
ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
CUSTOMER INFORMATION SHEET –ICICI Lombard Criti Shield Plus
Description is illustrative and not exhaustive
S.NO
Title
Description
Policy Clause No.
1
Product Name
ICICI Lombard Criti Shield Plus
2
What am I covered for?
Section A : Critical Illness
Benefit 1 : Comprehensive Critical Illness
Part III of Wordings
This cover has been broadly divided into five critical illness buckets.
Name of the bucket
No. of illnesses covered
Bucket 1 - Cancer and blood
disorders
4 Major/1 Minor
Bucket 2 -Heart and Blood Vessel
10 Major/11 Minor
Bucket 3 -Major Organs
14 Major /12 Minor
Bucket 4 -Nervous System
24 Major/8 Minor
Bucket 5 -Other Illness
3 Major/5Minor
In the event of any minor illness the company shall pay 25% of
the Sum Insured subject to a maximum of 12.50lac specified in
the Policy Schedule against that bucket and for any major critical
illness the company shall pay 100 % of the Sum Insured
specified in the Policy Schedule against that bucket. If a major
illness is followed by a minor illness from the same bucket the
company shall only pay the remaining 75% of the sum insured
as specified against that bucket in the Policy Schedule.
The amount payable will be on the First Diagnosis of any one of
the Critical Illnesses listed in the policy wordings.
There is a survival period and waiting period applicable to this
cover as specified on the policy schedule.
Illustration 1
Insured can opt for any of the Critical Illness bucket as per plan
available at inception. The SI payable will be independent for each
bucket if more than one bucket is selected.
1. e.g At policy inception if Mr. XYZ opts for all buckets Cancer
and blood disorders, Heart and Blood Vessel, Major Organs,
Nervous System, Other Illness, he can intimate a claim under all
these buckets independently/simultaneously.
Incase Mr. XYZ is diagnosed with Stroke resulting in permanent
symptoms (Nervous System -Major) in 5
th
month, if the claim is
payable as per policy Terms and conditions we will pay 100% of
SI allocated for Nervous System bucket.
The Nervous System bucket will be exhausted and no renewal
of this bucket will be allowed to the customer.
In the 7
th
month Mr. XYZ is diagnosed with Pulmonary Embolism
(Heart and Blood Vessel-Minor),he can claim for 25% of SI from
Heart and Blood Vessel bucket.
Incase Mr. XYZ consequently suffers from a Myocardial
Infarction (Heart and Blood Vessel -Major) we will pay balance
75% (since we have already paid minor claim of 25% under this
bucket) once this claim has been paid the Heart and Blood
Vessel bucket will be exhausted and no subsequent renewal will
be done for this bucket
Illustration 2:
Mr. PQR a 33yr old has opted for plan which has “Heart and Blood
Vessel” bucket for 1 year Policy Tenure and 3lac SI for a base
premium of 270/- . After the waiting period of the policy is over Mr.
PQR is diagnosed with Other Serious Coronary Artery Diseases in
the 5
th
month. He is eligible to claim for 25% SI which is 75000/-.
Now only 75% of the SI is remaining in “Heart and Blood Vessel
bucket. At the time of renewal, we will be collecting the premium for
100% of SI however our liability will be only towards the balance
Sum Insured which is 75% of SI(in this example 225000).
Under Section A
1.1
Benefit 2: ICU Benefit (Add On)
Part III of Wordings

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
In the event of a hospital admission if an insured is admitted in ICU
on account of any surgery or infection for a minimum of 5 or 7 days
as specified in Policy Schedule, the company shall pay the Sum
Insured as specified in the Policy Schedule against this benefit, in
consideration of payment of additional premium. The surgery or
infection and stay in the ICU must be directly due to the same cause
and confirmed as necessary medical treatment. Add on cover will
not be renewed incase base bucket is exhausted
Under Section A
2.1
Benefit 3: Cancer Restore Benefit (Add On)
Part III of Wordings
In consideration of payment of additional premium this cover pays
the sum insured specified against this Benefit on account of a re
diagnosed or recurred major cancer once a Major cancer (Cancer
of Specified Severity) claim has already been considered and paid
under this policy. A Waiting period of 3 years will be applicable from
the date of diagnosis of the first Major Cancer (Cancer of Specified
Severity) claim admitted under this policy for this Benefit to be
triggered
This Benefit 3 cannot be opted at the time of renewal or during the
policy period.
Illustration 3:
Mr. RST a 40yr old male has opted for plan which has ‘Cancer and
blood disorders’ bucket and add on ‘Cancer Restore Benefit’ for 1
year tenure for 5lac SI with base premium as 970/- & 340/- for
‘Cancer and blood disorders Bucket’ and ‘Cancer Restore Cover’
respectively. After the initial waiting period Mr. RST is diagnosed
with Major Cancer (Cancer of Specified severity),after evaluation of
required documents we pay the major claim with 100% payout of 5
lac sum insured. Since the customer has opted for cancer restore
benefit he will be eligible to claim under this benefit provided the
customer renews this policy subject to having received the premium
for the ‘Cancer and blood disorders’ bucket under benefit 1 and
cancer restore benefit as per the original Sum Insured and age at
the time of renewal. Mr. RST is diagnosed with Cancer relapse after
the 3 years waiting period he will be eligible to claim for ‘Cancer
Restore’ Benefit.
Under Section A
3.1
Section B : Add on Cover
Benefit: 4: Major Surgical Procedures
Part III of Wordings
In the event an Insured Person is Hospitalized on the written advice
of the treating Medical Practitioner due to an Illness contracted or
any Injury sustained during the Period of Cover, and is advised by a
Medical Practitioner qualified as a Surgeon to undergo a Surgical
Procedure specified in Annexure 2 of this Policy and has undergone
the surgery, we will pay the percentage of the Sum Insured as a
lumpsum specified in the Policy Schedule in the manner specified in
the Annexure 2 for each of the listed surgeries. This cover can only
be availed with benefit 1. Add on cover will not be renewed incase
base bucket is exhausted
Illustration 4:
Ms. PQR has opted for plan which has Cancer and blood disorders
bucket and add on Section B: Major Surgical Procedures. After the
initial waiting period she undergoes Pericardectomy. She is eligible
to claim for 50% payout under Major Surgical Procedures(Add on
Cover). Subsequently she has to undergo Amputation of Leg she
will be eligible to claim for 100% payout under Major Surgical
Procedure, however as we have already honoured a 50% claim on
Under Section B
4.1

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
account of Pericardiactomy now she will be eligible to claim for
balance 50% only. Hence we will be honouring 50% payout here
subject to policy terms and conditions
Section C: PERSONAL ACCIDENT(Add on)
Benefit 5: Accidental Death Benefit
Part III of Wordings
We will pay the specified Sum Insured in the manner specified in the
Policy Schedule, if an Insured Person suffers an Injury due to an
Accident that occurs during the Period of Cover and that Injury solely
and directly results in the Insured Person’s death within 365 days
from the date of the Accident. On the acceptance of a claim under
this Benefit and any other applicable Benefit pertaining to the same
event, all Benefit under this Policy shall immediately and
automatically cease in respect of that Insured Person and no
subsequent Renewals of the Policy will be allowed. Add on cover
will not be renewed incase base bucket is exhausted
Under Section C
5.1.1
Benefit 6: Permanent Total Disablement (PTD) Benefit:
Part III of Wordings
We will pay the Sum Insured specified against this Benefit in the
Policy Schedule in the manner specified in the Policy Schedule if an
Insured Person suffers an Injury due to an Accident that occurs
during the Period of Cover and that Injury solely and directly results
in the Permanent Total Disablement of the Insured Person within
365 days from the date of the Accident. Add on cover will not be
renewed incase base bucket is exhausted
Under Section C
5.1.2
Benefit 7 : Permanent Partial Disablement (PPD) Benefit:
Part III of Wordings
We will pay the percentage of the specified Sum Insured in the
manner specified in the policy wordings if an Insured Person suffers
an Injury due to an Accident that occurs during the Period of Cover
and that Injury solely and directly results in the Permanent Partial
Disablement of the Insured Person (which is of the nature specified
in the table below) within 365 days from the date of the Accident.
Add on cover will not be renewed incase base bucket is exhausted
Under Section C
5.1.3
Section D : Value Added Services
1. Tele-consultation:
We will arrange consultations and recommendations for any
listed Critical illnesses under Annexure 1 by a qualified General
Practitioner. For the purpose of this benefit Telephonic/Virtual
consultation shall mean consultation provided by a qualified
General Practitioner through various mode of communication
like audio, chat or mobile app. The services provided under this
Benefit will be made available subject to the terms and
conditions, and in the manner prescribed below:
The General Practitioner may suggest /recommend
/prescribe over the counter medications based on the
information provided, if required on a case to case basis.
However, the services under this Benefit should not be
construed to constitute medical advice and/or substitute the
Insured Person's visit/ consultation to an independent
Medical Practitioner/Healthcare professional*.
This service will be available 24 hours a day, and 365 days
in a year.
Part III of Wordings
Under Section D
6.1
ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
The General Practitioner may refer the Insured Person to a
specialist or a general physician, if required**, and the
charges for such specialist or a general physician will have
to be borne by the Insured Person.
We shall not be liable for any discrepancy in the information
provided under this Benefit.
Choosing the services under this Benefit is purely upon the
customer’s own discretion and at own risk.
You will be eligible to avail maximum of 4 tele-consultation
per policy period.
The insured will be able to use this service only with respect
to the listed Critical Illnesses under Annexure 1.
This benefit will lapse incase not used during the policy
tenure
*The proposer should seek assistance from a health care
professional when interpreting and applying them to the Insured
person’s individual circumstances. If the Insured person has any
concerns about His/ her health, He/ She may consult His/ her
general practitioner.
**Consultations charges would be applicable.
2. E-opinion (second opinion)
In the event of your diagnosis with any of the critical illness
covered under your policy and during the policy period, we shall
facilitate in arranging an E-Consultation second opinion from a
super specialty medical practitioner within our Network with
respect to that critical illness only, subject to the following
condition. It will be based on the medical records submitted by
the insured person which should include investigation reports
citing the final diagnosis and relevant consultation papers. We
will not be reimbursing/bearing the cost for E-
opinion/consultation (second opinion).
3. Health and Wellness Offers
Health and Wellness Offers on services/products provided
by our network providers/ Health service providers – We shall
only facilitate the Insured Person in availing offers and
discounts on services/products offered by our network providers/
health service providers. Customer can avail Health and
Wellness Offers on our app on various health, fitness and
wellness products and other services available on the app.
4. Health assistance:
We also provide Health Assistance as a part of Our Value added
services, Our Health Assistance Team (HAT) will assist the
Insured Person in understanding his/her health condition better
by providing answers to any queries related to health and health
care providers on Our dedicated helpline. To avail this service,
the Insured Person may call Our helpline on 040-66274205
(please note that this number is subject to change).
The services provided under this shall include:
Identifying a Physician/ Specialist
Scheduling an appointment with any Medical Practitioner
empanelled with Us
Scheduling appointments for a second opinion

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Providing suitable options with respect to Hospitals as well
as providing assistance in Cashless facility, wherever
applicable.
Providing preventive information on ailments
Providing guidance on post Hospitalization care, such as
Physiotherapy/ Nursing at home.
Please note that services provided under this Benefit are solely
for assistance, and should not be construed to be a substitute for
a visit/ consultation to an independent Medical Practitioner. This
Benefit does not include the charges for any independent
Medical Practitioner/nutritionist consulted on HAT’s
recommendation, and such charges are to be borne by the
Insured Person. We do not accept any liability towards quality of
the services made available by our network providers/ service
providers and are not liable for any defects or deficiencies on
their part
While deciding to obtain such value-added service, You
expressly note and agree that it is entirely for You to decide
whether to obtain these services and also to decide the use (if
any) to which these services is to be put for
3
What are the major
exclusions in the policy
Please refer to the policy wordings for the complete list.
We shall not be liable under this Policy for payment for any claim in
respect of an Insured person, caused by, arising from or in any way
attributable to any of the following:
Section A:
Benefit 1 : Comprehensive Critical Illness
Part III of Wordings
1. Any Critical Illness where the symptoms indicative of such
Critical Illness have first manifested or first occurred prior to the
Risk Inception Date or arisen within the waiting period of
90/120/150 days as specified in the Policy Schedule at
commencement of the Period of Cover.
2. Insured should survive for 0/3/7/14 days as mentioned in the
Policy Schedule from the date of diagnosis and fulfilment of the
critical illness definition(definitions mentioned in Annexure 1)
before the claim benefit will be paid.
3. Any Critical Illness arising on account of or in connection with
any Pre-Existing Disease(s).
4. Any Critical Illness or Surgery/Surgical Procedure arising out of
any external Congenital Anomaly or internal Congenital
Anomaly known at the commencement of the policy.
5. Any physical, medical or mental condition or treatment or service
that is specifically excluded in the Policy Schedule under the
head “Special Conditions”.
6. Any claim made without a medical certificate from the treating
Medical Practitioner evidencing the diagnosis of such Critical
Illness.
7. Any Critical Illness traceable to pregnancy, childbirth, abortion,
or related consequences.
Under Section A
1.2
Section A:
Benefit 2: ICU Benefit (Add on)
Part III of Wordings
1. Any ICU hospitalization where the appearance of first
(signs/symptom/diagnosis) of the infection or advice for surgery
was done during or prior to the initial waiting period of 90/120/150
days (as specified on the Policy Schedule) shall not be
considered payable under this Benefit.
2. We shall not consider any domiciliary/Home ICU care under this
Benefit.
Under Section A
2.3

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
3. We shall not consider ICU stay in an AYUSH hospital as payable
for this Benefit
4. Any Critical Illness or Surgery/Surgical Procedure arising out of
any external Congenital Anomaly or internal Congenital
Anomaly known at the commencement of the policy.
5. Any physical, medical or mental condition or treatment or service
that is specifically excluded in the Policy Schedule under the
head “Special Conditions”.
6. Any claim made without a medical certificate from the treating
Medical Practitioner mandating the stay in ICU.
7. Any claim traceable to pregnancy, childbirth, abortion, or related
consequences.
8. ICU admissions on account of Sterility/Infertility or any plastic
surgery for cosmetic purpose.
9. ICU admission due to any treatment necessitated due to
participation as a professional in hazardous or adventure sports,
including but not limited to, para-jumping, rock climbing,
mountaineering, rafting, motor racing, horse racing or scuba
diving, hand gliding, sky diving, deep-sea diving.
10. ICU admission directly arising from or consequent upon any
Insured Person committing or attempting to commit a breach of
law with criminal intent.
11. ICU admission on account of Alcoholism, drug or substance
abuse or any addictive condition and consequences thereof.
12. ICU admission on account of Intentional self-injury (whether
arising from an attempt to commit suicide or otherwise)
13. Any ICU admission arising from or attributed to war, invasion,
acts of foreign enemies, hostilities (whether war be declared or
not), civil war, commotion, unrest, rebellion, revolution, military
or usurped power or confiscation or nationalisation or requisition
of or damage by or under the order of any government or public
local authority
14. Any ICU admission caused by or contributed to by nuclear
weapons/materials or contributed to by or arising from ionising
radiation or contamination by radioactivity by any nuclear fuel or
from any nuclear waste or from the combustion of nuclear fuel
Section A:
Benefit 3: Cancer Restore Benefit (Add On)
Part III of Wordings
No claim shall be payable within the waiting period of 3 years
from the date of diagnosis of first Major Cancer.
In the event of death of the insured during the 3 years waiting
period, the claim shall not be payable.
Under Section A
3.2
Section B:
Benefit: 4: Major Surgical Procedures (Add On)
Part III of Wordings
1. Any covered Surgery/Surgical Procedure arising out of an
Illness diagnosed/contracted prior to Risk Inception Date or
arising within the waiting period of 90/120/150 days as specified
in policy schedule. However, no Waiting Period will be
applicable in case of any Surgical Procedure arising out of/due
to an Accident during the Period of Cover.
2. Any Surgery/Surgical Procedure arising out of an Accident
which occurred prior to Risk Inception Date.
3. Any Pre-Existing Disease(s) or any disability arising out of a Pre-
Existing Disease or any complication arising therefrom.
Under Section B
4.2

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
4. Any Critical Illness or Surgery/Surgical Procedure arising out of
any external Congenital Anomaly or internal Congenital
Anomaly known at the commencement of the policy.
5. Any of the covered Surgery/Surgical Procedure performed
which was otherwise deemed unnecessary, or against standard
health practices.
6. Any Unproven/Experimental treatment.
7. Any Surgery/Surgical Procedure performed solely due to
cosmetic or aesthetic reasons.
8. Any claim made without a medical certificate from the treating
Medical Practitioner evidencing the diagnosis of such Illness or
Injury or the undergoing of the medical / Surgical Procedure.
Section C: Personal Accident (Add On)
Benefit 5: Accidental Death Benefit
Part III of Wordings
Benefit 6: Permanent Total Disablement (PTD) Benefit:
Benefit 7 : Permanent Partial Disablement (PPD) Benefit:
1. War, invasion, act of foreign enemy hostilities or warlike
operations (whether war be declared or not) or civil commotion
or rebellion, revolution, insurrection, mutiny, arrests,
detainments of all kinds and political gatherings, engaging in
aviation other than as a passenger (fare paying or otherwise) in
any licensed standard type of aircraft.
2. Any Injury sustained while performing duty in army, navy, air
force, paramilitary force, police or any other such institution,
except to the extent it is expressly covered under any Benefit
3. Any event which occurs whilst the Insured Person is operating
or learning to operate any aircraft or common carrier, or
performing duties as a member of the crew on any aircraft, or
scheduled airlines or is engaging in aviation, or whilst the
Insured Person is mounting into, or dismounting from or
traveling in any balloon or aircraft other than as a passenger
(fare-paying or otherwise) in any scheduled airline anywhere in
the world.
4. Breach of law/ statutory provisions or while being involved in any
unlawful activity.
5. Any Injury / Illness arising from full-time involvement in
professional sports for livelihood and remuneration, except to
the extent it is expressly covered under any Benefit.
6. Any Injury / Illness arising from intentional self- Injury, suicide or
attempted suicide.
7. Any Injury / Illness arising from a failure to take reasonable
precautions to avoid a claim under the Policy.
8. Any Injury / Illness arising whilst under the influence of alcohol
or intoxicating drugs or substance abuse of any kind.
9. Any Injury / Illness occurring whilst working in underground
mines or explosives magazines, or involving electrical
installation with high tension supply, or as jockeys or circus
personnel or any other high risk occupations.
10. Any Injury that has occurred prior to the commencement of
Policy of Benefit whether or not the same has been treated, or
medical advice, diagnosis, care or treatment has been sought.
11. Any Illness, complication or ailment not arising out of or
connected to Injury.
12. Payment of compensation in respect of death, disablement
(whether of a permanent nature or of a temporary nature), Injury,
Illness or Hospitalization of the Insured Person resulting directly
from, or indirectly caused by, or contributed to or aggravated or
prolonged by, childbirth or pregnancy or in consequence thereof.
13. Payment of compensation in respect of death, disablement
(whether of a permanent nature or of a temporary nature), Injury,
Illness or Hospitalization of Insured Person due to an insect or
mosquito bite.
14. Death, disablement (whether of a permanent nature or of a
temporary nature), Injury, Illness or Hospitalization arising from
or caused by ionizing radiation or contamination by radioactivity
Under Section C
5.2

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
from any nuclear fuel (explosive or hazardous form) or resulting
from or from any other cause or event contributing concurrently
or in any other sequence to the loss, claim or expense from any
nuclear waste from the combustion of nuclear fuel, nuclear,
chemical or biological attack.
GENERAL EXCLUSIONS
Part IV of Wordings
1. Any physical, medical or mental condition or treatment or service
that is specifically excluded in the Policy Schedule under the
head “Special Conditions”.
2. Any breach of the law by the Insured Person with a criminal
intent.
3. War, invasion, act of foreign enemy, hostilities (whether war be
declared or not) civil war, rebellion, revolution, insurrection,
mutiny, military or usurped power, seizure, capture, arrests,
restraints and detainment of citizens of whatever nation, riots or
civil commotion.
4. Any Injury sustained while performing duty in army, navy, air
force, paramilitary force, police or any other such institution,
except to the extent it is expressly covered under any Benefit.
5. Ionising radiation or contamination by radioactivity from any
nuclear fuel or from any nuclear waste or from nuclear weapon
materials or from the combustion of nuclear fuel. For the purpose
of this exclusion, combustion shall include any self-sustaining
process of nuclear fission.
6. Use or misuse of intoxicating drugs and/or alcohol.
7. Participation (aggravation) in any kind of strike, processions,
riots etc.
8. Any act of self-destruction or self-inflicted injury, attempted
suicide or suicide and deliberate participation of the Insured in
an illegal or criminal act with criminal intent.
9. Any Injury / Illness occurring whilst working in underground
mines or explosives magazines, or involving electrical
installation with high tension supply, or as jockeys or circus
personnel
10. Any consequential or indirect losses or expenses related to any
Insured Event.
11. Any tests and treatment relating to infertility and in vitro
fertilization.
12. Any Injury / Illness occurring whilst engaging in any Adventure
Sports, either as an instructor/ trainer, or as a participant.
13. Any natural peril (including but not limited to storm, tempest,
avalanche, earthquake, volcanic eruptions, hurricane, or any
other kind of natural hazard).
4
Waiting Period
Following Waiting Periods shall be applicable under the Policy,
unless specified otherwise in the Policy Certificate.
Section A:
Benefit 1 – 90/120/150 Days
Benefit 2 – 90/120/150 Days
Benefit 3 – There is a 3 Year waiting period from the date of first
diagnosis of a major cancer
Section B:
Benefit 4 – 90/120/150 Days
Section C:
Benefit 5,6,7 – No Waiting Period
Part III of Wordings
Section A
Section B
Section C
& Policy Certificate
5
Payment Basis
We shall make payment of an admissible claim to the Insured
Person’s nominee/assignee, as the case may be, or in the
absence of an assignee, to the Insured Person or the Insured
Person’s nominee. If there is no assignee or Nominee and the
Insured Person is incapacitated or deceased, we will pay to the
Insured Person’s heir, executor or validly appointed legal
representative.
Part V of Wordings
“Specific Terms and
Conditions”
Clause No.1 “Payments”
ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Any payment we make in this manner will be a complete and
final discharge of our obligations under this Policy and Our
liability towards the claim.
6
Loss Sharing
NA
7
Renewal Conditions
1. The Policy may be renewed by mutual consent under the then
prevailing (ICICI Lombard Criti Shield Plus) Policy or its nearest
substitute product (in case of product withdrawal) approved by
the IRDAI, and in such event the Renewal premium should be
paid to Us on or before the date of expiry of the Policy and in no
case later than the Grace Period of 30 days from the expiry of
the Policy. We will not be liable to pay for any Claim arising out
of an Insured Event that occurs during the Grace Period.
2. Once the Sum Insured under any of the Benefits opted and
available to the insured is exhausted any future renewal under
that Benefit shall not be allowed.
3. You shall on tendering any premium for the Renewal of this
Policy give notice in writing to Us of any Illness, physical defect
or infirmity with which any of the Insured Person(s) have become
affected since the payment of the expiring Policy start date.
4. Renewals will not be denied except on grounds of
misrepresentation, moral hazard, fraud, non-disclosure of
material facts. We may, revise the Renewal premium payable
under the Policy or the terms of Benefit, provided that all such
changes are approved in accordance with the IRDAI rules and
regulations as applicable from time to time. We will intimate You
of any such changes at least 3 months prior to date of such
revision or modification.
5. We shall not be bound to give any notice to You/ Insured Person
that the premium for the Renewal is due.
6. Policyholder will not be allowed to make any changes in his/her
policy coverage’s, terms and conditions and Sum Insured at the
time of renewal in case a claim has already been settled
7. Policyholder will not be allowed to make any changes in his/her
policy coverage’s, terms and conditions at the time of renewal,
unless decided by Us on exceptional call or case to case basis
8. In the event where the base cover(s) has been exhausted the
insured shall not be allowed to renew the add on cover(s)
9. The above conditions for Renewal are to be read in unison, and
not standalone.
Part V of Wordings
“Specific Terms and
Conditions”
Clause No. 2 “Terms of
Renewal”
8
Renewal Benefits
No Waiting Periods shall be applicable in case of subsequent
Renewals, subject to no Break In Policy.
Part I of Wordings
“General Definitions”
Definition No. 23 “Waiting
Period”
9
Cancellation
1. The policyholder may cancel this policy by giving 15days'written
notice and in such an event, the Company shall refund premium
for the unexpired policy period as detailed below.
2. We shall from the date of receipt of the notice cancel the Policy,
retain the premium for the period this Policy has been in force,
and refund at Our short period scales as per the Refund Grid
provided below, provided that no refund of premium shall be
made if any claim has been made under the Policy by or on
behalf of the Insured Person.
3. Notwithstanding anything contained herein or otherwise, no
refunds of premium shall be made in respect of the Insured
Person where any Claim has been admitted by Us or has been
lodged with Us or any Benefit has been availed by the Insured
Person under the Policy.
4. In case of a cancellation request by You/ Insured Person, the
Policy will be cancelled in its entirety, and any selected Benefits
or Sections under the Policy cannot be cancelled.
5. The Company may cancel the policy at any time on grounds of
misrepresentation non-disclosure of material facts, fraud by the
Part V of Wordings
“General Terms and
Conditions”
Clause No. 6
“Cancellation/
Termination”

