
Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
1
LOUISIANA DEPARTMENT OF HEALTH
MEDICAID SERVICES CHART
August 2024

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
2
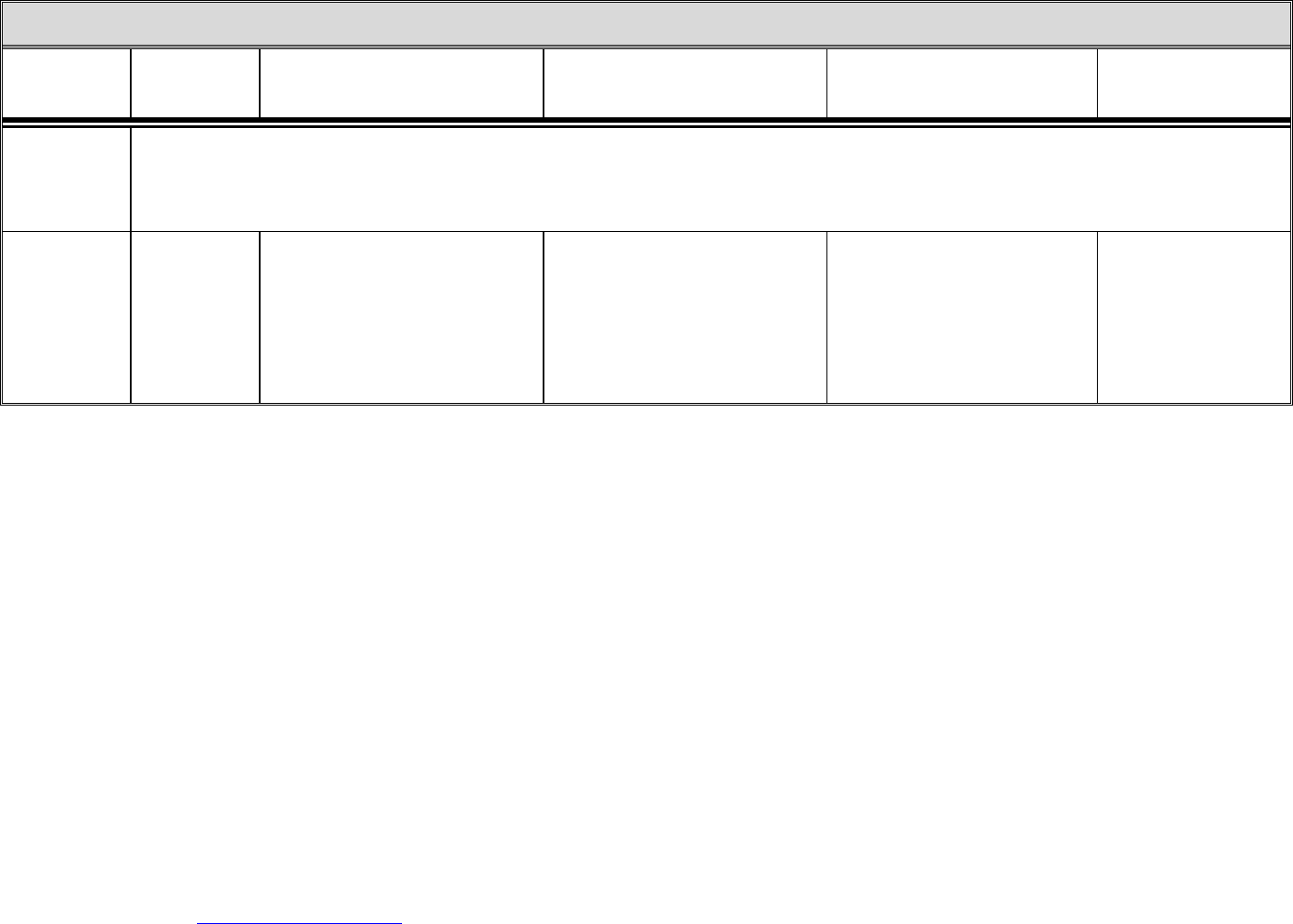
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
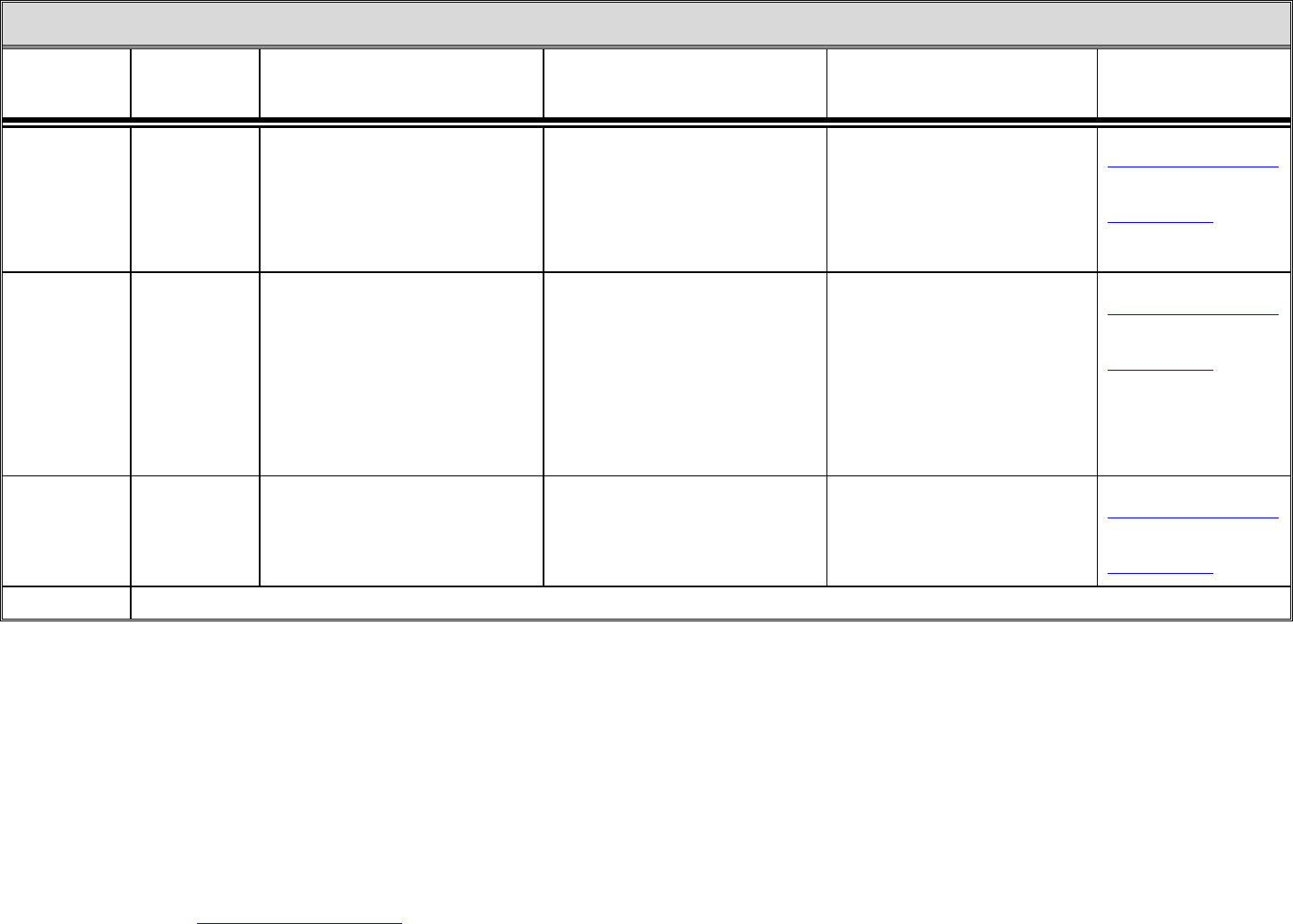
Adult Denture
Services
Dentist
Medicaid beneficiaries 21 years of age
and older.
(Adults, 21 and over, certified as
Qualified Medicare Beneficiary
(QMB), Specified Low Income
Medicare Beneficiary (SLMB) only,
PACE, Take Charge Plus or other
programs with limited benefits are
not eligible for dental services.)
Examination, x-rays (are only covered if
in conjunction with the construction of a
Medicaid-authorized denture) dentures,
denture relines, and denture repairs.
Only one complete or partial denture per
arch is allowed in an eight-year period.
The partial denture must oppose a full
denture. Two partials are not covered in
the same oral cavity (mouth). Additional
guidelines apply.
DentaQuest and MCNA Dental
administer the dental benefits for
eligible Medicaid beneficiaries.
Contact your plan to locate a network
provider and for questions about
covered dental services.
DentaQuest
1-800-685-0143
www.DentaQuest.com
MCNA Dental
1-855-702-6262
www.MCNALA.net
Andrea Perry
225-342-7476
Tiffany Hayes
225-342-7877
Adult Waiver
Dental Services
Dentist
Medicaid beneficiaries 21 years of age
and older enrolled in New Opportunities
Waiver, Residential Options Waiver or
Supports Waiver.
The Adult Waiver Dental Program
provides coverage of certain diagnostic;
preventive; restorative; endodontic;
periodontic; removable prosthodontic;
maxillofacial prosthetic; oral and
maxillofacial surgery; orthodontic; and
adjunctive general services. Specific
policy guidelines apply.
DentaQuest and MCNA Dental
administer the dental benefits for
eligible Medicaid beneficiaries.
Contact your plan to locate a network
provider and for questions about
covered dental services.
DentaQuest
1-800-685-0143
www.DentaQuest.com
MCNA Dental
1-855-702-6262
www.MCNALA.net
Andrea Perry
225-342-7476
Tiffany Hayes
225-342-7877

