
Oregon’s Health Care
Workforce Needs
Assessment 2023
February 2023
Tao Li, MD, PhD
Jeff Luck, MBA, PhD
Veronica Irvin, PhD, MPH
Collin Peterson, MAT, ATC
Alexandra Kaiser, BS
Prepared for:
Oregon Health Authority
Oregon Health Policy Board
1
Table of Contents
Executive Summary............................................................................................................ 2
Findings and Recommendations .................................................................................... 2
Conclusions ..................................................................................................................... 4
Background ......................................................................................................................... 5
Investments in Workforce Development......................................................................... 8
Workforce Resiliency .................................................................................................... 17
Health Care Workforce Trends ........................................................................................ 25
Health Care Workforce Reporting Program Data ........................................................ 25
Areas of Unmet Health Care Need ............................................................................... 32
Impacts of COVID-19 ....................................................................................................... 35
Impacts of COVID-19 on Health Care Visits ................................................................ 35
Impacts of COVID-19 on the Health Care Workforce .................................................. 38
Telehealth during the COVID-19 pandemic ..................................................................... 43
The Health Care Workforce Going Forward .................................................................... 51
Traditional Health Workers ........................................................................................... 51
Health Care Interpreters ............................................................................................... 59
Nursing Workforce ........................................................................................................ 63
Primary Care Providers ................................................................................................. 71
Behavioral Health Providers ......................................................................................... 78
Oral Health Providers .................................................................................................... 85
Long-Term Care Workforce .......................................................................................... 92
Public Health Workforce ............................................................................................... 97
Conclusions/Recommendations .................................................................................... 104
Conclusion ................................................................................................................... 106
Acknowledgments .......................................................................................................... 108
List of Abbreviations ....................................................................................................... 110

2
Executive Summary
2023 Oregon Health Care Workforce Needs Assessment
Note—The full report may be found at: https://www.oregon.gov/oha/HPA/HP-
HCW/Documents/2023-Oregon-Health-Care-Workforce-Needs-Assessment.pdf
This biennial Health Care Workforce Needs Assessment informs Oregon’s efforts
to ensure culturally and linguistically responsive care for all.
House Bill 3261 (2017) directs the Oregon Health Policy Board (OHPB) and Oregon
Health Authority (OHA) to produce a biennial assessment of the health care workforce
needed to meet the needs of patients and communities throughout Oregon by February
1 of each odd-numbered year. Oregon’s goal of eliminating health inequities requires
the preparation, recruitment, and retention of a diverse workforce that can deliver
culturally and linguistically responsive health care. This is the fourth such report, which
provides insights into workforce needs in communities across Oregon as well as
general guidance on how to expand and diversify the health care workforce, including
distributing health care provider incentives.
Findings and Recommendations
The report synthesizes policy recommendations across all segments of Oregon’s health
care workforce, based on its review of health care workforce development investments,
workforce resiliency, trends and COVID-19 impacts, and specific workforces requiring
attention. The findings point to some priority recommendations that are provided below.
Improve the diversity of health care providers
Oregon must have a more diverse workforce to achieve the strategic goal of
eliminating health inequities. Key recommendations include:
• Increase investments in training, recruiting, and retaining health care workers
who can provide culturally and linguistically responsive care
• Reduce barriers to entry and advancement for people of color in the workforce
Improve the supply and distribution of the health care workforce
The COVID-19 pandemic exacerbated Oregon’s shortage of many types of health
care providers, especially in rural areas. Key recommendations include:
• Continue to fund financial incentives to increase opportunities for training and
education, such as those in the Health Care Provider Incentive Program
• Invest in workforce training through the public workforce system and allied health
educational partners

3
• Address other factors that influence workforce recruitment and retention—
especially in rural areas—such as housing cost and supply, economic
opportunities for partners/spouses, and quality of K-12 education
Enhance the resiliency and well-being of the health care workforce
Health care worker burnout exacerbates workforce shortages, quality of care,
health inequities, and health disparities. Addressing workforce wellness and
resiliency is essential and will require collective action to be effective. Key
recommendations include:
• Coordinate collective actions from public and private stakeholders, as well as
community partners, to cultivate a health system that supports health care
workers, including action to create trauma-informed, anti-racist workplaces
• Invest in assessment and research to inform evidence-based and practice-based
strategies to optimize health care workforce well-being
Expand training/education and career pathways for many segments of
the health care workforce
Expanding training is especially urgent for segments of Oregon’s workforce
where shortages are most acute, such as behavioral health and long-term care.
Education and clinical training opportunities should be expanded for all types of
health care providers. Key recommendations include:
• Ensure adequate numbers of faculty and clinical training placements for nurses
and other licensed professionals
• Establish and fund clear pathways for positions that do not have defined career
ladders based on licensure, including parallel training and work, with a
progression to increased pay and responsibility based on training and experience
Expand use of care delivery models that improve patient access and
promote workforce retention
Although Oregon has been a leader in transforming its health care delivery
system, innovative care models can be expanded to improve patients’ access to
care, promote culturally and linguistically appropriate care, and increase
workforce satisfaction. Key recommendations include:
• Expand telehealth, coupled with health care interpreters, to improve access to
culturally specific or linguistically appropriate services
• Continue to invest in the integration of physical, behavioral, and oral health
care delivery
4
Increase health care systems’ use of community-based health care
providers
Traditional health workers—including peer wellness specialists—and health care
interpreters come from and/or share common lived experiences with their local
communities. OHA should continue to reduce barriers to recruit and retain this
workforce. A key recommendation is:
• Find ways to increase compensation for many health professionals, in particular
traditional health workers—including peer wellness specialists—and health care
interpreters who are underpaid and are underrepresented in certain regions of
the state and among persons of color relative to Oregon’s population
Improve data collection to promote evidence-informed strategies and
diversify the health care workforce
Data collection must be improved to help improve the understanding of
challenges to the workforce. Key recommendations include:
• Ensure that standardized REALD (race, ethnicity, language, and disability) and
SOGI (sexual orientation and gender identity) data are collected for all Oregon
providers and patients
• Expand data collection to include more provider types that incorporate
community-defined evidence practices and improve consistency of data
collection over time
Conclusions
Workforce shortages and lack of diversity in many areas of the health care workforce
are a national problem experienced in Oregon, stemming from historic underinvestment,
current economic and social forces, and systemic racism. There are barriers to entry
and advancement for people of color in the health care workforce, and to receiving
culturally and linguistically responsive care for people experiencing health inequities. In
order to stabilize, expand, and diversify Oregon’s health care workforce so that it can
deliver culturally responsive, effective health care services to all:
• Some professions need increased compensation to attract new individuals and
increase retention
• Many professions with unclear career pathways need better, focused paths for
increasing skills, pay, and impact
• All professions need more support around resiliency and well-being
All the report’s recommendations warrant action by government and non-governmental
entities to ensure Oregon has the workforce it needs to deliver on the commitments of
optimal health for everyone and the elimination of health inequities.
5
Background
Why a Health Care Workforce Needs Assessment?
Oregon has long been working to transform its health care system to achieve health
equity, expand access to care, improve population health outcomes, and ensure a
financially sustainable and high-quality health care system. Thus, it is critical that
Oregon has the workforce needed to effectively deliver high-value care to patients
across the state.
House Bill 3261, passed in 2017, directs the Oregon Health Policy Board (OHPB) to
assess the health care workforce needed to meet the needs of patients and
communities throughout Oregon. The assessment must consider:
1. The workforce needed to address health disparities among medically
underserved populations in Oregon
2. The workforce needs that result from continued expansion of health insurance
coverage in Oregon
3. The need for health care providers in rural communities
The needs assessment informs the disposition of the Health Care Provider Incentive
Fund to improve the diversity and capacity of Oregon’s health care workforce.
This is the fourth report Oregon Health Authority (OHA) has published in accordance
with House Bill 3261. (The legislation required an initial needs assessment report in
2018 and then biennial reports starting in 2019.) As stated in previous reports, it is not
feasible to determine the exact numbers of additional health care workers needed, or
the ideal ratios of health care providers required in each Oregon community to serve the
population’s health care needs. However, these reports can provide insights into the
workforce needs in communities across Oregon, identify needed provider types, and
provide general guidance for distributing health care provider incentives.
Current Context: Health Equity
OHA set an ambitious 10-year strategic goal of eliminating health inequities in the state.
Going forward, an increased focus on equity is needed to ensure that all people in
Oregon can reach their full health potential and well-being. The Health Care Workforce
Committee of the OHPB developed the Health Equity Framework to guide its efforts to
center equity in discussions and decision-making. It is grounded in the Health Equity
Definition adopted by OHPB (Figure 1.1), and OHA’s commitment to anti-racism.

6
Figure 1.1. OHA/OHPB Health Equity definition, updated October 2020
The Healthier Together Oregon: 2020–2024 State Health Improvement Plan, launched
in September 2020, focuses on the following vision:
Oregon will be a place where health and well-being are achieved across the
lifespan for people of all races, ethnicities, disabilities, genders, sexual
orientations, socioeconomic status, nationalities, and geographic locations.
The goals of the State Health Improvement Plan include:
• Implement standards for workforce development that address bias and improve
delivery of equitable, trauma-informed, and culturally and linguistically responsive
services
• Create a behavioral health workforce that is culturally and linguistically reflective
of the communities served
• Ensure cultural responsiveness among health care providers through increased
training and collaboration with Traditional Health Workers
• Require sexual orientation and gender identity training for all health and social
service providers
• Support alternative health care delivery models in rural areas
This focus on equity must include the training, recruitment, and retention of a diverse
workforce that can deliver culturally and linguistically appropriate care. The Oregon
Primary Care Office (PCO) “administers health care workforce recruitment and retention
programs that target federal and state resources to improve care delivery in
communities experiencing inequities, and coordinates with other organizations to
maximize collective impact statewide.”
Oregon will have established a health system that creates health equity when all
people can reach their full health potential and well-being and are not disadvantaged
by their race, ethnicity, language, disability, age, gender, gender identity, sexual
orientation, social class, intersections among these communities or identities, or
other socially determined circumstances.
Achieving health equity requires the ongoing collaboration of all regions and sectors
of the state, including tribal governments to address:
• The equitable distribution or redistributing of resources and power; and
• Recognizing, reconciling, and rectifying historical and contemporary
injustices.

7
Development of the Framework was informed by community input, which included
recommendations to increase the diversity of the health care workforce, and to make
the workplace more welcoming for diverse providers in the areas of:
• Pipeline and career pathways development
• Education, training, and credentialing
• Recruitment, hiring, and retention
• Compensation
• Culturally responsive services and practices environments
• Structure of health care provider incentives
Input from the community engagement was used to develop a set of questions to help
guide discussion and decisions to ensure that Oregon’s health care workforce
development efforts advance opportunities for communities experiencing inequities
(Figure 1.2). The Committee will use these questions in its work moving forward to
reimagine the necessary changes to infuse equity into workforce development policies
and programs that meet OHA’s 10-year goal to eliminate health inequities.
Figure 1.2. Health Care Workforce Committee guiding questions for Equity
Framework
How do Oregon’s health care workforce development efforts advance
opportunities for communities experiencing health inequities?
1. Who are the racial/ethnic communities and communities that are experiencing
health inequities? What is the potential impact of the resource allocation to these
communities?
2. Do the PCO programs ignore or worsen existing health inequities or produce
unintended consequences? What is the impact of intentionally recognizing the
health inequity and making investments to improve it?
3. How have we intentionally involved community representatives affected by the
resource allocation? How do we validate our assessment in questions 1 and 2?
How do we align and leverage public and private resources to maximize impact?
4. How should we modify or enhance strategies to ensure recipient and community
needs are met?
5. How are we collecting REALD and SOGI data (race/ethnicity, language, and
disability and sexual orientation and gender identity data) in PCO awards and
matching recipient demographics with communities served?
6. How are we resourcing and/or influencing system partners to ensure programs
optimize equity?

8
Current Context: COVID-19
The COVID-19 pandemic has resulted in significant changes to the health care system
and workforce needs. The disruption from the COVID-19 pandemic, and the response
and recovery, provide an opportunity for further health care transformation going
forward. This report analyzes trends from data collected before and during the COVID-
19 pandemic and then describes impacts of the COVID-19 pandemic on Oregon’s
health care workforce.
Investments in Workforce Development
Oregon Workforce Investments
In addition to national efforts, Oregon has made concerted efforts to invest in the
expansion, retention, and diversity of the health care workforce using multiple
strategies. Several programs have been introduced to achieve these goals across a
variety of health care professions.
Health Care Provider Incentive Program
In 2017, the passage of House Bill 3261 established the Health Care Provider Incentive
program (HCPIP) and the Health Care Provider Incentive Fund with the intent of
building health care workforce capacity in rural and medically underserved parts of
Oregon and pooling existing incentive programs into one flexible program. Table 2.1
details the allocation for each incentive for the current biennium. Implementation is
directed by the Oregon Health Policy Board (OHPB) and administered by Oregon
Health Authority (OHA) in collaboration with the Oregon Office of Rural Health. Since
the publication of the last report, additional flexibility for awardees to practice via
telehealth has been approved, significant funding has been made available to the
behavioral health workforce, and there has been an increased focus on how incentives
can better address inequities. HCPIP collected race, ethnicity, and language data for
several incentives using the federal Office of Management and Budget race and
ethnicity categories.
Additionally, two other incentive programs separate from HCPIP are reviewed: Healthy
Oregon Workforce Training Opportunity Grant Program and Rural Medical Practitioner
Tax Credit Program

9
Table 2.1. Incentive Allocation for the 2021-2023 Biennium.
Source: Health Care Provider Incentive Program: Allocation Request, 2022, Oregon Health Authority
*$3 million carried over from the previous biennium
Primary Care Loan Forgiveness
Loan Forgiveness is an incentive for students to receive funding during their education
in exchange for a future service obligation in an underserved rural community that
qualifies as a Health Professional Shortage Area and serves the same percentage of
Medicaid and Medicare patients that exist in the county in which the clinic is located.
Students may receive a loan equal to the cost of their post-graduate training for each
year they choose to practice in a qualified Health Professional Shortage Area for up to
three years. Eligible providers include certain specialties of Physicians, Physician
Assistants, Dentists, Pharmacists, and Nurse Practitioners.
Over the past 5 annual award cycles, 51 students have been awarded $2.6 million
through the Loan Forgiveness incentive. Table 2.2 details the programs and the
average amount of funding received from 2018 to 2022. The number of students who
have applied for the Loan Forgiveness incentive has exceeded the awards that can be
made with available funds.
Incentive
2019-2021 expenditure
2021-2023 allocation
Loan repayment to
primary care, oral health,
and behavioral health
clinicians
$6.5 million
$8.7 million*
Loan forgiveness for
primary care clinicians in
training
$1.0 million
$1.5 million
Rural medical malpractice
insurance subsidies
$2.9 million
$4.0 million
Scholars for a Healthy
Oregon Initiative (SHOI) at
OHSU
$5.0 million
$5.0 million
“SHOI-like” scholarships
at non-OHSU education
institutions
$0.7 million
$2.0 million
Administrative costs
$1.1 million
$1.3 million
Totals
$17.3 million
$22.5 million

10
Table 2.2. Primary Care Loan Forgiveness awards, 2018-2022
School and Discipline
Average Award Amount Per Recipient
OHSU
School of Medicine / MD
$76,383
Physician Assistant / PA
$42,700
School of Nursing / DNP
$32,600
School of Dentistry / DMD
$52,200
School of Pharmacy / PharmD
$35,200
Subtotal
$51,043
Pacific University
Physician Assistant / PA
$35,000*
School of Pharmacy / PharmD
$35,200*
Subtotal
$42,065
Western University COMP-NW
Osteopathic Medicine / DO
$89,371
Overall Average
$52,255
*These numbers have been provided as medians rather than averages to prevent backward calculation to small
numbers.
Source: Evaluation of the Effectiveness of Health Care Provider Incentive Programs in Oregon, 2023, Oregon Health
Authority
Loan Repayment Program
The Loan Repayment Program was designed to help support underserved communities
in the recruitment and retention of health care providers. Providers receive funds to
repay student loan debt based on the balance owed upon joining the Loan Repayment
Program and must be practicing at a qualifying site. Qualifying sites must be in a Health
Professional Shortage Area, serve at a minimum the same percentage of Medicaid and
Medicare patients that exist in the county in which the clinic is located, and been
approved by the Oregon Office of Rural Health. Eligible providers include a range of
health care professionals across primary care, dental, and behavioral health.
From 2018 to 2022, the Loan Repayment Program has allocated more than $16.7
million in loan repayment to 295 clinicians in Oregon including dentists (DDS/DMD),
dental hygienists, physicians (MD/DO), physician assistants, naturopathic doctors,
nurse practitioners, pharmacists, licensed social workers, and several different
behavioral health providers. HCPIP transitioned behavioral health loan repayment in
11
April 2022 to the new incentives available for behavioral health workforce incentives.
(See the Behavioral Health Providers section).
Figure 2.3 shows the distribution of loan repayment recipients across Oregon. A third of
loan repayment recipients have language skills in addition to English, about the same
as the previous report. Over 34% of incentive recipients identified as a person of color
or from Tribal communities, a notable increase from the 27% in the previous evaluation.
In a survey of awardees, over 90% reported satisfaction with the loan repayment
program, highlighting the mental and financial relief it brings as well as the opportunity
to work with underserved populations:
“It has freed me up to do what I love - helping underserved populations with my dental
skills and not drown in student loan debt.” – Oral Health Professional, Urban
“It has made it easier for me to focus on serving the underserved rural populations
without having to worry about my loan repayments.” – Primary Care Professional, Rural

12
Figure 2.3. Loan Repayment Program recipients across Oregon, 2018-2022
Source: Evaluation of the Effectiveness of Health Care Provider Incentive Programs in Oregon, 2023, Oregon Health
Authority
Rural Medical Insurance Subsidy
OHA provides subsidies for provider malpractice insurance premiums for physicians
and nurse practitioners serving in rural areas of Oregon that they would otherwise pay
in full. Reimbursement varies by specialty with providers in obstetric care receiving the
highest reimbursement at 80% of the cost. Family or general practice providers that
offer obstetrical services can receive 60% reimbursement. Providers in anesthesiology,
family practice, general practice, general surgery, geriatrics, internal medicine,
pediatrics, and pulmonary medicine can receive 40% reimbursement. Providers of other
practices not previously listed can receive up to 15% reimbursement. In 2021, 516
recipients received an insurance subsidy. Table 2.4 shows the number of participants
the previous 4 years.