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
insured person by giving 15 days' written notice. There would be
no refund of premium on cancellation on grounds of
misrepresentation, non-disclosure of material facts or fraud.
6. For any cancellation initiated by Us, due to any other reason the
company may choose to refund the premium on pro-rata basis.
10
Claims
The Company shall settle or reject a claim, as the case may be,
within 30 days from the date of receipt of last necessary
document.
In the case of delay in the payment of a claim, the Company
shall be liable to pay interest to the policyholder from the date of
receipt of last necessary document to the date of payment of
claim at a rate 2% above the bank rate.
However, where the circumstances of a claim warrant an
investigation in the opinion of the Company, it shall initiate and
complete such investigation at the earliest, in any case not later
than 30 days from the date of receipt of last necessary
document- In such cases, the Company shall settle or reject the
claim within 45 days from the date of receipt of last necessary
document.
In case of delay beyond stipulated 45 days, the Company shall
be liable to pay interest to the policyholder at a rate 2% above
the bank rate from the date of receipt of last necessary
document to the date of payment of claim.
On occurrence of an any event that may give rise to a Claim
under this Policy, You shall-
Notify Us immediately on toll free number 1800 2666 or on our
website www.icicilombard.com or email us at
Along with the completed and signed Claim form, provide all the
relevant documents, specified within the relevant Section of the
Policy for the Benefit being claimed, must be submitted in full
within 30 days.
Wherever details pertaining to happening of Claim are conveyed
by you to Us after reasonable period, You shall provide the
reasons of such delay to Us.
Customer to send documents to Us at :- ICICI Lombard General
Insurance Company Limited ICICI Bank Tower, Plot No. 12,
Financial District, Nanakram Guda, Gachibowli, Hyderabad,
Andhra Pradesh- 500032
If any claim is not made within 30 days of the Insured Event,
then We will condone such delay on merits only where the delay
has been proved to be for reasons beyond the claimant’s control.
All claims will be investigated (as required) and settled in
accordance with the applicable regulatory guidelines, including
the IRDAI (Protection of Policyholders Interests) Regulations,
2017.
The admissible Claim amount will be calculated post
applicability of Deductible, Co-pay, Sub-limits, if any, and as
specifically defined in Policy Schedule.
The role of the TPA (if any) would be limited to facilitate the flow
of information between Us and the Insured Person.
Part V of Wordings
“Standard General Terms
and Clauses”
Clause No. 3 :Claim
Settlement”
&
“Specific Terms and
Conditions”
Clause No. 3 “Claim
Procedure”
11
Policy Servicing/
Grievances/Complaints
Call Us at toll free number: 1800 2666 or email us at
If You are not satisfied with the resolution then You may
successively write to Manager- Service Quality, Corporate
Manager- Service Quality, National Manager- Operations &
finally Director-services and Business development at the
following address:
ICICI Lombard General Insurance Company Limited,
ICICI Lombard House,
414, Veer Savarkar Marg,
Near Siddhi Vinayak Temple,
Prabhadevi, Mumbai 400025
Part V of Wordings
“General Terms and
Conditions”
Clause No. 15
“Redressal of
Grievances”

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
If the issue still remains unresolved, You may, subject to vested
jurisdiction, approach Insurance Ombudsman for the redressal
of the grievance.
Please refer to the policy wordings for the details of Insurance
Ombudsman.
12
Insured’s Rights
The insured person shall be allowed free look period of fifteen days
(30 days when policy is sourced through distance marketing) from
date of receipt of the policy document to review the terms and
conditions of the policy, and to return the same if not acceptable.
lf the insured has not made any claim during the Free Look
Period, the insured shall be entitled to
A refund of the premium paid less any expenses incurred by the
Company on medical examination of the insured person and the
stamp duty charges or
Where the risk has already commenced and the option of return
of the policy is exercised by the insured person, a deduction
towards the proportionate risk premium for period of cover or
Where only a part of the insurance coverage has commenced,
such proportionate premium commensurate with the insurance
coverage during such period
The Policy can be cancelled only if no claims have been made
under the Policy. All Your rights under this Policy will
immediately stand extinguished on the free look cancellation of
the Policy.
In case the request for cancellation comes 15 days after the
receipt of Policy by the Insured Person, We would refund the
premium paid as per the applicable refund grid provided in the
Cancellation clause of the Policy.
The Company shall settle or reject a claim, as the case may be,
within 30 days from the date of receipt of last necessary
document.
In the case of delay in the payment of a claim, the Company
shall be liable to pay interest to the policyholder from the date of
receipt of last necessary document to the date of payment of
claim at a rate 2% above the bank rate.
However, where the circumstances of a claim warrant an
investigation in the opinion of the Company, it shall initiate and
complete such investigation at the earliest, in any case not later
than 30 days from the date of receipt of last necessary
document- In such cases, the Company shall settle or reject the
claim within 45 days from the date of receipt of last necessary
document.
In case of delay beyond stipulated 45 days, the Company shall
be liable to pay interest to the policyholder at a rate 2% above
the bank rate from the date of receipt of last necessary
document to the date of payment of claim.
If any claim is not made within 30 days of the Insured Event,
then We will condone such delay on merits only where the delay
has been proved to be for reasons beyond the claimant’s control.
All claims will be investigated (as required) and settled in
accordance with the applicable regulatory guidelines, including
the IRDAI (Protection of Policyholders Interests) Regulations,
2017.
The admissible Claim amount will be calculated post
applicability of Deductible, Co-pay, Sub-limits, if any, and as
specifically defined in Policy Schedule.
Part V of Wordings
“General Terms and
Conditions”
&
Clause No. 14 “Free look
period”
“Standard General Terms
and Clauses”
Clause No. 3 :Claim
Settlement”
&
“Specific Terms and
Conditions”
Clause No. 3 “Claim
Procedure”
13
Insured’s Obligations
Please disclose all material information (Including Pre-existing
illnesses) before buying the Policy.
The Policy shall be null and void and no Benefit shall be payable
in the event of untrue or incorrect statements,
misrepresentation, mis-description or on non-disclosure in any
material particular in the proposal form, personal statement,
Part V of Wordings
“General Terms and
Conditions”
“Standard General Terms
and Clauses”

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
declaration and connected documents, or any material
information having been withheld.
Cooperation from the Insured/ Person claimant is solicited in
providing all or sufficient documents as per the claims procedure
in support of claim.
Clause No. 1 “Disclosure
of Information”

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Benefit Illustration in respect of policies offered individual basis or family floater basis
Age of
the
member
s insured
Coverage opted on
individual basis
covering each
member of the family
separately (at a single
point in time)
Coverage opted on individual basis covering
multiple members of the family under a single
policy (Sum insured is available for each member
of the family)
Coverage opted on family floater basis with
overall Sum insured (Only one sum insured
is available for the entire family)
Premium(
Rs)
Sum
Insured(
Rs)
Premium(
Rs)
Discount
if any
Premium(
After
Discount)(
Rs)
Sum
Insured(Rs
)
Premium
or
consolida
ted
premium
for all
members
of
family(Rs
)
Floate
r
disco
unt if
any
Premium
after
discount(
Rs)
Sum
Insured(
Rs)
3mon-
20yrs
214
5,00,000
214
11
204
5,00,000
NA
NA
NA
NA
21 - 25
yrs
254
5,00,000
254
13
241
5,00,000
NA
NA
NA
NA
26 - 30
yrs
299
5,00,000
299
15
284
5,00,000
NA
NA
NA
NA
31 - 35
yrs
452
5,00,000
452
23
429
5,00,000
NA
NA
NA
NA
36 - 40
yrs
1,112
5,00,000
1,112
56
1,056
5,00,000
NA
NA
NA
NA
41 - 45
yrs
2,105
5,00,000
2,105
105
2,000
5,00,000
NA
NA
NA
NA
46 - 50
yrs
3,572
5,00,000
3,572
179
3,394
5,00,000
NA
NA
NA
NA
51 - 55
yrs
6,174
5,00,000
6,174
309
5,866
5,00,000
NA
NA
NA
NA
56 - 60
yrs
9,566
5,00,000
9,566
478
9,088
5,00,000
NA
NA
NA
NA
61 - 65
yrs
12,552
5,00,000
12,552
628
11,924
5,00,000
NA
NA
NA
NA
>65 yrs*
14,431
5,00,000
14,431
722
13,710
5,00,000
NA
NA
NA
NA
Total Premium for all members of
the family is Rs. 965/-, when each
member is covered separately.
Sum Insured available for each
individual is 500000/-**
Total Premium for all members of the family is Rs.
917/-, when each member is covered separately.
Sum Insured available for each individual is
500000/-**
NA
Note: Premium rates specified in the above illustration are standard premium rates without considering any loading. The premium
rates are exclusive of taxes applicable
Plan considered above is Cancer Shield plan without any Add on cover for 1 year policy tenure has been opted. Waiting period
considered here is 90 days and 0 days Survival period
1. The above Illustration is considering primary applicant to be 35yrs of age, spouse 30yrs of age and child 10yrs of age. If they opt
for individual policies the total base premium would be 965/-. Incase Multi Life option is chosen 917/-.
2.**The above illustration is considering an equal Sum Insured for entire family, however the Sum Insured offered to spouse/child will
be as per the company's UW guidelines.
3. *Premium rates are for renewal only.
4. Please refer rate chart for more details

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
ICICI Lombard Criti Shield Plus
PREAMBLE
ICICI Lombard General Insurance Company Limited (“We / Us”),
having received a Proposal and the premium from the Proposer
named in Part I of the Policy (hereinafter referred to as the “Policy
Schedule”) and the said Proposal and Declaration together with
any statement, report or other document leading to the issue of
this Policy and referred to therein having been accepted and
agreed to by Us and the Proposer as the basis of this contract do,
by this Policy agree, in consideration of and subject to the due
receipt of the subsequent premiums, as set out in the Policy
Schedule, and further, subject to the terms and conditions
contained in this Policy that on proof to Our satisfaction of the
compensation having become payable as set out in the Policy
Schedule to the title of the said person or persons claiming
payment or upon the happening of an event upon which one or
more benefits become payable under this Policy, the Annual Sum
Insured / appropriate benefit amount will be paid by Us.
Part II of Schedule: Policy Wordings
I GENERAL DEFINTIONS
Standard Definitions
1. Accident: An accident means sudden, unforeseen and
involuntary event caused by external, visible and violent
means.
2. Any one illness: Any one illness means continuous period
of illness and includes relapse within 45 days from the date
of last consultation with the Hospital/Nursing Home where
treatment was taken.
3. AYUSH Hospital: An AYUSH Hospital is a healthcare
facility wherein medical/surgical/para-surgical treatment
procedures and interventions are carried out by AYUSH
Medical Practitioner(s) comprising of any of the following:
a. Central or State Government AYUSH Hospital; or
b. Teaching hospital attached to AYUSH College
recognized by the Central Government/Central Council
of Indian Medicine/Central Council for Homeopathy; or
c. AYUSH Hospital, standalone or co-located with in-patient
healthcare facility of any recognized system of medicine,
registered with the local authorities, wherever applicable,
and is under the supervision of a qualified registered
AYUSH Medical Practitioner and must comply with all the
following criterion:
i. Having at least 5 in-patient beds;
ii. Having qualified AYUSH Medical Practitioner in
charge round the clock;
iii. Having dedicated AYUSH therapy sections as
required and/or has equipped operation theatre
where surgical procedures are to be carried out;
iv. Maintaining daily records of the patients and making
them accessible to the insurance company’s
authorized representative.
4. Cashless facility: Cashless facility means a facility
extended by the insurer to the insured where the payments,
of the costs of treatment undergone by the insured in
accordance with the policy terms and conditions, are
directly made to the network provider by the insurer to the
extent pre-authorization is approved.
5. Condition Precedent: Condition Precedent means a policy
term or condition upon which the Insurer's liability under the
policy is conditional upon.
6. Congenital Anomaly: Congenital Anomaly means a
condition which is present since birth, and which is
abnormal with reference to form, structure or position.
a) Internal Congenital Anomaly Congenital anomaly which
is not in the visible and accessible parts of the body.
b) External Congenital Anomaly Congenital anomaly which
is in the visible and accessible parts of the body
7. Day Care Centre: A day care centre means any institution
established for day care treatment of illness and/or injuries
or a medical setup with a hospital and which has been
registered with the local authorities, wherever applicable,
and is under supervision of a registered and qualified
medical practitioner AND must comply with all minimum
criterion as under –
i) has qualified nursing staff under its employment;
ii) has qualified medical practitioner/s in charge;
iii) has fully equipped operation theatre of its own
where surgical procedures are carried out;
iv) maintains daily records of patients and will make
these accessible to the insurance company’s
authorized personnel.
8. Day Care Treatment: Day care treatment means medical
treatment, and/or surgical procedure which is:
i. undertaken under General or Local Anesthesia in
a hospital/day care centre in less than 24 hrs
because of technological advancement, and
ii. which would have otherwise required
hospitalization of more than 24 hours. Treatment
normally taken on an out-patient basis is not
included in the scope of this definition.
9. Disclosure to information norm: The policy shall be void and
all premium paid thereon shall be forfeited to the Company
in the event of misrepresentation, mis-description or non-
disclosure of any material fact.
10. Domiciliary Hospitalization: Domiciliary hospitalization
means medical treatment for an illness/disease/injury
which in the normal course would require care and
treatment at a hospital but is actually taken while confined
at home under any of the following circumstances:
i) the condition of the patient is such that he/she is
not in a condition to be removed to a hospital, or
ii) the patient takes treatment at home on account of
non-availability of room in a hospital.
11. Emergency Care: Emergency care means management for
an illness or injury which results in symptoms which occur

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
suddenly and unexpectedly, and requires immediate care
by a medical practitioner to prevent death or serious long
term impairment of the insured person’s health.
12. Grace Period: Grace period means the specified period of
time immediately following the premium due date during
which a payment can be made to renew or continue a policy
in force without loss of continuity Benefits such as waiting
periods and coverage of pre-existing diseases. coverage is
not available for the period for which no premium is
received.
13. Hospital: A hospital means any institution established for
in-patient care and day care treatment of illness and/or
injuries and which has been registered as a hospital with
the local authorities under Clinical Establishments
(Registration and Regulation) Act 2010 or under
enactments specified under the Schedule of Section 56(1)
of the said act Or complies with all minimum criteria as
under: i) has qualified nursing staff under its employment
round the clock; ii) has at least 10 in-patient beds in towns
having a population of less than 10,00,000 and at least 15
in-patient beds in all other places; iii) has qualified medical
practitioner(s) in charge round the clock; iv) has a fully
equipped operation theatre of its own where surgical
procedures are carried out; v) maintains daily records of
patients and makes these accessible to the insurance
company’s authorized personnel;
14. Hospitalization: Hospitalization means admission in a
Hospital for a minimum period of 24 consecutive ‘In-patient
Care’ hours except for specified procedures/ treatments,
where such admission could be for a period of less than 24
consecutive hours.
15. Illness: Illness means a sickness or a disease or
pathological condition leading to the impairment of normal
physiological function and requires medical treatment.
(a) Acute condition - Acute condition is a disease, illness or
injury that is likely to respond quickly to treatment which
aims to return the person to his or her state of health
immediately before suffering the disease/ illness/ injury
which leads to full recovery
(b) Chronic condition - A chronic condition is defined as a
disease, illness, or injury that has one or more of the
following characteristics:
1. it needs ongoing or long-term monitoring through
consultations, examinations, check- ups, and /or tests
2. it needs ongoing or long-term control or relief of
symptoms
3. it requires rehabilitation for the patient or for the patient
to be specially trained to cope with it
4. it continues indefinitely
5. it recurs or is likely to recur
16. Injury: Injury means accidental physical bodily harm
excluding illness or disease solely and directly caused by
external, violent, visible and evident means which is verified
and certified by a Medical Practitioner.
17. Inpatient Care: Inpatient care means treatment for which
the insured person has to stay in a hospital for more than
24 hours for a covered event.
18. Intensive Care Unit: Intensive care unit means an identified
section, ward or wing of a hospital which is under the
constant supervision of a dedicated medical practitioner(s),
and which is specially equipped for the continuous
monitoring and treatment of patients who are in a critical
condition, or require life support facilities and where the
level of care and supervision is considerably more
sophisticated and intensive than in the ordinary and other
wards.
19. ICU Charges: ICU (Intensive Care Unit) Charges means
the amount charged by a Hospital towards ICU expenses
which shall include the expenses for ICU bed, general
medical support services provided to any ICU patient
including monitoring devices, critical care nursing and
intensivist charges.
20. Medical Advice: Medical Advice means any consultation or
advice from a Medical Practitioner including the issuance
of any prescription or follow-up prescription.
21. Medical Expenses: Medical Expenses means those
expenses that an Insured Person has necessarily and
actually incurred for medical treatment on account of Illness
or Accident on the advice of a Medical Practitioner, as long
as these are no more than would have been payable if the
Insured Person had not been insured and no more than
other hospitals or doctors in the same locality would have
charged for the same medical treatment.
22. Medical Practitioner: Medical Practitioner means a person
who holds a valid registration from the Medical Council of
any State or Medical Council of India or Council for Indian
Medicine or for Homeopathy set up by the Government of
India or a State Government and is thereby entitled to
practice medicine within its jurisdiction; and is acting within
its scope and jurisdiction of license. The registered
practitioner should not be the insured or close member of
the family.
23. Medically Necessary Treatment: Medically necessary
treatment means any treatment, tests, medication, or stay
in hospital or part of a stay in hospital which:
i) is required for the medical management of the
illness or injury suffered by the insured;
ii) must not exceed the level of care necessary to
provide safe, adequate and appropriate medical
care in scope, duration, or intensity;
iii) must have been prescribed by a medical
practitioner;
iv) must conform to the professional standards widely
accepted in international medical practice or by
the medical community in India.
24. Migration: Migration means, the right accorded to individual
health insurance policyholders (including all member under
family cover and members of group health insurance

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
policy), to transfer the credit gained for pre-existing
conditions and time bound exclusions, with same insurer.
25. Network Provider: Network Provider means hospitals or
health care providers enlisted by an insurer, TPA or jointly
by an Insurer and TPA to provide medical services to an
insured by a cashless facility.
26. New Born Baby: Newborn baby means baby born during
the Policy Period and is aged upto90 days.
27. Non- Network Provider: Non-Network means any hospital,
day care centre or other provider that is not part of the
network.
28. Notification of Claim: Notification of claim means the
process of intimating a claim to the insurer or TPA through
any of the recognized modes of communication.
29. OPD treatment: OPD treatment means the one in which the
Insured visits a clinic / hospital or associated facility like a
consultation room for diagnosis and treatment based on the
advice of a Medical Practitioner. The Insured is not
admitted as a day care or in-patient.
30. Portability: Portability means, the right accorded to
individual health insurance policyholders (including all
member under family cover), to transfer the credit gained
for pre-existing conditions and time bound exclusions, from
one insurer to another insurer.
31. Post-hospitalization Medical Expenses means medical
expenses incurred during predefined number of days
immediately after the insured person is discharged from the
hospital provided that: i. Such Medical Expenses are for the
same condition for which the insured person’s
hospitalization was required, and ii. The inpatient
hospitalization claim for such hospitalization is admissible
by the insurance company.
32. Pre-Existing Disease: Pre-existing Disease means any
condition, ailment, injury or disease:
a) That is/are diagnosed by a physician within 48 months
prior to the effective date of the policy issued by the insurer
or
b) For which medical advice or treatment was
recommended by, or received from, a physician within 48
months prior to the effective date of the policy or its
reinstatement.
33. Pre-hospitalization Medical Expenses Pre-hospitalization
Medical Expenses means medical expenses incurred
during pre-defined number of days preceding the
hospitalization of the Insured Person, provided that:
i. Such Medical Expenses are incurred for the
same condition for which the Insured Person’s
Hospitalization was required, and
ii. The In-patient Hospitalization claim for such
Hospitalization is admissible by the Insurance
Company.
34. Qualified Nurse: Qualified nurse means a person who holds
a valid registration from the Nursing Council of India or the
Nursing Council of any state in India.
35. Reasonable and Customary Charges: Reasonable and
Customary charges means the charges for services or
supplies, which are the standard charges for the specific
provider and consistent with the prevailing charges in the
geographical area for identical or similar services, taking
into account the nature of the illness / injury involved.
36. Renewal: Renewal means the terms on which the contract
of insurance can be renewed on mutual consent with a
provision of grace period for treating the renewal
continuous for the purpose of gaining credit for pre-existing
diseases, time-bound exclusions and for all waiting periods.
37. Room Rent: Room Rent means the amount charged by a
Hospital towards Room and Boarding expenses and shall
include the associated medical expenses.
38. Surgery or Surgical Procedure: Surgery or Surgical
Procedure means manual and / or operative procedure (s)
required for treatment of an illness or injury, correction of
deformities and defects, diagnosis and cure of diseases,
relief from suffering and prolongation of life, performed in a
hospital or day care centre by a medical practitioner.
39. Unproven/Experimental treatment: Unproven/Experimental
treatment means the treatment including drug experimental
therapy which is not based on established medical practice
in India, is treatment experimental or unproven
Specific Definitions:
1. Admission means admission of the Insured Person in a
Hospital as an in-patient for the purpose of medical
treatment of an Injury and/or Illness, for a minimum duration
of 24 hours.
2. Adventure Sport means sports/activities including but not
limited to Sky Diving, Bungee Jumping, Bungee swoop,
Bungee slingshot, Dune sliding, Hot air ballooning, Bridge
Swinging, Zip Lining, Zip Trekking, Rock Climbing, Bicycle
Polo, Bamboo rafting, Rock Scrambling, Rappelling, Via
Ferrata, Fell Running, Fell Walking, Gorge Walking, Indoor
Rock Climbing, Mountain Biking, Mountaineering, Body
Boarding, Sailing, Ski boarding, Scuba Diving, Snorkeling,
Shark Diving, Sky Diving, Swimming with Dolphins, Banana
boating/donuts/inflatable’s behind power boat Diving with
Whales, Wakeboarding, Surfing, Auto (car) racing, Motor
rallying, Motorcycle racing, Air racing, Kart racing, Boat
racing, Hovercraft racing, Lawn mower racing, Snowmobile
racing, Zorbing, and Truck racing.
3. Age means the completed years of the Insured Person on
his/her last birthday as per the English calendar as on the
Risk Inception Date.
4. Break In Policy means the period that occurs at the end of
the existing policy term, when the premium due for
Renewal on a given Policy is not paid on or before the

