning
and
WVell-
Being.
The
Medical
Outcomes
Study
Approach.
Durham,
NC:
Duke
University
Press;
1992.
15.
Guyatt
G,
XValter
S,
Norman
G.
Measuring
change
over
time:
Assessing
the
usefulness
of
evaluative
instruments.
J
Chronic
Dis
1989;40:171-178.
16.
Deyo
RA,
Diehr
P,
Patrick
DL.
Reproducibility
and
responsive-
ness
of
health
status
measures:
Statistics
and
strategies
for
evalua-
tion.
Conitrol
Clin
Trials
1991;12:142S-158S.
17.
Kazis
LE,
Anderson
JJ,
Meenan
RF.
Effect
sizes
for
interpreting
changes
in
health
status.
Med
Care
1989;27:S178-S189.
18.
Bernth-Petersen
P
Visual
functioning
in
cataract
patients.
Methods
of
measuring
and
results.
Acta
Ophthalnwl
1981;59:198-205.
19.
Bernth-Petersen
P
Outcome
of
cataract
surgery.
I.
A
prospective,
observational
study.
Acta
Ophthalmol
1982;60:235-242.
20.
Bernth-Petersen
P.
Outcome
of
cataract
surgery.
II.
Visual
func-
tioning
in
aphakic
patients.
Acta
Ophthalnol
1982;60:243-251.
21.
Bernth-Petersen
P
Cataract
surgery.
Outcome
assessments
and
epidemiologic
aspects.
Acta
Ophthalmtiol
1985;Suppl
174:9-47.
22.
Bernth-Petersen
P.
Outcome
of
cataract
surgery.
IV
Socio-eco-
nomic
aspects.
Acta
Ophthalrmol
1982;60:461-468.
23.
Brenner
MH,
Curbow
B,
Javitt
JC,
et
al.
Vision
change
and
quali-
ty
of
life
in
the
elderly.
Response
to
cataract
surgery
and
treatment
of
other
chronic
ocular
conditions.
Arch
Ophthalmol
1993;111:680-685.
24.
Mangione
CM,
Orav
EJ,
Lawrence
MG,
et
al.
Prediction
of
visual
function
after
cataract
surgery.
A
prospectively
validated
model.
Archi
Ophthalmnol
1995;113:1305-1311.
25.
Javitt
JC,
Steinberg
EP,
Sharkey
P,
et
al.
Cataract
surgery
in
one
eve
or
both.
A
billion
dollar
per
year
issue.
Ophthalmnology
1995;102:1583-1593.
26.
Gresset
J,
Boisjoly
H,
Nguyen TQ,
et
al.
Validation
of
French-lan-
guage
versions
of
the
Visual
Functioning
Index
(VF-14)
and
the
Cataract
Symptom
Score.
Can
J
Ophthalnml
1997;32:31-37.
27.
Alonso
J,
Espallargues
M,
Andersen
TF,
et
al.
International
appli-
cability
of
the
VF-14.
Ophthalmology
1997;104:799-807.
28.
Uusitalo
RJ,
Brans
T,
Pessi
T,
et
al.
Evaluating
cataract
surgery
gains
by
assessing
patients'
quality
of
life
using
the
VF-7.
J
Cataract
Refract
Surg
1999;25:989-994.
29.
Musch
DC,
Farjo
AA,
Meyer
RF,
et
al.
Assessmnent
of
health-relat-
ed
quality
of
life
after
corneal
transplantation.
Anm
J
Ophthalmol
1997;124:1-8.
30.
Lundstroim
M,
Roos
P,
Jensen
S,
et
al.
Catquest
questionnaire
for
use
in
cataract
surgery
care:
Description,
validity,
and
reliability.
J
Cataract
Refract
Surg
1997;23:1226-1236.
31.
Fletcher
A,
Ellwein
LB,
Selvaraj
S,
et
al.
Measurements
of
vision
function
and
quality
of
life
in
patients
with
cataracts
in
southern
India.
Report
of
instrument
development.
Arch
Ophthalmol
1997;115:767-774.
32.
Natchiar
GN,
Thulasiraj
RD,
Negrel
AD,
et
al.
The
Madurai
Intraocular
Lens
Study:
I.
A
randomized
clinical
trial
comparing
complications
and
vision
outcomes
of
intracapsular
cataract
extrac-
tion
and
extracapsular
cataract
extraction
with
posterior
chamber
intraocular
lens.