13
Table 2.4. Rural Medical Insurance Subsidy Program Participants
Year
Number of Participants
2018
628
2019
546
2020
491
2021
516
Source: Evaluation of the Effectiveness of Health Care Provider Incentive Programs in Oregon, 2023, Oregon Health
Authority
Scholarships and Scholars for a Healthy Oregon Initiative (SHOI)
SHOI provides full tuition for Oregon Health & Science University (OSHU) students that
agree to practice as a health care provider in a rural or underserved community in
Oregon upon graduation using the Health Care Provider Incentive Fund. “SHOI-like”
programs were later established in the 2019-2021 biennium as a part of the Health Care
Provider Incentive Program at other Oregon universities. Table 2.5 shows the average
amount awarded for “SHOI-like” scholarships. Eligible providers include doctors,
dentists, physician assistants, and nurse practitioners. SHOI awardees must agree to
practice in an underserved Oregon community for a minimum of one year longer than
the total years SHOI funding was received. SHOI awardees can practice at a Federally
Qualified Health Center, a correctional facility, a community mental health clinic, urban
non-profit facility seeing at least 50% Medicaid patients in a health professional
shortage area, rural hospitals or clinics, rural Veterans Affairs facilities, and rural tribal
clinics.
Table 2.5. SHOI-like programs and average awards, 2019-2022
Program
Profession
Average
Award
National University of Natural Medicine
Naturopathic Doctor
$63,785
Pacific University School of Physician
Assistant Studies
Physician Assistant
$75,000
Western University – College of
Osteopathic Medicine of the Pacific
Northwest
Doctor of
Osteopathic Medicine
$117,600
Overall
$84,107
Source: Evaluation of the Effectiveness of Health Care Provider Incentive Programs in Oregon, 2023, Oregon Health
Authority

14
Funding for SHOI is $5 million for the 2021-2023 biennium. Since HCPIP’s inception,
close to $7 million has been distributed to 55 OHSU students in SHOI scholarships from
2019 to 2021. Over one-third of recipients are nurse practitioner students, 25% are
dental students, 24% are physician assistant students, and 15% are medical doctor
students.
Healthy Oregon Workforce Training Opportunity Grant Program (HOWTO)
The Healthy Oregon Workforce Training Opportunity (HOWTO) Grant Program seeks to
expand health professional training within the state to address shortages and expand
the diversity of the health care workforce. Under the direction of the OHPB, the HOWTO
Grant Program supports locally developed health care workforce programs using
innovative, community-based initiatives. Examples of recent HOWTO grantees include
a Peer Wellness Specialist training program in Portland and workplace learning
programs aimed at providing medical, dental, and behavioral workers to the Latino/a/x
Community in Medford; 345 new workers have been trained across a variety of health
care disciplines. Funding for the HOWTO Grant Program has increased over the years
from $8.4 million in the 2017-2019 biennium to $10.6 million in the 2021-2023 biennium.
Rural Medical Practitioner Tax Credit Program
Rural practitioner tax credits are also available to providers for practicing in areas that
meet the requirements of a designated rural area and whose individual adjusted gross
income does not exceed $300,000. Certified registered nurse anesthetists, dentists,
doctors of medicine (MD), doctors of osteopathic medicine (DO), nurse practitioners,
optometrists, physician assistants, and podiatrists are eligible for participation. Tax
credit amounts are tiered based on distance from city centers with a population of more
than 40,000 people. Providers at practices 10-20 miles away from an urban center
receive $3,000, 20-50 miles away receive $4,000, and 50+ miles away receive $5,000.
A separate rural tax credit is also offered to emergency medical services providers who
serve in rural areas. Table 2.6 shows the number of recipients of the rural medical tax
credit over the previous 4 years.
Table 2.6. Participants in the Rural Medical Tax Credit Program
Year
Number of Participants
2018
2,347 participants
2019
2,265 participants
2020
2,215 participants
2021
1,892 participants
Source: Evaluation of the Effectiveness of Health Care Provider Incentive Programs in Oregon, 2023, Oregon Health
Authority

15
Other Oregon Workforce Investment Programs
Behavioral Health Investment
There are several investments to address behavioral health workforce shortages and
improve diversity in Oregon. House Bill 2949 (2021) and subsequently House Bill 4071
(2022) created the Behavioral Health Workforce Initiative (BHWi) and allocated $80
million to provide incentives to increase the recruitment and retention of providers in the
behavioral health care workforce with a focus on equity and priority populations. House
Bill 4004 (2022) further requires OHA to distribute $132 million in grants to agencies to
be used to increase wages and other compensation for behavioral health practitioners.
There are additional investments at the national and state level to increase
compensation and provide incentives for behavioral health workers. Refer to the
Behavioral Health Providers section for more details.
Public Health Investments
Funding for Public Health Modernization from the Oregon Legislature has increased
from $5 million in 2017 to $30 million in 2021. OHA has requested $286 million for the
2023-2025 biennium for Public Health Modernization which will include workforce
development and retention strategies. OHA Public Health Division has also applied for a
$32 million CDC public health infrastructure grant, with some funding focused on
workforce development. OHA has also contracted out for work such as with universities
to train students to perform activities like case investigation, contact training, data entry
and quality assurance, and vaccine outreach. Refer to the Public Health Workforce
section for more details.
Future Ready Oregon
Future Ready Oregon is a $200 million investment package established under Senate
Bill 1545 (2022) aimed at supporting the education and training of Oregonians in need
of family-wage careers. The Higher Education Coordinating Commission primarily
oversees administering funds and has established different grants to support
recruitment, retention, and career advancement opportunities especially in
manufacturing, technology, and health care industry sectors for historically underserved
communities. As of September 19, 2022, the Higher Education Coordinating
Commission had received 146 applications and is in the process of evaluation for the
Future Ready Oregon Workforce Ready Grants. Seventy-six percent of the applications
were from the health care sector. $9.8 million is to be distributed through the first round
of grant applications.
Oregon Health & Science University (OHSU) 30-30-30 Plan
Oregon Health & Science University’s 30-30-30 plan was developed to address health
care workforce shortages and health care inequities that have worsened during the

16
COVID-19 pandemic and have disproportionately affected underserved communities.
OHSU 30-30-30 goal is to increase graduates from OHSU health care programs by
30% and increase student diversity within these programs by 30% by 2030. Under
House Bill 5202, the Oregon Legislature invested $45 million in OHSU 30-30-30. $20
million will be allocated to OHSU to expand current class sizes for health care
professional programs and increase diversity through existing learner programs like
Oregon Consortium of Nursing Education, Area Health Education Centers,
HealthESteps, Wy’east, and OnTrack OHSU!. Another $25 million will go towards the
OHSU Opportunity Fund to provide tuition assistance, loan repayment, and other
student resources to help with recruitment and retainment of more diverse student
bodies at OHSU. Through philanthropy, the OHSU Foundation will seek to match this
investment in its OHSU Opportunity Fund.
National Workforce Investments
National Health Services Corps Program
The National Health Services Corps program is a federal program administered by the
Health Resources and Services Administration. Students and health care providers can
receive scholarships and loan repayments for providing services in federally designated
Health Professional Shortage Areas. Student recipients of National Health Services
Corps scholarships must serve a minimum of 2 years at an approved site within an
Health Professional Shortage Area and be enrolled in an accredited program for
physicians, dentists, nurse practitioners, nurse midwives, or physician assistants. The
National Health Services Corps Loan Repayment Program offers several different loan
repayment opportunities for a variety of health care providers. Recipients can receive
anywhere between $25,000 to $100,000 in loan repayment funds depending on the
health care discipline and amount of service commitment years. Primary care providers,
dental providers, and behavioral health providers working at an approved site in a
Health Professional Shortage Area are eligible for loan repayment. The Health
Resources and Services Administration also provides grant funding to states to conduct
their own loan repayment programs based on state needs. Oregon has received over
$1.4 million in State Loan Repayment Program funds over the last 3 years.
Physician Visa Waiver Program
The Physician Visa Waiver Program (also called the J-1 Visa Waiver Program) is a
federal program that allows international medical students that completed residencies or
fellowships in the United States to stay in the country to practice medicine in an Health
Professional Shortage Area or other medically underserved area. OHA’s Primary Care
Office coordinates the program in Oregon and has state-specific requirements that a
minimum of 40% of all patient visits must be Medicaid, Medicare, and low-income
uninsured patients. The Primary Care Office gives preference to applicants who work as

17
primary care providers, work in rural areas, work in federally qualified health centers,
and work in a facility with a high Health Professional Shortage Area score. Ninety
percent of the physicians participating in the Oregon Physician Waiver Program who
started work three or more years ago completed their contractual obligations in Oregon.
Eighty-eight percent remained with their employer upon completion of their service
contract. All 30 positions were filled for 2022; typically, the program uses all available
slots each program year.
Workforce Resiliency
The Importance of Workforce Resiliency
Work stress refers to “the harmful physical and emotional effects when job requirements
do not match workers’ resources or needs”. It can lead to poor mental and physical
health and cause burnout. A range of socio-cultural and organizational factors can also
contribute to health care workforce burnout. The health care workforce is faced with a
high risk of work stress and burnout due to challenging working conditions such as
excessive workloads, long hours and unpredictable schedules, intense emotions, and
administrative burdens. The National Institute for Occupational Safety and Health
(NIOSH) found that health care workers are faced with stigma when seeking care for
mental health concerns or substance use disorders.
Burnout has been exacerbated by extreme mental and physical fatigue, isolation, and
moral and traumatic distress and injury during the COVID-19 pandemic. The health care
workforce experienced increased workload in the face of short staffing and shortages in
personal protective equipment (PPE). They experienced anxiety and fear of working
conditions with ongoing risk for hazardous exposures. The health care workforce also
experienced intensely stressful and emotional situations in caring for patients, many of
whom died. According to NIOSH, some health care workers reported symptoms
consistent with post-traumatic stress disorder related to the pandemic, and some
reported residual symptoms due to personal infection with COVID-19.
A recent survey of about 2,500 physicians found a dramatic increase in physician
burnout during the pandemic. Over 60% of physicians reported manifestations of
burnout in 2021 compared with 38% in 2020. Physician satisfaction with work-life
integration declined from 46% in 2020 to 30% in 2021.
18
In Oregon, data from the Larry Green Center survey of primary care showed that as of
November 2021, 39.3% of respondents reported their mental stress/exhaustion at an
all-time high. Over 70% of Oregon respondents reported that mental stress/exhaustion
in their practices at an all-time high, compared to around 60% at national level.
The Oregon Center for Nursing (OCN) recently conducted a statewide survey of well-
being and resiliency among nurses (Figure 3.1). Among more than 5,000 respondents,
83% of nurses reported stress, with the highest reports in long-term care, home
health/hospice, and hospital settings. Eighty percent of respondents felt frustration, and
over 60% reported anxiety, exhaustion, burnout, and being overwhelmed and
undervalued. Top work stressors included “heavy or increased workload,” “uncertainty
about when things will settle down,” and “burnout.” A national study surveyed more than
50,000 registered nurses and found that more than 30% of nurses who left their job
reported burnout as a reason. Nurses who worked more than 40 hours per week were
more likely to report burnout as a reason they left their job.

19
Figure 3.1. Nurses’ well-being survey by the Oregon Center for Nursing
Source: Oregon Center for Nursing. RN Well-Being Mental Health Survey, April 2020.
Governmental public health has also assessed state and local health worker burnout
since COVID-19. The public health workforce has operated under strained resources
even before the COVID-19 pandemic. The pandemic brought long work hours,

20
increased scrutiny from local elected officials and the public, and in some cases, threats
of violence against public health professionals and their families. Misinformation and
opposition to local public health guidance has led many to discredit public health
officials. These working conditions have led to job-related mental health impacts and an
exodus from the field for public health professionals. In Oregon, almost half of local
health administration roles experienced turnover. Turnover in administration and those
in supervisory roles may mean that remaining staff may have not been well-supported.
Health worker burnout can have many negative consequences. A study estimated the
national cost for burnout-related turnover at $17 billion for physicians and $14 billion for
nurses annually. In 2022, the U.S. Surgeon General’s Advisory on Building a Thriving
Health Workforce suggested that “health worker burnout harms all of us,” as “the health
worker burnout crisis will make it harder for patients to get care when they need it,
cause health costs to rise, hinder our ability to prepare for the next public health
emergency, and worsen health disparities.” It also highlighted groups of health workers
whose health and well-being have been disproportionately impacted before and during
the pandemic, including health workers of color, immigrant health workers, female
health workers, low wage health workers, health workers in rural communities, and
health workers in tribal communities.
Programs to Improve Workforce Resiliency
In 2017, the National Academy of Medicine launched the Action Collaborative on
Clinician Well-Being and Resilience, a network of more than 200 organizations
committed to reversing trends in clinician burnout. The goals of this collaborative include
raising the visibility of clinician anxiety, burnout, depression, stress, and suicide;
improving baseline understanding of challenges to clinician well-being, and advancing
evidence-based, multidisciplinary solutions to improve patient care by caring for the
caregiver.
In October 2022, the National Academy of Medicine Clinician Well-Being Collaborative
published a National Plan for Health Workforce Well-Being. The National Plan calls on
multiple actors – including health care and public health leaders, government, payers,
industry, educators, and leaders in other sectors - to “cultivate a health system to
support care providers and optimize their well-being.” To better support the health
workforce and the health of all communities, the National Plan highlighted seven
priorities, including:
• Create and sustain positive work and learning environments and culture.
• Invest in measurement, assessment, strategies, and research.
• Support mental health and reduce stigma.
• Address compliance, regulatory, and policy barriers for daily work.

21
• Engage effective technology tools.
• Institutionalize well-being as a long-term value.
• Recruit and retain a diverse and inclusive health workforce.
As the National Plan pointed out, these priorities are urgent and complex, as “no single
actor or sector can move the needle on its own.” It needs collective action by everyone
—from health workers to the public to multi-sectoral leaders— to strengthen health
workforce well-being.
The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce in 2022
called for collaboration from a variety of public and private stakeholders, including
federal, state, and local government and health care organizations, health insurers,
technology companies, training programs, and accrediting bodies, to tackle health care
worker burnout (Figure 3.2). Actions called for include:
• Protecting the health, safety, and well-being of all health workers
• Eliminating punitive policies for seeking mental health and substance use care
• Reducing administrative and other workplace burdens to help health workers
make time for what matters
• Transforming organizational cultures to prioritize health worker well-being and
show all health workers that they are valued
• Recognizing social connection and community as a core value of the health care
system
• Investing in public health and public health workforce.

22
Figure 3.2. Solutions to health worker burnout, from the U.S. Surgeon General’s
Advisory on Building a Thriving Health Workforce
Source: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce.
In 2021, the U.S. Department of Health and Human Services (HHS), through the Health
Resources and Services Administration (HRSA), allocated $103 million from the
American Rescue Plan to be spent over a three-year period to reduce burnout and to
promote mental health among the health workforce. Funding will be provided to health
care organizations to promote resilience and mental health among health professional
workforce, and for educational institutions and other appropriate entities training those

23
early in their health careers to promote resiliency within the workforce. Awards will also
be made to provide tailored training and technical assistance to HRSA's workforce
resiliency programs. In Oregon, Northeast Oregon Network and Legacy Emanuel
Hospital & Health Center both received over $2 million HRSA awards to support health
workforce resiliency.
The passage of the Dr. Lorna Breen Health Care Provider Protection Act (HR 1667) in
2022 established grants and requires activities to support the mental and behavioral
health of health workers. For example, it establishes grants for training health
professions students, residents, or health care professionals in evidence-informed
strategies to reduce and prevent suicide, burnout, mental health conditions, and
substance use disorders. The legislation also establishes a national evidence-based
education and awareness campaign targeting health care professionals to encourage
them to seek support and treatment for mental and behavioral health concerns.
The Oregon Wellness Program provides wellness support for physicians, nurses, and
other health care professionals in Oregon. The program promotes health care
professionals’ well-being through free counseling, education, and research. In 2021, the
OCN launched the RN Well-Being Project to aid workplaces in developing interventions
that nurses feel are necessary to improve their mental and emotional well-being. OCN
compiles resources to help nurses access care and build resilience. It is also working on
innovative solutions for employers to make systematic culture change to best support
their nurses.
The Oregon Health Authority (OHA) is taking the following steps to support behavioral
health providers (see the Behavioral Health Providers section):
• Childcare for workers: OHA provided $8 million to hundreds of licensed
behavioral health providers for childcare stipends. The stipends went directly to
staff, improved supervision, and working environment improvements.
• Retention and hiring bonuses: OHA provided $15 million to provide retention
and hiring bonuses of up to $2,000. The bonuses went to more than 7,000
workers serving clients directly in residential settings.
• Residential emergency staffing needs: OHA provided staff support to both
children’s and adults’ licensed behavioral health facilities to offset the impact of
COVID-19 on the workforce.
• Vacancy payments and rate increases: Vacancy payments are Medicaid-
reimbursed and are allowed for empty beds when the reason for the bed
vacancy is due to the pandemic. OHA has provided more than $30 million
vacancy payments to residential providers impacted by the pandemic and
helped provide stable income. OHA also implemented a temporary 10% rate

24
increase for residential behavioral health providers during COVID-19. Almost
$13 million has been paid directly to providers and to CCOs for providers.
• Reducing administrative burdens: OHA reduced administrative burdens on
behavioral health programs, pausing more than 40 reporting requirements.

25
Health Care Workforce Trends
Health Care Workforce Reporting Program Data
Methodology
Oregon was one of the first states in the country to legislatively mandate reporting by
health care professionals. Oregon Health Authority’s Health Care Workforce Reporting
Program was created in 2009 with the passage of House Bill 2009, which required
Oregon Health Authority (OHA) to collaborate with seven health profession licensing
boards to collect health care workforce data during their license renewal processes.
During the 2015 Oregon Legislative session, Senate Bill 230 added ten more health
licensing boards to this data collection program. Oregon’s 17 licensing boards
participating in this data collection are outlined in Table 4.1, with the 40 occupations that
they license. The data collected on these providers include information submitted to the
licensing boards and data from the Health Care Workforce Survey. This data is used to
understand Oregon’s health care workforce, inform public and private educational and
workforce investments, and provide data to inform policy recommendations for state
agencies and the Legislative Assembly regarding Oregon’s health care workforce.
Table 4.1. Oregon Health Care Licensing Boards
Licensing Board
Licenses
Oregon Medical Board
Doctor of Medicine (MD), Doctor of Osteopathy
(DO), Doctor of Podiatry (DPM), Licensed
Acupuncturist, Physician Assistant (PA)
Oregon Board of Dentistry
Dentist (DMD/DDS), Registered Dental Hygienist
(RDH)
Oregon Board of Optometry
Optometrists (OD)
Oregon Board of Naturopathic Medicine
Naturopathic Physician (ND)
Oregon State Board of Nursing
Registered Nurse (RN), Nurse Practitioner (NP),
Certified Registered Nurse Anesthetist (CRNA),
Clinical Nurse Specialist (CNS), Licensed
Practical Nurse (LPN), Certified Nursing Assistant
(CNA)
Oregon Board of Chiropractic Examiners
Chiropractic Examiners (DC),
Chiropractic Assistants (CA)
Oregon Occupational Therapy Licensing
Board
Occupational Therapist (OT),
Occupational Therapy Assistant (OTA)
Oregon Board of Physical Therapy
Physical Therapist (PT),
Physical Therapist Assistant (PTA)
Oregon Board of Massage Therapists
Licensed Massage Therapist (LMT)

26
Licensing Board
Licenses
Respiratory Therapist and
Polysomnographic Technologist
Licensing Board
Polysomnographic Technologists (LPSGT),
Respiratory Therapists (LRCP)
Oregon Board of Licensed Dieticians
Licensed Dietitian (LD)
Oregon Board of Psychology
Psychologist (PSY)
Oregon Board of Licensed Clinical Social
Workers
Licensed Clinical Social Worker (LCSW),
Clinical Social Worker Associate (CSWA)
Oregon Board of Licensed Professional
Counselors and Therapists
Licensed Marriage and Family Therapist (LMFT),
Licensed Professional Counselor (LPC)
Oregon Board of Pharmacy
Pharmacists (RPH),
Certified Pharmacy Technician (CPhT)
Oregon Board of Medical Imaging
Nuclear Medicine Technologist (NMT), MRI
Technologist (MRI), Radiation Therapist (RDT),
Radiographer (RDG), Sonographer (SNG),
Limited Permit X-ray Machine Operator (LXMO)
Oregon Board of Examiners for Speech-
Language Pathology and Audiology
Audiologist (AUD), Speech-Language
Pathologists (SLP), Speech-Language
Pathologists Assistants (SLPA)
Source: OHA Office of Health Analytics, Oregon’s Health Care Workforce Reporting Program
Findings
In total, there were nearly 192,000 licensed health care professionals in this reporting
program dataset as of January 2022. The direct patient care FTE by occupation and
year from 2016-2022 is shown in Figure 4.2, along with the annual average percent
change in that time period. Noteworthy average annual increases were observed for
counselors and therapists (13.5%), clinical social work associates (9.4%), nurse
practitioners (8.1%), physician assistants (8.1%), and licensed dietitians (7.8%).

27
Figure 4.2. Average annual percent change in direct patient care FTE varies by
occupation.
Source: OHA Office of Health Analytics, 2022 Oregon’s Licensed Health Care Workforce Supply.
Table 4.3 shows primary care provider FTE changes by occupation over years. Primary
care physician FTE decreased in 2022 compared to 2020, as did naturopathic
physicians. At the same time, nurse practitioners and physician assistants FTE
increased. Overall, there is a 2% increase in primary care provider FTE from 2020 to
2022.

28
Table 4.3 Primary care provider FTE changes by occupation
Occupation
2020
2022
Change
Physicians
4,716
4,638
- 1.7 %
Nurse practitioners
1,020
1,241
21.7%
Physician assistants
685
694
1.3%
Naturopathic Physicians
220
206
- 6.4%
TOTAL
6,641
6,779
2.1%
Source: OHA Office of Health Analytics, 2022 Oregon’s Licensed Health Care Workforce Supply.
Figure 4.4 shows health care professionals’ plans to increase hours, reduce hours, or
leave the workforce in 2021 and 2022. Clinical nurse specialists (7.8 %) and certified
pharmacy technicians (6.5%) had the highest rates of plan to leave the Oregon
workforce. Those who intended to increase practice hours at the highest rates were
licensed massage therapists (14.7%) and occupational therapy assistants (12.5 %). See
The Health Care Workforce Going Forward section for more detail on provider specialty
groups.
30
Starting in 2021, the Health Care Workforce Reporting Program’s survey of providers
began using the REALD tool. REALD outlines how to collect data on race, ethnicity,
language, and disability with more granularity. The tool can be used to more accurately
identify inequities and subpopulations that may benefit from focused interventions, and
help address unique inequities that occur at the intersections of race, ethnicity,
language, and disability.
The gender and race/ethnicity breakdown for health care provider compared with
Oregon’s general population is shown in Table 4.5. Female providers are
overrepresented in most professions, though men tend to be overrepresented in fields
requiring more years of formal training, such as physicians and dentists. Latino/a/x
providers are underrepresented in most health care professions. See The Health Care
Workforce Going Forward section for more detail on provider specialty groups.