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
premium Renewal date, or within 30 days thereof. In case
of Premium collected on Installment basis the grace period
is 7 days.
5. Common Carrier shall mean to include any commercial
public airline, railway, bus, or water borne vessel carrying
fare paying passengers and licensed by the appropriate
authority for transportation of passengers
6. Family means, the Family that consists of the proposer and
any one or more of the family members as mentioned
below:
i. Legally wedded spouse.
ii. Dependent Children (i.e. natural or legally adopted)
between 3months of age to 25 years. If the child above 18
years of age is financially independent, he or she shall be
ineligible for coverage.
7. Financial Institution shall have the same meaning assigned
to the term under Section 45-I of the Reserve Bank of India
Act, 1934, and shall include a Non-Banking Financial
Company as defined under Section 45-I of the Reserve
Bank of India Act, 1934.
8. First Diagnosis shall mean the point in time at which the
requirements of any Critical Illness under this Policy were
first satisfied with respect to the Insured Person, including
the availability of the test reports and medical reports
evidencing such diagnosis and confirmed by a medical
practitioner
9. Infection: means an invasion of human body by pathogenic
microorganisms including bacteria, viruses, parasites and
fungi.
10. Income means and includes the amount that the Insured
Person earns each month from his/her Primary Occupation.
For Salaried Individuals, this would mean salary including
regular bonuses, regular commissions, superannuation
contributions or any other allowances, any Benefits
explicitly mentioned in CTC (Cost to Company) or any
compensation structure provided to the Insured Person by
his/her employer for the financial year, or as declared in the
previous ITR (Income Tax Return) filed by the Insured
Person. For self-employed individuals having an ownership
in a business, or operating as a sole trader or under a
partnership, company or trust, Income will be considered
as the gross annual income (before tax) filed before the
relevant tax authorities in the previous assessment year.
11. Insured Event means any event or occurrence specifically
mentioned as covered under this Policy for which
applicable premium has been received by Us.
12. Insured Person means the individual(s) whose name(s) are
specifically appearing under the heading “Insured name” in
the Policy Schedule to the Policy, and for whom the Insured
Events are covered in lieu of the applicable premium
received by Us under the Policy.
13. Loan means the sum of money lent at interest or otherwise
to the Insured Person by any Financial Institution, as
identified by a Loan Account Number. .
14. Nominee means the person(s) nominated by the Insured
Person to receive the applicable Benefits under this Policy
payable in the event of death of the Insured Person caused
by any Critical Illness or Surgical Procedure defined and
specified under the Policy. For the purpose of avoidance of
doubt it is clarified that if the Nominee is a minor, the legal
guardian appointed by the Insured Person will take care of
any relevant proceedings.
15. Permanent Total Disablement means any of the following:
i. Total and irrevocable loss of sight in both eyes, and
ii. Total and irrevocable physical separation of two entire
hands or two entire feet, or
iii. Total and irrevocable loss of one entire hand and one
entire foot, or
iv. Total and irrevocable loss of sight of one eye and
physical separation of one entire hand or physical
separation of one entire foot, or Total and irrevocable loss
of use of two hands or two feet, or
v. Total and irrevocable loss of use of one hand and one
foot, or
vi. Total and irrevocable of loss of sight of one eye and
loss of use of one hand or one foot. For the purpose of this
definition:
i. Physical separation of a hand or foot means separation
of the hand at or above the wrist, and of the foot at or
above the ankle.
ii. Loss of use or Loss of sight means total paralysis of
one or more limb, or loss of vision respectively, which is
certified in writing by a Medical Practitioner to be
permanent, complete and irreversible and substantiated
by physical examination and investigation to be
permanent, complete and irreversible.
16. Policy Period means the period commencing from the
Policy Start Date and ending at the Policy End Date as
specifically appearing in the Policy Schedule, inclusive of
both dates. It is the duration in which the policy is valid and
the Insured Person is liable to get a claim subject to any
applicable waiting Periods and the terms and conditions
under this Policy.
17. Public Authority means any governmental or quasi-
governmental organization, statutory body, or duly
authorized organization which exercises autonomous
authority in a regulatory or supervisory capacity.
18. Risk Inception Date means the date of commencement of
the Period of cover, as specified in the Policy Schedule for
the Insured Person.
19. Salaried Individuals means those Insured Persons who
work as an employee or a worker, with government or
private organization, whether confirmed or on probation as
on the Risk Inception Date, and earn a fixed amount of
compensation at a fixed frequency as salary.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
20. Sum Insured means the amount specified in the Policy
Schedule against a Benefit or set of Benefits that
represents Our maximum, total and cumulative liability for
any and all claims made in respect of that Insured Person
during the Period of cover under that Benefit/set of
Benefits.
21. Surgeon means a specialist Medical Practitioner who is
fully qualified as per applicable law to practice
Surgery/carry out Surgical Procedures in India.
22. Survival period- refers to the period from the diagnosis and
fulfilment of the critical illness definition which the life
assured or Insured Person must survive before the claim
benefit will be paid
23. Waiting Period means a time-bound exclusion period
related to condition(s) specified in the Policy Schedule
which shall be served before a claim related to such
condition becomes admissible. No Waiting Periods shall be
applicable in case of subsequent Renewals, subject to no
Break In Policy.
24. We/Our/Ours/Us/ Company means the ICICI Lombard
General Insurance Company Limited.
25. You/Your/Yours/Yourself means the person or the entity
named as the policyholder in the Policy Schedule and who
is responsible for payment of premium.
II. SCOPE OF COVER:
This Policy is a contract of insurance between the Policyholder
and Us which is subject to the receipt of premium against each
Benefit in full (or first instalment, where the Premium payment in
Instalment Clause is opted) in respect of the Insured Persons, and
the terms, conditions and exclusions of this Policy.
The Policy Schedule will specify which of the following Benefits
and Endorsements are applicable and in force for the Insured
Person. Claims made in respect of an Insured Person for any
Benefit applicable to the Insured Person shall be subject to the
occurrence of the Insured Event during the Period of cover,
availability of the Sum Insured specified against the Benefit
claimed, applicable sublimits for such Benefit as may be specified
in the Policy Schedule and the terms, conditions and exclusions
of this Policy.
All claims shall be made in accordance with the procedures set
out in this Policy. The coverage under each Benefit terminates in
relation to an Insured Person(s) in the event of one or more
claim(s) in respect of that Insured Person becoming admissible
and accepted by Us to the extent of the Sum Insured specified
against each Benefit in the Policy Schedule. Admitted claims will
be payable to the Insured Person or the Nominee (as applicable).
III Benefits under Product
Section A: Critical Illness
1.1 Base Cover: Benefit 1: Comprehensive Critical Illness
This Benefit has been bucketed under 5 Critical Illness buckets.
Each Bucket has further been divided into major and minor Critical
Illness. If an Insured Person(s) is First Diagnosed with any of the
Critical Illnesses from the bucket, based on the categorization We
will pay the Sum Insured specified in the Policy Schedule against
that bucket in the manner as described below.
In the event of any minor illness listed in Annexure 1 the company
shall pay 25% of the Sum Insured subject to a maximum of 12.50lac,
as specified in the Policy Schedule against that bucket. In the event
of any major critical illness listed in Annexure 1 the company shall
pay 100 % of the Sum Insured specified in the Policy Schedule
against that bucket. In any scenario if a major illness is followed by
a minor illness from the same bucket the company shall only pay
the remaining 75% of the sum insured as specified against that
bucket in the Policy Schedule .
The company shall only allow an insured to make one major critical
illness claim and one minor Critical Illness claim from each of the
buckets opted upto the exhaustion of the sum insured against that
bucket.
Once the sum Insured has been exhausted against a bucket, it will
cease and the policyholder shall not be allowed to renew that bucket
in any subsequent renewals and only the remaining buckets if not
exhausted up to their respective Sum Insured can be renewed in
subsequent renewals
The policy holder cannot opt for any new bucket at the time of
renewal
The Insured can claim independently from each of the critical illness
bucket opted and specified in the Policy Schedule upto the Sum
Insured specified against each of these buckets in the Policy
Schedule subject to due receipt of premium(or premium instalment,
incase premium payment in instalment clause is opted) as the case
may be.
The list of minor and major conditions under each bucket and their
definitions have been stated in Annexure 1 of these wordings
Note:
The maximum payout against any minor Critical Illness under
any Critical illness bucket is restricted to 25% of the base cover
Sum Insured upto a maximum of 12.5lacs however for “Cardiac
Arrhythmia with surgical intervention” and “Angioplasty ” the
Sum Insured is further restricted to a maximum of 5lac
Illustration 1
Insured can opt for any of the Critical Illness bucket as per plans
available at inception. The SI payable will be independent for each
bucket if more than one bucket is selected.
e.g At policy inception if Mr. XYZ opts for all buckets-Cancer
and blood disorders, Heart and Blood Vessel, Major Organs,
Nervous System, Other Illness he can intimate a claim under
all these buckets independently/simultaneously.
Incase Mr. XYZ is diagnosed with Stroke resulting in
permanent symptoms (Nervous System -Major) in 5
th
month, if the claim is payable as per policy Terms and
Conditions we will pay 100% of SI allocated for Nervous
System bucket.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
The Nervous System bucket will be exhausted and no
renewal of this bucket will be allowed to the customer.
In the 7th month Mr. XYZ is diagnosed with Pulmonary
embolism (Heart and Blood Vessel -Minor)he can claim
for 25% of SI from Heart and Blood Vessel bucket.
Incase Mr. XYZ consequently suffers from a
Myocardial Infarction (Heart and Blood Vessel -Major)
we will pay balance 75% (since we have already paid
minor claim of 25% under this bucket) once this claim
has been paid the Heart and Blood Vessel bucket will
be exhausted and no subsequent renewal will be done
for this bucket.
Illustration 2:
Mr. PQR a 33yr old has opted for plan which has Heart and Blood
Vessel bucket for 1 year Policy Tenure and 3lac SI for a base
premium of 270/- . After the waiting period of the policy is over Mr.
PQR is diagnosed with Other Serious Coronary Artery Diseases
in the 5
th
month.
He is eligible to claim for 25% SI which is 75000/-. Now only 75%
of the SI is remaining in Heart and Blood Vessel bucket.
At the time of renewal, we will be collecting the premium as per
the original 100% of SI however our liability will be only towards
the balance Sum Insured which is 75% of SI(in this example
225000).
1.2 Exclusions applicable to Section A: Benefit 1:
We shall not be liable to make any payment for any claim under
Benefit 1 of Section A of this Policy in respect of an Insured
Person, directly or indirectly for, caused by, arising from or in any
way attributable to any of the following:
a) Any Critical Illness where the symptoms indicative of
such Critical Illness have first manifested or first
occurred prior to the Risk Inception Date or arisen within
the waiting period of 90/120/150 days as specified in the
Policy Schedule at commencement of the Period of
Cover.
b) Insured should survive for 0/3/ 7/14 days as mentioned
in the Policy Schedule from the date of diagnosis and
fulfilment of the critical illness definition (definitions
mentioned in Annexure 1) before the claim benefit will
be paid.
c) Any Critical Illness arising on account of or in connection
with any Pre-Existing Disease(s).
d) Any Critical Illness or Surgery/Surgical Procedure
arising out of any external Congenital Anomaly or
internal Congenital Anomaly known at the
commencement of the policy.
e) Any physical, medical or mental condition or treatment
or service that is specifically excluded in the Policy
Schedule under the head “Special Conditions”.
f) Any claim made without a medical certificate from the
treating Medical Practitioner evidencing the diagnosis of
such Critical Illness.
g) Any Critical Illness traceable to pregnancy, childbirth,
abortion, or related consequences.
1.3 Claim Documents for Section A: Benefit 1:
On the occurrence of an Insured Event which may give rise
to a claim under this Benefit, We shall be provided with the
necessary and mandatory information specified in A:
Common documents required for all claims under this Benefit
for all claims, within 30 days of occurrence of the Insured
Event:
A: Common documents required for all claims under
this Benefit:
1.
Claim Form duly filled and signed by Insured
Person/Nominee/claimant
2.
EMS Paper
3.
Discharge Card/Summary papers
4.
Indoor Case papers
5.
Hospital Bills
6.
All Investigation Reports – blood, pathology, radiology, etc.
7.
Certificate by treating Medical Practitioner confirming
diagnosis
8.
Current and past consultation papers
9.
Certificate of Medical Cause of Death issued by last
attending Medical Practitioner (wherever applicable)
10.
Certificate from last attending Medical Practitioner /medical
authority for underlying medical condition/s leading to death
of the Insured Person
11.
Post Mortem Report, FSL Report, Viscera and Chemical
Analysis Report, Histopathoilogy Report (wherever
applicable)
12.
Any other specific investigation / document to support the
diagnosis of such Critical Illness, as may be reasonably
required by Us in addition to the documents specified under
this Section.
13.
Income Proof(ITR/Salary Slip,etc)
The Company shall seek for specific investigation reports
depending on the nature of ailment. The list of the specific
requirements will be shared with the insured/ nominee at the time
of claim
2.1 Add on cover: Benefit 2: ICU Benefit
In the event of a hospital admission if an insured is admitted in ICU
on account of any surgery or infection for a minimum of 5 or 7 days
as specified in Policy Schedule the company shall pay the Sum
Insured as specified against this Benefit on the Policy Schedule in
consideration of payment of additional premium
The surgery or infection and the stay in the ICU must be directly
due to the same cause and confirmed as necessary medical
treatment.
2.2 Terms and conditions applicable to Benefit 2
This Benefit is paid only once during the entire Policy
Period.
Once a claim has been paid under this Benefit the Benefit
shall stand terminated and no subsequent renewals of
this Benefit will be allowed.
This Benefit shall be paid as a lump sum to the extent of
Sum Insured specified in the Policy Schedule against this
Benefit.
This Benefit shall not reimburse any expenses incurred
during the stay of the insured in the hospital(ICU) or any

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
expenses incurred prior or post hospitalization/ICU stay.
We shall be liable to only pay the Sum Insured
irrespective of the expenses incurred during the stay in
the hospital.
The 5 or 7 day stay in ICU(as specified in policy schedule)
should form part of single hospitalization stay relating to
insured peril.
For ICU benefit cover: No Waiting Period will be
applicable in case of ICU stay on account of any
Surgery/infection arising out of/due to an Accident during
the Period of Cover.
The surgery or infection and the stay in the ICU must be
directly due to the same cause and confirmed as
necessary medical treatment.
We will not consider a stay in ICU as necessary medical
treatment if the insured can be safely and adequately
treated in any other facility.
This Benefit shall be payable subject to providing proof of
Surgery or Infection to the satisfaction of the Company.
All Procedures claimed should be confirmed as Medically
Necessary, by a qualified Physician or Surgeon, to the
satisfaction of the Company.
The Stay in an ICU shall only be considered subject to
the definition of ICU being met as defined above in the
Policy Wordings and subject to the satisfaction of the
Company.
In the event of death in ICU the claim shall be considered
payable subject to the insured having survived for
minimum 3 days of continuous stay in ICU
In the event where the base cover(s) has been exhausted
the insured shall not be allowed to renew the add on
cover(s)
2.3 Exclusions applicable to Section A: Benefit 2:
a) Any ICU hospitalization where the appearance of first
(signs/symptom/diagnosis) of the infection or advice for
surgery was done during or prior to the initial waiting
period of 90/120/150 days (as specified on the Policy
Schedule) shall not be considered payable under this
Benefit.
b) We shall not consider any domiciliary/Home ICU care
under this Benefit.
c) We shall not consider ICU stay in an AYUSH hospital as
payable for this Benefit
d) Any Critical Illness or Surgery/Surgical Procedure
arising out of any external Congenital Anomaly or
internal Congenital Anomaly known at the
commencement of the policy.
e) Any physical, medical or mental condition or treatment
or service that is specifically excluded in the Policy
Schedule under the head “Special Conditions”.
f) Any claim made without a medical certificate from the
treating Medical Practitioner mandating the stay in ICU.
g) Any claim traceable to pregnancy, childbirth, abortion, or
related consequences.
h) ICU admissions on account of Sterility/Infertility or any
plastic surgery for cosmetic purpose.
i) ICU admission due to any treatment necessitated due to
participation as a professional in hazardous or adventure
sports, including but not limited to, para-jumping, rock
climbing, mountaineering, rafting, motor racing, horse
racing or scuba diving, hand gliding, sky diving, deep-
sea diving.
j) ICU admission directly arising from or consequent upon
any Insured Person committing or attempting to commit
a breach of law with criminal intent.
k) ICU admission on account of Alcoholism, drug or
substance abuse or any addictive condition and
consequences thereof.
l) ICU admission on account of Intentional self-injury
(whether arising from an attempt to commit suicide or
otherwise)
m) Any ICU admission arising from or attributed to war,
invasion, acts of foreign enemies, hostilities (whether
war be declared or not), civil war, commotion, unrest,
rebellion, revolution, military or usurped power or
confiscation or nationalisation or requisition of or
damage by or under the order of any government or
public local authority
n) Any ICU admission caused by or contributed to by
nuclear weapons/materials or contributed to by or arising
from ionising radiation or contamination by radioactivity
by any nuclear fuel or from any nuclear waste or from
the combustion of nuclear fuel
2.4 Claim Documents for Section A: Benefit 2:
Documents required for claims under this Benefit:
1.
Claim Form duly filled and signed by Insured
Person/Nominee/claimant
2.
EMS Paper
3.
Discharge Card/Summary papers
4.
Indoor Case papers
5.
Hospital Bills
6.
All Investigation Reports – blood, pathology, radiology, etc.
7.
Certificate by treating Medical Practitioner confirming
diagnosis
8.
Current and past consultation papers
9.
Certificate of Medical Cause of Death issued by last
attending Medical Practitioner (wherever applicable)
10.
Certificate from last attending Medical Practitioner /medical
authority for underlying medical condition/s leading to death
of the Insured Person
11.
Post Mortem Report, FSL Report, Viscera and Chemical
Analysis Report, Histopathoilogy Report (wherever
applicable)
12.
Any other specific investigation / document to support the
diagnosis of such Critical Illness, as may be reasonably
required by Us in addition to the documents specified under
this Section.
13.
ICU admission papers
14.
Proof for advice on ICU admission by Medical practitioner
15.
Income Proof(ITR/Salary Slip,etc)

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
The Company shall seek for specific investigation reports
depending on the nature of ailment. The list of the specific
requirements will be shared with the insured/ nominee at the time
of claim
3.1 Add on cover: Benefit 3: Cancer Restore Benefit
In consideration of payment of additional premium this cover pays
the sum insured specified against this Benefit on account of a re
diagnosed or recurred major cancer once a Major cancer (Cancer
of Specified Severity) claim has already been considered and paid
under this policy. A Waiting period of 3 years will be applicable
from the date of diagnosis of the first Major Cancer (Cancer of
Specified Severity) claim admitted under this policy.
The insured can claim under this Benefit only if he has opted for
this Benefit 3 along with the Cancer Bucket under Benefit 1 at the
time of first purchase of this policy subject to due receipt of
premium by the company.
This Benefit 3 cannot be opted at the time of renewal or during
the policy period
“Re-diagnosed Major Cancer” (Cancer of Specified Severity)
means cancer for which any of the following conditions are met
after the stipulated waiting period of 3 years from the date of
diagnosis of the last Major Cancer(Cancer of Specified Severity)
claim admitted under this policy.
The Major Cancer(Cancer of Specified Severity)
persists since first diagnosis;
The Major Cancer(Cancer of Specified Severity)
relapses, that is, though recovered temporarily (in
remission), the same Major Cancer(Cancer of Specified
Severity) recurs at the same organ as the preceding
Major Cancer(Cancer of Specified Severity);
Metastasis of the preceding Major Cancer (Cancer of
Specified Severity) to other parts of the body; or
The new Major Cancer (Cancer of Specified Severity) is
unrelated to the preceding Major Cancer(Cancer of
Specified Severity).
Re-diagnosed Major Cancer(Cancer of Specified Severity) must
be confirmed by an oncologist on the basis of histopathological
diagnosis. Clinical re-diagnosis of Cancer can only be adopted if
histopathological diagnosis is medically not possible; in which
case, the Insured must have medical documentary proof or record
from a certificated oncologist of ongoing cancer therapy (including
but not limited to radiotherapy or chemotherapy or surgery).
Ongoing preventive cancer therapy (including but not limited to
Tamoxifen or Raloxifene) will not be accepted as a basis of clinical
re-diagnosis.
The date of diagnosis of Re-diagnosed Major Cancer (Cancer of
Specified Severity) refers to the date of the histopathological
report.
If histopathological diagnosis is medically not possible; the date
of diagnosis of Re-diagnosed Major Cancer(Cancer of Specified
Severity) refers to the date of documentary proof or record from
a certificated oncologist of ongoing cancer therapy (including but
not limited to radiotherapy or chemotherapy or surgery).
The rediagnosed cancer must meet the definition of “Cancer of
specified severity” as stated in the policy wordings
This feature is only applicable only once during the entire policy
period Once the Cancer restore Benefit feature has been utilised
and exhausted, this Benefit terminates and no subsequent
renewal of Cancer Bucket under Benefit 1 and of this Benefit 3
will be allowed
3.2 Exclusions applicable to Section A: Benefit 3:
a) No claim shall be payable within the waiting period of 3
years from the date of diagnosis of first Major
Cancer(Cancer of Specified Severity).
b) In the event of death of the insured during the 3 years
waiting period the claim shall not be payable.
3.3 Claim Documents for Section A: Benefit 3:
Claim Form duly filled and signed by Insured
Person/Nominee/claimant
EMS Paper
Discharge Card/Summary papers
Indoor Case papers
Hospital Bills
All Investigation Reports – blood, pathology, radiology, etc.
Certificate by treating Medical Practitioner confirming diagnosis
Current and past consultation papers
Certificate of Medical Cause of Death issued by last attending
Medical Practitioner (wherever applicable)
Certificate from last attending Medical Practitioner /medical
authority for underlying medical condition/s leading to death of
the Insured Person
Post Mortem Report, FSL Report, Viscera and Chemical
Analysis Report, Histopathoilogy Report (wherever applicable)
Any other specific investigation / document to support the
diagnosis of such Critical Illness, as may be reasonably
required by Us in addition to the documents specified under
this Section.
All histology/cytology/FNAC/Biopsy/Immuno-chemistry
reports, X-ray, CT Scan, MRI, PET Scan, Bone Marrow Test,
Cancer Markers, all other pathological tests

