
2023 Beeson Annual Meeting
November 15 – 17, 2023
Program Book - Table of Contents
Agenda
Hyatt Regency Tamaya Hotel Maps and Wifi Instructions
Beeson Scholars’ Meeting Mentor Assignments
Clin-STAR – Beeson ‘Office (half) Hour’ Assignments
Datablitz! Assignments
Consultancy Assignments
Aims Page Workshop Assignments
Poster Session Small Group Assignments and Poster Abstracts
Thursday Dinner Table Groupings by Cohort
Speed Mentoring Assignments
2023 Beeson Scholars and 2023 Beeson Travel Awardees
Meeting Attendee Contact List (Clin-STAR/Beeson)
Zoom Instructions
Tag us in your Beeson Meeting 2023 posts on Twitter/X: #Beeson2023
Funding for this meeting was made possible, in part, by 1 R13AG058415-01 from the National
Institute on Aging.
Meals for the 2023 Beeson Annual Meeting are underwritten by the American
Federation for Aging Research.

Beeson Annual Meeting
Hyatt Regency Tamaya Resort and Spa, New Mexico
November 15 – 17, 2023
All sessions marked Virtual below can be accessed through this zoom link:
https://us02web.zoom.us/j/86471125703?pwd=NmlRLzY1ZVVrZk9sR0E2azdpR3gzZz09
Wednesday, November 15, 2023 (jointly with Clin-STAR Meeting)
3:00 pm Hotel Check-in Time
4:45 – 5:45 pm Registration and Reception
Tamaya D
5:45 – 7:00 pm Welcome, Introduction of New Scholars, and
Tamaya E Keynote Address
[VIRTUAL] Steven N. Austad, PhD
Interim Chair and Senior Scientific Director, AFAR
Distinguished Professor and Protective Life Endowed Chair in Healthy
Aging Research, Department of Biology
University of Alabama at Birmingham
Kristine Yaffe, MD
Scola Endowed Chair and Leon Epstein Chair and Vice Chair
Professor, Departments of Psychiatry and Behavioral Science,
Neurology, and Epidemiology & Biostatistics
Director, Center for Population Brain Health
Weill Institute of Neurosciences
University of California, San Francisco
Beeson Program Advisory Committee; 2001 Beeson Scholar
Shoshana Kahana, PhD
Deputy Director, Office of Strategic Extramural Programs (OSEP)
National Institute on Aging

Wednesday, November 15, 2023 (continued)
Robin Barr Keynote Address
Robin Barr, PhD was the DEA Director at NIA until he retired in early
2020 after 33 years with the Institute. He oversaw training initiatives,
anticipated the need for new kinds of training, and worked with NIH
peers to steer overall research training policy. He led efforts to
substantially expand NIA’s career development awards program. Dr.
Barr was instrumental in transitioning the Beeson Program from
private sponsorship to its unique public-private partnership.
“What About that 5 Year Plan?”
Marie A. Bernard, MD
Chief Officer for Scientific Workforce Diversity (COSWD)
National Institutes of Health
7:00 – 9:00 pm Dinner
Tamaya FGH
Thursday, November 16, 2023
7:00 – 9:00 am Breakfast
Tamaya FGH
7:30 – 8:00 am Clin-STAR – Beeson ‘Office (half) Hour’
Tamaya D Office Hours connects early career clinician-scientists with Beeson
scholars for one-on-one, confidential conversations about career
development in aging research. By advance sign-up only.
8:00 – 9:00 am Speed Networking – Beeson Scholars only
Tamaya E
9:00 – 9:15 am Break

Thursday, November 16, 2023 (continued)
9:15 – 10:45 am Advocating for Diversity
Tamaya E
[VIRTUAL] Introduction:
Heidi Zapata, MD, PhD, Yale University, 2019 Beeson Scholar
Overview of NIH policies and activities
Marie A. Bernard, MD
Chief Officer for Scientific Workforce Diversity (COSWD)
National Institutes of Health
Panel Discussions
How to incorporate diversity into research
Moderator:
Alison A. Moore, MD, MPH, FACP, AGSF
Larry L. Hillblom Chair in Geriatric Medicine
Professor of Medicine
Chief, Division of Geriatrics, Gerontology and Palliative Care
Vice Chair for Justice, Equity, Diversity and Inclusion,
Department of Medicine
University of California San Diego
Panelists:
Raele Donetha Robison, PhD, CCC-SLP, University of Wisconsin (Clin-
STAR Health Equity Scholar)
Jason Falvey, DPT, PhD, University of Maryland (2021 Beeson)
Rebecca Brown, MD, MPH, University of Pennsylvania (2018 Beeson)
Diversity in the Mentor/Mentee relationship - how to advocate for
diversity in your group
Moderator:
Roland J. Thorpe, Jr., PhD, MS
Director, Program for Research on Men's Health, Hopkins Center for
Health Disparities Solutions
Johns Hopkins Bloomberg School of Public Health
Panelists:
Heidi Zapata, MD, PhD, Yale University (2019 Beeson)
Darina V. Petrovsky, PhD, RN, Rutgers School of Nursing (Clin-STAR
Health Equity Scholar)
Amy Kind, MD, PhD, University of Wisconsin (2010 Beeson Scholar)
10:45 – 11:15 am Break

Thursday, November 16, 2023 (continued)
11:15 am – 12:15 pm Graduating Scholars Presentations: Group 1
Tamaya E Introductions: Malaz Boustani, MD, MPH (2005 Beeson)
[VIRTUAL]
Charles Brown, MD (2017 Beeson)
Johns Hopkins University
Rebecca Brown, MD, MPH (2018 Beeson)
University of Pennsylvania
Kathryn Callahan, MD (2018 Beeson)
Wake Forest School of Medicine
Jason Roh, MD (2019 Beeson)
Massachusetts General Hospital
12:15 – 1:30 pm Lunch – Consultancies and Aims Workshops (sign-up only)
Tamaya FGH
Aims Workshop Group 1 – Bear A
Aims Workshop Group 2 – Bear B
Aims Workshop Group 3 – Elk A
Aims Workshop Group 4 – Elk B
Consultancies Group 1 – Puma A
Consultancies Group 2 – Puma B
Consultancies Group 3 – Puma C
1:30 – 3:00 pm Free time/Mentoring Activities
A private session is scheduled for the NIA staff and travel stipend
awardees in Elk B
3:15 – 5:00 p.m. Data Blitz! – by assignment, but open to all attendees
Also known as “lightning talks”, this is the academic equivalent of
speed dating – a fast-track vehicle to understand research and has led
to collaborations and other networking opportunities with other
Scholars. Each session involves a research theme and 8 to 10
presenters. This is a chance to share a snapshot of your research with
an audience of peers and learn about what other Scholars are working
on. There will be time for questions after each presentation.