32
As shown in Figure 4.6, Spanish is the most common language spoken other than
English among licensed providers (about 10%). The next most common languages
spoken are Chinese (including Mandarin and Cantonese), Tagalog, Vietnamese,
French, and Russian. Less than 1% of the licensed health care providers are native
speakers or have advanced proficiency in each of those languages. Thus, many
patients who speak a language other than English need the assistance of a Health Care
Interpreter (see the Health Care Interpreters section).
Figure 4.6. Top Languages Spoken by the Workforce: Workforce Stratified by
Proficiency, Compared to Oregon Population
Source: OHA Office of Health Analytics, Oregon’s Health Care Workforce Reporting Program
Areas of Unmet Health Care Need
Methodology
The Oregon Office of Rural Health at Oregon Health & Science University (OHSU)
produces a report annually on Oregon Areas of Unmet Health Care Need, presenting
community-level data on access to care and health care workforce capacity. Nine
measures of access to primary physical, behavioral, and oral health care are included in
the report:
• Travel time to nearest Patient-Centered Primary Care Home
• Primary care capacity (percent of primary care visits able to be met)

33
• Dentist FTE per 1,000 population
• Licensed behavioral health provider FTE per 1,000 population
• Percent of population between 138% and 200% of the federal poverty level
• Inadequate prenatal care rate per 1,000 births
• Preventable hospitalizations per 1,000 population
• Emergency department non-traumatic dental visits per 1,000 population
• Emergency department mental health/substance abuse visits per 1,000
population
A composite score of unmet need is calculated from these measures, ranging from 0 to
90, with lower numbers indicating greater unmet need. Scores are calculated for each of
the 128 primary care service areas in the state. The Office of Rural Health defines
primary care service areas using zip code data, with at least 800 people in each service
area. Generally, service areas are defined considering topography, social and political
boundaries, and travel patterns, and health resources are located within 30 minutes
travel time in any given service area. For 2022, the unmet health care need scores by
service area ranged from 18 (worst) to 79 (best), with a statewide average of 49. (Figure
5.1). It is important to note that the Areas of Unmet Health Care Needs report does not
fully assess unmet health care needs by race/ethnicity in different parts of the state.
Equitable health care access is dependent on the diversity and language abilities of
providers, and the intersectionality of urban/rural geography and race/ethnicity is an
important consideration.

34
Figure 5.1. Unmet Health Care Needs Scores by Service Area
Source: The Oregon Office of Rural Health. The Oregon Area of Unmet Health Care Need report.
Table 5.2 shows scores for unmet need for 2022 by geographic area: urban, rural, and
frontier. Rural areas are defined as geographic areas that are ten or more miles from
the centroid of a population center of 40,000 people or more. Counties with six or fewer
people per square mile are defined as frontier. On average, rural and frontier areas
have more unmet health care need than urban areas in Oregon. See The Health Care
Workforce Going Forward section for more detail on provider specialty groups.
Table 5.2. Average Unmet Health Care Need Score by Geographic Area
Unmet Health Care Need Score
Lower numbers indicate more unmet need
Statewide-Oregon
49.4
Urban
62.1
Rural (not frontier)
45.9
Frontier
48.9
Source: The Oregon Office of Rural Health. The Oregon Area of Unmet Health Care Need report.

35
Impacts of COVID-19
Impacts of COVID-19 on Health Care Visits
Early in the pandemic, planning and preparing for the care of an unknown number of
anticipated COVID-19 patients consumed health care resources. Other initial impacts
on the health care system included a statewide ban on elective surgeries, people
choosing not to go to clinics in person because of concerns about being exposed to the
Coronavirus, and health care facilities changing operating practices (including
temporary closures). The impacts of COVID-19 on reduced health care visits were
greatest during the first months of the pandemic. The Larry Green Center, in partnership
with the Primary Care Collaborative, began conducting a weekly nationwide survey in
mid-March 2020 about the impacts of COVID-19 on primary care, and Oregon-specific
responses are available through the Oregon Rural Practice-based Research Network.
Data from the Larry Green Center showed that in April 2020, about 90% of respondents
in Oregon reported high or severe impacts of COVID-19 on their practice, and almost all
respondents indicated that their practice experienced a decline in patient volume.
As shown in Figure 6.1, by early April 2020, the number of outpatient visits nationally
decreased by more than half, according to an analysis of national data published by the
Commonwealth Fund. By October 2020 outpatient visits had returned to baseline levels.
Due to a COVID-19 surge during the last two months of 2020, outpatient visit volume
remained lower than the levels during winter months in prior years.

36
Figure 6.1. Outpatient visit trends in 2020
Change in U.S. Outpatient Visits Compared with Baseline Week of March 1, 2020
Source: Ateev Mehrotra et al., The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite
a Late Surge in Cases (Commonwealth Fund, Feb. 2021).
Data on hospitalizations in Oregon also showed sharp reductions in April 2020 (as
shown in Figure 6.2). Hospital inpatient discharges were down 34% in April 2020
compared with January 2020. In March 2022, there were about 26,700 inpatient
discharges statewide, which was close to the number in March 2021 and about 5%
higher compared with March 2020.

37
Figure 6.2. Inpatient discharges trend in Oregon, January 2020 - March 2022
Source: Oregon Health Authority Hospital Reporting Program (2022). Hospital Financial & Utilization Dashboard.
As shown in Figure 6.3, the reduction in hospital outpatient surgery visits was even
greater, with April 2020 being 76% lower than January 2020. With the third upsurge of
COVID-19 cases in the fall of 2020, hospitals were operating at closer to full capacity. In
March 2022, there were about 18,800 outpatient surgeries statewide, which was slightly
lower than March 2021 but was 54% higher compared with March 2020.
Figure 6.3. Outpatient surgeries trend in Oregon, January 2020 - March 2022
Source: Oregon Health Authority Hospital Reporting Program (2022). Hospital Financial & Utilization Dashboard.
Note: Outpatient surgeries include surgeries performed at the hospital that do not require an inpatient admission.
The 2021 Survey of Dental Practice by the American Dental Association showed that
due to the pandemic in early 2020, hours worked declined by about 17% and net

38
incomes declined by about 18% for general practitioners compared to 2019. Dental
specialists’ hours worked declined by about 12% and net incomes declined by about
7%. The COVID-19 Economic Impact on Dental Practices survey showed that as of
December 2021, about 47% of practices in Oregon were open but had lower patient
volume than usual.
Impacts of COVID-19 on the Health Care Workforce
The COVID-19 pandemic has had direct impacts on the health care workforce.
According to the Oregon Health Authority’s (OHA) COVID-19 Report, there had been
about 9,500 reported cases of COVID-19 among health care workers in 2020 and 9,900
cases in 2021. The pandemic exacerbated health care workforce burnout to an alarming
level (see the Workforce Resiliency section). The reductions in health care visits and
revenues also led to layoffs. The impacts of COVID-19 on reduced health care
employment were greatest during the first months of the pandemic.
States took a variety of actions to address health care workforce needs, including
recruiting additional health workers from within and out-of-state, modifying licensing
requirements to quickly build workforce capacity, and shifting existing staff to areas of
greater need. The state of Oregon paid for temporary staff when there were workforce
shortages in hospitals and long-term care facilities. Health care facilities greatly
increased their use of temporary staffing agencies, and the costs for temporary staff
increased dramatically. Rural communities that had long-standing problems of health
care workforce shortages were faced with exacerbating challenges during the
pandemic.
Current employment estimates from the Oregon Employment Department show a rapid
reversal of pandemic recession job losses. Within the health care sector, employment
trends varied (see Figure 7.1). Employment in ambulatory health care had bigger
declines in spring 2020, but also has had a stronger growth since then. The number of
people employed in ambulatory health care declined 17% from February to April 2020
but had rebounded to pre-pandemic levels by August 2020. Employment in ambulatory
health care in August 2022 increased by 5% compared to August 2021 and is 3%
higher than February 2020. There were slower but steadier declines in employment by
hospitals and nursing and residential care facilities. As of August 2022, the number of
people employed in hospitals and in nursing and residential care facilities were still
about 4% and 6% lower, respectively, compared to February 2020.

39
Figure 7.1. Employment trends varied within health care, January 2020 - August
2022
Source: Oregon Employment Department, Current Employment Statistics. (February 2020=100)
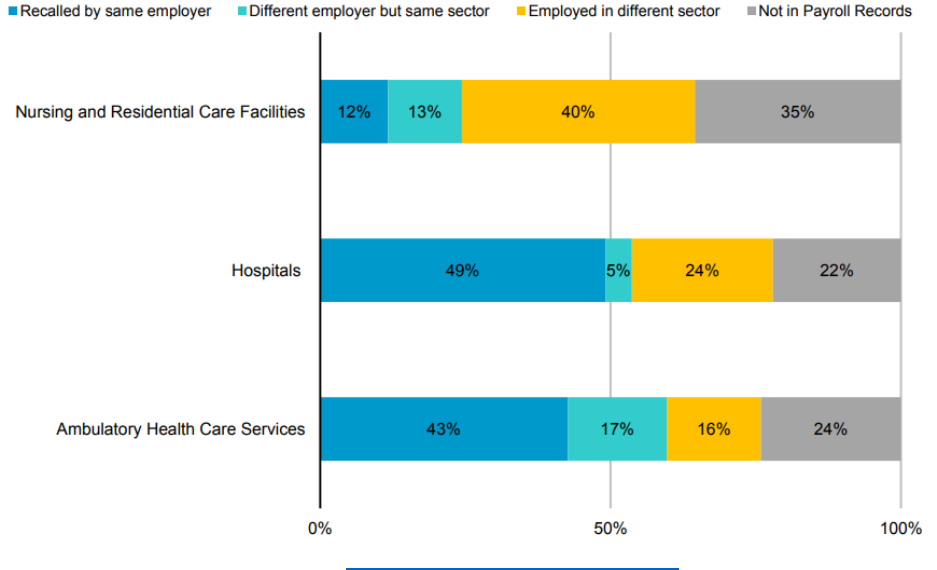
The lower employment in nursing and residential care facilities can be partly explained
by the re-employment trends reported by the Oregon Employment Department. It shows
that workers laid off from nursing and residential care facilities were far more likely to
switch sectors compared to other health care workers (Figure 7.2). Only about 25% of
former nursing and residential care workers still worked in the same sector as of winter
2022, as opposed to 54% of workers laid off from hospitals and more than 60% of
workers laid off from ambulatory care services.
75
80
85
90
95
100
105
Jan-2020
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan-2021
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Jan-2022
Feb
Mar
Apr
May
Jun
Jul
Aug
Ambulatory health care services Hospitals Nursing and residential care facilities
40
Figure 7.2. Re-employment patterns of health care workers with pandemic
unemployment claims in Oregon
Source: Oregon Employment Department, Health Care Workforce Trends in Oregon.
Figure 7.3 shows the number of monthly online health care job postings from January
2019 to September 2022 analyzed by the Oregon Employment Department. In May
2020, the number of monthly postings was about one-third lower than pre-pandemic
levels, and the number of job postings began to rebound by July 2020. There were
16,947 online health care job postings in September 2022, compared to 15,480 (a 9%
increase) in September 2021, 8,440 (a 100% increase) in September 2020, and 9,115
(an 86% increase) in September 2019. The changes in Help Wanted online postings
varied by region. Comparing September 2022 to September 2019, Clackamas and East
Cascades had more than a 110% increase in job postings, and Southwestern had only
a 21% increase.

41
Figure 7.3. Monthly online health care job postings in Oregon, January 2019 -
September 2022
Source: The Conference Board Help Wanted OnLine
TM
(HWOL), analysis by the Oregon Employment Department.
A September 2022 report on health care workforce trends in Oregon showed difficulty
filling health care vacancies, as health care occupations represented nearly 10% of job
vacancies in Oregon. About 70% of “difficult-to-fill” positions are full-time positions,
compared to 92% of “not-difficult-to-fill” positions. Education beyond high school is
required for 53% of “difficult-to-fill” positions and for 92% of “not-difficult-to-fill” positions.
A few employers in health care also reported that vaccination mandates made it harder
to fill positions, particularly in rural areas.
As many health care workers left the sector during the pandemic, hospitals competed
for contract workers to fill vacancies. A recent hospital workforce report showed that
contract labor as a percentage of total hours increased from 1% before the pandemic to
5% as of March 2022, while the contract labor as a percentage of total labor expenses
increased from 2% to 11%. Hospital labor expenses increased by more than 30% from
pre-pandemic levels. Compared to other regions, the West had the largest percentage
of using contract labor (6% of total paid hours) and the highest labor expenses (a
median of about $7,500 per adjusted discharge) as of March 2022.
4,000
6,000
8,000
10,000
12,000
14,000
16,000
18,000
20,000
Jan
2019
May
2019
Sept
2019
Jan
2020
May
2020
Sept
2020
Jan
2021
May
2021
Sept
2021
Jan
2022
May
2022
Sept
2022

42
The demand for travel nurses substantially increased as hospitalizations surged during
COVID-19 outbreaks. As COVID-19 hospitalization rates stabilized and hospitals’
financial challenges increased, demand for travel nurses dropped substantially in early
2022. There have also been state and federal moves toward regulations for staffing
agencies and limiting their pay rates. In Oregon, Senate Bill 1549 (2022) directs the
Oregon Health Authority to submit “A policy proposal and recommendations to establish
a process to determine annual rates that a temporary staffing agency may charge to or
receive from an entity that engages the temporary staffing agency.” This report will be
released by December 31, 2022.
The public health workforce was increased during the COVID-19 pandemic and many of
their current employees were redirected to focus on the pandemic. Nationally, nearly
three in four public health employees (72%) participated in the response to the COVID-
19 pandemic in some way. As of August 2021, Oregon’s local public health authority
workforce was made up of 1,143.9 FTEs for non-COVID roles. Between March 2020
and August 2021, FTE of local public health authority workforce increased 67% by
adding 761 FTE for the COVID-19 response for a total workforce of 1,905 FTE.
In summary, the COVID-19 pandemic continues to impact the health care system and
health care workforce. The workforce shortages, in addition to the omicron surge and
rising inflation, exacerbated hospitals’ financial challenges in early 2022. The financial
strains led to layoffs in the health care workforce and reduction of services in some
hospitals. Meanwhile, a study by the American Medical Association found that 2020 was
the first year in which less than 50% of patient care physicians worked in a private
practice. A report from the Physicians Advocacy Institute/Avalere Health found that
4,800 physician practices were acquired by hospitals and 31,300 were acquired by
corporate entities between January 2019 and January 2022. These findings suggest the
COVID-19 pandemic may lead to long-term changes in physician practice
arrangements, as physician group consolidations and shifts toward larger practices
have accelerated.

43
Telehealth during the COVID-19 pandemic
Telehealth is a collection of means or methods for enhancing health care, public health,
and health education delivery and support using telecommunications technologies.
Telehealth includes:
• Live audio and/or video conference between patient and clinician (e.g., by
telephone or Internet)
• Store and forward (e.g., specialist reviewing x-rays at a remote location)
• Telementoring or teleconsultation between clinicians. (e.g., clinician getting
advice from an offsite specialist to support care of a patient, using technology
such as video conference)
• Remote patient monitoring (e.g., devices that monitor blood glucose levels at
home and transmit to a physician)
• Mobile health (e.g., use of mobile applications to track health information)
Telehealth played a crucial role in maintaining access to health care at the beginning of
the COVID-19 pandemic due to limitations on in-person visits; telehealth utilization
remains much higher now compared to the period before the pandemic. In the longer
term, telehealth can potentially magnify the impact of Oregon’s limited and unevenly
distributed health care workforce by allowing patients to access clinicians and other
resources outside their home city or region.
Benefits and Potential Shortcomings of Telehealth
Telehealth can be very beneficial in health care shortage areas where patients have
difficulty finding providers close to their location, as in many rural areas of Oregon.
Patients who need services in a language other than spoken English can also benefit
from telehealth if a local in-person interpreter is not available for their visit. Telehealth
can also enhance access for patients who have transportation barriers, limited access
to childcare, or difficulty getting time off work. From a provider perspective, the
California Telehealth Resource Center notes that telehealth may improve workforce
retention by allowing more clinicians to work from home or on flexible schedules.
Patients appear to be mostly satisfied with using telehealth. McKinsey found that more
than half of surveyed patients were more satisfied with telehealth than in-person, and
that four in ten expected to keep using telehealth after the COVID-19 pandemic.
However, physicians generally found telehealth less convenient for themselves and
expected telehealth utilization to decline in the future; physicians also fear that future
telehealth reimbursement will be lower than for in-person care. This suggests a
fundamental disconnect between patient preferences and physician perceptions and
preferences, which could lead to future underuse of telehealth.

44
Telehealth holds the potential either to mitigate or to worsen health inequities. The
National Association of Insurance Commissioners explain that on one hand, telehealth
may improve access for patients from disadvantaged populations, who
disproportionately face transportation challenges and live in neighborhoods with fewer
specialty clinicians. On the other hand, racial/ethnic minority, low-income, rural, or
uninsured patients are also more likely to face technological or privacy barriers to
telehealth. Patients with limited English proficiency may also not benefit from telehealth
if interpreters are unavailable or patients have difficulty hearing them.
Technological and other barriers can limit access to telehealth services. Many patients
in rural regions or low-income households lack the broadband internet access that
enables video telehealth. The Oregon Statewide Broadband Assessment and Best
Practices Study found that one in four Oregonians lived in areas that did not have high-
speed broadband Internet access in 2020. Video telehealth also requires a camera,
video display, and digital literacy, which many older or low-income patients may not
have. Lack of privacy can also prevent patients form using telehealth for sensitive
discussions. Finally, visits that require a physical examination or procedure cannot be
conducted via telehealth.
Policy Context for Telehealth
Prior to the COVID-19 pandemic, telehealth utilization was growing rapidly, but
accounted for only 0.1% of all medical claim lines according to FAIR Health. Payers
often restricted coverage of telehealth, including lower reimbursement rates for
telehealth versus in-person visits. Federal regulations limited the communication
modalities that could be used for telehealth, and the Oregon Health Plan (OHP)
required patients to be at a clinic or other remote site (not their own home) to participate
in telehealth for physical health services.
Demand for telehealth visits increased dramatically at the beginning of the COVID-19
pandemic, driven by the risk of Coronavirus exposure and limited personal protective
equipment (PPE). Several policy changes to increase access to telehealth were rapidly
adopted in 2020, including:
• The Oregon Department of Consumer and Business Services and Oregon Health
Authority published guidance for health insurance plans to enhance the
availability and use of telehealth.
• An OHP temporary rule and a voluntary agreement between Governor Brown,
the Department of Consumer and Business Services, and several major
commercial health insurers increased coverage and reimbursement rates for
telehealth in Oregon.