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Income Proof(ITR/Salary Slip,etc)
The Company shall seek for specific investigation reports
depending on the nature of ailment. The list of the specific
requirements will be shared with the insured/ nominee at the time
of claim
Illustration 3:
Mr. RST a 40yr old male has opted for plan which has ‘Cancer
and blood disorders’ bucket and add on ‘Cancer Restore Benefit’
for 1 year tenure for 5lac SI with base premium as 970/- & 340/-
for ‘Cancer and blood disorders Bucket’ and ‘Cancer Restore
Cover’ respectively. After the initial waiting period Mr. RST is
diagnosed with Major Cancer (Cancer of Specified severity),after
evaluation of required documents we pay the major claim with
100% payout of 5 lac sum insured. Since the customer has opted
for cancer restore benefit he will be eligible to claim under this
benefit provided the customer renews this policy subject to having
received the premium for the ‘Cancer and blood disorders’ bucket
under benefit 1 and cancer restore benefit as per the original Sum
Insured and age at the time of renewal. Mr. RST is diagnosed
with Cancer relapse after the 3 years waiting period he will be
eligible to claim for ‘Cancer Restore’ Benefit.
4.1 Section B: Add on cover : Benefit: 4: Major Surgical
Procedures
In consideration of payment of additional premium if the Insured
Person is Hospitalized on the written advice of the treating
Medical Practitioner due to an Illness contracted or any Injury
sustained during the Period of Cover, and is advised by a Medical
Practitioner qualified as a Surgeon to undergo a Surgical
Procedure specified in Annexure 2 of this Policy and has
undergone the surgery, then We will pay the percentage of the
Sum Insured as a lumpsum (specified against this Benefit in the
Policy Schedule) in the manner specified in the Annexure 2 for
each of the listed surgeries.
This Benefit shall be payable subject to the following:
1. We will consider more than one claim in respect of the
Insured Person under Section B Major Surgical Procedure
of the Policy), subject to the availability of the Sum Insured
as specified in the Policy Schedule against Section B, and
provided that the Illness/Accident causing the Injury is
distinct and unrelated for each such claim. On exhaustion of
the Sum Insured, the Benefit under this Benefit will terminate
in relation to the Insured Person.
2. Once a claim has been considered admissible and payable
by Us under this Benefit and Sum Insured has been
exhausted no subsequent Renewal of this Cover will be
allowed
3. In case of multiple Surgeries/Surgical Procedures
performed in a single Admission to a Hospital, or arising out
of the same Illness/Injury, We will pay the amount specified
against only one such Surgical Procedure, having the higher
payout
4. 24 hours of continuous and completed Hospitalization is
mandatory for any claim to be admissible.
5. In case the customer has opted for both Comprehensive
Critical Illness and Major Surgical Procedures Benefit, in a
scenario where the customer is covered for a surgical
procedure under both these Benefits the company, shall be
liable to pay under either of the Benefits whichever is having
a higher payout and the Insured shall not be eligible to claim
for it in the future.
6. Add on cover will not be renewed incase all Critical Illness
buckets under base cover are exhausted
4.2 Exclusions applicable to Section B: Benefit 4 :
We shall not be liable to make any payment for any claim under
Benefit 4 of Section B of this Policy in respect of an Insured
Person, directly or indirectly for, caused by, arising from or in any
way attributable to any of the following:
a) Any covered Surgery/Surgical Procedure arising out of an
Illness diagnosed/contracted prior to Risk Inception Date
or arising within the 90/120/150 days waiting period as
specified in policy schedule. However, no Waiting Period
will be applicable in case of any Surgical Procedure arising
out of/due to an Accident during the Period of Cover
b) Any Surgery/Surgical Procedure arising out of an Accident
which occurred prior to Risk Inception Date.
c) Any Pre-Existing Disease(s) or any disability arising out of
a Pre- Existing Disease or any complication arising
therefrom.
d) Any Critical Illness or Surgery/Surgical Procedure arising
out of any external Congenital Anomaly or internal
Congenital Anomaly known at the commencement of the
policy.
e) Any of the covered Surgery/Surgical Procedure performed
which was otherwise deemed unnecessary, or against
standard health practices.
f) Any Unproven/Experimental treatment.
g) Any Surgery/Surgical Procedure performed solely due to
cosmetic or aesthetic reasons.
h) Any claim made without a medical certificate from the
treating Medical Practitioner evidencing the diagnosis of
such Illness or Injury or the undergoing of the medical /
Surgical Procedure.
Illustration 4:
Ms. PQR has opted for plan which has Cancer bucket and add
on Section B: Major Surgical Procedures. After the initial
waiting period she undergoes Pericardectomy.
She is eligible to claim for 50% payout under Major Surgical
Procedures(Add on Cover).
Subsequently she has to undergo Amputation of Leg she will
be eligible to claim for 100% payout under Major Surgical
Procedure, however as we have already honoured a 50%
claim on account of Pericardiactomy now she will be eligible
to claim for balance 50% only.
Hence we will be honouring 50% payout here subject to policy
terms and conditions
4.3 Claim Documents for Section B:Benefit 4:
Claim Documents On the occurrence of an Insured Event which
may give rise to a claim under this Benefit, We shall be provided
with the following necessary and mandatory information and

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
documentation specified in relation to the Benefit being claimed
within 30 days of occurrence of the Insured Event:
1. Duly filled claim form and signed by the Insured Person
or claimant
2. Scan copy of original Hospital discharge summary
3. All pre and post-Surgery investigation reports/scans
4. Scan copy of original Policy copy
5. Consultation papers of the surgeon advising for the
Surgical Procedure
6. If the claim amount is more than ₹1 lakh, AML Documents
- Pan Card Copy, Residence Proof, and 2 passport sized
color photos of Insured Person/claimant
7. Cancelled cheque and NEFT mandate form - duly filled in
by the Insured Person/claimant
8. All post Hospitalisation, consultation or treatment details
and documents.
9. Copies of Indoor case papers from the Hospital
10. Income Proof(ITR/Salary Slip,etc)
5.1 Section C: Add on Cover: PERSONAL ACCIDENT
Our maximum, total and cumulative liability for claims arising in
respect of the Insured Person during the Period of Cover under
Benefit 5, Benefit 6, and Benefit 7 under Section C, shall be the
Sum Insured as specified against this set of Benefits in the Policy
Schedule.
5.1.1 Benefit 5: Accidental Death Benefit:
We will pay the Sum Insured specified against this Benefit in the
Policy Schedule in the manner specified in the Policy Schedule if
an Insured Person suffers an Injury due to an Accident that occurs
during the Period of Cover and that Injury solely and directly
results in the Insured Person’s death within 365 days from the
date of the Accident. On the acceptance of a claim under this
Benefit and any other applicable Benefit pertaining to the same
event, all Benefit under this Policy shall immediately and
automatically cease in respect of that Insured Person and no
subsequent Renewals of the Policy will be allowed.
Add on cover will not be renewed incase base bucket is
exhausted
5.1.2 Benefit 6: Permanent Total Disablement (PTD) Benefit:
We will pay the Sum Insured specified against this Benefit in the
Policy Schedule in the manner specified in the Policy Schedule if
an Insured Person suffers an Injury due to an Accident that occurs
during the Period of Cover and that Injury solely and directly
results in the Permanent Total Disablement of the Insured Person
within 365 days from the date of the Accident.
This Benefit shall be payable subject to the following:
i. If the Insured Person dies inconsequence to the accident
event before a claim has been admitted under this Benefit,
then no amount will be payable under this Benefit, but a claim
will be considered under Benefit 5, if in force for the Insured
Person.
ii. If the Insured Person suffers Injuries resulting in more than
one of the Permanent Total Disablements, then Our
maximum, total and cumulative liability under this Benefit shall
be limited to the Sum Insured.
iii. If We have admitted a claim for Permanent Total
Disablement in accordance with this Benefit, then We shall not
be liable to make any payment under the Policy under Benefit
5 on the death of the Insured Person, if the Insured Person
subsequently dies.
iv. We will only accept one claim under this Benefit in the
lifetime of the Insured Person. On the acceptance of a claim
under this Benefit, all Benefit under this Benefit in respect of
the Insured Person shall immediately and automatically
cease.
v. On the acceptance of a claim under this Benefit, this
Benefit will terminate and no subsequent renewal of this
Benefit will be allowed
vi. Add on cover will not be renewed incase base bucket is
exhausted
vii. This benefit has been capped at flat 1lac Sum Insured for
less than 10 yrs of age
5.1.3 Benefit 7: Permanent Partial Disablement (PPD) Benefit:
We will pay the percentage of the Sum Insured (specified against
this Benefit in the Policy Schedule) in the manner specified in the
table below if an Insured Person suffers an Injury due to an
Accident that occurs during the Period of Cover and that Injury
solely and directly results in the Permanent Partial Disablement
of the Insured Person (which is of the nature specified in the table
below) within 365 days from the date of the Accident.
For the purpose of this Benefit, Permanent Partial Disablement
means total and/or partial irreversible loss of use or the actual loss
by physical separation of the body parts as specified in the table
below
PPD Table:
Sr
No.
LOSSES COVERED
% OF
SUM
INSU
RED
payab
le
1
Loss of one entire hand
70
2
Loss of one entire foot
70
3
Loss of use of one eye
50
4
Loss of all toes
20
5
Loss of great toe - both phalanges
5
6
Loss of great toe - one phalanx
2
7
Other than great toe if more than one toe
lost each
5
8
Loss of use of both ears
75
9
Loss of use of one ear
30
10
Loss of four fingers and thumb of one
hand
40
11
Loss of four fingers
35
12
Loss of thumb - both phalanges
25
13
Loss of thumb - one phalanx
10
14
Loss of index finger - three phalanges
10
15
Loss of index finger - two phalanges
8

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
16
Loss of index finger - one phalanx
4
17
Loss of middle finger - three phalanges
6
18
Loss of middle finger - two phalanges
4
19
Loss of middle finger - one phalanx
2
20
Loss of ring finger - three phalanges
5
21
Loss of ring finger - two phalanges
4
22
Loss of ring finger - one phalanx
2
23
Loss of little finger - three phalanges
4
24
Loss of little finger - two phalanges
3
25
Loss of little finger - one phalanx
2
26
Loss of metacarpus - first or second
(additional)
3
27
Loss of metacarpus - third, fourth or fifth
(additional)
2
This Benefit shall be payable subject to the following:
i. If the Insured Person dies in consequence to the
accident event before a claim has been admitted
under this Benefit, then no amount will be payable
under this Benefit, but a claim will be considered
under Benefit 5, if in force for the Insured Person.
ii. If a claim is accepted under this Benefit in respect
of an Insured Person and the amount due under this
claim and claims already admitted under the Benefit
in respect of the Insured Person will cumulatively
lead to the Sum Insured being exceeded then Our
maximum, total and cumulative liability under any
and all such claims will be limited to the Sum
Insured.
iii. On exhaustion of Sum Insured, this Benefit shall
terminate and cease to operate in relation to such
Insured Person.
iv. Once a claim has been considered admissible and
payable by Us under this Benefit, any subsequent
Renewal of this this Benefit will be solely as per Our
discretion, on a case to case basis.
v. Add on cover will not be renewed incase base
bucket is exhausted
vi. This benefit has been capped at flat 1lac Sum
Insured for less than 10 yrs of age, however claim
will be payable in accordance to the above PPD
table.
5.2 EXCLUSIONS AND LIMITATIONS APPLICABLE TO
SECTION C
We shall not be liable to make any payment for any claim under
Section C of this Policy in respect of an Insured Person, directly
or indirectly for, caused by, arising from or in any way attributable
to any of the following:
a) War, invasion, act of foreign enemy hostilities or warlike
operations (whether war be declared or not) or civil
commotion or rebellion, revolution, insurrection, mutiny,
arrests, detainments of all kinds and political gatherings,
engaging in aviation other than as a passenger (fare
paying or otherwise) in any licensed standard type of
aircraft.
b) Any Injury sustained while performing duty in army, navy,
air force, paramilitary force, police or any other such
institution, except to the extent it is expressly covered
under any Benefit
c) Any event which occurs whilst the Insured Person is
operating or learning to operate any aircraft or common
carrier, or performing duties as a member of the crew on
any aircraft, or scheduled airlines or is engaging in
aviation, or whilst the Insured Person is mounting into, or
dismounting from or traveling in any balloon or aircraft
other than as a passenger (fare-paying or otherwise) in
any scheduled airline anywhere in the world.
d) Breach of law/ statutory provisions or while being involved
in any unlawful activity.
e) Any Injury / Illness arising from full-time involvement in
professional sports for livelihood and remuneration,
except to the extent it is expressly covered under any
Benefit.
f) Any Injury / Illness arising from intentional self- Injury,
suicide or attempted suicide.
g) Any Injury / Illness arising from a failure to take
reasonable precautions to avoid a claim under the Policy.
h) Any Injury / Illness arising whilst under the influence of
alcohol or intoxicating drugs or substance abuse of any
kind.
i) Any Injury / Illness occurring whilst working in
underground mines or explosives magazines, or involving
electrical installation with high tension supply, or as
jockeys or circus personnel or any other high risk
occupations.
j) Any Injury that has occurred prior to the commencement
of Policy of Benefit whether or not the same has been
treated, or medical advice, diagnosis, care or treatment
has been sought.
k) Any Illness, complication or ailment not arising out of or
connected to Injury.
l) Payment of compensation in respect of death,
disablement (whether of a permanent nature or of a
temporary nature), Injury, Illness or Hospitalization of the
Insured Person resulting directly from, or indirectly
caused by, or contributed to or aggravated or prolonged
by, childbirth or pregnancy or in consequence thereof.
m) Payment of compensation in respect of death,
disablement (whether of a permanent nature or of a
temporary nature), Injury, Illness or Hospitalization of
Insured Person due to an insect or mosquito bite.
n) Death, disablement (whether of a permanent nature or of
a temporary nature), Injury, Illness or Hospitalization
arising from or caused by ionizing radiation or
contamination by radioactivity from any nuclear fuel
(explosive or hazardous form) or resulting from or from
any other cause or event contributing concurrently or in
any other sequence to the loss, claim or expense from
any nuclear waste from the combustion of nuclear fuel,
nuclear, chemical or biological attack.
5.3 Claim documents applicable to Section C:
On the occurrence of an Insured Event which may give rise to a
claim under this Section, We shall be provided with the following

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
necessary and mandatory information and documentation as
specified in relation to the particular Benefit being claimed within
30 days of occurrence of the Insured Event:
Benefit 5 – Accidental Death Benefit
1
Duly filled claim form by the claimant
2
Scan of original policy report
3
MLC / FIR
4
Cause of Death Certificate
5
Death Certificate issued by the Government Authority
6
Post Mortem Report
7
Viscera / Chemical Analysis / Forensic Report
8
Police Final Charge sheet / Court Final Order
9
Spot Inquest / Panchnama
10
RACT award in case of rail accident
11
Indoor Case Papers
12
If the claim amount is more than ₹1 lakh, AML Documents
- Pan Card Copy, Residence Proof, and 2 passport sized
color photos of Insured Person/claimant
13
Cancelled cheque and NEFT mandate form - duly filled in
by the Insured Person/claimant
14
Income Proof(ITR/Salary Slip,etc)
Benefit 6 – Permanent Total Disablement (PTD) Benefit
1
Duly filled claim form by the claimant
2
Scan of original policy report
3
MLC or FIR
4
Police Final Charge sheet / Court Final Order
5
Spot Inquest / Panchnama
6
Indoor Case Papers
7
Disability Certificate by Civil Surgeon / Government
Hospital
8
Certificate from treating Medical Practitioner
9
RACT award in case of rail accident
10
Hospitalisation records and Discharge
summary(wherever applicable)
11
If the claim amount is more than ₹1 lakh, AML Documents
- Pan Card Copy, Residence Proof, and 2 passport sized
color photos of Insured Person/claimant
12
Cancelled cheque and NEFT mandate form - duly filled in
by the Insured Person/claimant
13
Income Proof(ITR/Salary Slip,etc)
Benefit 7 - Permanent Partial Disablement (PPD) Benefit
1
Duly filled claim form by the claimant
2
Scan of original policy report
3
MLC or FIR
4
Police Final Charge sheet / Court Final Order
5
Spot Inquest / Panchnama
6
Indoor Case Papers
7
Disability Certificate by Civil Surgeon / Government
Hospital
8
Certificate from treating Medical Practitioner
9
If the claim amount is more than ₹1 lakh, AML Documents
- Pan Card Copy, Residence Proof, and 2 passport sized
color photos of Insured Person/claimant
10
Cancelled cheque and NEFT mandate form - duly filled in
by the Insured Person/claimant
11
Income Proof(ITR/Salary Slip,etc)
Section D: Value Added Services
1. Tele-consultation:
We will arrange consultations and recommendations for any
listed Critical illnesses under Annexure 1 by a qualified
General Practitioner. For the purpose of this benefit
Telephonic/Virtual consultation shall mean consultation
provided by a qualified General Practitioner through various
mode of communication like audio, chat or mobile app. The
services provided under this Benefit will be made available
subject to the terms and conditions, and in the manner
prescribed below:
The General Practitioner may
suggest/recommend/prescribe over the counter
medications based on the information provided, if
required on a case to case basis. However, the
services under this Benefit should not be construed to
constitute medical advice and/or substitute the
Insured Person's visit/ consultation to an independent
Medical Practitioner/Healthcare professional*.
This service will be available 24 hours a day, and 365
days in a year.
The General Practitioner may refer the Insured
Person to a specialist or a general physician, if
required**, and the charges for such specialist or a
general physician will have to be borne by the Insured
Person.
We shall not be liable for any discrepancy in the
information provided under this Benefit.
Choosing the services under this Benefit is purely
upon the customer’s own discretion and at own risk.
You will be eligible to avail maximum of 4 tele-
consultation per policy period
The insured will be able to use this service only with
respect to the listed Critical Illnesses under Annexure
1.
This benefit will lapse incase not used during the
policy tenure
*The proposer should seek assistance from a health care
professional when interpreting and applying them to
the Insured person’s individual circumstances. If the
Insured person has any concerns about His/ her
health, He/ She may consult His/ her general
practitioner.
**Consultations charges would be applicable.
2. E-opinion (second opinion)

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
In the event of your diagnosis with any of the critical illness
covered under your policy and during the policy period, we
shall facilitate in arranging an E-Consultation second opinion
from a super specialty medical practitioner within our Network
with respect to that critical illness only, subject to the following
condition. It will be based on the medical records submitted by
the insured person which should include investigation reports
citing the final diagnosis and relevant consultation papers. We
will not be reimbursing/bearing the cost for second E-
opinion/consultation.
3. Health and Wellness Offers:
Health and Wellness Offers on services/products provided
by our network providers/ Health service providers – We shall
only facilitate the Insured Person in availing offers and
discounts on services/products offered by our network
providers/ health service providers. Customer can avail
Health and Wellness Offers on our app on various health,
fitness and wellness products and other services available on
the app.
4. Health assistance:
We also provide Health Assistance as a part of Our Value
added services, Our Health Assistance Team (HAT) will assist
the Insured Person in understanding his/her health condition
better by providing answers to any queries related to health
and health care providers on Our dedicated helpline. To avail
this service, the Insured Person may call Our helpline on 040-
66274205 (please note that this number is subject to change).
The services provided under this shall include:
Identifying a Physician/ Specialist
Scheduling an appointment with any Medical
Practitioner empanelled with Us
Scheduling appointments for a second opinion
Providing suitable options with respect to Hospitals as
well as providing assistance in Cashless facility, wherever
applicable.
Providing preventive information on ailments
Providing guidance on post Hospitalization care, such as
Physiotherapy/ Nursing at home.
Please note that services provided under this Benefit are
solely for assistance, and should not be construed to be a
substitute for a visit/ consultation to an independent Medical
Practitioner. This Benefit does not include the charges for any
independent Medical Practitioner/nutritionist consulted on
HAT’s recommendation, and such charges are to be borne by
the Insured Person. We do not accept any liability towards
quality of the services made available by our network
providers/ service providers and are not liable for any defects
or deficiencies on their part
While deciding to obtain such value-added service, You
expressly note and agree that it is entirely for You to decide
whether to obtain these services and also to decide the use (if
any) to which these services is to be put for
IV GENERAL EXCLUSIONS:
We shall not be liable to make any payment for any claim under
this Policy in respect of an Insured Person, directly or indirectly
for, caused by, arising from or in any way attributable to any of the
following:
1. Any physical, medical or mental condition or treatment or
service that is specifically excluded in the Policy Schedule under
the head “Special Conditions”.
2. Any breach of the law by the Insured Person with a criminal
intent.
3. War, invasion, act of foreign enemy, hostilities (whether war be
declared or not) civil war, rebellion, revolution, insurrection,
mutiny, military or usurped power, seizure, capture, arrests,
restraints and detainment of citizens of whatever nation, riots or
civil commotion.
4. Any Injury sustained while performing duty in army, navy, air
force, paramilitary force, police or any other such institution,
except to the extent it is expressly covered under any Benefit.
5. Ionising radiation or contamination by radioactivity from any
nuclear fuel or from any nuclear waste or from nuclear weapon
materials or from the combustion of nuclear fuel. For the purpose
of this exclusion, combustion shall include any self-sustaining
process of nuclear fission.
6. Use or misuse of intoxicating drugs and/or alcohol.
7. Participation (aggravation) in any kind of strike, processions,
riots etc.
8. Any act of self-destruction or self-inflicted injury, attempted
suicide or suicide and deliberate participation of the Insured in an
illegal or criminal act with criminal intent.
9. Any Injury / Illness occurring whilst working in underground
mines or explosives magazines, or involving electrical installation
with high tension supply, or as jockeys or circus personnel
10. Any consequential or indirect losses or expenses related to
any Insured Event.
11. Any tests and treatment relating to infertility and in vitro
fertilization.
12. Any Injury / Illness occurring whilst engaging in any Adventure
Sports, either as an instructor/ trainer, or as a participant.
13. Any natural peril (including but not limited to storm, tempest,
avalanche, earthquake, volcanic eruptions, hurricane, or any
other kind of natural hazard).
V. GENERAL TERMS AND CONDITIONS
i. Standard General Terms and Clauses
1. Disclosure of lnformation
The policy shall be void and all premium paid thereon shall
be forfeited to the Company in the event of
misrepresentation, mis description or non-disclosure of
any material fact by the policyholder.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
"Material facts" for the purpose of this policy shall mean
all relevant information sought by the company in the
proposal form and other connected documents to enable
it to take informed decision in the context of underwriting
the risk
2. Condition Precedent to Admission of Liability:
The terms and conditions of the policy must be fulfilled by
the insured person for the Company to make any payment
for claim(s) arising under the policy.
3. Claim Settlement
i. The Company shall settle or reject a claim, as
the case may be, within 30 days from the date
of receipt of last necessary document.
ii. In the case of delay in the payment of a claim,
the Company shall be liable to pay interest to
the policyholder from the date of receipt of last
necessary document to the date of payment of
claim at a rate 2% above the bank rate.
iii. However, where the circumstances of a claim
warrant an investigation in the opinion of the
Company, it shall initiate and complete such
investigation at the earliest, in any case not
later than 30 days from the date of receipt of
last necessary document- In such cases, the
Company shall settle or reject the claim within
45 days from the date of receipt of last
necessary document.
iv. In case of delay beyond stipulated 45 days, the
Company shall be liable to pay interest to the
policyholder at a rate 2% above the bank rate
from the date of receipt of last necessary
document to the date of payment of claim.
4. Complete Discharge Any payment to the policyholder,
insured person or his/ her nominees or his/ her legal
representative or assignee or to the Hospital, as the case
may be, for any benefit under the policy shall be a valid
discharge towards payment of claim by the Company to
the extent of that amount for the particular claim.
5. Fraud
lf any claim made by the insured person, is in any respect
fraudulent, or if any false statement, or declaration is
made or used in support thereof, or if any fraudulent
means or devices are used by the insured person or
anyone acting on his/her behalf to obtain any benefit
under this policy, all benefits under this policy and the
premium paid shall be forfeited.
Any amount already paid against claims made under this
policy but which are found fraudulent later shall be repaid
by all recipient(s)/policyholder(s), who has made that
particular claim, who shall be jointly and severally liable
for such repayment to the insurer.
For the purpose of this clause, the expression "fraud"
means any of the following
acts committed by the insured person or by his agent or
the hospital/doctor/any
other party acting on behalf of the insured person, with
intent to deceive the insurer or to induce the insurer to
issue an insurance policy:
a) the suggestion, as a fact of that which is not true and
which the insured person does not believe to be true;
b) the active concealment of a fact by the insured
person having knowledge or belief of the fact;
c) any other act fitted to deceive; and
d) any such act or omission as the law specially
declares to be fraudulent
The Company shall not repudiate the claim and / or
forfeit the policy benefits on the ground of Fraud, if the
insured person / beneficiary can prove that the
misstatement was true to the best of his knowledge and
there was no deliberate intention to suppress the fact or
that such misstatement of or suppression of material fact
are within the knowledge of the insurer.
6. Cancellation/ Termination
i. The policyholder may cancel this policy by giving
15days'written notice and in such an event, the
Company shall refund premium for the unexpired
policy period as detailed below.
ii. We shall from the date of receipt of the notice
cancel the Policy, retain the premium for the period
this Policy has been in force, and refund at Our
short period scales as per the Cancellation Grid
provided below, provided that no refund of
premium shall be made if any claim has been made
under the Policy by or on behalf of the Insured
Person.
iii. Notwithstanding anything contained herein or
otherwise, no refunds of premium shall be made in
respect of the Insured Person where any Claim has
been admitted by Us or has been lodged with Us
or any Benefit has been availed by the Insured
Person under the Policy.
iv. In case of a cancellation request by You/Insured
Person, the Policy will be cancelled in its entirety,
and any selected Benefits or Sections under the
Policy cannot be cancelled.
v. The Company may cancel the policy at any time on
grounds of misrepresentation non-disclosure of
material facts, fraud by the insured person by
giving 15 days' written notice. There would be no
refund of premium on cancellation on grounds of
misrepresentation, non-disclosure of material facts
or fraud.
vi. For any cancellation initiated by Us, due to any
other reason the company may choose to refund
the premium on prorata basis.
vii.
Cancellation Grid:

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Time of
cancellation
Policy Duration
1Yr
2Yrs
3Yrs
15 days - 30 days
77%
80%
82%
31 days - 90 days
62%
72%
77%
91 days - 180 days
42%
62%
70%
181 days - 270
days
20%
52%
62%
271 days - 365
days
0%
42%
55%
366 days - 455
days
30%
47%
456 days - 545
days
20%
42%
546 days - 635
days
10%
35%
636 days - 730
days
0%
27%
731 days - 820
days
20%
821 days - 910
days
12%
911 days - 1000
days
5%
Above 1000 days
0%
7. Migration: The insured person will have the option to
migrate the policy to other health insurance
products/plans offered by the company by applying for
migration of the policy atleast 30 days before the policy
renewal date as per IRDAI guidelines on Migration. lf
such person is presently covered and has been
continuously covered without any lapses under any
health insurance product/plan offered by the company,
the insured person will get the accrued continuity benefits
in waiting periods as per IRDAI guidelines on migration.
Migration benefit will be offered to the extent of sum of
previous sum insured, this benefit shall not apply to any
additional sum insured.
For Detailed Guidelines on migration, kindly refer the link
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layou
t.aspx?page=PageNo3986andflag=1
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layou
t.aspx?page=PageNo3987andflag=1
8. Portability: The insured person will have the option to
port the policy to other insurers by applying to such
insurer to port the entire policy along with all the members
of the family, if any, at least 45 days before, but not earlier
than 60 days from the policy renewal date as per IRDAI
guidelines related to portability. lf such person is presently
covered and has been continuously covered without any
lapses under any health insurance policy with an lndian
General/Health insurer, the proposed insured person will
get the accrued continuity benefits in waiting periods as
per IRDAI guidelines on portability.
For Detailed Guidelines on portability, kindly refer the
link
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.
aspx?page=PageNo3986andflag=1
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.
aspx?page=PageNo3987andflag=1
9. Renewal of Policy: The policy shall ordinarily be
renewable except on misrepresentation by the insured
person
i. The Company shall endeavor to give notice for
renewal. However, the Company is not under
obligation to give any notice for renewal.
ii. Request for renewal along with requisite premium
shall be received by the Company before the end of
the policy period.
iii. At the end of the policy period, the policy shall
terminate and can be renewed within the Grace
Period of 30 days
iv. No loading shall apply on renewals based on
individual claims experience
10. Withdrawal of Policy: in the likelihood of this product
being withdrawn in future, the Company will intimate the
insured person about the same 90 days prior to expiry of
the policy. lnsured Person will have the option to migrate
to similar health insurance product available with the
Company at the time of renewal with all the accrued
continuity benefits such as cumulative bonus, waiver of
waiting period. as per IRDAI guidelines, provided the
policy has been maintained without a break.
11. Moratorium
Period After completion of eight continuous years under the
policy no look back to be applied. This period of eight years
is called as moratorium period. The moratorium would be
applicable for the sums insured of the first policy and
subsequently completion of 8 continuous years would be
applicable from date of enhancement of sums insured only
on the enhanced limits. After the expiry of Moratorium Period
no health insurance claim shall be contestable except for
proven fraud and permanent exclusions specified in the
policy contract. The policies would however be subject to all
limits, sub limits, co-payments, deductibles as per the policy
contract.
12. Premium Payment in installments
lf the insured person has opted for Payment of Premium on
an instalment basis i.e. Half Yearly, Quarterly or Monthly, as
mentioned in the policy Schedule/Certificate of lnsurance,
the following Conditions shall apply (notwithstanding any
terms contrary elsewhere in the policy)
i. Grace Period of 7 days would be given to pay the
instalment premium due for the policy.
ii. During such grace period, coverage will not be
available from the due date of instalment premium
till the date of receipt of premium by Company.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
iii. The insured person will get the accrued continuity
benefit in respect of the "Waiting Periods", "Specific
Waiting Periods" in the event of payment of premium
within the stipulated grace Period.
iv. No interest will be charged lf the instalment premium
is not paid on due date
v. ln case of instalment premium due not received
within the grace period, the policy will get cancelled.
We shall not be liable under this Policy for any loss
occurring thereafter, including the intervening period,
nor shall any refund of premium become due under
the Policy. We shall not be bound to give any notice
that such Premium Installment is due.
vi. ln the event of a claim, all subsequent premium
instalments shall immediately become due and
payable.
vii. We shall not be obligated to give any notice to the
Insured Person/Policyholder for payment of premium
installment, and will recover and deduct any or all the
pending premium installments from the claim amount
falling due under the Policy.
13. Possibility of Revision of Terms of the Policy
lncluding the Premium Rates
The Company, with prior approval of lRDAl, may revise or
modify the terms of the policy including the premium
rates. The insured person shall be notified three months
before the changes are effected.
14. Free look period
The Free Look Period shall be applicable on new individual
health insurance policies and not on renewals or at the time of
porting/migrating the policy. The insured person shall be
allowed free look period of fifteen days(30days when policy is
sourced through distance marketing) from date of receipt of
the policy document to review the terms and conditions of the
policy, and to return the same if not acceptable.
lf the insured has not made any claim during the Free Look
Period, the insured shall be entitled to
i. a refund of the premium paid less any expenses incurred
by the Company on medical examination of the insured
person and the stamp duty charges or
ii. where the risk has already commenced and the option of
return of the policy is exercised by the insured person, a
deduction towards the proportionate risk premium for period
of cover or
iii. Where only a part of the insurance coverage has
commenced, such proportionate premium commensurate
with the insurance coverage during such period
The Policy can be cancelled only if no claims have been made
under the Policy. All Your rights under this Policy will immediately
stand extinguished on the free look cancellation of the Policy.
In case the request for cancellation comes 15 days after the
receipt of Policy by the Insured Person, We would refund the
premium paid as per the applicable refund grid provided in the
Cancellation clause of the Policy.
15. Redressal of Grievances:
ln case of any grievance the insured person may contact the
company through
Website: www. icicilombard.com (Customer Support
section).
Toll free: 1800 2666
E-mail: [email protected]
Fax : ……..
Courier: ICICI Lombard General Insurance Company
Ltd.
ICICI Lombard House,
414, Veer Savarkar Marg,
Near Siddhi Vinayak Temple,
Prabhadevi, Mumbai- 400025
Insured person may also approach the grievance cell at
any of the company's branches with the details of
grievance lf Insured person is not satisfied with the
redressal of grievance through one of the above
methods, insured person may contact the grievance
officer at Manager- Service Quality, Corporate
Manager- Service Quality, National Manager-
Operations & finally Director-services and Business
development at the following address:
ICICI Lombard General Insurance Company Limited,
ICICI Lombard House,
414, Veer Savarkar Marg,
Near Siddhi Vinayak Temple,
Prabhadevi, Mumbai 400025
For updated details of grievance officer, kindly refer the link.
.https://www.icicilombard.com/grievance-redressal...
As per the IRDAI’s guidelines on special provision for senior
citizens, We will provide a separate channel for addressing
grievances of Insured Persons who are senior citizens. You
may avail the service by contacting the above mentioned toll
free no and selecting suitable option provided on the
Interactive Voice Response System (IVRS)
If lnsured person is not satisfied with the redressal of
grievance through above methods, the insured person may
also approach the office of lnsurance Ombudsman of the
respective area/region for redressal of grievance as per
lnsurance Ombudsman Rules 2017.
If You are not satisfied with Our response or do not receive
a response from Us within 15 days, You may approach the
Grievance Cell of the Authority at:
Insurance Regulatory and Development Authority of India;
Grievance Call Centre (IGCC) Toll Free No:155255 Email
Grievance may also be lodged at IRDAI lntegrated
Grievance Management System - https:/ligms. irda.qov. in
You can also register Your complaint through fax/letter by
submitting Your complaint to:
Consumer Affairs Department Insurance Regulatory and
Development Authority of India; Sy No. 115/1 Financial
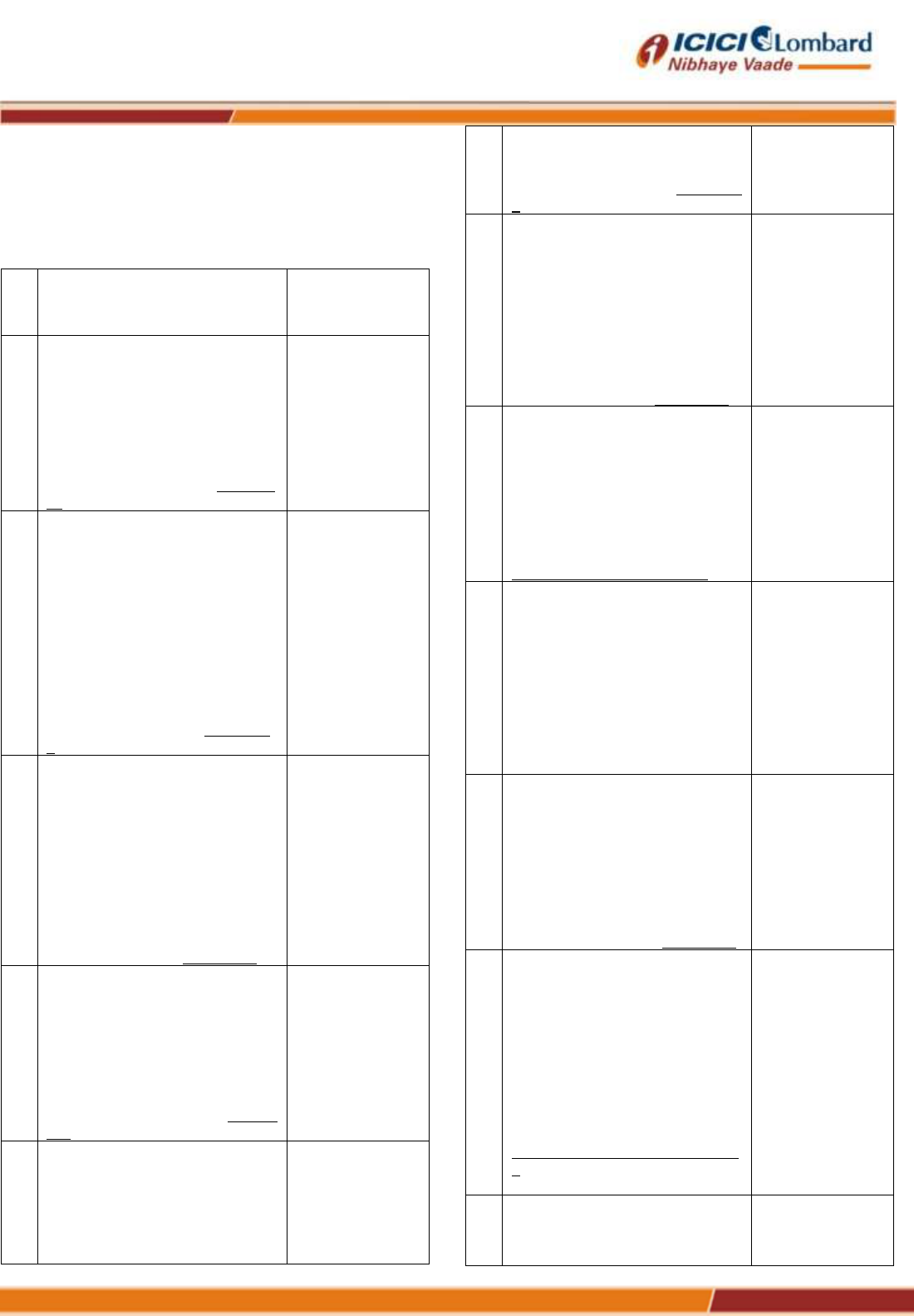
ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
District Nanakramguda Gachibowli -500032 If the issue still
remains unresolved,
You may, subject to vested jurisdiction, approach Insurance
Ombudsman for the redressal of the grievance.
The details of Insurance Ombudsman are available below:
S
no
.
Name of office of insurance
Ombudsman
Territorial Area of
jurisdiction
1
AHMEDABAD
Office of the Insurance
Ombudsman, Jeevan Prakash
Building, 6th floor,
Tilak Marg, Relief Road,
Ahmedabad – 380 001. Tel.: 079 -
25501201/02/05/06
Email:
.in
Gujarat, Dadra
and Nagar Haveli,
Daman and Diu.
2
BENGALURU
Office of the Insurance
Ombudsman,
Jeevan Soudha Building,PID No.
57-27-
N-19
Ground Floor, 19/19, 24th Main
Road,
JP Nagar, Ist Phase,
Bengaluru – 560 078.
Tel.: 080 - 26652048 / 26652049
Email:
n
Karnataka
3
BHOPAL
Office of the Insurance
Ombudsman,
Janak Vihar Complex, 2nd Floor,
6, Malviya Nagar, Opp. Airtel
Office,
Near New Market,
Bhopal – 462 003.
Tel.: 0755 - 2769201 / 2769202
Fax: 0755 - 2769203
Email:
Madhya Pradesh
Chattisgarh.
4
BHUBANESHWAR
Office of the Insurance
Ombudsman,
62, Forest park,
Bhubneshwar – 751 009.
Tel.: 0674 - 2596461 /2596455
Fax: 0674 - 2596429
Email:
o.in
Orissa.
5
CHANDIGARH
Office of the Insurance
Ombudsman,
S.C.O. No. 101, 102 and 103, 2nd
Floor,
Batra Building, Sector 17 – D,
Chandigarh – 160 017.
Punjab,
Haryana,
Himachal
Pradesh,
Jammu and
Kashmir,
Chandigarh.
6
CHENNAI
Office of the Insurance
Ombudsman,
Fatima Akhtar Court, 4th Floor,
453,
Anna Salai, Teynampet,
CHENNAI – 600 018.
Tel.: 044 - 24333668 / 24335284
Fax: 044 - 24333664
Email:
Tamil Nadu,
Pondicherry Town
and
Karaikal (which
are part of
Pondicherry).
7
DELHI
Office of the Insurance
Ombudsman,
2/2 A, Universal Insurance
Building,
Asaf Ali Road,
New Delhi – 110 002.
Tel.: 011 - 23232481/23213504
Email:
Delhi
8
ERNAKULAM
Office of the Insurance
Ombudsman,
2nd Floor, Pulinat Bldg.,
Opp. Cochin Shipyard, M. G. Road,
Ernakulam - 682 015.
Tel.: 0484 - 2358759 / 2359338
Fax: 0484 - 2359336
Email:
n
Kerala,
Lakshadweep,
Mahe-a part of
Pondicherry.
9
GUWAHATI
Office of the Insurance
Ombudsman,
Jeevan Nivesh, 5th Floor,
Nr. Panbazar over bridge, S.S.
Road,
Guwahati – 781001(ASSAM).
Tel.: 0361 - 2632204 / 2602205
Email:
Assam,
Meghalaya,
Manipur,
Mizoram,
Arunachal
Pradesh,
Nagaland and
Tripura.
10
HYDERABAD
Office of the Insurance
Ombudsman,
6-2-46, 1st floor, "Moin Court",
Lane Opp. Saleem Function
Palace,
A. C. Guards, Lakdi-Ka-Pool,
Hyderabad - 500 004.
Tel.: 040 - 67504123 / 23312122
Fax: 040 – 23376599
Email:
n
Andhra Pradesh,
Telangana,
Yanam and
part of Territory of
Pondicherry.
11
JAIPUR
Office of the Insurance
Ombudsman,
Jeevan Nidhi – II Bldg., Gr. Floor,
Rajasthan.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
12
KOLKATA
Office of the Insurance
Ombudsman,
Hindustan Bldg. Annexe, 4th Floor,
4, C.R. Avenue,
KOLKATA - 700 072.
Tel.: 033 - 22124339 / 22124340
Fax : 033 - 22124341
Email:
West Bengal,
Sikkim,
Andaman and
Nicobar Islands.
13
LUCKNOW
Office of the Insurance
Ombudsman,
6th Floor, Jeevan Bhawan, Phase-
II,
Nawal Kishore Road, Hazratganj,
Lucknow - 226 001.
Tel.: 0522 - 2231330 / 2231331
Fax: 0522 - 2231310
Email:
Districts of Uttar
Pradesh :
Laitpur, Jhansi,
Mahoba,
Hamirpur,
Banda, Chitrakoot,
Allahabad,
Mirzapur,
Sonbhabdra,
Fatehpur,
Pratapgarh,
Jaunpur,Varanasi,
Gazipur, Jalaun,
Kanpur, Lucknow,
Unnao, Sitapur,
Lakhimpur,
Bahraich,
Barabanki,
Raebareli,
Sravasti,
Gonda, Faizabad,
Amethi,
Kaushambi,
Balrampur, Basti,
Ambedkarnagar,
Sultanpur,
Maharajgang,
Santkabirnagar,
Azamgarh,
Kushinagar,
Gorkhpur,
Deoria, Mau,
Ghazipur,
Chandauli,
Ballia,
Sidharathnagar.
14
MUMBAI
Office of the Insurance
Ombudsman,
3rd Floor, Jeevan Seva Annexe,
S. V. Road, Santacruz (W),
Mumbai - 400 054.
Tel.: 022 - 26106552 / 26106960
Fax: 022 - 26106052
Email:
Goa,
Mumbai
Metropolitan
Region
excluding Navi
Mumbai and
Thane.
15
NOIDA
Office of the Insurance
Ombudsman,
Bhagwan Sahai Palace
4th Floor, Main Road,
State of
Uttaranchal and
the following
Districts of Uttar
Pradesh:
Naya Bans, Sector 15,
Distt: Gautam Buddh Nagar,
U.P-201301.
Tel.: 2514252 / 2514253
Email:
Agra, Aligarh,
Bagpat, Bareilly,
Bijnor, Budaun,
Bulandshehar,
Etah,
Kanooj, Mainpuri,
Mathura, Meerut,
Moradabad,
Muzaffarnagar,
Oraiyya,
Pilibhit, Etawah,
Farrukhabad,
Firozbad,
Gautambodhanag
ar,
Ghaziabad,
Hardoi,
Shahjahanpur
16
PATNA
Office of the Insurance
Ombudsman,
1st Floor,Kalpana Arcade
Building,,
Bazar Samiti Road,
Bahadurpur,
Patna 800 006.
Tel.: 0612-2680952
Email:
Bihar,
Jharkhand.
17
PUNE
Office of the Insurance
Ombudsman,
Jeevan Darshan Bldg., 3rd Floor,
C.T.S. No.s. 195 to 198,
N.C. Kelkar Road, Narayan Peth,
Pune – 411 030.
Tel.: 020-41312555
Email:
Maharashtra,
Area of Navi
Mumbai and
Thane
excluding Mumbai
Metropolitan
Region.
16. Nomination
The policyholder is required at the inception of the policy to
make a nomination for the purpose of payment of claims
under the policy in the event of death of the policyholder. Any
change of nomination shall be communicated to the
company in writing and such change shall be effective only
when an endorsement on the policy is made. ln the event of
death of the policyholder, the Company will pay the nominee
{as named in the Policy Schedule/Policy
Certificate/Endorsement (if any)} and in case there is no
subsisting nominee, to the legal heirs or legal
representatives of the policyholder whose discharge shall be
treated as full and final discharge of its liability under the
policy.
ii. Specific Terms and Clauses:
1. PAYMENTS
We shall make payment of an admissible claim to the
Insured Person’s Nominee/assignee, as the case may be,
or in the absence of an assignee, to the Insured Person or

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
the Insured Person’s nominee. If there is no assignee or
Nominee and the Insured Person is incapacitated or
deceased, We will pay to the Insured Person’s heir, executor
or validly appointed legal representative.
Any payment We make in this manner will be a complete
and final discharge of Our obligations under this Policy and
Our liability towards the claim.
2. TERMS OF RENEWAL
The Policy may be renewed by mutual consent under
the then prevailing (ICICI Lombard Criti Shield
Plus)Policy or its nearest substitute product (in case of
product withdrawal) approved by the IRDAI, and in
such event the Renewal premium should be paid to Us
on or before the date of expiry of the Policy and in no
case later than the Grace Period of 30 days from the
expiry of the Policy. We will not be liable to pay for any
Claim arising out of an Insured Event that occurs
during the Grace Period.
Once the Sum Insured under any of the Benefits opted
and available to the insured is exhausted any future
renewal under that Benefit shall not be allowed.
You shall on tendering any premium for the Renewal
of this Policy give notice in writing to Us of any Illness,
physical defect or infirmity with which any of the
Insured Person(s) have become affected since the
payment of the expiring Policy start date.
Renewals will not be denied except on grounds of
misrepresentation, moral hazard, fraud, non-
disclosure of material facts. We may, revise the
Renewal premium payable under the Policy or the
terms of Benefit, provided that all such changes are
approved in accordance with the IRDAI rules and
regulations as applicable from time to time. We will
intimate You of any such changes at least 3 months
prior to date of such revision or modification.
We shall not be bound to give any notice to
You/Insured Person that the premium for the Renewal
is due.
Policyholder will not be allowed to make any changes
in his/her policy coverages, terms and conditions and
Sum Insured at the time of renewal in case a claim
has already been settled
Policyholder will not be allowed to make any changes
in his/her policy coverages, terms and conditions at the
time of renewal, unless decided by Us on exceptional
call or case to case basis and subject to fresh proposal
form
In the event where the base cover(s) has been
exhausted the insured shall not be allowed to renew
the add on cover(s)
The above conditions for Renewal are to be read in
unison, and not standalone.
3. CLAIM PROCEDURE:
The fulfillment of the terms and conditions of this Policy
(including payment of premium by the due dates
mentioned in the Policy Schedule) insofar as they
relate to anything to be done or complied with by You
or any Insured Person, including complying with the
procedures and requirements in relation to claims,
shall be Conditions Precedent to Our liability under this
Policy.
We shall be under no obligation to make any payment
under this Policy unless We have received all premium
payments in full and on time in respect of the Insured
Person’s Benefit under the Policy and all payments
have been realised.
On occurrence of an any event that may give rise to a
Claim under this Policy, You shall-
o Notify Us immediately on toll free number 1800
2666 or on our website www.icicilombard.com
or also in writing at Our address specified in the
Policy Schedule or email us at
o Along with the completed and signed Claim
form, provide all the relevant documents,
specified within the relevant Section of the
Policy for the Benefit being claimed, must be
submitted in full within 30 days.
o Wherever details pertaining to happening of
Claim are conveyed by you to Us after
reasonable period, You shall provide the
reasons of such delay to Us.
If any Claim is not made within 30 days of the Insured
Event, then We will condone such delay on merits only
where the delay has been proved to be for reasons
beyond the claimant’s control.
All claims will be investigated (as required) and settled
in accordance with the applicable regulatory
guidelines, including the IRDAI (Protection of
Policyholders Interests) Regulations, 2017.
The admissible Claim amount will be calculated post
applicability of Deductible, Co-pay, Sub-limits, if any,
and as specifically defined in Policy Schedule.
The role of the TPA (if any) would be limited to facilitate
the flow of information between Us and the Insured
Person.
4. Incontestability and Duty of Disclosure :
The Policy shall be null and void and no Benefit shall be
payable in the event of untrue or incorrect statements,
misrepresentation, mis description or on non-disclosure in
any material particular in the proposal form, personal
statement, declaration and connected documents, or any
material information having been withheld, or a claim being
fraudulent or any fraudulent means or devices being used
by the Insured Person or any one acting on his/her behalf to
obtain any Benefit under this Policy.
5. Observance of terms and conditions