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
3
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
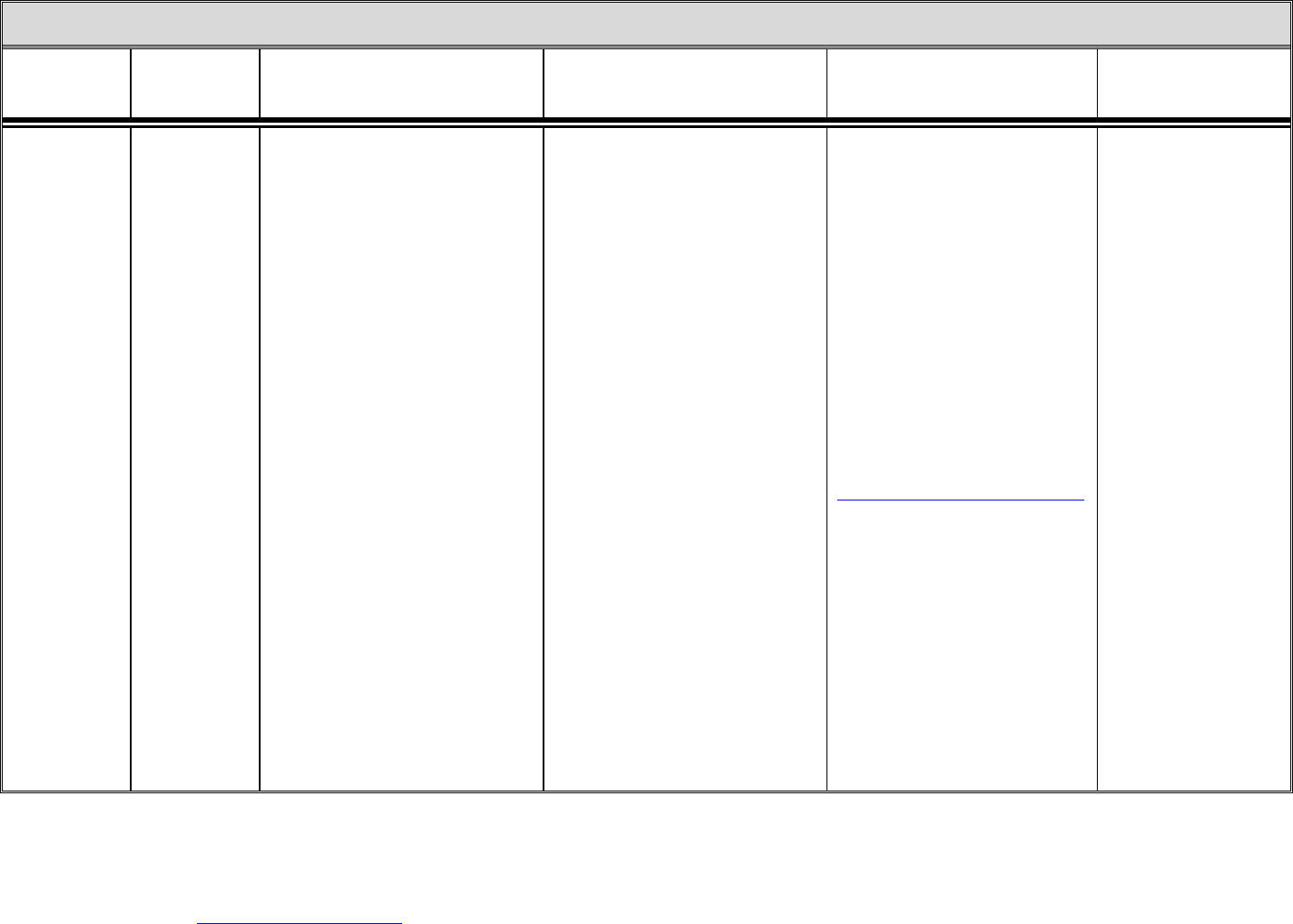
Applied
Behavior
Analysis (ABA)
Medicaid
enrolled ABA
provider
Age from birth up to 21 years of age;
and
1. Exhibit the presence of excesses
and/or deficits of behaviors that
significantly interfere with home or
community activities (examples
include, but are not limited to
aggression, self-injury, elopement,
etc.);
2. Be diagnosed by a qualified health
care professional with a condition for
which ABA-based therapy services
are recognized as therapeutically
appropriate, including autism
spectrum disorder;
3. Have a comprehensive diagnostic
evaluation by a qualified health care
professional; and
4. Have a prescription for ABA-based
therapy services ordered by a
qualified health care professional.
ABA-based therapy services shall be
rendered in accordance with the
beneficiary’s treatment plan.
All medically necessary services must
be prescribed and Prior Authorized.
The provider of services will submit
requests for Prior Authorization.
Aetna
1-855-242-0802
www.aetnabetterhealth.
com/louisiana
AmeriHealth Caritas
1-888-756-0004
www.amerihealthcaritasla.
com
Healthy Blue
1-844-521-6941
www.myhealthybluela.
com
Humana Healthy
Horizons in Louisiana
1-800-448-3810
www.humana.com/
medicaid/louisiana
Louisiana Healthcare
Connections
1-866-595-8133
www.louisianahealth
connect.com
United Healthcare
Community Plan
1-844-253-0667
www.uhccommunityplan.
com
Crystal Faison
225-342-8233
Audiological
Services
See: EarlySteps; EPSDT Screening Services; Hospital – Outpatient services; Physician/Professional Services; Rehabilitation Clinic Services; Therapy Services

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
4
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Behavioral
Health Services
– Adults
Any Medicaid
eligible adult
beneficiary may
receive the
following
behavioral
health service if
medical
necessity is
established by a
licensed mental
health
professional
(LMHP) or
physician.
Adult Medicaid beneficiaries eligible to
receive Mental Health Rehabilitation
(MHR) services under Medicaid State
Plan include those who meet the
following criteria:
• Must have a mental health diagnosis
and
• Must be assessed by an LMHP
Beneficiaries receiving Community
Psychiatric Support & Treatment
(CPST) and/or Psychosocial
Rehabilitation (PSR):
• Must have at least a level of care of
three on the Level of Care
Utilization System (LOCUS).
• Must have a rating of three or
greater on the functional status
domain on the LOCUS.
Beneficiaries receiving Individual
Placement Supports (IPS) and Personal
Care Services (PCS) must be:
• 21 years of age or older
• Transitioned from a nursing facility
or been diverted from nursing
facility level of care through the My
Choice Louisiana program.
For more information, please refer to the
BHS Provider Manual.
1. Community Psychiatric Support &
Treatment (CPST)
2. Psychosocial Rehabilitation (PSR)
3. Crisis Intervention (CI)
4. Assertive Community Treatment
(ACT)
5. Crisis Responses Services
a. Mobile Crisis Response (MCR)
b. Behavioral Health Crisis Care
(BHCC)
c. Community Brief Crisis Service
(CBCS)
6. Crisis Stabilization (CS)
7. Individual Placement and Supports
(IPS)
8. Personal Care Services (PCS)
9. Peer Support Services (PSS)
10. Outpatient Therapy with Licensed
Practitioners (medication
management, individual, family,
and group counseling)
11. Addiction Services (outpatient,
residential, and inpatient)
12. Psychiatric Inpatient Hospital 18-21
years and over 65 years of age
13. Opioid Treatment Programs (OTPs)
Adult Behavioral Health services are
administered by the Healthy Louisiana
Plans. CPST, PSR, CI follow-up,
ACT, CBCS, CS, IPS, PCS, and PSS
must be Prior Authorized.
Aetna
1-855-242-0802
www.aetnabetterhealth.
com/louisiana
AmeriHealth Caritas
1-888-756-0004
www.amerihealthcaritasla.
com
Healthy Blue
1-844-521-6941
www.myhealthybluela.
com
Humana Healthy
Horizons in Louisiana
1-800-448-3810
www.humana.com/
medicaid/louisiana
Louisiana Healthcare
Connections
1-866-595-8133
www.louisianahealth
connect.com
United Healthcare
Community Plan
1-844-253-0667
www.uhccommunityplan.
com

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
5
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Chemotherapy
Services
See also:
Hospital-
Outpatient
Services;
Physician/
Professional
Services
Hospital
Physician’s
office or clinic
All Medicaid beneficiaries.
Chemotherapy administration and
treatment drugs, as prescribed by
physician.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233
(Please utilize the above
contact for questions
related to Fee For Service
coverage.)

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
6
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Chiropractic
Services
EPSDT Medical
Screening
Provider/PCP
Medicaid beneficiaries 0 through 20
years of age.
Spinal manipulations.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233
(Please utilize the above
contact for questions
related to Fee For Service
coverage.)

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
7
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Coordinated
System of Care
(CSoC)
Program
To make a
referral, contact
Magellan
directly or the
child/youth’s
Healthy
Louisiana Plan.
Note that the
parent/caregiver
must participate
in the referral.
Children, youth and families eligible for
CSoC include Medicaid beneficiaries
between the ages of 5 and 20, who have
a severe emotional disturbance (SED) or
a serious mental illness (SMI) and who
are in or at risk of out of home
placement. A beneficiary must meet the
level of care or level of need through a
Child and Adolescent Needs and
Strengths (CANS) comprehensive
assessment.
For more information, please refer to the
BHS Provider Manual.
1. Parent Support & Training
2. Youth Support & Training
3. Independent Living/Skills Building
4. Short Term Respite Care
5. Case Conference
CSoC services are administered by
Magellan Health Services of
Louisiana.
NOTE: The Healthy Louisiana Plan
will connect you with Magellan to
complete the referral.
Magellan Health
Services of Louisiana
1-800-424-4489
Aetna
1-855-242-0802
www.aetnabetterhealth.
com/louisiana
AmeriHealth Caritas
1-888-756-0004
www.amerihealthcaritasla.
com
Healthy Blue
1-844-521-6941
www.myhealthybluela.
com
Humana Healthy
Horizons in Louisiana
1-800-448-3810
www.humana.com/
medicaid/louisiana
Louisiana Healthcare
Connections
1-866-595-8133
www.louisianahealth
connect.com
United Healthcare
Community Plan
1-844-253-0667
www.uhccommunityplan.
com
Dental Care
Services
See: Adult Denture Services; Adult Waiver Dental Services; and EPSDT Dental Services