AmJ
Ophthalnwl
1998;125:1-13.
33.
Prajna
NV,
Chandrakanth
KS,
Kim
R,
et
al.
The
Madurai
Intraocular
Lens
Study:
II.
Clinical
outcomes.
Am
J
Ophthalmol
1998;125:14-25.
34.
Fletcher
A,
Vijaykumar
V,
Selvaraj
S,
et
al.
The
Madurai
Intraocular
Lens
Study:
III.
Visual
functioning
and
quiality
of
life
outcomes.
Am
J
Ophthalmol
1998;125:26-35.
35.
Bourque
LB,
Rubenstein
R,
Cosand
B,
et
al.
Psychosocial
charac-
teristics
of
candidates
for
the
prospective
evaluation
of
radial
kera-
totomy
(PERK)
study.
Arch
Ophthalmol
1984;102:1187-1192.
36.
Bourque
LB,
Cosand
BB,
Drews
C,
et
al.
Reported
satisfaction,
fluctuation
of
vision,
and
glare
among
patients
one
year
after
sur-
gery
in
the
Prospective
Evaluation
of
Radial
Keratotomy
(PERK)
Study.
Arch
Ophthalmiwl
1986;104:356-363.
37.
Bourque
LB,
Lynn
MJ,
Waring
GO
III,
et
al.
The
Prospective
Evaluation
of
Radial
Keratotomy
Study
Group.
Spectacle
and
con-
tact
lens
wearing
six
years
after
radial
keratotomy
in
the
Prospective
Evaluation
of
Radial
Keratotomy
Study.
Ophthalmwlogy
1994;100:421-431.
38.
Waring
GO
III,
Casebeer
JC,
Dru
RM.
One-year
results
of
a
prospective
multicenter
study of
the
Casebeer
system
of
refractive
keratotomy.
Casebeer
Chiron
Study
Group.
Ophthalmology
1996;103:1337-1347.
39.
Werblin
TP,
Krider
DW,
Stafford
GM.
Casebeer
System
for
refractive
keratotomy:
Patient
satisfaction.
J
Cataract
Refract
Surg
1997;23:407-412.
40.
Kahle
G,
Seiler
T,
Wollensak
J.
Report
on
psychosocial
findings
and
satisfaction
among
patients
1
year
after
excimer
laser
photore-
fractive
keratectomy.
Refract
Corneal
Surg
1992;8:286-289.
41.
Hamberg-Nystrom
H,
Tengroth
B,
Fagerholm
P,
et
al.
Patient
sat-
isfaction
following
photorefractive
keratectomy
for
myopia.
J
Refract
Sturg
1995;11(Suppl):229-233.
42.
Rushood
AA,
Nassim
HM,
Azeemuddin
T.
Patient
satisfaction
after
photorefractive
keratectomy
for
lowu
myopia
uising
the
visual
analogue
scale.
J
Refract
Surg
1997;13:S438-440.
43.
Hersh
PS,
Schwartz-Goldstein
BH.
Corneal
topography
of
Phase
III
excimer
laser
photorefractive
keratectomy.
Characterization
and
clinical
effects.
Summit
Photorefractive
Keratectomy
Topography
Study
Group.
Ophthalmtwlogy
1995;102:963-978.
44.
Schwartz-Goldstein
BH,
Hersh
PS.
Corneal
topography
of
Phase
III
excimer
laser
photorefractive
keratectomy.
Optical
zone
cen-
tration
analysis.
Summit
Photorefractive
Keratectom,y
Topography
Stuldy
Group.
Ophthalmlology
1995;102:951-962.
45.
Hersh
PS,
Shah
SI,
Geiger
D,
et
al.
Corneal
optical
irregularity
after
excimer
laser
photorefractive
keratectomy.
The
Summit
Photorefractive
Keratectomy
Topography
Study
Group.
J
Cataract
Refract
Surg
1996;22:197-204.
46.
Hersh
PS,
Shah
SI,
Holladay
JT.
Corneal
asphericity
following
excimer
laser
photorefrativ
e
keratectomy.
Summit
PRK
Topography
Study
Group.
Ophthalmttic
Surg
Lasers
1996;27(Suppl):
S421-428.
47.
Shah
SI,
Hersh
PS.
Photorefractive
keratectomy
for
myopia
with
a
6-mm
beam
diameter.
J
Refract
Surg
1996;12:341-346.
48.
Halliday
BL.
Refractive
and
visual
results
and
patient
satisfaction
after
excimer
laser
photorefractive
keratectomy
for
Inyopia.
