
EVERNORTH Coverage Policy: EN0086 1
Behavioral Health Coverage Policy
Effective Date 02/15/2024
Next Review Date 02/15/2025
Coverage Policy Number EN0086
Complementary and Alternative Medicine
Table of Contents
Overview .............................................................. 2
Coverage Policy ................................................... 2
General Background ............................................ 4
Medicare Coverage Determinations .................. 36
Coding Information ............................................ 37
References ........................................................ 39
Revision Details ................................................. 57
Related Coverage Resources
Acupuncture
Atherosclerotic Cardiovascular Disease Risk
Assessment: Emerging Laboratory Evaluations
Attention-Deficit/Hyperactivity Disorder (ADHD):
Assessment and Treatment
Autism Spectrum Disorders/Pervasive Developmental
Disorders: Assessment and Treatment
Biofeedback
Chiropractic Care
Drug Testing
Hyperbaric and Topical Oxygen Therapies
Physical Therapy
INSTRUCTIONS FOR USE
Coverage Policies are intended to provide guidance in interpreting benefit plans administered by Evernorth
Behavioral Health, Inc. Please note, the terms of a customer’s particular benefit plan document [Group Service
Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan
document] may differ significantly from the standard benefit plans upon which these Coverage Policies are
based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic
addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always
supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage
mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage
determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan
document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source
materials including Coverage Policies and; 4) the specific facts of the particular situation. Each coverage request
should be reviewed on its own merits. Medical directors are expected to exercise clinical judgment where
appropriate and have discretion in making individual coverage determinations. Where coverage for care or
services does not depend on specific circumstances, reimbursement will only be provided if a requested
service(s) is submitted in accordance with the relevant criteria outlined in the applicable Coverage Policy,
including covered diagnosis and/or procedure code(s). Reimbursement is not allowed for services when billed for
conditions or diagnoses that are not covered under this Coverage Policy (see “Coding Information” below).
When billing, providers must use the most appropriate codes as of the effective date of the submission. Claims
submitted for services that are not accompanied by covered code(s) under the applicable Coverage Policy will
be denied as not covered. Coverage Policies relate exclusively to the administration of health benefit plans.
Coverage Policies are not recommendations for treatment and should never be used as treatment guidelines.

Page 2 of 57
Medical Coverage Policy: EN0086
Overview
This Coverage Policy addresses complementary and alternative medicine diagnostic testing methods, systems,
therapies and treatments that are proposed to reduce disease-based clinical symptoms and improve health and
wellness.
Coverage Policy
Coverage for complementary and alternative testing and therapies varies across plans. Please refer to
the customer’s benefit plan document for coverage details.
For information on Acupuncture and Biofeedback, refer to the applicable Cigna Coverage Policies.
Each of the following complementary or alternative medicine diagnostic testing methods, systems,
therapies or treatments is considered experimental, investigational or unproven:
Category
Therapy
Diagnostic testing methods
• applied kinesiology (AK)
• chemical hair analysis
• Greek cancer cure test
• iridology
• live blood cell analysis
• nutrient panel testing, including micronutrient panel testing
• antioxidant function testing (e.g., Spectrox™)
• Ream's Testing
• salivary hormone panels
Whole medical systems
• Ayurveda
• homeopathy
• macrobiotics
• naprapathy
• naturopathy
• polarity therapy
Biologically-based practices
• antineoplastons
• auto urine therapy
• cellular therapy
• Coley’s Toxin
• hydrogen peroxide, intravenous
• immunoaugmentative therapy
• Kelley-Gonzales therapy
• Laetrile
• megavitamin therapy
• MTH-68
• over-the-counter biologics (e.g., glucosamide, coenzyme
Q10, fish oil [omega-3 fatty acids])
• ozone therapy
• Revici’s Guided Chemotherapy
• Trichuris suis ova therapy
Energy medicine
• acupressure
• biofield therapeutics
• crystal healing
• cupping
• gemstone therapy
• magnet therapy
• magnetic resonance therapy

EVERNORTH Coverage Policy: EN0086 3
Category
Therapy
• meridian therapy
• millimeter wave therapy
• moxibustion therapy
• Qigong Longevity
• Reiki
• therapeutic touch
Manipulative and body-based methods
• Alexander’s technique
• AMMA Therapy
®
• Bio Photonic Lymphatic Drainage
Treatment (BELD)
• colonic irrigation, colonic lavage, colonic cleansing
• craniosacral therapy
• ear candling
• Feldenkrais therapy
• inversion therapy
• myotherapy
• neural therapy
• Pfrimmer Deep Muscle Therapy
®
• Pilates
• reflexology (zone therapy)
• remedial massage
• Rolfing
• Trager
®
• Tui Na
• visceral massage
Mind-body medicine
• art therapy
• bioenergetics’ analysis
• color therapy
• dance movement therapy
• equestrian therapy (hippotherapy)
• faith healing
• guided imagery interactive
• Hellerwork
• humor therapy
• hypnosis
• Martial Arts including Chung Moo Doe therapy
• meditation/Transcendental Meditation (TM
®
)
• mirror box therapy
• music therapy
• outdoor youth programs
• pet therapy
• primal therapy
• psychodrama
• recreational therapy
• wilderness therapy
• yoga
Prescription medications are generally subject to a separate pharmacy benefit. Many pharmacy and
medical benefit plans specifically exclude coverage of over-the-counter (OTC) medications, including
OTC vitamins and nutritional and dietary supplements.

EVERNORTH Coverage Policy: EN0086 4
General Background
Complementary and alternative medicine (CAM), also called unconventional, nonconventional, or nontraditional
healthcare, is a group of diverse medical and healthcare systems, practices and products that are not typically
considered to be part of traditional Western medicine (i.e., conventional medicine). CAM assessments and
therapies are proposed to reduce disease-based clinical symptoms and improve health and wellness.
Complementary medicine may be used in conjunction with Western medicine, as opposed to alternative
medicine which may be used in place of Western medicine. Integrative medicine, as defined by the National
Center for Complementary and Alternative Medicine (NCCAM), combines conventional medical therapies and
CAM therapies for which there is scientific evidence of safety and effectiveness (NCCAM, 2016; updated 2018).
Classifications of CAM practices include the following:
• Whole Medical Systems: Whole medical systems are built upon complete systems of theory and
practice. Often, these systems have evolved apart from, and earlier than, the conventional medical
approach used in the United States.
• Biologically-Based Practices: Biologically-based practices, also referred to as natural products, in
CAM use substances found in nature including herbs, foods, and vitamins. Examples of these
substances include dietary supplements, herbal products, and other natural products that have not been
scientifically proven (e.g., using shark cartilage to treat cancer).
• Energy Medicine: Energy medicine involves the use of energy fields and consists of two types of
therapies:
Biofield therapies are intended to affect energy fields that purportedly surround and penetrate
the human body. The existence of such fields has not yet been scientifically proven. Some forms
of energy therapy are proposed to manipulate biofields by applying pressure, heat or body
manipulation.
Bioelectromagnetic-based therapies involve the unconventional use of electromagnetic fields,
such as pulsed fields, magnetic fields, or alternating current or direct current fields.
• Manipulative and Body-Based Methods: Manipulative and body-based methods are based on
manipulation and/or movement of one or more parts of the body.
• Mind-Body Medicine: Mind-body medicine uses a variety of techniques designed to enhance the mind's
capacity to affect bodily function and symptoms.
Some CAM therapies are supported by some degree of scientific evidence, but most of the other CAM therapies
lack data in the peer-reviewed published evidence supporting the safety and efficacy of these therapies for
specific conditions and are not yet considered an established treatment option.
U.S. Food and Drug Administration (FDA)
The Federal Food and Drug Act of 1906, The Wiley Act, empowers the FDA Center for Food Safety and Nutrition
to remove unsafe food substances and botanicals from the market, and gives the FDA regulatory oversight for
substances added to food, including monitoring safe use. The FDA maintains that a drug is any substance or
mixture of substances intended for the cure, mitigation, diagnosis or prevention of disease (FDA, 2009; updated
2019).
Dietary supplements are regulated differently than prescription and over-the-counter drug products.
Manufacturers of dietary supplements are responsible for ensuring that their products are safe. While the FDA
monitors adverse effects after dietary supplement products are on the market, newly marketed dietary
supplements are not subject to premarket approval or a specific post-market surveillance period. Per the Dietary
Supplement Health and Education Act of 1994 (DSHEA), the burden of proof rests on the FDA to show that a
product is unsafe. Manufacturers are not required to submit substantiation of benefit data to the FDA. The
Federal Trade Commission (FTC) is charged with accurate marketing and advertising claims (FDA, 2015;
updated 2019).
EVERNORTH Coverage Policy: EN0086 5
According to the FDA, dietary supplements in today’s market include one or a combination of: vitamins, minerals,
herbals, botanicals, amino acids, any dietary substance used to supplement the diet by increasing total dietary
intake, and a concentrate, metabolite, constituent or extract. The FDA states that, while some supplements may
help ensure that the individual consumes adequate amounts of essential nutrients needed for optimal health and
performance, dietary supplements cannot be promoted as a treatment or a cure.
In December 2006, the FDA issued a draft guidance document for the regulation of CAM products. The draft was
issued because increased use of CAM in the United States had caused confusion regarding which products are
subject to regulation under the Federal Food, Drug, and Cosmetic Act (Act) or the Public Health Service Act
(PHS Act) and because the number of CAM products being imported into the United States had increased. The
document provides guidance as to when a CAM product is subject to the Act or the PHS Act. The FDA cites the
NCCAM’s definition and categories of CAM in the draft. According to the new guidance, if the labeling of a
dietary supplement includes the term “to treat,” that supplement will be regulated as a drug under the Act.
Biological products (e.g., virus, therapeutic serum, toxin, antitoxin, vaccine) will be regulated under the PHS Act
(FDA, 2006; updated 2020).
Diagnostic Testing Methods
Applied Kinesiology (AK): AK is a form of diagnostic testing that uses muscle testing as a type of functional
neurological evaluation. According to their guidelines on allergy diagnostic testing, the American Academy of
Allergy, Asthma and Immunology and the American College of Allergy, Asthma and Immunology stated there is
“no evidence of diagnostic validity” of AK (Bernstein, et al., 2008).
Chemical Hair Analysis: Chemical hair analysis is a test in which a person’s hair is analyzed for mineral
content. Hair analysis has been proposed to aid in the evaluation of a person’s general state of health, mental
and physical conditions (e.g. autism, cancer, hypertension, myocardial infarction, kidney disease, osteoarthritis
and diabetes mellitus), skin diseases (e.g., alopecia), detect heavy metals (e.g., lead, mercury, arsenic) and
pesticides, identify nutritional/mineral deficiencies, analyze deoxyribonucleic acid (DNA), and identify the
presence of illegal drugs (e.g., cocaine, marijuana) (Guo, et al., 2019; Wolowiec, et al., 2013; Caprara, et al.,
2006; Balíková, 2005). However, evidence to support the accuracy and clinical utility of hair analysis is lacking.
Greek Cancer Cure: Greek cancer cure also known as METBAL
®
, Cellbal
®
, and Alivizatos, consists of a blood
test that allegedly diagnoses the location and extent of cancer in a person's body. Following diagnosis, treatment
consists of intravenous injections of a serum containing sugars, vitamins, amino acids, and other factors.
Available scientific evidence does not support claims that the Greek Cancer Cure is effective in preventing,
detecting, or treating cancer.
Iridology: Iridology sometimes referred to as iris diagnosis, is based on the belief that each area of the body is
represented by a corresponding area in the iris of the eye. According to their guidelines on allergy diagnostic
testing, the American Academy of Allergy, Asthma and Immunology and the American College of Allergy,
Asthma and Immunology stated there is “no evidence of diagnostic validity” of iridology (Bernstein, et al., 2008).
Live Blood Cell Analysis: Live blood cell analysis by dark field microscopy is an unproven means to study the
"biologic terrain" and offer practical, nutritional, herbal, and lifestyle solutions for various medical conditions. It
involves taking a drop of blood and viewing it under a microscope using a dark field condenser, allowing the
viewer to see all components of the blood and tiny particles to enable early detection of disease. There is
insufficient evidence to support the accuracy and clinical utility of live blood cell analysis.
Nutrient Panel Testing: Nutrient panel testing assesses the level of multiple nutrients in the body. These panels
may include measurement of numerous vitamins, minerals, amino acids, fatty acids, oxidation products, organic
acids, toxins and antioxidants. The test results are proposed to help determine the cause of various symptoms,
such as hair loss and fatigue, and various disease processes. Antioxidant function testing (e.g., Spectrox™) has
been proposed as a method to evaluate the ability of cells to resist damage caused by free radicals and other
forms of oxidative stress. SpectraCell Laboratories, Inc., (Houston, TX) offers a micronutrient testing panel
proposed to measure how micronutrients function within the white blood cell. The Individual Optimal Nutrition
(ION) (Genova Diagnostics, Asheville, NC) is a blood test that measures levels of vitamins, minerals,
antioxidants, and organic, fatty and amino acids. ExaTest
®
, offered by IntraCellular Diagnostics, Inc
®
(Bedford,

EVERNORTH Coverage Policy: EN0086 6
OR) is an intracellular tissue analysis of mineral electrolytes. The test is proposed to provide information on
mineral electrolyte deficiencies or imbalances not available by blood testing. The analysis is made from an
epithelial cell scraping from the sublingual area. The sample is analyzed using high energy photos (x-rays).
At this time, there is insufficient evidence in the published, peer-reviewed, scientific literature to establish the
clinical utility of nutrient panel testing or antioxidant function testing or to demonstrate that the use of such testing
results in improved health outcomes.
In their practice parameter for the screening and diagnosing of autism, the American Academy of Neurology and
the Child Neurology Society stated that there is insufficient evidence to support testing for micronutrients such as
vitamin levels (Filipek, et al., 2000; posted 2013).
Ream's Testing: Ream's Testing is promoted as a noninvasive investigation of the body's overall metabolic
function, utilizing urine and saliva samples. An individual’s pancreatic function, blood sugar control, pH levels,
digestive function, liver function, hydration status, mineral status, kidney and adrenal function, and systemic
inflammation are reviewed with recommendations made for diet, specific pH and supplementation of other
nutrients. It is used by proponents to monitor progress with various treatment regimes. There is insufficient
evidence to support the accuracy and clinical utility of Ream’s testing.
Salivary Hormone Panels: Salivary testing for various hormones in the form of hormone panels (i.e., testing
several different hormone levels in one test at the same time) has been proposed for numerous indications
including screening and monitoring of menopause, aging and various other conditions. Diagnos-Techs
™
, Inc.
(Kent, WA) offers several different types of these hormone panels including Post- and PeriMenopausal Hormone
Panels
™
. The Postmenopause Panel
™
(PostM
™
) is a diagnostic study that measures estrone (E1), estradiol (E2),
estriol (E3), progesterone (P), testosterone (T), dehydroepiandrosterone (DHEA), and dehydroepiandrosterone–
sulfate (DHEA-S). The Perimenopause Panel™ (PeriM™) measures the same six hormones as the PostM Panel
but two samples are analyzed 13-15 days apart. The initial sample is obtained, frozen and sent for analysis with
the second sample. The expanded Postmenopause Panel (ePostM™) and the expanded Perimenopause Panel
(ePeriM™) include analyses of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in addition to the
six hormones offered in the nonextended panels. Proposed clinical applications of these tests include: to monitor
women who are perimenopausal, postmenopausal or have had a total hysterectomy; to aid in risk assessment of
breast/uterine proliferative diseases; to detect early disruption in the hypothalamic pituitary ovarian axis in
women approaching menopause; to monitor FSH and LH and/or investigate libido changes and emotional
vulnerability problems (Diagnos-Tech, 2019).
Diagnos-Techs also offers Male Hormone Panels
™
performed on saliva samples. The regular Male Hormone
Panel
™
(MHP
™
) is proposed to evaluate the androgen pathway by measuring progesterone, DHEA, DHEA-S,
androstenedione, estrogens, dihydrotestosterone (DHT) and testosterone. The Expanded Male Hormone Panel
™
(eMHP
™
) includes the seven hormones plus follicle stimulating hormone (FSH) and luteinizing hormone (LH).
The proposed clinical utility of the test is to diagnose andropause and hypogonadism; monitor hormone
replacement therapy and balancing of hormones; investigate prostate hypertrophy, thinning of hair and hirsutism;
and evaluate low-libido.
The Adrenal Stress Index
™
(ASI), which analyzes five saliva samples, is proposed for evaluation of chronic
stress and fatigue, glycemic dysregulation, and chronic pain and inflammation. The ASI test includes cortisol,
DHEA-S, 17-Hydroxyprogesterone, two insulin tests (fasting and after meals), total secretory IgA (SigA), and
wheat gluten sigA for grain intolerance. The proposed indications for ASI are to evaluate stress and conditions
associated with adrenal disturbances such as chronic pain/fibromyalgia, chronic fatigue syndrome, glycemic
dysregulation, allergies, autoimmune disorders, depression and attention deficit disorders.
The Bone Health Panel
™
(BHP
™
) saliva test includes progesterone, estradiol, testosterone, cortisol, FSH and
DHEA and as a bone marker, Pyrilinks-D in urine. The panel is proposed for screening and monitoring for
osteoporosis, identifying high risk hip fracture patients and screening for metabolic bone diseases, rheumatoid
arthritis and other connective tissue diseases, Paget’s disease and bone malignancies.
There is insufficient evidence in the published peer-reviewed literature to support the clinical utility (e.g.,
appropriate medication dosage, diagnosis and monitoring menopause, risk assessment) of salivary hormone
EVERNORTH Coverage Policy: EN0086 7
panels. Studies comparing salivary hormone panels to established individual hormone serum testing and impact
on health outcomes are lacking.
In 2011 guidelines on the diagnosis and treatment of menopause, The American Association of Clinical
Endocrinologists (AACE) stated that salivary hormone level testing is recommended by many bioidentical
hormone proponents as a means of providing patients with “individualized” therapy, but the methods are not
approved by either the FDA or the Clinical Laboratory Improvement Amendments (CLIA). AACE noted that
“accurate studies have revealed large intrasubject variability in salivary sex hormone concentrations which
fluctuate depending on numerous variables (e.g., diet, hydration, circadian rhythm).” This guideline was
reaffirmed in 2017.
In a 2023 Committee Opinion on compounded bioidentical hormones (e.g., dehydroepiandrosterone,
pregnenolone, testosterone, progesterone, estrone, estradiol, and estriol), the American College of Obstetricians
and Gynecologists (ACOG) stated, “salivary testing does not offer accurate or precise assessment of hormone
levels”. ACOG goes on to explain that salivary levels do not consistently provide a reasonable representation of
endogenous, circulation serum hormones because of the large variability in salivary hormones depending on
diet, time of testing and the hormone being tested. Because the pharmacokinetics of exogenously administered
compounded hormones cannot be known, it is not possible to estimate with reliability how and when to test
saliva to obtain a representative result. Lastly, saliva contains far lower concentrations of hormone than serum
and is prone to contamination with blood, infections agents, and epithelia cells which may affect the level of
hormone to be measured. “Hormone levels should not be titrated to hormone levels (serum, urinary, or salivary).”
Currently, there are no FDA-approved salivary or urinary tests for steroid hormone measurement (ACOG, 2023).
Whole Medical Systems
Ayurveda: Ayurveda provides an integrated approach to preventing and treating illness through lifestyle, based
upon the premise that all disease begins with an imbalance or stress in the individual's consciousness. Lifestyle
interventions are a major Ayurvedic preventive and therapeutic approach and include diet and herbal remedies.
This approach emphasizes the use of body, mind and spirit in disease prevention and treatment.
Ng et al. (2019) conducted a systematic review of Withania somnifera (Ashwagandha), a popular herb in
Ayurvedic medicine, in managing cognitive dysfunction. Five randomized, placebo-controlled, double-blind
studies (n=267) were reviewed, but meta-analysis was unsuitable due to small number of trials and dissimilar
study designs and outcome measures. The studies’ diverse populations included children with intellectual
disabilities, healthy adults, older adults with mild cognitive impairment, and adults with schizophrenia,
schizoaffective disorder, or bipolar disorder. Withania somnifera was found to improve performance on cognitive
tasks and be well tolerated, with good adherence and minimal side effects in almost all of the studies. Limitations
of the studies included: heterogeneous small patient populations, limited clinical data and lack of follow-up.
Additional rigorous clinical trials with large, well-defined patient populations are needed to support meaningful
clinical outcome of Ashwaganda.
Homeopathy: Homeopathy is a complementary and alternative medicine system that has been proposed to
assist the body's efforts to heal physically, mentally, and emotionally. This system encompasses the belief that
"like cures like", meaning that small, highly diluted quantities of medicinal substances are given to cure
symptoms, when the same substances given at higher or more concentrated doses would actually cause those
symptoms. There are over 3000 homeopathic remedies. Homeopathic intravenous (IV) therapy or IV nutrient
therapy is the intravenous administration of multiple minerals, vitamins, amino acids, chelating agents, botanical
and/or herbal supplements to allow maximum concentrations of these substances in the body. IV therapy has
been proposed for the treatment of cancer, malabsorption syndromes (e.g., Crohn’s, colitis), metal toxicities,
infectious diseases (e.g., Epstein Barr, Lyme disease), and neurological disorders.
A Cochrane systematic review (Hawke, et al., 2018) of randomized controlled trials investigating oral
homeopathic medicinal products for the prevention and treatment of acute respiratory tract infections in children
(age <16 years) concluded that the evidence did not show any benefit of homeopathic medicinal products
compared to placebo. Eight randomized controlled trials (n=1562) met inclusion criteria. Limitations of the studies
included: methodological inconsistencies, high attrition rates, selective reporting, protocol deviations and unclear
or high risk of bias. Methodological inconsistencies and significant clinical and statistical heterogeneity precluded
robust quantitative meta-analysis.

EVERNORTH Coverage Policy: EN0086 8
Banerjee et al. (2017) conducted a systematic review of randomized controlled trials evaluating homeopathy for
allergic rhinitis. Eleven studies (n=1654) met inclusion criteria and ten were placebo-controlled trials. Six trials
used isopathy (i.e., the causal agent is used for the cure), but they were unsuitable for meta-analysis due to
problems of heterogeneity and data extraction. Patient populations ranged from 34–142. Due to the high level of
heterogeneity across studies in terms of medical condition and outcome measures and the poor quality of results
reported, only three studies could be used for meta-analysis. Meta-analysis of the three studies using Galphimia
glauca showed that relief of nasal and ocular symptoms favored homeopathy. A homeopathic and a conventional
nasal spray produced equivalent improvements in nasal and ocular symptoms. Due to the overall low or
uncertain quality of the evidence, firm conclusions could not be drawn about the clinical benefit of homeopathy
medicine for the treatment of allergic rhinitis.
Posadzki et al. (2012) conducted a systematic review of case series and case reports to evaluate adverse
effects (AEs) of homeopathy. Thirty-five case studies (n=1159) met inclusion criteria. Direct AEs included
abdominal pain, acute pancreatitis, severe allergic reactions, and nausea and vomiting. Occasionally
homeopathy was reported to result in serious outcomes (e.g., cancer, cardiac arrest, coma, death). Multiple
indirect AEs (e.g., hypertension, seizures, organ failure) were also reported. The duration of AEs ranged from 22
hours to seven months with four reported deaths.
Davidson et al. (2011) conducted a systematic review of randomized placebo-controlled trials (n=25) of
homeopathy for psychiatric conditions (i.e., anxiety, depression, sleep problems, attention-deficit/hyperactivity
disorder [ADHD], premenstrual syndrome [PMS], mild traumatic brain injury [TBI] and somatic spectrum
disorders). Efficacy was reported for fibromyalgia and chronic fatigue syndrome, but not for anxiety or stress.
Mixed effects were reported for the other disorders. No studies were found for depression. Meta-analysis could
not be performed due to the limited number of studies and heterogeneity of the data sets. The authors concluded
that firm conclusions about the safety and efficacy of homeopathy for any of these conditions could not be made.
Traumeel (Tr14) injection solution is a homeopathic combination formula consisting of 12 botanical and 2 mineral
substances with proposed anti-inflammatory, anti-edematous, anti-exudative properties (Vanden Bossche and
Vanderstraeten, 2015). Schneider et al. (2008) conducted an observational cohort study of 133 patients with
various musculoskeletal injuries, 69 treated with Traumeel injections and 64 conventionally treated. A greater
number of patients reported complete resolution of the principal symptom with no adverse events. Physician-
assessed tolerability was significantly better in the patients that received Traumeel. In addition to the small
patient population, the studies were limited by the heterogeneous selection of type of injuries. Additional studies
with larger patient populations and long-term evaluations are needed to establish the safety and effectiveness of
Tr14.
Macrobiotics: Macrobiotics is the art and science of health and longevity through the study and understanding
of the relation and interactions between oneself, foods, lifestyles, and the environment. The clinical utility of
macrobiotics has not been established.
Naprapathy: Naprapathy or naprapathic medicine is a system that employs manual medicine (e.g., spinal
manipulation), nutritional counseling and therapeutic modalities (e.g., heat, cold, ultrasound, electrical
stimulation) for the treatment of pain caused by connective tissue disorders. Naprapaths are connective tissue
specialists who propose to have a specialized, holistic approach to address connective tissue problems
(American Naprapathic Association, 2020).
Naturopathy: Naturopathy is a system of healing that views disease as a manifestation of alterations in the
processes by which the body naturally heals itself. It emphasizes health restoration as well as disease treatment.
The core modalities utilized include diet modification, nutritional supplements, herbal medicine, acupuncture,
Chinese medicine, hydrotherapy, massage, joint manipulation, and lifestyle counseling.
Cochrane systematic reviews of randomized or quasi-randomized controlled trials have reported on the effects of
Chinese herbal medicine (CHM) for various conditions including the treatment of subfertile women with
polycystic ovarian syndrome (Zhou, et al., 2016). Analysis of five studies (n=414) revealed that there is
insufficient evidence to support the use of CHM for women with this syndrome and subfertility. No data were
available on live births, and there was no consistent evidence to indicate that CHM influenced fertility outcomes.
EVERNORTH Coverage Policy: EN0086 9
The effectiveness of Chinese herbal medicine (CHM) for relief of menopausal symptoms in women over 18 years
of age was reviewed by Zhu et al. (2016) in this Cochrane review. Twenty-two randomized controlled trials
(n=2902) met inclusion criteria. CHM was compared to placebo, hormone therapy (HT), pharmaceutical drugs,
acupuncture, or another CHM formula. There was insufficient evidence that CHMs were any more or less
effective than placebo or HT for the relief of vasomotor symptoms. Effects on safety were inconclusive. The
quality of the evidence ranged from very low to moderate. Li et al. (2016) reported that analysis of nine
randomized controlled trials (n=861) showed limited evidence to assess the effectiveness of CHM for
unexplained recurrent miscarriage. No data were available to assess the safety of the intervention for the mother
or her baby. There were no data relating to any of the secondary outcomes including obstetrical and other
complications for the mother, infant death, perinatal complications, and congenital malformations.
Chen et al. (2016) assessed the efficacy and possible adverse effects of the addition of Chinese herbal medicine
to treatment with radiotherapy or chemotherapy for esophageal cancer. Nine randomized controlled trials
(n=490) were included in this Cochrane review and the authors found no evidence to determine whether
traditional Chinese medicine (TCM) was an effective treatment for esophageal cancer. The effect of TCM on
short-term therapeutic effects was uncertain.
Two Cochrane systematic reviews of randomized or quasi-randomized controlled trials reported on the effects of
Chinese herbal medicine (CHM) for the treatment of endometriosis and threatened abortion. Although two
studies (n=158) suggested that CHM might be useful in relieving endometriosis pain, the trials were of poor
methodological quality and the authors noted that the outcomes “must be interpreted cautiously” (Flower, et al.,
2012). Li et al. (2012) investigated the effects of CHM for the treatment of threatened abortion. A total of 44 trials
(n=5100) met inclusion criteria. There was insufficient evidence to assess the effectiveness of CHM alone for this
indication.
Polarity Therapy: Polarity therapy is a comprehensive health system involving energy-based bodywork, diet,
exercise, and self-awareness. It works with the human energy field and the electro-magnetic patterns expressed
in mental, emotional, and physical experience. Claims that polarity therapy is an effective treatment for cancer
and other serious diseases have not been proven.
Biologically-Based Practices
Antineoplastons: Antineoplastons are a group of synthetic compounds originally isolated from human blood
and urine. They include five urinary antineoplastons (i.e., A–1 to A–5) that have been theorized as having
antineoplastic activity against cancer. Antineoplastons are not approved for use by the FDA. The National
Cancer Institute (NCI) (2019) stated that antineoplastons are an experimental cancer therapy proposed to
provide a natural biochemical substance that is lacking in the body in people with cancer. According to NCI
(2019), no randomized controlled trials showing the effectiveness of antineoplastons have been published in the
peer-reviewed scientific literature.
Auto Urine Therapy: Auto urine therapy purports to purge embedded toxins and parasites from the colon,
bloodstream, arteries, and internal organs simply by drinking one’s own urine. There is insufficient evidence to
support the effectiveness of this therapy.
Cellular Therapy: Cellular therapy, also called live cell therapy, cellular suspensions, glandular therapy, fresh
cell therapy, sicca cell therapy, embryonic cell therapy and organotherapy, refers to various procedures in which
processed tissue from animal embryos, fetuses or organs is injected or taken orally. Those who practice cell
therapy believe that cell therapy acts like an organ transplant, having a rejuvenation effect.
Zhang et al. (2017) conducted a systematic review and meta-analysis to evaluate the safety and efficacy of
cellular therapy for the treatment of diabetic foot ulcer. Six randomized controlled trials (n=241) met inclusion
criteria. Outcomes included ankle-brachial index (ABI), amputation-free survival (AFS), transcutaneous oxygen
tension pressure (TcPO2), ulcer healing rate at 12 to 24 weeks post transplantation, pain scales and adverse
events. Two studies used mesenchymal stem cells from bone marrow or umbilical cord, three used mononuclear
cells (MNCs) from bone marrow or peripheral blood, and one study used bone marrow-derived mesenchymal
stem cells (BMMSCs) and bone marrow-derived MNCs (BMMNCs). The outcomes revealed that significant
improvements were seen in the ABI (five studies), TcPO2 (three studies), pain scores (three studies), AFC (four
EVERNORTH Coverage Policy: EN0086 10
studies) and ulcer healing rate (three studies). No serious complications were reported. Limitations of the studies
include: the limited number of studies, small patient populations (n=6–74), short-term follow-ups (12-24 weeks),
heterogeneity of cells used, variability of measurements and criterion of ulcer healing and baseline ulcer
conditions that would affect outcomes were not reported in some studies, and lack of information on allocation
concealment.
Chahla et al. (2016) conducted a systematic review to assess the safety and efficacy of cellular therapy as an
intra-articular injection of the knee for the treatment of osteoarthritis (n=124 knees) and focal cartilage defects
(n=176 knees). Four randomized controlled trials without blinding, one prospective cohort study, and one
retrospective therapeutic case-control study met inclusion criteria. Although some of the data suggested modest
improvement, a placebo effect could not be disregarded. The overall quality of the literature was poor, and the
methodological quality was fair. The data did not support cellular therapy for these indications.
Coley's Toxin: Coley's Toxin, also known as mixed bacterial vaccine (MBV) and Issel’s fever therapy, is a
treatment for cancer devised by Dr. William Coley. The toxins are the fluids derived from a bacterial culture of
two microorganisms, streptococcus pyogenes and serratia marcescesn, and are injected into affected tissue to
initiate a high fever, causing necrosis of cancer tissue. A major problem reported with bacterial therapy is their
toxicity when used at the dose required for therapeutic efficacy, including the risk of systematic toxicities (Patyar,
et al., 2010).
Hydrogen Peroxide: Hydrogen peroxide given intravenously is proposed to kill or inhibit bacteria and viruses,
precluding the need for antibiotic therapy. It may be given as a treatment for the common cold, influenza, and
sinus infections. It is also proposed by some as a treatment modality for acquired immune deficiency syndrome
(AIDS) and cancer.
Immunoaugmentative Therapy (IAT): IAT is an experimental form of cancer immunotherapy consisting of daily
injections of processed blood products. It is a developing treatment for mesothelioma that seeks to strengthen
the body's natural immune system by balancing four blood proteins.
Kelley-Gonzales Therapy: Kelley-Gonzales Therapy is based on belief in a relationship between diet and
detoxification with coffee enemas. According to Kelley, all cancers are one disease caused by a deficiency of
protein digestive enzymes which allows cancer cells to grow.
Laetrile: Laetrile is the trade name for laevo-mandelonitrile-beta-glucuronoside. The compound is chemically
related to amygdalin, a substance found naturally in the pits of apricots and various other fruits. Laetrile is
proposed for the treatment of cancer due to its ability to selectively kill cancer cells without being toxic to normal
cells. According to NCI (2017, updated 2019), Laetrile/Amygdalin is not approved for use in the United States
and has shown little anticancer activity in animal studies and no anticancer activity in human clinical trials. NCI
notes that inappropriate advertisement of laetrile as a cancer treatment has resulted in a U.S. Food and Drug
Administration investigation that culminated in charges and conviction of one distributor.
Milazzo and Horneber (2015) conducted a Cochrane systematic review of the literature to assess the proposed
anti-cancer effect and adverse effects of laetrile and amygdalin. Sixty-nine randomized controlled trials (RCTs)
and quasi-RCTs were identified but none met the inclusion criteria. Therefore, beneficial effects of laetrile for
cancer patients could not be recommended. According to the authors, there is a considerable risk of serious
adverse effects from cyanide poisoning after laetrile, especially after oral ingestion. The risk-benefit balance of
laetrile or amygdalin as a treatment for cancer is therefore unambiguously negative.
Megavitamin Therapy: Megavitamin therapy, orthomolecular medicine, megamineral therapy, intravenously or
orally, is the use of vitamins, minerals, or hormones in amounts considerably greater than the recommended
daily allowance in the belief that abundant use of vitamins can prevent or cure various ailments. An example of
megavitamin therapy is the Myers’ Cocktail, which is the intravenous infusion of a combination of Vitamins B1,
B2, B3, B5, B6, B12, Vitamin C, magnesium, and calcium. The solution is proposed for the treatment of fatigue,
fibromyalgia, migraines, allergies, and many other conditions (Ali, et al., 2009). There is a lack of evidence that
megavitamin therapy improves health outcomes.