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
8
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Durable
Medical
Equipment
(DME)
Physician
All Medicaid beneficiaries.
Medical equipment and appliances such
as wheelchairs, leg braces, etc.
Medical supplies such as ostomy
supplies, etc.
Diapers and blue pads are -only
reimbursable as durable medical
equipment items for Medicaid
beneficiaries 0 through 20 years of age.
All services must be prescribed by a
physician and must be Prior
Authorized.
DME providers will arrange for the
Prior Authorization request.
Irma Gauthier
225-342-5691
EarlySteps
(Infant &
Toddler Early
Intervention
Services)
1. Children from birth to 3 years of age
who have a developmental delay of
at least 1.5 Standard Deviations (SD)
below the mean in two areas of
development listed below:
a. Cognitive development
b. Physical development (vision &
hearing) - communication
development
c. Social or emotional development
d. Adaptive skills development (also
known as self-help or daily living
skills)
2. Children with a diagnosed medical
condition with a high probability of
resulting in developmental delay.
Covered Services (Medicaid Covered)
- Family Support Coordination (Service
Coordination)
- Occupational Therapy
- Physical Therapy
- Speech/Language Therapy
- Psychology
- Audiology
EarlySteps also provides the following
services, not covered by Medicaid:
- Nursing Services/Health Services
(Only to enable an eligible
child/family to benefit from the other
EarlySteps services).
- Medical Services for diagnostic and
evaluation purposes only.
- Special Instruction
- Vision Services
- Assistive Technology devices and
services
- Social Work
- Counseling Services/Family Training
- Transportation
- Nutrition
- Sign language and cued language
services.
All services are provided through a
plan of care called the Individualized
Family Service Plan (IFSP).
Early Intervention is provided through
EarlySteps in conformance with Part
C of the Individuals with Disabilities
Education Act (IDEA).
Office for Citizens with
Developmental
Disabilities (OCDD)
1-866-783-5553
or
1-866-EARLYSTEP
for families
Caroline Oglesby
225-342-8853

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
9
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
EPSDT
Behavioral
Health Services
Medicaid
eligible
beneficiaries
who meets the
medical
necessity
criteria for
behavioral
health services
as determined
by a licensed
mental health
professional
(LMHP) or
physician.
Meets medical necessity criteria for
rehabilitation services for beneficiaries
under the age of 21.
Beneficiaries eligible to receive Mental
Health Rehabilitation (MHR) services
under Medicaid State Plan include those
who meet one of the following criteria
and are 21 years or age or younger:
• Must have a mental health diagnosis
• Must be assessed by a LMHP
Beneficiaries receiving Community
Psychiatric Support & Treatment
(CPST) and/or Psychosocial
Rehabilitation (PSR), ages 6 through 18
years of age, must be assessed using the
Child and Adolescent Level of
Care/Service Intensity Utilization
System (CALOCUS).
Beneficiaries receiving CPST and/or
PSR, ages 19 through 20 years of age,
must be assessed using the Level of
Care/Service Intensity Utilization
System LOCUS.
Beneficiaries who receive Multi-
Systemic Therapy, Homebuilders,
Functional Family Therapy and
Functional Family Therapy-Child
Welfare are not required to be assessed
using the CALOCUS.
1. Community Psychiatric Support &
Treatment (CPST)
2. Psychosocial Rehabilitation (PSR)
3. Crisis Intervention
4. Crisis Stabilization
5. Outpatient Therapy with Licensed
Practitioners (medication
management, individual, family,
and group counseling)
6. Therapeutic Group Home
7. Psychiatric Residential Treatment
Facility (PRTF)
8. Psychiatric Inpatient Hospital
9. Addiction Services (outpatient,
residential, and inpatient)
10. Multi-systemic Therapy (MST)
11. Functional Family Therapy (FFT)
12. Homebuilders (HB)
13. Assertive Community Treatment
(ACT)
14. Child Parent Psychotherapy (CPP)
15. Parent-child interaction therapy
(PCIT)
16. Preschool PTSD Treatment (PPT)
and Youth PTSD Treatment (YPT)
17. Trauma-Focused Cognitive
Behavioral Therapy (TF-CBT)
18. Eye Movement Desensitization and
Reprocessing (EMDR) Therapy
19. Coordinated System of Care (CSoC)
(NOTE: Please see the CSoC
section)
20. Mobile Crisis Response (MCR)
21. Community Brief Crisis Support
(CBCS)
EPSDT Behavioral Health services
are administered by the Healthy
Louisiana Plans.
CPST, PSR, MST, FFT, HB, CBCS,
and ACT must be Prior Authorized.
Aetna
1-855-242-0802
www.aetnabetterhealth.
com/louisiana
AmeriHealth Caritas
1-888-756-0004
www.amerihealthcaritasla.
com
Healthy Blue
1-844-521-6941
www.myhealthybluela.
com
Humana Healthy
Horizons in Louisiana
1-800-448-3810
www.humana.com/
medicaid/louisiana
Louisiana Healthcare
Connections
1-866-595-8133
www.louisianahealth
connect.com
United Healthcare
Community Plan
1-844-253-0667
www.uhccommunityplan.
com
For CSoC Services:
Magellan Health
Services of Louisiana
1-800-424-4489
www.magellanoflouisiana
.com

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
10
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
EPSDT Dental
Services
Dentist
Medicaid beneficiaries 0 through 20
years of age.
The EPSDT Dental Program provides
coverage of certain diagnostic;
preventive; restorative; endodontic;
periodontic; removable prosthodontic;
maxillofacial prosthetic; oral and
maxillofacial surgery; orthodontic; and
adjunctive general services. Specific
policy guidelines apply.
Comprehensive Orthodontic Treatment
(braces) are paid only when there is a
cranio-facial deformity, such as cleft
palate, cleft lip, or other medical
conditions which possibly results in a
handicapping malocclusion. If such a
condition exists, the beneficiary should
see a Medicaid-enrolled orthodontist.
Patients having only crowded or
crooked teeth, spacing problems or
under/overbite are not covered for
braces, unless identified as medically
necessary.
DentaQuest and MCNA Dental
administer the dental benefits for
eligible Medicaid beneficiaries.
Contact your plan to locate a network
provider and for questions about
covered dental services.
DentaQuest
1-800-685-0143
www.DentaQuest.com
MCNA Dental
1-855-702-6262
www.MCNALA.net
Andrea Perry
225-342-7476
Tiffany Hayes
225-342-7877

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
11
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
EPSDT
Personal Care
Services (PCS)
For Medicaid
beneficiaries
age 65 or older,
or age 21 or
older with
disabilities, see:
Long Term –
Personal Care
Services (LT-
PCS)
Physician and
Personal Care
Attendant
Agencies
All Medicaid beneficiaries 0 through 20
years of age and have been prescribed
medically necessary, age appropriate
EPSDT-PCS by a practitioner
(physician, advance practice nurse, or
physician assistant). The practitioner
shall specify the health/medical
condition that necessitates EPSDT-PCS.
Medical necessity criteria shall be based
on functional and medical eligibility and
impairment in at least two activities of
daily living. To establish medical
necessity, the EPSDT eligible
beneficiary must be of an age at which
the tasks to be performed by the PCS
provider would ordinarily be performed
by the beneficiary, if not for being
disabled due to illness or injury.
Waiver services (beneficiaries age 0 to
20 years of age) and PCS may be
performed on the same date, but not at
the same time. If the beneficiary is
receiving home health, respite, and/or
any other related service, the PCS
provider cannot provide service at the
same time as the other Medicaid
covered service provider.
Basic personal care-toileting &
grooming activities.
Assistance with bladder and/or bowel
requirements or problems.
Assistance with eating and food
preparation.
Performance of incidental household
chores, only for the beneficiary.
Accompanying, not transporting,
beneficiaries to medical appointments.
Does NOT cover any medical tasks
such as medication administration, tube
feedings, urinary catheters, ostomy or
tracheostomy care.
The Personal Care Agency must
submit the Prior Authorization
request.
Beneficiaries receiving Support
Coordination (Case Management
Services) must also have their PCS
Prior Authorized by Gainwell
Technology.
PCS is not subject to service limits.
Units approved will be based on
medical necessity and the need for
covered services.
Beneficiaries receiving Personal Care
Services must have a practitioner’s
prescription and meet medical criteria.
Does NOT include medical tasks.
Provided by licensed providers
enrolled in Medicaid to provide
Personal Care Attendant services.
Norma Seguin
225-342-7513
EPSDT
Screening
Services
(Child Health –
Preventive
Services)
Physician
All Medicaid beneficiaries 0 through 20
years of age.
Medical Screenings (including
immunizations and certain lab services).
Vision Screenings
Hearing Screenings
Dental Screenings
Beneficiaries receive their screening
services from their primary care
provider (PCP) or appropriate health
care provider.
Norma Seguin
225-342-7513
Specialty Care Resource
Line
1-877-455-9955
Eyewear
See: Vision Services

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
12
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Family
Planning
Services
(Take Charge
Plus)
Any Medicaid
provider who
offers family
planning
services.
For assistance
with locating a
provider, call
1-877-455-9955
All Louisiana beneficiaries of child
bearing age regardless of gender with an
income at or below 138% of the Federal
Poverty level. Pregnant women are
excluded from this program.
Family planning related services and
care related to:
• Birth control (pills, implants,
injections, condoms, and IUDs)
• Cervical cancer screening and
treatment for most abnormal results
• Contraceptive counseling and
education
• Prescriptions, and follow-up visits
to treat STIs
• Treatment of major complications
from certain family planning
procedures
• Voluntary sterilization for males
and females (over age 21)
• Vaccines for both males and
females for the prevention of HPV
• Transportation to family planning
appointments
Take Charge Plus is limited to family
planning services and family planning
related services. There are no
enrollment fees, no premiums, co-
payments or deductibles. All
Medicaid providers including
American Indian “638” Clinics, RHCs
and FQHCs are reimbursed at
established fee-for-service rates
published in the Take Charge Plus fee
schedule.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233
(Please utilize the above
contact for questions
related to fee-for-service
coverage.)
Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
13
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Family
Planning
Services in
Physician’s
Office
See: Physician/Professional Services
Federally
Qualified
Health Centers
(FQHC)
Nearest FQHC
The American
Indian Clinic
All Medicaid beneficiaries.
Professional medical services furnished
by physicians, nurse practitioners,
physician assistants, nurse midwives,
clinical social workers, clinical
psychologists, and dentists
Covered benefits include medical,
behavioral health, and dental.
There are 3 components that may be
provided:
1. Encounter visits;
2. EPSDT Screening Services; and
3. EPDST Dental, and Adult Denture
Services.
Irma Gauthier
225-342-5691