Br
J
Ophthalmiwl
1995;79:881-887.
465

Schein
49.
Fichte
CM,
Bell
AM.
Ongoing
results
of
excimer
laser
photore-
fractive
keratectomy
for
myopia:
Stubjective
patienit
impressions.
J
Cataract
Refract
Surg
1994;20(Stippl):263-270.
50.
Gimbel
HV,
Van
\Vestenbrugge
JA,
Johnson
WH,
et
al.
V'isual,
refractive,
and
patient
satisfaction
results
follow7ing
bilateral
pho-
torefractive
keratectomy
for
myopia.
Refract
Cornieal
Snirg
1993;9(Suppl):S5-10.
51.
Gartr7y
DS,
Kerr
Muir
MG,
Marsball
J.
Excimer
laser
photorefrac-
tive
keratectomy.
18-montb
follow,-up.
Ophthlalmtiology
1992;99:1209-1219.
52.
Neumann
AC,
Osher
Rfl,
Fenzl
RE.
Radial
keratotomy:
A
collm-
prehensive
evaluiation.
Doc
Ophthaliniol
1984;56:275-301.
53.
Cowvden
JWV,
Bores
LD.
A
clinical
investigation
of
the
surgical
cor-
rection
of
myopia
by
the
method
of
Fyodorov.
Ophthalhtiology
1981;88:737-741.
54.
Powers
MK,
Meyerowvitz
BE,
Arrowsmith
PN,
et
al.
Psychosocial
findings
in
radial
keratotomy
patients
two
years
after
surgerv.
Ophthialmology
1984;91:
1193-1198.
55.
Duitt
S,
Steinert
RF,
Raizman
MB,
et
al.
One-year
results
of
excimer
laser
photorefractive
keratectomy
for
low
to
mn
oderate
myopia.
Arch
Ophthalmi0ol
1994;112:1427-1436.
56.
Pallikaris
I,
McDonald
MB,
Siganos
D,
et
al.
Tracker-assisted
pho-
torefractive
keratectomy
for
myopia
of
-1
to -6
diopters.
J
Refract
Sturg
1996;12:240-247.
57.
Hersh
PS,
Schein
OD,
Steinert
R,
Suimmit
Photorefractive
Keratectomy
Phase
III
Study
Group.
Characteristics
influencing
ouitcomes
of
excimer
laser
photorefractive
keratectomy.
Ophthalmtiology
1996;
103:1962-1969.
58.
Freitas
C,
Oliveiros
BM,
Marques
E,
et
al.
Effect
of
photorefrac-
tive
keratectomy
on
visual
functioning
and
quality
of
life.
J
Refract
Sturg
1995;11(SuIppl):S327-334.
59.
McGhee
CNM,
Orr
D,
Kidd
B,
et
al.
Psychological
aspects
of
excimer
laser
surgery
for
myopia:
Reasons
for
seeking
treatment
and
patient
satisfaction.
BrJ
Ophthalmol
1996;80:874-879.
60.
Stewlart
AL,
Hays
RD,
Ware
JE
Jr.
Methods
of
constructing
health
measures.
In:
Stewart
AL,
WVare
JE
Jr,
eds.
Measurinig
Ftu
nctioning
and
WVell-Being.
The
Medical
Outcomnes
Study
Approach.
Durham,
NC:
Duke
University
Press;
1992:
chap
5.
61.
WNaring
GO
III,
Carr
JD,
Stulting
RD,
et
al.
Prospective
random-
ized
comparison
of
simultaneous
and
sequential
bilateral
laser
in
situ
keratomileusis
for
the
correction
of
myopia.
Ophthalmtiology
1999;106:732-738.
62.
Stulting
RD,
Carr
JD,
Thompson
KP,
et
al.
Complications
of
laser
in
situi
keratomileusis
for
the
correction
of
myopia.
Ophthalmology
1999;106:13-20.
63.
Cohen
J.
Statistical
Potwer
Analysis
for
the
Behavioral
Sciences.
2nd
ed.
Hillsdale,
NJ:
Lawrence
Erlbaum
Associates;
1988.
64.
Froberg
DG,
Kane
RL.
Methodology
for
measuring
health-state
preferences:
II.
Scaling
methods.
J
Clin
Epilemiol
1989;42:459-471.
65.
Torrance
GCV,
Feeny
D.
Utilities
and
quality-adjusted
life
years.