45
• Modified regulations by some Oregon health care licensing boards made it easier
for out-of-state providers to obtain licensure and provide telehealth services to
Oregonians.
• At the Federal level, the Centers for Medicare & Medicaid Services (CMS) policy
changes permitted use of non-HIPAA-compliant platforms such as Facetime and
Skype, allowed patients and providers to access telehealth from homes and
community settings, and increased the types of Medicare providers that could
offer telehealth and the types of services that could be offered.
In June 2021, House Bill 2508 made many of these changes permanent in Oregon. It
required that the OHP and commercial insurance plans regulated by the Department of
Consumer and Business Services reimburse providers at the same rate for telehealth
and in-person visits, and that telehealth and in-person visits meet the same
requirements for prior authorization, medical necessity, or out-of-network
reimbursement. Subsequent OHP regulations made most of the pandemic telehealth
policies permanent, including allowing members to access telehealth services from
home; allowing telehealth for new patients and interpreter services; and paying audio-
only telehealth at parity with in-person services.
Flexibilities in Medicare telehealth policies were instituted under the COVID-19 Public
Health Emergency, which has been extended to January 11, 2023. Federal legislation
passed in March 2021 extended many of these flexibilities for approximately 5 months
(151 days) after the expiration of the Public Health Emergency. However, the omnibus
Federal spending bill passed in late December 2022 extended Federal telehealth
flexibilities (except those allowing prescription of controlled substances by telehealth)
through 2024.
Telehealth Utilization
Telehealth use increased dramatically during the COVID-19 pandemic, to 13.0% of
commercial health insurance claim lines in April 2020, according to FAIR Health.
Telehealth use was approximately one-third lower for rural patients than urban patients.
By July 2022, telehealth use had dropped to 5.3% of commercial health insurance claim
lines nationally, but was 7.4% in the western states. Among Medicare beneficiaries,
telehealth use also jumped dramatically during the first year of the COVID-19 pandemic,
then gradually declined to a plateau higher than the pre-COVID-19 level.
A U.S. Department of Health and Human Services (HHS) study of US adults found that
almost one in four had at least one telehealth visit in 2021. Black and Latino/a/x patients
were more likely to use any telehealth services, but Whites were more likely to use
video telehealth. Another HHS study of fee-for-service Medicare beneficiaries found that
one in three had a Part B (outpatient) telehealth service during 2021. This study also

46
found that White beneficiaries were less likely to use telehealth than those from other
racial/ethnic groups, and that rural beneficiaries had lower rates of telehealth use than
urban beneficiaries. J.D. Power found that patients in poorer health were less satisfied
with telehealth services than were patients with better self-reported health.
Figure 8.1 shows that telehealth use by OHP members rose very sharply from less than
1% before the COVID-19 pandemic to a peak of over 15% in September 2020. The
proportion of telehealth claims varies by month but remains at more than 8%.
Figure 8.1 Percentage of OHP Claims that are telehealth
Source: Medicaid Management Information System (MMIS). Data from OHA telehealth dashboard as of 9/30/2022.
Figure 8.2 shows the proportion of OHP ambulatory care claims for each major racial
ethnic/group that were provided via telehealth during Oregon fiscal year 2022. The
proportion of telehealth visits is similar for African-American (10%), American Indian
(10%), and Latino/a/x (9%) OHP members, higher for White members (11%), and lower
for Asian members (8%). Other racial/ethnic groups in these data are quite small;
because the data precede full REALD availability, race/ethnicity was Unknown for more
than a quarter of OHP members.
0.6%
8.7%
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
16.0%
18.0%
January 2020
February 2020
March 2020
April 2020
May 2020
June 2020
July 2020
August 2020
September 2020
October 2020
November 2020
December 2020
January 2021
February 2021
March 2021
April 2021
May 2021
June 2021
July 2021
August 2021
September 2021
October 2021
November 2021
December 2021
January 2022
February 2022
March 2022
April 2022
May 2022
June 2022
July 2022
August 2022
September 2022

47
Figure 8.2. Percentage of OHP ambulatory claims that are telehealth, by race and
ethnicity, Oregon fiscal year 2022
Source: Medicaid Management Information System (MMIS). Data from OHA telehealth dashboard as of 9/30/2022.
Excludes inpatient, dental, and pharmacy claims.
Notes: Proportion of total claims by race/ethnicity is shown below each bar. State fiscal year 2022 is July 2021 – June
2022.
Figure 8.3 shows the proportion of Oregon fiscal year 2022 OHP ambulatory care
claims that were provided via telehealth, by rurality of the member’s residence. The
proportion of telehealth visits is highest in urban areas (13%) and lower in rural areas
(9%).
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
African American or
Black
American Indian or
Alaska Native
Asian
Latinx
Middle Eastern or
North African
Native Hawaiian or
Pacific Islander
White
Other
Unknown
3% 3% 2% 8% <1% <1% 55% 1% 28%

48
Figure 8.3. Percentage of OHP ambulatory claims that are telehealth, by rurality of
residence, Oregon fiscal year 2022
Notes: Proportion of total claims by rurality is shown below each bar. State fiscal year 2022 is July 2021 – June 2022.
Source: Medicaid Management Information System (MMIS). Data from OHA telehealth dashboard as of 9/30/2022.
Excludes inpatient, dental, and pharmacy claims.
Both nationally and in Oregon, the rate of telehealth use varies widely across clinical
specialties. Multiple sources report that behavioral health accounts for more than half of
all telehealth visits nationally. OHP claims show a similar pattern, with 62% of OHP
telehealth claims in state fiscal year 2022 being for behavioral health and 25% for
primary care. Oregon Health & Science University (OHSU) researchers found that
adoption of telehealth in behavioral health helped mitigate the precipitous nationwide
drop in in-person visits early in the COVID-19 pandemic, but that that effect was smaller
for severe conditions such as schizophrenia.
Primary care providers adopted telehealth very rapidly in the early months of the
COVID-19 pandemic, according to AthenaHealth. Another study found that more than
one-third of primary care visits were via telehealth in the second quarter of 2020, with
telehealth utilization higher in the Pacific sates (including Oregon) than any other region.
Future of Telehealth in Oregon
The COVID-19 pandemic dramatically accelerated telehealth utilization and policy
changes. Future efforts should ensure that policy does not retrogress, the needs of
vulnerable groups are understood and addressed, and both patients and providers are
engaged in realizing the benefits of telehealth.
Continuing payment parity for telehealth services by commercial insurers, Medicare,
and Medicaid should be a policy priority. The Western Governors’ Association has
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
Urban Rural Frontier
62% 35% 3%

49
developed a detailed list of federal telehealth policy regulations, some of which can be
implemented by CMS but some of which require Congressional action. Oregon has also
collaborated with Washington, Nevada, and Colorado to develop a set of guiding
principles for telehealth and to coordinate their states’ telehealth policies.
Ongoing policy refinement by OHA, CMS, and commercial insurers will also be
required. For example, OHA has recently clarified that telehealth-only providers can be
reimbursed during the Public Health Emergency. However, concerns about the quality
of care from such providers, and their economic impact on Oregon health care providers
with physical offices must be monitored in the future.
Telehealth policy should also focus on measuring and addressing several potential
equity concerns:
• Racial/ethnic and other disparities. Data presented above, as well as other
recent research, suggest that racial/ethnic and socioeconomic disparities in
telehealth use were moderated during the COVID-19 pandemic, although age-
related disparities remain. Some health systems, such as Kaiser and Texas’s
Harris Health System have developed successful models for promoting
telehealth use in diverse populations. Nevertheless, ongoing efforts are
necessary to monitor and address disparities in telehealth use. In Oregon, more
comprehensive collection of REALD data should allow better measurement of
health care disparities among OHP members. It will also be important for health
systems, providers, and insurers to reach out and partner with diverse
populations and communities as they implement and refine telehealth programs.
• Specialty care. Recent studies have documented that COVID 19-era rates of
telehealth utilization vary dramatically across medical specialties outside
behavioral health and primary care. Some of this variation is due to the frequency
of medical or surgical procedures in some specialties, where the potential
contribution of telehealth is limited. Nevertheless, patients from vulnerable
populations, especially those with the most severe physical or behavioral health
conditions, need access to a full range of specialty care to protect their health.
• Rural residents. Telehealth plays a crucial role in rural areas for specialty care
and behavioral health, where the rural workforce is especially limited. Studies by
Oregon State University and Canadian researchers showed that rural areas saw
a slower increase than urban areas in telehealth use during the COVID-19
pandemic. Federal or state efforts to expand broadband Internet access would
allow more rural patients to access needed care via telehealth. Other policy
efforts noted above would also directly benefit rural residents in Oregon and
other states.

50
As described above, understanding and responding to patient preferences will be
necessary to maintain and expand telehealth successfully. For example, learning for
which services they prefer telehealth, or video vs. audio telehealth, can help to guide
the most effective allocation of providers’ telehealth resources. Coordinated Care
Organizations (CCOs) could use their Community Advisory Councils to solicit their
members’ preferences for telehealth services, and regular consumer assessments of
health plans and providers should explicitly evaluate telehealth encounters.
Finally, providers must be guided and supported to implement telehealth effectively and
achieve the potential workforce benefits. Physicians broadly support the use of
telehealth, but also harbor concerns about reimbursement and whether the proportion of
telehealth visits is too high. The Oregon Health Leadership Council has developed
detailed recommendations to guide telehealth implementation by adult and pediatric
primary care providers. But expanding and tailoring telehealth services to meet patients’
preferences will require significant investments by providers in digital infrastructure and
organization redesign. Financial support from insurers, states, or CMS could help to
encourage providers to make these important investments.

51
The Health Care Workforce Going Forward
According to the Oregon Employment Department’s recent analysis of health care
workforce trends in Oregon, the aging of Oregon’s population and the continued
development of medical treatments will drive strong growth in health care employment.
It is estimated that health care employment will grow 19% between 2020 and 2030,
which is higher than the statewide overall employment growth rate of 16%. It also
showed that more than half of jobs in health care require postsecondary education. To
support workforce education and training in health care as well as manufacturing and
technology industry sectors, Future Ready Oregon includes a comprehensive $200
million investment package with focus on advancing opportunities for historically
underserved communities. (See the Investments in Workforce Development section).
Health care providers need to reflect the populations they serve in order to provide
culturally and linguistically appropriate services. A recent report from the Urban Institute
calls for collaboration from a variety of stakeholders, including higher education,
philanthropy, and state and federal governments, to promote a diverse, equitable, and
inclusive health care workforce.
An equitable health care system that integrates physical, behavioral, and oral health
care and ensures access to culturally and linguistically appropriate health care requires
a robust workforce of Traditional Health Workers, Health Care Interpreters, nurses,
primary care providers, behavioral health providers, oral health providers, long-term
care workers, and a public health workforce. Each of these provider types is examined
below, with a focus on the importance of the providers and the services they deliver, the
current status of the provider workforce in Oregon, and efforts to support these
providers.
Traditional Health Workers
The Importance of Traditional Health Workers
Traditional Health Workers are trusted individuals from their local communities who
provide person- and community-centered care by bridging communities and the health
systems they serve. Traditional Health Workers can help increase the appropriate use
of care by connecting people with health systems, advocating for their clients,
supporting adherence to care and treatment, and empowering individuals to be agents
in improving their own health. The effectiveness of Traditional Health Workers is
enhanced when they have similar lived experience or are members of the same

52
community as the patients they serve. Traditional Health Workers also have knowledge
of health issues and understand how to help patients navigate the health system.
Traditional Health Workers help to assure the delivery of high-quality, culturally
responsive care which is instrumental in achieving the Oregon Health Authority’s (OHA)
overarching strategic goal: eliminate health inequities in Oregon by 2030.
Traditional Health Worker roles were defined in the original bill that created Oregon’s
Coordinated Care Organizations (CCOs) in 2011, House Bill 3650. As now codified in
ORS 414.665, there are five specialty types of Traditional Health Workers in Oregon:
• Community Health Workers share ethnicity, language, socioeconomic status, and
life experiences of the community they serve. They assist individuals and their
community to achieve positive health outcomes, including facilitating linkages
between health/social services and the community; and improve the quality and
cultural competence of service delivery.
• Peer Wellness Specialists are informed by their own experiences with recovery
and assist with recovery from addiction, mental health, and physical conditions
by helping to integrate behavioral health and primary care and help individuals
achieve well-being.
• Peer Support Specialists provide services to individuals who share a similar life
experience with the Peer Support Specialist (addiction to addiction, mental health
condition to mental health condition, family member of an individual with a mental
health condition to family member of an individual with a mental health condition).
Types of Peer Support Specialists include recovery peers, mental health peers,
family support specialists, and youth support specialists.
• Personal Health Navigators provide information, assistance, tools, and support to
enable a patient to make the best health care decisions.
• Birth Doulas are birth companions who provide personal, nonmedical support to
women and families throughout a person’s pregnancy, childbirth, and postpartum
experience.
In 2021, House Bill 2088 was passed that requires OHA to adopt by rule qualification
criteria for Tribal Traditional Health Workers as additional category of Traditional Health
Workers effective in 2022 for tribal health care providers that supports tribal-based
practices.
OHA’s Traditional Health Worker Program, housed in the Equity and Inclusion Division,
assists Traditional Health Workers in becoming trained and certified to meet current
standards and provide high-quality and culturally competent care. The Traditional
Health Worker program works to promote the roles, engagements, and utilization of the

53
traditional health workforce, and, in partnership with stakeholders, community-based
organizations, and health systems, strives to ensure that Traditional Health Workers are
uniquely positioned to work with communities to identify and address the underlying
causes of health problems and health inequities. The Traditional Health Worker
Commission advises and makes recommendations to OHA, to ensure the program is
responsive to consumer and community health needs. Traditional health workers can
become certified in Oregon if they are at least 18 years old, submit required
documentation, and successfully complete the training requirements for certification
specific to the type of Traditional Health Worker.
Traditional Health Workers in Oregon
As of October 2022, there were more than 4,400 Traditional Health Workers certified in
Oregon. Below is a breakdown of the traditional health workforce in Oregon and its
composition by worker types.
Figure 10.1. Current number of Certified Traditional Health Workers in Oregon,
October 2022
Source: OHA Traditional Health Worker certification dashboard as of 11/21//2022
For a breakdown of demographics by Traditional Health Worker types, please refer to
Figures 10.2 and 10.3. Traditional Health Workers identified as primarily female and
White. Community Health Workers identified more as persons of color than the other
Traditional Health Worker types. Females represented the overwhelming proportion of
doulas and Community Health Workers; however, approximately one-third of peer

54
support specialists and peer wellness specialists identified as male. Language use
varied greatly between groups, with Community Health Workers being most likely to use
a language other than English at home (42.6%) compared to doulas (12.5%), peer
support specialists (8.5%), and peer wellness specialists (14.0%). Doulas report the
youngest age (average age 39 years) compared to all other Traditional Health Workers
(Community Health Worker (average age 45 years), peer support specialists (average
age 47 years), and peer wellness specialists (48 years)). The percent of Traditional
Health Workers who reported having a disability was lowest among doulas and
Community Health Workers (5%) and highest among peer wellness specialists (32.6%).
Doulas and Community Health Workers are most likely to have completed a bachelor’s
degree or higher.
Figure 10.2. Race, ethnicity, and gender by Traditional Health Worker type
Source: Pilot Survey of OHA Registered Traditional Health Workers, Office of Health Analytics, Oregon Health
Authority, 2021
Notes: ^ may be statistically unreliable, interpret with caution and * estimate suppressed; sample too small.

55
Figure 10.3. Highest level of education obtained by Traditional Health Worker
types
Source: Pilot Survey of OHA Registered Traditional Health Workers, Office of Health Analytics, Oregon Health
Authority, 2021
Notes: ^ may be statistically unreliable, interpret with caution and * estimate suppressed; sample too small.
Most respondents were actively working in the field with 80-90% reported working of
doulas, Community Health Workers, and peer support specialists (but only 63% peer
wellness specialists). Most Traditional Health Workers have been practicing for less
than 5 years.
Among those that were unemployed or employed in another field, 37% were not
seeking paid work as a Traditional Health Worker often because of the low pay or
because they were employed in another field. Most Traditional Health Workers are
employed primarily by organizations (doulas are the exception). The most common
organization type to be employed by was a non-profit agency. Doulas are concentrated
in Willamette Valley and peer wellness specialists in the Portland metro area (See
Figure 10.4). Doulas and peer support specialists are more likely to see Oregon Health
Plan (OHP) clients compared with Community Health Workers and peer wellness
specialists. The average hours per week worked was 20 and average number of clients
per month was 49. Doulas work the fewest hours per week and have fewer clients per
month than the other types of Traditional Health Workers. Nearly 70% of doulas
reported having to turn away clients.
Most Traditional Health Workers report practicing telehealth (doulas 84%, peer support
specialists 72%, Community Health Workers 68%, and peer wellness specialists 58%).
Top reasons for registration with OHA were that the registration was a requirement by
their employer, hope for an opportunity for improved communication about qualifications
with employers and clients, and a mentor or training program encouraged them to
register.

56
Figure 10.4. Current number of certified Traditional Health Workers by regions in
Oregon, October 2022
Source: OHA Traditional Health Worker regional report as of 11/21//2022

57
Figure 10.5. County of primary employing organization for those that reported
working for organizations by type of Traditional Health Worker
Source: Pilot Survey of OHA Registered Traditional Health Workers, Office of Health Analytics, Oregon Health
Authority, 2021
OHA requires contracted Coordinated Care Organizations (CCOs) to develop an annual
Traditional Health Worker Integration and Utilization Plan. These CCO plans must
include strategies for integrating Traditional Health Workers into the delivery of services,
communicating with members and providers about the benefits of Traditional Health
Worker services, and evaluating the delivery and effectiveness of Traditional Health
Worker services. OHA’s Traditional Health Worker Program facilitates integration of the
Traditional Health Worker workforce across health systems, and recently launched a
toolkit with information for health systems, providers, and Traditional Health Workers.

58
Future Workforce of Traditional Health Workers
In recent years, OHA has worked with community-based organizations to conduct
assessments of the Traditional Health Worker workforce, including a Community Health
Worker Needs Assessment, a Doula Workforce Needs Assessment, and a Peer-
Delivered Services Workforce Needs Assessment. These assessments used key
informant interviews, focus groups, and surveys of the workforce and employers to
understand the landscape for Traditional Health Workers. These assessments generally
found that there needs to be greater understanding of the roles of Traditional Health
Workers, better efforts to integrate Traditional Health Workers into the health care
system, higher reimbursement rates for Traditional Health Workers, clarity around billing
issues, and improved processes for training and certification.
A recent study interviewed 75 individual birth doulas and doula organizations who work
with underserved and historically excluded populations across the country. Doulas
engaged in specific activities to advance perinatal equity and felt called to do it.
However, many birth doulas experienced several work-related stressors, including
witnessing discrimination against clients, experiencing discrimination in medical
environments, and struggling with financial instability. Barriers to further training
included cost and accessibility. Recommendations included doula peer support to
lessen these stressors; increased compensation; a focus on attracting, training, and
employing providers of color and from other underrepresented communities.
Results from the pilot survey showed that Traditional Health Workers are still underpaid
and are underrepresented in certain regions of the state and underrepresented in
persons of color relative to Oregon’s population and possibly among other communities
such as LGBTQ+. These surveys will provide more accurate data on the providers in
Oregon and can be used to inform future studies of the workforce, including their
demographics, work environments, and training needs.
The Oregon Office of Rural Health has partnered with OHA to coordinate a CDC grant-
funded program that will support the capacity of Oregon’s rural public health agencies
and Critical Access Hospitals by growing the community health worker workforce in
rural Oregon. This is a pilot grant program to fund the training of community health
workers for employment at Critical Access Hospitals and rural public health departments
in Oregon. Community health workers training education can be taken through the
Northeast Oregon Network or Oregon State University. The Oregon Office of Rural
Health is currently recruiting for this program and plan to coordinate training of 25
community health workers by spring of 2023 (training will likely begin in Jan. 2023). The
Oregon Office of Rural Health will support a peer-to-peer network for community health
workers students.