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
14
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Free Standing
Birthing
Centers
Certified Nurse
Midwife or
Licensed
Midwife
All Medicaid eligible pregnant women
Vaginal delivery services for females
who have had a low risk, normal
pregnancy, prenatal care and that are
expected to have an uncomplicated
labor and normal vaginal delivery.
A Free Standing Birthing Center is a
free standing facility, separate from a
hospital.
Stays for delivery are usually less than
24 hours.
Epidural anesthesia is not provided for
deliveries at Free Standing Birthing
Centers.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
15
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Hearing Aids
See also:
Durable
Medical
Equipment
Durable
Medical
Equipment
Provider
Medicaid beneficiaries 0 through 20
years of age.
Hearing Aids and any related ancillary
equipment such as earpieces, batteries,
etc. Repairs are covered if the Hearing
Aid was paid for by Medicaid.
All services must be Prior
Authorized and the DME provider
will arrange for the request of Prior
Authorization.
Irma Gauthier
225-342-5691
Hemodialysis
Services
See also:
Hospital –
Outpatient
Services
Dialysis Centers
Hospitals
All Medicaid beneficiaries.
Dialysis treatment (including routine
laboratory services); medically
necessary non-routine lab services; and
medically necessary injections.
Justin Owens
225-342-6888
Home Health
Physician
All Medicaid beneficiaries.
Medically Needy (Type Case 20 & 21)
beneficiaries are not eligible for Aide
Visits, Physical Therapy, Occupational
Therapy, and Speech/Language
Therapy.
EPSDT Home Health is provided to the
medically needy if the beneficiary is
under the age of 21.
• Intermittent/part-time nursing
services including skilled nurse
visits.
• Aide Visits
• Physical Therapy
• Occupational Therapy
• Speech/Language Therapy
Beneficiaries receiving Home Health
must have an authorized healthcare
provider’s prescription and signed
plan of care.
PT, OT, and Speech/Language
Therapy require Prior Authorization.
Crisis Response Team – for Medicaid
beneficiaries 0 through 20 years of
age AND under a waiver program
(Supports, ROW, NOW, Children’s
Choice) AND not receiving prescribed
medically necessary intermittent
nursing services for 2 consecutive
weeks
Justin Owens
225-342-6888
Crisis Response Team
1-866-729-0017
crisisresponseteam@la.
gov

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
16
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Home Health –
Extended
Physician
Medicaid beneficiaries 0 through 20
years of age.
Multiple hours of skilled nurse services.
All medically necessary medical tasks
that are part of the plan of care can be
administered in the home.
Beneficiaries receiving extended
nursing services must have a letter of
medical necessity and an authorized
healthcare provider’s prescription.
Extended Skilled nursing services
require Prior Authorization.
Crisis Response Team – for Medicaid
beneficiaries 0 through 20 years of
age AND under a waiver program
(Supports, ROW, NOW, Children’s
Choice) AND not receiving prescribed
medically necessary Extended Home
Health nursing services for 2
consecutive weeks.
Justin Owens
225-342-6888
Crisis Response Team
1-866-729-0017
crisisresponseteam@la.
gov
Hospice
Services
Hospice
Provider/
Physician
All Medicaid beneficiaries.
Hospice eligibility information:
1-800-877-0666 Option 2
Medicare allowable services.
Justin Owens
225-342-6888
Hospital Claim
Questions –
Inpatient and
Outpatient
Services,
including
Emergency
Room Services
Physician/
Hospital
All Medicaid beneficiaries.
Medically Needy beneficiaries (Type
Case 20 & 21) under the age of 21 are
not eligible for Inpatient Psychiatric
Services.
Inpatient and Outpatient Hospital
Services, including Emergency Room
Services
All questions regarding denied claims
and/or bills for Inpatient and
Outpatient Hospital services,
including Emergency Room services.
Beneficiaries should first
contact the provider, then
may contact an MMIS
Staff Member at
225-342-3855 if the issue
cannot be resolved
Providers should contact
Provider Relations at
1-800-473-2783
Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
17
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Hospital –
Inpatient
Services
Physician/
Hospital
All Medicaid beneficiaries.
Medically Needy beneficiaries (Type
Case 20 & 21) under the age of 21 are
not eligible for Inpatient Psychiatric
Services.
Inpatient hospital care needed for the
treatment of an illness or injury which
can only be provided safely &
adequately in a hospital setting.
Includes those basic services that a
hospital is expected to provide.
For providers:
ProviderRelatio[email protected]
For members:
Healthy@la.gov
Hospital –
Outpatient
Services
Physician/
Hospital
All Medicaid beneficiaries.
Diagnostic & therapeutic outpatient
services, including outpatient surgery
and rehabilitation services.
Therapeutic and diagnostic radiology
services.
Chemotherapy
Hemodialysis
Outpatient rehabilitation (physical
therapy, occupational therapy, and
speech therapy) require Prior
Authorization. Provider will submit
request for Prior Authorization.
For providers:
ProviderRelatio[email protected]
For members:
Healthy@la.gov
Hospital –
Emergency
Room Services
Physician/
Hospital
All Medicaid beneficiaries.
Emergency Room services.
No service limits.
For providers:
ProviderRelatio[email protected]
For members:
Healthy@la.gov
Immunizations
See: FQHC; EPSDT Screening Services; Physician/Professional Services; Rural Health Clinics

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
18
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Laboratory
Tests and
Radiology
Services
Physician
All Medicaid beneficiaries.
Most diagnostic testing and radiological
services ordered by the attending or
consulting physician.
Portable (mobile) x-rays are covered
only for beneficiaries who are unable to
leave their place of residence without
special transportation or assistance to
obtain physician ordered x-rays.
All requests for any radiology services
requiring prior approval are initiated
by the ordering physician.
Beneficiaries may follow up with the
ordering physician for the status of
any ordered radiology service.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
19
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Long Term –
Personal Care
Services
(LT-PCS)
For Medicaid
beneficiaries
ages 0 through
20, see: EPSDT
Personal Care
Services
Contact
Louisiana
Options in Long
Term Care
(Conduent)
1-877-456-1146
for information,
eligibility
information,
assessments and
service
requirements
All Medicaid beneficiaries age 65 or
older, or age 21 or older with disabilities
(meets Social Security Administration
disability criteria), meet the medical
standards for admission to a nursing
facility and additional targeting criteria,
and be able to participate in their care
and direct the services provided by the
worker independently or through a
responsible representative. Applicant
must require at least limited assistance
with at least one Activity of Daily
Living.
- Basic personal care-toileting &
grooming activities.
- Assistance with bladder and/or bowel
requirements or problems.
- Assistance with eating and food
preparation.
- Performance of incidental household
chores, only for the beneficiary.
- Accompanying, not transporting, the
beneficiary to medical appointments.
- Grocery shopping, including personal
hygiene items.
Beneficiaries or the responsible
representative must request the
service.
This program is NOT a substitute for
existing family and/or community
supports, but is designed to
supplement available supports to
maintain the beneficiary in the
community.
Once approved for services, the
selected PCS agency must obtain
Prior Authorization.
Amount of services approved will be
based on assessment of assistance
needed to perform activities of daily
living.
Provided by PCS agencies enrolled in
Medicaid.
Louisiana Options in
Long Term Care
(Conduent)
1-877-456-1146
Office of Aging and
Adult Services (OAAS)
1-866-758-5035
Christy Sawyer
225-362-7644

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
20
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Medical
Transportation
(Emergency)
Emergency
ambulance
providers
All Medicaid beneficiaries, who are
eligible for emergency medical
treatment (EMT) services.
Emergency ambulance transportation is
provided for a medical condition
manifesting itself by acute symptoms of
sufficient severity (including severe
pain) such that a prudent layperson, who
possesses an average knowledge of
health and medicine, could reasonably
expect the absence of immediate
medical attention to result in:
- Placing the health of the beneficiary
(or, with respect to a pregnant woman,
the health of the woman or her unborn
child) in serious jeopardy
- Serious impairment to bodily function
- Serious dysfunction of any bodily
organ or part.
A beneficiary may also require
emergency ambulance transportation if
they are psychiatrically unmanageable
or needs restraint.
Beginning January 1, 2023, Medicaid
will only reimburse for a beneficiary's
transportation services to a FFS provider
and/or managed care provider if that
provider has enrolled through the
Medicaid Provider Enrollment Portal. A
subset of EMT is physician directed
treatment-in-place service, which
facilitates a telehealth visit by an
ambulance provider. If a beneficiary
being treated-in-place has a real-time
deterioration in their clinical condition,
the ambulance provider, telehealth
provider or beneficiary may determine
that immediate transport to an
emergency department is required.
Medicaid
Transportation Division
225-342-9566
MedicaidTransportation@
la.gov

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
21
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Medical
Transportation
(Non-
Emergency)
Healthy
Louisiana
managed care
plan
beneficiaries
should contact:
Aetna
1-877-917-4150
AmeriHealth
Caritas
1-888-913-0364
Healthy Blue
1-866-430-1101
Humana
Healthy
Horizons in
Louisiana
1-844-613-1638
Louisiana
Healthcare
Connections
1-855-369-3723
United
Healthcare
Community
Plan
1-866-726-1472
Legacy
Medicaid or
FFS
beneficiaries
should contact:
Verida
1-855-325-7626
All Medicaid beneficiaries who are
eligible for non-emergency medical
transportation (NEMT) services.
Transportation provided to and/or from
a Medicaid covered service, including
carved out services, or value added
benefits (VAB) when no other means of
transportation is available.
Beginning January 1, 2023, Medicaid
will only reimburse for a beneficiary's
transportation services to a FFS provider
and/or managed care provider if that
provider has enrolled through the
Medicaid Provider Enrollment Portal.
Eligible expenses include the following
when necessary to ensure the delivery of
medically necessary services:
- Transportation for the beneficiary and
one attendant; and
- Meals, lodging, and other related
travel expenses for the beneficiary and
one attendant when long distance
travel is required. Long distance is
defined as when the total travel time,
including the duration of the
appointment plus the travel to and
from the appointment, exceeds 12
hours. Medicaid covers meals and
lodging for trips that are not otherwise
covered in the inpatient per diem,
primary insurance, or other payer
source.
With the exception of urgent transportation
requests and discharges from inpatient
facilities, when requesting transportation
services the beneficiaries and healthcare
providers should schedule all services a
minimum of 48 hours prior to the requested
appointment. The 48-hour minimum does not
include non-business days. However, the
MCO and/or transportation broker must make
a reasonable attempt to schedule the trip with
less than 48 hour notice.
Urgent transportation refers to a request for
transportation made by a healthcare provider
for a medical service, which does not warrant
emergency transport but cannot be postponed.
All non-emergency out-of-state transportation
must be prior approved by the MCO or
transportation broker. The MCO may approve
transportation to out-of-state medical care
only if the beneficiary has been granted
approval to receive medical treatment out of
state.
An attendant shall be required when the
beneficiary is under the age of 17. The
attendant must be a parent, legal guardian, or
responsible person designated by the
parent/legal guardian, and be able to authorize
medical treatment and care for the
beneficiary.
Attendants may not be under the age of 17 or
be a Medicaid provider or employee of a
Medicaid provider that is providing services
to the beneficiary being transported, except
for employees of a mental health facility in
the event a beneficiary has been identified as
being a danger to themselves or others or at
risk for elopement. They also may not be a
transportation provider or an employee of a
transportation provider. Exception: All
females, regardless of their age, seeking
prenatal and/or postpartum care shall not be
required to have an attendant.
Medicaid
Transportation Division
225-342-9566 or
225-333-7473
MedicaidTransportation@
la.gov