Int
J
Technol
Asses
Health
Care
1989;5:559-575.
66.
Bass
EB,
Steiniberg
EP,
Pitt
HA,
et
al.
Comparison
of
the
rating
scale
and
standard
gamble
approaches
in
measturing
patient
pref-
erences
for
outcomes
of
gallstone
disease.
Med
Decis
Making
1994;14:307-314.
67
Hersh
PS,
Brint
SF,
Maloney
RK,
et
al.
Photorefractive
keratectomy
versus
laser
in
situ
keratomileusis
for
moderate
to
high
myopia:
A
randomized
prospective
study.
Ophthalnmology
1998;105:1512-1523.
APPENDIX
REFRACTIVE
STATUS
AND
VISION
PROFILE
1.
Center:
2.
Chart
Number:
3.
Patieitt
Name
(last,
first)
4.
Telephone
numbers:
-
(h)
-
-
(Xv)
5.
Date
(mitonth/day/year):
/
/
BACKGROUND
INFORMATION
Patient
Information
c.
About
equally,
glasses
and
contacts
(
3)
1.
Age
d.
Mostly
contacts,
sometimes
glasses
(
4)
years
e.
Only
contacts
(
5)
2.
Sex
(check
only
one)
4.
In
the
past
month,
did
you
wear
different
glasses
(or
Female
(
')
bifocals)
to
see
close
up?
Male
(
2)
(s
)
(,,,
2)
5.
If
you
wore
contacts
in
the
past
month,
were
they:
Glasses
and
Contact
Lens
Use
la.
Rigid
gas
permeable
(hard)
(
)
b.
Soft
lenses
(
2)
3.
In
the
past
month,
to
see
far
away,
I
wore:
C.
Disposable
lenses
(
3)
a.
Only
glasses
(
)
d.
Didn't
wear
in
the
past
month
(
4)
b.
Mostly
glasses,
sometimes
contacts
(
2)
466

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
6.
If
you
wore
contacts
in
the
past
month,
did
you
ever
wear
them
overnight
(re
)
(n
2)
We
are
interested
in
your
vision
during
the
past
month.
For
the
following
3
questions,
please
answer
by
writing
a
number
between
0
and
10,
where
0
means
completely
blind
and
10
means
per-
fect
vision:
8.
Rate
your
vision,
over
the
past
month,
with
glasses:
Have
not
worn
glasses
at
all
in
the
past
month
9.
Rate
your
vision
over
the
past
month
with
contact
lenses:
L
Dissatisfied
Neither
satisfied
nor
dissatisfied
Satisfied
Very
satisfied
(
2)
(
3)
(
4)
(
5)
15.
In
general,
during
the
past
month,
would
you
say
your
health
has
been
(check
only
1):
Excellent
Very
good
Good
Fair
Poor
(
l)
(
2)
(
3)
(
4)
(
5)
16.
How
concerned
about
your
health
have
you
been
during
the
past
1
month
(check
only
1):
Have
not
worn
contact
lenses
at
all
in
the
past
month
D
10.
Rate
your
vision,
over
the
past
month,
with
no
glasses
or
contact
lenses:
11.
During
the
past
month,
how
satisfied
have
you
been
with
your
abil-
ity
to
do
reading
and
near
work
(using
the
glasses
or
contact
lenses
you
ordinarily
use
for
reading,
if
you
did
(check
only
1):
Very
dissatisfied
Dissatisfied
Neither
satisfied
nor
dissatisfied
Satisfied
Very
satisfied
Not
applicable
(
l)
(
2)
(
3)
(
4)
(
5~)
(
6)
12.
During
the
past
month,
how
satisfied
have
you
been
with
your
current
vision
with
glasses
(check
only
1):
Very
dissatisfied
Dissatisfied
Neither
satisfied
nor
dissatisfied
Satisfied
Very
satisfied
Not
applicable
(did
not
wear
glasses
at
all
during
the
past
month).
(
1)
(
2)
(
3)
(
4)
(
5)
(
6)
0
(not
at
all
concerned)
1
2
3
4
5
6
7
8
9
10
Never
Rarely
Sometimes
Often
Always
18.
My
vision
is
a
concern
in
my
life
(check
only
1):
13.
During
the
past
month,
how
satisfied
have
you
been
with
your
current
vision
with
contact
lenses
(check
only
1):
Very
dissatisfied
(
l)
Dissatisfied
(
2)
Neither
satisfied
nor
dissatisfied
(
3)
Satisfied
(
4)
Very
satisfied
(
5)
Not
applicable
(did
not
wear
contact
lenses
at
all
(
6)
during
the
past
month).