Group 1 – Bear A
Group 2 – Bear B
Group 3 – Eagle A
Group 4 – Eagle B
Group 5 – Puma A
Group 6 – Puma B
Thursday, November 16, 2023 (continued)
5:00 – 6:00 pm Free time/mentoring activities
(Those presenting posters please put them up during this time, push
pins will be available, poster boards are 4’ high x 8’ wide.)
6:00 – 7:00 pm Poster Session and Reception
Tamaya D Note: Please remove your poster at the conclusion of the session.
7:00 – 9:00 pm Dinner – assigned seating by Beeson Cohort
Cottonwoods The Cottonwoods is a short walk from the main hotel building, but
shuttles will also be available at the equestrian turnaround starting at
6:45 pm.
9:00 pm – whenever… Sing-along Singers and non-singers welcome, no sign-up necessary.
The location is TBD, but if it is at the firepit, s’more makings are
available at the front desk.
Friday, November 17, 2023
7:00 – 9:00 am Breakfast
Tamaya FGH Note: A private breakfast meeting for the Program Advisory
Committee and other invited participants will be held from 7:30 – 8:45
am in Puma A
8:00 – 9:00 am Speed Mentoring, assignments in the program booklet
Tamaya E By sign-up only. Please have your breakfast first or bring it with you
into the meeting room.
This session provides an opportunity for scholars to have brief,
informal, but focused discussions with senior investigators outside
their own institutions.
Friday, November 17, 2023 (continued)
9:00 – 10:00 am Graduating Scholars Presentations: Group 2
Tamaya E Introductions: Emily Finlayson, MD, MS (2006 Beeson)
[VIRTUAL]
Indranil Sinha, MD (2018 Beeson)
Brigham and Women’s Hospital
Miles Berger, MD, PhD (2017 Beeson)
Duke University Medical Center
Lauren Ferrante, MD, MHS (2017 Beeson)
Yale School of Medicine
Biren Kamdar, MD, MBA, MHS, University of California, San Diego
School of Medicine (2018 Beeson)
10:00 – 11:30 am Critical Team Science Skills: Setting Expectations and
Tamaya E Having Difficult Conversations
[VIRTUAL]
Introduction: Sikandar H. Khan, MS, DO, Indiana University School of
Medicine, 2022 Beeson Scholar
L. Michelle Bennett, PhD
LMBennett Consulting, LLC, and Senior Vice President, Roger Schwarz &
Associates
Discussion Question: What have been the most difficult and gratifying
situations you have had in relation to team science?