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
22
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Medical
Transportation
(Non-
Emergency
Ambulance)
Healthy
Louisiana
managed care
plan
beneficiaries
should contact:
Aetna
1-877-917-4150
AmeriHealth
Caritas
1-888-913-0364
Healthy Blue
1-866-430-1101
Humana
Healthy
Horizons in
Louisiana
1-844-613-1638
Louisiana
Healthcare
Connections
1-855-369-3723
United
Healthcare
Community
Plan
1-866-726-1472
Legacy
Medicaid or
FFS
beneficiaries
should contact:
Verida
1-855-325-7626
All Medicaid beneficiaries who are
eligible for non-emergency ambulance
transportation (NEAT) services.
Transportation provided to a beneficiary
by ground/air ambulance to and/or from
a Medicaid covered service, including
carved out services and VABs when:
No other means of transportation is
available; the beneficiary’s condition is
such that use of any other method of
transportation is contraindicated or
would make the beneficiary susceptible
to injury; and the nature of the trip is not
an emergency, but the beneficiary
requires the use of an ambulance
Beginning January 1, 2023, Medicaid
will only reimburse for a beneficiary's
transportation services to a FFS provider
and/or managed care provider if that
provider has enrolled through the
Medicaid Provider Enrollment Portal.
An attendant shall be required when the
beneficiary is under the age of 17. The
attendant must be a parent, legal
guardian, or responsible person
designated by the parent/legal guardian;
and be able to authorize medical
treatment and care for the beneficiary.
Attendants may not be under the age of
17 or be a Medicaid provider or
employee of a Medicaid provider that is
providing services to the beneficiary
being transported, except for employees
of a mental health facility in the event a
beneficiary has been identified as being
a danger to themselves or others or at
risk for elopement. Exception: All
females, regardless of their age, seeking
prenatal and/or postpartum care shall
not be required to have an attendant.
A beneficiary or a medical facility
may schedule NEAT services through
an ambulance provider or the
transportation broker.
The beneficiary’s treating physician, a
registered nurse, the director of
nursing at a nursing facility, a nurse
practitioner, a physician assistant, or a
clinical nurse specialist must certify
on the Certification of Ambulance
Transportation (CAT) that the
transport is medically necessary and
describe the medical condition, which
necessitates ambulance services.
Beneficiaries may seek medically
necessary services in another state
when it is the nearest option available.
All out-of-state NEAT transportation
to facilities that are not the nearest
available option, must be prior
approved by the MCO and/or
transportation broker.
Beneficiaries should schedule NEAT
services at a minimum of 48 hours
prior to the requested transportation
services. The 48-hour minimum does
not include non-business days.
However, the MCO and/or
transportation broker must make a
reasonable attempt to schedule the trip
with less than 48 hours’ notice.
Urgent transportation may be
scheduled by the beneficiary’s
physician's office or healthcare
facility.
Medicaid
Transportation Division
225-342-9566 or
225-333-7473
MedicaidTransportation@
la.gov

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
23
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Midwife
Services
For Certified Nurse Midwife, see: FQHC; Physician/Professional Services; Rural Health Clinics
For Licensed Midwife, see: Freestanding Birthing Center
Nurse
Practitioners/
Clinical Nurse
Specialists
See FQHC; Physician/Professional Services; Rural Health Clinics
Nursing
Facility
Medicaid beneficiaries and persons who
would meet Medicaid Long Term Care
financial eligibility requirements and
who meet nursing facility level of care
as determined by OAAS.
Skilled Nursing or medical care and
related services; rehabilitation needed
due to injury, disability, or illness;
health-related care and services (above
the level of room and board) not
available in the community, needed
regularly due to a mental or physical;
condition.
Louisiana Options in
Long Term Care
(Conduent)
1-877-456-1146
Office of Aging and
Adult Services (OAAS)
1-866-758-5035
Occupational
Therapy
Services
See: EarlySteps; Home Health; Hospital – Outpatient Services; Rehabilitation Clinic Services; Therapy Services

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
24
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Optical
Services
For eyewear,
see: Vision
Services
Ophthalmologist
All Medicaid beneficiaries.
Beneficiaries ages 0 through 20
Examinations and treatment of eye
conditions, including examinations for
vision correction, refraction error.
Other related services, if medically
necessary.
Beneficiaries age 21 and over
Examinations and treatment of eye
conditions, such as infections, cataracts,
etc.
If the beneficiary has both Medicare and
Medicaid, some vision related services
may be covered. The beneficiary should
contact Medicare for more information
since Medicare would be the primary
payer.
NON-COVERED SERVICES:
Beneficiaries age 21 and over
- Routine eye examinations for vision
correction
- Routine eye examinations for
refraction error
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
For ophthalmology:
Crystal Faison
225-342-8233
For eyewear:
Irma Gauthier
225-342-5691
Orthodontic
Services
See Dental Care Services

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
25
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Pediatric Day
Health Care
(PDHC)
Physician or
PDHC Agencies
Medicaid beneficiaries ages 0 through
20 who have a medically fragile
condition and who require nursing
supervision and possibly therapeutic
interventions all or part of the day due
to a medically complex condition.
• Nursing Care
• Respiratory Care
• Physical Therapy
• Speech-language Therapy
• Occupational Therapy
• Personal Care Services
• Transportation to/from PDHC
facility
PDHC services require Prior
Authorization. The PDHC facility
must submit the Prior Authorization
request.
In order to receive PDHC, the
beneficiary must have a prescription
from their prescribing physician and
meet the medical criteria.
PDHC may be provided up to 7 days
per week and up to 12 hours per day
for Medicaid beneficiaries as
documented by the beneficiary’s Plan
of Care.
Services are provided by licensed
providers enrolled in Medicaid to
provide PDHC services.
The following services are not
covered:
- Before and after school care
- Medical equipment, supplies and
appliances
- Parenteral or enteral nutrition
- Infant food or formula
Prescribed medications are to be
provided each day by the
beneficiary’s parent/guardian.
Norma Seguin
225-342-7513

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
26
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Program of
All-Inclusive
Care for the
Elderly
(PACE)
Program
available in
New Orleans,
Baton Rouge,
Lafayette, and
Alexandria
area.
Beneficiaries are persons age 55 years
or older, who live in the PACE provider
service area, are certified to meet
nursing facility level of care and
financially eligible for Medicaid long-
term care.
Participation is voluntary and
beneficiaries may dis-enroll at any time.
All Medicaid and Medicare services,
both acute and long-term care
- Emphasis is on enabling
beneficiaries to remain in
community and enhance quality of
life.
- Interdisciplinary team performs
assessment and develops
individualized plan of care.
- Each PACE program serves a
specific geographic region.
- PACE programs bear financial risk
for all medical support services
required for beneficiaries.
- PACE programs receive a monthly
capitated payment for Medicaid and
Medicare eligible beneficiaries.
Office of Aging and
Adult Services (OAAS)
1-866-758-5035
PACE Greater New
Orleans
504-945-1531
Franciscan PACE
Baton Rouge
225-490-0640
Franciscan PACE
Lafayette
337- 470-4500
Trinity Health PACE
Alexandria
318- 206-1000

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
27
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Pharmacy
Services
Pharmacies
All Medicaid beneficiaries except some
who are Medicare/Medicaid dual
eligible.
Beneficiaries who are full benefit dual
eligible (Medicare/Medicaid) receive
their pharmacy benefits through
Medicare Part D.
Beneficiaries enrolled in an MCO with
only behavioral health services receive
prescription benefits through the fee-
for-service Medicaid program.
Covers prescription drugs
Exceptions:
• Cosmetic drugs (Except Accutane);
• Cough & cold preparations;
• Anorexics (Except for Xenical);
• Fertility drugs when used for
fertility treatment;
• Experimental drugs;
• Compounded prescriptions;
• Drug Efficacy Study
Implementation (DESI) drugs;
• Erectile Dysfunction (ED)
Medications
• Over the counter (OTC) drugs with
some exceptions;
Co-payments ($0.50-$3.00) are
required except for some beneficiary
categories.
NO co-payments for the following:
• Under age 21
• Pregnant women
• Long Term Care beneficiaries
• American Indians/Alaska Natives
• Home and Community Based
Waiver
• Emergency Services
• Family planning services
• Preventive medications as
designated by the US Preventive
Services Task Force A and B
Recommendations
• Individuals receiving hospice care
• Women whose basis of Medicaid
eligibility is breast or cervical
cancer
Prescription limits:
4 per calendar month (The physician
can override this limit when medically
necessary.)
Limits do not apply to beneficiaries
under age 21, pregnant women, or
those in Long Term Care.
Prior Authorization is required for
some drug categories if the medication
is not on the Preferred Drug List
(PDL). Children are not exempt
from this process. The PDL can be
accessed at www.lamedicaid.com.
Gabriell Johnson-
Stewart
225-219-4151
Sue Fontenot
225-342-2768
General pharmacy
questions
1-800-437-9101

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
28
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Physical
Therapy
See: EarlySteps; Home Health; Hospital-Outpatient Services; Rehabilitation Clinic Services; Therapy Services
Physician
Assistants
See FQHC; Physician/Professional Services; Rural Health Clinics
Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
29
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Physician/
Professional
Services
Physician or
Healthcare
Professional
All Medicaid beneficiaries.
Professional medical services including
those of a physician, nurse midwife,
nurse practitioner, clinical nurse
specialists, physician assistant.
Certain family planning services when
provided in a physician’s office.
Some services require Prior
Authorization. Providers will submit
requests for Prior Authorization to
Gainwell Technologies.
Services are subject to limitations and
exclusions. Your physician or
healthcare professional can help with
this.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
For immunizations:
Norma Seguin
225-342-7513
For professional services:
Crystal Faison
225-342-8233