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
The due observance and fulfilment of the terms, conditions
and endorsement of this Policy in so far as they relate to
anything to be done or complied with by the Insured Person,
shall be a condition precedent to Our liability to make any
payment under this Policy.
6. Records to be maintained
The Insured Person shall keep an accurate record
containing all relevant particulars and shall allow Us to
inspect such record.
7. No constructive Notice
Any knowledge or information of any circumstances or
condition in relation to the Insured Person, or in connection
with which a claim may be made under this Policy coming to
the knowledge or possession of any of Our officials shall not
be construed as notice to or be held to bind or prejudicially
affect Us notwithstanding subsequent acceptance of any
premium.
8. Notice of Charge
We shall not be bound to take notice or be affected by any
notice of any trust, charge, lien, assignment or other dealing
with or relating to this Policy, but the payment by Us to the
Insured Person, Nominee, assignee or his legal heirs of any
amount under the Policy shall in all cases be an effectual
discharge to Us.
9. Special Provisions
Any special provisions subject to which this Policy has been
entered into and endorsed in the Policy, Policy Schedule or
in any separate instrument or Endorsement shall be deemed
to be part of this Policy and shall have effect accordingly.
10. Overriding effect of Part II of the Schedule
The terms and conditions contained herein and in Policy
Schedule(Policy certificate or Certificate of Insurance) shall
be deemed to form part of the Policy and shall be read as if
they are specifically incorporated herein; however in case of
any inconsistency of any term and condition with the scope
of Benefit contained in Policy Schedule, then the term(s) and
condition(s) contained herein shall be read mutatis mutandis
with the scope of Benefit/terms and conditions contained in
Policy Schedule and shall be deemed to be modified
accordingly or superseded in case of inconsistency being
irreconcilable.
11. Electronic Transactions
The Insured Person agrees to adhere to and comply with
all such terms and conditions as We may prescribe from
time to time, and hereby agrees and confirms that all
transactions effected by or through facilities for conducting
remote transactions including the internet, the world wide
web, electronic data interchange, call centres, teleservice
operations (whether voice, video, data or combination
thereof) or by means of electronic, computer, automated
machines network or through other means of
telecommunication, established by or on Our behalf, for and
in respect of the Policy or its terms, or Our other products
and services, shall constitute legally binding and valid
transactions when done in adherence to and in compliance
with Our terms and conditions for such facilities, as may be
prescribed from time to time. The Insured Person agrees
that We may exchange, share or part with any information
with any government institution or statutory body, as may be
determined by Us and shall not hold Us liable for such
use/application.
12. Right to inspect
In case of any loss or occurrence to the Insured Person that
has given or may give rise to a claim under the Policy, If
required by Us, Our agent/representative, including any loss
assessor or surveyor/investigator or any individual or entity
appointed on Our behalf shall be permitted at all reasonable
times to examine the circumstances of such loss or
occurrence. The Insured Person shall on being required to
do so by Us, produce all books of accounts, receipts,
documents relating to or containing entries relating to the
loss or such circumstance in his/her possession and furnish
copies of or extracts from such of them as may be required
by Us so far as they relate to such claim(s), or may in any
way assist Us to ascertain the correctness thereof or Our
liability under the Policy.
13. Policy Disputes
Any dispute concerning the interpretation of the terms,
conditions, limitations and/or exclusions contained herein is
understood and agreed to by both the Insured Person and
Us to be subject to Indian Law. Each party agrees to submit
to the jurisdiction of the Courts in India and to comply with all
requirements necessary to give such Court the jurisdiction.
All matters arising hereunder shall be determined in
accordance with the law and practice of such Court.
14. Arbitration clause
i. If any dispute or difference shall arise as to the
quantum of claim to be paid under this Policy
(liability/claim being otherwise admitted by the
Insurer), such difference shall independently of
all other question be referred to the decision of a
sole arbitrator to be appointed mutually in writing
by the Insurer and the Insured who has made
claim under this Policy or if they cannot agree
upon a single arbitrator within 30 days of any
party [the Insurer or the and the Insured who has
made claim under this Policy] invoking
arbitration, the same shall be referred to a panel
of three arbitrators, comprising of two arbitrators
one to be appointed by the Insured who has
made claim under this Policy and the Insurer,
respectively, who are the parties to the dispute/
difference and the third arbitrator to be appointed
by such two appointed arbitrators and arbitration
shall be conducted under and in accordance with
the provisions of the Arbitration and Conciliation

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Act, 1996 as amended from time to time. The law
of the arbitration will be Indian law.
ii. It is clearly agreed and understood that no
difference or dispute shall be referable to
arbitration as herein before provided if the Insurer
has disputed or not accepted/admitted the
liability/claim under the Policy.
iii. It is hereby expressly stipulated and declared that
it shall be a Condition Precedent to any right of
action or suit read with this Policy that the award
by such arbitrator/ arbitrators of the amount of the
benefits shall be first obtained
iv. It is also hereby further expressly agreed and
declared that if the Insurers shall
disclaim/repudiate the liability to the Insured for
any claim under the Policy, and such claim shall
not, within 12 calendar months from the date of
such disclaimer/repudiation have been made the
subject matter of a suit in a court of law, then all
benefits under the Policy shall be forfeited and
the rights of Insured shall stand extinguished and
the liability of the Insurer shall also stand
discharged.
15. Notices:
Any notice, direction or instruction given under this Policy
shall be in writing and delivered by hand, post, or facsimile
to:
In case of You, at the address specified in Policy Schedule,
and in case of the Insured Person, at the Insured Person’s
address specified in the Policy Schedule.
In case of Us:
ICICI Lombard General Insurance Company Limited, ICICI
Lombard House,
414, Veer Savarkar Marg, Near Siddhi Vinayak Temple,
Prabhadevi,
Mumbai 400025, Toll-free number: 1800-2666
Notice and instructions will be deemed served 7 days after
posting or immediately upon receipt in the case of hand
delivery, facsimile or e mail.
16. Customer Service
If at any time the Insured Person (or his Nominee/ legal heir,
as the case may be) requires any clarification or assistance,
they may contact Our offices at the address specified below,
during normal business hours.
ICICI Lombard General Insurance Company Limited
ICICI Lombard House 414, Veer Savarkar Marg,
Siddhi Vinayak Temple, Prabhadevi, Mumbai 400025.
You could also call us on Toll free No: 1800 2666 or E-mail:
Please inform Us immediately of any change in the
address, occupation, state of health, or of any other
changes affecting the Insured Person (or his Nominee/
legal heir, as the case may be).
VI OTHER TERMS AND CONDITIONS
1. AGE LIMIT
The age of proposer: minimum and maximum age of
entry for proposer into the Policy is 18 years and 65
years respectively
Age of insured: minimum and maximum age of entry
for an insured into the Policy is 3 months and 65 years
respectively
2. In case You choose to pay the premium in instalments,
then You shall not be able to change the frequency of
payments within the Period of Cover
3. In case You have opted for auto renewal, the Policy shall
be Renewed with the same terms and conditions
including but not limited to the Sum Insured, coverage,
premium paying terms and claim payment terms.
4. The scope of Benefit shall be worldwide unless specified
otherwise.
5. Any change in the policy terms and conditions including
but not limited to Sum Insured and/or coverage shall not
be permitted within the policy period
6. Nationality: The policy can only be opted by Indian
Nationality citizens or Non Residents of India holding an
Indian Passport & account
VII ADDITIONAL CLAUSES AVAILABLE UNDER THIS
POLICY
1. Assignment clause
It is hereby declared and agreed that upon due written consent
granted by the Proposer as stated under the head of “Proposer
name” in the Policy Schedule to the Policy:
i. Any amount becoming payable to the Insured
Person in accordance with policy terms and
conditions) including all rights, title, benefits and
interest of the Insured Person under this Policy
stand assigned in favour of the Financial Institution
(assignee) specified in the Policy Schedule of the
Policy with respect to only that Loan Account
Number, as specified in the Policy Schedule.
ii. The receipt of such amount in the manner aforesaid
by the Financial Institution (assignee) specified in
the Policy Schedule of this Policy, shall completely
discharge Us from all Our liability under the Policy
in respect of such payable amount, and this shall
be binding on the Insured Persons and their legal
heirs, executors, administrators, and successors.
iii. This is to clarify that such assignment shall be
subject to the condition that in the event of the
Insured Person’s death during the Period of Cover,
the amounts payable as per the Policy terms and
conditions will be paid to the said Financial
Institution (assignee) only to the extent of the Loan
amount outstanding, if any, and any amount in

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
excess after such payment shall be paid to the
Insured Person’s Nominee.
2. Auto Renewal Clause
a. On due consent by the Proposer We will automatically
renew the Policy for the Period of Cover as opted by the
Insured Person. However, after completing an entire auto
Renewal period on expiry of the Policy on the Policy End
Date, We shall not be bound to accept any Renewal
premium nor give notice that such Renewal premium is due.
b. Every Renewal premium shall be paid and accepted as
per the terms of Renewal specified under this Policy and
upon the distinct understanding that no alteration has taken
place in the facts contained in the Proposal and Declaration
Form herein before mentioned and that nothing is known to
the Insured Person that may result to enhance the risk of We
under the guarantee hereby given. Any change in the risk
will be intimated to Us by the Policyholder/ Insured Person.
Nothing herein or otherwise shall affect Our right to impose
any additional terms and conditions on Renewal or restrict
any Renewal terms as to premium or otherwise.
No Renewal receipt shall be valid unless it is on the printed
form of Our and signed by Our authorized official.
3. Increase/decrease in sum insured:
Sum insured can be changed (increased/ decreased)
only at the time of renewal or at any time, subject to
underwriting by the Company subject to revised proposal
form. For any increase in Sum Insurance, the waiting
period and survival period if any shall start afresh only
for the enhanced portion of the sum insured.
Annexure 1:
Major(55)
Minor(37)
Cancer and
blood
disorders(4/1)
Cancer of Specified
severity(Major
Cancer)
Early stage
cancer/Carcinoma-
in- Situ
Bone Marrow
Transplant
Aplastic Anaemia
Primary
Myelofibrosis
Heart and
Blood Vessel
(10/11)
Takayasu Arteritis
Pulmonary Artery
Graft Surgery
Refractory Heart
Failure
Cardiac Arrhythmia
with surgical
intervention(Sum
Insured capped at 5
lacs)
Eisenmenger's
Syndrome
Other Serious
Coronary Artery
Diseases
Myocardial
Infarction (First
Heart Attack - Of
Specified Severity
Insertion of a
Permanent Cardiac
Defibrillator
Cardiomyopathy of
specified severity
Complete Heart
Block or Third
Degree Heart Block
with pacemaker
Open Chest CABG
Pericardectomy
Open Heart
Replacement Or
Repair Of Heart
Valves
Balloon Valvotomy or
Valvuloplasty
Surgery Of Aorta
Angioplasty (Sum
Insured capped at 5
lacs)
Primary (Idiopathic)
Pulmonary
Hypertension
Minimally Invasive
Surgery to Aorta
Infective
Endocarditis
Pulmonary embolism
Moderately Severe
Cardiomyopathy
Major
Organs(14/12)
Systemic Lupus
Erythematous With
Renal Involvement
Severe Acquired Or
Secondary
Pulmonary Alveolar
Proteinosis (Pap)
Rheumatoid
Arthritis
Glomerulonephiritis
with Nephrotic
Syndrome
Scleroderma
Moderately Severe
Kidney Disease
Good Pastures
Syndrome With
Lung or Renal
Involvement
Moderately Severe
Systemic Lupus
Erythematous With
Lupus Nephritis
Myasthenia Gravis
Intestinal Gangrene
End Stage Lung
Failure
Portal Vein
Thrombosis
Kidney Failure
Requiring Regular
Dialysis
Surgical Removal of
One Lung
Medullary Cystic
Kidney Disease
Moderately Severe
Crohn's Disease
Fulminant Hepatitis
Moderaterly Severe
Ulcerative Colitis.
End Stage Liver
Failure
Small bowel
transplant
Major Organ
transplant
Ankylosing
Spondylytis
Severe Crohn’s
Disease
Surgical Removal of
one kidney
Severe Ulcerative
Colitis
Chronic Relapsing
Pancreatitis
Nervous
System(24/8)

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Stroke Resulting in
Permanent
Symptoms
Loss of Hearing of
One Ear
Permanent
Paralysis of Limbs
Loss Of Sight In One
Eye
Motor Neuron
Disease With
Permanent
Symptoms
Dissolution of the
nerve roots of
Brachial Plexus
Parkinson's
Disease
Syringomelia or
Syringobulbia
Requiring Surgery
Benign Brain Tumor
Carotid Artery
Surgery
Alzheimer's
Disease
Loss of Use of One
Limb
Progressive
Supranuclear Palsy
Idiopathic Scoliosis
Multiple Sclerosis
with Persisting
Symptoms
Coma 72 Hours
Creutzfeldt-Jakob
Disease
Muscular Dystrophy
Coma of Specified
Severity
Apallic Syndrome
Major Head Trauma
Guillain-Barre
Syndrome
Deafness
Loss Of Speech
Blindness
Spinal Stroke
Benign Spinal Cord
Tumour with
Neurological Deficit
Poliomyelitis
Bacterial Meningitis
Encephalitis
Tuberculousis
Meningitis
Severe Progressive
Bulbar Palsy
Other
Illness(3/5)
Third Degree Burns
Elephantiasis
Necrotising Fasciitis
Adrenalectomy for
Adrenocortical
Adenoma
Pheochromocytoma
Wilson's Disease
Optic Neuropathy
Facial
Reconstructive
Surgery due to
accident
Note:
The maximum payout against any minor Critical Illness under
any Critical illness bucket is restricted to 25% of the base cover
Sum Insured upto a maximum of 12.5lacs however for “Cardiac
Arrhythmia with surgical intervention” and “Angioplasty” the
Sum Insured is further restricted to a maximum of 5lac
Definitions:
1. Cardiomyopathy of specified severity
An impaired function of the heart muscle, unequivocally
diagnosed as Cardiomyopathy by a registered Medical
Practitioner who is a cardiologist, and which results in permanent
physical impairment to the degree of New York Heart Association
Classification Class IV, or its equivalent, based on the following
classification criteria:
Class IV - Inability to carry out any activity without discomfort.
Symptoms of congestive cardiac failure are present even at rest.
With any increase in physical activity, discomfort will be
experienced. The Diagnosis of Cardiomyopathy has to be
supported by echocardiographic findings of compromised
ventricular performance.
Irrespective of the above, Cardiomyopathy directly related to
alcohol or drug abuse is excluded.
2. Surgery of Aorta :
The actual undergoing of medically necessary major surgery for
a disease of the aorta needing excision and surgical replacement
of the diseased aorta with a graft. For the purpose of this definition
aorta shall mean the thoracic and abdominal aorta but not its
branches.
Traumatic injury of the aorta is excluded.
Surgery performed using only minimally invasive or intra-arterial
techniques are excluded.
3. Complete Heart Block or Third Degree Heart Block with
pacemaker:
A specific kind of abnormality of heart beat (arrhythmia)
characterized by complete cessation of transmission of
electrical impulses to the ventricles (lower chambers) of the
heart. The diagnosis of Complete Heart Block or Third
Degree Heart Block must be made by a cardiologist and
substantiated by findings in ECG suggestive of Complete
Heart Block or Third Degree Heart Block .The insured must
have undergone pacemaker insertion for treating Complete
Heart Block.
4. Eisenmenger's Syndrome
Development of severe pulmonary hypertension and shunt
reversal resulting from heart condition. The diagnosis must be
made by a registered Medical Practitioner who is a specialist with
echocardiography and cardiac catheterisation resulting in
permanent physical impairment to the degree of New York Heart
Association Classification Class IV, or its equivalent, based on the
following classification criteria:
Class IV - Inability to carry out any activity without discomfort.
Symptoms of congestive cardiac failure are present even at rest.
With any increase in physical activity, discomfort will be
experienced.
5. Infective Endocarditis
Inflammation of the inner lining of the heart caused by infectious
organisms, where all of the following criteria are met:

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
• Positive result of the blood culture proving presence of the
infectious organism(s);
• Presence of at least moderate heart valve incompetence
(meaning regurgitant fraction of 20% or above) or moderate heart
valve stenosis (resulting in heart valve area of 30% or less of
normal value) attributable to Infective Endocarditis; and
• The Diagnosis of Infective Endocarditis and the severity of
valvular impairment are confirmed by a registered Medical
Practitioner who is a cardiologist
6. Pulmonary Embolism
The medically necessary surgical insertion of a veno-caval filter
after there has been documented proof of recurrent pulmonary
emboli. The need for the insertion of a veno-caval filter must be
certified to be absolutely necessary by a specialist in the relevant
field.
7. Bacterial Meningitis
Bacterial infection resulting in severe inflammation of the
membranes of the brain or spinal cord resulting in significant,
irreversible and permanent neurological deficit. The neurological
deficit must persist for at least 6 weeks resulting in permanent
inability to perform three or more
Activities of Daily Living.
This diagnosis must be confirmed by:
a. The presence of bacterial infection in cerebrospinal fluid by
lumbar puncture; and
b. A consultant neurologist certifying the diagnosis of bacterial
meningitis.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an
upright chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room
on level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain
a satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
8. Encephalitis
Severe inflammation of the brain tissue due to infectious agents
like viruses or bacteria which results in significant and permanent
neurological deficits for a minimum period of 6 weeks, certified by
a specialist Medical Practitioner (Neurologist)
The permanent deficit must result in permanent inability to
perform three or more Activities of Daily Living.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room
on level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain
a satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
9. Tuberculosis Meningitis
Meningitis caused by tubercle bacilli. Such a diagnosis must
be supported by:
1) Findings in the cerebrospinal fluid (csf) report
2) Presence of acid fast bacilli in the cerebrospinal fluid or
growth of M. Tuberculosis demonstrated in the culture report
or Nucleic acid amplification tests like PCR
3) Certification by a registered doctor who is a specialist in
neurology, or a physician with a degree of MD
The condition must have resulted in irreversible and
permanent neurological deficit which persist for at least 6
weeks and resulting in permanent inability to perform three
or more Activities of Daily Living.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room
on level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain
a satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
10. Progressive Supranuclear Palsy
Confirmed by a registered doctor who is a specialist in neurology
of a definite diagnosis of progressive supranuclear palsy.
The condition must have resulted in irreversible and permanent
neurological deficit which persist for at least 6 weeks and resulting
in permanent inability to perform three or more Activities of Daily
Living.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room
on level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain
a satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
11. Fulminant Hepatitis
A sub-massive to massive necrosis of the liver by the Hepatitis
virus, leading precipitously to liver failure. This diagnosis must be
supported by all of the following:
a. Rapid decreasing of liver size;
b. Necrosis involving entire lobules, leaving only a collapsed
reticular framework;
c. Rapid deterioration of liver function tests;
d. Deepening jaundice; and
e. Hepatic encephalopathy.
Acute Hepatitis infection or carrier status alone does not meet the
diagnostic criteria.
12. Pheochromocytoma
Presence of a neuroendocrine tumour of the adrenal or extra‐
chromaffin tissue that secretes excess catecholamines requiring
the actual undergoing of surgery to remove the tumour.
The Diagnosis of Pheochromocytoma must be supported by
plasma metanephrine levels and / or urine catecholamines and
metanephrines and confirmed by a registered doctor who is an
endocrinologist.
13. Guillain Barre Syndrome:
It is a disorder in which the immune system of a person attacks
the person’s peripheral nervous system resulting in irreversible
and permanent neurological deficit which persist for at least 6
weeks and resulting in permanent inability to perform three or
more Activities of Daily Living. The diagnosis has to be confirmed
by a neurologist and substantiated by typical findings in CSF,
EMG and NC studies.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room on
level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain a
satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
14. Takayasu’s Arteritis:
It is a specific kind of arteritis and the inflammation damages the
aorta and its main branches resulting in the medically necessary
bypass surgery or aortic valve surgery. The diagnosis has to be
confirmed by a specialist medical practitioner and substantiated
by typical findings in angiography.
15. Rheumatoid Arthritis
Widespread chronic progressive joint destruction with major
deformity, where all of the following criteria are met:
Unequivocal diagnosis of Rheumatoid Arthritis made
based on the American College of Rheumatology
criteria;
Damage and deformity of at least 3 (three) of the following
joints: hand (metaphalangeal joints), wrist, elbow, knee,
hip, or feet (metatarsophalangeal joints). Such deformity
must be confirmed by imaging studies showing such
changes; and Disability resulting in the inability of the
Insured to perform (whether aided or unaided) at least 3
of the following 6 “Activities of Daily Living” for a
continuous period of at least 6 months.
Activities of Daily Living are defined as:
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room on
level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain a
satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
16. Ankylosing spondylitis:
It is a type of arthritis that causes inflammation between the
vertebrae and in the joints between the spine and pelvis. The
condition must have progressed to the extent of irreversible and
permanent neurological deficit which persist for at least 6 weeks
and resulting in permanent inability to perform three or more
Activities of Daily Living. The diagnosis must be made by a
specialist medical practitioner and substantiated by typical
findings in MRI.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room on
level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain a
satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
17. Intestinal Gangrene:
Death of a part or whole of the intestine due to lack of blood flow
and superimposed infection. The diagnosis must be made by a
specialist medical practitioner and substantiated by typical
findings in MRI and histopathology report.
18. Severe Crohn’s Disease
Crohn’s Disease is a chronic, transmural inflammatory disorder of
the bowel. To be considered as severe, there must be evidence
of continued inflammation in spite of optimal therapy, with all of
the following having occurred:
• Stricture formation causing intestinal obstruction requiring
admission to Hospital, and
• Fistula formation between loops of bowel, and
• At least one bowel segment resection.
The diagnosis must be made by a registered Medical
Practitioner who is a specialist Gastroenterologist and be
proven histologically on a pathology report and/or the results of
sigmoidoscopy or colonoscopy.
19. Severe ulcerative colitis
Acute fulminant ulcerative colitis with life threatening electrolyte
disturbances.
All of the following criteria must be met:
• The entire colon is affected, with severe bloody diarrhoea; and
• The necessary treatment is total colectomy and ileostomy; and
• The diagnosis must be based on histopathological features
and confirmed by a registered Medical Practitioner who is a
specialist in gastroenterology
20. Chronic Relapsing Pancreatitis
More than three attacks of pancreatitis resulting in pancreatic
dysfunction causing malabsorption needing enzyme replacement
therapy.
The Diagnosis must be made by a gastroenterologist and
confirmed by Endoscopic Retrograde Cholangio
Pancreatography (ERCP).
21. Elephantiasis
The result and complication of filariasis, characterized by massive
swelling in the tissues of the body as a result of obstructed
circulation in lymphatic vessels. Unequivocal Diagnosis of
elephantiasis must be clinically confirmed by a Specialist in the
relevant medical field, including laboratory confirmation of
microfilariae, and must be supported by our medical adviser.
The benefit does not cover Lymphoedema caused by infection
with a sexually transmitted disease, trauma, postoperative
scarring, congestive heart failure, or congenital lymphatic system
abnormalities.
22. Primary Myelofibrosis
A disorder which can cause fibrous tissue to replace the normal
bone marrow and results in severe anaemia below 10 g/dl, low
platelet count below 100,000 microL and enlarged spleen. The
condition must have progressed to the point that it is permanent,
and the severity is such that the Insured
Person requires a blood transfusion at least monthly over at least
six (6) consecutive months. The diagnosis of Primary
Myelofibrosis must be supported by bone marrow biopsy and
confirmed by a registered Medical Practitioner who is a specialist.
Secondary Myelofibrosis is excluded.
23. Carcinoma-In-Situ(Cis) / Early Stage Cancer
Carcinoma -in-situ
Carcinoma-in-situ shall mean a histologically proven, localized
pre-invasion lesion where cancer cells have not yet penetrated
the basement membrane or invaded (in the sense of infiltrating
and / or actively destroying) the surrounding tissues or stroma in
any one of the following covered organ groups, and subject to any
classification stated:
(a) breast, where the tumour is classified as Tis according to the
TNM Staging method;
(b) corpus uteri, vagina, vulva or fallopian tubes where the
tumour is classified as Tis according to the TNM Staging
method ;
(c) cervix uteri, classified as Tis according to the TNM Staging
method;
(d) ovary –include borderline ovarian tumours with intact
capsule, no tumour on the ovarian surface, classified as
T1aN0M0, T1bN0M0 (TMN Staging) or FIGO 1A, FIGO 1B
(e) Colon and rectum;
(f) Penis;
(g) Testis;
(h) Lung;
(i) Liver;
(j) Stomach and esophagus;
(k) Urinary tract, for the purpose of in-situ cancers of the
bladder, stage Ta of papillary carcinoma is included
(l) Nasopharynx
For purposes of this Policy, Carcinoma-in-situ must be confirmed
by a biopsy.
Pre-malignant lesions and Carcinoma-in-situ of any organ unless
listed above are excluded.
Early Stage Cancer
Early Stage Cancer shall mean the presence of one of the
following malignant conditions:
(i) Prostate tumour histologically described as TNM
Classification T1a or T1b or T1c or of another
equivalent or lesser classification.
(ii) Chronic lymphocytic leukaemia classified as RAI Stage I or
II;
(iii) Any malignant tumor of the thyroid, positively diagnosed with
histological confirmation and characterised by the uncontrolled
growth of malignant cells and invasion of tissue, which is
histologically classified as T1N0M0 according to the TNM
classification system, or another equivalent classification.
This benefit will be payable only when total thyroidectomy is
performed to treat this condition.
The Diagnosis must be based on histopathological features and
confirmed by a Pathologist. Pre-malignantlesions and conditions,
unless listed above, are excluded.
24. Necrotizing Fasciitis