Collaboration Agreement Template: https://zenodo.org/records/6394789
11:30 am – 1:00 pm Lunch – Consultancies and Aims Workshops (sign-up only)
Tamaya FGH
Aims Workshop Group – Bear A
Consultancy Group 1 – Puma A
Consultancy Group 2 – Puma B
1:00 pm Adjourn

7.18
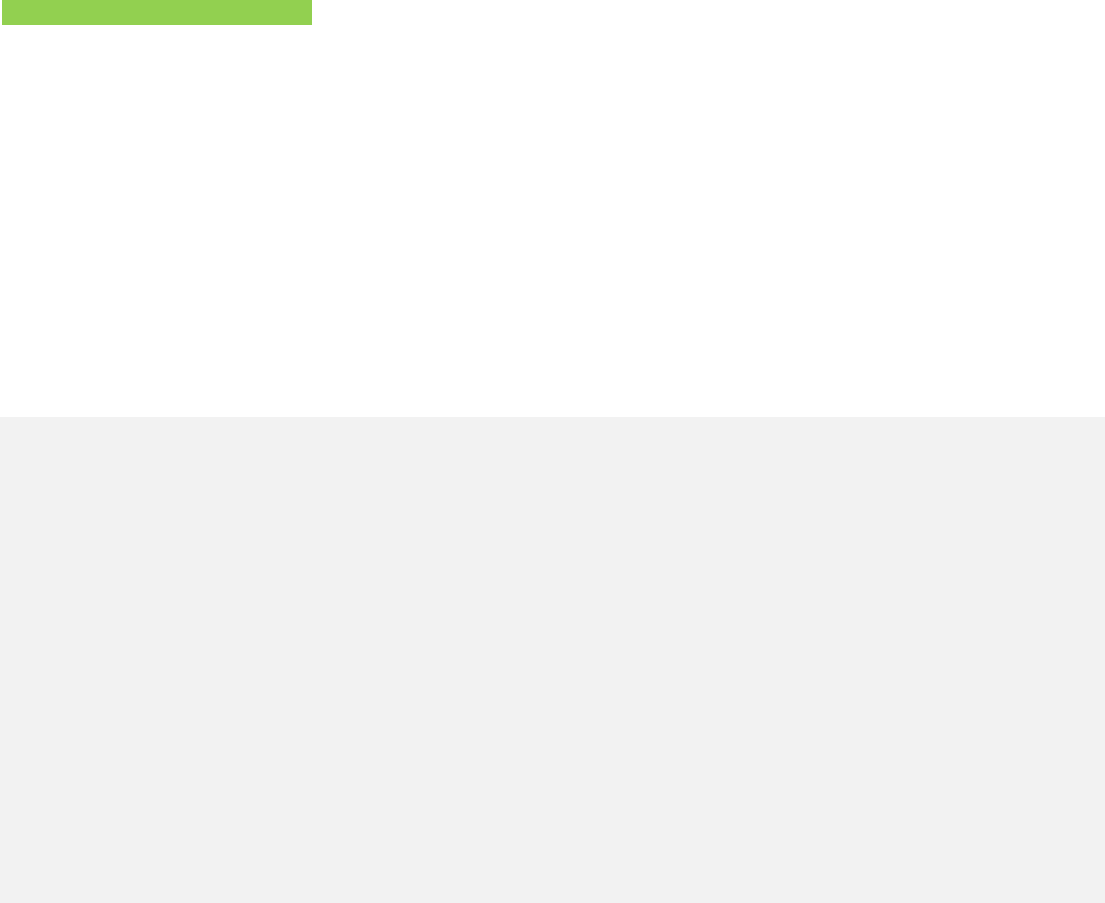
HYATT REGENCY TAMAYA
RESORT AND SPA
1300 Tuyuna Trail,
Santa Ana Pueblo, NM 87004
USA
T +1 505 867 1234
F +1 505 771 6180
tamaya.regency.hyatt.com
C
B
A
C
B D E
A
H
G
F
A
B
A
B
C
B
A
CBA CBA
RESTROOMSRESTROOMS
WOLF PUMA
PREFUNCTION
AIRWALL POCKET
VERANDA
PATIO
PATIO
TAMAYA BALLROOM
NOTE: 10 FT. MEDIA
PLATFORM RUNNING THE
LENGTH OF THE BALLROOM
BADGER
BADGER
BADGER
HAWK
HAWK
HAWK
BEAR
EAGLE
SUNRISE
AMPHITHEATRE
(outdoors)
COTTONWOODS
PAVILION
COUNCIL
RIO LOUNGE
ELK RIO
MOUNTAIN VIEW
FOYER
HOUSE OF THE
HUMMINGBIRD
(outdoors)
AIRWALL POCKET
KIVA
POOL
(outdoors)
OXBOW POOL
& LAWN
(outdoors)

Hyatt Regency Tamaya Resort & Spa Facility Map
The Cottonwoods
Pavilion
The Hummingbird
Garden

Hyatt Regency Tamaya Resort & Spa
Internet Instructions
▪ Connect to the wireless network (SSID) called @Hyatt_Meeting
▪ Launch your Internet browser and follow the log-on instructions on
the portal page and enter the following access code: STAR23
Need additional information?
For assistance, please dial “0” from a house phone or telephone
Clin-STAR and Beeson Annual Meeting

Program Advisory Committee Mentor Assignments
Committee
Thursday, Nov 16
7:00 - 7:45 am
Thursday, Nov 16
1:30 - 2:15 pm
Thursday, Nov 16
2:15 - 3:00 pm
Thursday, Nov 16
5:00 - 5:45 pm
Where to meet Breakfast
Lobby Lobby Lobby
Sara Espinoza Sikandar Khan Mina Sedrak Sandra Aleksic Daniel Roh
Emily Finlayson Courtney Balentine Carolyn Seib Sevdenur Cizginer Bharati Kochar
Tom Gill XX XX XX XX
Angela Jefferson Felipe Jain
Nicole Rogus-Pulia Carmen Quatman
Lauren Hunt
Dan Matlock Parag Goyal Anand Iyer Elissa Kozlov Jennifer Vincenzo
Donovan Maust Jason Falvey Tim Anderson Katie Schenning Claire Ankuda
Manish Shah Katherine Buck John Mafi Kei Ouchi Jasmine Travers
Manjula Tamura XX XX XX XX
Kristine Yaffe Brienne Miner Carolyn Presley Miyeon Jung
2018 and 2019
Scholars have
not been
assigned to
mentors.