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
30
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Podiatry
Services
Podiatrist
All Medicaid beneficiaries.
Office visits.
Certain radiology & lab procedures and
other diagnostic procedures.
Some Prior Authorization,
exclusions, and restrictions apply.
Providers will submit request for
Prior Authorization to Gainwell
Technologies.
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
31
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Pre-Natal Care
Services
Physicians or
Healthcare
Professional
Female Medicaid beneficiaries of child
bearing age.
• Office visits
• Lab and radiology services
NOTE: The contact person and
number provided should not be
utilized for making appointments.
Beneficiaries that are enrolled with
one of the Healthy Louisiana plans
should contact Healthy Louisiana via
the information below:
Web
https://www.myplan.healthy.la.gov/en
Phone
1-855-229-6848
Monday through Friday from 8:00
a.m. to 5:00 p.m.
For hearing impaired (TTY) please
call 1-855-526-3346.
Mail
Healthy Louisiana
P.O. Box 1097
Atlanta, GA 30301-9913
Fax
1-888-858-3875
Crystal Faison
225-342-8233
Psychiatric
Hospital Care
Services
See Hospital – Inpatient Services
Rehabilitation
Clinic Services
Physician
Medicaid beneficiaries 0 through 20
years of age.
• Occupational Therapy
• Physical Therapy
• Speech, Language and Hearing
Therapy
All services must be Prior
Authorized.
The provider of services will submit
the request for Prior Authorization.
Justin Owens
225-342-6888

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
32
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Rural Health
Clinics
Rural Health
Clinic
The American
Indian Clinic
All Medicaid beneficiaries.
Professional medical services furnished
by physicians, nurse practitioners,
physician assistants, nurse midwives,
clinical social workers, clinical
psychologists, and dentists.
Covered benefits include medical,
behavioral health, and dental.
There are 3 components that may be
provided:
1. Encounter visits;
2. EPSDT Screening Services; and
3. EPDST Dental, and Adult Denture
Services.
Irma Gauthier
225-342-5691
Sexually
Transmitted
Disease Clinics
(STD)
OPH Public
Health Units
All Medicaid beneficiaries.
Testing, counseling, and treatment of all
sexually transmitted diseases (STD).
Confidential HIV testing.
Public Health Unit
Directory
http://ldh.la.gov/index.cfm
/directory/category/192
Speech and
Language
Evaluation and
Therapy
See: EarlySteps; Home Health; Hospital – Outpatient Services; Rehabilitation Clinic Services; Therapy Services
Support
Coordination
Services (Case
Management) –
Children’s
Choice Waiver
See: Eligibility
Medicaid beneficiaries must be in the
Children’s Choice Waiver.
There is a Request for Services
Registry (RFSR) for those requesting
waiver services. To get on the RFSR,
call the Office for Citizens with
Developmental Disabilities
District/Authority/Local Regional
Office.
Contact information is located at:
http://ldh.la.gov/index.cfm/page/134/n/1
37
Coordination of Medicaid and other
services. The Support Coordinator (Case
Manager) helps to identify needs, access
services and coordinate care.
Services available through the Waiver
are identified in the waiver section of
this document.
Support Coordination services must
be prior authorized by LDH, Office
for Citizens with Developmental
Disabilities, Waiver Supports and
Services.
The Support Coordination Agency
will submit requests for the Prior
Authorization.
Office for Citizens with
Developmental
Disabilities (OCDD),
Waiver Supports and
Services
1-866-783-5553
Complaint Line:
1-800-660-0488

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
33
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Support
Coordination
Services (Case
Management) –
Community
Choices
Waiver
See: Eligibility
Medicaid beneficiaries must be in the
Community Choices Waiver (CCW).
There is a Request for Services
Registry (RFSR) for those requesting
waiver services. To get on the RFSR,
contact Louisiana Options in Long Term
Care at 1-877-456-1146.
Coordination of Medicaid and other
services. The Support Coordinator (Case
Manager) helps to identify needs, access
services and coordinate care.
Services available through the Waiver
are identified in the waiver section of
this document.
Support Coordination services must
be prior authorized by LDH, Office
of Aging and Adult Services (OAAS).
The Support Coordination Agency
will submit requests for the Prior
Authorization.
Office of Aging and
Adult Services (OAAS)
1-866-758-5035
Beneficiaries should call
1-866-758-5035 or
225-219-0643
Support
Coordination
Services (Case
Management) –
EPSDT
Targeted
Populations
See: Eligibility
Must be Medicaid eligible and on the
DD Request for Services Registry
(RFSR) prior to receipt of case
management services; or any
Medicaid beneficiaries 3 through 20
years of age for whom support
coordination is medically necessary.
To get on the RFSR, call the Office for
Citizens with Developmental
Disabilities District/Authority/Local
Regional Office.
Coordination of Medicaid and other
services. The Support Coordinator (Case
Manager) helps to identify needs, access
services and coordinate care.
Support Coordination services must
be prior authorized by LDH, BHSF,
and Medicaid Program Support &
Waivers (MPSW) Section.
The Support Coordination Agency
will submit requests for the Prior
Authorization to SRI.
For other EPSDT services, see that
portion of the chart.
SRI
1-800-364-7828
Must be on the DD
Request for Services
Registry. However, if the
beneficiary is no longer
eligible to remain on the
registry, the family can
appeal the notice that is
sent out.
MPSW will evaluate the
beneficiary’s eligibility to
receive “special needs”
case management.
Tracy Barker
225-342-8156
Support
Coordination
Services (Case
Management) –
Infants and
Toddlers
See: Eligibility
Medicaid beneficiaries must be 0 to 3
years of age and have a developmental
delay or an established medical
condition and eligible for the EarlySteps
program.
Contact information is located at:
http://ldh.la.gov/index.cfm/page/139/n/1
39
Coordination of Medicaid and other
services. The Support Coordinator (Case
Manager) helps to identify needs, access
services and coordinate care in
EarlySteps.
Support Coordination services must
be prior authorized by EarlySteps.
Prior Authorizations are approved
through the Individualized Family
Service Plan (IFSP) process.
Office for Citizens with
Developmental
Disabilities (OCDD)
1-866-783-5553
Caroline Oglesby
225-342-8853

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
34
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Support
Coordination
Services (Case
Management) –
New
Opportunities
Waiver
See: Eligibility
Medicaid beneficiaries must be in the
New Opportunities Waiver.
There is a Request for Services
Registry (RFSR) for those requesting
waiver services. To get on the RFSR,
call the Office for Citizens with
Developmental Disabilities
District/Authority/Local Regional
Office.
Contact information is located at:
http://ldh.la.gov/index.cfm/page/134/n/1
37
Coordination of Medicaid and other
services. The Support Coordinator (Case
Manager) helps to identify needs, access
services and coordinate care.
Services available through the Waiver
are identified in the waiver section of
this document.
Support Coordination services must
be prior authorized by LDH, Office
for Citizens with Developmental
Disabilities, Waiver Supports and
Services.
The Support Coordination Agency
will submit requests for the Prior
Authorization.
Office for Citizens with
Developmental
Disabilities (OCDD),
Waiver Supports and
Services
1-866-783-5553
Complaint Line:
1-800-660-0488
Support
Coordination
Services (Case
Management) –
Residential
Options
Waiver
See: Eligibility
Medicaid beneficiaries must be in the
Residential Options Waiver.
There is a Request for Services
Registry (RFSR) for those requesting
waiver services. To get on the RFSR,
call the Office for Citizens with
Developmental Disabilities
District/Authority/Local Regional
Office.
Contact information is located at:
http://ldh.la.gov/index.cfm/page/134/n/1
37
Coordination of Medicaid and other
services. The Support Coordinator (Case
Manager) helps to identify needs, access
services and coordinate care.
Services available through the Waiver
are identified in the waiver section of
this document.
Support Coordination services must
be prior authorized by LDH, Office
for Citizens with Developmental
Disabilities, Waiver Supports and
Services.
The Support Coordination Agency
will submit requests for the Prior
Authorization.
Office for Citizens with
Developmental
Disabilities (OCDD),
Waiver Supports and
Services
1-866-783-5553
Complaint Line:
1-800-660-0488

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
35
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Support
Coordination
Services (Case
Management) –
Supports
Waiver
See: Eligibility
Medicaid beneficiaries must be in the
Supports Waiver.
There is a Request for Services
Registry (RFSR) for those requesting
this waiver. To get on the RFSR, call
the Office for Citizens with
Developmental Disabilities
District/Authority/Local Regional
Office.
Contact information is located at:
http://ldh.la.gov/index.cfm/page/134/n/1
37
Coordination of Medicaid and other
services. The Support Coordination
(Case Manager) helps to identify needs,
access services and coordinate care.
Some services available through this
waiver are identified in the waiver
section of this document.
Support Coordination services must
be prior authorized by LDH, Office
for Citizens with Developmental
Disabilities, Waiver Supports and
Services.
The Support Coordination Agency
will submit requests for the Prior
Authorization.
Office for Citizens with
Developmental
Disabilities (OCDD),
Waiver Supports and
Services
1-866-783-5553
Complaint Line:
1-800-660-0488
Therapy
Services
Beneficiaries
have the choice
of services from
the following
provider types:
Home Health;
Hospital –
Outpatient
Services;
Rehabilitation
Clinic Services
Medicaid beneficiaries 0 through 20
years of age.
• Audiological Services (Available in
Rehabilitation Clinic and Hospital-
Outpatient settings only.)
• Occupational Therapy
• Physical Therapy
• Speech & Language Therapy
Covered services can be provided in
the home through Home Health and
Rehabilitation Clinics. Services
provided by Rehabilitation Clinics can
also be provided at the clinic. Services
provided through Hospital –
Outpatient Services must be provided
at the facility/clinic. Covered services
may be provided in addition to
services provided by EarlySteps/EICs
or School Boards if prescribed by a
physician and prior authorized.
All medically necessary services must
be prescribed by a physician and
Prior Authorization is required.
The provider of services will submit
requests for Prior Authorization.
Justin Owens
225-342-6888
NOTE: For details on
services provided in Home
Health, Rehabilitation
Clinic, or Hospital –
Outpatient settings,
please refer to those
sections of this Medicaid
Services Chart.