59
The COVID-19 pandemic has exposed inequities in access to resources, both the
pandemic and the collective response to the pandemic caused greater distress in
certain communities. One of the tenets of the Traditional Health Worker approach is that
people from the community are best at identifying and implementing solutions to health
challenges, including those related to social determinants of health. Traditional Health
Workers can be part of an effective workforce to implement interventions that address
social determinants of health as well as equitable access to health care. Lessons
learned from this community-based approach to COVID-19 can be carried forward to
inform the use of Traditional Health Workers to address other community challenges in
the future.
Recommendations for the future of the Traditional Health Worker workforce come from
survey data asked of Traditional Health Workers, assessments by community-based
organizations, and from OHA staff and study authors. Recommendations for Traditional
Health Worker workforce include:
• increased compensation
• improved reach to all counties across the state
• strategies to recruit, train and employ providers of color and from other
underrepresented communities.
Health Care Interpreters
The Importance of Health Care Interpreters
Health Care Interpreters are bilingual individuals who help people in their communities
with limited English proficiency or persons who communicate in sign language, to
interact effectively with health care providers. Health Care Interpreters provide high
quality health care interpretation at in-person medical appointments or over the phone
or video. Certified and qualified interpreters must have formal training and must pass
national certification exams or language proficiency assessments in the case of
qualified interpreters. Health care interpreting can improve the quality of patient-provider
communications and health literacy. Research has shown that effective health care
interpreting can reduce rates of adverse events and unnecessary exams, increase
uptake of preventive care, and increase patient and provider satisfaction.
Health Care Interpreters in Oregon
The Health Care Interpreter program at the Oregon Health Authority (OHA) was
established in 2010 to help develop a well-trained workforce of Health Care Interpreters
60
to address language and communication barriers to accessing health care services. The
Oregon Council on Health Care Interpreter advises OHA on administrative rules and
policy standards for the Health Care Interpreter Program. The program has developed
training standards, curricula, and a Health Care Interpreter registry enrollment process;
and there are now over 1,200 Qualified and Certified Interpreters in the Oregon registry.
As Oregon becomes more linguistically diverse, the need for well-trained Health Care
Interpreters increases.
OHA’s Health Care Interpreter training standards are among the highest in the country.
The requirements for becoming a Qualified or Certified Health Care Interpreter in
Oregon include 60 hours of formal Health Care Interpreter training from an OHA-
approved training center, and completing an equivalent language proficiency
assessment in English and a second language. Certified Health Care Interpreters in
Oregon must additionally pass a national certification exam from an OHA recognized
organization. The two national Health Care Interpreter certifying organizations are the
National Board of Certification for Medical Interpreters and the Certification Commission
for Healthcare Interpreters, which together offer exams for seven languages: Arabic,
Cantonese, Korean, Mandarin, Russian, Spanish, and Vietnamese. To increase the
supply of Certified spoken and sign language Health Care Interpreters in Oregon,
Certified Interpreters from the following organizations can apply to be listed on Oregon’s
Health Care Interpreter registry, if they complete additional Health Care Interpreter
training requirements: Oregon Certified Court Interpreters, Federal Court Interpreters,
and American Sign Language (ASL) Interpreters from the Registry of Interpreters for the
Deaf.
In addition to the requirements to provide interpretation services as part of the non-
discrimination provisions of Title VI of the Civil Rights Act of 1964, the Oregon
Legislature passed House Bill 2359 in 2021 mandating that health care providers who
are reimbursed with public funds work with a qualified or certified Health Care
Interpreter who is listed on the state registry. The law went into effect on July 1, 2022,
and does allow some exceptions for working with a Health Care Interpreter not listed on
the central registry.
OHA oversees policies and processes to improve and enforce trainings and certification
standards and has collaborated with community partners to identify changes to increase
the number of qualified and certified Health Care Interpreters on the central registry.
OHA removed all application fees and streamlined the application requirements for both
those inside and outside of Oregon; eliminated background checks for inclusion as a
qualified or certified Health Care Interpreter on the central registry (but it may be
required by employers); and arranged for free or low-cost Health Care Interpreter

61
trainings. Prior to the changes made by House Bill 2359, there was reliance on Health
Care Interpreters from outside of Oregon and who were not yet on Oregon’s central
registry. OHA has given health care providers and interpreting service companies until
July 1, 2023, to transition to the new policies around the central registry.
In 2021, the Health Care Interpreter program conducted a survey of Health Care
Interpreters to gain a better understanding of Oregon’s interpreter workforce. The
survey was sent to all 719 Health Care Interpreters on the state registry at the time. A
total of 149 Health Care Interpreters completed the survey results in a 21.8% response
rate. Among the 30 languages spoken by the 2021 survey respondents, Spanish was
spoken most frequently (60% of respondents). With many languages, including
Spanish, it is important to match the particular dialects of the patient and interpreter, as
there can be significant differences in dialects based on country of origin, and regions
within a country. Most respondents identified as female (78%) and were an average age
of 46 years and 3.4% reported having a disability. Over half (58%) of the respondents
were college graduates, including those with bachelor’s degrees (30%), and graduate
professional degrees (28%). Over 90% had completed a certification program with at
least 60 hours, over half (57%) had completed an OHA approved training program, and
11% had completed the Registry of Interpreters for the Deaf for fluency in American
Sign Language.
The majority (94%) of respondents reported currently working in the field. Over half of
responding Health Care Interpreters have been practicing for more than 5 years. Most
Health Care Interpreters were employed by organizations, most frequently language
service companies. Most Health Care Interpreters worked at a clinic (88%) or hospital
(76%), and they mostly worked onsite (70%), with some working via phone (16%) or
video (14%). More than 80% of respondents reported that their primary employer was
based in Multnomah (67%), Washington (7%), Marion (7%), or Jackson counties (96%).
Most Health Care Interpreters worked 20 hours per week and were paid within a range
from $25-$28/hour, with those certified obtaining a higher median hourly rate.
The most common reason Health Care Interpreters registered with the state was to be
able to communicate to employers and clients their qualifications as a Health Care
Interpreter. Other reasons included expanded skills and certifications, increased pay,
and serving their community. Barriers to the registration process were the cost and
difficulty in reaching someone at the registry if the Health Care Interpreter had
questions. The largest barriers to certification were the cost and the exam difficulty,
completing continuing education hours, and availability of trainings. Individuals applying
to become a certified Health Care Interpreter are notified of the determination of their
application within 60 days after submitting a completed application.
62
Future Workforce of Health Care Interpreters
A report from OHA’s Equity & Inclusion Division summarized recommendations for
improving health care interpreting in Oregon. Additional recommendations for the future
of the Health Care Interpreter workforce come from survey data asked of Health Care
Interpreters, and from OHA staff and study authors. Recommendations for the Health
Care Interpreter workforce include:
• policy options to improve compensation (e.g., paying for a two-hour minimum
and for patient no-shows)
• additional programs for training Qualified and Certified Interpreters, especially in
rural communities experiencing growth in language access needs
• technical assistance for providers and health care systems to improve their
language access plans for forecasting language access needs and auditing the
quality of language access services
• studies to determine the best model for an online Health Care Interpreter
scheduling platform and national standards and best practices for sight
translation.
Increasing the use of Qualified and Certified Interpreters would improve the quality of
health care interpreting and thus the quality of health care for patients who need
interpreting services.
OHA’s work with Coordinated Care Organizations (CCOs) includes contract
requirements to improve data collection that can provide insights into the demand for
interpreter services by CCO members, and how health care systems are working with
OHA Qualified and Certified Health Care Interpreters to provide effective interpreter
services. In order to achieve meaningful language access to culturally responsive health
care services, the utilization of qualified and certified Health Care Interpreters was
adopted as a CCO incentive metric.
In 2021, CCOs were required to conduct a self-assessment of language access and
attest to work to identify and assess communication needs, provide language
assistance services, train staff and provide notice of language assistance services. All
but one of the CCOs met this measure. In 2022, the measure will also require CCOs to
report on how often interpreter services were provided when CCO members with
identified interpreter needs had physical, behavioral, or dental health visits.

63
Nursing Workforce
The Importance of the Nursing Workforce
Nurses play a central role in all Oregon health care settings, including primary and
specialty outpatient care, inpatient and post-acute care, home health, and behavioral
health. Nurses practice at different levels of licensure, where increased clinical
responsibilities and independence require higher levels of training:
• Certified nursing assistants (CNAs) work under the direction of licensed nurses to
provide basic care such as assistance with activities of daily living (bathing,
dressing, using the toilet, etc.)
• Licensed practical nurses (LPNs) provide basic nursing care such as medication
administration or dressing changes. LPNs must complete a community college or
vocational education program and pass a national licensing exam.
• Registered nurses (RNs) provide advanced nursing services such as patient
assessment, care planning, patient education, and care coordination. RNs must
obtain either an associate or bachelor’s degree and pass a national licensing
exam. RNs work in hospitals as well as almost every other health care and public
health setting, often developing specialized expertise.
• Advanced practice registered nurses (APRNs) must complete a masters or
doctoral degree. The most numerous APRNs are nurse practitioners (NPs), who
can practice independently and are often primary care providers. Nurse
midwives, nurse anesthetists, and clinical nurse specialists are also APRNs.
In 2022, researchers from the University of California, San Francisco (UCSF) and the
Oregon Center for Nursing (OCN) submitted to the Oregon Health Authority (OHA) and
the Health Care Workforce Committee a report entitled “The Future of Oregon’s Nursing
Workforce: Analysis and Recommendations.” The following pages summarize key
aspects of that report, but interested readers should refer to it for more detail on many
topics. This section also draws on other research and journalistic sources, which are
cited when their findings are described.
Oregon’s Nursing Workforce
In the United States, nurses are licensed at the state level. The Oregon State Board of
Nursing (OSBN) works within the requirements of the Oregon Nurse Practice Act and
other state legislation.
Two in three of Oregon’s approximately 90,000 licensed nurses are RNs. Table 12.1
shows the number of nurses at each level of licensure, and the estimated proportion
who are currently practicing in Oregon.

64
Table 12.1. Licensed and practicing nurses in Oregon
Certified
Nursing
Assistants
(CNA)
Licensed
Practical
Nurses (LPN)
Registered
Nurses (RN)
Advanced
Practice
Registered
Nurses (APRN)
Licensed
18,640
5,644
59,778
5,574
Practicing
16,200
4,680
44,900
4,330
Percent
practicing
86.9%
82.9%
75.1%
77.7%
Source: OCN analysis of OHA 2020 Public Use Nursing Workforce Data File
Oregon community colleges offer eight LPN programs and 17 associate degree of
nursing (ADN) programs. There are also 10 bachelor of science in nursing (BSN)
programs, including five Oregon Health & Science University (OHSU) campuses. In
recent years, Oregon BSN programs have produced an increasing number of
graduates, while the number of ADN graduates has remained relatively flat (Figure
12.2). In contrast, the number of Oregon LPN graduates in 2020 was 38% smaller than
in 2012.
Figure 12.2. RN graduates in Oregon
Source: OSBN Annual Surveys of Nursing Education Programs, 2022
RN program graduates who successfully complete the national licensing exam in
Oregon are licensed via “examination.” RNs who are licensed in other states can also
apply to the OSBN to be licensed in Oregon via “endorsement.” The number of RNs
licensed by endorsement began to increase very rapidly in about 2010 (Figure 12.3)
and has greatly exceeded licenses via examination in recent years. OCN research

65
estimates that only about one in three RNs licensed via endorsement since 2010
actually practice in Oregon. Importantly, RNs licensed via endorsement are more likely
to practice in Oregon’s small, rural communities.
Figure 12.3 Oregon RN licenses by year
Source: OCN analysis of OHA 2020 Public Use Nursing Workforce Data File
During the COVID-19 pandemic, Oregon created a new category of Emergency
Authorization License. This allowed employers to hire travel nurses (who work on a
short-term basis) more quickly. The emergency authorization license expired in Summer
2022, but some of these nurses applied for and were granted licensure via endorsement
from OSBN.
In 35 states, the Nursing Licensure Compact allows a nurse licensed in one Compact
state to practice in any other Compact state. This does not increase the overall size of
the national nursing workforce, but does allow greater flexibility for in-person nursing
care (such as during disaster response) or telehealth. Oregon is not currently a member
of the Compact.
Across all license types, 84.6% of Oregon nurses are female. Among RNs licensed in
Oregon, 86% are female, compared to 91.6% nationally. The median age of Oregon
RNs is 51, compared to 52 nationally. The distribution of Oregon nurses has shifted
toward younger ages: the largest age cohort of RNs was 55-60 years in 2012, but was
30-35 in 2020.
Table 12.4 shows that Oregon CNAs and LPNs are more racially and ethnically diverse
than RNs and APRNs. Overall, the proportion of nurses who are Hispanic or Latino/a/x
is significantly lower than among the overall Oregon population. Recent graduates of

66
Oregon nursing programs are more diverse than practicing nurses, with 52%, 63%, and
67% of LPN, associate degree RN, and bachelors degree RN graduates, respectively,
being White.
Table 12.4. Race and ethnicity of Oregon’s nursing workforce and population
Race/Ethnicity
CNA
LPN
RN
APRN
All
Nurses
Oregon
Population
American Indian/Alaska
Native
0.9%
0.7%
0.5%
0.3%
0.6%
1.9%
Asian
5.9%
4.1%
4.1%
3.7%
4.4%
5.0%
Black or African
American
5.9%
4.1%
1.4%
1.7%
2.4%
2.3%
Hispanic or Latino/a/x
14.7%
7.8%
3.9%
3.5%
6.1%
14.0%
Native Hawaiian/Pacific
Islander
1.0%
0.6%
0.4%
0.3%
0.5%
0.5%
White
57.0%
68.3%
76.8%
78.6%
72.6%
74.1%
Multiple race
3.5%
3.6%
2.5%
2.1%
2.7%
4.2%
Other race
0.5%
0.4%
0.4%
0.5%
0.4%
N/A
Declined to answer
10.6%
10.4%
10.2%
9.1%
10.2%
N/A
Source: OCN analysis of OHA 2020 Public Use Nursing Workforce Data File
The setting in which Oregon nurses are most likely to practice varies widely by type of
license (Figure 12.5). The large majority of CNAs practice in long-term care facilities
(45%) or hospitals (40%). Most LPNs practice in long-term (39%) or outpatient (26%)
care. Just over half (55%) of RNs practice in hospitals, while half (51%) of APRNs
practice in outpatient care.

67
Figure 12.5. Oregon nurse practice settings
Source: OCN analysis of OHA 2020 Public Use Nursing Workforce Data File
* Long-term care includes Skilled nursing facilities, Assisted living, Residential care, Adult foster homes
Demand for nurses is driven by the number and acuity of patients who need inpatient,
outpatient, and long-term care. The need for such care is increasing as Oregon’s
population ages, but the level of demand also depends on nurse workload in each care
setting. For example, home care workload is driven by Medicare and Medicaid
reimbursement requirements. Skilled nursing facilities are required to provide 24-hour
nursing care, but individual facilities decide how to meet that requirement. In August
2022, the Centers for Medicare & Medicaid Services (CMS) began a major study that
aims to define minimum staffing needs in skilled nursing facilities, which will inform new
regulations in Spring 2023.
Many states, including Oregon, have regulations regarding maximum nursing workload
in hospitals. Determining the appropriate nursing workload on any inpatient unit is
complex, based on the ever-changing balance of patient volume, acuity, and nurse
experience. Oregon law therefore does not mandate minimum nurse-to-patient ratios,
but rather requires each hospital to develop and implement a nurse staffing plan,
approved by the hospital nurse staffing committee, which sets the minimum number of
RNs, LPNs, and CNAs per shift. The law’s requirements and audit processes were
strengthened in 2015, and hospitals have faced challenges with compliance. On
average, RN staffing ratios (full-time equivalent employment per 1000 adjusted patient
days) were higher in Oregon (5.21) than in other states (4.74), but that may reflect
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
CNA LPN RN APRN
Hospital Office/Clinic Long term care* Home health/Hospice Other

68
higher acuity of Oregon’s hospital patients. Oregon also has lower staffing ratios for
LPNs and CNAs than other states.
Nursing maldistribution and shortages. Research by OCN suggested that, prior to
the COVID-19 pandemic, Oregon was not facing an overall nursing shortage. However,
a “maldistribution” of the nursing workforce was apparent, with some practice settings in
Oregon having much greater difficulty recruiting or retaining nurses than others.
Vacancy rates were lowest in hospitals (5.3%), higher in-home health/hospice (12.2%)
and public health (10.5%), and highest of all in long-term care (28.3%). Other OCN
research found that some of the variation across practice setting was caused by nurses
moving to different practice settings across their careers. Specifically, recently
graduated nurses are more likely to work in hospital or long-term care settings, while
more experienced nurses are more likely to work in outpatient care, home
health/hospice, public health, or education.
OCN also found that nurses are not evenly distributed across all 36 Oregon counties,
with many rural counties having fewer nurses than would be expected based on their
population. Although the reasons for this geographic maldistribution are not clear, it is
likely that the factors causing it to differ across communities, and may include limited
educational opportunities, housing, and spouse/partner employment opportunities in
smaller communities.
More recent OCN research highlighted reasons for concern about potential future
shortages. Only about 72% of Oregon’s annual demand for new RNs is met by
graduates of the state’s nursing education programs, with the balance made up by an
increasing number of RNs from other states gaining Oregon licenses by endorsement. If
in-migration from other states slows, or if the proportion of endorsed nurses who
actually practice in Oregon continues to fall, nursing shortages may become more
acute, particularly in non-hospital settings in smaller cities and rural areas.
The COVID-19 pandemic exacerbated the existing maldistribution and created
shortages. Nationwide, nursing employment in all practice settings dropped early in the
pandemic, but then recovered in all settings except long-term care. In Oregon, this has
created a bottleneck in post-acute care and contributed to severe capacity shortages at
hospitals: patients who are too ill to go home cannot be discharged, and so hospitals
cannot admit new patients who need care. Higher turnover among LPNs than RNs,
driven by LPNs leaving the health care workforce, also disproportionately affected the
long-term care where LPNs often work.

69
Although comprehensive data are not yet available, journalistic reports and UCSF study
interviews indicate that Oregon hospitals are facing severe nurse staffing challenges in
Fall 2022 as a result of the COVID-19 pandemic. Staffing shortages affect RNs, LPNs,
and CNAs, leading to emergency room delays and excessive inpatient workload.
Burnout among nurses spiked early in the pandemic and continued through multiple
waves of COVID-19 admissions, even after vaccines became available. Many nurses
left full-time hospital positions to work as travel nurses for higher pay and fewer hours.
This increases the workload for the remaining nurses, and travel nurses take time to
learn work processes in new hospitals. Travel nurse costs also overload hospitals’
budgets and limit their ability to hire support staff. Support staff shortages further
increase nurse workload and stress because RNs then must perform both higher level
tasks (such as basic respiratory therapy) or lower-level tasks (such as phlebotomy)
more frequently than they usually would.
Before the COVID-19 pandemic, retention of Oregon nurses was higher than the
national average. However, anecdotal reports indicate that retention has declined
recently.
Burnout among nurses. OCN researchers recently found high levels of burnout (see
the Workforce Resiliency section) in Oregon, based on almost 5,000 responses to an
April 2022 survey of nurses at all licensure levels. Four in five nurses reported
experiencing increased levels of work stress and frustration in the previous three
months, and two in three reported increased anxiety. Seven in ten nurses reported
“heavy or increased workload” and “uncertainty about return to normal” as major work
stressors, and over six in ten reported burnout. More than half of nurses were
questioning their career path. Key informant interviews point to the extended COVID-19
pandemic as the main source of these stressors.
Fewer than half of nurses believed they received adequate emotional support at work,
but more than nine in ten believed their employers could make changes to improve their
mental and emotional well-being. The most important changes nurses said they needed
from employers were more nurses (66%), more support staff (59%) and meaningful
recognition (50%).
Nursing education capacity & transition to practice. Oregon’s community college
and university programs do not have adequate capacity to meet the state’s demand for
newly trained nurses. One major cause of this shortfall is faculty shortages. The number
of Oregon faculty to train RNs has increased since 2017, especially in BSN programs,
but still remains inadequate. Nurse educators earn salaries 10% to 40% less than they
could earn in clinical practice and must perform numerous other academic duties in
addition to teaching.