Assignments
One of features of the Beeson Program is that we match current scholars with members of the program committee. One of the roles
of the members of the Program Committee is to serve as external mentors to the Beeson Scholars. This is an informal mentorship
and will give active Scholars the opportunity to discuss career and research issues with another senior investigator in aging research
outside his/her own institution. Most of the interactions will be at this meeting, but Scholars may also call on this external mentor
during the Beeson Award. Assignments are listed above (note this sheet has two tabs, assignments per mentor, and assignments per
scholar.) For Scholars whose mentors could not attend the meeting, we will be in touch to arrange virtual sessions.
11/10/2023

2018 Scholars NOT ASSIGNED
Brown, Rebecca
University of Pennsylvania
Improving aging in place for older adults living in subsidized
housing
Malaz Boustani
Callahan, Kathryn
Wake Forest School of Medicine
Identifying Frailty in Primary Care: Implementation of an
Electronic Medical Record-Based Frailty Index
Malaz Boustani
Cohen, Andrew
Yale University
Dementia and Decision-Making for Older Adults without
Surrogates
Cynthia Carlsson
Falcone, Guido
Yale School of Medicine
Genetic analyses of radiological severity, short-term functional
outcome and long-term health status in spontaneous intracerebral
Nicholas Musi
Gilmore-Bykovskyi, Andrea
University of Wisconsin-Madison
Novel Approaches to Identifying and Engaging Disadvantaged
Patients with Alzheimer's Disease (AD) in Clinical Research
NOT ATTENDING/Malaz Boustani
Hall, Rasheeda
Duke University Medical Center Deprescribing for Older Dialysis Patients Manjula Tamura
Kamdar, Biren
University of California, San Diego
School of Medicine
Multicomponent Intervention to Improve Delirium and Sleep-
Wake Rhythms in Older ICU Patients
Cynthia Carlsson
Portz, Jennifer
Coloardo State University
Social Convoy Palliative Care (Convoy-Pal) Mobile Health for
Older Adults with Advanced Heart Failure
Tom Gill
Schoenborn, Nancy
Johns Hopkins University
Improving cancer screening in older adults with limited life
expectancy
Allison Moore/Manjula Tamura
Sinha, Indranil
Harvard Medical School/ Brigham and
Women's Hospital
Aging-associated dysregulation of the hypoxia pathway limits
skeletal muscle regeneration
Nicholas Musi
2019 Scholars NOT ASSIGNED
Goldberg, Elizabeth Univrsity of Colorado
GAPcare II: The Geriatric Acute & Post-Acute Care Coordination
Program for Fall Prevention in the Emergency Department
Tom Gill
Greene, Meredith University of California, San Francisco
Tailored Geriatric Assessment and Management for HIV Care
Settings
Tom Gill/
Kilpela, Lisa University of Texas Health San Antonio
Binge Eating Spectrum Treatment in Older Women (BESTOW):
An Investigation and Intervention-Tailoring Project
Emily Finlayson
Magnuson, Allison University of Rochester
Mitigating Cancer-Related Cognitive Dysfunction in Older Adults
with Breast Cancer
Liana Apostolova/Angela Jefferson
Marcum, Zachary University of Washington Antihypertensives and the Aging Brain
Kristine Yaffe/NO LONGER IN
ACADEMIA
McBeath, Rowena Jefferson University In Vivo Model of Human Enthesis Regeneration Nicholas Musi
Phongtankuel, Veerawat Weill Cornell Medical College
Developing and piloting a multi-component technology-based
care intervention to address patient symptoms and caregiver
Malaz Boustani/NOT ATTENDING
Roh, Jason Massachusetts General Hospital
Activin Type II Receptor Activity in Age-related Frailty and Heart
Failure
Emily Finlayson
Schrag, Matthew Vanderbilt University
Defective Lysosomal Membrane Fission Mediates Axonal
Lysosome Accumulation in Dystrophic Neurites in Alzheimer's
Kristine Yaffe
Tang,Victoria University of California,San Francisco
Improving Outcomes of Older Adults with Psychosocial
Vulnerability Undergoing Major Surgery
Cynthia Carlsson
Wong, Melisa University of California, San Francisco
Advancing Patient-Centered Decision Making in Older Adults with
Lung Cancer: Incorporating Risk of Functional Decline into
Dan Matlock
Zapata, Heidi Yale School of Medicine
NLRP3 Inflammasome Activation and Mitochondrial Function in
the Setting of Aging and HIV Infection
Nicholas Musi
2020 Scholars
Ankuda, Claire Icahn School of Medicine at Mount Sinai
Health Care Use After Functional Disability: Opportunities to
Improve the Care of Older Adults