EVERNORTH Coverage Policy: EN0086 11
MTH-68: MTH-68 (i.e., more than hope-68) vaccine is a nonpathogenic virus (i.e., Newcastle disease virus
[NDV]) that is believed to interfere with cancer growth in humans. The virus is reported to enhance the immune
system and selectively kill cancer cells. According to the NCI, NDV-based anticancer therapy has been reported
to be of benefit in more than a dozen clinical studies, but the results of these studies must be considered
inconclusive because the study designs were weak, and the study reports were generally incomplete (NCI,
2018).
Over-the-Counter Biologics: Although proposed for a variety of conditions, over-the-counter biologics are not
supported by the peer-reviewed evidence to have a positive impact on health care outcomes. Over-the-counter
biological products include the following (this list may not be all inclusive):
• Actra-Rx (Yillshen)
• Apitherapy
• Aromatherapy
• Bilberry
• Black Cohosh (cimicifuga racemosa, rattle root, snake root)
• Bovine Cartilage Products
• Cancell/Entelev (Sheridan’s Formula, Jim’s Juice, Crocinic Acid, JS–114, JS–101, 126–F, Cantron)
• Cat’s Claw (uncaria tomentosa)
• Coenzyme Q10 (CoQ10, Q10, vitamin Q10, ubiquinone, ubidecarenone)
• Coriolus (versicolor, trametes versicolor, Yun Zhi)
• Echinacea
• Essiac
• Fish Oil
• Flower Essence
• Gerson Therapy
• Ginkgo Biloba (maidenhair tree)
• Glucosamine
• Hoxsey Herbal Therapy
• Hydrazine Sulfate (sehydrin)
• Kava (piper methysticum)
• Lorenzo’s Oil
• Milk Thistle (silybum marianum; silymarin)
• Mistletoe (Iscador
®
)
• Saw Palmetto
• 714-X
• Shark Cartilage Products
• St. John’s Wort
• Valerian (Valeriana officinalis)
• Yohimbe
Ozone Therapy: Ozone therapy is also known as oxygen therapies or oxidative therapies. The delivery method
of ozone traditionally takes one of three forms: gaseous ozone exposure within a hyperbaric chamber, ozonated
oils, and ozonated water. Ozone therapies include the following: autohemotherapy, auricular insufflation,
colonics, intramuscular, intra-arterial, ozonated olive oil, ozonated steam, ozonated water, rectal insufflation, and
hydrogen peroxide. It is proposed that the extra oxygen increases the body's ability to destroy disease-causing
cells but scientific evidence supporting this claim is lacking. Ozone therapy has been proposed for the treatment
of various conditions including painful temporomandibular joint (TMJ) disorder (TMD), diabetic foot ulcers, acute
back pain, lumbar disc herniation, back pain, and hearing loss. However, there is insufficient evidence to support
the clinical benefit of ozone therapy.
Sconza et al. (2021) conducted a systematic review of randomized controlled trials for the application of oxygen-
ozone therapy in the treatment of lower back pain. Fifteen studies (n=2,597) met the inclusion criteria of
randomized controlled trials published in the last 20 years dealing with oxygen-ozone therapy in patients with
lower back pain and herniated disc, comparing the results with those of other treatments. Patients in the control
groups received different treatments including corticosteroids, analgesic therapy, placebo, microdiscectomy,
EVERNORTH Coverage Policy: EN0086 12
laser-therapy, TENS and postural rehabilitation, percutaneous radiofrequency intradiscal thermocoagulation, and
psoas compartmental block. The primary outcome of the present review was the analysis of patient’s reported
subjective scores and pain at six months’ follow-up. Looking at the quality of the literature, none of the studies
included reached “good quality” standard. Comparison of oxygen-ozone therapy results with other approaches
showed that, in the majority of studies, oxygen-ozone therapy was superior to the control treatment, and also
when compared to microdiscectomy, ozone showed non inferiority in terms of clinical outcomes. No major
complications or serious adverse events were reported in any of the trials included. Limitations of the studies
include heterogeneity of the treatment regimen, heterogeneity of the assessment methods, lack of comparison
with sham or consistent comparator, and unclear or high risk of bias in most categories. Although oxygen-ozone
therapy appears to be a safe treatment with beneficial effects, the quality of the evidence is poor.
Fitzpatrick et al. (2018) conducted a systematic review and meta-analysis of randomized controlled trials to
evaluate the safety and efficacy of ozone therapy for the treatment of chronic wounds. Nine studies (n=453) met
inclusion criteria and investigated the use of ozone therapy in the topical treatment of chronic wounds (e.g., war
wounds, burns, and non-healing diabetes, venous, or arterial ulcers). Primary outcomes included: the number of
ulcers completely healed, change in wound size, presence, or absence of biomarkers in favor of healing, and for
diabetic foot ulcers the general appearance of the wound as assessed by Wagner’s ulcer classification scale.
Secondary outcomes included the complications of pain, toxicity, amputation, infection, and developed
pathologies. Meta-analysis revealed a significant (p<0.05) improvement in wound closure (wound healing and
percent wound closure). However, there was no conclusive evidence that ozone therapy was superior to
standard treatments. No adverse events from the ozone therapy were reported. Limitations of the studies include
heterogeneous small patient populations; heterogeneity of the treatment regimen (e.g., ozone concentration,
treatment duration, frequency of treatment) and type of wounds; and moderate to high risk of bias in the majority
of studies. Due to the heterogeneity of the studies, firm conclusions could not be made regarding the
effectiveness of ozone therapy for the treatment of chronic wounds.
Li et al. (2018) conducted a systematic review and meta-analysis to investigate the safety and efficacy of intra-
articular hyaluronic acid (HA) and oxygen-ozone for the treatment of knee osteoarthritis (OA). Four randomized
controlled trials (RCTs) met the following criteria: age 18 years or older; diagnosis of end-staged knee OA;
intervention groups received intra-articular HA for pain management; control groups received intra-articular
oxygen-ozone therapy; outcomes were pain, stiffness, and function using the visual analog scale (VAS), the
Western Ontario and McMaster Universities Arthritis Index (WOMAC) questionnaire; and adverse effects. There
was no significant difference between the groups regarding VAS at three months follow-up (p=0.202). There was
significant heterogeneity of the studies (p<0.0001). Four studies showed no significant difference in VAS
between the groups at six months (p=0.255). There was no significant difference in WOMAC pain scores at six
months (p=0.380). Based on four RCTs the outcome of WOMAC for stiffness at six months was significantly
improved in favor of HA (p=0.013), but there were no significant differences in WOMAC function (p=0.037) and
adverse events (p=0.837). Limitations of the analysis include: the limited number of studies, small patient
populations; heterogeneity of the studies (e.g., doses of medication, patient characteristics) and short-term
follow-ups. This meta-analysis does not support ozone therapy for the treatment of knee OA.
Liu et al. (2015) conducted a Cochrane systematic review to assess the effectiveness of ozone therapy for the
treatment of foot ulcers in diabetics. Three (n=212) randomized controlled trials “with unclear methodology” met
inclusion criteria. Ozone treatment was compared to antibiotics, and usual care vs. usual care plus ozone
therapy. The use of ozone did not appear to affect the number of ulcers healed or make a difference in the
reduction of the ulcer area.
Magalhaes et al. (2012) conducted a systematic review and meta-analysis to evaluate the effectiveness of
percutaneous injections of ozone for the treatment of low back pain secondary to disc herniation. Four
randomized controlled trials (n=306) and eight observations studies (n=6699) met inclusion criteria. From the
randomized studies, intervention was found to be superior to the control (e.g., sham, steroid, or steroid with local
anesthetic) (p<0.00001). Overall, the observational studies revealed positive results for short- and long-term
relief of pain. Complications were rarely documented. The indicated level of evidence for long-term pain relief
(≥ 6 months) was II-3 (evidence from diagnostic studies of uncertainty); for ozone therapy applied intradiscally, II-
1 (evidence from at least one properly conducted diagnostic accuracy study of adequate size); for ozone therapy
applied paravertebrally; 1C (strong recommendation, low-quality or very low quality evidence) for intradiscal
ozone therapy; and 1B (strong recommendation, moderate quality evidence) for paravertebral ozone therapy.
EVERNORTH Coverage Policy: EN0086 13
Limitations of the studies included a lack of precise diagnosis, use of mixed therapeutic agents, and short-term
follow-up.
Revici’s Guided Chemotherapy: Revici's guided chemotherapy, also known as biologically guided
chemotherapy, Revici’s cancer control, lipid therapy, or Revici’s method, is a chemical therapy given by mouth or
injection. It is promoted as an alternative cancer treatment, as well as treatment for heart disease, arthritis, AIDS,
chronic pain, drug addiction, injury from radiation, and schizophrenia. The therapy varies for every patient but
can include a chemical formulation consisting of lipid alcohols, caffeine, zinc and iron, or a formulation consisting
of fatty acids, selenium, magnesium, and sulfur.
Trichuris Suis Ova Therapy: Trichuris suis ova, T suis ova, ova worm, or porcine whipworm, therapy is a form
of helminth immunomodulation or ova therapy. Helminths (i.e., worms) have the capacity to prevent excessive
inflammatory responses and inhibit immune responsiveness, including gastrointestinal inflammation as seen in
ulcerative colitis and Crohn’s disease (Schölmerich, et al., 2017; Summers, 2007). Ova therapy is also being
evaluated for the treatment of multiple sclerosis, allergic rhinitis, and autism spectrum disorders (Rosche, et al,
2013; Siniscalco and Antonucci, 2013). Evidence supporting the safety and clinical effectiveness of this therapy
is lacking.
Huang et al. (2018) conducted a systematic review and meta-analysis of randomized controlled trials to assess
the effectiveness of Trichuris suis ova (TSO) for the treatment of inflammatory bowel disease (IBD). Six
randomized controlled trials (RCTs) that compared TSO therapy with placebo were included. Three of the
included studies were registered clinical trials. Outcomes included efficacy and safety. There was no significant
difference (p>0.26) in remission and response rates for the treatment of ulcerative colitis (3 RCTs; n=74). Nine
patients in each group experienced one adverse event. Three studies (n=538) investigated TSO for the
treatment of Crohn’s disease study. There was no significant difference in remission and response rates
between the two groups. Studies were limited by the small patient populations and short-term follow-up of 12
weeks and sparse data were lacking on adverse events (gastrointestinal signs and symptoms). Meta-analysis
could not draw a conclusion regarding TSO dosage due to the limited data. There was no statistically significant
clinical benefit using TSO for the treatment of IBD.
Bager et al. (2010) conducted a randomized controlled trial to determine the efficacy of T suis ova for the
treatment of allergic rhinitis (n=100). No therapeutic effect was reported and significant gastrointestinal adverse
events (p=0.007) (e.g., diarrhea and abdominal pain) occurred in 76% of the T suis group compared to 49% in
the placebo group. Summers et al. (2005) (n=54) reported at 12-weeks follow-up that a significant improvement
(p=0.4) was seen with ova therapy compared to placebo in patients with active ulcerative colitis. The placebo
group showed significant improvement in stool frequency (p=0.0488) compared to baseline. Limitations of the
study include the small patient population and the short-term follow-up.
Energy Medicine
Acupressure: Acupressure is an ancient Chinese technique based on the principles of acupuncture, and
involves the use of finger pressure, without needles, on specific points along the body. It is a proposed way of
accessing and releasing blocked or congested energy centers in the body. Chinese cultures believe the points to
be junctures of meridian pathways that carry energy called “chi.” Teishin, also called needleless acupuncture, is
an example of an acupressure therapy.
Clinical trials have been conducted investigating acupressure for various conditions including weight loss
(Huang, et al., 2019), chronic low back pain (Godley and Smith, 2020), allergic rhinitis, labor pain, initiation of
labor, cancer-related pain, nausea and vomiting, dysmenorrhea, glaucoma, insomnia, cognitive function of older
adults, uremic pruritus, and end-stage renal disease. Limitations of the studies included: small patient
populations, short-term follow-ups, conflicting outcomes, no significant improvement, or some improvement but
concluding that additional research is needed comparing acupressure to sham for definitive conclusions.
Chen et al. (2021) performed a systematic review and meta-analysis of randomized controlled trials to evaluate
acupressure in combination with standard procedures during labor and delivery, compared with standard
procedures with/without sham acupressure. Thirteen RCTs (n=1586) met criteria resulting in moderate evidence
indicating that acupressure may have promising effects on labor pain and duration. There were no adverse
events, but the data was inconclusive on how acupressure affects Cesarean sections rates. Makvandi et al.

EVERNORTH Coverage Policy: EN0086 14
(2016) previously conducted a systematic review and meta-analysis (n=13 studies) of randomized controlled
trials (RCTs) to assess the evidence regarding the effects of acupressure on duration of labor and mode of
delivery. Studies were included if they examined the effect of acupressure at any acupoint during childbirth for
these indications. The results were that acupressure increased the chance of vaginal delivery when compared
with placebo/no intervention (p=0.002) and decreased the duration of the active phase by 1.310 hours (p=0.001)
and the second stage of labor by 5.808 minutes (p=0.001). However, there were several limitations to the studies
including: high risk of bias; inadequate and/or unclear allocation concealment; and significant heterogeneity
between the studies regarding the research questions, study design, intervention protocols, and outcome
measures. Conclusions from Chen et al. and Makvandi et al. were that more high-quality trials are needed to
support these findings.
In a randomized controlled trial (n=162), Torkzaharni et al. (2017) reported that the use of acupressure vs.
acupressure sham and control showed no significant differences between the groups in spontaneous initiation of
labor.
Hmwe et al. (2016) conducted a systematic review of the literature to evaluate the effectiveness of acupressure
in promoting sleep quality in adults. Eight randomized controlled trials met inclusion criteria. The studies were
conducted in hemodialysis units, long-term care facilities, nursing homes, psychogeriatric inpatients, and in a
cardiology outpatient department. Comparators were routine care or conventional medical treatment, sham,
transcutaneous electrical acupoints stimulation or acupressure with light touch. The results showed that the
quality of sleep was significantly improved in the acupressure group compared with usual care, but there was no
difference between the acupressure and sham acupressure groups. The studies were limited by the small patient
populations, heterogeneity of acupoints and methodological limitations and unclear risk of bias. Further studies
with well-designed trials are needed to confirm the efficacy and safety of acupressure for sleep.
Matthews et al. (2014; reviewed 2015) conducted a systematic review of randomized controlled trials to assess
the safety and effectiveness of various types of interventions for nausea, vomiting and retching in early
pregnancy. Of the 41 trials that met inclusion criteria, five studies used acupressure. Four of the studies
compared P6 acupressure to placebo and there were no statistically significant effects with acupressure.
Biofield Therapeutics: Biofield therapeutics, also called energy healing or “laying on of hands” (e.g., healing
touch, spiritual touch), is one of the oldest forms of untested healing known to humankind. It involves the transfer
of energy from healer to patient and the manipulation of the human body’s energy fields (Jain and Mills, 2010).
Crystal Healing: Crystal healing is the belief that certain stones and crystals contain special healing energy that
can be transferred into people to provide protection against illness and disease and provide spiritual guidance.
Multiple types of crystals are proposed for healing of all types of conditions and diseases (e.g., amethyst for
headaches and balancing blood sugar and aquamarine for heart and immune system problems).
Cupping: Cupping uses one of several types of cups (e.g., glass, bamboo) placed on the desired acupoints of
the skin to make a local place of hyperemia or hemostasis for the purpose of curing disease (e.g., fibromyalgia,
knee osteoarthritis, low back pain, urticaria, asthma, cough, herpes zoster). There are several types of cupping
including: retained cupping, flash cupping, water cupping, bleeding or wet cupping, moving cupping, needle
cupping, medicinal or herbal cupping, and combined cupping (Li, et al., 2017; Al Bedah, et al. 2016; Cao, et al.,
2012).
Ma et al. (2018) conducted a systematic review and meta-analysis of five randomized controlled trials (n=564) to
assess the effectiveness of cupping for the management of ankylosing spondylitis (AS). Studies were included if
cupping therapy was used as the sole intervention or as an adjunct therapy in conjunction with Western medicine
therapy and patients were diagnosed with AS using definitive modified New York criteria. The primary outcome
was the functional condition measured by recognized scales including the Bath Ankylosing Spondylitis
Functional Index (BASFI). Other outcomes were disease activity as measured on the Bath Ankylosing Disease
Activity Index (BADAI), and serum levels of erythrocyte sedimentation rate (ESR) and C reactive protein (CRP).
Four studies (n=294) showed cupping plus Western medicine had a significantly better response rate than
Western medicine alone (p<0.001). Three RCTs (n=242) showed significantly better BASFI (p<0.001), BASDAI
(p<0.01), ESR (p<0.01), and CRP (p<0.01) outcomes with Western medicine plus cupping. Limitations of the
analysis include the limited number of studies with small patient populations, high risk of bias, and lack of

EVERNORTH Coverage Policy: EN0086 15
blinding to the intervention. The authors noted that caution must be taken when attempting to generalize the
results of this systematic review due to the low quality of the studies and that the power of the analysis based on
small sample size effects may be exaggerated. Most of included RCTs were conducted on Chinese populations
making it difficult to apply the result to the general population.
Al Bedah et al. (2016) conducted a systematic review to evaluate the safety and efficacy of wet cupping.
Fourteen randomized controlled trials (n=863) met inclusion criteria. The included studies evaluated wet cupping
for multiple conditions including: nonspecific low back pain (three studies), hypertension (one study), brachialgia
(one study), carpal tunnel syndrome (one study), chronic neck pain (two studies), metabolic syndrome (one
study), migraine headaches (one study), oxygen saturation in smokers with chronic obstructive pulmonary
disease (one study), physiologic and biochemical parameters of healthy individuals (two studies) and oral and
genital ulcers due to Behcet disease (one study). Outcomes were conflicting with nine studies favoring cupping
for various conditions and five studies reporting no statistically significant difference was seen when cupping was
used. Adverse effects included fainting, discomfort, headache, skin laceration, whole body itching, pain,
generalized body pain, circulatory instability, migraine attack, repeating tinnitus, and wound-healing itch.
Limitations of the studies included the heterogeneity of the conditions, limited number of studies per condition,
variable risk of bias, small patient populations (n=20–126) with no power of calculations, heterogeneity of
treatment regimens (e.g., number of sessions, length of each session; frequency of sessions) and comparators
(e.g., acetaminophen; conventional treatment, no treatment), lack of blinding and no control for placebo effect.
Due to the limitations of the studies and poor overall methodology, firm conclusions could not be made regarding
the clinical effectiveness of wet cupping.
In a systematic review of 135 randomized controlled trials (RCTs) (Cao, et al., 2012) cupping therapy (mainly wet
cupping) was used for the treatment of “herpes zoster, facial paralysis (Bell’s palsy), cough and dyspnea, acne,
lumbar disc herniation, and cervical spondylosis”. Data on cupping therapy combined with other treatments, such
as acupuncture or medications, showed significant benefit (e.g., p<0.00001) over other treatments used alone in
the treatment of herpes zoster, acne, facial paralysis, and cervical spondylosis. Despite the number of RCTs
included in this analysis, the authors stated that there was a lack of well-designed studies and 84.4% of the
studies were at high risk of bias. Additional limitations of the studies included: lack of blinding, especially of
outcome assessors and statistics; lack of reporting of methodology details; and heterogeneity of treatment
regimens.
Gemstone Therapy: Gemstone therapy is an alternative technique proposed for strengthening the body and
resolving issues and patterns. It is based on the theory that gemstones carry vibrational rates and, when placed
within a person’s aura, can change the person’s vibrational rates.
Magnet Therapy: Magnet therapy may also be referred to as biomagnetic therapy, magnetherapy,
magnotherapy, static magnetic field therapy, or therapeutic magnets. The therapy involves static (unmoving)
magnets and is claimed to have healing powers. These therapeutic magnets are typically integrated into
bracelets, rings, shoe inserts, magnetic mattresses and clothing. Some health care providers claim that magnets
can help broken bones heal faster, but most proponents advocate that the magnets relieve pain.
Arabloo et al. (2017) conducted a technology assessment of systematic reviews of randomized and non-
randomized studies that compared magnet therapy with other conventional therapies for the treatment of local
pain. Eight studies met inclusion criteria. Magnet therapy was investigated for the treatment of pain in various
organs, arthritis, myofascial muscle pain, lower limb muscle cramps, carpal tunnel syndrome and pelvic pain.
Comparators included placebo, weak magnet, sham, chiropractic therapy, and traditional therapies. According to
the results, magnet therapy was not an effective treatment for relieving different types of pain.
Magnetic Resonance Therapy (MRT): MRT, based on nuclear magnetic resonance imaging (MRI), uses low
frequency, nuclear electromagnetic fields to redirect molecular activity in the body. The electromagnetic fields
generated by an MRT device are around 10,000 times weaker than those used in MRI. MRT is based on the
theory that the human body is controlled by electric and magnetic fields. When there is tissue damage there is
interference with the normal body healing signals, inhibiting healing and tissue repair. MRT is proposed to
redirect the abnormal signals into normal, healthy signals by exposing and acting on the nuclei of hydrogen
atoms. This in turn is proposed to stimulate the regeneration and repair of cartilage and bone tissue. MRT is
proposed for the treatment of multiple conditions including arthritis, osteoporosis, ligament and tendon injuries,