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
36
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Therapy
Services
(continued)
EPSDT Health
Services – Early
Intervention
Centers (EIC) or
EarlySteps
Program
Medicaid beneficiaries under 3 years of
age.
• Audiological Services
• Occupational Therapy
• Physical Therapy
• Speech & Language Therapy
• Psychological Therapy
All EPSDT Health Services through
EICs and EarlySteps must be included
in the infant/toddler’s Individualized
Family Services Plan (IFSP).
If services are provided by an EIC or
EarlySteps, Prior Authorization
requirements are met through
inclusion of services on the IFSP.
Caroline Oglesby
225-342-8932
EPSDT Health
Services –
Local Education
Agencies (LEA)
e.g. School
Boards
Medicaid beneficiaries 3 through 20
years of age.
• Audiology Services
• Behavioral Health Services
• Applied Behavioral Analyst Therapy
(ABA)
• Occupational, Physical, Speech and
Respiratory Therapy
• Optometry Services
• Personal Care Services
• Physician/Nursing Services
• Transportation
• Services are performed within
schools by Local Education
Agencies (LEAs).
• EPSDT Health Services on the
Medicaid approved Periodicity
Table may be reimbursed when
provided by a licensed practitioner
within the scope of their practice.
All other health services must be
included in a completed
authorizing document pursuant to
34 C.F.R. § 104.36:
- Individualized Education Plan
(IEP);
- Section 504 Accommodation
Plan;
- Individualized Health Care
Plan; or
- Any other medically necessary
written plan of care.
Anissa Young-Ned
225-342-6885
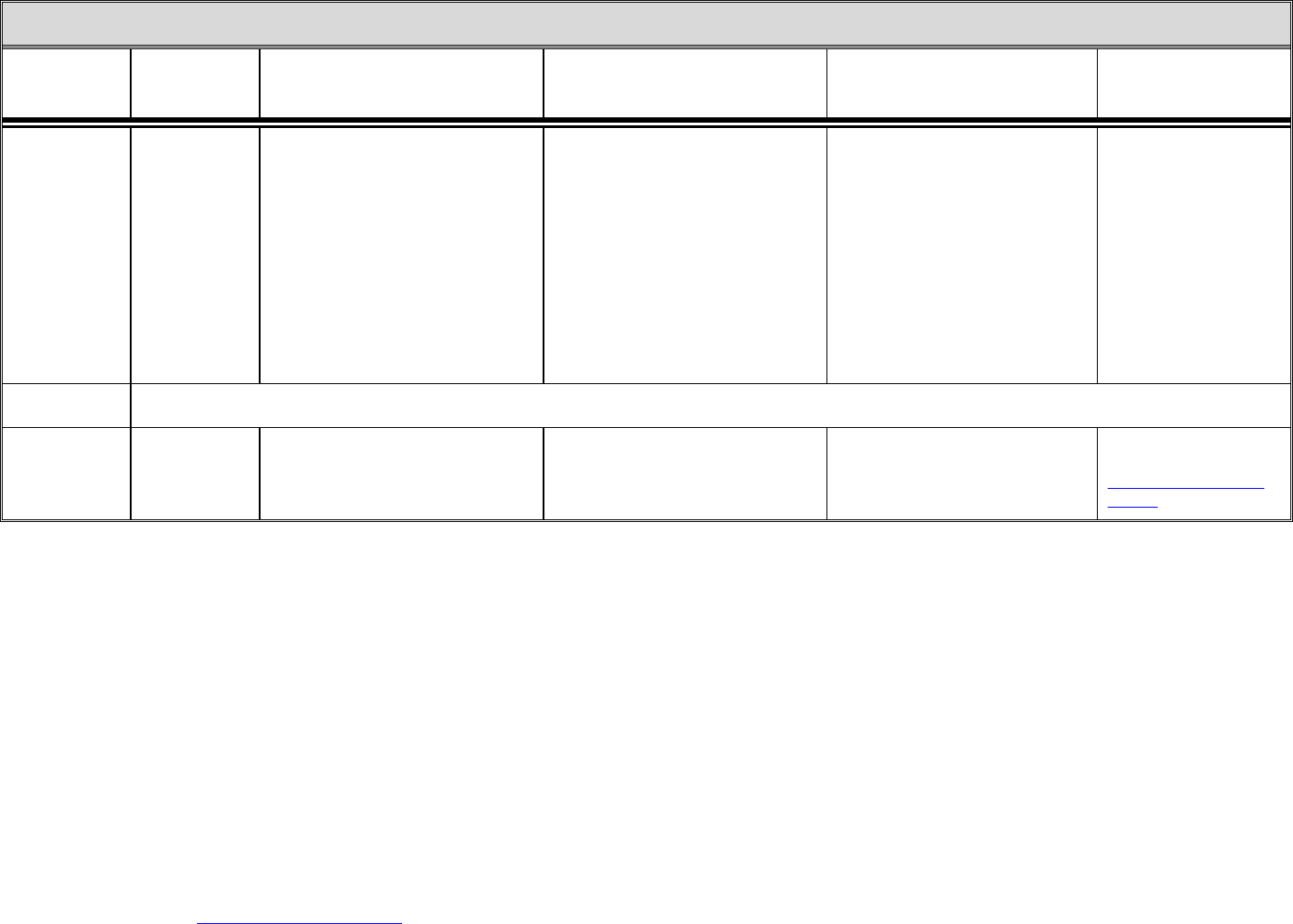
Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
37
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Therapy
Services
(continued)
Physician
Beneficiaries 21
years of age and
older may
access Therapy
Services
through
Hospital –
Outpatient
Services or
Home Health
Services.
Medicaid beneficiaries 21 years of age
and older.
Medically Needy (Type Case 20 & 21)
beneficiaries are not eligible for
Physical Therapy, Occupational
Therapy, and Speech/Language Therapy
in a Home Health setting.
• Physical Therapy
• Occupational Therapy
• Speech/Language Therapy
PT, OT, and Speech/Language
Therapy require a physician’s
prescription.
PT, OT, and Speech/Language
Therapy require Prior Authorization.
Justin Owens
225-342-6888
NOTE: For details on
services provided in Home
Health, Rehabilitation
Clinic, or Hospital –
Outpatient settings,
please refer to those
sections of this Medicaid
Services Chart.
Transportation
See: Medical Transportation
Tuberculosis
Clinics
Office of Public
Health Local
Health Unit
All Medicaid beneficiaries.
Treatment and disease management
services including physician visits,
medications and x-rays.
TB Control Directory
found at:
TBControlDirectory.pdf
(la.gov)

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
38
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Vision Services
(Eyewear)
Optometrist,
Ophthalmologist
or Optical
Supplier
Beneficiaries 0 through 20
Regular eyeglasses when they meet a
certain minimum strength requirement.
Medically necessary specialty eyewear
and contact lenses with prior
authorization. Contact lenses are
covered if they are the only means for
restoring vision.
Beneficiaries 21 and over
ONLY if the beneficiary receives both
Medicare and Medicaid, and Medicare
covers the required eyewear. In this
instance, Medicaid may pick up a
calculated portion of the payment as a
Medicare cross-over claim.
Beneficiaries 0 through 20
Specialty eyewear and contact lenses,
if medically necessary for EPSDT
beneficiaries, requires prior
authorization. The provider will
submit requests for the prior
authorization. A prior authorization
approval does not guarantee patient
eligibility.
Prescriptions are required for all
glasses/contacts. After a prescription
is obtained, the beneficiary may see
an optical supplier to receive the
glasses/contacts.
NON-COVERED SERVICES:
Beneficiaries 21 and over
Eyeglasses
Irma Gauthier
225-342-5691
X-Ray Services
See: Laboratory Tests and Radiology Services
WAIVER SERVICES
There is a Request for Services Registry (RFSR) for those requesting any of the waiver services below.
Adult Day
Health Care
(ADHC)
Waiver
To get on the
Request for
Services
Registry
(RFSR), contact
Louisiana
Options in Long
Term Care at
1-877-456-1146.
Beneficiaries 65 years of age or older,
who meet Medicaid financial eligibility,
imminent risk criteria and meet the
criteria for admission to a nursing
facility; or age 22-64 who are disabled
according to Medicaid standards or SSI
disability criteria, meet Medicaid
financial eligibility and meet the criteria
for admission to a nursing facility.
- ADHC services
- Transition Services
- Support Coordination
- Transition Intensive Support
Coordination
- Activity and Sensor Monitoring
- ADHC Health Status Monitoring
- Assistive Technology
- Home Delivered Meals
- Personal Emergency Response
System
This is a home and community-based
alternative to nursing facility
placement.
Louisiana Options in
Long Term Care
(Conduent)
1-877-456-1146
Office of Aging and
Adult Services (OAAS)
1-866-758-5035
Beneficiaries should call
1-866-758-5035 or
225-219-0643

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
39
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Children’s
Choice (CC)
Waiver
To get on the
Request for
Services
Registry
(RFSR), call the
Office for
Citizens with
Developmental
Disabilities
District /
Authority /
Local Regional
Office.
Contact
information is
located at:
http://ldh.la.gov/
index.cfm/page/
134/n/137
Child must be on the DD Request for
Services Registry (RFSR), less than 21
years old, disabled according to SSI
criteria, require ICF/DD level of care,
have income less than 3 times SSI
amount, resources less than $2,000 and
meet all Medicaid non-financial
requirements.
- Support Coordination
- Center Based Respite
- Environmental Accessibility
Adaptations
- Specialized Medical Equipment and
Supplies, including Remote
Technology (Incontinence Supplies
are covered under DME for
beneficiaries age 4 through 20)
- Family Training
- Professional Services: Aquatic
Therapy, Art Therapy, Music
Therapy, Sensory Integration,
Hippotherapy/Therapeutic Horseback
Riding
- Housing Stabilization/Housing
Stabilization Transition -Crisis and
Non-Crisis Provisions
- Financial Management Services
There is a $20,200 limit per individual
plan year. ($1,950 for Support
Coordination balance for other
services).
Call the Office for Citizens with
Developmental Disabilities or Local
Districts/Authorities for status on the
Request for Services Registry.
Office for Citizens with
Developmental
Disabilities (OCDD)
Districts / Authorities
/
Local Regional Offices
(SYSTEM ENTRY)
http://ldh.la.gov/index.cfm
/page/134/n/137
Tracy Joshua-Guy
225-342-0943
Complaint Line:
1-800-660-0488