Manish Shah/Donovan Maust

Goyal, Parag Weill Cornell Medical College
A Novel Deprescribing Intervention for Heart Failure with
Preserved Ejection Fraction (HFpEF): A Prototype for Older
Dan Matlock
Iyer, Anand University of Alabama Birmingham Aging Well with COPD through Geriatrics-Palliative Care Dan Matlock
Jain, Felipe Harvard Medical School
Mobile app delivered Mentalizing Imagery Therapy to augment
remote family dementia caregiver skills training: a pilot
Angela Jefferson
Mafi, John UCLA
Leveraging Electronic Health Records to Measure and Reduce
Harmful Low-Value Care Among Older Adults
Manish Shah
Ouchi, Kei Brigham and Women's Hospital
ED GOAL: An Advance Care Planning Intervention for Seriously
Ill Older Adults in the Emergency Department
Manish Shah
Rogus-Pulia, Nicole University of Wisconsin-Madison
Impact of Novel Rehabilitative Approaches for Dysphagia in
Patients with Alzheimer's Disease and Related Dementias
Angela Jefferson
Shinall, Myrick Vanderbilt University Specialist Palliative Care in Surgical Oncology Dan Matlock/NOT ATTENDING
Sutton, Nadia University of Michigan/Vanderbilt
Ectonucleotidase modulation of age-dependent vascular
calcification and stiffness
Manjula Tamura
2021 Scholars
Balentine, Courtney UT Southwestern
A Pilot Study of Local Anesthesia for Inguinal Hernia Surgery in
Older Adults
Emily Finlayson
Bauer, Scott
UCSF
Age-related changes in skeletal muscle and lower urinary tract
symptoms in older adults
Manjula Tamura
Dharmarajan, Kavita
Mount Sinai
Improving Outcomes for Older Adults Undergoing Palliative
Radiation Treatment
Manjula Tamura
Falvey, Jason
University of Maryland School of
Medicine
The ENRICH Study: Engaging Community and Municipal
Services to Promote High Quality Aging in Place After Hip
Malaz Boustani/Donovan Maust
Hunt, Lauren
UCSF
Hospice Use in Older Adults with Alzheimer's Disease and
Related Dementias: Patterns, Policies, and Caregiver
Cynthia Carlsson/Angela Jefferson
Kozlov, Elissa
Rutgers School of Public Health
Piloting an mHealth-delivered Mindfulness Therapy with Patients
with Serious Illness and their Caregivers to Alleviate Symptoms
Dan Matlock
Miner, Brienne
Yale Evaluating Sleep Deficiency in Aging Populations Kristine Yaffe
Presley, Carolyn
The Ohio State
Resiliency among Older Adults Receiving Lung Cancer
Treatment: A Supportive Care Intervention Study
Kristine Yaffe
Quatman, Carmen
The Ohio State
Transformative Solutions for Reducing Frequent 911 Fall Calls in
the Homes of Patients with Cognitive Impairments
Angela Jefferson
Seib, Carolyn
Stanford
Developing a framework to individualize surgical decision-making
for older adults with primary hyperparathyroidism
Emily Finlayson
Shah, Sachin
UCSF
Individualizing Anticoagulant use in Older Adults with Atrial
Fibrillation
Tom Gill
Travers, Jasmine
NYU
Identifying Unmet Needs Driving Disproportionate and Avoidable
Nursing Home Placements among Black and Latino Persons
Manish Shah
2022 Scholars
Anderson, Tim
University of Pittsburgh
Optimizing prescribing decisions for hospitalized older adults with
chronic conditions
Malaz Boustani/Donovan Maust
Buck, Katherine
The Ohio State
Establishing and Implementing Pneumonia Diagnosis in ED Older
Adults: A Mixed Methods Approach
Manish Shah
Cizginer, Sevdenur
Harvard Medical School
Optimizing care for older surgical patients: a theory-guided
implementation science approach
Malaz Boustani/Emily Finlayson
Dzeng, Liz
UCSF
Understanding and addressing structural racism and its impact on
the quality of end-of-life care in older Black adults
Manjula Tamura

Jung, Miyeon
Indiana University
Virtual Reality and Computerized Cognitive Intervention for Mild
Cognitive Impairment in Heart Failure
Cynthia Carlsson/Kristine Yaffe
Khan, Sikandar
Indiana University
Reactive Oxygen Species in Respiratory Failure, Delirium, and
Post-ICU Cognitive Impairment
Nick Musi/Sara Espinoza
Mattos, Meghan
University of Virginia
Internet-based insomnia intervention to prevent cognitive decline
in older adults with mild cognitive impairment
Tom Gill
Rameau, Anais
Weill Cornell Medical College
Developing an App-Based Voice Clinical Decision Support Tool to
Augment the Sensitivity of the Bedside Swallow Evaluation in
Tom Gill
Schenning, Katie
Oregon Health & Science University
Optimizing anesthesia to prevent postoperative cognitive and
functional decline in older adults
Cynthia Carlsson/Donvan Maust
Sedrak, Mina