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
The occurrence of necrotising fasciitis where the following
conditions are met:
(i) the usual clinical criteria of necrotising fasciitis are met;
and
(ii) the bacteria identified is a known cause of necrotising
fasciitis; and
(iii) there is widespread destruction of muscle and other
soft tissues that results in a total and permanent loss
of function of the affected body part.
The Unequivocal Diagnosis must be made by a Specialist in the
relevant medical field.
25. Idiopathic Scoliosis
Severe Idiopathic scoliosis with spinal curvature of more than 40
(forty) degrees Cobb angle where spinal surgery is necessitated
to correct idiopathic scoliosis (of unknown cause) in order to
restore the spinal cord to a normal vertical position.
Spinal deformity caused by congenital abnormalities and
neuromusclar diseases are excluded.
26. Dissolution of the nerve roots of Brachial Plexus
Permanent loss of sensory function of the upper limb caused by
the dissolution of 2 (two) or more brachial plexus nerve roots
caused by an accident or injury. The diagnosis must be confirmed
via electrodiagnostic tests performed by a consultant neurologist.
27. Optic Neuropathy
The Unequivocal Diagnosis of optic nerve atrophy affecting both
eyes leading to a permanent best corrected visual acuity of 6/60
or less on the Snellen Chart in both eyes. The optic nerve atrophy
and quantum of visual loss of sight must be certified by a
Specialist in the relevant medical field.
Optic nerve atrophy resulting from alcohol or drug abuse will be
excluded.
28. Wilson Disease
Wilson's disease is an inherited disorder that causes copper to
accumulate in your liver, brain and other vital organs. Following
criteria must be confirmed by a relevant specialist
1. Unequivocal diagnosis of Wilson’s Disease using relevant
blood tests, eye examination and other imaging techniques
2. Treatment of Wilsons disease with a chelating agent
documented for at least six(6) months
3. Diagnosis of liver cirrhosis based on abnormal liver
biochemistry and findings of the liver biopsy or Fibroscan/USG
liver
Liver disease secondary to alcohol and drug abuse is excluded.
29. Cardiac arrhythmia with surgical intervention
Procedures like Maze surgery, RF Ablation therapy or any
relevant procedure/surgery deemed absolutely necessary by a
cardiologist to treat life threatening arrhythmias. Diagnosis must
be evidenced by monitoring through a Holter monitor, event
monitor or loop recorder and should be confirmed by a consultant
cardiologist.
The following are excluded:
Cardio version and any other form of non-surgical
treatments
Claim arising due to Internal Congenital Anomalies
within 1 year from the date of commencement of cover
or revival of coverage, whichever occurs later.
30. Benign Spinal Cord Tumor with Neurological Deficit
Benign spinal cord tumor is defined as a life threatening, non-
cancerous tumor of the spinal cord or its meninges. The presence
of the underlying tumor must be confirmed by imaging studies
such as CT scan or MRI.
This spinal cord tumor must result in Permanent Neurological
deficit with persisting clinical symptoms for a continuous period of
at least 90 consecutive days and must be confirmed by the
relevant medical specialist. The Neurological deficit must result in
permanent inability to perform three or more Activities of Daily
Living.
Activities of Daily Living are defined as :
a. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
b. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
c. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
d. Mobility: the ability to move indoors from room to room
on level surfaces;
e. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain
a satisfactory level of personal hygiene;
f. Feeding: the ability to feed oneself once food has been
prepared and made available.
31. Facial Reconstructive Surgery due to accident
The actual undergoing of plastic or reconstructive surgery
(restoration or reconstruction of the shape and appearance of
facial structures above the neck which are defective, missing,
damaged due to Accident happened during the policy period)
which, in the opinion of a Specialist Medical Practitioner, is
deemed Medically Necessary for the treatment of facial
disfigurement due to Injury requiring in-patient treatment and
subsequently the performance of such surgery. Surgery solely for
cosmetic reasons, isolated dental restorations, isolated nasal
fractures or isolated skin wounds are excluded.
32. Pulmonary Artery Graft Surgery
The undergoing of surgery requiring median sternotomy (surgery
to divide the breastbone) on the advice of a Cardiologist for
disease of the pulmonary artery to excise and replace the
diseased pulmonary artery with a graft.
The following conditions are excluded:

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
o Pulmonary artery graft surgery necessitated as a result of
Coronary Artery Bypass Grafting
o Pulmonary artery graft surgery necessitated as a result of Post
trauma
33. Glomerulonephiritis with Nephrotic Syndrome
Primary or Secondary glomerulonephritis with Nephrotic
Syndrome for a continuous period of six (6) months.
The nephrotic syndrome is defined by the presence of all of the
below :
heavy proteinuria (protein excretion greater than 3.5
g/24 hours),
hypoalbuminemia (less than 3.0 g/dL),
peripheral edema.
The nephrotic syndrome must have continued for a period of at
least six (6) months with or without intervening periods of
remission and the life assured must have received treatment
regimen appropriate to the clinical presentation over the period of
time. Other forms of kidney disease are not covered.
34. Severe Acquired Or Secondary Pulmonary Alveolar
Proteinosis (PAP)
Pulmonary alveolar proteinosis (PAP)_ is a lung disorder
characterized by an abnormal accumulation of surfactant derived
lipoprotein compounds within the alveoli of the lung.
Only Secondary PAP is covered. The followings are excluded :
Autoimmune PAP
Genetic PAP / Congenital PAP
Secondary PAP must be confirmed by Certified Medical
Practitioner with evidence of the underlying cause and diagnosis
confirmed through any one of the following :
bronchoalveolar lavage fluid (BALF) staining ,
transbronchial lung biopsy
video-assisted thoracoscopic lung biopsy
35. Moderately Severe Kidney Disease
It means chronic renal insufficiency which meets all of the
following criteria :
(i) Creatinine Clearance corrected for body surface area
(CCr- corrected) is lower than 30mL/min/1.73 m2 and
this abnormality has been consistently documented for
at least ninety (90) consecutive calendar days; and
(ii) Such Unequivocal Diagnosis must be confirmed by a
Medical Practitioner who is an urologist or
nephrologist.
36. Moderately Severe Systemic Lupus Erythematous With
Lupus Nephritis
Means a multisystem autoimmune disorder, characterized by the
development of auto-antibodies.
All of the following criteria must be met:
(i) Presence of at least three (3) of the below five (5)
criteria;
a. Arthritis: non-erosive arthritis, involving two (2) or
more joints;
b. Serositis: pleuritis or pericarditis;
c. Renal Disorder: persistent proteinuria > 0.5 g per
day or cellular casts;
d. Hematologic disorder: hemolytic anemia,
Leukopenia, Lymphopenia, or thrombocytopenia; or
e. Positive anti-nuclear antibody, Anti-dsDNA or anti-
Smith antibody.
(ii) Such Unequivocal Diagnosis must be confirmed by a
Medical Practitioner who is a rheumatologist or
immunologist.
37. Syringomyelia or Syringobulbia Requiring Surgery
The unequivocal diagnosis of Syringomyelia or Syringobulbia with
evidence of a fluid-filled cavity or cyst found within the spinal cord
or brainstem resulting in neurological deficit for continuous period
of 3 months or more.
The insured must have undergone surgery for treatment of
Syringomyelia or Syringobulbia and the surgery must be certified
to be Medically Necessary by the relevant Medical Practitioner.
The following is excluded:
Congenital syringomyelia
38. Surgical removal of one lung
Complete surgical removal of the entire right or entire left lung
necessitated by an illness or an Accident of the Insured. The
surgery must be certified to be Medically Necessary by a Medical
Practitioner who is a pulmonologist or thoracic surgeon.
39. Moderately Severe Crohn's Disease
Crohn’s Disease is a chronic, transmural inflammatory disorder of
the bowel. For the purposes of this benefit, the Unequivocal
Diagnosis of Crohn's disease must be made by a Specialist in the
relevant medical field on the basis of an endoscopy and bowel
biopsy which confirms the Unequivocal Diagnosis of Crohn's
disease. The condition must require continuous
immunosuppressive treatment or continuous treatment with
immunomodulating drugs/steriod under the direction of a
Specialist in the relevant medical field for a period of at least six
(6) consecutive months
40. Moderately Severe Ulcerative Colitis
Ulcerative Colitis shall mean acute ulcerative colitis with life
threatening electrolyte disturbances usually associated with
intestinal distention and a risk of intestinal rupture. For the
purpose of Unequivocal Diagnosis, there must be biopsy

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
evidence which unequivocally confirms the presence of ulcerative
colitis and there must be imaging or endoscopic evidence that the
condition involves the entire colon.
For the purposes of this benefit, there must be a requirement for
ongoing systemic immunosuppression therapy or
immunomodulatory therapy for a period of at least six (6)
consecutive months supervised by a Specialist in
gastroenterology.
Other forms of inflammatory colitis are specifically excluded.
Ulcerative colitis confined to the rectum is specifically excluded.
41. Small Bowel Transplant
The actual undergoing of surgery to replace a diseased or
shortened small bowel (intestine) of the insured with a healthy
bowel to treat intestinal failure.
The surgery must be certified to be Medically Necessary by a
relevant Medical Practitioner.
42. Adrenalectomy for Adrenocortical Adenoma
Adrenalectomy for treatment of malignant systemic hypertension
that was secondary to an aldosterone secreting adrenal
adenoma. Malignant hypertension was uncontrolled by medical
therapy. The adrenalectomy must be considered Medically
Necessary for the management of poorly controlled hypertension
by a Specialist in the relevant medical field
43. Spinal Stroke
Death of spinal cord tissue due to inadequate blood supply or
haemorrhage within the spinal canal resulting in neurological
deficit with persisting clinical symptoms.
Evidence of
permanent neurological deficit lasting for at least 3
months has to be produced.Diagnosis has to be
confirmed by a
specialist medical practitioner and evidenced by typical clinical
symptoms as well as typical findings in CT Scan or MRI.
44. Portal Vein Thrombosis
The unequivocal diagnosis of Portal Vein Thrombosis evidenced
by the complete or partial obstruction of blood flow in the portal
vein. The diagnosis must be made by a specialist through doppler
ultrasonography, CT Scans , MRI or angiography requiring
surgical thrombectomy on an inpatient basis.
The surgery must be certified to be Medically Necessary by a
relevant Medical Practitioner.
45. Surgical Removal of One Kidney
The actual undergoing of surgical removal of one kidney due to
diseases or trauma of the kidney. The surgery must be considered
Medically Necessary by a Medical Practitioner who is a
nephrologist.
Removal of kidney as a donor or due to congenital kidney
condition including renal agenesis and non functioning kidney is
excluded
46. Severe Progressive Bulbar Palsy
Neurological disorder with paralysis in the head region, difficulties
in chewing and swallowing, problems in speaking, persistent
signs of involvement of the spinal nerves and the motor centres
in the brain and spastic weakness and atrophy of the muscles of
the extremities. The disease must be Unequivocally Diagnosed
by a Medical Practitioner who is a neurologist. The condition must
result in the permanent inability to perform, without assistance, at
least three (3) of the six (6) Activities of Daily Living. These
conditions have to be medically documented for at least three (3)
consecutive months.
The Activities of Daily Living are:
I. Washing: the ability to wash in the bath or shower
(including getting into
and out of the bath or shower) or
wash satisfactorily by other means;
II. Dressing: the ability to put on, take off, secure and
unfasten all garments
and, as appropriate, any braces,
artificial limbs or other surgical
appliances;
III. Transferring: the ability to move from a bed to an upright
chair or
wheelchair and vice versa;
IV. Mobility: the ability to move indoors from room to room on
level surfaces;
V. Toileting: the ability to use the lavatory or otherwise
manage bowel and
bladder functions so as to maintain
a satisfactory level of personal
hygiene;
VI. Feeding: the ability to feed oneself once food has
been prepared and
made available.
47. Coma 72 hours
A state of unconsciousness with no reaction or response to
external stimuli or
internal needs. This diagnosis must be
supported by evidence of all of the
following:
I. No response to external stimuli continuously for at least 72
hours;
II. Life support measures are necessary to sustain life; and
III. Permanent neurological deficit which must be assessed
at least 30 days
after the onset of the coma.
The condition has to be confirmed by a specialist medical
practitioner. Coma
resulting directly from alcohol or drug abuse is
excluded.
48. Moderately Severe Cardiomyopathy
The unequivocal Diagnosis of cardiomyopathy which has resulted
in the presence of permanent physical impairments to at least
Class III of the New York Heart Association (NYHA) classification
of Cardiac Impairment.
The Diagnosis must be confirmed by a Specialist in the relevant
field. Cardiomyopathy that is directly related to alcohol misuse is
excluded.
The NYHA Classification of Cardiac Impairment:
Class I: No limitation of physical activity. Ordinary physical activity
does not cause undue fatigue, dyspnea, or anginal pain.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Class II: Slight limitation of physical activity. Ordinary physical
activity results in symptoms.
Class III: Marked limitation of physical activity. Comfortable at
rest, but less than ordinary activity causes symptoms.
Class IV: Unable to engage in any physical activity without
discomfort. Symptoms may be present even at rest.
49. Other Serious Coronary Artery Diseases
Severe coronary artery disease in which at least three (3) major
coronary arteries are individually occluded by a minimum of sixty
percent (60%) or more, as proven by coronary angiogram only
(non-invasive diagnostic procedures excluded).
For purposes of this definition, “major coronary artery” refers to
any of the left main stem artery, left anterior descending artery,
circumflex artery and right coronary artery (but not including their
branches).
50. Insertion of a Permanent Cardiac Defibrillator
Insertion of a permanent cardiac defibrillator as a result of
cardiac arrhythmia which cannot be treated via any other
method. The surgical procedure must be certified to be
medically necessary by a specialist in the relevant field.
Documentary evidence of cardiac arrhythmia must be
provided.
51. Pericardiectomy
The undergoing of a pericardiectomy performed by open
heart surgery or keyhole techniques as a result of pericardial
disease. The surgical procedures must be certified to be
medically necessary by a consultant cardiologist.
The following are excluded:
Other procedures on the pericardium including pericardial
biopsies and pericardial drainage procedures by needle
aspiration.
52. Balloon Valvotomy or Valvuloplasty
The actual undergoing of Valvotomy or Valvuloplasty
necessitated by damage of the heart valve as confirmed by a
specialist in the relevant field and established by a cardiac
echocardiogram or any other appropriate diagnostic test that
is available.
The following are excluded:
Procedures done for treatment of Congenital Heart Disease
within 4 years from the date of commencement of cover or
revival of coverage, whichever occurs later.
53. Minimally Invasive Surgery to Aorta
The actual undergoing of minimally invasive surgical repair
(i.e. via percutaneous intra-arterial route) of a diseased
portion of an aorta to repair or correct an aneurysm,
narrowing, obstruction or dissection of the aorta. For the
purpose of this definition, aorta shall mean the thoracic and
abdominal aorta but not its branches.
The following are excluded:
Claim arising due to Internal Congenital Anomalies
within 4 years from the date of commencement of cover
or revival of coverage, whichever occurs later.
54. Loss of Hearing of One Ear
Total and irreversible loss of hearing in one ear as a result of
illness or accident. This diagnosis must be supported by pure tone
audiogram test and certified by an Ear, Nose and Throat (ENT)
specialist.
Total means “the loss of hearing to the extent that the loss is
greater than 90decibels across all
frequencies of hearing” in one ear.
55. Loss Of Sight In One Eye
Total, permanent and irreversible loss of all vision in one eye as
a result of illness or accident.
The Blindness is evidenced by:
I. corrected visual acuity being 3/60 or less in one eye
or;
II. the field of vision being less than 10 degrees in one
eye.
The diagnosis of blindness must be confirmed and must not be
correctable by aids or surgical procedure.
56. Carotid Artery Surgery
The actual undergoing of surgery to the Carotid Artery to treat
carotid artery stenosis of fifty percent (50%) or above, as proven
by angiographic evidence, of one (1) or more carotid arteries.
Both criteria (a) and (b) below must be met:
a) Either:
i). Actual undergoing of endarterectomy to alleviate the
symptoms; or
ii). Actual undergoing of an endovascular intervention
such as angioplasty and/or stenting or atherectomy to
alleviate the symptoms; and
b) The Diagnosis and medical necessity of the treatment must be
confirmed by a Registered Medical Practitioner who is a specialist
in the relevant field.
57. Loss of Use of One Limb
Total and irreversible loss of use of one or more limbs as a result
of injury or disease of the brain or spinal cord. A specialist medical
practitioner must be of the opinion that the paralysis will be
permanent with no hope of recovery and must be present for more
than 3 months.
58. MYOCARDIAL INFARCTION (First Heart Attack of
specific severity)

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
I. The first occurrence of heart attack or myocardial
infarction, which means the death of a portion of the heart
muscle as a result of inadequate blood supply to the
relevant area.
The diagnosis for Myocardial Infarction should be
evidenced by all of the following criteria:
1. A history of typical clinical symptoms consistent
with the diagnosis of acute myocardial infarction
(For e.g. typical chest pain)
2. New characteristic electrocardiogram changes
3. Elevation of infarction specific enzymes, Troponins
or other specific biochemical markers.
II. The following are excluded:
1. Other acute Coronary Syndromes
2. Any type of angina pectoris
3. A rise in cardiac biomarkers or Troponin T or I in
absence of overt ischemic heart disease OR
following an intra-arterial cardiac procedure.
59. REFRACTORY HEART FAILURE
Refractory heart failure is defined as a systolic dysfunction
that does not respond to optimal medical therapy (“triple
therapy”) and results in permanent physical impairment to
the degree of New York Heart Association Classification
Class IV, or its equivalent, for at least six months. The
diagnosis of refractory heart failure has to be supported by
echocardiographic findings of compromised ventricular
performance. The diagnosis must be made by a cardiology
specialist.
The following is excluded:
1. Reversible causes of heart failure such as
hypocalcemia, alcohol abuse, thyroid, anaemia.
60. END STAGE LUNG FAILURE
I. End stage lung disease, causing chronic respiratory
failure, as confirmed and evidenced by all of the
following:
1. FEV1 test results consistently less than 1 litre
measured on 3 occasions 3 months apart; and
2. Requiring continuous permanent supplementary
oxygen therapy for hypoxemia; and
3. Arterial blood gas analysis with partial oxygen
pressure of 55mmHg or less (PaO2 < 55mmHg);
and
4. Dyspnoea at rest.
61. PRIMARY (IDIOPATHIC) PULMONARY HYPERTENSION
I. An unequivocal diagnosis of Primary (Idiopathic)
Pulmonary Hypertension by a Cardiologist or specialist
in respiratory medicine with evidence of right ventricular
enlargement and the pulmonary artery pressure above
30 mm of Hg on Cardiac Cauterization. There must be
permanent irreversible physical impairment to the
degree of at least Class IV of the New York Heart
Association Classification of cardiac impairment.
II. The NYHA Classification of Cardiac Impairment are as
follows:
1. Class III: Marked limitation of physical activity.
Comfortable at rest, but less than ordinary activity
causes symptoms.
2. Class IV: Unable to engage in any physical activity
without discomfort. Symptoms may be present
even at rest.
III. Pulmonary hypertension associated with lung disease,
chronic hypoventilation, pulmonary thromboembolic
disease, drugs and toxins, diseases of the left side of the
heart, congenital heart disease and any secondary
cause are specifically excluded
62. END STAGE LIVER FAILURE
I. Permanent and irreversible failure of liver function that
has resulted in all three of the following:
1. Permanent jaundice; and
2. Ascites; and
3. Hepatic encephalopathy.
II. Liver failure secondary to drug or alcohol abuse is
excluded.
63. MULTIPLE SCLEROSIS WITH PERSISTING SYMPTOMS
I. The unequivocal diagnosis of Definite Multiple Sclerosis
confirmed and evidenced by all of the following:
1. Investigations including typical MRI findings which
unequivocally confirm the diagnosis to be multiple
sclerosis and
2. There must be current clinical impairment of motor
or sensory function, which must have persisted for
a continuous period of at least 6 months.
II. Other causes of neurological damage such as SLE and
HIV are excluded.
64. MOTOR NEURON DISEASE WITH PERMANENT
SYMPTOMS
I. Motor neuron disease diagnosed by a specialist medical
practitioner as spinal muscular atrophy, progressive bulbar
palsy, amyotrophic lateral sclerosis or primary lateral
sclerosis. There must be progressive degeneration of
corticospinal tracts and anterior horn cells or bulbar
efferent neurons. There must be current significant and
permanent functional neurological impairment with
objective evidence of motor dysfunction that has persisted
for a continuous period of at least 3 months.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
65. PERMANENT PARALYSIS OF LIMBS
Total and irreversible loss of use of two or more limbs as
a result of injury or disease of the brain or spinal cord. A
specialist medical practitioner must be of the opinion that
the paralysis will be permanent with no hope of recovery
and must be present for more than 3 months.
66. STROKE RESULTING IN PERMANENT SYMPTOMS
I. Any cerebrovascular incident producing permanent
neurological sequelae. This includes infarction of brain
tissue, thrombosis in an intracranial vessel, haemorrhage
and embolisation from an extracranial source. Diagnosis
has to be confirmed by a specialist medical practitioner
and evidenced by typical clinical symptoms as well as
typical findings in CT Scan or MRI of the brain. Evidence
of permanent neurological deficit lasting for at least 3
months has to be produced.
II. The following are excluded:
1. Transient ischemic attacks (TIA)
2. Traumatic injury of the brain
3. Vascular disease affecting only the eye or optic
nerve or vestibular functions.
67. COMA OF SPECIFIED SEVERITY
I. A state of unconsciousness with no reaction or response
to external stimuli or internal needs. This diagnosis must
be supported by evidence of all of the following:
1. No response to external stimuli continuously for at
least 96 hours;
2. Life support measures are necessary to sustain life;
and
3. Permanent neurological deficit which must be
assessed at least 30 days after the onset of the
coma.
II. The condition has to be confirmed by a specialist medical
practitioner. Coma resulting directly from alcohol or drug
abuse is excluded.
68. ALZEIMER’S DISEASE
Progressive and permanent deterioration of memory and
intellectual capacity as evidenced by accepted standardised
questionnaires and cerebral imaging.
The diagnosis of Alzheimer’s Disease must be confirmed by
an appropriate consultant and supported by a Medical
Practitioner appointed by Us. There must be significant
reduction in mental and social functioning requiring the
continuous supervision of the Insured Person. There must
also be an inability of the Insured Person to perform
(whether aided or unaided) at least three of the Activities of
Daily Living, for a continuous period of at least 3 months:
For the purpose of this clause, Activities of Daily Living are
defined as:
1. Washing – the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;
2. Dressing – the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
3. Transferring – the ability to move from a bed to an
upright chair or wheelchair and vice versa;
4. Toileting – the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain
a satisfactory level of personal hygiene;
5. Feeding – the ability to feed oneself once food has
been prepared and made available.
6. Mobility - the ability to move from room to room without
requiring any physical assistance.
The following are excluded:
• Any other type of irreversible organic
disorder/dementia
• Alcohol-related brain damage.
69. PARKINSON’S DISEASE
I. The occurrence of Parkinson’s Disease where there is an
associated Neurological Deficit that results in permanent inability
to perform independently at least three of the Activities of Daily
Living, for a continuous period of at least 3 months:
For the purpose of this clause, Activities of Daily Living are
defined as:
1. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means
2. Dressing: the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
3. Transferring: the ability to move from a bed to an upright
chair or wheelchair and vice versa;
4. Mobility: the ability to move indoors from room to room on
level surfaces;
5. Toileting: the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain a
satisfactory level of personal hygiene;
6. Feeding: the ability to feed oneself once food has been
prepared and made available.
The following is excluded:
Parkinson’s Disease accompanied with drug and/or alcohol
abuse.
70. APALLIC SYNDROME
Universal non-functioning of the brain cortex, with the brain
stem intact. Diagnosis of Apallic Syndrome must be
definitely confirmed by a registered Medical Practitioner who
is also a neurologist and substantiated by clinical and
investigation findings. This condition must be documented
for a continuous period of at least one month.