EVERNORTH Coverage Policy: EN0086 16
sports injuries, degenerative spine disease, autism, and posttraumatic stress syndrome. Specific devices have
been developed to treat different areas of the body and to treat specific conditions. Examples of these external
devices include MBST
®
Nuclear Magnetic Resonance Therapy, MBST
®
OpenSystem 350, and MBST
®
OpenSystem 700 (MedTec Medizintechnik, Germany). Other devices include the Magnesphere
™
and Halo
™
Home Unit (Pico-Testa Magnetic Therapies, LLC, Clearwater, FL). MRT is a patented technology. Treatment is
typically given daily in one-hour sessions for 5–10 consecutive days (Kernspin MBST, 2019).
There is insufficient evidence in the published, peer-reviewed literature to support the effectiveness of MRT for
any indication. Published studies have primarily been in the form of retrospective reviews, case reports and case
series with small, heterogeneous patient populations (e.g., n=21-103) and short-term follow-ups (≤12 months)
(Krpan, et al., 2015; Taghva, et al., 2015; Kullich, et al., 2013). Overall, randomized controlled trials have
reported no significant difference in outcomes with MBST vs. placebo.
Goksen et al. (2016) conducted a randomized controlled trial (n=97) to evaluate the efficacy of therapeutic
nuclear magnetic resonance (MRT) for the treatment of mild to moderate osteoarthritis (OA) of the knee.
Inclusion criteria included: age 35–75 years, symptomatic OA of a single knee, and radiological stage II or III
according to Kellgren and Lawrence scale. Patients received ten, one-hour daily sessions of MRT on weekdays.
Follow-ups occurred at two weeks and 12 weeks. Pain outcomes were measured by Visual Analogue Scale
(VAS), quality of life by the SF-36 and physical function by the Western Ontario and McMaster Universities
Arthritis Index (WOMAC). Ultrasound, magnetic resonance imaging and radiography were also used for knee
evaluation. At weeks two and 12 following treatment, significant improvements were reported in both groups
regarding pain, stiffness, physical functions and quality of life scores, but there were no significant differences
between the groups. There were no significant differences in ultrasonographic measurements and MRI Whole-
Organ Magnetic Resonance Imaging Scores (WORMS) or acetaminophen usage between the groups. No
adverse events were reported. This study showed that MRT was not superior to placebo in the treatment of OA
of the knee. Author-noted limitations included failure to use objective measurements like gait analysis, walking
distance, number of steps without pain and lack of evaluation of pre- and post-range knee joint motions. It was
also questioned if a ten-day course was the correct dosage to assess benefits and harms of MRT.
Salfinger et al. (2015) conducted a randomized controlled trial to assess the efficacy of therapeutic nuclear
magnetic resonance (tNMR) for lumbar radicular syndrome (LRS) in patients (n=94) with lumbar disc herniation.
Patients were randomized to the treatment group (n=48) or the control group (n=46). In addition to standard,
conservative therapy, the treatment group also received seven sessions of tNMR. Patients were included who
presented with lumbar disc herniation within 12 weeks of inclusion, radiation of pain into one or both legs and
clinical signs of a radicular lesion. Seven treatments on consecutive days were administered. Visual Analogue
Scale (VAS) scores improved significantly in both groups (p<0.000). The intensity of morning and evening pain
decreased significantly in both groups (p<0.000) with a statistically significant difference in pain perception in
favor to the treatment group in week four. Before and after week four, no statistically significant differences were
noted between the groups. There were no significant differences between the groups in the SF-36 physical
component and mental component scores or the Roland Morris Disability Questionnaire (RMDQ) scores. There
was no statistically significant difference in NSAID intake, but there was a significant decrease in the use of
opiates in both groups (p=0.05 in study group; p=0.024 in placebo group). Three months following therapy,
patients in the tNMR group reported a statistically significant lower duration of sick leave (p=0.026) compared to
the control group. Both groups reported fewer absences but there was no significant difference between the
groups. Fourteen patients dropped out of the study (13%). Overall, tNMR did not result in significant
improvements as an adjunctive therapy for this patient population.
Kullich et al. (2006) conducted a randomized controlled trial to evaluate the effects of adjunctive MBST
®
(n=30)
compared to placebo (n=32) for the treatment of chronic low back pain. Patients had been admitted for three-
weeks of inpatient rehabilitation therapy. Treatment was given for one hour on five consecutive days. Both
groups reported a significant improvement in reduction in the Visual Analogue Scale (VAS) starting at week one
following treatment. The MBST group maintained the improvement in pain under stress at the three-month
follow-up, but the placebo group did not. Neither group maintained significant improvement in pain at rest three
months after therapy. The MBST group showed a signification improvement (p<0.001) in the total Oswestry
score at three months compared to the placebo group. The placebo groups showed a significant improvement at
week one (p<0.05), but the improvement was not maintained. Both groups showed comparable improvement in
the walking and sleeping sections of the Oswestry Questionnaire at the three-month follow-up. No adverse

EVERNORTH Coverage Policy: EN0086 17
events were reported. Limitations of the study include the small patient population, short-term follow-up and
patients were part of an inpatient rehabilitation program with multiple other therapies.
Meridian Therapy: Meridian therapy or the knowledge of meridians, a self-healing system, focuses on
maintaining balance between body organs, and emotional and spiritual elements. Reflexologists propose that
keeping the body’s vital energies flowing aids the body in self-healing. Studies primarily include small patient
populations and short-term follow-up with lack of a sham comparator (Pan, et al., 2016). Evidence supporting the
clinical effectiveness of meridian therapy for the treatment of pain and other conditions is lacking.
Millimeter Wave Therapy: Millimeter wave therapy uses low-power millimeter wave (MW) irradiation to treat a
variety of conditions ranging from skin diseases and wound healing to various types of cancer, gastrointestinal
and cardiovascular diseases and psychiatric illnesses.
Moxibustion Therapy: Moxibustion is a variation of acupuncture and involves the application of heat from the
burning of the herb moxa (i.e., Artemisia vulgaris or mugwort) at the acupuncture point. The ingredients of moxa
smoke include terpene compounds, aliphatic hydrocarbons, alcohols, aromatic hydrocarbons, and their oxides.
Indirect moxibustion involves placing an insulating material (e.g., ginger, salts) between the moxa cone and skin.
Moxibustion has been proposed for the treatment of pain, joint soreness (e.g., osteoarthritis) and for other
conditions such as hypertension and cancer.
Systematic reviews and meta-analysis of randomized controlled trials have investigated moxibustion for the
treatment of heart failure (Liang, et al., 2019), polycystic ovary syndrome (Kwon, et al., 2018), spasticity following
stroke (Yang, et al., 2018), chronic fatigue syndrome (Wang, et al., 2017), primary insomnia (Sun, et al., 2016),
osteoarthritis (Li, et al., 2016; Song, et al., 2016; Choi, et al., 2012), hypertension (Kim, et al., 2010) and
ulcerative colitis (Lee, et al., 2010a), for stroke patients to improve motor and/or urinary function during
rehabilitation (Lee, et al., 2010b), as well as for the relief of chemotherapy side effects in cancer patients (Lee, et
al., 2010c). Firm conclusions regarding significant effectiveness of moxibustion cannot be made due to the
limitation of the studies which included: small patient populations; high risk of bias; lack of reporting of adverse
events (e.g., second degree burns, pruritus); heterogeneity of treatment regimens (e.g. stimulating process,
original materials, duration, frequency, selection of acupoints) and control groups; and the low methodological
quality of the studies. Overall moxibustion is not recommended for these indications.
Qigong Longevity: Qigong longevity exercise, or qigong (alternatively spelled chi gung or chi kung), is a
component of traditional Chinese medicine that combines movement, meditation and regulation of breathing to
enhance the flow of Qi (an ancient term given to what is believed to be vital energy) in the body, improve blood
circulation and enhance immune function. Qigong has been proposed for the prevention of disease (e.g., stroke)
and for treatment of various symptoms, conditions and diseases including fatigue, sleep, cognitive function,
cancer and chemotherapy related symptoms, diabetes mellitus, hypertension, Parkinson disease, infectious
diseases and chronic obstructive lung disease (Meng, et al., 2018; Lauche, et al., 2017; Van, et al., 2017; Wang
et al., 2012). Due to the poor quality of the studies and high risk of bias, the effectiveness of Qigong has not
been established.
Reiki: Reiki is a Japanese word representing universal life energy. Reiki is based on the belief that when
spiritual energy is channeled through a Reiki practitioner, the patient's spirit is healed, which in turn heals the
physical body. Systematic reviews have been conducted to assess the therapeutic effect of Reiki, including pain
control, but firm conclusions regarding its clinical effectiveness have not been established due to the limited
number of studies, small patient populations, poor study methodology, various outcome measures and the
possibility of a high level of bias (Demir, 2018; VanderVaart, et al., 2009).
Therapeutic Touch: Therapeutic Touch assumes the human energy field is abundant and flows in balanced
patterns in health but is depleted or unbalanced in illness or injury. Practitioners believe they can restore health
by sensing and adjusting such fields.
Manipulative and Body-Based Methods
Alexander's Technique: Alexander's technique seeks to rectify learned habits by reteaching the most basic
elements of movement, posture and alignment. Practitioners expect improved coordination and balance, ease of
movement, greater flexibility, reduction of tension and pain relief as the most basic benefits.
EVERNORTH Coverage Policy: EN0086 18
AMMA Therapy
®
:
AMMA Therapy,
an integration of Chinese medical principles, is a specialized form of
massage that focuses on the balance and movement of energy within the body. Hand techniques are used to
balance the flow of energy in the channels of the body through which energy passes. The therapist relies on the
sensitivity and strength of hand massage and manipulation of the energy movement.
Bio Photonic Lymphatic Drainage
Treatment (BELD): BELD (Center for Natural & Integrative Medicine,
Orlando FLA) is a proprietary therapeutic technological device proposed for removing blockage from the
lymphatic system by repolarizing proteins throughout the body. The reversal of the polarity is proposed to
remove blockages and allow elimination of toxins from the body through the urine. BELD is recommended for
many conditions including breast lumps, inflammation, chronic pain, joint pain, allergies, sinus pressure and
infections, respiratory problems, headaches, prostate problems, hormone imbalance, chronic female conditions,
dental trauma, heavy metal toxicity, neuromuscular, immune and fatigue syndromes. BELD is proposed to be
more effective than manual massage. There is a lack of evidence in the published, peer reviewed literature to
support the safety and efficacy of Bio-Photonic Lymphatic Detoxification and Drainage for any indication.
Colonic Irrigation, Colonic Lavage, Colonic Cleansing: Colonic irrigation, colonic hydrotherapy, or colonic
lavage involves inserting a tube into the rectum and gently flushing it with water. Colonic cleansing involves
ingesting a variety of powdered or liquid laxative substances. These methods are proposed for cleansing the
colon of waste and toxic materials.
Craniosacral Therapy: Craniosacral therapy, also referred to as cranial osteopathy, cranial therapy, bio-cranial
therapy, bio cranial stretching, craniopathy, or sacro occipital technique, involves intrinsic movements of the
bones of the skull which are believed to reveal different rhythmic tidal motions in the body. These movements
are measured with scientific instruments and are thought to be a direct expression of the health of the system,
linked with physical, mental and emotional health.
Haller et al. (2020) conducted a systematic review and meta-analysis of randomized controlled trials to assess
the effectiveness of craniosacral therapy (CST) for the treatment of chronic pain. Ten RCTs (n=681) met
inclusion criteria which included: adult patients with a chronic, non-malignant pain condition, examining a type of
CST regardless of length or content, and reported at least one primary or secondary outcome assessed at the
end of the intervention period or at a follow-up point closest to six months. The studies included patients with
neck and back pain, migraines, tension-type headaches, fibromyalgia, epicondylitis, and pelvic girdle pain.
Primary outcome measures were pain intensity and functional disability. Secondary outcome measures included:
physical quality of life, mental quality of life, global involvement, and safety. The studies that compared CST to
treatment as usual found small to medium size pooled effects immediately following CST intervention for pain
intensity, functional disability, and physical quality of life. Studies that compared manual and non-manual sham
controls found medium to large, pooled effects directly after, as well as six months after for pain intensity,
functional disability, physical quality of life, and global involvement. Only minor adverse events were reported
across the studies. The results suggested significant effects of craniosacral therapy on pain and function
compared to general treatment. The limitations of the review included the small number of studies in the meta-
analysis, small patient populations, unclear risk of bias profile, lack of subgroup analyses, and patient-reported
outcomes.
Ear Candling: Ear candling is accomplished by a process called convection through which softer waxes and
toxins are drawn out of the ear, oxidized and turned into vapors during the treatment. High-quality ear candles
are hand-made from beeswax and unbleached cotton cloths. These specially fabricated candles are typically
9–12 inches long and will burn for approximately ten minutes.
Feldenkrais Therapy: Feldenkrais is a method of exercise therapy designed to improve coordination. It is a
bodywork system in which the person is viewed as a complex system of intelligence and function and all
movement reflects the state of the nervous system and the individual’s self-awareness. The process of intention,
action, gaining feedback, making decisions, and reenacting with adaptations constitutes the learning framework
(Hillier and Worley, 2015).
Inversion Therapy: Inversion therapy is proposed to relieve back and neck pain by gently stretching the
vertebrae using the person's own body weight by hanging upside down. It is proposed that inversion therapy can
EVERNORTH Coverage Policy: EN0086 19
relieve back pain, decompress the spine, stretch muscles and ligaments, relieve stress, improve circulation and
help maintain overall good health. However, inversion is contraindicated in numerous conditions, including bone
weakness, recent fractures, conjunctivitis, glaucoma, heart disorders, hernias and many others.
Myotherapy: Myotherapy is a method of relaxing muscle spasms, improving circulation and alleviating pain. To
diffuse trigger points, pressure is applied to the muscle for several seconds by means of fingers, knuckles and
elbows. The success of this method is said to depend on the use of specific corrective exercise for the freed
muscles.
Neural Therapy: Neural therapy is an injection technique intended to provide instant relief of pain, increased
motion and return of function. It relies on anesthetic injections to clear up electrical interference causing
problems in the body. The therapy is typically used to treat chronic pain, but proponents say that the people most
likely to benefit are those who have failed to respond to chiropractic care, acupuncture, or physical therapy. It is
recommended if surgery or nerve block treatments fail.
Pfrimmer Deep Muscle Therapy
®
: Pfrimmer Deep Muscle Therapy involves working across the muscles to
manipulate deep tissues. The goal of treatment is to stimulate circulation and regenerate lymphatic flow to
promote detoxification and oxygenation of stagnant tissues.
Pilates: Pilates is an exercise system that focuses on improving body flexibility, strength, and awareness without
adding bulk. It involves a series of controlled movements performed on exercise equipment and/or on the floor
and resistance training that is proposed to cause spinal cord alignment and build muscle strength. Systematic
reviews and meta-analysis of randomized controlled trials have investigated Pilates for the treatment of the
following: Parkinson’s disease (Suarez-Iglesias et al., 2019); breast cancer; diabetes; chronic stroke; chronic
obstructive pulmonary disease; cystic fibrosis; heart failure; arterial hypertension; obesity (Wang, et al., 2021);
non-specific acute, subacute or chronic low back pain. There is insufficient evidence to support the clinical
effectiveness of Pilates for any condition. Studies primarily include small patient populations, short-term follow-
ups and lack of significant improvement with Pilates.
A systematic review of randomized controlled trials was conducted by Miranda and Marques (2018) to
investigate the effectiveness of Pilates on non-communicable diseases. Twelve studies (n=491) were included.
Diagnoses included: breast cancer (three studies), diabetes (three studies), chronic stroke (two years post
stroke) (two studies), chronic obstructive pulmonary disease (one study), cystic fibrosis (one study), heart failure
(one study) and arterial hypertension (one study). The best-evidence synthesis revealed strong evidence for
improving exercise tolerance, moderate evidence for improving symptoms, muscle strength and health-related
quality of life, and limited or conflicting evidence on vital signs, metabolic parameters, body composition,
respiratory function, functional status, balance, flexibility and social support. Meta-analysis was not possible due
to the paucity of evidence. Limitations of the studies included: small patient populations, 4–16 weeks follow-ups,
heterogeneity of study design, lack of a clear description of usual care in the control groups, and conflicting
outcomes. Patient populations were mainly composed of female participants preventing generalization of results
to both genders. Future studies with homogeneous outcome measures are needed to establish the effects of
Pilates on these subpopulations.
In a Cochrane review of Pilates, Yamato et al. (2015) reported that no high-quality evidence was found for any of
the treatment comparisons, outcomes or follow-up periods investigated for the treatment of non-specific acute,
subacute or chronic low back pain. There was some evidence for the effectiveness of Pilates for low back pain,
but there was no conclusive evidence that Pilates was superior to other forms of exercises. Ten randomized
controlled trials (n=510) met inclusion criteria.
In a systematic review and meta-analysis of five studies (n=139), Pereira et al. (2012) reported no improvement
in functionality or pain with Pilates compared to lumbar stabilization exercises. Lim et al. (2011) conducted a
systematic review and meta-analysis of seven randomized controlled trials and analysis of the pooled data
showed significant pain relief (p=0.04) with Pilates. However, when Pilates was compared to standard exercises
there were no significant differences in pain relief or in disability scores. Studies were limited by small patient
populations, short-term follow-ups, possible publication bias, heterogeneity of Pilates and conventional
interventions, and poor methodological quality.
EVERNORTH Coverage Policy: EN0086 20
Reflexology: Reflexology, or zone therapy, is the study of the reflexes organized around a system of points on
the hands and feet that correspond, or reflex, to every part of the body. The theory is that stimulating and
applying pressure to the feet or hands increases circulation and promotes specific bodily and muscular functions.
Huang et al. (2021) conducted a systematic review and meta-analysis to systematically summarize and quantify
the effects of foot reflexology on improvements in sleep disturbances. Forty-two articles (n=3,928) met the
following inclusion criteria: the target population was adults over 18 years old; the type of foot reflexology was
individual foot reflexology or foot reflexology with other interventions (e.g., foot bath, acupressure, or
acupuncture); the comparison group(s) received routine care, no treatment, prescribed medications, or other
activity controls; outcomes were any changes in sleep disturbances after the intervention; the study design was
limited to randomized controlled trials; and articles were written in the English or Chinese language. Results
revealed that foot reflexology resulted in a greater reduction in the sleep quality score compared with the controls
(Hedges’ g=−1.37; 95% confidence interval (CI)=−1.81~-0.94). As for the therapeutic effect, participants in the
intervention group were less likely to have sleep problems than those in the control group (pooled odds
ratio=0.25; 95% CI=0.19~0.31). Limitations include: all articles were assessed to have a high risk of bias;
heterogeneity in patient populations; lack of detailed descriptions of interventions. The findings suggested that
foot reflexology produced improvements in sleep disturbances, but well-designed, large-scale randomized
controlled trails are needed to assess long-term effects to confirm findings.
In a systematic review of 23 randomized controlled trials, Ernst et al. (2011) concluded that there was insufficient
evidence to support reflexology for the treatment of “any medical condition.” Fourteen studies reported that
reflexology was not an effective treatment compared to eight studies that reported positive outcomes. Positive
outcomes were reported for the treatment of “diabetes, premenstrual syndrome, cancer patients, multiple
sclerosis, symptomatic idiopathic detrusor over-activity and dementia.” Overall, the studies were of poor
methodological quality and included heterogeneous patient populations, various outcome measures, various
treatment regimens and short-term follow-ups.
Remedial Massage: Remedial massage is the rhythmical kneading and stroking of the body's soft tissues to
relieve accumulated tension, restore flexibility to muscles, and offer relief from pain. In addition, holistic massage
is proposed to have a calming effect on the neuromuscular system bringing about deep relaxation and restoring
energy.
A systematic review and meta-analysis of 34 randomized controlled trials concluded that the evidence did not
support infant massage for promoting physical and mental health on low-risk groups of infants under age six
months. Available evidence was of poor quality, and many studies did not address the biological plausibility of
the outcomes being measured or the mechanisms by which change might be achieved (Bennett, et al., 2013).
Rolfing: Rolfing, or structural integration, is a holistic system of soft-tissue manipulation and movement
education that is intended to bring the body’s natural structure into proper balance and alignment. The intent is to
realign the body structurally and harmonize its fundamental movement patterns to enhance vitality and well-
being.
Trager
®
Bodywork: Trager bodywork is an approach that utilizes gentle, nonintrusive, natural movements to
help release deep-seated physical and mental patterns and facilitate deep relaxation, increased physical
mobility, and mental clarity. These patterns may have developed in response to accidents, illnesses, or any kind
of physical or emotional trauma, including the stress of everyday life.
Tui Na: Tui Na, or Tuina, uses massage and manipulation techniques to establish a more harmonious flow of Qi
through the channels and collaterals in the body, allowing natural healing. Methods include the use of hand
techniques to massage muscles and tendons, acupressure techniques, and manipulation techniques to realign
the musculoskeletal and ligamentous relationships. External herbal poultices, compresses, liniments, and salves
are used to enhance the massage and manipulation. Tui Na is proposed for the treatment of musculoskeletal
disorders and chronic stress-related disorders of the digestive, respiratory and reproductive systems.
Contraindications include conditions involving fractures, phlebitis, infectious conditions, open wounds, and
lesions. There is a paucity of evidence investigating the clinical effectiveness of Tui Na.
EVERNORTH Coverage Policy: EN0086 21
Wei et al. (2017) conducted a systematic review of the literature to assess the evidence on Tui Na for cervical
radiculopathy. Five randomized controlled trials (n=448) investigated Tui Na alone or Tui Na combined with
cervical traction. The pooled analysis from three studies indicated that Tui Na alone showed a significant
immediate lowering effect on pain scores (p=0.002) compared to cervical traction. Meta-analysis from two trials
revealed significant immediate pain lowering effects using Tui Na plus cervical traction vs cervical traction alone
(p<0.00001). No adverse effects were reported. Limitations of the studies included: small patient populations
(n=60–120), short treatment duration (14–28 days) and variation in treatment regimens and study methodology.
Due to the weak evidence and study limitation, firm conclusions could not be made. Well-designed randomized
controlled trials with large patient populations and long-term follow-ups are needed to support these findings.
Also, the safety of Tui Na could not be determined from the data.
Visceral Massage: Visceral massage, or visceral manipulation, is massage of the internal muscular viscera
proposed to relieve pain anywhere including back, abdomen, legs, as well as relieve migraine headaches. It is
also proposed to improve function by relieving postpartum adhesions and adhesions around the lungs, liver,
pancreas, kidneys and gall bladder.
Mind-Body Medicine
Art Therapy: Art therapy is a creative process utilizing art as a healing and life-affirming technique. The term
typically applies to the use of the visual arts in psychotherapy to improve a feeling of emotional well-being. Art
therapy is used in mental health therapy and other settings to help focus on an individual’s creative process, and
to enhance their use of leisure as a stress reduction activity.
Jiang et al. (2020) conducted a systematic review and meta-analysis of twelve randomized control trials (n=587)
to evaluate the effect of art therapy on cancer patients' quality of life and physical and psychological symptoms.
The results determined art therapy reduced anxiety symptoms, depression symptoms, and fatigue and improved
the quality of life. Wood et al. (2011) previously conducted a systematic review to assess the available evidence
on the effectiveness of art therapy for symptomatic control of patients with cancer. Twelve randomized controlled
trials and case series (n=402) met inclusion criteria. The studies showed that art therapy is most frequently used
by women with breast cancer. Due to the heterogeneity of the studies included in these reviews, variations in the
model and content of the interventions, and various outcome measures, no overall effect was determined.
Schouten et al. (2015) conducted a systematic review of the effectiveness of art therapy in trauma treatment for
adults. Six controlled, comparative studies (n=223) (one randomized controlled trial) met inclusion criteria.
Subjects had to be traumatized adults (independent of type of trauma or type of trauma population), and the
design of the included studies had to be a comparison outcome trial with a control group. Type of trauma
included posttraumatic stress disorder (PTSD), sexual assault and traumatized incarcerated women. Some of
the included studies reported a significant decrease in psychological trauma symptoms in the treatment group
and one study reported a significant decrease in depression. Outcomes were conflicting with studies reporting a
decrease in symptom severity (some significant and some not) and no significant decrease in symptoms. The
most statistically significant decrease in trauma symptom severity was found when art therapy was used with
psychotherapy. Author-noted limitations of the studies included: small patient populations; methodological
weakness with moderate quality at best; heterogeneity of art therapy interventions (type and duration of the
interventions), control conditions, follow-up assessments, and characteristics of the study population; and patient
age primarily less than 22 years. No firm conclusions can be made for the use of art therapy for this patient
population.
Uttley et al. (2015) conducted a systematic review of randomized controlled trials investigating art therapy for
people with non-psychotic (e.g., depression, anxiety, and phobias) mental health disorders. Eleven randomized
controlled trials (n=533 patients) met inclusion criteria. Subjects included children or adolescents with asthma,
sickle cell disease or post-traumatic stress disorder and adults with Alzheimer’s disease, dementia, cancer, or
depression and incarcerated males. Follow-ups occurred from four weeks to 12 months. Control groups
included: no treatment/wait-list, attention placebo controls and psychological therapy comparators. Primary
outcomes included treatment effectiveness, response as determined by changes in mental health rating scales
and a variety of scales and questionnaires. There was a high risk of bias. Some studies reported significant
positive effects compared to controls. Meta-analysis was not possible due to clinical heterogeneity and
insufficient comparable data on outcome. Due to the small patient populations (n=18–111) and the low quality of
EVERNORTH Coverage Policy: EN0086 22
the studies, a definitive statement regarding the clinical effectiveness of art therapy could not be made for people
with non-psychotic disorders.
Bioenergetics’ Analysis: Bioenergetics’ analysis is a somatic psychotherapy that works with both body and
mind to help individuals resolve emotional problems and increase their potential for pleasure and joy in living.
Color Therapy: Color therapy, or chromotherapy, uses energies and sensitivities to color to identify and correct
imbalances in body energies. It is proposed that disorders can be healed by applying color through visualization
or verbal suggestions.
Dance Movement Therapy: Dance movement therapy is the psychotherapeutic use of movement and dance to
engage a person creatively in a process believing to further their emotional, cognitive, physical and social
integration. It is founded on the principle that movement reflects an individual’s patterns of thinking and feeling.
Karkou and Meekums (2017) conducted a Cochrane systematic review to assess the effects of dance movement
therapy on behavioral, social, cognitive and emotional symptoms of patients with dementia. No studies met the
inclusion criteria.
Equestrian Therapy: Equestrian therapy (i.e., horseback riding or hippotherapy) is proposed to offer a person
with a disability a means of physical activity that aids in improving balance, posture, coordination, the
development of a positive attitude and a sense of accomplishment.
Guindos-Sanchez et al. (2020) conducted a systematic review and meta-analysis of ten randomized control trials
(n=452) to analyze the effectiveness of hippotherapy interventions on gross motor function in subjects with
Cerebral Palsy. The studies showed that hippotherapy interventions were effective in improving gross motor
function and had positive effects on balance recovery and muscle spasticity reduction in subjects with Cerebral
Palsy. However, due to the small patient populations, short-term follow-up and heterogeneity of the protocols,
additional randomized control trials with larger sample sizes and specified protocols are needed to support the
effectiveness of these interventions.
Bronson et al. (2010) conducted a systematic review of the literature to evaluate the ability of hippotherapy to
improve balance in multiple sclerosis patients. Three case series with less than 11 patients each met inclusion
criteria. The patients engaged in a mean 7.75 hours of therapy over a mean 11.2 weeks. There is insufficient
evidence to support hippotherapy for this indication.
Faith Healing: Faith healing is the belief that some people are able to channel divine powers to heal injury and
cure disease. Patients who seek the assistance of a faith healer must believe strongly in the healer’s divine gifts
and ability to focus on illness.
Following a systematic review of five randomized controlled trials (n=1130), Candy et al. (2012) found
“inconclusive evidence” that interventions with spiritual or religious components for adults in the terminal phase
of a disease enhanced well-being. Limitations of the studies included: all studies were undertaken in the same
country; in the multi-disciplinary palliative care interventions it was unclear if all participants received support
from a chaplain or a spiritual counselor; it was unclear whether the participants in the comparative groups
received spiritual or religious support, or both, as part of routine care or from elsewhere; and there was a
“paucity of quality research”.
Guided Imagery, Interactive: Guided imagery promotes the use of imagery to help a patient connect with
deeper resources at the cognitive, affective and somatic levels. The guide’s role is to facilitate an enhanced
awareness of the unconscious imagery the patient has and train them to work effectively with this imagery on
their own behalf.
In a systematic review of 15 randomized controlled trials (n=1172), Posadzki et al. (2012) reported that the
evidence for guided imagery for the relief of non-musculoskeletal pain was inconclusive. Overall, the
methodology was poor; outcomes were conflicting; and patient populations, study design, outcome measures
and types of guided imagery were heterogeneous.
EVERNORTH Coverage Policy: EN0086 23
Hellerwork: Hellerwork is a form of deep-tissue bodywork designed to realign and rebalance the body, releasing
chronic tension and stress, producing a more relaxed, youthful state. The central premise is that a structurally
misaligned body experiences gravity as stressful. When movement and flexibility are limited, there is energy
loss, aging and deterioration.
Humor Therapy: Humor therapy targets laughter as a means to lower blood pressure, reduce stress hormones,
increase muscle flexion and boost immune function. It is proposed to raise levels of infection-fighting T-cells,
disease-fighting proteins called Gamma-interferon, and B-cells, which produce disease-destroying antibodies.
Laughter is also thought to trigger the release of endorphins, the body's natural painkillers, and to produce a
general sense of well-being.
Hypnosis: Hypnosis is a psychological condition in which an individual may be induced to show apparent
differences in behavior and thinking. It employs techniques to induce states of selective attentional focusing or
diffusion combined with enhanced imagery. It is often used to induce relaxation. Hypnosis is recognized as a
treatment modality for pain control, weight control, irritable bowel syndrome, and as an adjunct to cognitive
behavioral and other therapies. Hypnosis has also been proposed for reducing fear and anxiety, reducing the
frequency and severity of headaches, and controlling bleeding and pain during dental procedures.
Systematic reviews and randomized controlled trials have reported that there is insufficient evidence to support
hypnosis for insomnia (Chamine, et al., 2018; Lam et al., 2015); burn wound pain and anxiety (Provencal, et al.,
2018); stress reduction (Fisch, et al., 2017); breast cancer (Cramer, et al., 2015); cancer-related anxiety, fatigue,
pain (Chen, et al., 2017); management during labor and childbirth (Madden, et al., 2016); children undergoing
dental treatment (Al-Harasi, et al., 2017) and treatment of irritable bowel syndrome (Webb, et al., 2007).
Although some studies have reported improved outcomes with hypnosis, studies have been limited by small
patient population, short-term follow-ups, and heterogeneity of treatment regimens and controls. Overall, the
authors concluded that the quality of the trials was inadequate to make firm conclusions and outcomes were
conflicting in some studies improvements were reported and in other studies there were no significant
differences in outcomes when hypnosis was used.
Martial Arts: Martial arts are best known as a means of self-defense and are divided into armed and unarmed
sports. Many of the forms and derivatives thereof are practiced as a means of mental and spiritual development
(Cochrane Complementary Medicine, 2020). Many martial arts originate in China with only 20–30% coming from
other East Asian countries. Unarmed combat forms of martial arts include judo, sumo, karate and Chung Moo
Doe. Chung Moo Doe therapy is a martial art that has been practiced for over 1500 years in East Asia under
various names. Along with Tai Chi, Chung Moo Doe includes Kung Fu, Ai-Ki-Do/Hap-Ki-Do, Jujitsu, Tae-Kwon-
Do, Bagwa Chang, Ship Pal Gae/18 weapons and Samurai Sword.
Systematic reviews of randomized and nonrandomized controlled trials have evaluated the effectiveness of Tai
Chi as a supportive treatment for low back pain (Qin, et al., 2019); type 2 diabetes mellitus (n=14 studies) (Chao,
et al., 2018); stroke rehabilitation (n=15 studies) (Ding, 2012) and gait training (n=five studies) (Li, et al., 2018);
the treatment of stress, anxiety, depression and mood disturbance (n=3817) (Wang, et al., 2010); a therapeutic
intervention for the treatment of patients with cardiovascular risk factors or cardiovascular conditions (e.g.,
coronary artery disease, congestive heart failure) (n=29 studies) (Yeh, et al., 2009); and cancer-related fatigue
and quality of life in cancer patients (n=17 studies) (Sur, et al., 2021). Definitive conclusions were limited due to
poor to moderate study quality; possible publication bias; wide variety of Tia Chi styles, frequency, duration and
follow-up; inadequate or no controls; combinations of various treatment activities; and heterogeneity of outcome
measures.
Meditation/Transcendental Meditation (TM
®
): Meditation/Transcendental Meditation is proposed to be the
single most effective technique available for gaining deep relaxation, eliminating stress, promoting health,
increasing creativity and intelligence and attaining inner happiness and fulfillment. TM is one type of meditation
involving a mantra meditation technique where consciousness is directed towards repetition of a word, or a
phrase, as an object of focus. Meditation has been proposed for the treatment of numerous conditions including
depression (González-Valero, et al., 2019), anxiety, stress (Araujo, et al., 2019), chronic pain, asthma,
posttraumatic stress syndrome, hypertension, headache, dementia, attention deficit disorder, and for smoking
cessation. Systematic review and meta-analysis have reported some benefit from meditation, but based on the