14.
During
the
past
month,
how
satisfied
have
you
been
with
your
current
vision
WITHOUT
glasses
or
contact
lenses
(check
only
1):
Never
Rarely
Sometimes
Often
Always
19.
My
vision
holds
me
back
(check
only
1):
Never
Rarely
Sometimes
Often
Always
(
l)
(
2)
(
3)
(
4)
(
5)
(
6)
(
7)
(
8)
(
9)
(
10)
(
11)
Vision
Please
respond
to
the
questions
as
they
apply
to
you
over
the
past
month
17.
I
worry
about
my
vision
(check
only
1):
(
l)
(
2)
(
3)
(
4)
(
5)
(
1)
(
2)
(
3)
(
4)
(
5)
(
2)
(
3)
(
4)
(
5)
467
Very
dissatisfied
(
1)

20.
I
am
frustrated
with
my
vision
(check
only
1):
Never
Rarely
Sometimes
Often
Always
21.
My
vision
makes
me
less
self
sufficient
(check
only
1):
Never
Rarely
Sometimes
Often
Always
(
I)
(
2)
(
3)
(
4)
(
5)
(
2)
(
3)
(
4)
(
5)
22.
Because
of
my
vision,
there
are
things
I
am
afraid
to
do
(check
only
1):
Never
Rarely
Sometimes
Often
Always
(
I)
(
2)
(
3)
(
4)
(
5)
Shein
23.
I
could
accept
less
than
perfect
vision
if
I
didn't
need
glasses
or
contact
lenses
any
more
(check
only
1):
Strongly
disagree
(
l)
Disagree
(
2)
Neither
agree
nor
disagree
(
3)
Agree
(
4)
Strongly
agree
(
5)
Do
not
need
to
use
glasses
or
contact
lenses
to
get
(
6)
the
best
possible
vision
24.
As
long
as
I
could
see well
enough
to
drive
without
wearing
glass-
es
or
contact
lenses,
I
wouldn't
mind
having
vision
that
was
less
than
perfect
(check
only
1):
Strongly
disagree
Disagree
Neither
agree
nor
disagree
Agree
Strongly
agree
(
2)
(
3)
(
4)
(
5)
We
are
interested
in
whether
your
vision
caused
you
any
difficulty
with
some
common
activities
during
the
past
month.
The
following
questions
ask
seperately
about
difficulty
you
may
have
had
doing
the
activity
with
glasses,
with
contact
lenses,
and
with
no
correction
(neither
glasses
nor
contact
lenses).
Please
give
an
answerfor
all
3
types
of
correction
(there
is
a
choice
for
"not
applicable").
The
choices
for
answers
are:
0
Not
applicable
1
No
difficulty
at
all
2
A
little
difficulty
3
Moderate
difficulty
4
Severe
difficulty
5
So
much
difficulty
that
I
did
not
do
the
activity
with
this
type
of
correction
6
Never
did the
activity
for
other
reasons
(not
related
to
vision)
During
the
past
month,
how
much
difficulty
have
you
had
with
each
activity,
using
these
types
of
corrections?
With
Glasses
(circle
a
number)
With
Contacts
(circle
a
number)
With
No
Correction
(circle
a
number)
21.
WatchingTVormovies
0123456
0123456
0123456
22.
Playing
orworking
outside
0
1
2
3
4
5
6
0
1
2
3
4
5
6
0
1
2
3
4
5
6
23.
Taking
care
of
or
playing
with
children
0
1
2
3
4
5
6
0
1
2
3
4
5
6
0
1
2
3
4
5
6
24.
Seeingyouralarmclock
0123456
0123456
0123456
25.
Seeing
clearlywhen
you
wake
up
0
1
2
3
4
5
6
0
1
2
3
4
5
6
0
1
2
3
4
5
6
26.
Seeingaclockonthewall
0123456
0123456
0123456
27.
Doingyourjob
0123456
0123456
0123456
28.
Doing
sports/recreation
0
1
2
3
4
5
6
0
1
2
3
4
5
6
0
1
2
3
4
5
6
29.
Swimming
0123456
0123456
0123456
30.
Yoursociallife
0123456
0123456
0123456
31.
Readingandnearwork
0123456
0123456
0123456
32.
Drivingatnight
0123456
0123456
0123456
33.