70
Another barrier to expanding nurse training in Oregon is securing enough clinical
placements for students during their education. Identifying placements for hundreds of
students annually, mostly in hospital settings, was an ongoing challenge before the
COVID-19 pandemic, and then worsened dramatically. The staff shortages and stresses
described above have severely limited the capacity of experienced nurses to supervise
students in their practice settings.
In the first two or three years after graduation, new nurses must first master basic skills
and then learn to manage increasingly complex clinical situations. Increasing
administrative and organizational complexity also challenges new nurses. Robust
transition-to-practice programs offer new nurses structured training and simulations, as
well as mentoring from experienced nurses. However, not all Oregon workplaces offer
these programs, and the COVID-19 pandemic has reduced employers’ ability to offer
them.
Oregon also has some unique barriers to CNA education and certification. It requires
more than twice as many training hours as the federal standard, even though CNAs
from other states with less stringent requirements can be certified to practice in Oregon.
There are also two levels of CNA in Oregon, with somewhat overlapping requirements.
This appears to cause confusion among persons considering becoming a CNA.
Future of the Nursing Workforce
Oregon has implemented some short-term measures to mitigate the problems outlined
above:
• The Oregon Wellness Program provides free counseling and education to health
care professionals. It was originally established to support physicians, physician
assistants, dentists, and APRNs, but an additional $500,000 has been allocated
to expand this program to RNs, LPNs, and CNAs.
• In September 2022 the Oregon Legislature approved $39.5 million (including
federal matching funds) to help alleviate capacity shortages at Oregon hospitals
over the subsequent six months. These funds will support contract nurses at
long-term care facilities and hospitals, provide incentives for adult foster homes,
residential care facilities and home care agencies to accept patients from
hospitals and skilled nursing facilities, fund respite shelter beds for skilled nursing
facility patients, and support behavioral health facilities.
In their report, UCSF and OCN researchers outlined a wide range of longer term policy
recommendations to strengthen Oregon’s nursing workforce. Their recommendations
were to:

71
• Create healthier work environments to retain nurses:
o In addition to providing adequate nursing and support staff, employers
should implement interventions such as increased professional recognition
and autonomy, shared governance, and team-based care models.
o The state can support these efforts by continuing and expanding the
Oregon Wellness Program, and providing employers with best practice
guidance, financial incentives, and seed funding.
• Strengthen Oregon’s nurse training system at all stages:
o Support middle and high schools to prepare their graduates for nursing
education
o Support LPN and RN education programs to expand enrollment by
increasing faculty pay, expanding to rural areas, and strengthening the
LPN-to-RN pathway.
o Develop centralized clinical placement systems and expand simulation
facilities
o Establish more apprenticeships, internships, and/or residencies that
support new nurses’ transition to practice
• Consider other actions including:
o Streamlining CNA education and scope of practice
o Joining the Nurse Licensure Compact
o Evaluating and revising Oregon’s nurse staffing law
o Encouraging local solutions to nursing shortages
o Systematically collecting data from employers, projecting future nurse
supply and demand, and understanding the causes of racial and ethnic
disparities in nursing
Primary Care Providers
The Importance of Primary Care Providers
Primary care providers can be any of four licensed occupations, including physicians
(MD/DO), nurse practitioners, physician assistants, and naturopathic physicians.
According to the American Academy of Family Physicians, “A primary care practice
serves as the patient's entry point into the health care system and as the continuing
focal point for all needed health care services.” Primary care providers not only care for
patients with differentiated and undifferentiated problems, but also perform health
promotion, disease prevention, health maintenance, counseling, and patient education.
Primary care practices are located in a variety of health care settings, such as office,
inpatient, critical care, long-term care, home care, schools, and telehealth, and are

72
important to facilitate access to health care and provide comprehensive and continuing
care.
Primary care providers play a critical role in patient care and education, especially
during national health emergencies like the COVID-19. Based on the 2021 evidence-
based report by the Primary Care Collaborative, residents in communities with greater
primary care access had better COVID-19-related outcomes such as less likely to get
infected or die from COVID-19. Primary care also faced significant financial losses
during the COVID-19 pandemic (see Impacts of COVID-19 section). Researchers
estimated primary care lost $67,774 in gross revenue per FTE physician and lost $15.1
billion nationally in 2020. The COVID-19 pandemic has highlighted the long-standing
problems like underinvestment and workforce shortage in primary care. According to the
Larry Green Center reports, primary care is responsible for 50% of all medical visits
each year, but only receives less than 7% of national health expenditures.
Primary Care Providers in Oregon
The National Center for Health Workforce Analysis estimates that from 2018 to 2030,
the number of primary care providers needed will increase by 13%, while the number of
active primary care providers will increase by only 6%. The 2022 Licensed Health Care
Workforce Supply report by the Oregon Health Authority (OHA) estimated there were
8,905 primary care providers actively practicing in Oregon, the majority of which were
physicians (Table 13.1) .
Table 13.1. Primary care providers FTE by occupation in Oregon, 2022
Occupation
Direct patient care
FTE
Actively practicing
professionals
Physicians
4,638
6,041
Nurse practitioners
1,241
1,642
Physician assistants
694
889
Naturopathic Physicians
206
333
TOTAL
6,779
8,905
Source: OHA Office of Health Analytics. 2022 Oregon’s Licensed Health Care Workforce Supply.
Figure 13.2 shows the direct patient care FTE for primary care professional to
population ratios at state and county levels. The statewide ratio was 16.2 FTE per
10,000 Oregonians. The county ratios varied widely, ranging from 6.1 per 10,000
(Columbia) to 30.9 per 10,000 (Wallowa).

73
Figure 13.2. Primary Care Professional FTE per 10,000 Population, 2022
Source: OHA Office of Health Analytics. 2022 Oregon’s Licensed Health Care Workforce Supply.
Figure 13.3 shows the primary care capacity by service area, with the shaded areas
being below the statewide primary care capacity ratio. A primary care capacity ratio of
1.00 means that primary care supply should be equal to demand if access and
affordability were equal for everyone. A ratio less than 1.00 means that there is more
demand for primary care visits than supply. The statewide primary care capacity ratio is
1.21, meaning that with adequate distribution of providers across the state, there should
be enough primary care capacity to meet patient needs. Urban areas have a primary
care capacity ratio of 1.38. Rural areas have a primary care capacity ratio less than 1 ,
indicating that the number of health care providers is insufficient to meet the demand for
primary care health delivery as calculated.

74
Figure 13.3. Primary Care Capacity by Service Area
Source: The Oregon Office of Rural Health. The Oregon Area of Unmet Health Care Need report.
As illustrated in Figure 13.4, Oregon’s primary care workforce is less racially and
ethnically diverse than the general population with Latino/a/x, African American/Black,
American Indian/Alaska Native, and Native Hawaiian/Pacific Islander providers being
underrepresented. (See the Health Care Workforce Reporting Program Data section for
detail by occupation).

75
Figure 13.4. Race and ethnicity of primary care providers in Oregon
Note: Preliminary data provided from the 2022 Diversity of Oregon's Licensed Health Care Workforce Report Draft
(01/2023). Providers with missing data were excluded from the analysis. Some Workforce records are missing race
and ethnicity data because licensees declined to report race or ethnicity. Middle-Eastern and White combined for this
presentation. Participants choosing multi-race recategorized using rarest race methodology.
Source: OHA Office of Health Analytics, Oregon’s Health Care Workforce Reporting Program
Future Workforce of Primary Care Providers
High-quality primary care is the foundation of a high-functioning health care system. The
National Academies of Sciences, Engineering, and Medicine defines high-quality
primary care as “the provision of whole-person, integrated, accessible, and equitable
health care by interprofessional teams who are accountable for addressing the majority
of an individual’s health and wellness needs across settings and through sustained
relationships with patients, families, and communities.” To achieve high-quality primary
care and rebuild a strong foundation for the U.S. health care system, the 2021 report by
the National Academies of Sciences, Engineering, and Medicine recommended five
implementation objectives, including:
• Pay for primary care teams to care for people, not doctors to deliver
services. This includes payers shifting primary care payments from fee-for-
service (FFS) toward a hybrid of part-FFS-part-capitated models, CMS
increasing spending to primary care, and states facilitating multi-payer
collaboration and increasing primary care spending.
• Ensure that high-quality primary care is available to every individual and
family in every community. For example, the U.S. Department of Health and
Human Services should invest in the creation of new health centers, particularly
in areas that are underserved or have a physician shortage. Payers should also
ask all covered individuals to declare a usual source of primary care.
• Train primary care teams where people live and work. To promote a
community-oriented model and better align the workforce with the communities

76
they serve, state and federal governments should expand and diversify the
primary care workforce, particularly in areas that are underserved or have a
physician shortage.
• Design information technology that serves the patient, family, and the
interprofessional care team. The Office of the National Coordinator for Health
Information Technology (ONC) and CMS should develop the next phase of
electronic health record certification standards to improve user experience of
clinicians and patients
• Ensure that high-quality primary care is implemented in the United States.
Primary care research is currently less than 0.4% of research funding by the
National Institutes of Health. To support evidence for primary care practices,
research funding for primary care should be prioritized. Stakeholders at state and
federal levels should also track the progress of these implementation plans.
The Primary Care Collaborative described the medical home “as a model or philosophy
of primary care that is patient-centered, comprehensive, team-based, coordinated,
accessible, and focused on quality and safety.” In 2009, the Oregon Legislature created
the Patient-Centered Primary Care Home (PCPCH) Program through passage of House
Bill 2009 as part of a comprehensive statewide strategy for health system
transformation. The PCPCH is Oregon’s version of the patient-centered medical home
which is a model of primary care organization and delivery. At its heart, this model of
care fosters strong relationships with patients and their families to better care for the
whole person. Primary care homes reduce costs and improve care by identifying
problems early, focusing on prevention and wellness, and managing chronic conditions.
The PCPCH Program works with partners across Oregon to set the standards for high-
quality, patient-centered primary care. There are 35 standards which fall under six core
attributes of high-quality care (Figure 13.5). Practices attest to performing at varying
degrees—or “measures”—within each of these standards. The Program administers the
application, recognition, and verification process for practices applying to become
PCPCHs. There are over 600 primary care practices in Oregon that participate in the
PCPCH program, and more than three million people living in Oregon receive care at a
PCPCH.

77
Figure 13.5. Core attributes of patient-centered primary care homes
Source: Patient-Centered Primary Care Home Program: Recognition Criteria Technical Specifications and Reporting
Guide, Oregon Health Authority.
The 2020 PCPCH program standards include revisions emphasizing health equity, such
as a new standard for health-related social needs/social determinants of health
screening and intervention, a new standard for alternative visit type (e.g., in-home visits,
mobile vans, telehealth visits) to an in-person office visit, the addition of the adjective
“diverse” when describing patients, families, and caregivers in the technical
specifications, and including a Traditional Health Worker as a care team member when
describing the technical specifications.
In December 2020, OHA initiated a process to ensure that the PCPCH Program
supports a primary care system that addresses community-identified needs, especially
the needs of those who experience systemic racism, barriers in accessing care, and
health inequities. The PCPCH Program convened the Standards Advisory Committee
starting in August 2023 to advise OHA on the program standards and implementation to
further guide primary care transformation.
With the passage of House Bill 3261 the Oregon Legislature created the Health Care
Provider Incentive Fund to build health care workforce capacity in rural and medically
underserved parts of Oregon. The OHA’s Health Care Provider Incentive Program helps

78
support underserved communities in their recruitment and retention of high-quality
providers who serve patients regardless of their source of coverage or ability to pay.
(See the Investments in Workforce Development section).
Behavioral Health Providers
The Importance of Behavioral Health Providers
Behavioral health services, including mental health treatments, substance use disorder
services and gambling addiction treatments, are an important component of whole-
person care. Behavioral health services are provided by a variety of licensed, certified,
as well as practitioners with lived experience. Licensed providers include psychologists,
counselors and therapists, clinical social workers, clinical social worker associates, and
other licensed professions when the provider has a specialty in behavioral health (e.g.,
MDs with a specialty in psychiatry). Certified providers include Qualified Mental Health
Associates (QMHAs), Qualified Mental Health Professionals (QMHPs), Certified Alcohol
and Drug Counselors (CADCs) and Certified Recovery Mentors. There are other health
care professionals who may not have a specialty in behavioral health that are licensed
to provide prescription-based treatment for behavioral health conditions. This group
generally includes physicians (MD/DO), nurse practitioners (NP), and physician
assistants (PA). Unlicensed providers include trained or certified addiction specialists,
Traditional Health Workers, crisis counselors, case managers, and community support
personnel.
The behavioral health system has been faced with a workforce crisis. The 2019-20
Kaiser Family Foundation analysis found that 10.4% of adults in Oregon reported an
unmet need for mental health treatment in the past year, which was the 5
th
highest in
the country. According to the ECONorthwest survey of Oregon health care providers,
over 60% of respondents reported their organizations needed more behavioral health
providers, and 76% of respondents stated that it is very important to expand Oregon’s
capacity to educate, train, and develop more behavioral health professionals. A 2021
national survey conducted by the National Council for Mental Wellbeing found 78% of
its members had seen an increase in demand for behavioral health services and 97%
reported difficulties recruiting and retaining employees.
Behavioral Health Providers in Oregon
The 2022 Licensed Health Care Workforce Supply report by the Oregon Health
Authority (OHA) showed behavioral health professionals were the largest specialty

79
group with 13,919 licensees actively practicing (Table 14.1). Around 65% of behavioral
health professionals were counselors and therapists and licensed clinical social
workers. From 2018-2022, direct patient care FTE of counselors and therapists is
increasing more than 13% annually, licensed clinical social workers FTE is increasing
about 6% annually, and clinical social work associates FTE is increasing over 9%
annually (see the Health Care Workforce Reporting Program Data section).
Table 14.1. Behavioral health providers FTE by occupation in Oregon, 2022
Occupation
Direct patient
care FTE
Actively practicing
professionals
Counselors and
therapists
2,460
4,669
Licensed clinical
social workers
2,327
4,418
Psychologists
1,018
1,928
Clinical social work
associates
727
1,137
Physicians
511
829
Nurse practitioners
564
809
Naturopathic
physicians
54
104
Physician assistants
17
25
TOTAL
7,677
13,919
Source: OHA Office of Health Analytics. 2022 Oregon’s Licensed Health Care Workforce Supply.
Figure 14.2 shows the direct patient care FTE for behavioral health professional to
population ratios at state and county levels. The statewide ratio was 17.1 FTE per
10,000 Oregonians. The county ratios varied widely, ranging from 2.3 per 10,000
(Grant) to 31.9 per 10,000 (Multnomah).

80
Figure 14.2. Behavioral health professional FTE per 10,000 Population, 2022
Source: OHA Office of Health Analytics. 2022 Oregon’s Licensed Health Care Workforce Supply.
Figure 14.3 shows the licensed behavioral health provider FTE per 1,000 population by
service area, with an average of 1.48 FTE per 1,000 population in urban areas, and an
average of 0.54 FTE per 1,000 population in rural areas.

81
Figure 14.3. Behavioral health provider FTE per 1,000 population by service area
Source: The Oregon Office of Rural Health. The Oregon Area of Unmet Health Care Need report.
As illustrated in Figure 14.4, people of color are underrepresented in Oregon’s licensed
behavioral health provider workforce. (See the Health Care Workforce Reporting
Program Data section for detail by occupation) Data from the Mental Health and
Addiction Counseling Board of Oregon show that about 28% of unlicensed behavioral
health providers were people of color.

82
Figure 14.4. Race and ethnicity of behavioral health providers in Oregon
Note: Preliminary data provided from the 2022 Diversity of Oregon's Licensed Health Care Workforce Report Draft
(01/2023). Providers with missing data were excluded from the analysis. Some Workforce records are missing race
and ethnicity data because licensees declined to report race or ethnicity. Middle-Eastern and White combined for this
presentation. Participants choosing multi-race recategorized using rarest race methodology.
Source: OHA Office of Health Analytics, Oregon’s Health Care Workforce Reporting Program
The Oregon Health & Science University (OHSU)-Portland State University (PSU)
School of Public Health recently produced a report on substance use disorder services
in Oregon. Researchers estimated the number of services missing (refer to as “gaps in
services”) by comparing the recommended number of services to the estimated number
of existing services. Results showed an overall gap of 66% statewide between positions
filled and workers needed, with the largest gaps among Certified Prevention Specialists
(94% gap, an estimated 906 more positions needed) and Qualified Mental Health
Professionals (93% gap, an estimated 11,740 more people needed). The report also
found disparities in substance use disorder workforce compared to the demographics of
the state. The largest disparities were among people who are Hispanic or Latino/a/x,
with only 6.3% of non-prescribers and 0.4% of prescribers in the workforce compared to
13.2% of population in Oregon. The Mental Health and Addiction Counseling Board of
Oregon found in a survey that 21% of respondents were no longer working in the
behavioral health field or were performing limited duties.
Future Workforce of Behavioral Health Providers
A variety of factors contribute to shortages in the behavioral health workforce. The
recent Behavioral Health Workforce Report suggests that low reimbursement rates and
low wages are the major issues that make recruiting and retaining behavioral health
providers difficult. The report included recommendations for how to increase wages for
behavioral health providers. For example, the state can increase Medicaid fees for
organizations who pay a pre-specified minimum wage to health care providers. The
83
state can also fund retention and recruitment bonuses to directly increase wages. The
report also recommended making direct adjustment to reimbursement, such as
increasing fee-for-service (FFS) rates for behavioral health services, incentivizing a
fixed portion of the global budget to be allocated to behavioral health services,
expanding billable services to remedy disparities, and adjusting reimbursement rates for
client characteristics and social complexity. Other adjustments, such as reducing
paperwork burden and improving work environment, are also important to address
workforce shortages in behavioral health. Diversity in leadership could help to support
the recruitment and retention of a diverse workforce more broadly.
A recent report by the Coalition of Communities of Color found that people of color were
more likely to utilize culturally specific and community-based behavioral health services.
Their recommendations to improve behavioral health access included partnering with
culturally appropriate community-based partners, investing in culturally responsive
training for health care providers, and investing in diversifying the behavioral health
workforce.
There are several national and state efforts to address behavioral health workforce
shortages and improve diversity. The federal American Rescue Plan Act of 2021
includes a number of provisions to address the behavioral health workforce shortages. It
provides $800 million in funding increases for the National Health Service Corps, and an
additional $100 million for the Behavioral Health Workforce Education Training
Program. It allocates $80 million to the Health Resources and Services Administration
(HRSA) for behavioral health training to reduce and address suicide, burnout, mental
health conditions, and substance use disorder among health care professionals, and it
provides $122.8 billion in grants to state education agencies to support school-based
mental health systems.
A recent evidence review published by the Milbank Memorial Fund found that
conducting behavioral health visits by telehealth can reduce costs, and can be just as
effective as in-person care for certain behavioral health conditions. This review
suggested use of telehealth could potentially expand behavioral health treatment
options, especially for people living in underserved areas or who may have difficulties
with accessing an in-person visit. The 2022 report by the Medicaid and CHIP Payment
and Access Commission made recommendations to encourage health information
technology adoption in behavioral health. It recommended that the Secretary of the U.S.
Department of Health and Human Services direct the Centers for Medicare & Medicaid
Services (CMS), the Substance Abuse and Mental Health Services Administration
(SAMHSA), and the Office of the National Coordinator for Health Information
Technology (ONC) to develop joint guidance on how states can use Medicaid

84
authorities and other federal resources to promote behavioral health information
technology adoption and interoperability. It also recommended the ONC and SAMHSA
jointly develop a voluntary certification for behavioral health information technology.
In the 2021-2023 biennium, the Oregon Legislature allocated more than $1.35 billion in
funding to transform Oregon’s behavioral health system. Major categories of investment
include the behavioral health workforce, aid and assist population, behavioral health
crisis system, ballot measure 110, and behavioral health housing/social determinants of
health. Specifically, investment and legislation on the behavioral health workforce
include the Behavioral Health Workforce Initiative (House Bill 2949) and the Behavioral
Health Workforce Stability Grants (House Bill 4004).
Created through House Bill 2949 (2021) and subsequently House Bill 4071 (2022), the
Behavioral Health Workforce Initiative (BHWi) seeks to provide incentives to increase
the recruitment and retention of providers in the behavioral health care workforce with a
focus on equity and priority populations. The goal of the BHWi is to increase the
behavioral health system’s capacity to provide culturally responsive care that is deeply
embedded in equity-centered cultural responsiveness. The BHWi, when possible,
engages community (e.g., behavioral health providers, individuals with lived experience)
feedback with the intention of having those responses shape the direction of the work
done related to BHWi. House Bill 2949 (updated to House Bill 4071) allocates $60
million to develop a behavioral health workforce to licensed, certified and non-licensed
occupations though scholarships, loan repayment, and retention activities (e.g. retention
bonuses), and $20 million for a grant program to licensed and certified (e.g. Certified
Alcohol and Drug Counselors) behavioral health providers to provide supervised clinical
experience to associates or other individuals so they may obtain a license or
certification to practice.
House Bill 4004 aims to promote staff compensation and workforce recruitment and
retention. The legislation provides two specific investments:
1. $132.3 million General Fund investment for OHA to distribute grants to
behavioral health care providers to increase compensation to staff and pay hiring
and retention bonuses, if necessary, to recruit new staff or retain the providers’
staff. Grants to agencies were awarded in May of 2022.
2. Contract funds focused on nurses and behavioral health professionals to provide
care in adult and child residential behavioral health treatment facilities, opioid
treatment programs, withdrawal management programs and sobering centers.
State goals in the addiction area are outlined in the 2020-2025 Oregon Statewide
Strategic Plan from the Alcohol and Drug Policy Commission (ADPC). The strategic