EVERNORTH Coverage Policy: EN0086 24
poor quality of the studies, firm conclusions have not been made regarding the clinical effectiveness of this
modality.
Hilton et al. (2017) conducted a systematic review and meta-analysis of 38 randomized controlled trials
investigating mindfulness meditation for chronic pain (e.g., back pain, headache, fibromyalgia, cancer,
musculoskeletal pain, irritable bowel syndrome). Treatments ranged from 3–12 weeks. Interventions included
mindfulness-based stress reduction (MBSR), mindfulness-based cognitive therapy (MBCT) and other types of
meditation. Some interventions were monotherapy while others used meditation as an adjunctive therapy.
Comparators included: treatment as usual, education, support groups, stress management, massage,
multidisciplinary pain interventions, relaxation/stretching, nutritional information/food diaries, and cognitive-
behavioral therapy. These low quality, heterogeneous studies reported some evidence that meditation was
associated with a small decrease in pain. Well-designed, rigorous, and large-scale RCTs are needed to
decisively provide data for the efficacy of mindfulness meditation for chronic pain.
In an analysis of eight systematic reviews (SR) and meta-analyses, Ooi et al. (2017) reported that transcendental
meditation may potentially reduce systolic blood pressure by ∼4 mm Hg and diastolic blood pressure by ∼2 mm
Hg. The SRs included 5–15 studies and follow-ups ranged from six weeks to 18 months. The outcomes were
comparable to those seen with other lifestyle interventions including weight-loss and exercise. However, the
strength of evidence was considered weak due to conflicting findings across reviews and potential risks of bias.
Further research is still needed to validate these findings.
Salhofer et al. (2016) conducted a Cochrane systematic review of randomized controlled trials investigating the
benefits and harms of meditation as an adjunctive therapy for adults with hematological malignancies. One
abstract was found. There is insufficient evidence to support meditation for this patient population.
Mirror Box Therapy: Mirror box therapy is the use of visual illusions created by a mirror and is proposed for the
treatment for phantom limb pain, complex regional pain syndrome (CRPS)/reflex sympathetic dystrophy
syndrome (RSD), stroke, arthritis and carpal tunnel syndrome. Mirror therapy is based on the theory that visual
feedback provides a substitute for missing proprioceptive feedback to reduce pain. The limbs are positioned
inside a box separated by a mirror. The patient looks into the mirror and sees the image of the unaffected limb,
thinking that the affected limb is moving effortlessly. The underlying mechanism accounting for the effectiveness
of the therapy has not been established (Thieme, et al., 2018; Moseley, et al., 2008; Selles, et al., 2008).
Systematic reviews and meta-analysis of randomized controlled trials and case series have evaluated box
therapy for the treatment of stroke patients, phantom limb pain, complex regional pain syndrome (CRPS), and
various upper extremity conditions. Zeng et al. (2018) evaluated the treatment effect of mirror therapy on motor
function of the upper extremity in patients with stroke. Eleven studies (n=347) were included in the meta-
analysis. Although some improvement in motor function was seen, the heterogeneity of the studies, including the
patient (n=15–60) characteristics and treatment regimens, prevented firm conclusions from being drawn
regarding the clinical effectiveness of mirror box therapy.
Thieme et al. (2018) investigated mirror therapy compared to no treatment, placebo/sham therapy, or other
treatments for improving motor function and motor impairment after stroke. Randomized controlled trials (RCTs)
and randomized cross-over trials comparing mirror therapy with any control intervention were included (n=62
studies; 1982 subjects). Mirror therapy was provided 3–7 times a week, for 15–60 minutes for 2–8 weeks
(average of five times a week, 30 minutes a session for four weeks). There was moderate-quality evidence that
mirror therapy had a significant positive effect on motor function and motor impairment. The authors noted that
effects on motor function were influenced by the type of control intervention. Based on moderate-quality
evidence, it was reported that mirror therapy may improve activities of daily living. There was low-quality
evidence for a significant positive effect on pain (n=248) and no clear effect for improving visuospatial neglect
(failure to orientate, to report or to respond to stimuli located on the contralesional side) (n=175). No adverse
effects were reported. The major limitations of the studies included the small patient populations, short-term
therapy and lack of reporting of methodological details, resulting in uncertain evidence quality.
Barbin et al. (2016) conducted a systematic review to evaluate the efficacy of mirror therapy on phantom limb
pain. Five randomized controlled trials and 15 nonrandomized studies met inclusion criteria. Study
methodologies were heterogeneous with low level evidence, patient populations were small, and outcomes were

EVERNORTH Coverage Policy: EN0086 25
conflicting. Meta-analysis was not possible. The data did not support the use of mirror therapy for the treatment
of phantom limb pain.
Music Therapy: Music therapy includes music sessions for individuals and groups based on client needs. Music
therapists assess emotional well-being, physical health, social functioning, communication abilities and cognitive
skills through musical responses, using improvisation, receptive listening, song writing, lyric discussion, imagery,
performance and learning through music.
Systematic reviews of randomized controlled trials have investigated music therapy for individuals with multiple
conditions including: burn injuries (seven trials; n=524) (Wu, et al., 2021); anxiety (32 studies; n=1,924) (Lu, et
al., 2021); dementia (van der Steen, et al., 2018; Gómez-Romero, et al., 2017); depression (nine studies; n=421)
(Aalbers,et al., 2017); substance abuse (40 studies; n=1381) (Hohman, et al., 2017);
schizophrenia and
schizophrenia-like disorders (18 studies; n=1215) (Geretsegger, et al., 2017); acquired brain injuries (29 studies;
n=775) (Magee, et al., 2017); symptoms of cancer (29 trials; n=3731) (Bradt, et al., 2016); and postoperative
pain management after orthopedic surgery (nine studies) (Lin, et al., 2020). Although some studies suggested
that music therapy may be effective for some outcome measures, overall the quality of the studies was very low
to moderate, clinical effectiveness could not be determined, outcomes were inconsistent, treatment regimens
were heterogeneous, and long-term outcomes have not been reported.
In a systematic review of 51 randomized controlled trials (n=3663), Cepeda et al. (2006) concluded that listening
to music reduced the intensity of pain and opioid requirements, but the “magnitude of the benefits was small, and
the clinical importance of music was unclear”.
Outdoor Youth Programs: Outdoor youth programs (outdoor adventure programs, outward bound schools,
outdoor education) are associated with social, recreational, developmental, educational and therapeutic aims. In
general, outdoor education can be described as teaching and/or learning and/or experiencing in an outdoor
and/or out-of-school environment. The content of learning and teaching varies and depends on the general aim
of the program (e.g., gaining of knowledge in natural sciences; increased physical activity, leadership skills,
personal and social development; survival skills; improved skills in relation to nature-oriented sports), the target
group and the outdoor setting. Most programs are designed to fit the needs of a specific target group (e.g.,
substance abuse, school truancy, failing school) and work with teens or at-risk teens. Outdoor adventures are
proposed to have direct positive impacts on well-being and perceived stress, as well as foster the psychological
concepts related to resilience, self-efficacy, mindfulness and subjective well-being. Outdoor activities include
backpacking, climbing, swimming, canoeing, scuba diving, and biking. Programs range from 5–30 days
(Wilderness Adventures, 2020; Becker, et al., 2017; Voyageur 2017; Mutz, et al., 2016). There is insufficient
evidence to support the clinical effectiveness of outdoor youth programs. Studies are primarily in the form of
small case series. Currently, the key components of these programs and the benefits gained by participants
have not been established.
Becker et al. (2017) conducted a systematic review of the literature (n=13 studies) to identify the potential
benefits of regular compulsory school- and curriculum-based outdoor education programs (OEPs) for children
and adolescents. The review concentrated on programs that were embedded within the curriculum and
conducted regularly within the school schedule. These programs focused on student-centered classes and
interdisciplinary subjects, hands-on learning, possibilities to explore and experience oneself and the
environment, and the use of natural and cultural places as a “classroom.” Thirteen studies met inclusion criteria:
nine case series, three quasi-experimental designs and one cross-sectional design. Inclusion criteria were: all
types of study designs; any type of formal school- and curriculum-based outdoor education program involving
children and adolescents (age 5–18 years); regular weekly or bi-weekly classes in a natural or cultural
environment outside the classroom with at least four hours of compulsory educational activities per week over a
period of at least two months; and at least one reported outcome on a student level. Environmental settings
included gardens, local forests, prairies, farmland and sailing. Eight studies described outcomes in terms of
social dimensions, seven studies in learning dimensions, and four studies included physical activity and health.
Sample sizes ranged from 5–230. Eleven studies reported positive results, one study reported positive and
negative results and one study reported negative effects. Tendencies indicated that regular compulsory school-
and curriculum-based outdoor education programs could advance students in the physical, psychological,
learning and social dimensions. However, the wide heterogeneity in the program aims, intervention length (e.g.,
biweekly for eight weeks vs. full weeks for six months), participant groups, age, learning environments,
EVERNORTH Coverage Policy: EN0086 26
methodology and reported effects, prevented any firm conclusions from being made regarding the effectiveness
of these programs. Evidence on the effect of these programs on physical activity and mental health were lacking.
Pet Therapy: Pet therapy (PT) or animal-assisted therapy (AAT) involves the use of animals for therapeutic
purposes. PT is proposed to help people recover from and/or better cope with psychological and/or physical
health problems. The intent is that pet therapy aids in the psychological, educational and physical rehabilitation
of a patient to improve their general sense of well-being and improve their quality of life. Dogs and cats are the
most commonly used animals. Studies have reported that pet therapy decreases cortisol and catecholamine
levels in the blood and increases endorphins, reducing stress and producing a calming effect. Pet therapy has
been proposed for the treatment of dementia, cognitive dysfunction, stroke, mental health disorders (e.g.,
depression, autism spectrum disorder), stress, pain, fatigue, cardiovascular rehabilitation, cancer support,
pregnancy, post-traumatic stress disorder and hospice care. The therapy is used by inpatient facilities, nursing
homes, universities, as well as at home (Zafra-Tanaka, et al., 2019; Fiori, et al., 2018; Ein, et al., 2018; O’Haire
et al., 2013; Moretti, et al., 2011).
There is insufficient evidence in the peer-reviewed literature supporting the clinical effectiveness of pet therapy.
Studies have primarily been in the form of case reports or case series with less than 100 subjects and studied for
a variety of conditions. Outcomes are conflicting with some studies reporting no significant difference with pet
therapies (Gaudet, et al., 2021; Fiori, et al., 2018; O’Haire et al., 2013; Moretti, et al., 2011).
Ein et al. (2018) conducted a systematic review and meta-analysis to examine the efficacy of pet therapy (PT) on
reducing physiological stress levels (i.e., blood pressure and heart rate) and self‐reported stress and anxiety
scores. Studies with the following characteristics were included: subjects all ages, healthy, or had psychological
and/or medical illnesses; used novel living animals (e.g., an animal that was unfamiliar to the subject and not the
subject’s personal pet) as the sole therapeutic tool; used PT programs to create a calming environment with
minimal physical activity (e.g., petting the animal); and incorporated pre- and post-therapy changes in blood
pressure and heart rate and/or changes in self‐reported measures of stress and/or anxiety. A total of 28 studies
(n=1310) met inclusion criteria. All but two studies used dogs for the animal therapy. Overall, analysis of eight
studies showed significantly reduced heart rates (HR) (p<0.001). Subgroup analysis showed that healthy
subjects maintained the significant HR effect (p=0.012) but subjects that had medical and/or psychological
conditions did not show a significant reduction in HR (p=0.68). Significant effects were shown in a group setting
(p=0.007) vs. no effect in individual therapy (p=0.403). PT did not significantly reduce systolic blood pressure
(p=0.149). Overall self-reported anxiety was significantly reduced in adults (p<0.001) and remained significant in
subgroup analysis of healthy adults (p<0.001) and adults with a medical (p<0.001) or psychological condition
(p=0.001). There were an insufficient number of subjects to determine the effect of self-reported anxiety on
children and elderly adults. The authors reported that the majority of medical and psychological subjects had
taken medication (e.g., pain medication) prior to or during PT. Limitations of the studies include the
heterogeneous, small patient populations (n=4–135); lack of self-reported data on stress reduction; use of self-
reported data; use of medication by some of the subjects before and/or during the study; and the use of only
dogs in all but two of the studies.
Primal Therapy: Primal therapy explores, studies, researches and promotes certain forms of psychotherapy and
growth, including those that emphasize uncovering and resolving traumatic experiences. It also aims to develop
a community that is congruent with the principles developed from this work.
Psychodrama: Psychodrama is a method involving improvisational dramatic action under the guidance of a
trained practitioner known as the director. The script is written moment by moment, out of the purposes and
concerns of an individual, or the group where the method is being applied. Group members take an active part in
the dramas so that they bring it as close to life as possible.
Recreational Therapy: Recreation therapy (RT), also call therapeutic recreation, is a therapy that utilizes
recreation and other activity-based interventions to address the needs of individuals with illnesses and/or
disabling conditions. The proposed purpose of RT is to improve or maintain physical, cognitive, social, emotional
and spiritual functioning in order to facilitate full participation in life and maintain optimal levels of independence,
productivity and quality of life. Recreational therapy includes arts and crafts, sports, games, dance and
movement, drama, music, and community outings. RT seeks to reduce depression, stress, and anxiety, recover
basic motor functioning and reasoning abilities, build confidence, and socialize effectively. Services are provided

EVERNORTH Coverage Policy: EN0086 27
or directly supervised by a Certified Therapeutic Recreation Specialist (CTRS). Recreational therapists practice
in various settings including: inpatient and outpatient physical rehabilitation, inpatient and outpatient mental
health, skilled nursing facilities and assisted living, adult day programs, park and recreation, adapted sports
programs, acute care hospitals, and school systems (CTRS) (American Therapeutic Recreation Association,
2019; National Council for Therapeutic Recreation Certification, 2020). There is a lack of evidence investigating
the clinical efficacy of recreational therapy.
Wilderness Therapy: Wilderness therapy (WT), also called wilderness adventure therapy (WAT), is a multi-
faceted program, consisting of outdoor life and various sequenced tasks and challenges. Wilderness therapy is
also used synonymously with other terms including: adventure therapy, wilderness experience programs, bush
adventure therapy, eco-therapy, adventure-based counseling, outdoor adventure intervention, therapeutic
camping, and outdoor behavioral healthcare. The program seeks to enhance the restorative qualities of nature
combined with structured individual and group-based therapeutic work. WT offers a prevention, early
intervention, and treatment modality for individuals with behavioral, psychological, psychosocial and/or
substance abuse issues (Dobud and Harper, 2018; Fernee, et al., 2017; Bowen, et al., 2016). WT has, for the
most part, replaced military style boot camps.
There is a wide diversity of philosophies, theories, and formats being used in WT. Activities often include rope
challenge courses, group games, trust activities, residential camps, and wilderness-based expeditions. The
programs are typically led by a multi-disciplinary therapist team and often serve a heterogeneous population of
adolescent clients. Participants engage in group living with peers and therapists, undergo individual and group
therapy sessions, and learn basic outdoor skills proposed to foster personal, emotional, and social growth.
Typically, WT is a 10-week, part-time program, facilitated by three practitioners for six to eight participants.
Treatment involves seven day-based adventure activities (e.g., bushwalking, cross country skiing, white water
rafting), a two-day overnight training expedition, and a five-day expedition. Parents, teachers, and support
workers also participate in up to eight weekly indoor adventurous problem-solving activities incorporated within
group therapy sessions (Dobud and Harper, 2018; Fernee, et al., 2017; Bowen, et al., 2016).
The wilderness environment is proposed to be a healing place that may facilitate change. After having
experienced difficulties, turmoil and/or loss in their lives, participants may find peace in the wilderness. A primary
sense of despair may gradually be replaced by self-confidence through reflecting on life and managing the basic
tasks of simple outdoor life and the inherent challenges of this approach to treatment. A proposed advantage of
WT over conventional therapy is that the stigma of psychological therapy dissolves former resistance, making
individual and group psychotherapy less intimidating and more natural. The duration and context of the WT
treatment may provide the necessary time and space to address and process emotional upheaval and stimulate
personal issues to surface that have not been revealed in previous treatment settings (Dobud and Harper, 2018;
Fernee, et al., 2017; Bowen, et al., 2016).
Alexander et al. (2016) discussed the safety concerns related to wilderness therapy and the importance of being
prepared for traumatic and minor injuries and illness. Adverse events of WT may occur from contaminated water;
insect and tick bites; heat-related illness; hypothermia; allergic reactions to plants; insects or foods; head injuries;
fractures; sprains; dislocations; burns; lacerations; and blisters.
Studies investigating the effectiveness of wilderness therapy have primarily been in the form of case series with
small heterogeneous patient populations, reporting short-term effects and investigating various outcome
measures. Overall, studies on WT have not provided detailed program descriptions and guiding theories. The
efficacy of WT across programs and populations and how the treatment stimulates change has not been
established (Fernee, et al., 2017).
Dobud and Harper (2018) conducted a systematic review of randomized controlled trials in an effort to identify
the specific activities contributing to adventure therapy (AT) outcomes. Fourteen direct comparison studies met
inclusion criteria. Studies indicating the presence of qualified practitioners working in clinical settings were
included. Studies without a control group or experimental conditions and lacking the presence of a therapeutic
rational or practitioner were excluded. Study groups included: adapted outward bound therapy, wilderness
survival, therapeutic services with AT, integrated wilderness therapy (WT), adventure camp, and outdoor
behavioral healthcare. Comparators included: traditional probation treatment; wilderness survival without family
therapy; treatment as usual; no specific intervention; alternative group therapy; behavior modification, residential
EVERNORTH Coverage Policy: EN0086 28
program, inpatient program, a second outdoor adventure program; and AT plus psychological counseling,
psychological counseling alone and psychological and group counseling. In ten of the 13 studies, intense social
environments were assumed to contribute to positive outcomes. Three studies reported that problem-solving
activities would lead to feelings of success or mastery. Seven studies reported that time in nature and pristine
wilderness environments would provide a more effective setting for therapeutic healing to occur and asserted
that time in nature was an active ingredient contributing to outcomes. However, the differences were not
significant. Studies were limited in number and varied regarding the treatment setting, therapeutic ingredients,
social setting and outcome measures. It was noted that there was limited discussion about the experimental
groups and the treatments provided made it difficult in some cases to determine whether a control group was
designed to be therapeutic. Based on these studies, the authors concluded that the active ingredients regarded
as unique to AT made little difference in outcomes across the 13 studies, and the unique components of AT may
not have greater influence than the factors shared with all other forms of therapeutic interventions.
Fernee et al. (2017) conducted a systematic review of the literature to investigate the effectiveness of WT on
adolescence (aged 12 to 18 years) and to identify the descriptions of the treatment programs and their
outcomes. Seven studies met inclusion criteria and were in the form of case series with small patient populations
(n=4–47). The intent of the studies was heterogeneous and included: 1) understanding how adolescents who
were involuntarily enrolled in the program responded to parents and therapists (n=13); 2) understanding how
backpacking was related to self-reported outcomes for troubled adolescent women (n=9); 3) gaining insight into
the effect of a residential wilderness program on self-evaluation of male adolescents and what specific aspects
of the program caused the changes (n=13); 4) interviewing participants > age 20 years following involvement in a
10-day WT program at age 14–16 years to discover the impact of WT on their lives (n=4) 5) investigating WT
and the outcomes from the intervention (n=4 men); 6) examining WT and identifying the key change agents and
outcomes (n=12); and 7) evaluating youth well-being 24 months after the conclusion of WT treatment (n=47).
Reported outcomes of the studies included: despair was gradually replaced by self-confidence; the wilderness
environment was a healing place and facilitated change; time alone allowed reflection and personal insight;
avoidance of the “stigma” attached to mental health treatment; physical demands of the wilderness lifestyle
contributed to the changes experienced including competence and sense of accomplishment; and enhanced
self-awareness, self-efficacy; and socialization skills with therapists and peers. The authors noted that the lack of
client characteristics in relation to the therapeutic process and to each participant’s specific set of outcomes
prevented conclusion regarding who the best candidates are for WT, as well as the programmatic circumstances
that might facilitate individual change. Another limitation of the studies is the inability to generalize effects to a
larger population due to the limited number of studies and small patient populations. Additional studies are
needed to define a comprehensive and useful framework that is applicable to the general population and who the
ideal candidates are for WT.
Yoga: Yoga is a highly diversified mind-body practice that has evolved into many areas, including fitness
training, a system of healing, a purification program, mind-training, a philosophical system, a religious practice or
a spiritually-based lifestyle. It typically involves physical postures, breathing techniques, and meditation or
relaxation.
Systematic reviews have evaluated peripartum outcomes of yoga, yoga for the prevention of coronary heart
disease, as antihypertensive lifestyle therapy, Parkinson’s, stroke rehabilitation, depression, substance abuse,
posttraumatic stress disorder, treatment of cancer pain and treatment-related side effects, anxiety and stress,
diabetes mellitus, schizophrenia and epilepsy, chronic non-specific low back pain, rheumatic diseases and
asthma, headaches, sleep quality and insomnia (Ban, et al., 2021; Brinsley, et al., 2021; Lenoir Dit Caron, et al.,
2021; Walia, et al., 2021; Wang, et al., 2020; Anheyer, et al., 2020; Gothe, et al., 2019; Sieczkowska, et al.,
2019; Wu, et al., 2019; Kuppili, et al., 2018; Bridges and Sharma, 2017; Broderick, et al., 2017; Lawrence, et al.,
2017; Cramer, et al., 2017; Wieland, et al., 2017; Cui, et al., 2017; Yang, et al., 2016; Panebianco, et al., 2017;
Babbar, et al., 2012; Bussing, et al., 2012; Harder, et al., 2012; Li, et al., 2012; Vancampfort, et al., 2012).
Although some studies suggested improvement in outcomes with yoga, other studies reported that the
effectiveness of yoga remained uncertain. Limitations of the studies included: small patient populations; short-
term follow-ups; and heterogeneity of yoga protocols, number of sessions and length per session; and lack of
blinding. Data are conflicting and studies have not been well designed. Data on adverse events is limited. Large-
scale, well-designed studies using objective measures and long-term follow-up are needed to draw definitive
conclusions regarding the clinical effectiveness of yoga.
EVERNORTH Coverage Policy: EN0086 29
Multi-Therapy Systematic Reviews
Several systematic reviews have evaluated multiple CAM therapies for the treatment of various conditions
including asthma, cancer, dementia, depression, diabetes, hypertension, irritable bowel syndrome, pain
management (Garland, et al., 2019), psoriasis, Raynaud’s phenomenon, rheumatoid arthritis, and rhinitis.
Although some studies reported clinical improvement with some modalities, overall, the authors agreed that
there is insufficient evidence to support CAM for the treatment of these conditions. Studies are limited by small
patient populations, minimal and short-term follow-ups, variability in dosage and unknown quality of oral
supplements, few evaluations of side effects, inconsistent and inconclusive outcomes, and no controls or
comparisons to traditional Western medical therapies.
Abdominal Pain: Abbott et al. (2017) conducted a Cochrane systematic review that included 18 randomized
controlled trials to assess the effectiveness of four types of psychosocial therapy (cognitive behavioral therapy,
hypnotherapy including guided imagery, yoga, written self-disclosure) for the treatment of recurrent abdominal
pain in school-aged children. Regarding four studies on hypnotherapy (n=143), greater treatment success was
reported post-intervention (p=0.0003). Reduced pain intensity (p<0.00001) and frequency (p<0.00001) were
achieved with hypnotherapy compared to controls. Studies were considered low-quality with short term follow-up
and small patient populations. One study reported long-term benefit of hypnotherapy at five years (68%)
compared to control (20%) (p=0.005). For yoga therapy compared to control, there was no evidence of
effectiveness on reduction of pain intensity post-intervention (p=0.09). The three yoga studies included 122
children and were low-quality evidence.
Asthma: Kohn and Paudyal (2017) conducted a systematic review and meta-analysis of 23 randomized
controlled trials to evaluate the safety and efficacy of CAM for the treatment of asthma in adults. CAM therapies
included the following: curcumin; New Zealand green-lipped mussel; solanum xanthocarpum and solanum
trilobatum; coenzyme Q10; selenium; auranofin; vitamins B6, C, D or E; aqueous extract of propolis; AKL1#
(picrorrhiza kurroa, zingiber officinale, ginkgo biloba and apocynin); lactose powder; TJ-96; Pingchuan Yiqi
Granule, magnesium, n-3 polyunsaturated fatty acids; and anti-asthma herbal medicine intervention (ASHMI; a
Chinese herbal formula containing Ku-Shen [Sophora flavescens], Gan-Cao [Glycyrrhiza uralensis] and Ling-Zhi
[Ganoderma lucidum]. Controls included standard asthma treatment, placebo, and pharmacotherapy. The results
of meta-analysis on magnesium, vitamin C and vitamin D, indicated that these supplements were not beneficial
in improving the lung function of asthma patients. Eight single trials showed improvement in lung function and
symptom control but there was no overall trend in one outcome measure across trials. In addition, many of the
trials had a poor methodological quality, restricting the reliability and applicability of these results. The analysis
did not provide sufficient evidence to recommend any of the included CAM compounds for the treatment of
asthma. Limitations of the studies included: short-term duration of treatment (range one day to 36 weeks), small
patient populations (n=14–232), poor methodological quality; heterogeneity of treatment regimens, and the
unclear or high risk of bias in the majority of studies.
Cancer: Duong et al. (2017) conducted a systematic review and meta-analysis of randomized controlled trials
that compared non-physical mind and body practices with control interventions for the management of fatigue in
cancer and hematopoietic stem cell transplant (HSCT) recipients. A total of 55 trials (n=4975) met inclusion
criteria. Interventions included acupuncture or acupressure (n=12 studies), mindfulness meditation (n=11 study),
relaxation techniques (n=10 studies), massage (n=6 studies), energy therapy (n=5 studies), energizing yogic
breathing (n=3 studies) and others (n=8 studies). Mindfulness and relaxation were effective at reducing fatigue
severity, but the authors noted that how to translate these findings into clinical practice had yet to be determined.
Acupuncture, acupressure, massage, energy therapy and yogic breathing were not effective. Limitations of the
studies included: limited number of studies for some modalities; short-term treatment durations; variation in the
definition of fatigue; and heterogeneity of treatment regimens, comparators (e.g., usual care, wait list, sham,
education), types of cancers, and timing of interventions (before, during and/or after treatment).
In a Cochrane systematic review investigating massage therapy with or without aromatherapy for symptom relief
in patients with cancer, Shin et al. (2016) reported that there was a lack of evidence on the clinical effectiveness
of massage therapy for this subpopulation. Nineteen studies (n=1274) met inclusion criteria and were considered
“very low-quality evidence”. Thirteen studies (n= 596 participants) compared massage with no massage. Six
studies (n=561) compared aromatherapy massage with no massage. Two studies (n=117) compared massage
with aromatherapy and massage without aromatherapy. Overall, the patient populations were too small to be
reliable and key outcomes (pain and psychological symptoms) were not reported. From the limited evidence