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
71. BENIGN BRAIN TUMOR
I. Benign brain tumor is defined as a life threatening, non-
cancerous tumor in the brain, cranial nerves or meninges
within the skull. The presence of the underlying tumor
must be confirmed by imaging studies such as CT scan
or MRI.
II. This brain tumor must result in at least one of the
following and must be confirmed by the relevant medical
specialist.
1. Permanent Neurological deficit with persisting
clinical symptoms for a continuous period of at least
90 consecutive days or
2. Undergone surgical resection or radiation therapy
to treat the brain tumor.
III. The following conditions are excluded:
Cysts, Granulomas, malformations in the arteries or
veins of the brain, hematomas, abscesses, pituitary
tumors, tumors of skull bones and tumors of the spinal
cord.
72. CREUTZFELDT-JAKOB DISEASE (CJD)
A diagnosis of Creutzfeldt Jakob Disease must be made by
a specialist Medical Practitioner who is a neurologist and the
diagnosis must be substantiated by CSF examination, EEG,
CT Brain and MRI of the brain. There must be permanent
clinical loss of the ability in mental, physical and social
functioning for a minimum period of 30 days to the extent
that permanent supervision or assistance by a third party is
required.
73. MAJOR HEAD TRAUMA
I. Accidental head injury resulting in permanent
Neurological deficit to be assessed no sooner than 3
months from the date of the accident. This diagnosis must
be supported by unequivocal findings on Magnetic
Resonance Imaging, Computerized Tomography, or other
reliable imaging techniques. The accident must be caused
solely and directly by accidental, violent, external and
visible means and independently of all other causes
II. The Accidental Head injury must result in an inability to
perform at least three (3) of the following Activities of Daily
Living either with or without the use of mechanical
equipment, special devices or other aids and adaptations
in use for disabled persons. For the purpose of this Benefit,
the word “permanent” shall mean beyond the scope of
recovery with current medical knowledge and technology.
III. The Activities of Daily Living are:
I. Washing: the ability to wash in the bath or shower
(including getting into and out of the bath or
shower) or wash satisfactorily by other means;
II. Dressing: the ability to put on, take off, secure
and unfasten all garments and, as appropriate,
any braces, artificial limbs or other surgical
appliances;
III. Transferring: the ability to move from a bed to an
upright chair or wheelchair and vice versa;
IV. Mobility: the ability to move indoors from room to
room on level surfaces;
V. Toileting: the ability to use the lavatory or
otherwise manage bowel and bladder functions
so as to maintain a satisfactory level of personal
hygiene;
VI. Feeding: the ability to feed oneself once food has
been prepared and made available.
IV. The following are excluded:
i. Spinal cord injury;
74. KIDNEY FAILURE REQUIRING REGULAR DIALYSIS
I. End stage renal disease presenting as chronic irreversible
failure of both kidneys to function, as a result of which
either regular renal dialysis (haemodialysis or peritoneal
dialysis) is instituted or renal transplantation is carried out.
Diagnosis has to be confirmed by a specialist medical
practitioner.
75. MEDULLARY CYSTIC DISEASE
I. Medullary Cystic Disease where the following criteria are
met:
i. The presence in the kidney of multiple cysts in the
renal medulla accompanied by the presence of
tubular atrophy and interstitial fibrosis;
ii. Clinical manifestations of anaemia, polyuria, and
progressive deterioration in kidney function; and
iii. The diagnosis of Medullary Cystic Disease is
confirmed by renal biopsy along with specialist
Medical Practitioner opinion.
II. The following are excluded
i. Isolated or benign kidney cysts are specifically
excluded from this Benefit
ii. Any condition is which cysts are absent
76. MUSCULAR DYSTROPHY
Diagnosis of muscular dystrophy by a registered Medical
Practitioner who is a neurologist based on the presence of
following conditions:
1. Clinical presentation including weakness and loss of
muscle mass, absence of sensory disturbance, normal
cerebrospinal fluid and mild tendon reflex reduction;
2. Characteristic electromyogram
3. Clinical suspicion confirmed by muscle biopsy.
The condition must result in the inability of the Insured Person
to perform (whether aided or unaided) at least three of the
Activities of Daily Living, for a continuous period of at least 6
months.
For the purpose of this clause, Activities of Daily Living are
defined as:
1. Washing – the ability to wash in the bath or shower
(including getting into and out of the bath or shower) or
wash satisfactorily by other means;

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
2. Dressing – the ability to put on, take off, secure and
unfasten all garments and, as appropriate, any braces,
artificial limbs or other surgical appliances;
3. Transferring – the ability to move from a bed to an upright
chair or wheelchair and vice versa;
4. Toileting – the ability to use the lavatory or otherwise
manage bowel and bladder functions so as to maintain a
satisfactory level of personal hygiene;
5. Feeding – the ability to feed oneself once food has been
prepared and made available.
6. Mobility - the ability to move from room to room without
requiring any physical assistance
77. POLIOMYELITIS
The occurrence of Poliomyelitis, where the following
conditions are met:
I. Poliovirus is identified as the cause through
laboratory investigation
II. Paralysis of the limb muscles or respiratory
muscles must be present and persist for at least
3 months.
The diagnosis of Poliomyelitis must be confirmed by a
registered Medical Practitioner who is a neurologist.
78. APLASTIC ANEMIA
Irreversible persistent bone marrow failure which results in
anaemia, neutropenia and thrombocytopenia requiring
treatment with at least two (2) of the following:
1. Blood product transfusion;
2. Marrow stimulating agents;
3. Immunosuppressive agents; or
4. Bone marrow transplantation.
The diagnosis of Aplastic anaemia must be confirmed by a
bone marrow biopsy. Atleast two of the following values
should be present:
1. Absolute Neutrophil count of 500 per cubic
millimetre or less;
2. Absolute Reticulocyte count of 20,000 per cubic
millimetre or less; and
3. Platelet count of 20,000 per cubic millimetre or less.
79. Systemic lupus erythematosus (SLE) with renal
involvement
I. Multi-system, autoimmune disorder characterized by the
development of auto-antibodies, directed against various
self-antigens. For purposes of the definition of “SLE”
under this policy is restricted to only those forms of
systemic lupus erythematosus, which involve the
kidneys and are characterized as Class III, Class IV,
Class V or Class VI lupus nephritis under the
Abbreviated International Society of Nephrology/Renal
Pathology Society (ISN/RPS) classification of lupus
nephritis (2003) below based on renal biopsy.
Diagnosis by a nephrologist, supported by renal biopsy
report is mandatory. There must be positive antinuclear
antibody test
II. The following are excluded
i. Other forms such as discoid lupus, and those forms
with only hematological and joint involvement are
specifically excluded.
ii. Class I - Minimal mesangial lupus nephritis
iii. Class II - Mesangial proliferative lupus nephritis
80. MYASTHENIA GRAVIS
I. An acquired autoimmune disorder of neuromuscular
transmission leading to fluctuating muscle weakness
and fatigability, where all of the following criteria are met:
1. Presence of permanent muscle weakness
categorized as Class IV or V according to the
Myasthenia Gravis Foundation of America Clinical
Classification below; and
2. The diagnosis of Myasthenia Gravis and
categorization are confirmed by a registered
Medical Practitioner who is a neurologist.
Myasthenia Gravis Foundation of America Clinical
Classification is as follows:
Class I: Any eye muscle weakness, possible ptosis, no
other evidence of muscle weakness elsewhere.
Class II: Eye muscle weakness of any severity, mild
weakness of other muscles.
Class III: Eye muscle weakness of any severity,
moderate weakness of other muscles.
Class IV: Eye muscle weakness of any severity, severe
weakness of other muscles.
Class V: Intubation needed to maintain airway.
II. The following are excluded:
1. Congenital myasthenic syndrome
2. Transient neonatal or juvenile myasthenia gravis
81. SCLERODERMA
A systemic collagen-vascular Illness causing progressive
diffuse fibrosis in the skin, blood vessels and visceral
organs. This diagnosis must be unequivocally supported by
biopsy and serological evidence and the disorder must have
reached systemic proportions to involve the heart, lungs or
kidneys.
The following conditions are excluded:
1. Localised scleroderma (linear scleroderma or
morphea);
2. Eosinophilic fascitis; and
3. CREST syndrome.
82. GOOD PASTURES SYNDROME with lung or renal
involvement

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Goodpastures Syndrome is an autoimmune disease in
which antibodies attack the lungs and kidneys, leading to
permanent lung and kidney damage. The permanent
damage should be for continuous period of at least 30 days.
The diagnosis must be proven by kidney biopsy and
confirmed by a specialist Medical Practitioner who is a
rheumatologist.
83. BLINDNESS
I. Total, permanent and irreversible loss of all vision in both
eyes as a result of illness or accident.
II. The Blindness is evidenced by:
1. Corrected visual acuity being 3/60 or less in both
eyes or ;
2. The field of vision being less than 10 degrees in
both eyes.
III. The diagnosis of blindness must be confirmed and must
not be correctable by aids or surgical procedure.
84. DEAFNESS
I. Total and irreversible loss of hearing in both ears as a
result of illness or accident. This diagnosis must be
supported by pure tone audiogram test and certified by
an Ear, Nose and Throat (ENT) specialist. Total means
“the loss of hearing to the extent that the loss is greater
than 90 decibels across all frequencies of hearing” in
both ears.
85. CANCER OF SPECIFIED SEVERITY
I. A malignant tumor characterized by the uncontrolled
growth and spread of malignant cells with invasion and
destruction of normal tissues. This diagnosis must be
supported by histological evidence of malignancy. The term
cancer includes leukemia, lymphoma and sarcoma.
II. The following are excluded –
1. All tumors which are histologically described as
carcinoma in situ, benign, pre-malignant,
borderline malignant, low malignant potential,
neoplasm of unknown behaviour, or non-invasive,
including but not limited to: Carcinoma in situ of
breasts, Cervical dysplasia CIN-1, CIN -2 and CIN-
3.
2. Any non-melanoma skin carcinoma unless there is
evidence of metastases to lymph nodes or beyond;
3. Malignant melanoma that has not caused invasion
beyond the epidermis;
4. All tumors of the prostate unless histologically
classified as having a Gleason score greater than
6 or having progressed to at least clinical TNM
classification T2N0M0
5. All Thyroid cancers histologically classified as
T1N0M0 (TNM Classification) or below;
6. Chronic lymphocytic leukaemia less than RAI stage
3
7. Non-invasive papillary cancer of the bladder
histologically described as TaN0M0 or of a lesser
classification,
8. All Gastro-Intestinal Stromal Tumors histologically
classified as T1N0M0 (TNM Classification) or
below and with mitotic count of less than or equal
to 5/50 HPFs;
9. All tumors in the presence of HIV infection.
86. THIRD DEGREE BURNS
There must be third-degree burns with scarring that cover at
least 20% of the body’s surface area. The diagnosis must
confirm the total area involved using standardized, clinically
accepted, body surface area charts covering 20% of the
body surface area.
87. LOSS OF SPEECH
I. Total and irrecoverable loss of the ability to speak as a
result of injury or disease to the vocal cords. The inability
to speak must be established for a continuous period of
12 months. This diagnosis must be supported by medical
evidence furnished by an Ear, Nose, throat (ENT)
specialist.
II. All psychiatric related causes are excluded.
88. OPEN HEART REPLACEMENT OR REPAIR OF HEART
VALVES
I. The actual undergoing of open-heart valve surgery is to replace
or repair one or more heart valves, as a consequence of defects
in, abnormalities of, or disease affected cardiac valve(s). The
diagnosis of the valve abnormality must be supported by an
echocardiography and the realization of surgery has to be
confirmed by a specialist medical practitioner. Catheter based
techniques including but not limited to, balloon
valvotomy/valvuloplasty are excluded.
89. Major Organ Transplant
I. The actual undergoing of a transplant of:
i. One of the following human organs: heart, lung, liver, kidney,
pancreas, that resulted from irreversible end-stage failure of the
relevant organ,
II. The following are excluded:.
i. Where only islets of Langerhans are transplanted.
90. BONE MARROW TRANSPLANT
The actual undergoing of a transplant of:
Human bone marrow using haematopoietic stem cells. The
undergoing of a transplant has to be confirmed by a specialist
medical practitioner.
II. The following are excluded:

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Other stem-cell transplants
91. OPEN CHEST CABG
I. The actual undergoing of heart surgery to correct blockage or
narrowing in one or more coronary artery(s), by coronary artery
bypass grafting done via a sternotomy (cutting through the breast
bone) or minimally invasive keyhole coronary artery bypass
procedures. The diagnosis must be supported by a coronary
angiography and the realization of surgery has to be confirmed by
a cardiologist.
II. The following are excluded:
I. Angioplasty and/or any other intra-arterial procedures
92. Angioplasty
I. Coronary Angioplasty is defined as percutaneous coronary
intervention by way of balloon angioplasty with or without
stenting for treatment of the narrowing or blockage of
minimum 50 % of one or more major coronary arteries. The
intervention must be determined to be medically necessary
by a cardiologist and supported by a coronary angiogram
(CAG)
II. Coronary arteries herein refer to left main stem, left anterior
descending, circumflex and right coronary artery.
III. Diagnostic angiography or investigation procedures
without angioplasty/stent insertion are excluded.
Annexure 2
Final Major Surgical Procedures List
Payout
Open Heart Replacement Or Repair Of Heart
Valves
100%
Valvotomy/Valvuloplasty
50%
CABG (Coronary Artery Bypass Grafting)
100%
Other vascular bypass grafts( eg. Femoral
popliteal grafts)
50%
Clipping or repair of Aneurysm(including aortic,
cerebral, femoral or iliac ) with or without graft
50%
Coronary Angioplasty with Stent implantation
50% -inr
5lac
which
ever
lower
Excision of benign mediastinal lesions (evidence
of thoracotomy needs to be ascertained)
50%
Heart Proximal aortic aneurysm, Aortic root
transplantation with coronary artery
reimplantation
50%
Initial implantation of permanent
pacemaker/ICD/VAD device in heart
50%
Major Surgery of Aorta
100%
Major vein repair with or without grafting for
traumatic & non traumatic lesions
50%
Pericardiotomy / Pericardectomy
50%
Carotid endarterectomy/ Ext carotid Int. carotid
bypass/Carotid tumour excision
50%
Closure Of Semilunar Valve
50%
Minimally Invasive Surgery to Aorta
50%
Pulmonarry Artery Graft
50%
Cardiac Arrhythmia with Ablative Procedure
50%-
capping
of 5lac
Hemicolectomy
50%
Partial Gastrectomy
50%
Complete Gastrectomy
100%
Partial Eosophagectomy
50%
Complete Eosophagectomy
100%
Pancrepancreaticoduodenectomy- Whipples
surgery
100%
Partial Hepatectomy
50%
Complete Hepatectomy
100%
Partial splenectomy
50%
Complete splenectomy
100%
small bowel transplant
50%
Resection/anastamosis for small intestine
50%
Partial Pancreatectomy
50%
Complete Pancreatectomy
100%
Amputation of arm
100%
Amputation of foot
100%
Amputation of hand
100%
Amputation of leg
100%
Excision reconstruction of joint(small joints-hand
& feet)
50%-cap
of 2lac
microvascular replantation of finger due to trauma
50%-cap
of 2lac
Implantation of prosthesis for limb for amputees
100%
Open/closed Reduction and Internal fixation of
fracture Long bone (Humerus, Radius, ulna,
Femur, Tibia, Fibula, clavicle) with or without
Bone grafting-
50%-cap
3lac
Osteomyelitis - Surgical Drainage and Curettage
50%-cap
of 2lac
core decompression with graft for osteonecrosis
of femoral head
50%
Replantation of lower limb
100%
Replantation of upper limb
100%
Spinal Fusion (arthrodesis of spine with bone
graft/internal fixation)
50%
Therapeutic endoscopic operations on cavity of
knee/hip joint
50%-cap
of 2lac
Therapeutic endoscopic operations on cavity of
Shoulder/elbow joint
50%-cap
of 2lac
ACL/PCL repair/reconstruction
50%-cap
of 2lac
Total replacement of
hip/knee/shoulder/elbow/head of femur/head of
humerus-unilateral
50%
reconstruction or arthroplasty of
hip/knee/shoulder/elbow/head of femur/head of
humerus(unilateral/bilateral)
50%

ICICI Lombard General Insurance Company Limited
IRDA Reg. No. 115 CIN: L67200MH2000PLC129408 UIN : ICIHLIP22131V012122 ICICI Lombard Criti Shield Plus
Mailing Address: Registered Office Address: Toll free no : 1800 2666
601 & 602, 6th Floor, Interface 16, ICICI Lombard House, 414, Veer Savarkar Marg, Alternate no : 86552 22666 (chargeable)
New Linking Road, Malad (West) Near Siddhi Vinayak Temple, Prabhadevi, E-mail : customersupport@icicilombard.com
Mumbai - 400 064 Mumbai 400 025 Website : www.icicilombard.com
Total replacement of
hip/knee/shoulder/elbow/head of femur/head of
humerus-bilateral
100%
HIND QUARTER AMPUTATION
100%
Open Reduction And Internal Fixation Of
Fracture Of Small Bones /patella With Or Without
Graft
50%-cap
to 1lac
Prosthetic Replacement of small joints
50%-cap
to 2lac
Multiple (more than 2)Tendon Transfer - Sts Hand
/ Foot
50%
Surgery for Idiopathic Scoilosis
50%
Bur-hole Drainage of Extradural, subdural or
intracerebral space
50%
Craniotomy for non malignant space occupying
lesions
100%
Craniotomy for Drainage of Extradural, subdural
or intracerebral space
100%
Craniotomy for malignant Brain tumors
100%
Decompression surgery for Entrapment
Syndrome
100%
Embolectomy / Thrombectomy/ Endarterectomy
with or without Graft
100%
Excision of deep seated peripheral nerve tumor
100%
Excision of pineal gland
100%
Fixation of fracture of spine
100%
Free Fascia Graft for Facial Nerve Paralysis
50%
Intracranial transection of Cranial nerve
100%
Laminectomy/Discectomy for Spinal nerve root
decompression
100%
Microvascular decompression of cranial
nerves/nervectomy
100%
Multiple Microsurgical Repair of digital nerve
100%
Operations on Subarachnoid space of brain
100%
Other operations on the meninges of the Brain
100%
Peripheral nerve Graft
100%
Repair of Cerebral or Spinal Arterio- Venous
Malformations or aneurysms
100%
Total or Partial Excision of the pituitary gland - Any
approach (Transforntal or Trans Sphenoid)
100%
Surgery for ACOUSTIC NEUROMA
50%
Brachial Plexus Surgery
50%
neuro endoscopy for removal of brain tumor/
foreign body
50%
STA MCA BYPASS SURGERY
50%
SYMPATHECTOMY
CERVICAL/LUMBAR/THORACOLUMBAR
50%
Bone Marrow transplant (as recipient)
100%
Heart/Heart-Lung Transplant
100%
Liver Transplantation
100%
Lung Transplantation
100%
Renal transplant (recipient)
100%
Pancrease Transplant
100%
Major reconstructive oro-maxillafacial surgery due
to trauma or burns and not for cosmetic purpose
100%
Osteotomy including segmental resection with
bone grafting for Mandibular and maxillary lesions
100%
Commando Operation-for only cancer
100%
Total Larygectomy And Neck Dissection And
Flap-only for cancer
100%
Excision and Major Flap Repair of skin and
Subcutaneous tissue due to Major Burns
100%
Surgical treatment of cancer with removal of
organ & excluding biopsy & other diagnostics
100%
Surgical removal of an eye ball
50%
Surgical treatment of cancer without removal of
organ excluding biopsy & other diagnostics
50%
THYMECTOMY
50%
Amputation of penis
50%
Excision of ureter
50%
Total excision of bladder
50%
Partial nephrectomy due to medical advice (not
as a transplant donor)
50%
Total nephrectomy due to medical advice (not as
a transplant donor)
100%
Bilateral excision of testes
50%
Urinary diversion
50%
Adrenelectomy
50%
Pneumonectomy/Lobectomy/removal of 1 lung
50%
Pleurectomy/lung decortication
50%
Chronic bronchopleural fistula requiring a surgical
procedure for closure of the fistula through an
open thoracotomy
50%
pulmonary embolectomy/enderectomy
50%