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
40
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Community
Choices
Waiver (CCW)
To get on the
Request for
Services
Registry
(RFSR), contact
Louisiana
Options in Long
Term Care at
1-877-456-1146.
Beneficiaries 65 years of age or older,
who meet Medicaid financial eligibility
and meet the criteria for admission to a
nursing facility; or age 21-64 who are
disabled according to Medicaid
standards or SSI disability criteria, meet
Medicaid financial eligibility, and meet
the criteria for admission to a nursing
facility
- Support Coordination
- Environmental Accessibility
Adaptations
- Transition Intensive Support
Coordination
- Transition Services
- Personal Assistance Services
- Adult Day Health Care Services
- Monitored In-Home Caregiving
- Assistive Devices and Medical
Supplies
- Assistive Technology
- Skilled Maintenance Therapy:
Physical, Occupational, and Speech
- Nursing Services
- Home Delivered Meals
- Personal Emergency Response
System
- Caregiver Temporary Support
Services
- Financial Management Services
- Permanent Supportive Housing
This is a home and community-based
alternative to nursing facility
placement.
Louisiana Options in
Long Term Care
(Conduent)
1-877-456-1146
Office of Aging and
Adult Services (OAAS)
1-866-758-5035
Beneficiaries should call
1-866-758-5035 or
225-219-0643

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
41
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
New
Opportunities
Waiver (NOW)
To get on the
Request for
Services
Registry
(RFSR), call the
Office for
Citizens with
Developmental
Disabilities
District /
Authority /
Local Regional
Office.
Contact
information is
located at:
http://ldh.la.gov/
index.cfm/page/
134/n/137
Beneficiaries three (3) years of age or
older who have a developmental
disability as defined in LA R.S.
28:451.2. who are disabled according to
Medicaid standards or SSI disability
criteria, meet all Medicaid financial and
non- financial eligibility criteria.
- Individual Family Support: Day,
Night, and Shared Supports
- Center Based Respite
- Community Life Engagement
Development
- Environmental Accessibility
Adaptations
- Specialized Medical Equipment and
Supplies, including Incontinence
Supplies and Remote Technology
- Substitute Family Care Services
- Supported Independent Living
- Day Habilitation
- Supported Employment: Individual
and Group
- Prevocational Services
- Professional Services:
Dietician/Nutritionist, Psychologist,
Social Worker
- One Time Transitional Expense
- Skilled Nursing
- Housing Stabilization/Housing
Stabilization Transition
- Personal Emergency Response
System
- Monitored In-Home Caregiving
- Financial Management Services
- Dental Services
- Adult Companion Care
Call the Office for Citizens with
Developmental Disabilities or local
Districts/Authorities for status on the
Request for Services Registry.
Office for Citizens with
Developmental
Disabilities (OCDD)
Districts / Authorities
/
Local Regional Offices
(SYSTEM ENTRY)
http://ldh.la.gov/index.cfm
/page/134/n/137
Ed Harris
225-342-8537
Complaint Line:
1-800-660-0488

Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
42
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Residential
Options
Waiver (ROW)
To get on the
Request for
Services
Registry
(RFSR), call the
Office for
Citizens with
Developmental
Disabilities
District /
Authority /
Local Regional
Office.
Contact
information is
located at:
http://ldh.la.gov/
index.cfm/page/
134/n/137
Beneficiaries, birth to end of life, who
have a developmental disability as
defined in LA R.S. 28:451.2. who are
disabled according to Medicaid
standards or SSI disability criteria, meet
all Medicaid financial and non- financial
eligibility criteria.
- Support Coordination
- Community Living Supports
- Host Home Services
- Companion Care Services
- Shared Living
- Respite Care-Out of Home
- Personal Emergency Response
System
- One Time Transition Services
- Environmental Accessibility
Adaptations
- Assistive Technology/Specialized
Medical Equipment and Supplies,
including Incontinence Supplies and
Remote Technology
- Transportation – Community Access
- Professional Services: Speech
Therapy, Occupational Therapy,
Physical Therapy, Social Work, and
Psychological Services
- Nursing Services
- Dental Services
- Supported Employment
- Prevocational Services
- Day Habilitation
- Housing Stabilization/Housing
Stabilization Transition
- Adult Day Health Care
- Monitored In-Home Caregiving
- Financial Management Services
- Community Life Engagement
Development
Call the Office for Citizens with
Developmental Disabilities or local
Districts/Authorities for status on the
Request for Services Registry
(RFSR).
Office for Citizens with
Developmental
Disabilities (OCDD)
Districts / Authorities
/
Local Regional Offices
(SYSTEM ENTRY)
http://ldh.la.gov/index.cfm
/page/134/n/137
Office for Citizens with
Developmental
Disabilities (OCDD),
Waiver Supports and
Services
1-866-783-5553
Denise Boyd
225-342-0095
Complaint Line:
1-800-660-0488
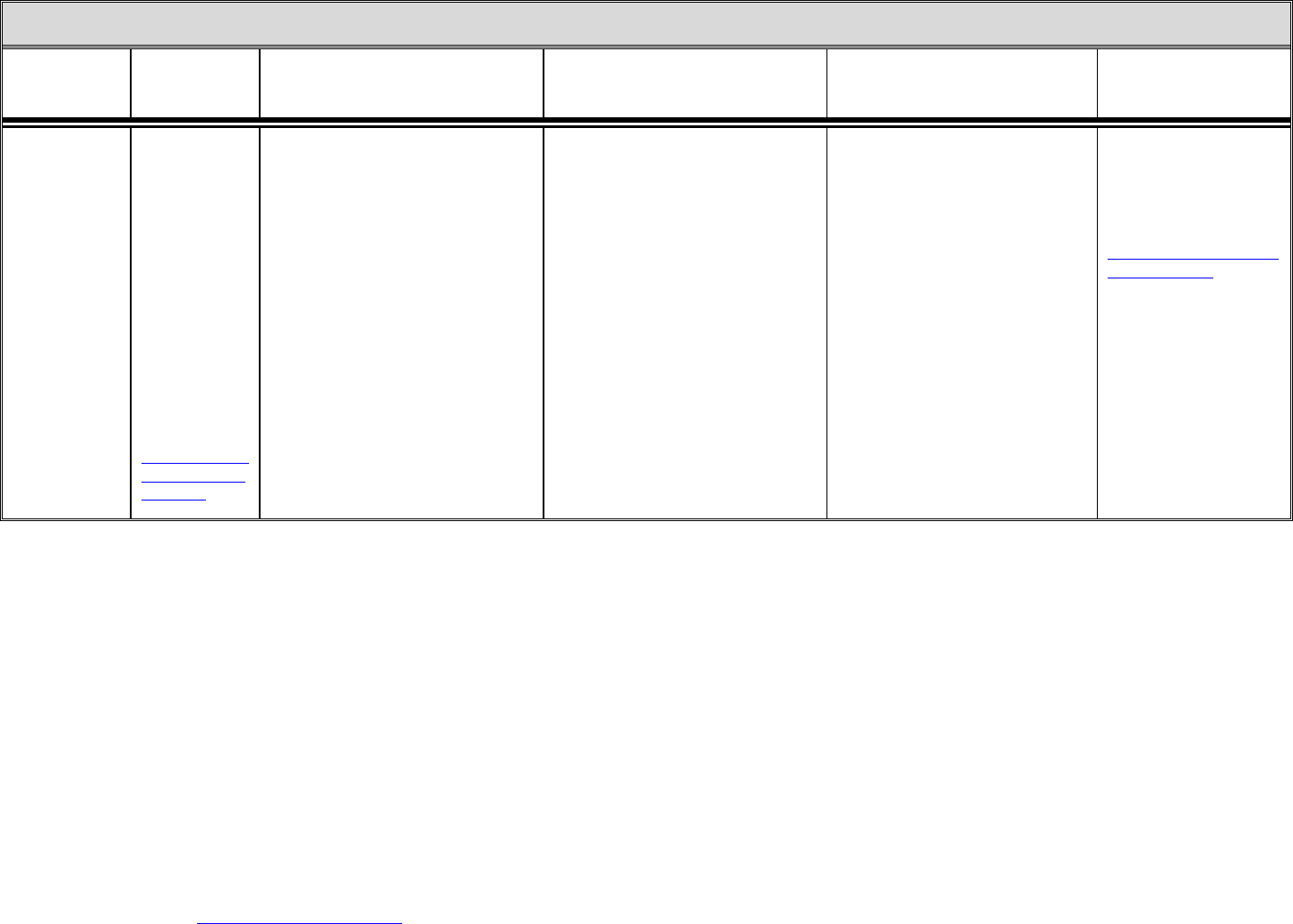
Exclusion from this list does not necessarily mean that a service is not covered. Please call one of the appropriate contacts for questions regarding coverage of services not listed on
this chart. NOTE: The points of contact listed in this document is applicable to Medicaid beneficiaries in the fee-for-service Medicaid program. Healthy Louisiana Plan members
should contact their Plan’s member services department with questions about how to access care.
43
MEDICAID SERVICES
SERVICE
HOW TO
ACCESS
SERVICES
ELIGIBILITY COVERED SERVICES COMMENTS CONTACT PERSON
Supports
Waiver (SW)
To get on the
Request for
Services
Registry
(RFSR), call the
Office for
Citizens with
Developmental
Disabilities
District /
Authority /
Local Regional
Office.
Contact
information is
located at:
http://ldh.la.gov/
index.cfm/page/
134/n/137
Beneficiaries 18 and older who have a
developmental disability as defined in
LA R.S. 28:451.2. who are disabled
according to Medicaid standards or SSI
disability criteria, and meet Medicaid
financial and non- financial eligibility,
and meet all Medicaid non-financial
requirements.
- Support Coordination
- Supported Employment
- Day Habilitation
- Prevocational Services
- Respite (In Home and Center Based)
- Personal Emergency Response
System
- Housing Stabilization
Transition/Housing Stabilization
Service
- Habilitation
- Specialized Medical Equipment and
Supplies, including Incontinence
Supplies and Remote Technology
- Dental Services
- Community Life Engagement
Development
Call the Office for Citizens with
Developmental Disabilities or local
Districts/Authorities for status on the
Request for Services Registry
(RFSR).
Office for Citizens with
Developmental
Disabilities (OCDD)
Districts / Authorities
/
Local Regional Offices
(SYSTEM ENTRY)
http://ldh.la.gov/index.cfm
/page/134/n/137
Rosemary Morales
225/342-0095
Complaint Line:
1-800-660-0488