85
goals include increasing system ability to recruit, develop, and retain a highly effective
workforce; and strengthening the workforce’s ability to implement culturally tailored and
linguistically responsive services/strategies across the lifespan for historically
underserved communities, such as seniors, people with disabilities, LGBTQ+, persons
of color, tribal nations, and rural Oregonians.
To support the ADPC’s strategic plan and address gaps in substance use disorder
workforce, the recent report produced by the OHSU-PSU School of Public Health calls
on the state to incentivize equitable distribution of linguistically and culturally relevant
services, and increase support for service organizations to employ and bill for certified
peer support specialists. The report also recommended provider training, telemedicine,
and mobile services to expand access to care for opioid use disorder.
House Bill 5202 (2022) included a recommendation for $42.5 million in state general
funds with intent to increase behavioral health reimbursement rates by an average of
30%, contingent on federal CMS approval. The $42.5 million in state general funds are
anticipated to have approximately $154.5 million total fund impact after the federal
Medicaid match. The Oregon Behavioral Health Loan Repayment Program supports
rural and urban underserved communities in the recruitment and retention of behavioral
health care providers. Oregon also has other investments and strategies to support
workforce development. (See the Investments in Workforce Development and
Workforce Resiliency sections).
Oral Health Providers
The Importance of Oral Health Providers
Oral health is critical to overall health. Oral health conditions such as gum disease are
associated with diabetes, heart disease, low birth weight babies, and certain types of
cancers. Only about 21% of Oregonians live in areas with fluoridated water, which is
critical for the prevention of tooth decay and caries. Poor oral health can lead to missed
school and work and can have a negative impact on overall well-being. People of color
and individuals with low incomes are disproportionately likely to experience poor oral
health. Oral health should be an essential component of comprehensive primary care.
However, oral health services have historically been delivered separately from medical
care, and most often the two systems do not communicate well. Approximately 44% of
children on Medicaid and over one-third of adult Medicaid beneficiaries have a
preventive dental visit in any given year. According to the CCO Performance Metrics
Dashboard, which reports on all Oregonians covered by Medicaid via CCOs, the

86
percentage of OHP members who received any dental service improved in 2021 to 28%
of adults, 54% of children ages 6-14, and 41% for children ages 1-5.
Oral Health Providers in Oregon
One of the key goals of Oregon’s coordinated care model is to integrate physical, oral,
and behavioral health care to treat the whole person. Recognizing the importance of
oral health across the lifespan, Oregon is one of only 23 states that offer extensive
dental benefits to all adults with Medicaid, as well as children. Dental benefits for
Medicaid adults are not required by federal law but can be offered as a state option, and
most states provide limited coverage, such as only extractions or emergency services.
Extensive coverage includes a comprehensive mix of services, including more than 100
diagnostic, preventive, and minor and major restorative procedures approved by the
ADA; and a per-person annual expenditure cap of at least $1,000. In the U.S.,
approximately 33% of dentists treat at least one Medicaid patient and those dentists
were more likely to practice in high-poverty or rural areas, and work in large practices.
Approximately 40% of Oregon dentists accept Medicaid patients with a quarter of those
comprising the majority of the Medicaid claims.
There are four main types of dental health providers in Oregon:
• Dentist (DMD/DDS) – Doctor of Medicine in Dentistry (DMD) or Doctor of Dental
Surgery (DDS) who can diagnose oral health disease, interpret x-rays, monitor
the growth and development of the teeth and jaws, and perform surgical
procedures on the teeth.
• Dental Therapist – Dental therapist with training and licensure can provide
preventative dental care, restorative dental treatment, and other educational,
clinical, and therapeutic patient services as part of a dental care team, including
the services described under ORS 679.621.
• Expanded Practice Dental Hygienist (EPDH) – Hygienist with the training and
experience to qualify for an expanded practice permit who can operate
independently without the direct supervision of a dentist; authorized to work in
specific settings such as community health clinics, nursing homes, and other
locations described in ORS 680.200.
• Dental Hygienist – Paraprofessional that works under the supervision of a
licensed dentist to provide preventive and therapeutic oral prophylaxis and
educate patients in dental hygiene.
• Dental Assistant – Unlicensed professional that helps with infection control by
sterilizing and disinfecting instruments, setting up instrument trays, and assisting
with dental procedures.
The 2022 Licensed Health Care Workforce Supply report by OHA estimated there were
2,424 dentists and 260 expanded practice dental hygienist actively practicing in Oregon.

87
The workforce FTE in Oregon increased slightly by 1.2% for dentists and 1.0% for
hygienists between 2016 and 2022 (see Figure 4.2 in the Health Care Workforce
Reporting Program Data section).
There is significant variation across the U.S. in the scope of activities of dental
hygienists. As of 2019, Oregon allows one of the broadest scopes of practice for dental
hygienists compared with other states. In Oregon, dental hygienists can formulate
treatment plans within the dental hygiene scope; prescribe, administer, and dispense
fluoride, topical medications, and chlorohexidine; and administer local anesthesia with
authorization from a dentist. Dental hygienists working in a public health setting can
provide sealants and prophylaxis without prior examination by a dentist.
Figure 15.1 shows the direct patient care FTE for oral health professional to population
ratios at state and county levels. The statewide ratio was 5.8 FTE per 10,000
Oregonians. The county ratios ranged from 0.7 per 10,000 (Morrow) to 9.2 per 10,000
(Hood River).
Figure 15.1. Oral health professional FTE per 10,000 Population, 2022
Source: OHA Office of Health Analytics. 2022 Oregon’s Licensed Health Care Workforce Supply.
The number of dentist FTE per 1,000 population by service area is shown in Figure
15.2. The average in urban areas is 0.58 dentist FTE per 1,000 population, and the
average in rural areas is 0.32.

88
Figure 15.2. Dentist FTE per 1,000 population by service area
Source: The Oregon Office of Rural Health. The Oregon Area of Unmet Health Care Need report.
As illustrated in Figure 15.3, Oregon’s oral health providers are less racially and
ethnically diverse than the general population with Latino/a/x, African American/Black,
American Indian/Alaska Native, and Native Hawaiian/Pacific Islander providers being
underrepresented. (See the Health Care Workforce Reporting Program Data section for
detail by occupation).

89
Figure 15.3. Race and ethnicity of oral health providers in Oregon
Note: Preliminary data provided from the 2022 Diversity of Oregon's Licensed Health Care Workforce Report Draft
(01/2023). Providers with missing data were excluded from the analysis. Some Workforce records are missing race
and ethnicity data because licensees declined to report race or ethnicity. Middle-Eastern and White combined for this
presentation. Participants choosing multi-race recategorized using rarest race methodology.
Source: OHA Office of Health Analytics, Oregon’s Health Care Workforce Reporting Program
Future of the Oral Health Workforce
Recommendations for the future of the oral health workforce come from Oregon
workforce development and needs reports, recommendations from external reports of
national organizations, and from OHA staff and study authors. Recommendations for
the oral health workforce include:
• Increase student engagement into oral health education programs.
• Identify pathways for dental hygienists to grow into dental therapists.
• Recruit oral health care professionals who identify as Hispanic/Latino/a/x,
American Indian/Alaska Native, and Black/African American.
• Allow flexibility in state licensing for travelling providers or those out of state.
• Reach underserved populations through provider incentives, tiny mobile
dentistry, and teledentistry.
In Oregon, there is only one post-baccalaureate program for pre-dentistry, located at the
University of Oregon, Health Professions Program. This public program serves students
who have already received degrees in the sciences but intend to extend their education
by taking additional advanced coursework. Oregon does not have any post-
baccalaureate programs that serve students who have received non-science degrees or
who have not completed sufficient coursework, or programs that have an explicit focus
on helping students from underrepresented populations matriculate into health
professions education programs. Research has shown that these programs can help
address oral health disparities by improving the diversity of the dentist workforce.

90
OHA’s Dental Pilot Project Program encourages the development of innovative
practices in oral health care delivery systems to improve care to populations with the
least access to dental care and the highest disease rates. One recent program trained
dental hygienists to become dental therapists through a unique one-year education
program that allowed the dental hygienists to complete the dental therapy education
program while they maintained their current employment as a dental hygienist. Currently
dental therapists are only being licensed through training in the dental pilot project
program, as there are currently no CODA-accredited dental therapy schools in Oregon.
Oregon’s oral health providers are eligible for several workforce development programs
including loan forgiveness, loan repayment programs, tax credits which provide the
benefit to providers in underserved areas of the state or who work with underserved
Patients such as those on Medicaid and Medicare. For example, the Loan Repayment
program was designed to help support underserved communities in the recruitment and
retention of health care providers. To date, 53 dentists and 11 expanded practice dental
hygienists in Oregon have participated. Please see figure 15.4 which maps oral provider
loan repayment recipients in Oregon. Please refer to the Investments in Workforce
Development section in this report for more details about the programs listed above.

91
Figure 15.4. Oral Health Provider loan repayment recipients, 2018-2022
Source: Evaluation of the Effectiveness of Health Care Provider Incentive Programs in Oregon, 2023, Oregon Health
Authority
In 2022, OHA received an Oral Health Workforce Grant from the Health Resources &
Services Administration (HRSA) for $1.6 million over the next four years. These grants
help states develop and implement innovative programs to address dental workforce
needs appropriate to the state’s individual needs. This grant aligns with OHA’s 10- year
goal of eliminating health inequities. OHA’s grant focuses on Josephine, Jackson, Lane,
and Douglas Counties which aligns with some of the most underserved areas and has
three objectives:
1) Expansion of teledentistry by funding community-based organizations to
integrate teledentistry services into their facilities, specifically by allocating funds
towards the procurement of teledentistry equipment and recruitment incentives
for providers.

92
2) Partner with dental care organization(s) to maintain and place mobile dental vans
to offer new patient exams, x-rays, intraoral photos, charting, and preventive
service (dental cleanings for patients of all ages, sealants, fluoride, periodontal
maintenance, scaling and root planning, fillings, and extractions)
3) Partner with OHSU School of Dental Public Health to incorporate the ECHO
program into Dental Preceptor sites to expand preceptor capacity and incentivize
more dentists to become preceptors.
Some oral health services may be delivered by telehealth, sometimes referred to as
teledentistry. For some oral health ailments, teledentistry can allow dental professionals
such as expanded practice dental hygienists to conduct examinations and send the data
to a dentist to remotely review records and diagnose patients over video or using store
and forward technology. If a procedure or further examination is necessary, patients are
referred for an in-person visit with the dentist. A dental hygienist must have an
Expanded Practice Permit in order to render services via teledentistry. Expanded
Practice Dental Hygienists need training to use the technology to submit oral health
assessments to a dentist and conduct x-rays remotely.
Long-Term Care Workforce
Long-term Care Settings in Oregon
Many older adults and people with disabilities need long-term services and supports,
which include: assistance with incidental activities of daily living such as housekeeping,
shopping, and meal preparation; assistance with activities of daily living such as
bathing, dressing, or transferring from bed to chair; medication management or
assistance with other medical needs; and rehabilitative services.
Oregon offers long-term services and supports in a continuum of long-term care
settings:
• In-home care, primarily for assistance with incidental activities of daily living and
activities of daily living. This assistance is often provided by family members or
other informal caregivers, but many Oregonians also receive assistance from
paid caregivers.
• Independent living facilities, which have separate apartments but offer
housekeeping and dining services. Residents may also receive in-home care
services.
• Community-based care facilities that include assisted living, residential care, and
adult foster homes. Community-based care residents may require more

93
assistance with activities of daily living than in-home consumers, and often with
medication management.
o Some residential care or assisted living facilities with specialized facilities
and an additional endorsement provide memory care to residents with
advanced dementia.
• Intermediate Care Nursing Facilities serve people, including those with
developmental disabilities, who need access to 24-hour nursing care.
• Skilled nursing facilities serve residents needing more intensive nursing services
in addition to activities of daily living assistance. In Oregon, skilled nursing
facilities emphasize post-acute care, often including physical, occupational, or
speech therapy, for residents recently discharged from hospitals.
Each of these long-term care settings is progressively more expensive. Medicare only
pays for short-term home care or post-acute care in skilled nursing facilities, while
Medicaid funds long-term services and supports for low-income Oregonians. Most long-
term services and supports recipients also prefer to be in least intensive setting that
meets their needs. Oregon leads the nation in accomplishing this, allocating a higher
proportion (88%) of its Medicaid long-term services and supports spending to home and
community based services than any other state. These proactive long-term services and
supports policies are administered by the Oregon Department of Human Services
(ODHS).
Oregon’s Long-Term Care Workforce
Workers who provide long-term services and supports in Oregon must meet different
levels of certification, depending on the setting in which they work:
• Home care workers, including personal support workers and personal care
attendants, must have 12 hours or orientation and training (with four additional
hours if they administer medications) and complete six hours of continuing
education annually.
• Community-based care facility staff must complete a training program at their
facility and demonstrate proficiency in topics such as resident care services,
safety, and dementia needs. Twelve hours of annual continuing education are
required.
• Certified Nursing Assistants (CNA) in skilled nursing facilities must complete 155
hours of training, pass an examination, and complete 12 hours of continuing
education annually.

94
Recent analysis by PHI showed that there were 47,850 members of Oregon’s direct
care workforce in 2021, including 35,390 personal care or home health aides and
12,460 CNAs
1
. Among this workforce:
• Eight in 10 are female
• One in three is a person of color
• One in six is an immigrant
• Two in five live in households with incomes less than 138% of the Federal
Poverty Level
• One in three receives some sort of public food and nutrition assistance
• One in four is insured by Medicaid, and one in eight (almost three times the
statewide average) is uninsured
The Oregon Health Care Association (OHCA) estimates that the direct care workforce
provided care to approximately 75,000 Oregonians in 2021. This population is
increasing rapidly: the number of Oregonians aged 65-84 is expected to grow by 17%
by 2030, and the number age 85 and older (who are most likely to receive long-term
services and supports) by 26%. As a result, the need for home care aides and personal
care workers is expected to grow 29% by 2030.
Recruiting and retention challenges in Long-Term Care. The direct care workforce
in long-term care faced numerous severe challenges nationwide even before the
COVID-19 pandemic. As described above, direct care workers in long-term care are
disproportionately women of color and likely to live in or near poverty and are often
immigrants. The Economic Policy Institute recently documented that direct care workers
in community-based care facilities and skilled nursing facilities are paid wages one-third
lower than the national average, and are less likely than the average worker to receive
employer-sponsored benefits or be represented by a union, but more likely to work
multiple jobs. The Economic Policy Institute also found that home care workers have
similarly low pay levels. A 2021 Washington state report showed that direct care
workers in long-term care are paid less than for similar positions in hospitals, and that
some categories of direct care workers had begun to shrink even before the COVID-19
pandemic. PHI further explains that direct care work in long-term care has a high risk of
physical injury and requires significant relational skills and emotional labor, yet offers
limited opportunity for career advancement. Finally, low pay and challenging work
conditions contribute to high turnover among direct care workers.
Despite these challenges, long-term care facilities’ and home care agencies’ ability to
raise direct care workers’ pay is limited by low Medicaid reimbursement levels as well
1
Not all Oregon CNAs work in LTC, but the available analyses do not provide the breakdown across workforce
segments.

95
tight family budgets for home care. Some analysts further note that “care work” in long-
term care, child care, and teaching is systematically undervalued, in large part because
it is most often performed by women of color and immigrants.
Long-Term Care during the COVID-19 pandemic. The COVID-19 pandemic
exacerbated an ongoing workforce crisis in long-term care, nationwide and in Oregon.
In the early months of the pandemic, half of all COVID-19 deaths nationally were among
long-term care facility residents and staff. Home care workers were also at very high
risk of COVID-19 exposure because they could not obtain adequate personal protective
equipment. Mortality in long-term care facilities dropped sharply in early 2021 as most
residents and staff were vaccinated, but by January 2022, long-term care facilities still
accounted for one-fourth of cumulative COVID-19 deaths.
Long-term care employment dropped dramatically at the beginning of the COVID-19
pandemic, but unlike other segments of health care, the size of the long-term care
workforce never recovered. As of March 2022, employment in skilled nursing facilities
remained 15% lower than in February 2020, and assisted living employment was 6%
lower, with a total of 400,000 long-term care jobs lost nationwide. Analyses by UCSF
and PHI showed that direct care workers who lost jobs during the early stage of the
pandemic did not return, and were not replaced by workers who had lost jobs in other
occupations. One reason appears to be that employers in other occupations (such as
food preparation or retail sales) were able to raise wages to attract workers, while long-
term care employers could not.
By mid-2022, 9 in 10 skilled nursing facilities nationwide were experiencing staffing
shortages, and 6 in 10 were limiting new admissions. Skilled nursing facilities report
operating costs increase of 40% in the past year and nearly all have increased workers’
pay, but 7 in 10 still report being unable to find interested or qualified candidates.
Although home health employment had recovered to the pre-pandemic level, employers
still report major challenges in hiring enough home care workers.
Long-term care facilities in Oregon face these same COVID-19 impacts, struggling with
staff shortages and rising costs. As described in the Nursing section of this report,
Oregon skilled nursing facility’s’ inability to admit new patients has created capacity
shortages at many hospitals. Pursuant to Senate Bill 703, Portland State University
studied direct care worker compensation in Oregon’s assisted living and residential care
facilities; findings will be available in early 2023.
Several federal and Oregon initiatives were implemented in response to COVID-19’s
impact on long-term care. The American Rescue Plan increased Medicaid funding for

96
home & community based services by 10% from April 2021 through March 2022. The
federal Build Back Better legislation proposed in 2021 would have provided substantial
additional funding to support the long-term care workforce, but was never passed by the
Congress. In 2021 Oregon established a Nurse Crisis Team to provide nurse and
medication technician staffing to skilled nursing facilities that were unable to accept new
patients. In July 2021, the Oregon Legislature passed a Long-Term Care Investment
Package that included funds to increase wages for community-based care facility and
skilled nursing facility workers, as well as a $12.2M budget note to enhance workforce
development and training. Those workforce efforts are being led by a new Strategic
Initiatives Unit within ODHS. This unit is building collaborations among ODHS, OHA,
and external stakeholders to grow the direct care workforce and enhance its well-being.
The largest effort is financial support for the RISE Partnership to expand its
apprenticeship training program for CNAs. Support will also be provided for the
NurseLearn program to train community health nurses, the Oregon Care Partners
training clearinghouse for family caregivers and direct care workers, and other training
and well-being programs.
Future of the Long-Term Care Workforce
A range of long-term strategies for states to strengthen the direct care workforce have
been proposed, perhaps most comprehensively by PHI. Two crucial strategies have
been endorsed in reports by organizations that include the National Governors
Association, National Conference of State Legislatures, National Academy of State
Health Policy, UCSF, Leading Age:
• Increase compensation for direct care workers, many of whom do not currently
earn a living wage and can often find better-paid work outside long-term care.
The biggest constraint on direct care worker compensation is low reimbursement
by Medicaid, which funds more than half of long-term services and supports
spending nationwide. Increasing Medicaid reimbursement will be difficult, but
Leading Age has outlined the benefits of doing so, and example approaches in
other states are described by the Center for American Progress and the National
Governors Association.
• Streamline and strengthen training programs and career growth pathways for
direct care workers. For example, the Oregon Home Care Commission is
currently redesigning its website to make it much simpler for prospective home
care workers to apply for positions, and offers increased pay for higher levels of
certification. Apprenticeship programs that combine training and paid work (of
which the RISE Partnership CNA apprenticeship is an example) can support
individuals newly entering the direct care workforce. Washington state has
proposed other innovative approaches, such as online simulation training and an
explicit CNA-to-LPN career ladder.

97
In addition to better pay and benefits, providing higher quality work environments can
help employers to motivate and retain direct care workers. These work environment
improvements include team-based care, providing high-quality supervision, and
delegating tasks from nurses to direct care workers. Concrete approaches to making
direct workers more valued have been outlined by Leading Age, the Commonwealth
Fund, and PHI. The Oregon Legislature, ODHS, and other state agencies can facilitate
long-term care employers’ implementation of such approaches.
As described above, Oregon is currently implementing short- and medium-term
strategies to mitigate long-term care workforce shortages, but a higher and sustained
level of investment—ideally in selected strategies that are shown to be effective—will be
needed to grow and maintain a direct care workforce to meet the state’s future demand
for long-term services and supports in coming decades. This will require coordinated
action by Oregon’s Legislature, ODHS and other state agencies, labor organizations,
and long-term care employers.
Public Health Workforce
Importance of the Public Health Workforce
Public health promotes and protects the health of people and the communities where
they live, learn, work and play. The Oregon public health system includes federal, state,
and local agencies, private organizations and other diverse partners working together to
prevent disease, protect people from harm, and promote actions that make us healthier.