Drivingwhenitisraining
0123456
0123456
0123456
34.
Drivingwhenthereisaglare
0123456
0123456
0123456
from
oncoming
headlights
We
are
interested
in
whether
you
experienced
certain
problems
with
your
eyes
or
vision
during
the
past
month.
468
Activity

The
Measurement
of
Patient-Reported
Outcomes
of
Refractive
Surgery
The
following
questions
ask
seperately
about
each
problem
for
glasses,
contact
lenses,
and
no
correction
(neither
glasses
nor
contact
lenses).
Please
give
an
answerfor
all
3
types
of
correction
(there
is
a
choicefor
"not
applicable").
The
choices
for
answers
are:
0
Not
applicable
1
No
trouble
at
all
2
A
little
trouble
3
Moderate
trouble
4
Severe
trouble
5
So
much
trouble
that
I
did
not
do
the
activity
with
this
type
of
correction
During
the
past
month,
how
bothered
have
you
been
by
each
of
the
following
things,
using
these
types
of
corrections?
With
Glasses
(circle
a
number)
With
Contacts
(circle
a
number)
With
No
Correction
(circle
a
number)
35.
Your
eyes
feeling
irritated
0
1
2
3
4
5
6
0
1
2
3 4
5
6
0
1
2
3
4
5 6
36.
Drafts
(from
heating
or
air-conditioning)
0
1
2 3 4
5 6
0
1
2
3
4
5
6
0
1
2
3
4
5 6
blowing
in
your
eyes
37.
Eyesbeingsensitivetolight
0123456
0123456
0123456
38.
Paininyoureyes
0123456
0123456
0123456
39.
Changesinyourvisionduringtheday
0123456
0123456
0123456
40.
Your
vision
being
cloudy
or
foggy
0
1
2
3
4
5 6
0
1
2 3
4
5
6
0
1
2
3
4 5
6
41.
Glare
(reflections
off
shiny
surfaces,
snow)
0
1
2 3 4
5 6
0
1 2
3
4
5
6
0
1
2
3
4
5
6
42.
Things
looldng
different
out
of
one
eye
0
1
2
3
4
5
6
0
1
2 3 4
5
6
0
1
2
3
4
5
6
versus
the
other
43.
Seeing
ahalo
aroundlights
0
1
2
3
4
5
6
0
12
3
4
5 6
0
12
3
4
5
6
44.
Seeingindimlight
0123456
0123456
0123456
45.
Yourdepthperception
0123456
0123456
0123456
46.
Things
appearing
distorted
0
1
2
3
4
5
6
0
1
2
3
4
5 6
0
1
2 3 4 5
6
47.
Judging
distance
when
going
up
or
0
1
2 3
4
5
6
0
1
2
3
4
5
6
0
1
2
3
4
5
6
down
steps
(stairs,
curbs)
The
next
set
of
questions
ask
about
problems
you
may
have
experienced
during
the
past
month
with
glasses
or
contact
lenses.
Please
give
an
answerfor
each
item
(there
is
a
choicefor
"not
applicable").
The
choices
for
answers
are:
0
Not
applicable
(did
not
use
this
type
of
correction
during
this
past
month)
1
No
trouble
at
all
with
this
problem
2
A
little
trouble
with
this
problem
3
Moderate
trouble
with
this
problem
4
Severe
trouble
with
this
problem
5
So
much
trouble
with
this
problem
I
have
not
used
this
type
of
correction
in
the
past
month
During
the
past
month,
how
bothered
have
you
been
with
each
of
the
following?
48.
Glasses
getting
dirty
or
scratched
49.
Glasses
getting
fogged
up
or
wet
50.
Contacts
popping
out/falling
out
of
your
eye
51.
Contacts
getting
caught
up
under
your
eyelid,
or
moving
around
in
your
eye
52.
The
sensation
of
having
contacts
in
your
eye
53.
Not
being
able
to
wear
contacts
as
long
as
you
need
to
54.
Losing
a
contact
lens
(circle
a
number)
0
1
2
3
4
5
0
1
2
3
4
5
0
1
2
3 4
5
0
1
2
3 4
5
0
1
2
3 4
5
0
1
2
3
4
5
END
OF
QUESTIONNAIRE
Thank
you
for
your
time.
Any
comments
or
questions?
469
Problem
Reprinted,
with
permission,
from
Refractive
Status
and
Vision
Profile,
copyright
Johns
Hopkins
University.
01998