EVERNORTH Coverage Policy: EN0086 30
available, the authors stated that they were unable to assess the effect of adding aromatherapy to massage on
the relief of pain, psychological symptoms including anxiety and depression, physical symptom distress, or
quality of life.
Leggett et al. (2015) conducted a systematic review of the literature to evaluate the effectiveness of oral CAM
substances for women with breast cancer. Studies of women receiving or who had completed conventional
treatments for breast cancer and reported using oral CAM products (e.g., tablets, capsules, powders, liquids) for
the alleviation of cancer-related symptoms were included. Outcomes of the studies included treatment side
effects, improvement of quality of life, physical and emotional wellbeing, survival, and mortality Twenty-two
randomized and nonrandomized controlled trials met inclusion criteria. The CAM substances included: black
cohosh, a range of Chinese medicinal herbal mixtures, estrogen botanical supplements (EBS), essiac,
Ganoderma lucidum, ginseng, glutamine, grape seed proanthocyanidin extract (GSPE), guarana, herbal
remedies, and soy isoflavones. No more than four studies were found for each modality. Although there was
some weak evidence for support for relief of various symptoms by various substances, the authors advised that
the results should be viewed with caution due to the poor methodological quality of the studies. The overall
strength and quality rating of the body of evidence was considered to be limited. In conclusion, there was little
evidence to make definitive recommendations regarding the effectiveness for individual CAM therapies in women
receiving conventional treatments for breast cancer.
Rada et al. (2010) conducted a systematic review of the literature to assess the efficacy of non-hormonal
therapies for the treatment of hot flushes in women with a history of breast cancer. Sixteen randomized
controlled trials met inclusion criteria and included relaxation therapy (n=2 studies), homeopathy (n=2 studies)
and vitamin E (n=1 study). The vitamin E study reported no beneficial effects and one study on relaxation
therapy showed significant beneficial effects. Homeopathy did not lead to any differences in number and severity
of the hot flushes. Data on continuous outcomes were inconsistent.
Another systematic review evaluated the use of Chinese herbs (e.g., shenmai, pishentang) for the treatment of
chemotherapy side effects in women with breast cancer (n=542 patients) (Zhang, et al., 2007). Bardia et al.
(2006) included acupuncture, support groups, hypnosis, relaxation/imagery, herbal supplements, music therapy,
healing touch, and massage therapy (N=1499 patients) for the relief of cancer pain. Ernst et al. (November–
December 2006) also reviewed CAM for the treatment of breast cancer pain (n=15 studies) including
“psychosocial support, herbal medicine, thymus extract, transfer factor, melatonin, and factor AF2 (xenogenic
peptides)”. Due to the poor quality of the trials (e.g., small patient population without sample size justification,
short-term follow-up, lack of statistical comparison, poor definition of outcomes, and lack of control group), none
of these therapies could be recommended for pain relief in cancer patients.
Depression, Anxiety and/or Sleep Disorders: Asher et al. (2017) conducted a systematic review and meta-
analysis to compare the effectiveness of exercise and CAM therapies for the treatment of major depressive
disorder (MDD). A total of 22 randomized controlled trials were included for direct comparisons and 127 trials
were used for network meta-analyses. CAM studies included acupuncture (three studies), omega-3 fatty acids
(three trials), S-adenosyl methionine (SAMe) (one trial), and St. John’s wort (12 trials; n=1806). Two studies
comparing aerobic exercise monotherapy with SSRIs were also included. The primary outcome measure was
response to treatment on the Hamilton Depression Rating Scale (HAM-D), which was defined as a 50%
improvement of scores from baseline. Overall, there was no significant difference in outcomes with the use of a
CAM therapy and the risk of harms of CAM therapies was not adequately assessed. The studies were limited by
the unclear randomization methods, high loss to follow up, small patient populations, inadequate dosing for the
Selective serotonin reuptake inhibitors (SSRIs), and medium to high risk of bias. The overall quality of the
studies was poor. The authors did caution that SSRIs may lead to more adverse events and treatment cessation
when compared with acupuncture or St. John’s wort.
Lakhan and Vieira (2010) conducted a systematic review to evaluate the effectiveness of herbs and dietary
supplements for the treatment of anxiety and related symptoms. Twenty-one randomized controlled trials and
three open-label, uncontrolled observational studies (n=2619) met inclusion criteria. A total of 1786 patients had
a diagnosis of depression or anxiety disorder and 877 were healthy volunteers with anxiety related to acute
conditions/situations. The authors concluded that nutritional and herbal supplements were an effective method
for the treatment of anxiety but also stated that the positive effects could be due to a placebo effect. Extracts of
passionflower or kava and combinations of L-lysine and L-arginine may be treatment options for anxiety
EVERNORTH Coverage Policy: EN0086 31
symptoms and disorders, but additional studies are needed to evaluate magnesium-containing and other herbal
combinations. There was in sufficient evidence to support St. John’s wort for the treatment of anxiety. Due to the
heterogeneity of the studies and the small patient populations, meta-analysis was not possible.
In a systematic review of randomized controlled trials, Morgan and Jorm (2008) investigated multiple CAM
therapies for the treatment of depression including: herbal remedies or dietary supplements (i.e., borage,
carnitine/acetyl-L-carnitine, chromium, ginkgo biloba, Korean ginseng, Panax ginseng, lavender, lecithin,
melatonin, omega 3 fatty acids, fish oil, S-Adenosylmethionine [SAMe], saffron/cocus sativus L, selenium, St.
John’s wort), vitamins (i.e., B1, B12, C, D, and multivitamins), folate, caffeine, autogenic training, bibliotherapy,
computerized interventions, distraction, meditation, relaxation training, humor, Qigong, Tai Chi, yoga,
aromatherapy, hydrotherapy, light therapy, music, and negative air ionization. There was limited to no evidence
on these therapies, as well as inconsistent reporting of active ingredients and mechanisms, ideal dosages, side
effects and safety issues for herbs and dietary supplements. Some therapies resulted in immediate but not
sustained benefit, and tools for measuring outcomes were inconsistent and/or not well defined. Other limitations
included small patient populations, short duration, and minimal or no follow-up.
Additional systematic reviews of randomized and nonrandomized controlled trials have investigated CAM for the
treatment of depression, anxiety and/or sleep disturbances. Therapies included yoga, meditation, relaxation,
music, various herbs and vitamin supplements, Tai Chi, and Qigong (n=33 randomized controlled trials) (Meeks,
et al., 2007), St. John’s wort, homeopathy, relaxation training, music therapy, aromatherapy massage, and yoga
(n=19 studies) (Thachil, et al., 2007). Although some studies reported a therapeutic effect following a CAM
intervention (e.g., Tai Chi, relaxation techniques, and music for sleep disturbances and acupressure for sleep
and anxiety), the studies had methodological limitations (e.g., small patient populations, lack of use of systematic
psychiatric diagnoses, loss to follow-up, inadequate controls, and lack of inclusion/exclusion criteria and
assessment and reporting of CAM side effects). There is insufficient evidence to support the safety and
effectiveness of CAM for the treatment of depression.
Fibromyalgia: Zech et al. (2017) conducted a systematic review of nine randomized controlled trials (n=457) to
evaluate the efficacy, acceptability and safety of guided imagery/hypnosis (GI/H) in the treatment of fibromyalgia.
Primary outcomes included: ≥ 50% pain relief; ≥ 20% improvement of health-related quality of life; psychological
distress; disability, acceptability and safety at end of therapy; and three-month follow-up. Controls included GI/H
placebo (e.g., education, emotional support, pure relaxation), usual treatment, waiting list and active
pharmacological or nonpharmacological interventions. There was a significant benefit of GI/H compared to
controls on ≥ 50% pain relief and psychological distress at the end of therapy. Acceptability was not significantly
different compared to the control. No study reported on safety. Overall, the quality of evidence was rated as low.
Limitations of the studies included the small patient populations (n=16–100); short-term follow-ups (one week to
six months); heterogeneity of therapies (e.g., home alone therapy, individual therapy, group therapy, non-pain
related suggestions, pain-relation suggestions, number of sessions) and outcome measures. The authors noted
that it was unclear if patients with anxiety and/or depressive disorder, which are frequently associated with
fibromyalgia, were included in most studies. There is insufficient data to support GI/H for the treatment of
fibromyalgia.
Heart Failure: Gok Metin et al. (2018) conducted a systematic review including 24 randomized controlled trials
(n=1314) to evaluate the effectiveness of mind-body interventions for the treatment of high functioning individuals
with heart failure. The analysis included: seven Tai Chi studies; four studies on yoga and relaxation; two studies
each on meditation, acupuncture, and biofeedback; and one study each on stress management, Pilates and
reflexology. Studies ranged from four minutes to 26 weeks in duration. Patient populations ranged from 8–65 per
study group. Small-to-moderate improvements were reported for quality of life (14/14 studies), exercise capacity
(8/9 studies), depression (5/5 studies), anxiety and fatigue (4/4 studies), blood pressure (3/5 studies), heart rate
(5/6 studies), heart rate variability (7/9 studies), and B-type natriuretic peptide (3/4 studies). Due to the limited
number of studies, small patient populations, short duration of the studies, and poor description of the
randomization procedures conclusions could not be drawn regarding the clinical effectiveness of these
interventions for the treatment of heart failure.
Inflammatory Bowel Disease: Langhorst et al. (2015) conducted a systematic review of the literature to
evaluate the safety and effectiveness of CAM for the treatment of inflammatory bowel disease (IBD). A total of 36
randomized controlled trials and three controlled trials met inclusion criteria. CAM interventions included: herbal
EVERNORTH Coverage Policy: EN0086 32
medicine (e.g., aloe-vera gel, andrographis paniculata, artemisia absinthium, barley foodstuff, boswellia serrata,
cannabis, curcumin, evening primrose oil, Myrrhinil intest
®
, plantago ovata, silymarin, sophora, tormentil,
wheatgrass-juice, wormwood); trichuris suis ovata; mind/body interventions (e.g., lifestyle modification,
hypnotherapy, relaxation training, mindfulness); and acupuncture. Studies were eligible if they assessed at least
one of the following outcomes: induction or maintenance of remission, disease activity or symptom severity,
quality of life, or psychological variables. Overall, the studies included small patient populations and short-term
follow-ups. Due to the low number of trials for each modality and the heterogeneity of the methodology of the
studies, firm conclusions could not be made. Author-noted limitations of the studies included: high risk of bias,
data on compliance was not reported in almost half of the studies, lack of blinding, trials of traditional Chinese
medicine were not considered; and due to the small number of trails, meta-analysis could not be performed.
Because most trials tested interventions for ulcerative colitis, conclusions were mainly limited to patients with this
condition.
Otitis Media: Marom et al. (2016) conducted a systematic review of CAM therapies for the treatment of otitis
media in children. The CAM therapies considered included: acupuncture, homeopathy, herbal
medicine/phytotherapy, osteopathy, chiropractic, xylitol, ear candling, vitamin D supplement, and systemic and
topical probiotics. Overall, limitations of the studies included: small patient populations, short-term follow-ups,
high dropout rates, lack of a control group, and conflicting outcomes. Following review of the data for each CAM
intervention, it was concluded that CAM is not considered a treatment option of otitis media due to the limited
and inconsistent evidence.
Pain Management: A systematic review of data from ten randomized controlled trials (n=1055) compared
manual healing methods (i.e., massage, warm packs, other thermal manual methods, and music) to standard
care, no treatment, other non-pharmacological forms of pain management in labor or placebo. Massage provided
a greater reduction in pain intensity (measured using self-reported pain scales) than usual care during the first
stage of labor (six trials, n=362) and second and third stage of labor (two trials). Other studies showed no clear
benefit of massage over usual care for the length of labor and pharmacological pain relief. One trial reported less
anxiety during the first stage of labor for women receiving massage. One trial found an increased sense of
control from massage and two studies reported higher satisfaction with the childbirth experience with the use of
massage. All evidence was considered low to very low in quality. Very low quality showed reduced pain and
shortened labor with the use of warm packs and other thermal methods. One trial that compared manual
methods with music found very low-quality evidence of reduced pain intensity during labor in the music group
with no evidence of benefit for reduced use of pharmacological pain relief. Further research is needed to support
the clinical benefit of these modalities during labor (Smith, et al., 2018).
Smith et al. (2006) conducted a systematic review and meta-analysis of 14 randomized controlled trials (n=1537)
that compared complementary and alternative medicine (i.e., three acupuncture trials, one audio-analgesia trial,
two acupressure trials, one aromatherapy trial, one massage trial, one relaxation trial, and five hypnosis trials) to
placebo, no treatment or pharmacotherapy for pain management in labor. Acupuncture and self-hypnosis
decreased the need for pain relief and requirements for pharmacotherapy, respectively. There was insufficient
evidence to support the effectiveness of the other therapies. With the exception of the acupuncture and hypnosis
trials, the authors noted that the number of women studied was small, and few complementary therapies had
“been subjected to proper scientific study.”
Pregnancy: In a 2015 Cochrane systematic review, Matthews et al. evaluated the safety and effectiveness of
interventions for nausea, vomiting and retching in early pregnancy (up to 20 weeks’ gestation). A total of 41 trials
(n=5449) met inclusion criteria. Interventions included: acupressure, acustimulation, acupuncture, ginger,
chamomile, lemon oil, mint oil, vitamin B6 and several antiemetic drugs. Acupressure and acustimulation of P6
showed no significant benefit to this subgroup. The evidence for ginger was limited and not consistent. Meta-
analysis was not possible due to the heterogeneity of the patient populations, interventions, comparison groups,
and outcomes measures. Selection bias risk was unclear for many studies and almost half of the studies did not
fully or clearly report all pre-specified outcomes. There is a lack of high-quality evidence to support any one
intervention.
Psoriasis: Smith et al. (2009) conducted a systematic review of randomized controlled trials to identify the
evidence-based information about CAM for the treatment of psoriasis. The studies were categorized as either
vitamins/herbs/minerals; fish oil, climatotherapy, acupuncture/Chinese medicine, or mind/body. The vitamins,
EVERNORTH Coverage Policy: EN0086 33
herbs and minerals category included studies on vitamin D, inositol, zinc, selenium, neem, aloe vera, vitamin
B12 with avocado oil, mahonia aquifolium (i.e., bayberry or Oregon grape), and oleum horwathiensis. The
authors concluded that due to the low quality of the studies and conflicting results, additional studies are needed
to establish the safety and efficacy of these modalities before recommendations for CAM for the treatment of
psoriasis can be made. There is also the potential risk of side effects from aloe vera, Chinese medicine and
climatotherapy, such as allergic contact dermatitis, hepatotoxicity, and increased risk for skin cancer,
respectively.
Rheumatic Diseases: Phang et al. (2018) conducted a systematic review of randomized controlled trials to
evaluate the safety and efficacy of CAM therapies for the treatment of rheumatic diseases including rheumatoid
arthritis, osteoarthritis, fibromyalgia, gout, vasculitides, systemic sclerosis, systemic lupus erythematosus,
ankylosing spondylitis and psoriatic arthritis. A total of 60 studies met inclusion criteria and included the following
CAM therapies: acupuncture (n=9 studies); Ayurvedic treatment (n=3 studies); homeopathic treatment (n=3
studies); electricity (n=2 studies); natural products, nonvitamin and nonmineral (e.g., Dehydroepiandrosterone
[DHEA], traditional Chinese medicine, Chuanhu) (n=31 studies); megavitamin therapies (n=8 studies);
chiropractic or osteopathic manipulation (n=3 studies); and energy healing therapy (n=1 study). Most studies
investigated these therapies for the treatment of rheumatoid arthritis or osteoarthritis. Minor or no adverse events
were reported. Due to the poor quality of the evidence the clinical benefit of these therapies could not be
established. Limitations of the studies included: small patient populations; short-term follow-ups; and
heterogeneity in the study designs, treatment regimens, outcome measures, disease entities, interventions and
statistical analysis.
Rhinitis and Asthma: A systematic review by Passalacqua et al. (2006) on CAM for the treatment of rhinitis and
asthma included randomized controlled trials (n=57) involving acupuncture, herbal medicines, homeopathy,
breathing techniques, yoga, and chiropractic-spinal manipulation. The authors concluded that from a scientific
viewpoint, there was no “definitive or convincing proof of efficacy” for the use of CAM in rhinitis or asthma, and
there was an absence of quantitative measures in the studies. Therefore, it was not possible to provide
evidence-based recommendations for the use of these modalities.
Professional Societies/Organizations
American Academy of Allergy, Asthma & Immunology (AAAAI): In their clinical review of CAM (Mainardi, et
al., 2009) which included vitamins D, E, C and A, magnolol, quercetin, resveratrol, ma huang (ephedrine sinica),
Ayurvedic medicine, Kampo medicine for the treatment of asthma, atopic dermatitis, and allergic rhinitis, the
AAAAI concluded that further studies are needed using larger sample sizes, longer study durations, comparable
absolute measures, and well-constructed study designs that control for biases. They also stated that the
following are unknown: the true efficacy and safety of CAM therapies, the efficacy of CAM therapies alone (as
alternatives) in the treatment of various disorders, the individual CAM therapeutic mechanism of effects (some
may be multiple), the active component of individual CAM therapies, the potential drug-drug and drug-herb-
phytochemical and vitamin interactions.
American Academy of Neurology (AAN): AAN (2014) conducted a systematic review of the literature to
develop recommendations for CAM for the treatment of multiple sclerosis. Due to the lack of evidence or the
poor quality of the evidence, AAN concluded that the evidence was insufficient to support or refute the use of
Chinese medicine, hippotherapy, massage therapy, hypnosis, mindfulness training, music therapy, naturopathic
medicine, neural therapy, progressive muscle relaxation, tai chi, and yoga. Bases on available studies, AAN
concluded the following: 1) Ginkgo biloba is ineffective for improving cognitive function but possibly effective in
reducing fatigue; 2) low-fat diet with omega-3 fatty acid supplement is probably ineffective for reducing MS-
related relapse, disability, or MRI lesions, or for improving fatigue or quality of life (QOL); 3) reflexology is
possibly effective for reducing MS-associated paresthesia but there is a lack of data to support or refute this
modality for pain, health-related QOL, disability, spasticity, fatigue, cognition, bowel/bladder function, depression,
anxiety, or insomnia. This practice guideline was reaffirmed in February 2023.
American Academy of Pediatrics (AAP): The 2008 AAP Task Force on Complementary and Alternative
Medicine, the Provisional Section on Complementary, Holistic, and Integrative Medicine (Kemper, et al., 2008;
reaffirmed Hyman et al., 2020) published guidance on the use of CAM in pediatrics. The Task Force concluded
that pediatricians and other clinicians who care for children have the responsibility to advise and counsel patients
about relevant, safe, effective, and age-appropriate health therapies including CAM and should routinely inquire
EVERNORTH Coverage Policy: EN0086 34
as to whether or not the patient is using any specific CAM therapies. They advised the clinician to work with the
parents to consider and evaluate all appropriate treatments and monitor the patient’s response to treatments.
They also stated that the physician should be knowledgeable about CAM therapies and evidence-based
information.
In guidelines for the management of autism spectrum disorders (ASDs), the AAP (Myers, et al., 2007; reaffirmed
2020) stated that CAM therapies used to treat ASDs have included “immunoregulatory interventions (e.g., dietary
restriction of food allergens, administration of immunoglobulin or antiviral agents), detoxification therapies (e.g.,
chelation), gastrointestinal treatments (e.g., digestive enzymes, antifungal agents, probiotics, “yeast-free diet,”
gluten/casein-free diet), and dietary supplement regimens (e.g., vitamin A, vitamin C, vitamin B-6, magnesium,
folic acid, folinic acid, vitamin B-12, dimethylglycine, trimethylglycine, carnosine, omega-3 fatty acids, inositol,
various minerals),” “auditory integration training, behavioral optometry, craniosacral manipulation, dolphin-
assisted therapy, music therapy and facilitated communication”. AAP noted that many CAM therapies have been
inadequately evaluated because of methodological flaws, insufficient numbers of patients or lack of replication
and cannot be recommended. Appropriately designed trials have demonstrated no significant benefit from the
use of dimethylglycine (an amino acid), vitamin B-6 and magnesium, auditory integration training, omega-3 fatty
acids, and gluten/casein-free diet.
American College of Chest Physicians (ACCP): The ACCP (Deng, et al., 2013) published evidence-based
clinical practice guidelines on complementary therapies and integrative medicine and suggested that mind-body
modalities could be used as part of a multidisciplinary approach to treating the symptoms of cancer-related pain,
nausea and vomiting associated with chemotherapy, anxiety, and sleep and mood disturbances. Yoga and
massage therapy may be beneficial in reducing fatigue, anxiety and/or pain.
American College of Medical Toxicology (ACMT) and the American Academy of Clinical Toxicology
(AACT): In a 2015 Choosing Wisely statement, ACMT and AACT stated “Don’t use homeopathic medications,
non-vitamin dietary supplements or herbal supplements as treatments for disease or preventive health
measures”. The Societies explained that these therapies are assumed safe and effective because they are
considered “natural” products. Although reliable evidence that these products are effective is often lacking,
substantial evidence exists that they may cause harm. In addition, risks can occur us of these substances delay
or replace known effective forms of treatment or compromise the efficacy of conventional medicines. The
Societies also stated that hair testing for metal poisoning screening should not be performed for screening
purposes. Hair and nail testing are rarely required, frequently unreliable and provide limited utility after metal
exposures.
In a 2015 Choosing Wisely statement, ACMT and AACT stated, “Don’t recommend ‘detoxification’ through colon
cleansing or promoting sweating for disease treatment or prevention.” According to the Societies, there is no
objective evidence or US FDA-approved colonic hydrotherapy systems that support colonic irrigation or cleaning
for detoxification. Doing so may result in cramping, pain, dehydration, electrolyte imbalances, infections and
bowel perforation.
American College of Physicians (ACP): In clinical guidelines on the nonpharmacologic versus pharmacologic
treatment of adult patients with major depressive disorder (Qaseem, et al., 2023), ACP evaluated the use of
complementary and alternative medicines (including acupuncture, w-3 fatty acids, S-adenosyl-L-methionine, St.
John's wort [Hypericum perforatum]), and did not recommend their use. Per the ACP, areas with no evidence for
initial treatment of adults with MDD included: behavior therapy, behavior modification, humanistic therapies, yoga
and meditation. No evidence was found to support any second-line treatment strategies that involved CAM or
exercise. No evidence was available to determine differences in comparative effectiveness and risk for harms of
psychological treatments, CAM, or exercise according to different demographic characteristics, such as age, sex,
race, or ethnicity.
American College of Rheumatology (ACR): The ACR (2022) guideline on complementary and alternative
medicine for rheumatic diseases supports the integration of CAM modalities “proven to be safe and effective by
scientifically rigorous clinical trials published in the biomedical peer review literature” and advised caution in
using those therapies not scientifically studied. For interventions for which randomized controlled trials are not
feasible, “innovative methods of evaluation are needed, as are measures and standards for the generation and
EVERNORTH Coverage Policy: EN0086 35
interpretation of evidence.” The group does not recommend formally defined diet (other than Mediterranean
style), dietary supplements, electrotherapy or chiropractic therapy for the management of rheumatoid arthritis.
American Heart Association (AHA): AHA conducted a systematic review of the literature to review the data on
the potential benefits of meditation on cardiovascular risk. Some studies suggested that meditation could have
long-standing effects on the brain which provides some biological plausibility for beneficial consequences on
cardiovascular risk. Studies of the effects of meditation on cardiovascular risk included stress reduction, smoking
cessation, blood pressure reduction, insulin resistance and metabolic syndrome, endothelial function, inducible
myocardial ischemia, and primary and secondary prevention of cardiovascular disease. Overall, the studies
suggested a possible though not definitively established benefit of meditation on cardiovascular risk reduction.
The overall quality and, in some cases, quantity of study data were modest. AHA stated that given the low costs
and low risks of this intervention, meditation may be considered as an adjunct to guideline-directed
cardiovascular risk reduction by those interested in this lifestyle modification, with the understanding that the
benefits of such intervention need to be better established. Further research on meditation and cardiovascular
risk in the form of randomized controlled trials, adequately powered to meet the primary study outcome, striving
to achieve low drop-out rates, and including long-term follow-up are warranted (Levine, et al., 2017).
American Psychiatric Association: The American Psychiatric Association’s Task Force on Complementary
and Alternative Medicine (Freeman, et al., 2010) conducted a systematic review of randomized controlled trials
to evaluate the evidence on commonly used CAM therapies for the treatment of major depressive disorder
(MDD). Therapies included omega-3 fatty acids, St. John’s wort (Hypericum), folate, S-adenosyl-L-methionine
(SAMe), bright light therapy, exercise, and mindfulness psychotherapies (i.e., mindfulness-based cognitive
therapy, problem-solving therapy, well-being therapy). The Task Force concluded that although some CAM
therapies were promising, more rigorous studies to determine their role in the treatment of MDD were necessary.
It was noted that the greatest risk of pursuing a CAM therapy is the possible delay of other well-established
treatments.
National Cancer Institute (NCI): Per NCI (2023), cancer patients using or considering complementary or
alternative therapy should discuss this decision with their health care provider to ensure coordination of care.
NCI notes that some complementary and alternative therapies may interfere with standard treatment or be
harmful when used with conventional treatment.
National Comprehensive Cancer Network
®
(NCCN
®
): In their Clinical Practice Guidelines on Cancer-Related
Fatigue™, NCCN (2020) stated that complementary therapies including muscle relaxation, music therapy,
hypnosis and stress reduction based on mindfulness have been evaluated in some studies and the data
suggested that these therapies may be effective in reducing fatigue and improve sleep quality in cancer patients.
NCCN (2020) noted that yoga, cognitive distraction, relaxation exercises, biofeedback, systemic desensitization
and hypnosis with guided imagery are interventions that may be used for anticipatory nausea and vomiting. For
adult pain, NCCN (2020) lists consideration of cognitive behavioral therapy (CBT), biofeedback, breathing
exercises, distraction techniques, relaxation techniques, guided imagery, graded task assignments, hypnosis,
mindfulness-based stress reduction, cognitive restructuring and behavior activation for pain reduction.
Society for Integrative Oncology (SIO) / American Society of Clinical Oncology (ASCO): In 2022,
SIO/ASCO conducted a systematic review of the literature to develop guidelines on integrative therapies for
supportive care of adult cancer patients. The recommendations were divided into categories which included:
aromatase inhibitor (AI) related joint pain, general cancer or musculoskeletal pain, chemotherapy induced
peripheral neuropathy, procedural or surgical pain, and pain during palliative care. While the group admits many
of the recommendations are weak and based on low-quality evidence, the interventions do have clinical
relevance, with a favorable benefit-to-harm ratio. The group defined intermediate evidence as, “Intermediate
confidence that the available evidence reflects the true magnitude and direction of the net effect. Further
research is unlikely to alter the direction of the net effect; however, it might alter the magnitude of the net effect.”
Low quality of evidence was defined as, “Low confidence that the available evidence reflects the true magnitude
and direction of the net effect. Further research may change the magnitude and/or direction of this net effect.”
Moderate recommendations held “moderate confidence” of the intervention reflecting best practice. Weak
recommendations indicated “some confidence” offered of “best current guidance for practice.” SIO/ASCO
recommendations included:

EVERNORTH Coverage Policy: EN0086 36
• Evidence quality: Intermediate; Strength of recommendation: Moderate
Yoga may be offered to patients experiencing AI-related joint pain in breast cancer.
Reflexology or acupressure may be offered to patients experiencing pain during systemic
therapy for cancer treatment.
Hypnosis may be offered to patients experiencing procedural pain in cancer treatment or
diagnostic workups.
Massage may be offered to patients experiencing pain during palliative and hospice care.
• Evidence quality: Low; Strength of recommendation: Moderate
Massage may be offered to patients experiencing chronic pain following breast cancer
treatment.
• Evidence quality: Low; Strength of recommendation: Weak
Hatha yoga may be offered to patients experiencing pain after treatment for breast or head and
neck cancers.
Guided imagery with progressive muscle relaxation may be offered to patients experiencing
general pain from cancer treatment.
Reflexology or acupressure may be offered to patients experiencing chemotherapy-induced
peripheral neuropathy from cancer treatment.
Music therapy may be offered to patients experiencing surgical pain from cancer surgery.
The authors summarize several limitations of the included studies: limited methodologic rigor; inadequate
blinding; variation in dosing and format of interventions; dosing unmonitored and rarely standardized; and
inconsistent methods to assess pain among trials, which created difficulties in interpreting the data. Additionally,
most of the studies failed to report any adverse events from these interventions. The group concludes a large
RCT of a specific intervention (e.g., acupuncture) for a specific outcome (e.g., AI-related joint pain, or massage
for pain in palliative care setting) is often limited to one large trial, which does not allow for adequate replication
of data (Mao, et al., 2022).
Veterans Administration/Department of Defense (VA/DoD): In the clinical practice guideline for major
depressive disorder (MDD) (2022) the VA/DoD addressed the use of some CAM therapies. The
recommendations included the following:
• There is insufficient evidence to recommend for or against yoga, tai chi, or qi gong either as
monotherapy or as an adjunctive treatment to pharmacotherapy.
• For patients with mild MDD who are not pregnant or breastfeeding and who prefer herbal treatments to
first-line psychotherapy or pharmacotherapy, we suggest standardized extract of St. John’s wort (SJW)
as a medication monotherapy (weak evidence). The guideline noted that there is not good evidence that
dosing of SJW is consistent across formulations from different manufacturers.
• Suggested against using omega-3 fatty acids or vitamin D for treatment of MDD (weak evidence).
Medicare Coverage Determinations
Contractor
Policy Name/Number
Revision Effective
Date
NCD
National
Cellular Therapy (30.8)
Longstanding
NCD
National
Colonic Irrigation (100.7)
Longstanding
NCD
National
Hair Analysis (190.6)
8/1/1978
NCD
National
Laetrile and Related Substances (30.7)
Longstanding
NCD
National
Transcendental Meditation (30.5)
11/11/1995
LCD
CGS
Administrators, LLC
Outpatient Physical and Occupational Therapy
Services (L34049)
05/25/2023
LCD
CGS
Administrators, LLC
Outpatient Psychiatry and Psychology Services
(L34353)
05/19/2023
LCD
First Coast Service
Options, Inc.
Allergy Testing (L33261)
07/11/2021

EVERNORTH Coverage Policy: EN0086 37
Contractor
Policy Name/Number
Revision Effective
Date
LCD
First Coast Service
Options, Inc.
Psychiatric Diagnostic Evaluation and
Psychotherapy Services (L33252)
07/01/2020
LCD
National
Government
Services, Inc.
Outpatient Physical and Occupational Therapy
Services (L33631)
01/01/2020
LCD
National
Government
Services, Inc.
Psychiatry and Psychology Services (L33632)
11/28/2019
LCD
Noridian Healthcare
Solutions, LLC
Measurement of Salivary Hormones (L36846 &
L36857)
11/01/2019
LCD
Novitas Solutions,
Inc.
Allergy Testing (L36241)
07/11/2021
LCD
Novitas Solutions,
Inc.
Assays for Vitamins and Metabolic Function
(L34914)
07/01/2020
LCD
Novitas Solutions,
Inc.
Psychiatric Codes (L35101)
07/01/2020
LCD
Palmetto GBA
Outpatient Occupational Therapy (L34427)
04/03/2023
LCD
Wisconsin
Physicians Service
Insurance
Corporation
Allergy Testing (L36402)
10/01/2022
LCD
Wisconsin
Physicians Service
Insurance
Corporation
Psychiatry and Psychology Services (L34616)
10/01/2022
Coding Information
Notes:
1. This list of codes may not be all-inclusive since the American Medical Association (AMA) and Centers for
Medicare & Medicaid Services (CMS) code updates may occur more frequently than policy updates.
2. Deleted codes and codes which are not effective at the time the service is rendered may not be eligible
for reimbursement.
Experimental/Investigational/Unproven
Considered Experimental/Investigational/Unproven:
CPT
®
*
Codes
Description
90880
Hypnotherapy
0736T
Colonic lavage, 35 or more liters of water, gravity-fed, with induced defecation, including
insertion of rectal catheter
HCPCS
Codes
Description
A9152
Single vitamin/mineral/trace element, oral, per dose, not otherwise specified
A9153
Multiple vitamins, with or without minerals and trace elements, oral, per dose, not otherwise
specified
G0176
Activity therapy, such as music, dance, art or play therapies not for recreation, related to the
care and treatment of patient's disabling mental health problems, per session (45 minutes or
more)
H2032
Activity therapy, per 15 minutes

EVERNORTH Coverage Policy: EN0086 38
HCPCS
Codes
Description
J3570
Laetrile, amygdalin, vitamin B-17
M0075
Cellular therapy
S8940
Equestrian/hippotherapy, per session
S9451
Exercise classes, nonphysician provider, per session
T2036
Therapeutic camping, overnight, waiver, each session
T2037
Therapeutic camping, day waiver, each session
Considered Experimental/Investigational/Unproven when used to report chemical hair analysis:
CPT
®
*
Codes
Description
80178
Lithium
82108
Aluminum
82175
Arsenic
82300
Cadmium
82310
Calcium; total
82525
Copper
83018
Heavy metal (eg, arsenic, barium, beryllium, bismuth, antimony, mercury); quantitative, each,
not elsewhere classified
83540
Iron
83655
Lead
83735
Magnesium
83785
Manganese
83825
Mercury, quantitative
83885
Nickel
84100
Phosphorus inorganic (phosphate);
84255
Selenium
84302
Sodium; other source
HCPCS
Codes
Description
P2031
Hair analysis (excluding arsenic)
Considered Experimental/Investigational/Unproven when used to report a salivary
hormone panel:
CPT
®
*
Codes
Description
80426
Gonadotropin releasing hormone stimulation panel This panel must include the following:
Follicle stimulating hormone (FSH) (83001 x 4), Luteinizing hormone (LH) (83002 x 4)
82157
Androstenedione
82530
Cortisol; free
82533
Cortisol; total
82626
Dehydroepiandrosterone (DHEA)
82627
Dehydroepiandrosterone–sulfate (DHEA-S)
82670
Estradiol; total
82677
Estriol
82679
Estrone
82681
Estradiol; free, direct measurement (eg, equilibrium dialysis)
82784
Gammaglobulin (immunoglobulin); IgA, IgD, IgG, IgM, each
82787
Gammaglobulin (immunoglobulin); immunoglobulin subclasses (eg, IgG1, 2, 3, or 4), each
83001
Gonadotropin; follicle stimulating hormone (FSH)
83002
Gonadotropin; luteinizing hormone (LH)
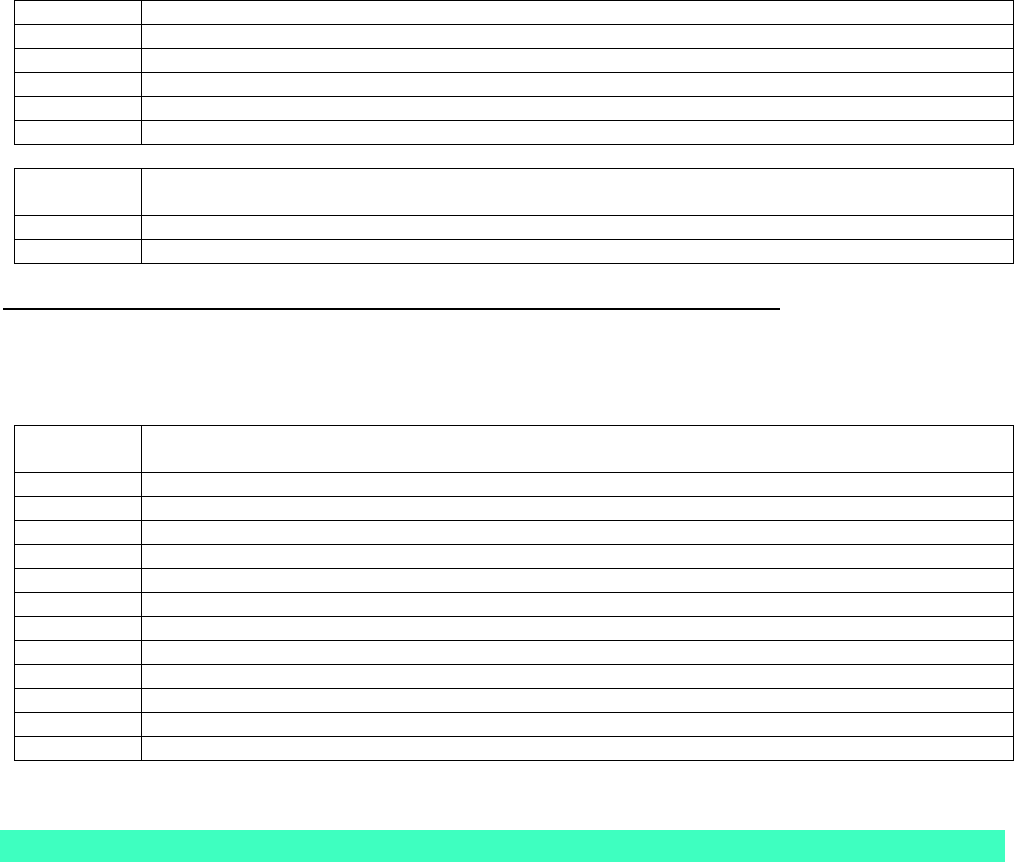
EVERNORTH Coverage Policy: EN0086 39
83498
Hydroxyprogesterone, 17-d
84144
Progesterone
84234
Receptor assay; progesterone
84402
Testosterone, free
84403
Testosterone, total
86001
Allergen specific IgG quantitative or semiquantitative, each allergen
HCPCS
Codes
Description
S3650
Saliva test, hormone level; during menopause
S3652
Saliva test, hormone level; to assess preterm labor risk
Other Complementary and Alternative Medicine Diagnostic Testing and Therapies
Considered Experimental/Investigational/Unproven when used to report any complementary or
alternative medicine diagnostic testing methods, systems, therapies or treatments listed in this
Coverage Policy that do not have an assigned code:
CPT
®
*
Codes
Description
45399
Unlisted procedure, colon
76498
Unlisted magnetic resonance procedure (eg, diagnostic, interventional)
84999
Unlisted chemistry procedure
86353
Lymphocyte transformation, mitogen (phytomitogen) or antigen induced blastogenesis
86849
Unlisted immunology procedure
90899
Unlisted psychiatric service or procedure
96379
Unlisted therapeutic, prophylactic, or diagnostic intravenous or intra-arterial injection or infusion
96549
Unlisted chemotherapy procedure
97039
Unlisted modality (specify type and time if constant attendance)
97139
Unlisted therapeutic procedure (specify)
97799
Unlisted physical medicine/rehabilitation service or procedure
99199
Unlisted special service, procedure or report
*Current Procedural Terminology (CPT
®
) ©2023 American Medical Association: Chicago, IL.
References
1. Aalbers S, Fusar-Poli L, Freeman RE, Spreen M, Ket JCF, Vink AC, Maratos A, Crawford M, Chen XJ,
Gold C. Music therapy for depression. Cochrane Database of Systematic Reviews 2017, Issue 11. Art.
No.: CD004517. DOI: 10.1002/14651858.CD004517.pub3.
2. Abbott RA, Martin AE, Newlove-Delgado TV, Bethel A, Thompson-Coon J, Whear R, Logan S.
Psychosocial interventions for recurrent abdominal pain in childhood. Cochrane Database of Systematic
Reviews 2017, Issue 1. Art. No.: CD010971. DOI:10.1002/14651858.CD010971.pub2.
3. Abraha I, Rimland JM, Trotta FM, Dell'Aquila G, Cruz-Jentoft A, Petrovic M, Gudmundsson A4, Soiza R,
O'Mahony D, Guaita A, Cherubini A. Systematic review of systematic reviews of non-pharmacological
interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop
series. BMJ Open. 2017 Mar 16;7(3):e012759.
4. Al Bedah AM, Khalil MK, Posadzki P, Sohaibani I, Aboushanab TS, AlQaed M, Ali GI. Evaluation of wet
cupping therapy: systematic review of randomized clinical trials. J Altern Complement Med. 2016
Oct;22(10):768-777.
EVERNORTH Coverage Policy: EN0086 40
5. Al‐Harasi S, Ashley PF, Moles DR, Parekh S, Walters V. Hypnosis for children undergoing dental
treatment. Cochrane Database of Systematic Reviews 2017, Issue 6. Art. No.: CD007154. DOI:
10.1002/14651858.CD007154.pub3.
6. Alexander W, Bright S , Burns P, Townes D. Wilderness Medicine. Med Clin North Am. 2016
Mar;100(2):345-56.
7. Ali A, Njike VY, Northrup V, Sabina AB, Williams AL, Liberti LS, Perlman AI, Adelson H, Katz DL.
Intravenous micronutrient therapy (Myers' Cocktail) for fibromyalgia: a placebo-controlled pilot study. J
Altern Complement Med. 2009 Mar;15(3):247-57.
8. Alraek T, Lee MS, Choi TY, Cao H, Liu J. Complementary and alternative medicine for patients with
chronic fatigue syndrome: a systematic review. BMC Complement Altern Med. 2011 Oct 7;11:87.
9. American Academy of Neurology (AAN): Summary of evidence-based guideline: complementary and
alternative medicine in multiple sclerosis. Mar 2014, reaffirmed Feb 25, 2023. Accessed Dec 12, 2023.
Available at URL address: https://www.aan.com/Guidelines/home/ByTopic?topicId=18
10. American Association of Clinical Endocrinologists (AACE). Medical guidelines for clinical practice for the
diagnosis and treatment of menopause. 2011. Updated 2017. Accessed Dec 12, 2023. Available at URL
address: American Association of Clinical Endocrinologists and American College of Endocrinology
Position Statement on Menopause–2017 Update - ScienceDirect
11. American College of Medical Toxicology (ACMT) and the American Academy of Clinical Toxicology
(AACT). Choosing Wisely. 2015. Accessed Dec 12, 2023. Available at URL address: ChoosingWisely.pdf
(acmt.net)
12. American College of Obstetricians and Gynecologists (ACOG). Committee Opinion. 532 Compounded
Bioidentical Menopausal Hormone Therapy Aug 2012; Reaffirmed 2020. Accessed Dec 13, 2021.
Available at URL address: Compounded Bioidentical Menopausal Hormone Therapy | ACOG
13. American College of Rheumatology. Position statement. Complementary and alternative medicine for
rheumatic diseases. 2023. Accessed Dec 12, 2023. Available at URL address: integrative-ra-treatment-
guideline-2022.pdf (contentstack.io)
14. American Therapeutic Recreation Association. About recreational therapy. 2020. Accessed Dec 12, 2023.
Available at URL address: https://www.atra-online.com/page/AboutRecTherapy
15. Anheyer D, Klose P, Lauche R, Saha FJ, Cramer H. Yoga for Treating Headaches: a Systematic Review
and Meta-analysis. J Gen Intern Med. 2020;35(3):846-854.
16. Arabloo J, Hamouzadeh P, Eftekharizadeh F, Mobinizadeh M, Olyaeemanesh A, Nejati M, Doaee S.
Health technology assessment of magnet therapy for relieving pain. Med J Islam Repub Iran. 2017 Jun
11;31:31.
17. Araujo RV, Fernandes AFC, Nery IS, Andrade EMLR, Nogueira LT, Azevedo FHC. Meditation effect on
psychological stress level in women with breast cancer: a systematic review. Rev Esc Enferm USP. 2019
Dec 2;53:e03529. doi: 10.1590/S1980-220X2018031303529. eCollection 2019.
18. Asher GN, Gartlehner G, Gaynes BN, Amick HR, Forneris C, Morgan LC, Coker-Schwimmer E, Boland E,
Lux LJ, Gaylord S, Bann C, Pierl CB, Lohr KN. Comparative Benefits and Harms of Complementary and
Alternative Medicine Therapies for Initial Treatment of Major Depressive Disorder: Systematic Review and
Meta-Analysis. J Altern Complement Med. 2017 Dec;23(12):907-919.
19. Babbar S, Parks-Savage AC, Chauhan SP. Yoga during pregnancy: a review. Am J Perinatol. 2012
Jun;29(6):459-64.
EVERNORTH Coverage Policy: EN0086 41
20. Bager P, Arnved J, Rønborg S, Wohlfahrt J, Poulsen LK, Westergaard T, Petersen HW, Kristensen B,
Thamsborg S, Roepstorff A, Kapel C, Melbye M. Trichuris suis ova therapy for allergic rhinitis: a
randomized, double-blind, placebo-controlled clinical trial. J Allergy Clin Immunol. 2010 Jan;125(1):123-
30.e1-3.
21. Balíková M. Hair analysis for drugs of abuse. Plausibility of interpretation. Biomed Pap Med Fac Univ
Palacky Olomouc Czech Repub. 2005 Dec;149(2):199-207.
22. Ban M, Yue X, Dou P, Zhang P. The Effects of Yoga on Patients with Parkinson's Disease: A Meta-
Analysis of Randomized Controlled Trials. Behav Neurol. 2021;2021:5582488. Published 2021 Jul 5.
23. Banerjee K, Mathie RT, Costelloe C, Howick J. Homeopathy for Allergic Rhinitis: A Systematic Review. J
Altern Complement Med. 2017 Jun;23(6):426-444.
24. Barbin J, Seetha V, Casillas JM, Paysant J, Pérennou D. The effects of mirror therapy on pain and motor
control of phantom limb in amputees: a systematic review. Ann Phys Rehabil Med. 2016 Sep;59(4):270-5.
25. Bardia A, Barton DL, Prokop LJ, Bauer BA, Moynihan TJ. Efficacy of complementary and alternative
medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol. 2006 Dec 1;24(34):5457-64.
26. Barić H, Đorđević V, Cerovečki I, Trkulja V. Complementary and Alternative Medicine Treatments for
Generalized Anxiety Disorder: Systematic Review and Meta-analysis of Randomized Controlled Trials. Adv
Ther. 2018 Mar;35(3):261-288.
27. Becker C, Lauterbach G, Spengler S, Dettweiler U, Mess F. Effects of Regular Classes in Outdoor
Education Settings: A Systematic Review on Students' Learning, Social and Health Dimensions. Int J
Environ Res Public Health. 2017 May 5;14(5). pii: E485.
28. Bennett C, Underdown A, Barlow J. Massage for promoting mental and physical health in typically
developing infants under the age of six months. Cochrane Database of Systematic Reviews 2013, Issue 4.
Art. No.: CD005038. DOI: 10.1002/14651858.CD005038.pub3.
29. Bernstein IL, Li JT, Bernstein DI, Hamilton R, Spector SL, Tan R, Sicherer S, Golden DB, Khan DA,
Nicklas RA, Portnoy JM, Blessing-Moore J, Cox L, Lang DM, Oppenheimer J, Randolph CC, Schuller DE,
Tilles SA, Wallace DV, Levetin E, Weber R, American Academy of Allergy, Asthma and Immunology,
American College of Allergy, Asthma and Immunology. Allergy diagnostic testing: an updated practice
parameter. Part 1. Ann Allergy Asthma Immunol 2008 Mar;100(3 Suppl 3):S15-S66. Accessed Dec 12,
2023. Available at URL address: https://www.aaaai.org/Allergist-Resources/Statements-Practice-
Parameters
30. Bowen D, Neill J, Crisp SJ. Wilderness adventure therapy effects on the mental health of youth
participants. Eval Program Plann. 2016 Oct;58:49-59.
31. Bradt J, Dileo C, Magill L, Teague A. Music interventions for improving psychological and physical
outcomes in cancer patients. Cochrane Database of Systematic Reviews 2016, Issue 8. Art. No.:
CD006911. DOI: 10.1002/14651858.CD006911.pub3.
32. Bridges L, Sharma M. The Efficacy of Yoga as a Form of Treatment for Depression. J Evid Based
Complementary Altern Med. 2017 Oct;22(4):1017-1028.
33. Brinsley J, Schuch F, Lederman O, et al. Effects of yoga on depressive symptoms in people with mental
disorders: a systematic review and meta-analysis. Br J Sports Med. 2021;55(17):992-1000.
34. Broderick J, Crumlish N, Waugh A, Vancampfort D. Yoga versus non-standard care for schizophrenia.
Cochrane Database of Systematic Reviews 2017, Issue 9. Art. No.: CD012052. DOI:
10.1002/14651858.CD012052.pub2.
EVERNORTH Coverage Policy: EN0086 42
35. Bronson C, Brewerton K, Ong J, Palanca C, Sullivan SJ. Does hippotherapy improve balance in persons
with multiple sclerosis: a systematic review. Eur J Phys Rehabil Med. 2010 Sep;46(3):347-53.
36. Büssing A, Ostermann T, Lüdtke R, Michalsen A. Effects of yoga interventions on pain and pain-
associated disability: a meta-analysis. J Pain. 2012 Jan;13(1):1-9.
37. Cacchio A, De Blasis E, De Blasis V, Santilli V, Spacca G. Mirror therapy in complex regional pain
syndrome type 1 of the upper limb in stroke patients. Neurorehabil Neural Repair. 2009 Oct;23(8):792-9.
38. Candy B, Jones L, Varagunam M, Speck P, Tookman A, King M. Spiritual and religious interventions for
well-being of adults in the terminal phase of disease. Cochrane Database of Systematic Reviews 2012,
Issue 5. Art. No.: CD007544.
39. Cao H, Han M, Li X, Dong S, Shang Y, Wang Q, Xu S, Liu J. Clinical research evidence of cupping therapy
in China: a systematic literature review. BMC Complement Altern Med. 2010 Nov 16;10:70.
40. Cao H, Li X, Liu J. An updated review of the efficacy of cupping therapy. PLoS One. 2012;7(2):e31793.
doi: 10.1371/journal.pone.0031793.
41. Caprara DL, Klein J, Koren G. Diagnosis of fetal alcohol spectrum disorder (FASD): fatty acid ethyl esters
and neonatal hair analysis. Ann Ist Super Sanita. 2006;42(1):39-45.
42. Carlson JJ, Farquhar JW, DiNucci E, Ausserer L, Zehnder J, Miller D, Berra, Hagerty L, Haskell WL.
Safety and efficacy of a ginkgo biloba-containing dietary supplement on cognitive function, quality of life,
and platelet function in healthy, cognitively intact older adults. J Am Diet Assoc. 2007 Mar;107(3):422-32.
43. Cassileth BR, Deng GE, Gomez JE, Johnstone PA, Kumar N, Vickers AJ; American College of Chest
Physicians. Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based
clinical practice guidelines (2nd edition). Chest. 2007 Sep;132(3 Suppl):340S-354S.
44. Centers for Medicare and Medicaid Services (CMS). Local Coverage Determinations (LCDs) alphabetical
index. Accessed Dec 12, 2023. Available at URL address: https://www.cms.gov/medicare-coverage-
database/indexes/lcd-alphabetical-index.aspx
45. Centers for Medicare and Medicaid Services (CMS). National Coverage Determination (NCDs)
alphabetical index. Accessed Dec 12, 2023. Available at URL address: https://www.cms.gov/medicare-
coverage-database/indexes/ncd-alphabetical-index.aspx
46. Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews
2013, Issue 10. Art. No.: CD004843. DOI: 10.1002/14651858.CD004843.pub3.
47. Chahla J, Piuzzi NS, Mitchell JJ, Dean CS, Pascual-Garrido C, LaPrade RF, Muschler GF. Intra-articular
cellular therapy for osteoarthritis and focal cartilage defects of the knee: a systematic review of the
literature and study quality analysis. J Bone Joint Surg Am. 2016 Sep 21;98(18):1511-21.
48. Chamine I, Atchley R, Oken BS. Hypnosis intervention effects on sleep outcomes: a systematic review. J
Clin Sleep Med.2018;14(2):271–283.
49. Chan CL, Wang CW, Ho RT, Ng SM, Chan JS, Ziea ET, Wong VC. A systematic review of the
effectiveness of qigong exercise in supportive cancer care. Support Care Cancer. 2012 Jun;20(6):1121-33.
doi: 10.1007/s00520-011-1378-3.
50. Chao M, Wang C, Dong X, Ding M. The Effects of Tai Chi on Type 2 Diabetes Mellitus: A Meta-Analysis. J
Diabetes Res. 2018 Jul 5;2018:7350567.
51. Chen PY, Liu YM, Chen ML. The effect of hypnosis on anxiety in patients with cancer: a meta-analysis.
Worldviews Evid Based Nurs. 2017 Mar 7. doi: 10.1111/wvn.12215. [Epub ahead of print].
EVERNORTH Coverage Policy: EN0086 43
52. Chen X, Deng L, Jiang X, Wu T. Chinese herbal medicine for oesophageal cancer. Cochrane Database of
Systematic Reviews 2016, Issue 1. Art. No.: CD004520. DOI: 10.1002/14651858.CD004520.pub7.
53. Chen Y, Xiang XY, Chin KHR, et al. Acupressure for labor pain management: a systematic review and
meta-analysis of randomized controlled trials. Acupunct Med. 2021;39(4):243-252.
54. Choi TY, Choi J, Kim KH, Lee MS. Moxibustion for the treatment of osteoarthritis: a systematic review and
meta-analysis. Rheumatol Int. 2012 Oct;32(10):2969-78.
55. Clement K, Covertson CR, Johnson MJ, Dearing K. St. John's wort and the treatment of mild to moderate
depression: a systematic review. Holist Nurs Pract. 2006 Jul-Aug;20(4):197-203.
56. Cochrane Complementary Medicine. Glossary of CAM terms. Accessed on Dec 12, 2023. Available at
URL address: https://cam.cochrane.org/glossary-cam-terms
57. Cooley K, Szczurko O, Perri D, Mills EJ, Bernhardt B, Zhou Q, Seely D. Naturopathic care for anxiety: a
randomized controlled trial ISRCTN78958974. PLoS One. 2009 Aug 31;4(8):e6628.
58. Cramer H, Anheyer D, Saha FJ, Dobos 2. Yoga for posttraumatic stress disorder - a systematic review and
meta-analysis. BMC Psychiatry. 2018 Mar 22;18(1):72.
59. Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality
of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane
Database of Systematic Reviews 2017, Issue 1. Art. No.: CD010802. DOI:
10.1002/14651858.CD010802.pub2.
60. Cramer H, Lauche R, Paul A, Langhorst J, Kümmel S, Dobos GJ. Hypnosis in breast cancer care: a
systematic review of randomized controlled trials. Integr Cancer Ther. 2015 Jan;14(1):5-15.
61. Crawford MJ, Gold C, Odell-Miller H, Thana L, Faber S, Assmus J, Bieleninik Ł, Geretsegger M, Grant C,
Maratos A, Sandford S, Claringbold A, McConachie H, Maskey M, Mössler KA, Ramchandani P, Hassiotis
A. International multicentre randomised controlled trial of improvisational music therapy for children with
autism spectrum disorder: TIME-A study. Health Technol Assess. 2017 Oct;21(59):1-40.
62. Crawford MJ, Killaspy H, Barnes TR, Barrett B, Byford S, Clayton K, Dinsmore J, Floyd S, Hoadley A,
Johnson T, Kalaitzaki E, King M, Leurent B, Maratos A, O'Neill FA, Osborn DP, Patterson S, Soteriou T,
Tyrer P, Waller D; MATISSE project team. Group art therapy as an adjunctive treatment for people with
schizophrenia: multicentre pragmatic randomised trial. BMJ. 2012 Feb 28;344:e846
63. Cui J, Yan JH, Yan LM, Pan L, Le JJ, Guo YZ. Effects of yoga in adults with type 2 diabetes mellitus: A
meta-analysis. J Diabetes Investig. 2017 Mar;8(2):201-209. doi: 10.1111/jdi.12548.
64. Davidson JR, Crawford C, Ives JA, Jonas WB. Homeopathic treatments in psychiatry: a systematic review
of randomized placebo-controlled studies. J Clin Psychiatry. 2011 Jun;72(6):795-805.
65. Demir Doğan M. The effect of reiki on pain: A meta-analysis. Complement Ther Clin Pract. 2018
May;31:384-387.
66. Deng GE, Rausch SM, Jones LW, Gulati A, Kumar NB, Greenlee H, Pietanza MC, Cassileth BR.
Complementary therapies and integrative medicine in lung cancer: Diagnosis and management of lung
cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest.
2013 May;143(5 Suppl):e420S-36S. doi: 10.1378/chest.12-2364. Accessed Dec 12, 2023. Available at
URL address: https://www.guidelinecentral.com/summaries/complementary-therapies-and-integrative-
medicine-in-lung-cancer-diagnosis-and-management-of-lung-cancer-3rd-ed-american-college-of-chest-
physicians-evidence-based-clinical-practice-guidelines/#section-society
EVERNORTH Coverage Policy: EN0086 44
67. Diagnos-Techs
™
. Our clinical approach. 2019. Accessed Dec 19, 2023. Available at URL address: Index of
Panels & Tests - DiagnosTechs, Inc.
68. Ding M. Tai Chi for stroke rehabilitation: a focused review. Am J Phys Med Rehabil. 2012
Dec;91(12):1091-6.
69. Dobud WW, Harper NJ. Of Dodo birds and common factors: A scoping review of direct comparison trials in
adventure therapy. Complement Ther Clin Pract. 2018 May;31:16-24.
70. Duong N, Davis H, Robinson PD, Oberoi S, Cataudella D, Culos-Reed SN, Gibson F, Götte M, Hinds P,
Nijhof SL, Tomlinson D, van der Torre P, Ladas E, Cabral S, Dupuis LL, Sung L. Mind and body practices
for fatigue reduction in patients with cancer and hematopoietic stem cell transplant recipients: A systematic
review and meta-analysis. Crit Rev Oncol Hematol. 2017 Dec;120:210-216.
71. Ebrahim Soltani A, Mohammadinasab H, Goudarzi M, Arbabi S, Mohtaram R, Afkham K, Momenzadeh S,
Darabi ME. Acupressure using ondansetron versus metoclopramide on reduction of postoperative nausea
and vomiting after strabismus surgery. Arch Iran Med. 2010 Jul;13(4):288-93.
72. Ein N, Li L, Vickers K. The effect of pet therapy on the physiological and subjective stress response: A
meta-analysis. Stress Health. 2018 Oct;34(4):477-489.
73. Ernst E, Pittler MH, Wider B, Boddy K. Complementary/alternative medicine for supportive cancer care:
development of the evidence-base. Support Care Cancer. 2007 May;15(5):565-8.
74. Ernst E, Posadzki P, Lee MS. Reflexology: an update of a systematic review of randomised clinical trials.
Maturitas. 2011 Feb;68(2):116-20.
75. Ernst E, Schmidt K, Baum M. Complementary/Alternative therapies for the treatment of breast cancer. A
systematic review of randomized clinical trials and a critique of current terminology. Breast J. 2006 Nov-
Dec;12(6):526-30.
76. Ezendam D, Bongers RM, Jannink MJ. Systematic review of the effectiveness of mirror therapy in upper
extremity function. Disabil Rehabil. 2009;31(26):2135-49.
77. Farhadi K, Choubsaz M, Setayeshi K, Kameli M, Bazargan-Hejazi S, Heidari Zadie Z, Ahmadi A. The
effectiveness of dry-cupping in preventing post-operative nausea and vomiting by P6 acupoint stimulation:
arandomized controlled trial. Medicine (Baltimore). 2016 Sep;95(38):e4770.
78. Fernee CR, Gabrielsen LE, Andersen AJ, Mesel T. Unpacking the Black Box of Wilderness Therapy: A
Realist Synthesis. Qual Health Res. 2017 Jan;27(1):114-129.
79. Filipek PA, Accardo PJ, Ashwal S, Baranek GT, Cook EH Jr, Dawson G, Gordon B, Gravel JS, Johnson
CP, Kallen RJ, Levy SE, Minshew NJ, Ozonoff S, Prizant BM, Rapin I, Rogers SJ, Stone WL, Teplin SW,
Tuchman RF, Volkmar FR. Practice parameter: screening and diagnosis of autism: report of the Quality
Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society.
Neurology. 2000 Aug 22;55(4):468-79. Posted Mar 26, 2013. Accessed Dec 18, 2023. Available at URL
address: http://www.childneurologysociety.org
80. Fiori G, Marzi T, Bartoli F, Bruni C, Ciceroni C, Palomba M, Zolferino M, Corsi E, Galimberti M, Moggi
Pignone A, Viggiano MP, Guiducci S, Calamai M, Matucci-Cerinic M. The challenge of pet therapy in
systemic sclerosis: evidence for an impact on pain, anxiety, neuroticism and social interaction. Clin Exp
Rheumatol. 2018 Jul-Aug;36 Suppl 113(4):135-141.
81. Fisch S, Brinkhaus B, Teut M. Hypnosis in patients with perceived stress - a systematic review. BMC
Complement Altern Med. 2017 Jun 19;17(1):323.
EVERNORTH Coverage Policy: EN0086 45
82. Fitzpatrick E, Holland OJ, Vanderlelie JJ. Ozone therapy for the treatment of chronic wounds: a systematic
review. Int Wound J, 15 (4), 633-644 Aug 2018.
83. Flower A, Liu JP, Lewith G, Little P, Li Q. Chinese herbal medicine for endometriosis. Cochrane Database
of Systematic Reviews 2012, Issue 5. Art. No.: CD006568. DOI: 10.1002/14651858.CD006568.pub3
84. Flyckt RL, Liu J, Frasure H, Wekselman K, Buch A, Kingsberg SA. Comparison of salivary versus serum
testosterone levels in postmenopausal women receiving transdermal testosterone supplementation versus
placebo. Menopause. 2009 Jul-Aug;16(4):680-8.
85. Freeman MP, Fava M, Lake J, Trivedi MH, Wisner KL, Mischoulon D. Complementary and alternative
medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin
Psychiatry. 2010 Jun;71(6):669-81.
86. Gagnier JJ, DeMelo J, Boon H, Rochon P, Bombardier C. Quality of reporting of randomized controlled
trials of herbal medicine interventions. Am J Med. 2006 Sep;119(9):800.e1-11.
87. Garland EL, Brintz CE, Hanley AW, et al. Mind-Body Therapies for Opioid-Treated Pain: A Systematic
Review and Meta-analysis [published online ahead of print, 2019 Nov 4]. JAMA Intern Med.
2019;180(1):91-105.
88. Gaudet LA, Elliott SA, Ali S, et al. Pet therapy in the emergency department and ambulatory care: A
systematic review and meta-analysis [published online ahead of print, 2021 Nov 24]. Acad Emerg Med.
2021;10.1111/acem.14421.
89. Genova Diagnostics. Test menu. 2023. Accessed Dec 19,2023. Available at URL address: Products |
Genova Diagnostics (gdx.net)
90. Geretsegger M, Mössler KA, Bieleninik , Chen XJ, Heldal TO, Gold C. Music therapy for people with
schizophrenia and schizophrenia-like disorders. Cochrane Database of Systematic Reviews 2017, Issue 5.
Art. No.: CD004025. DOI:10.1002/14651858.CD004025.pub4.
91. Godley E, Smith MA. Efficacy of acupressure for chronic low back pain: A systematic review. Complement
Ther Clin Pract. 2020;39:101146.
92. Gok Metin Z, Ejem D, Dionne-Odom JN, Turkman Y, Salvador C, Pamboukian S, Bakitas M. Mind-Body
Interventions for Individuals With Heart Failure: A Systematic Review of Randomized Trials. J Card Fail.
2018 Mar;24(3):186-201.
93. Goksen N, Calis M, Dogan S, Talay Calis H, Ozgocmen S. Magnetic resonance therapy for knee
osteoarthritis: a randomized, double blind placebo controlled trial. Eur J Phys Rehabil Med. 2016 Jan 22.
[Epub ahead of print]
94. Gómez-Romero M, Jiménez-Palomares M, Rodríguez-Mansilla J, Flores-Nieto A, Garrido-Ardila EM,
González López-Arza MV. Benefits of music therapy on behaviour disorders in subjects diagnosed with
dementia: a systematic review. Neurologia. 2017 May;32(4):253-263.
95. González-Valero G, Zurita-Ortega F, Ubago-Jiménez JL, Puertas-Molero P. Use of meditation and
cognitive behavioral therapies for the treatment of stress, depression and anxiety in students. A systematic
review and meta-analysis. Int J Environ Res Public Health. 2019 Nov 10;16(22). pii: E4394. doi:
10.3390/ijerph16224394.
96. Gothe NP, Khan I, Hayes J, Erlenbach E, Damoiseaux JS. Yoga Effects on Brain Health: A Systematic
Review of the Current Literature. Brain Plast. 2019 Dec 26;5(1):105-122. doi: 10.3233/BPL-190084.
97. Greenlee H, Balneaves LG, Carlson LE, Cohen M, Deng G, Hershman D, Mumber M, Perlmutter J, Seely
D, Sen A, Zick SM, Tripathy D; Society for Integrative Oncology Guidelines Working Group. Clinical
EVERNORTH Coverage Policy: EN0086 46
practice guidelines on the use of integrative therapies as supportive care in patients treated for breast
cancer. J Natl Cancer Inst Monogr. 2014 Nov;2014(50):346-58. Accessed Dec 19, 2023. Available at URL
address: Practice Guidelines (integrativeonc.org)
98. Guindos-Sanchez L, Lucena-Anton D, Moral-Munoz JA, Salazar A, Carmona-Barrientos I. The
Effectiveness of Hippotherapy to Recover Gross Motor Function in Children with Cerebral Palsy: A
Systematic Review and Meta-Analysis. Children (Basel). 2020;7(9):106. Published 2020 Aug 19.
99. Guo BQ, Li HB, Liu YY. Association between hair lead levels and autism spectrum disorder in children: A
systematic review and meta-analysis. Psychiatry Res. 2019;276:239-249.
100. Harder H, Parlour L, Jenkins V. Randomised controlled trials of yoga interventions for women with breast
cancer: a systematic literature review. Support Care Cancer. 2012 Dec;20(12):3055-64.
101. Hawke K, van Driel ML, Buffington BJ, McGuire TM, King D. Homeopathic medicinal products for
preventing and treating acute respiratory tract infections in children. Cochrane Database of Systematic
Reviews 2018, Issue 4. Art. No.: CD005974. DOI: 10.1002/14651858.CD005974.pub4.
102. Hillier S, Worley A. The effectiveness of the feldenkrais method: a systematic review of the evidence. Evid
Based Complement Alternat Med. 2015;2015:752160.
103. Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM,
Sorbero ME, Maglione MA. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-
analysis. Ann Beav Med. 2017 Apr;51(2):199-213.
104. Hilton MP, Zimmermann EF, Hunt WT. Ginkgo biloba for tinnitus. Cochrane Database of Systematic
Reviews 2013, Issue 3. Art. No.: CD003852.
105. Hmwe NT, Subramaniam P, Tan LP. Effectiveness of acupressure in promoting sleep quality: a systematic
review of randomized controlled trials. Holist Nurs Pract. 2016 Sep-Oct;30(5):283-93.
106. Hohmann L, Bradt J, Stegemann T, Koelsch S. Effects of music therapy and music-based interventions in
the treatment of substance use disorders: A systematic review. PLoS One. 2017 Nov 15;12(11):e0187363.
107. Huang CF, Guo SE, Chou FH. Auricular acupressure for overweight and obese individuals: A systematic
review and meta-analysis. Medicine (Baltimore). 2019 Jun;98(26):e16144. doi:
10.1097/MD.0000000000016144.
108. Huang HC, Chen KH, Kuo SF, Chen IH. Can foot reflexology be a complementary therapy for sleep
disturbances? Evidence appraisal through a meta-analysis of randomized controlled trials. J Adv Nurs.
2021;77(4):1683-1697.
109. Huang X, Zeng LR, Chen FS, Zhu JP, Zhu MH. Trichuris suis ova therapy in inflammatory bowel disease:
A meta-analysis. Medicine (Baltimore). 2018 Aug;97(34):e12087.
110. Hyman SL, Levy SE, Myers SM; Council on children with disabilities, section on developmental and
behavioral pediatrics. Identification, Evaluation, and Management of Children With Autism Spectrum
Disorder. Pediatrics. 2020 Jan;145(1):e20193447. doi: 10.1542/peds.2019-3447. Epub 2019 Dec 16.
PMID: 31843864.
111. IntraCellular Diagnosics, Inc
®
. ExaTest. 2019. Accessed Dec 19, 2023. Available at URL address:
http://www.exatest.com/
112. Jain S, Mills PJ. Biofield therapies: helpful or full of hype? A best evidence synthesis. Int J Behav Med.
2010 Mar;17(1):1-16.
EVERNORTH Coverage Policy: EN0086 47
113. Jiang XH, Chen XJ, Xie QQ, Feng YS, Chen S, Peng JS. Effects of art therapy in cancer care: A
systematic review and meta-analysis. Eur J Cancer Care (Engl). 2020;29(5):e13277.
114. Jing Z, Yang X, Ismail KMK, Chen XY, Wu T. Chinese herbal medicine for premenstrual syndrome.
Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No.: CD006414. DOI:
10.1002/14651858.CD006414.pub2.
115. Jorm AF, Allen NB, O'Donnell CP, Parslow RA, Purcell R, Morgan AJ. Effectiveness of complementary
and self-help treatments for depression in children and adolescents. Med J Aust. 2006 Oct 2;185(7):368-
72.
116. Karkou V, Meekums B. Dance movement therapy for dementia. Cochrane Database of Systematic
Reviews 2017, Issue 2. Art. No.: CD011022. DOI: 10.1002/14651858.CD011022.pub2.
117. Karsch-Völk M, Barrett B, Kiefer D, Bauer R, Ardjomand-Woelkart K, Linde K. Echinacea for preventing
and treating the common cold. Cochrane Database of Systematic Reviews 2014, Issue 2. Art. No.:
CD000530. DOI: 10.1002/14651858.CD000530.pub3.
118. Kemper KJ, Vohra S, Walls R; Task Force on Complementary and Alternative Medicine; Provisional
Section on Complementary, Holistic, and Integrative Medicine. American Academy of Pediatrics. The use
of complementary and alternative medicine in pediatrics. Pediatrics. 2008 Dec;122(6):1374-86.
119. Kernspin MBST. MBST Therapy. 2019. Accessed Dec 19, 2023. Available at URL address:
https://www.mbst.de/
120. Kim JI, Choi JY, Lee H, Lee MS, Ernst E. Moxibustion for hypertension: a systematic review. BMC
Cardiovasc Disord. 2010 Jul 5;10:33.
121. Kohn CM, Paudyal P. A systematic review and meta-analysis of complementary and alternative medicine
in asthma. Eur Respir Rev. 2017 Jan 31;26(143). pii: 160092.
122. Krpan D, Stritzinger B, Lukenda I, Overbeck J, Kullich W. Non-pharmacological treatment of osteoporosis
with Nuclear Magnetic Resonance Therapy (NMR-Therapy). Periodicum Biologorum. VOL. 117, No 1,
161–165, 2015.
123. Kullich W, Overbeck K, Spiegel HU. One-year-survey with multicenter data of more than 4,500 patients
with degenerative rheumatic diseases treated with therapeutic nuclear magnetic resonance. J Back
Musculoskelet Rehabil. 2013;26(1):93-104.
124. Kullich W, Schwann H, Machreich K, Ausserwinkler M. Additional outcome improvement in the
rehabilitation of chronic low back pain after nuclear resonance therapy. Rheumatologia. 2006;20(1):7–12.
125. Kuppili PP, Parmar A, Gupta A, Balhara YP2. Role of Yoga in Management of Substance-use Disorders: A
Narrative Review. J Neurosci Rural Pract. 2018 Jan-Mar;9(1):117-122.
126. Kwon CY, Lee B, Park KS. Oriental herbal medicine and moxibustion for polycystic ovary syndrome: A
meta-analysis. Medicine (Baltimore). 2018 Oct;97(43):e12942.
127. Kwong JSW, Lau HLC, Yeung PH. Yoga for secondary prevention of coronary heart disease. Cochrane
Database of Systemic Reviews 2015, Issue 7. Art No. CD009506. DOI:
10.1002/14651858.CD009506.pub4.
128. Lakhan SE, Vieira KF. Nutritional and herbal supplements for anxiety and anxiety-related disorders:
systematic review. Nutr J. 2010 Oct 7;9:42.
129. Lam TH, Chung KF, Yeung WF, Yu BY, Yung KP, Ng TH. Hypnotherapy for insomnia: a systematic review
and meta-analysis of randomized controlled trials. Complement Ther Med. 2015 Oct;23(5):719-32.
EVERNORTH Coverage Policy: EN0086 48
130. Langhorst J, Wulfert H, Lauche R, Klose P, Cramer H, Dobos GJ, Korzenik J. Systematic review of
complementary and alternative medicine treatments in inflammatory bowel diseases. J Crohns Colitis.
2015 Jan;9(1):86-106.
131. Lauche R, Peng W, Ferguson C, Cramer H, Frawley J, Adams J, Sibbritt D. Efficacy of Tai Chi and qigong
for the prevention of stroke and stroke risk factors: A systematic review with meta-analysis. Medicine
(Baltimore). 2017 Nov;96(45):e8517.
132. Lawrence M, Celestino Junior FT, Matozinho HHS, Govan L, Booth J, Beecher J. Yoga for stroke
rehabilitation. Cochrane Database of Systematic Reviews 2017, Issue 12. Art. No.: CD011483. DOI:
10.1002/14651858.CD011483.pub2.
133. Lee MS, Choi TY, Park JE, Lee SS, Ernst E. Moxibustion for cancer care: a systematic review and meta-
analysis. BMC Cancer. 2010c Apr 7;10:130.
134. Lee DH, Kim JI, Lee MS, Choi TY, Choi SM, Ernst E. Moxibustion for ulcerative colitis: a systematic review
and meta-analysis. BMC Gastroenterol. 2010a Apr 7;10:36.
135. Lee MS, Shin BC, Kim JI, Han CH, Ernst E. Moxibustion for stroke rehabilitation: systematic review.
Stroke. 2010b Apr;41(4):817-20.
136. Leggett S, Koczwara B, Miller M. The impact of complementary and alternative medicines on cancer
symptoms, treatment side effects, quality of life, and survival in women with breast cancer--a systematic
review. Nutr Cancer. 2015;67(3):373-91.
137. Lenoir Dit Caron R, Coquart J, Gilliaux M. Effect of yoga on health-related quality of life in central nervous
system disorders: A systematic review. Clin Rehabil. 2021;35(11):1530-1543.
138. Levine GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK, Michos ED, Norris K, Ray
IB, Saban KL, Shah T, Stein R, Smith SC Jr; American Heart Association Council on Clinical Cardiology;
Council on Cardiovascular and Stroke Nursing; and Council on Hypertension. Meditation and
Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. J Am Heart
Assoc. 2017 Sep 28;6(10). Accessed Dec 19, 2023. Available at URL address:
https://www.ahajournals.org/doi/10.1161/JAHA.117.002218
139. Li A, Wei ZJ, Liu Y, Li B, Guo X, Feng SQ. Moxibustion treatment for knee osteoarthritis: a systematic
review and meta-analysis. Medicine (Baltimore). 2016 Apr;95(14):e3244.
140. Li AW, Goldsmith CA. The effects of yoga on anxiety and stress. Altern Med Rev. 2012 Mar;17(1):21-35.
141. Li GY, Wang W, Liu GL, Zhang Y. Effects of Tai Chi on balance and gait in stroke survivors: A systematic
meta-analysis of randomized controlled trials. J Rehabil Med. 2018 Jul 17;50(7):582-588.
142. Li JQ, Guo W, Sun ZG, Huang QS, Lee EY, Wang Y, Yao XD. Cupping therapy for treating knee
osteoarthritis: The evidence from systematic review and meta-analysis. Complement Ther Clin Pract. 2017
Aug;28:152-160.
143. Li L, Dou L, Leung PC, Chung TKH,Wang CC. Chinese herbal medicines for unexplained recurrent
miscarriage. Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No.: CD010568. DOI:
10.1002/14651858.CD010568.pub2.
144. Li L, Dou L, Leung PC, Wang CC. Chinese herbal medicines for threatened miscarriage. Cochrane
Database of Systematic Reviews 2012, Issue 5. Art. No.: CD008510. DOI:
10.1002/14651858.CD008510.pub2.