City of Hope
Targeting Senescence to Improve Frailty in Older Cancer
Survivors
Nick Musi/Sara Espinoza
Simon, Corey
Duke University Medical Center
Stress Reactivity and Low Back Pain in Older Adults: Influences
on Disability (ReLOAD)
Tom Gill
Vincenzo, Jennifer
University of Arkansas for Medical
Sciences
Developing and testing implementation strategies to support the
STEADI for falls risk management in outpatient rehabilitation
Malaz Boustani/Donovan Maust
2023 Scholars
Aleksic, Sandra
Einstein College of Medicine
The Role of Hypothalamic Dysfunction in Accelerating Aging in
Humans
Sara Espinoza
Hampson, Lindsay
UCSF
Improving Patient-Centered Decision-Making for Stress Urinary
Incontinence Treatment in Older Men
Donovan Maust/NOT ATTENDING
Kochar, Bharati
Massachusetts General Hospital
Incorporating Geriatric Constructs into Management of
Inflammatory Bowel Diseases in Older Adults
Emily Finlayson
Roh, Daniel
Boston University Chobanian &
Avedisian School of Medicine
Targeting Senescence to Improve Wound Healing in Aging Sara Espinoza

Thurs, 11/16/23, 7:30-8:00 am
OFFICE (HALF) HOUR
(optional by sign up)
Room: Tamaya D
Table
#
Clin-STAR Scholar
Institution
Beeson Scholar
Institution
1
An Nguyen
Cedars Sinai
Jennifer Vincenzo
Univ Arkansas
2
Melissa (Kah Poh) Loh
Rochester
Mina Sedrak
UCLA
3
Pamela Dunlap
Pittsburgh
Kate Callahan
Wake Forest
4
Ayomide Bankole
UNC
Jason Falvey
Univ Maryland
5
Adam Faye
NYU
Allison Magnuson
Univ Rochester
6
Lingsheng Li
UCSF
Andrew Cohen
Yale
7
Anita Chary
Baylor
Tony Rosen
Weill Cornell
8
Jessica Rove
U Colorado
Carmen Quatman
Ohio State
9
Kerry Sheets
Hennepin
Liz Dzeng
UCSF
10
Johnson (Qiang) Zhang
Iowa
Brienne Miner
Yale
11
James Deardorff
UCSF
Tim Anderson
Univ Pittsburgh
12
Rachel Skains
Birmingham
Sachin Shah
Mass General
13
Yinan Zhang
Ohio
Rowena McBeath
Thomas
Jefferson
14
Arjune Dhanekula
Washington
Biren Kamdar
UC San Diego
15
Sandra Shi
Harvard
Rasheeda Hall
Duke
16
David Friedmann
NYU
Alexander Chern
JHU
17
Darina Petrovsky
Rutgers
Jasmine Travers
NYU
18
Germine Soliman
UConn
Sandra Aleksic
Einstein
19
Audrey Zhang
Duke
Jenny Portz
Univ Colorado
20
Laura Baehr
Temple
Courtney
Balentine
U Wisc Madison
21
Andrea Levine
Maryland
Carolyn Presley
Ohio State
22
Chris Mosher
Duke
Nicole Rogus-Pulia
U Wisc Madison
23
Leah Acker
Duke
Felipe Jain
Harvard
24
Rachel Litke
Icahn Sinai
Miriam Rodriguez
Indiana Univ
25
Stephanie Cham
UCSF
Nancy
Schoenborn
Johns Hopkins
26
Lolita Nidadavolu
JHMI
Victoria Tang
UCSF
27
Unwanaobong Nseyo
Cornell
Bharati Kochar
Mass General
Beeson Meeting
Datablitz Assignments
FIRST: LAST:
INSTITUTION:
research insterest key words
group
Sandra Aleksic
Einstein College of Medicine hypothalamus, MRI, endocrine system, cognitive aging, frailty, human, proteome
6
Timothy Anderson
University of Pittsburgh
pharmacoepidemiology, deprescribing, transitions of care, hospital medicine,
primary care
6
Claire Ankuda
Icahn School of Medicine at Mount
Sinai
Palliative care, Medicare, Medicare Advantage
1
Courtney
Balentine
University of Wisconsin Madison surgery, implementation science, clinical trials
5
Katherine Buck
The Ohio State University emergency medicine, pneumonia, diagnostics
3
Alexander Chern
Johns Hopkins University
Age-related hearing loss, cognition, epidemiology, qualitative methods, music
perception and enjoyment
6
Sevdenur Cizginer Konuk
Massachusetts General Hospital Geriatric surgery, Colorectal surgery, Qualitative research
4
Andrew Cohen
Yale University
Medical decision-making for persons with dementia, surrogate decision-making,
unrepresented ("unbefriended") older persons, social isolation.
1
Lyndsay DeGroot
University of Colorado School of
Medicine
Palliative care, heart failure, aging, nursing
1
Kavita Dharmarajan
Icahn School of Medicine at Mount
Sinai
palliative care, geriatric oncology
5
Elizabeth Dzeng
University of California, San Francisco
institutional cultures, health policy, equity, structural racism, community-based
participatory research methods, qualitative research, medical sociology, medical
6
Jason Falvey
University of Maryland School of
Medicine
Traumatic injury, neighborhood socioeconomic disadvantage; community
mobility; rehabilitation; falls; health disparities
4
Mikita Fuchita
University of Colorado
Sedation, delirium, and early mobility in the ICU; post-intensive care syndrome;
patient-centered care; implementation science; agile science.