98
Figure 17.1. The public health system in Oregon
Source: Oregon Health Authority, Public Health Division
Note: abbreviations in figures include CBO – community-based organizations, RHEC – regional health equity
coalitions, LPHA – local public health authority, OHA – Oregon Health Authority
Public Health Workforce in Oregon
Governmental public health is a network of federal, state, and local health authorities,
and government-to-government relationships with federally recognized Tribes. Oregon
has a decentralized public health system, which means that local and tribal
governments have authority over most public health functions in their jurisdictions. The
public health system works with community-based organizations to ensure that
communities are at the forefront of efforts to improve health and that public health
interventions are reaching those who experience a disproportionate burden of death
and disease.
Both local public health authorities and the state directly fund community-based
organizations and regional health equity coalitions. Oregon's Public Health Advisory
Board (PHAB) serves as an advisory body to the Oregon Health Authority (OHA).
OHA’s Public Health Division achieves its mission through work organized in three
centers. The Center for Prevention and Health Promotion houses programs to
implement policies, systems and environmental changes designed to prevent chronic
diseases and injury and support improved health across the lifespan. The Center for
Health Protection includes public health regulatory functions, such as licensing health
care facilities, inspecting restaurants and public water systems, as well as
environmental health protections. The Center for Public Health Practice houses
programs that protect the public from communicable diseases and prepare and respond
to public health emergencies. Finally, the Office of the State Public Health Director
provides leadership, fiscal and operations support, as well as coordination of policy and

99
partnership activities across the public health system. The OHA Public Health Division's
Policy and Partnerships unit provides technical assistance and consultation to local
public health authorities and Tribes, and coordinates local public health authority
reviews.
There are approximately 1,000 current staff within the OHA Public Health Division.
The Public Health Workforce Interests and Needs Survey (PH WINS) is a nationally
representative survey about the governmental public health workforce. The survey was
conducted during OHA Public Health Division's response to COVID-19 which included
the addition of hundreds of temporary and limited duration positions; with more of those
positions working in emergency response and communicable disease investigation and
control. Approximately 39% of OHA Public Health Division's staff completed the PH
WINS survey in 2021. Approximately 78% of OHA Public Health Division's staff identify
as female which is comparable to the national workforce. However, more OHA Public
Health Division's staff identify as White (78%) and have a higher percentage between
the age of 31-50 (64%) compared to the national workforce. Among OHA Public Health
Division staff, 28% have a public health degree compared with 14% of the national
public health workforce. More OHA Public Health Division employees hold a master’s
degree (48%) or doctoral degree (7%) compared to nationally (31% and 6%
respectively).
The majority of OHA Public Health Division staff are full-time (97%) and 63% work in
public health sciences such as program staff, epidemiologists, and contact tracers
compared with 43% of national workforce. At OHA Public Health Division, 49% had
served their agency for 5 years or less like the national level. At OHA Public Health
Division, 28% are considering leaving their organization within the next year and 13%
are planning to retire within the next 5 years. Top reasons for leaving work include
overload/burnout, lack of support, lack of advancement opportunities, organizational
culture, job satisfaction, stress, supervisor satisfaction. The majority of OHA Public
Health Division staff are satisfied with their job (79%), their organization (73%), and their
pay (67%.). Top reasons for staying include benefits, job stability, and flexibility. OHA
Public Health Division staff are well trained in their programmatic area, but want more
training in justice, equity, diversity, inclusion, and cross-sectoral partnerships.
Nationally, 25% of the public health workforce rate their mental health as either “poor” or
“fair,” but this percentage is higher in Oregon with 33% of OHA Public Health Division
staff rating their mental health as either “poor” or “fair.” More details about burnout and
post-traumatic stress are discussed in the Workforce Resiliency section in this report.
For intentions to leave the workforce following COVID-19, refer to the Impacts of
COVID-19 section of this report.
100
Tribal Public Health
There are nine federally recognized tribes in Oregon. Tribal governments are separate
sovereign nations with powers to protect the health, safety, and welfare of their
members and to govern their lands. OHA Public Health Division provides technical
assistance to tribal partners and supports tribes with Public Health Modernization
funding. Tribes can apply for funding opportunities from OHA. In 2020, the Northwest
Portland Area Indian Health Board (NPAIHB) received funding from the Centers for
Disease Control and Prevention’s (CDC’s) National Public Health Improvement Initiative
program to increase performance management capacity and improving the ability to
meet national public health standards.
Oregon’s Local Public Health Authorities
At the local level, there are 33 local public health authorities: 27 are part of county
governments; one serves a three-county district; and five are public-private
partnerships. Two of Oregon’s counties, Wallowa and Curry, ceded local authority back
to OHA in 2018 and 2021 respectively. Local public health authorities are funded
through a combination of county dollars, investments approved by the Oregon
Legislature, and grants through state and federal governments. Over half of the funding
to local public health authorities is to support Women, Infants, and Children (WIC),
family planning, and school-based health centers. The Coalition of Local Health Officials
(CHLO) is an association among local public health authorities in Oregon and recently
completed a workforce development report. As of August 2021, Oregon’s local public
health authorities workforce was made up of 1,144 FTEs for non-COVID roles. Between
March 2020 and August 2021, local public health authorities FTE increased 67% by
adding 761 FTE for the COVID-19 response for a total workforce of 1,905 FTE.
Approximately 22% of this total FTE serve in rural areas. Small health departments
(defined as those serving less than 50,000 people) make up 61% of all health
departments, but only serve 9% of the population. The local workforce was divided
between nurses (13.4%), epidemiologists (3.4%), and environmental health specialists
(5.4%), and 77.8% other. The average starting wage across all counties is $29.36 per
hour for public health nurses, $45.28 per hour for health administrators, $30.39 per hour
for epidemiologists, and $26.33 per hour for environmental health specialists. There is a
wide range of pay across counties especially for public health nurses.
Community-Based Organizations
OHA recognizes the essential role of community-based organizations in community-
driven, culturally, and linguistically responsive public health service. OHA
has funded more than 170 community based organizations to support culturally and
linguistically responsive services as a part of the state’s COVID-19
response. Community based organizations have been funded to work in: community

101
engagement, education, and outreach; contact tracing; and social services and
wraparound supports. OHA funded 153 community-based organizations to help
eliminate health inequities by 2030 which reflects a coordination of eight different OHA
programs coming together to center health equity and community priorities in one
centralized funding opportunity.
Future of the Public Health Workforce
The Public Health infrastructure has been underfunded for years before the COVID-19
pandemic. In 2017, the Oregon Legislature began to invest in public health through the
Public Health Modernization funding. This funding was for Public Health Modernization
to expand each accomplishment in public health into long-term systems change. Since
this initial investment, the Oregon Legislature has increased the funding amounts with
increased investments given to local public health authorities, Tribes, and community-
based organizations. Figure 17.2 below for details of Public Health Modernization
funding from 2017-2023. The request for the 2023-2025 biennium Public Health
Modernization funding request is for $286 million with about $100 for local public health
authorities, $103 million for community-based organizations, $30 million for tribes, and
$42 million for OHA. Specific activities are identified for investing in the development
and retention of the public health workforce that is representative of and from the
community served.
Figure 17.2. Legislative Investment in Public Health Modernization, 2017-2023
Source: Oregon Coalition of Local Health Officials. (2022)
In addition, the OHA Public Health Division has also applied for a $32 million CDC
public health infrastructure grant, with some funding focused on workforce development.
This funding will enable OHA, tribes, local public health authorities, and community-

102
based organizations to hire and retain public health workforce to strengthen
foundational capabilities. This funding would support 8 new positions and extend
support for 1.5 positions at OHA, and provide $23 million to tribes, local public health
authorities, and community-based organizations. These investments would be used to
cultivate and retain a diverse public health workforce reflective of the communities that
public health serves, as well as workforce development needed to respond to health
inequities with community-led approaches.
Lack of epidemiologists is a problem statewide. Of the 28 local public health authorities
that provided data in the CHLO report, only 12 reported having epidemiologists on staff.
Local public health authorities serving counties with less than 50,000 people have even
more limited epidemiological capacity. Several strategies to address this shortage
includes targeting or incentivizing recruitment of epidemiologists, sharing
epidemiologists across regions, or contracting out for services. OHA Public Health
Division contracted with the Oregon Health Sciences University (OHSU), University of
Oregon, and Oregon State University’s (OSU) Surge Bench to embed highly trained
students within OHA’s COVID Response and Recovery Unit to perform key
epidemiological activities like case investigation, contact training, data entry and quality
assurance, and vaccine outreach. Since July 2020, the OSU Surge Bench, for example,
has provided over 15,000 hours of COVID-19 response work in 24 different local public
health authorities, helping to address key workforce gaps during COVID surges.
Evaluation results indicate that Surge Bench students are more realistically prepared for
their future careers and improve the diversity of the public health workforce. Clinical
student affiliate agreements were in place with several schools of nursing across the
state to support clinical functions in the field COVID testing and vaccine response.
Additional funding of the program would continue this workforce pipeline and support
public health activities across the state.
Post COVID-19, the federal, state, and local governmental public work force needs at
least 80,000 additional FTE to deliver core foundational public health services.
Challenges to recruiting public health professionals include having a limited pool of
diverse and qualified applicants, offering competitive pay, and having limited affordable
housing options in their counties. Interviews with local health departments in Oregon
stated that the lack of affordable housing a major barrier to recruiting new, non-local
workers to work in health departments. Recruiting staff who identify as a person of color
or who are bicultural or bilingual is especially difficult in smaller counties.
Recommendations for the public health workforce come from reports form national
organizations, reports from Oregon organizations such as the Coalition of Local Health

103
Officials, recent survey data gathered from Oregon’s public health workforce, and from
OHA experts and study authors. Recommendations include:
• Increasing the workforce of “home-grown” professionals from within communities.
Strategies may include working with academic institutions at all levels (K-12,
community colleges, undergraduate programs, and graduate programs) to
increase awareness around public health careers, to recruit for internships and
jobs.
• Identifying online public health education, including certificates without needing a
bachelor’s or master’s degree.
• Providing more training in local public health practice, cross-sectional
partnerships, and justice, equity, inclusion, and diversity.
• Recruiting and retaining staff using strategies such as salary adjustments,
promotion opportunities, weighing lived experience over education to increase
diversity, allowing work experience to be substituted for advanced degrees,
reducing barriers for out-of-state professionals, flexible/remote work policies, job
rotations, and facilitating time off and backup support for time off.
• Supporting existing staff by creating local caucuses and support groups for local
and regional public health staff especially those who have few local counterparts
and/or those who wish to advance their careers. Oregon’s public health
workforce needs support from their elected officials and their community.

104
Conclusions/Recommendations
Improve the diversity of health care providers
Oregon must have a more diverse workforce to achieve the strategic goal of
eliminating health inequities. Recommendations include:
• Increase investments in training, recruiting, and retaining health care workers
who can provide culturally and linguistically responsive care.
• Reduce barriers to entry and advancement for people of color in the workforce.
• Engage communities in shared decision-making around the future of their health
care workforce.
• Use the Health Equity Framework to infuse equity into workforce development
policies and programs to meet OHA’s 10-year goal to eliminate health inequities.
Improve the supply and distribution of the health care workforce
The COVID-19 pandemic exacerbated Oregon’s shortage of many types of health
care providers, especially in rural areas. Recommendations include:
• Continue to fund financial incentives to increase opportunities for training and
education, such as those in the Health Care Provider Incentive Program.
• Invest in workforce training through the public workforce system and allied health
educational partners.
• Address other factors that influence workforce recruitment and retention—
especially in rural areas—such as housing cost and supply, economic
opportunities for partners/spouses, and quality of K-12 education.
• Ensure accountability of incentive programs by evaluating items such as cost-
per-placement year, multiplier effects of incentives, and retention effectiveness
over time for communities experiencing inequities.
• Support telehealth with clear, flexible policies and adequate reimbursement,
which can increase access in underserved areas.
Enhance the resiliency and well-being of the health care workforce
Health care worker burnout exacerbates workforce shortages, quality of care,
health inequities, and health disparities. Addressing workforce wellness and
resiliency is essential and will require collective action to be effective.
Recommendations include:
• Coordinate collective actions from public and private stakeholders, as well as
community partners, to cultivate a health system that supports health care
workers, including action to create trauma-informed, anti-racist workplaces.
• Invest in assessment and research to inform evidence-based and practice-based
strategies to optimize health care workforce well-being.

105
• Increase health care workforce diversity, and make workplaces more welcoming
for diverse providers.
• Invest in efforts to reduce stigma and support health care workers’ seeking
mental health care.
• Invest in interventions to address burn out with focus on societal, cultural,
structural, and organizational factors, and sustain a positive work environment
and culture.
Expand training/education and career pathways for many segments of
the health care workforce
Expanding training is especially urgent for segments of Oregon’s workforce
where shortages are most acute, such as behavioral health and long-term care.
Education and clinical training opportunities should be expanded for all types of
health care providers. Recommendations include:
• Invest in Oregon’s education pipeline for health care professionals, including K-
12 outreach, community colleges, bachelors, online certificate and education
programs.
• Ensure adequate numbers of faculty and clinical training placements for nurses
and other licensed professionals.
• Establish and fund clear pathways for positions that do not have defined career
ladders based on licensure, including parallel training and work, with a
progression to increased pay and responsibility based on training and
experience.
• Invest in a mix of reliable and new strategies to enhance training opportunities for
other segments of the workforce, including traditional health workers, primary
care providers (physician and non-physician), and dentists and dental therapists.
Expand use of care delivery models that improve patient access and
promote workforce retention
Although Oregon has been a leader in transforming its health care delivery
system, innovative care models can be expanded to improve patients’ access to
care, promote culturally and linguistically appropriate care, and increase
workforce satisfaction. Recommendations include:
• Expand telehealth, coupled with health care interpreters, to improve access to
culturally specific or linguistically appropriate services.
• Continue to invest in the integration of physical, behavioral, and oral health care
delivery.
• Encourage team-based models and delegation of tasks to allow for more
effective and efficient service delivery.
106
• Work with payment models and policy revisions to further expand primary care
teams to provide care during evenings and weekends.
Increase health care systems’ use of community-based health care
providers
Traditional health workers—including peer wellness specialists—and health care
interpreters come from and/or share common lived experiences with their local
communities. OHA should continue to reduce barriers to recruit and retain this
workforce. Recommendations include:
• Find ways to increase compensation for many health professionals, in particular
traditional health workers—including peer wellness specialists—and health care
interpreters who are underpaid and are underrepresented in certain regions of
the state and among persons of color relative to Oregon’s population.
• Improve outreach to all counties across the state, and deploy strategies to
recruit, train and employ providers of color and from other underrepresented
communities in these fields.
Improve data collection to promote evidence-informed strategies and
diversify the health care workforce
Data collection must be improved to help improve the understanding of
challenges to the workforce. Recommendations include:
• Ensure that standardized REALD (race, ethnicity, language, and disability) and
SOGI (sexual orientation and gender identity) data are collected for all Oregon
providers and patients.
• Invest in collecting data that improve the understanding of a range of social and
economic factors that influence workforce recruitment and retention.
• Invest in collecting data that improve the understanding of challenges to clinician
well-being and inform strategies to support workforce resiliency.
• Expand data collection to include more provider types that incorporate
community-defined evidence practices and improve consistency of data
collection over time.
Conclusion
Workforce shortages and lack of diversity in many areas of the health care workforce
are a national problem experienced in Oregon, stemming from historic underinvestment,
current economic and social forces, and systemic racism. There are barriers to entry
and advancement for people of color in the health care workforce, and to receiving
culturally and linguistically responsive care for people experiencing health inequities. In
107
order to stabilize, expand, and diversify Oregon’s health care workforce so that it can
deliver culturally responsive, effective health care services to all:
• Some professions need increased compensation to attract new individuals and
increase retention
• Many professions with unclear career pathways need better, focused paths for
increasing skills, pay, and impact
• All professions need more support around resiliency and well-being
All the report’s recommendations warrant action by government and non-governmental
entities to ensure Oregon has the workforce it needs to deliver on the commitments of
optimal health for everyone and the elimination of health inequities.
108
Acknowledgments
• Rick Allgeyer, Research Director, Oregon Center for Nursing
• Sara Beaudrault, Public Health Modernization Lead, Public Health Division, Oregon
Health Authority
• Cara Biddlecom, Deputy Health Director, Public Health Division, Oregon Health
Authority
• Jana Bitton, Executive Director, Oregon Center for Nursing
• Mackenzie Carroll, Legislative Lead for Health Policy and Analytics Division, Oregon
Health Authority
• Kari Christensen, Workforce Development Strategist, Office of the State Public
Health Director, Oregon Health Authority, Public Health Division
• Rachel Currans-Henry, Strategic Initiatives Administrator, Oregon Department of
Human Services – Aging and People with Disabilities
• Andy Davis, Lead Analyst of Health Care Workforce Reporting Program, Oregon
Health Authority
• Chris DeMars, Director of Delivery System Innovation Office, Oregon Health
Authority
• Victoria Demchak, Workforce Diversity Coordinator, Office of the State Public Health
Director, Oregon Health Authority
• Lorelle Dennis, Policy Analyst, Health Policy and Analytics Division
• Millie Dibble, Health Policy Project Manager, Oregon Health Authority
• Danna Drum, Local and Tribal Public Health Manager, Office of the State Public
Health Director, Oregon Health Authority
• Jen Eisele, Administrative Specialist 2 with behavioral health workforce initiative
team, Oregon Health Authority
• Jack Elliott, Community Leadership Council Coordinator, The Behavioral Workforce
Initiative, Oregon Health Authority
• Leah Festa, Community Programs Lead, Oregon Health Authority
• Neelam Gupta, Director of Clinical Supports, Integration, and Workforce Unit,
Oregon Health Authority
• Amy Harris, Patient Centered Primary Care Home Program Manager, Oregon
Health Authority
• Anna L. Johnson, Senior Economic Analyst, Research Division, Oregon
Employment Department
• Sarah Kowalski, Dental Pilot Project Program, Oregon Health Authority
• Kusuma Madamala, Public Health Systems and Services Researcher, Program
Design & Evaluation Services, Oregon Health Authority – Public Health Division and
Multnomah County Health Department
• Jon McElfresh, Oral Health Workforce Grant Coordinator, Oregon Health Authority
• Craig Mosbaek, Economist and Health Policy Analyst, Health Policy and Analytics
Division, Oregon Health Authority
109
• Abdiasis Mohamed, Traditional Health Worker Program Coordinator, Oregon Health
Authority
• Bhagavati (Adrienne) Mullock, Workforce Resilience Analyst, Strategic Initiatives
Oregon Department of Human Services – Aging and People with Disabilities
• Emerson Ong, Office of Rural Health, Oregon Health & Science University
• Marc Overbeck, Primary Care Office Policy Lead, Health Policy and Analytics
Divisions, Oregon Health Authority
• Jason Payton, Occupational Economist, Oregon Employment Department
• Amanda Peden, Senior Health Policy Analyst, Oregon Health Authority
• Wendy Polulech, Operations Strategic Manager, Office of the State Public Health
Director, Oregon Health Authority
• Alayna Schoblaske, General Dentist & Dental Director, La Clinica, East Medford
Dental Clinic
• Frederick D. Staten, Behavioral Health Workforce Development Manager, Oregon
Health Authority
• Sarah Wetherson, Transformation Analyst, Oregon Health Authority
• Kweku Wilson, Data Analytics Manager, Oregon Health Authority
110
List of Abbreviations
• ASL, American Sign Language
• ADN, Associate Degree of Nursing
• ADPC, Alcohol and Drug Policy Commission
• ASL, American Sign Language
• BHWi, the Behavioral Health Workforce Initiative
• BSN, Bachelor of Science in Nursing
• CCOs, Coordinated Care Organizations
• CMS, Centers for Medicare & Medicaid Services
• CNA, Certified Nursing Assistant
• DDS/DMD, Doctor of Dental Surgery/Doctor of Dental Medicine
• DO, Doctor of Osteopathy
• FFS, Fee-for-service
• FTE, Full-time equivalent
• HCPIP, Health Care Provider Incentive Program
• HHS, U.S. Department of Health and Human Services
• HIPPA, Health Insurance Portability and Accountability Act
• HOWTO, Healthy Oregon Workforce Training Opportunity Grant Program
• HRSA, Health Resources and Services Administration
• LPN, Licensed Practical Nurse
• MD, Doctor of Medicine
• NIOSH, National Institute for Occupational Safety and Health
• NP, Nurse Practitioner
• OCN, Oregon Center for Nursing
• ODHS, Oregon Department of Human Services
• OHA, Oregon Health Authority
• OHCA, Oregon Health Care Association
• OHP, Oregon Health Plan
• OHPB, Oregon Health Policy Board
• OHSU, Oregon Health & Science University
• ONC, Office of the National Coordinator for Health Information Technology
• OSBN, Oregon State Board of Nursing
• OSU, Oregon State University
• PA, Physician Assistant
• PCO, Oregon Primary Care Office
• PCPH, Patient-Centered Primary Care Home
• PH WINS, Public Health Workforce Interests and Needs Survey
• PHAB, Oregon Public Health Advisory Board
• PPE, Personal Protective Equipment
• RN, Registered Nurse
• SAMHSA, Substance Abuse and Mental Health Services Administration
• SHOI, Scholars for a Healthy Oregon Initiative
• UCSF, University of California San Francisco