EVERNORTH Coverage Policy: EN0086 49
145. Li Q, Qi X, Zhang Z. Intra-articular oxygen-ozone versus hyaluronic acid in knee osteoarthritis: A meta-
analysis of randomized controlled trials. Int J Surg. 2018 Oct;58:3-10.
146. Liang B, Yan C, Zhang L, Yang Z, Wang L, Xian S, Lu L. The effect of acupuncture and moxibustion on
heart function in heart failure patients: a systematic review and meta-analysis. Evid Based Complement
Alternat Med. 2019 Oct 20;2019:6074967. doi: 10.1155/2019/6074967. eCollection 2019.
147. Lim EC, Poh RL, Low AY, Wong WP. Effects of Pilates-based exercises on pain and disability in
individuals with persistent nonspecific low back pain: a systematic review with meta-analysis. J Orthop
Sports Phys Ther. 2011 Feb;41(2):70-80.
148. Lin CL, Hwang SL, Jiang P, Hsiung NH. Effect of Music Therapy on Pain After Orthopedic Surgery-A
Systematic Review and Meta-Analysis. Pain Pract. 2020;20(4):422-436.
149. Liu J, Zhang P, Tian J, Li L, Li J, Tian JH, Yang K. Ozone therapy for treating foot ulcers in people with
diabetes. Cochrane Database Syst Rev. 2015 Oct 27;(10):CD008474. doi:
10.1002/14651858.CD008474.pub2.
150. Lu G, Jia R, Liang D, Yu J, Wu Z, Chen C. Effects of music therapy on anxiety: A meta-analysis of
randomized controlled trials. Psychiatry Res. 2021;304:114137
151. Ma SY, Wang Y, Xu JQ, Zheng L. Cupping therapy for treating ankylosing spondylitis: The evidence from
systematic review and meta-analysis. Complement Ther Clin Pract. 2018 Aug;32:187-194.
152. Madden K, Middleton P, Cyna AM, Matthewson M, Jones L. Hypnosis for pain management during labour
and childbirth. Cochrane Database of Systematic Reviews 2016, Issue 5. Art. No.: CD009356. DOI:
10.1002/14651858.CD009356.pub3
153. Magalhaes FN, Dotta L, Sasse A, Teixera MJ, Fonoff ET. Ozone therapy as a treatment for low back pain
secondary to herniated disc: a systematic review and meta-analysis of randomized controlled trials. Pain
Physician. 2012 Mar-Apr;15(2):E115-29.
154. Magee WL, Clark I, Tamplin J, Bradt J. Music interventions for acquired brain injury. Cochrane Database
of Systematic Reviews 2017, Issue 1. Art. No.: CD006787. DOI: 10.1002/14651858.CD006787.pub3.
155. Mainardi T, Kapoor S, Bielory L. Complementary and alternative medicine: herbs, phytochemicals and
vitamins and their immunologic effects. J Allergy Clin Immunol. 2009 Feb;123(2):283-94.
156. Makvandi S, Mirzaiinajmabadi K, Sadeghi R, Mahdavian M, Karimi L. Meta-analysis of the effect of
acupressure on duration of labor and mode of delivery. Int J Gynaecol Obstet. 2016 Oct;135(1):5-10.
157. Mao JJ, Ismaila N, Bao T, Barton D, Ben-Arye E, Garland EL, Greenlee H, Leblanc T, Lee RT, Lopez AM,
Loprinzi C, Lyman GH, MacLeod J, Master VA, Ramchandran K, Wagner LI, Walker EM, Bruner DW, Witt
CM, Bruera E. Integrative Medicine for Pain Management in Oncology: Society for Integrative Oncology-
ASCO Guideline. J Clin Oncol. 2022 Dec 1;40(34):3998-4024. doi: 10.1200/JCO.22.01357. Epub 2022
Sep 19. PMID: 36122322.
158. Marom T, Marchisio P, Tamir SO, Torretta S, Gavriel H, Esposito S. Complementary and alternative
medicine treatment options for otitis media: a systematic review. Medicine (Baltimore). 2016
Feb;95(6):e2695.
159. Matthews A, Haas DM, O’Mathúna DP, Dowswell T. Interventions for nausea and vomiting in early
pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No.: CD007575. DOI:
10.1002/14651858.CD007575.pub4
160. McClafferty H, Vohra S, Bailey M, Brown M, Esparham A, Gerstbacher D, Golianu B, Niemi A, Sibinga E,
Weydert J, Ming Yeh A and SECTION ON INTEGRATIVE MEDICINE. American Academy of Pediatrics.
EVERNORTH Coverage Policy: EN0086 50
Pediatric integrative medicine. Pediatrics September 2017, 140 (3) e20171961; Accessed Dec 19, 2023.
Available at URL address: https://doi.org/10.1542/peds.2017-1961
161. Meeks TW, Wetherell JL, Irwin MR, Redwine LS, Jeste DV. Complementary and alternative treatments for
late-life depression, anxiety, and sleep disturbance: a review of randomized controlled trials. J Clin
Psychiatry. 2007 Oct;68(10):1461-71.
162. Meng D, Chunyan W, Xiaosheng D, Xiangren Y. The Effects of Qigong on Type 2 Diabetes Mellitus: A
Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2018 Jan 3;2018:8182938.
163. Milazzo S, Horneber M. Laetrile treatment for cancer. Cochrane Database Syst Rev. 2015 Apr
28;(4):CD005476. doi: 10.1002/14651858.CD005476.pub4.
164. Milling LS, Valentine KE, LoStimolo LM, Nett AM, McCarley HS. Hypnosis and the Alleviation of Clinical
Pain: A Comprehensive Meta-Analysis. Int J Clin Exp Hypn. 2021;69(3):297-322.
165. Miranda S, Marques A. Pilates in noncommunicable diseases: A systematic review of its effects.
Complement Ther Med. 2018 Aug;39:114-130.
166. Miyasaki JM, Shannon K, Voon V, Ravina B, Kleiner-Fisman G, Anderson K, Shulman LM, Gronseth G,
Weiner WJ; Quality Standards Subcommittee of the American Academy of Neurology. Practice Parameter:
evaluation and treatment of depression, psychosis, and dementia in Parkinson disease (an evidence-
based review): report of the Quality Standards Subcommittee of the American Academy of Neurology.
Neurology. 2006 Apr 11;66(7):996-1002.
167. Moretti F, De Ronchi D, Bernabei V, Marchetti L, Ferrari B, Forlani C, Negretti F, Sacchetti C, Atti AR. Pet
therapy in elderly patients with mental illness. Psychogeriatrics. 2011 Jun;11(2):125-9.
168. Morgan AJ, Jorm AF. Self-help interventions for depressive disorders and depressive symptoms: a
systematic review. Ann Gen Psychiatry. 2008 Aug 19;7:13.
169. Moseley GL, Gallace A, Spence C. Is mirror therapy all it is cracked up to be? Current evidence and future
directions. Pain. 2008 Aug 15;138(1):7-10.
170. Moser HW, Raymond GV, Lu SE, Muenz LR, Moser AB, Xu J, Jones RO, Loes DJ, Melhem ER, Dubey P,
Bezman L, Brereton NH, Odone A. Follow-up of 89 asymptomatic patients with adrenoleukodystrophy
treated with Lorenzo's oil. Arch Neurol. 2005 Jul;62(7):1073-80.
171. Mutz M, Müller J. Mental health benefits of outdoor adventures: Results from two pilot studies. J Adolesc.
2016 Jun;49:105-14.
172. Myers SM, Johnson CP; American Academy of Pediatrics Council on Children With Disabilities.
Management of children with autism spectrum disorders. Pediatrics. 2007 Nov;120(5):1162-82. Reaffirmed
Aug 2014. Accessed Dec 19, 2023. Available at URL address:
https://pediatrics.aappublications.org/content/120/5/1162.long
173. Nahas R, Moher M. Complementary and alternative medicine for the treatment of type 2 diabetes. Can
Fam Physician. 2009 Jun;55(6):591-6.
174. National Cancer Institute (NCI). Antioneoplastons (PDQ
®
). Nov 19, 2007. Published online Aug 15, 2019.
Accessed Dec 13, 2021. Available at URL address: https://www.ncbi.nlm.nih.gov/books/NBK65872/
175. National Cancer Institute (NCI). Complementary and alternative medicine. Apr 10, 2015, updated Nov 10,
2021. Updated Jun 12, 2023 Accessed Dec 19, 2023. Available at URL address:
http://www.cancer.gov/about-cancer/treatment/cam
EVERNORTH Coverage Policy: EN0086 51
176. National Cancer Institute (NCI). [MTH-68] Newcastle Disease Virus (PDQ
®
) [MTH-68] Health professional
version. Aug 2018. Accessed Dec 19, 2023. Available at URL address:
http://www.cancer.gov/cancertopics/pdq/cam/NDV/HealthProfessional
177. National Cancer Institute (NCI). Laetrile/Amygdalin PDQ
®
. Health professional version. Mar 15 2017,
updated Jun 14, 2022. Accessed Dec 19, 2023. Available at URL address: https://www.cancer.gov/about-
cancer/treatment/cam/hp/laetrile-pdq
178. National Cancer Institute (NCI). Health Professional Version. PDQ
®
(Physician Data Query). Cancer
information summaries [internet]. Health professional version. 2019, updated Dec 7, 2021. Accessed Dec
19, 2023. Available at URL address: https://www.ncbi.nlm.nih.gov/books/NBK82221/
179. National Center for Complementary and Alternative Medicine. Mar 7, 2019. Updated Dec 19, 2023. Health
Topics A-Z. Accessed Dec 19, 2023. Available at URL address: http://nccam.nih.gov/health/atoz.htm
180. National Center for Complementary and Integrative Health, Clinical Practice guidelines. Sept 24, 2017.
Updated Dec 19, 2023. Accessed Dec 19, 2023. Available at URL address:
https://nccih.nih.gov/health/providers/clinicalpractice.htm
181. National Center for Complementary and Alternative Medicine (NCCAM). Complementary, Alternative, or
Integrative Health: What’s In a Name? Jun 2016, last updated Dec 2023. Accessed Dec 19, 2023.
Available at URL address: http://nccam.nih.gov/health/whatiscam/
182. National Comprehensive Cancer Network
®
(NCCN
®
). NCCN clinical practice guidelines in oncology
™
.
Cancer-related fatigue. V.2.2024. Oct 30, 2023. Accessed Dec 19, 2023. Available at URL address:
https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1424
183. National Comprehensive Cancer Network
®
(NCCN
®
). NCCN clinical practice guidelines in oncology
™
.
Adult cancer pain. V.2.2023. Jul 31, 2023. Accessed Dec 19, 2023. Available at URL address:
https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1413
184. National Comprehensive Cancer Network
®
(NCCN
®
). NCCN clinical practice guidelines in oncology
™
.
Antiemesis. V 1.2024. Dec 13, 2023. Accessed Dec 19, 2023. Available at URL address: Supportive Care
(nccn.org)
185. Ng QX, Loke W, Foo NX, et al. A systematic review of the clinical use of Withania somnifera
(Ashwagandha) to ameliorate cognitive dysfunction. Phytother Res. 2020;34(3):583-590.
186. O'Haire ME, McKenzie SJ, Beck AM, Slaughter V. Social behaviors increase in children with autism in the
presence of animals compared to toys. PLoS One. 2013;8(2):e57010.
187. Ooi SL, Giovino M, Pak SC. Transcendental meditation for lowering blood pressure: An overview of
systematic reviews and meta-analyses. Complement Ther Med. 2017 Oct;34:26-34.
188. Palsson OS. Hypnosis Treatment of Gastrointestinal Disorders: A Comprehensive Review of the Empirical
Evidence. Am J Clin Hypn. 2015 Oct;58(2):134-58.
189. Pan RY, Hsu YC, Wong CS, Lin SL, Li TY, Cherng CH, Ko SC, Yeh CC. Comparing complementary
alternative treatment for chronic shoulder pain of myofascial origin: Collateral meridian therapy versus local
tender area-related meridians therapy. Medicine (Baltimore). 2016 Aug;95(35):e4634.
190. Panebianco M, Sridharan K, Ramaratnam S. Yoga for epilepsy. Cochrane Database of Systematic
Reviews. 2017, Issue 10. Art.No.: CD001524. DOI: 10.1002/14651858.CD001524.pub3
191. Passalacqua G. ARIA update: I – Systematic review of complementary and alternative medicine for rhinitis
and asthma. J Allergy Clin Immunol. 2006 May 1; 117(5): 1054-62.
EVERNORTH Coverage Policy: EN0086 52
192. Patyar S, Joshi R, Byrav DS, Prakash A, Medhi B, Das BK. Bacteria in cancer therapy: a novel
experimental strategy. J Biomed Sci. 2010 Mar 23;17(1):21.
193. Peckham EJ, Cooper K, Roberts ER, Agrawal A, Brabyn S, Tew G. Homeopathy for treatment of irritable
bowel syndrome. Cochrane Database Syst Rev. 2019 Sep 4;9:CD009710. doi:
10.1002/14651858.CD009710.pub3.
194. Pereira LM, Obara K, Dias JM, Menacho MO, Guariglia DA, Schiavoni D, Pereira HM, Cardoso JR.
Comparing the Pilates method with no exercise or lumbar stabilization for pain and functionality in patients
with chronic low back pain: systematic review and meta-analysis. Clin Rehabil. 2012 Jan;26(1):10-20.
195. Phang JK, Kwan YH, Goh H, Tan VIC, Thumboo J, Østbye T, Fong W. Complementary and alternative
medicine for rheumatic diseases: A systematic review of randomized controlled trials. Complement Ther
Med. 2018 Apr;37:143-157.
196. Posadzki P, Alotaibi A, Ernst E. Adverse effects of homeopathy: a systematic review of published case
reports and case series. Int J Clin Pract. 2012 Dec;66(12):1178-88. doi: 10.1111/ijcp.12026.
197. Posadzki P, Lewandowski W, Terry R, Ernst E, Stearns A. Guided imagery for non-musculoskeletal pain: a
systematic review of randomized clinical trials. J Pain Symptom Manage. 2012 Jul;44(1):95-104. doi:
10.1016/j.jpainsymman.2011.07.014.
198. Provençal SC, Bond S, Rizkallah E, El-Baalbaki G. Hypnosis for burn wound care pain and anxiety: A
systematic review and meta-analysis. Burns. 2018 May 23. pii: S0305-4179(18)30244-4. doi:
10.1016/j.burns.2018.04.017. [Epub ahead of print].
199. Qaseem A, Barry MJ, Kansagara D; Clinical Guidelines Committee of the American College of Physicians.
Nonpharmacologic versus pharmacologic treatment of adult patients with major depressive disorder: a
clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016 Mar
1;164(5):350-9. Updated Jan 24, 2023. Accessed Dec 19, 2023. Available at URL address:
Nonpharmacologic and Pharmacologic Treatments of Adults in the Acute Phase of Major Depressive
Disorder: A Living Clinical Guideline From the American College of Physicians | Annals of Internal
Medicine (acpjournals.org)
200. Qin J, Zhang Y, Wu L, He Z, Huang J, Tao J, Chen L. Effect of Tai Chi alone or as additional therapy on
low back pain: Systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore).
2019 Sep;98(37):e17099. doi: 10.1097/MD.0000000000017099.
201. Rada G, Capurro D, Pantoja T, Corbalán J, Moreno G, Letelier LM, Vera C. Non-hormonal interventions
for hot flushes in women with a history of breast cancer. Cochrane Database of Systematic Reviews 2010,
Issue 9. Art. No.: CD004923. DOI: 10.1002/14651858.CD004923.pub2.
202. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, Espie CA, et al. European
guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017 Dec;26(6):675-700.
203. Rosche B, Wernecke KD, Ohlraun S, Dörr JM, Paul F. Trichuris suis ova in relapsing-remitting multiple
sclerosis and clinically isolated syndrome (TRIOMS): study protocol for a randomized controlled trial.
Trials. 2013 Apr 25;14:112.
204. Rothgangel AS, Braun SM, Beurskens AJ, Seitz RJ, Wade DT. The clinical aspects of mirror therapy in
rehabilitation: a systematic review of the literature. Int J Rehabil Res. 2011 Mar ;34(1):1-13.
205. Salfinger H, Salomonowitz G, Friedrich KM, Hahne J, Holzapfel J, Friedrich M. Nuclear magnetic
resonance therapy in lumbar disc herniation with lumbar radicular syndrome: effects of the intervention on
pain intensity, health-related quality of life, disease-related disability, consumption of pain medication,
duration of sick leave. Eur Spine J. 2015 Jun;24(6):1296-308.