4
Elizabeth Goldberg
University of Colorado fall prevention, digital health, clinical trials
4
Parag Goyal
Weill Cornell Medicine cardiology, heart failure, polypharmacy, deprescribing
3
Meredith Greene
Indiana University HIV, care models, geriatric syndromes
3
Rasheeda Hall
Duke University Medical Center nephrology, deprescribing, geriatric assessment, frailty
6
Lauren Hunt
University of California, San Francisco hospice, dementia, policy and health services research
1
Beeson Meeting
Datablitz Assignments
Anand Iyer
University of Alabama at Birmingham
implementation science, intervention development, COPD, geriatrics, palliative
care, behavioral research
1
Felipe Jain
Harvard Medical School and
Massachusetts General Hospital
family caregivers, digital phenotyping, mHealth, neuroimaging, dementia,
depression, stress, mindfulness, guided imagery, caregiver skills, Latinx/Hispanic
1
Miyeon Jung
Indiana University School of Medicine
Cognitive interventions, virtual reality, clinical trials, mild cognitive impairment,
heart failure
3
Sikandar Khan
Indiana University School of Medicine
critical illness, delirium, acute respiratory failure, post-intensive care syndrome,
post-ICU aging, oxidative stress
2
Lisa Kilpela
University of Texas Health Science
Center San Antonio
women's health; nutrition pathology; health behavior change; mental health
6
Bharati Kochar
Massachusetts General Hospital
inflammatory bowel disease; Crohn's disease, ulcerative colitis, gastroenterology;
frailty; risk stratification; immunosuppression
6
Elissa
Kozlov
Rutgers School of Public Health Mental Health, Dyads, Caregiving, serious illness, palliative care
1
John Mafi
University of California, Los Angeles Access, quality, and costs of medical care, health policy, low-value care
4
Allison Magnuson
University of Rochester Geriatric Oncology
5
Meghan Mattos
University of Virginia Dementia, Alzheimer’s disease, sleep, digital health, intervention
2
Rowena McBeath
Jefferson University tendinosis, hypoxia, senescence, RhoA small GTPase, Rac1 GTPase, HIF1alpha
3
Brienne Miner
Yale University sleep, aging, Alzheimer's disease, patient-centered outcomes
2
Kei Ouchi
Brigham and Women's Hospital and
Harvard Medical School
emergency medicine, palliative care, serious illness communication, advance care
planning
1
Veerawat Phongtankuel
Joan & Sanford I. Weill Medical College
of Cornell University
Hospice, caregiving, symptom management, palliative care
1
Jennifer Portz
University of Colorado social work, palliative care, caregivers, digital health
1
Carolyn Presley
The Ohio State University
Comprehensive Cancer Center
geriatric and thoracic oncology; supportive care interventions; lung cancer
survivorship; IPE programmatic development
5
Carmen Quatman
The Ohio State University Wexner
Medical Center
Falls, Frailty, Cognitive Impairment, Emergency/Trauma, Fractures
5
Anais Rameau
Weill Cornell Medicine swallowing, dysphagia, voice
2
Miriam Rodriguez
Indiana University
Health disparities in Alzheimer's disease and related dementias (ADRD),
Hispanic/Latino ADRD patients and caregivers, ADRD Caregiver intervention,
2
Beeson Meeting
Datablitz Assignments
Nicole Rogus-Pulia
University of Wisconsin-Madison
Swallowing, Dysphagia, Alzheimer's Disease, Rehabilitation, Speech-Language
Pathology, Frailty
2
Daniel Roh
Boston University Chobanian &
Avedisian School of Medicine
Wound healing, senescence, tissue repair
3
Katie Schenning
Oregon Health & Science University postoperative neurocognitive disorders, frailty, delirium, surgery, anesthesiology
2
Nancy Schoenborn
Johns Hopkins University
Decision-making; communication; messaging; de-implementation; prognosis;
cancer screening; deprescribing
5
Matthew Schrag
Vanderbilt University School of
Medicine
Alzheimer's disease, cerebral amyloid angiopathy
3
Mina Sedrak
UCLA Cancer, Aging, Geroscience
5
Carolyn Seib
Stanford University School of Medicine Geriatric surgery, surgical decision support, endocrine disorders of aging
6
Sachin Shah
Massachusetts General Hospital
high risk/high reward clinical decisions, anticoagulants, atrial fibrillation,
lecanemab, generalizability of clinical trials to older adults
3
Corey
Simon
Duke University pain, inflammation, stress
4
Leigh Smith
University of Maryland School of
Medicine
infection control and prevention, nursing facilities, multi drug resistant organisms
4
Nadia Sutton
Vanderbilt University Medical Center vascular aging
3
Jasmine Travers
New York University Rory Meyers
College of Nursing
long-term care, nursing homes, workforce issues, equity, care quality
4
Jennifer Vincenzo
University of Arkansas for Medical
Sciences
implementation science, rehabilitation, fall prevention, health promotion
4
Melisa Wong
University of California, San Francisco
geriatric oncology, lung cancer, functional status, shared decision making, clinical
prediction
5
Heidi Zapata
Yale School of Medicine HIV and Aging, Innate Immune System,
3
DataBlitz! - Group 1
Thursday, November 16, 3:15 - 5:00 pm
Moderator: Caroline Stephens
AFAR Staff: Hattie Herman
Room: Bear A
FIRST: LAST:
INSTITUTION:
Research Insterests
Claire Ankuda
Icahn School of Medicine at Mount
Sinai
Palliative care, Medicare, Medicare Advantage
Andrew Cohen
Yale School of Medicine
Dementia, surrogate decision-making, unrepresented ("unbefriended")
patients, social isolation in older persons.
Lyndsay DeGroot
University of Colorado School of
Medicine
Palliative care, heart failure, aging, nursing
Lauren Hunt
University of California, San Francisco hospice and palliative care, dementia, policy
Anand Iyer
University of Alabama at Birmingham
Geriatrics, palliative care, COPD, pulmonary, end of life, intensive care
unit
Felipe Jain
Harvard Medical School and
Massachusetts General Hospital
caregiving, dementia, stress, depression, mHealth, digital phenotyping,
neuroimaging
Elissa Kozlov
Rutgers School of Public Health palliative care, mental health, geriatrics, mHealth
Kei Ouchi
Brigham and Women's Hospital and
Harvard Medical School
Palliative care, advance care planing, behavioral interventions, serious
illness communication, emergency department.