EVERNORTH Coverage Policy: EN0086 53
206. Salhofer I, Will A, Monsef I, Skoetz N. Meditation for adults with haematological malignancies. Cochrane
Database of Systematic Reviews 2016, Issue 2. Art. No.: CD011157. DOI:
10.1002/14651858.CD011157.pub2.
207. Sandborn WJ, Elliott DE, Weinstock J, Summers RW, Landry-Wheeler A, Silver N, Harnett MD, Hanauer
SB. Randomised clinical trial: the safety and tolerability of Trichuris suis ova in patients with Crohn's
disease. Aliment Pharmacol Ther. 2013 Aug;38(3):255-63.
208. Sawitzke AD, Shi H, Finco MF, Dunlop DD, Harris CL, Singer NG, Bradley JD, Silver D, Jackson CG, Lane
NE, Oddis CV, Wolfe F, Lisse J, Furst DE, Bingham CO, Reda DJ, Moskowitz RW, Williams HJ, Clegg
DO. Clinical efficacy and safety of glucosamine, chondroitin sulphate, their combination, celecoxib or
placebo taken to treat osteoarthritis of the knee: 2-year results from GAIT. Ann Rheum Dis. 2010
Aug;69(8):1459-64.
209. Schneider C, Schneider B, Hanisch J, van Haselen R. The role of a homoeopathic preparation compared
with conventional therapy in the treatment of injuries: an observational cohort study. Complement Ther
Med. 2008;16(1):22-27. doi:10.1016/j.ctim.2007.04.004
210. Schölmerich J, Fellermann K, Seibold FW, Rogler G, Langhorst J, Howaldt S, Novacek G, et al.;
International TRUST-2 Study Group. A Randomised, Double-blind, Placebo-controlled Trial of Trichuris
suis ova in Active Crohn's Disease. J Crohns Colitis. 2017 Apr 1;11(4):390-399.
211. Schouten KA, de Niet GJ, Knipscheer JW, Kleber RJ, Hutschemaekers GJ. The effectiveness of art
therapy in the treatment of traumatized adults: a systematic review on art therapy and trauma. Trauma
Violence Abuse. 2015 Apr;16(2):220-8.
212. Sconza C, Leonardi G, Kon E, et al. Oxygen-ozone therapy for the treatment of low back pain: a
systematic review of randomized controlled trials. Eur Rev Med Pharmacol Sci. 2021;25(19):6034-6046.
213. Selles RW, Schreuders TA, Stam HJ. Mirror therapy in patients with causalgia (complex regional pain
syndrome type II) following peripheral nerve injury: two cases. J Rehabil Med. 2008 Apr;40(4):312-4.
214. Sephton SE, Salmon P, Weissbecker I, Ulmer C, Floyd A, Hoover K, Studts JL. Mindfulness meditation
alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis
Rheum. 2007 Feb 15;57(1):77-85.
215. Shen YH, Nahas R. Complementary and alternative medicine for treatment of irritable bowel syndrome.
Can Fam Physician. 2009 Feb;55(2):143-8.
216. Shin ES, Seo KH, Lee SH, Jang JE, Jung YM, Kim MJ, Yeon JY. Massage with or without aromatherapy
for symptom relief in people with cancer. Cochrane Database of Systematic Reviews 2016, Issue 6. Art.
No.: CD009873. DOI: 10.1002/14651858.CD009873.pub3.
217. Sieczkowska SM, Casagrande PO, Coimbra DR, Vilarino GT, Andreato LV, Andrade A. Effect of yoga on
the quality of life of patients with rheumatic diseases: Systematic review with meta-analysis. Complement
Ther Med. 2019 Oct;46:9-18. doi: 10.1016/j.ctim.2019.07.006. Epub 2019 Jul 12.
218. Siniscalco D, Antonucci N. Possible use of Trichuris suis ova in autism spectrum disorders therapy. Med
Hypotheses. 2013 Jul;81(1):1-4.
219. Skillgate E, Bohman T, Holm LW, Vingård E, Alfredsson L. The long-term effects of naprapathic manual
therapy on back and neck pain - results from a pragmatic randomized controlled trial. BMC Musculoskelet
Disord. 2010 Feb 5;11:26.
220. Smith CA, Collins CT, Crowther CA. Aromatherapy for pain management in labour. Cochrane Database of
Systematic Reviews. 2011, Issue 7. Art. No.: CD009215. DOI: 10.1002/14651858.CD009215.
EVERNORTH Coverage Policy: EN0086 54
221. Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain
management in labour. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD003521.
DOI: 10.1002/14651858.CD003521.pub2.
222. Smith CA, Levett KM, Collins CT, Dahlen HG, Ee CC, Suganuma M. Massage, reflexology and other
manual methods for pain management in labour. Cochrane Database Syst Rev. 2018 Mar
28;3:CD009290. doi: 10.1002/14651858.CD009290.pub3.
223. Smith N, Weymann A, Tausk FA, Gelfand JM. Complementary and alternative medicine for psoriasis: a
qualitative review of the clinical trial literature. J Am Acad Dermatol. 2009 Nov;61(5):841-56.
224. Song GM, Tian X, Jin YH, Deng YH, Zhang H, Pang XL, Zhou JG. Moxibustion is an alternative in treating
knee osteoarthritis: the evidence from systematic review and meta-analysis. Medicine (Baltimore). 2016
Feb;95(6):e2790.
225. SpectraCell Laboratories. Nutritional status & health. 2020. Accessed Dec 19, 2023. Available at URL
address: http://www.spectracell.com/mnt/
226. Suárez-Iglesias D, Miller KJ, Seijo-Martínez M, Ayán C. Benefits of pilates in parkinson's disease: a
systematic review and meta-analysis. Medicina (Kaunas). 2019 Aug 13;55(8). pii: E476. doi:
10.3390/medicina55080476.
227. Summers RW. Novel and future medical management of inflammatory bowel disease. Surg Clin North Am.
2007 Jun;87(3):727-41.
228. Summers RW, Elliott DE, Urban JF Jr, Thompson RA, Weinstock JV. Trichuris suis therapy for active
ulcerative colitis: a randomized controlled trial. Gastroenterology. 2005 Apr;128(4):825-32.
229. Sun YJ, Yuan JM, Yang ZM. Effectiveness and safety of moxibustion for primary insomnia: a systematic
review and meta-analysis. BMC Complement Altern Med. 2016 Jul 13;16:217.
230. Sur D, Sabarimurugan S, Advani S. The Effects of Martial Arts on Cancer-Related Fatigue and Quality of
Life in Cancer Patients: An Up-to-Date Systematic Review and Meta-Analysis of Randomized Controlled
Clinical Trials. Int J Environ Res Public Health. 2021;18(11):6116. Published 2021 Jun 6.
231. Szczurko O, Cooley K, Mills EJ, Zhou Q, Perri D, Seely D. Naturopathic treatment of rotator cuff tendinitis
among Canadian postal workers: a randomized controlled trial. Arthritis Rheum. 2009 Aug 15;61(8):1037-
45.
232. Taghva A, Silvetz R, Ring A, Kim KY, Murphy KT, Liu CY, Jin Y. Magnetic Resonance Therapy Improves
Clinical Phenotype and EEG Alpha Power in Posttraumatic Stress Disorder. Trauma Mon. 2015
Nov;20(4):e27360.
233. Teut M, Lüdtke R, Schnabel K, Willich SN, Witt CM. Homeopathic treatment of elderly patients--a
prospective observational study with follow-up over a two year period. BMC Geriatr. 2010 Feb 22;10:10.
234. Thachil AF, Mohan R, Bhugra D. The evidence base of complementary and alternative therapies in
depression. J Affect Disord. 2007 Jan;97(1-3):23-35.
235. Thieme H, Morkisch N, Mehrholz J, Pohl M, Behrens J, Borgetto B, Dohle C. Mirror therapy for improving
motor function after stroke. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No.: CD008449.
DOI: 10.1002/14651858.CD008449.pub3.
236. Torkzahrani S, Mahmoudikohani F, Saatchi K, Sefidkar R, Banaei M. The effect of acupressure on the
initiation of labor: a randomized controlled trial. Women Birth. 2017 Feb;30(1):46-50.

EVERNORTH Coverage Policy: EN0086 55
237. U.S. Food and Drug Administration (FDA). Federal Food and Drugs Act of 1906 (The "Wiley Act"). May 20,
2009; updated Apr 24, 2019. Accessed Dec 19, 2023. Available at URL address:
https://www.fda.gov/aboutfda/history/forgshistory/evolvingpowers/ucm054819.htm
238. U.S. Food and Drug Administration (FDA). Draft guidance. Complementary and alternative medicine
products and their regulation by the Food and Drug Administration. Dec 2006; updated May 6, 2020.
Accessed Dec 19, 2023. Available at URL address:
http://www.fda.gov/RegulatoryInformation/Guidances/ucm144657.htm
239. U.S. Food and Drug Administration (FDA). Dietary supplements. Jun 8, 2015; updated Mar 6, 2023.
Accessed Dec 19, 2023. Available at URL address:
https://www.fda.gov/food/dietarysupplements/default.htm
240. U.S. Food and Drug Administration (FDA). Labeling & nutrition. 2016; updated Dec 13, 2023. Accessed
Dec 19, 2023. Available at URL address: https://www.fda.gov/food/labelingnutrition/default.htm
241. Uttley L, Stevenson M, Scope A, Rawdin A, Sutton A. The clinical and cost effectiveness of group art
therapy for people with non-psychotic mental health disorders: a systematic review and cost-effectiveness
analysis. BMC Psychiatry. 2015 Jul 7;15:151.
242. van der Steen JT, Smaling HJA, van der Wouden JC, Bruinsma MS, Scholten RJPM, Vink AC. Music-
based therapeutic interventions for people with dementia. Cochrane Database of Systematic Reviews
2018, Issue 7. Art. No.: CD003477. DOI:10.1002/14651858.CD003477.pub4.
243. Van Vu D, Molassiotis A, Ching SSY, Le TT. Effects of Qigong on symptom management in cancer
patients: A systematic review. Complement Ther Clin Pract. 2017 Nov;29:111-121.
244. Vancampfort D, Vansteelandt K, Scheewe T, Probst M, Knapen J, De Herdt A, De Hert M. Yoga in
schizophrenia: a systematic review of randomised controlled trials. Acta Psychiatr Scand. 2012
Jul;126(1):12-20.
245. Vanden Bossche L, Vanderstraeten G. A multi-center, double-blind, randomized, placebo-controlled trial
protocol to assess Traumeel injection vs dexamethasone injection in rotator cuff syndrome: the TRAumeel
in ROtator cuff syndrome (TRARO) study protocol. BMC Musculoskelet Disord. 2015;16(1):8. Published
2015 Feb 4.
246. VanderVaart S, Gijsen VM, de Wildt SN, Koren G. A systematic review of the therapeutic effects of Reiki. J
Altern Complement Med. 2009 Nov;15(11):1157-69.
247. Verma S, Thuluvath PJ. Complementary and alternative medicine in hepatology: review of the evidence of
efficacy. Clin Gastroenterol Hepatol. 2007 Apr;5(4):408-16.
248. Veterans Administration/Department of Defense (VA/DoD). Clinical practice guidelines. Major depressive
disorder (MDD). 2022. Accessed Dec 19, 2023. Available at URL address:
https://www.healthquality.va.gov/guidelines/mh/mdd/index.asp
249. Voyageur. Outward bound school. 2017. Accessed Dec 19, 2023. Available at URL address:
http://vobs.org/blog/tag/at-risk/
250. Walia N, Matas J, Turner A, Gonzalez S, Zoorob R. Yoga for Substance Use: A Systematic Review. J Am
Board Fam Med. 2021;34(5):964-973.
251. Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, Schmid CH. Tai Chi on psychological well-being:
systematic review and meta-analysis. BMC Complement Altern Med. 2010 May 21;10:23.
EVERNORTH Coverage Policy: EN0086 56
252. Wang CW, Ng SM, Ho RT, Ziea ET, Wong VC, Chan CL. The effect of qigong exercise on immunity and
infections: a systematic review of controlled trials. Am J Chin Med. 2012;40(6):1143-56. doi:
10.1142/S0192415X1250084X.
253. Wang T, Xu C, Pan K, Xiong H. Acupuncture and moxibustion for chronic fatigue syndrome in traditional
Chinese medicine: a systematic review and meta-analysis. BMC Complement Altern Med. 2017 Mar
23;17(1):163. doi: 10.1186/s12906-017-1647-x.
254. Wang WL, Chen KH, Pan YC, Yang SN, Chan YY. The effect of yoga on sleep quality and insomnia in
women with sleep problems: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):195.
Published 2020 May 1.
255. Wang Y, Chen Z, Wu Z, Ye X, Xu X. Pilates for Overweight or Obesity: A Meta-Analysis. Front Physiol.
2021;12:643455. Published 2021 Mar 11.
256. Webb AN, Kukuruzovic RH, Catto-Smith AG, Sawyer SM. Hypnotherapy for treatment of irritable bowel
syndrome. Cochrane. Database of Systematic Reviews 2007, Issue 4. Art. No.: CD005110. DOI:
10.1002/14651858.CD005110.pub2.
257. Wei X, Wang S, Li L, Zhu L. Clinical Evidence of Chinese Massage Therapy (Tui Na) for Cervical
Radiculopathy: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med.
2017;2017:9519285.
258. Wieland LS, Skoetz N, Pilkington K, Vempati R, D’Adamo CR, Berman BM. Yoga treatment for chronic
non-specific low back pain. Cochrane Database of Systematic Reviews 2017, Issue 1. Art. No.:
CD010671. DOI: 10.1002/14651858.CD010671.pub2.
259. Wilderness Adventures. Our Philosophy & Goals. 2020. Accessed Dec 19, 2023. Available at URL
address: https://www.wildernessadventures.com/philosophy-goals/
260. Wilkens P, Scheel IB, Grundnes O, Hellum C, Storheim K. Effect of glucosamine on pain-related disability
in patients with chronic low back pain and degenerative lumbar osteoarthritis: a randomized controlled trial.
JAMA. 2010 Jul 7;304(1):45-52.
261. Wołowiec P, Michalak I, Chojnacka K, Mikulewicz M. Hair analysis in health assessment. Clin Chim Acta.
2013 Apr 18;419:139-71. doi: 10.1016/j.cca.2013.02.001.
262. Wood MJ, Molassiotis A, Payne S. What research evidence is there for the use of art therapy in the
management of symptoms in adults with cancer? A systematic review. Psychooncology. 2011
Feb;20(2):135-45. doi: 10.1002/pon.1722.
263. World Health Organization (WHO). WHO Priorities on traditional, complementary and integrative
healthcare with civil society: 2014-2025 Jul 10, 2023. Accessed Dec 19, 2023. Available at URL address:
WHO Director-General discusses priorities on traditional, complementary and integrative healthcare with
civil society
264. Wu TJ, Chen KH, Chiu WK, et al. Optimal timing and effect of music therapy in patients with burn injuries:
Systematic review and meta-analysis of randomized controlled trials [published online ahead of print, 2021
Aug 3]. Burns. 2021;S0305-4179(21)00201-1.
265. Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, Park CL, Pescatello LS. Yoga as
antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc. 2019
Mar;94(3):432-446. doi: 10.1016/j.mayocp.2018.09.023. Epub 2019 Feb 18.
266. Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo RWJG, Cabral CMN, Menezes Costa LC,
Costa LOP. Pilates for low back pain. Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No.:
CD010265. DOI: 10.1002/14651858.CD010265.pub2.

EVERNORTH Coverage Policy: EN0086 57
267. Yang L, Tan JY, Ma H, Zhao H, Lai J, Chen JX, Suen LKP. Warm-needle moxibustion for spasticity after
stroke: A systematic review of randomized controlled trials. Int J Nurs Stud. 2018 Jun;82:129-138.
268. Yang ZY, Zhong HB, Mao C, Yuan JQ, Huang YF, Wu XY, Gao YM, Tang JL. Yoga for asthma. Cochrane
Database of Systematic Reviews 2016, Issue 4. Art. No.: CD010346. DOI:
10.1002/14651858.CD010346.pub2.
269. Yeh GY, Wang C, Wayne PM, Phillips R. Tai chi exercise for patients with cardiovascular conditions and
risk factors: a systematic review. J Cardiopulm Rehabil Prev. 2009 May-Jun;29(3):152-60.
270. Yun GJ, Chun MH, Park JY, Kim BR. The synergic effects of mirror therapy and neuromuscular electrical
stimulation for hand function in stroke patients. Ann Rehabil Med. 2011 Jun;35(3):316-21.
271. Zafra-Tanaka JH, Pacheco-Barrios K, Tellez WA, Taype-Rondan A. Effects of dog-assisted therapy in
adults with dementia: a systematic review and meta-analysis. BMC Psychiatry. 2019 Jan 24;19(1):41. doi:
10.1186/s12888-018-2009-z.
272. Zech N, Hansen E, Bernardy K, Häuser W. Efficacy, acceptability and safety of guided imagery/hypnosis in
fibromyalgia - a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2017
Feb;21(2):217-227.
273. Zeng W, Guo Y, Wu G, Liu X, Fang Q. Mirror therapy for motor function of the upper extremity in patients
with stroke: A meta-analysis. J Rehabil Med. 2018 Jan 10;50(1):8-15.
274. Zeng X, Liu M, Yang Y, Li Y, Asplund K. Ginkgo biloba for acute ischaemic stroke. Cochrane Database of
Systematic Reviews 2005, Issue 4. Art. No.: CD003691. DOI: 10.1002/14651858.CD003691.pub2
275. Zhang M, Liu X, Li J, He L, Tripathy D. Chinese medicinal herbs to treat the side-effects of chemotherapy
in breast cancer patients. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No.: CD004921.
DOI: 10.1002/14651858.CD004921.pub2.
276. Zhang Y, Deng H, Tang Z. Efficacy of Cellular Therapy for Diabetic Foot Ulcer: A Meta-Analysis of
Randomized Controlled Clinical Trials. Cell Transplant. 2017 Dec;26(12):1931-1939.
277. Zhou K, Zhang J, Xu L,Wu T, Lim CED. Chinese herbal medicine for subfertile women with polycystic
ovarian syndrome. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No.: CD007535. DOI:
10.1002/14651858.CD007535.pub3.
278. Zhu X, Liew Y, Liu ZL. Chinese herbal medicine for menopausal symptoms. Cochrane Database of
Systematic Reviews 2016, Issue 3. Art. No.: CD009023. DOI: 10.1002/14651858.CD009023.pub2.
Revision Details
Type of Revision
Summary of Changes
Date
Annual Review
• No policy statement changes.
02/15/2024
All Evernorth Health Services products and services are provided exclusively by or through affiliates of the
Evernorth companies. © 2024 Evernorth Health Services