Veerawat Phongtankuel
Joan & Sanford I. Weill Medical College
of Cornell University
Hospice, caregiving, symptom management, palliative care
Jennifer Portz
University of Colorado social work, palliative care, caregivers, digital health
DataBlitz! - Group 2
Thursday, November 16, 3:15 - 5:00 pm
Moderator: Andy Teich
AFAR Staff: Elizabeth Pritchett-Montavon
Room: Bear B
FIRS: LAST:
INSTITUTION: Research Interests
Sikandar Khan
Indiana University School of Medicine
critical illness, delirium, acute respiratory failure, post-intensive care
syndrome, post-ICU aging, oxidative stress
Meghan Mattos
University of Virginia
Alzheimer's disease, dementia, mild cognitive impairment,
intervention, digital health, sleep, insomnia, cognitive behavioral
Brienne Miner
Yale University Sleep deficiency, symptom burden, aging, dementia
Anais Rameau
Weill Cornell Medicine swallowing, dysphagia, voice
Miriam Rodriguez
Indiana University
Health disparities in Alzheimer's disease and related dementias
(ADRD), Hispanic/Latino ADRD patients and caregivers, ADRD Caregiver
Nicole Rogus-Pulia
University of Wisconsin-Madison Dysphagia, Alzheimer's Disease, Rehabilitation
Katie Schenning
Oregon Health & Science University
postoperative delirium, perioperative neurocognitive disorders, frailty,
patient-reported-outcomes, clinical-trial, anesthesiology
DataBlitz! - Group 3
Thursday, November 16, 3:15 - 5:00 pm
Moderator: Ray Yung
AFAR Staff: Hannah Polauf
Room: Eagle A
FIRST: LAST:
INSTITUTION: Research Interests
Katie Buck
The Ohio State University emergency medicine, pneumonia, diagnostics
Parag Goyal
Weill Cornell Medicine
cardiology, heart failure, polypharmacy, deprescribing, shared decision
making, readmissions, health services research, outcomes research,
Meredith Greene
Indiana University HIV, care models, geriatric syndromes
Miyeon Jung
Indiana University School of Nursing
Heart brain connection, heart failure, cognitive impairment, non-
pharmacological cognitive interventions, virtual reality, attention
Rowena McBeath
Thomas Jefferson University tendinosis, senescence, RhoA/Rac1 signaling, HIF1a signaling
Daniel Roh
Boston University Chobanian &
Avedisian School of Medicine
Wound healing, senescence, tissue repair
Matthew Schrag
Vanderbilt University School of
Medicine
Cerebral amyloid angiopathy, Alzheimer's disease, lysosome,
neuropathology
Sachin Shah
Massachusetts General Hospital
cardiovascular disease, atrial fibrillation, epidemiology, competing
risks, function, vascular dementia
Nadia Sutton
Vanderbilt University Medical Center vascular aging
Heidi Zapata
Yale School of Medicine Innate Immune response, Aging, HIV, Adipose tissue
DataBlitz! - Group 4
Thursday, November 16, 3:15 - 5:00 pm
Moderator: Eleni Linos
AFAR Staff: Andrea Sherman
Room: Eagle B
FIRST: LAST:
INSTITUTION: Research Interests
Sevde Cizginer
Harvard Medical School Geriatric surgery, Colorectal surgery, Qualitative research
Jason Falvey
University of Maryland School of
Medicine
Aging in place; disability; community mobility; neighborhood
environment; socioeconomic disadvantage
Mikita Fuchita
University of Colorado
Sedation, delirium, and early mobility in the ICU; post-intensive care
syndrome; patient-centered care; implementation science; agile
Liz Goldberg
University of Colorado Fall prevention, digital health, clinical trials
John Mafi
University of California, Los Angeles
Quality of Care Among Older Adults, Health Care Value and Costs,
Medicare Policy
Corey Simon
Duke University Geriatric Low Back Pain; Stress Reactivity; Disability
Leigh Smith
University of Maryland School of
Medicine
infection control and prevention, nursing facilities, multi drug resistant
organisms
Jasmine Travers
New York University Rory Meyers
College of Nursing
Long-term care, nursing home, workforce, disparities
Jennifer Vincenzo
University of Arkansas for Medical
Sciences
fall prevention, implementation science, health promotion, disease
prevention, rehabilitation, health education
DataBlitz! - Group 5
Thursday, November 16, 3:15 - 5:00 pm
Moderator: Harvey Cohen
Co-moderator: Dae Kim
Room: Puma A
FIRST: LAST:
INSTITUTION: Research Interests
Courtney Balentine
UW Madison Surgery, implementation science, clinical trials, cognition
Kavita Dharmarajan
Icahn School of Medicine at Mount
Sinai
radiation oncology; geriatric assessment; palliative care; palliative
radiation
Allison Magnuson
University of Rochester Geriatric oncology
Carolyn Presley
The Ohio State University
Comprehensive Cancer Center
geriatric oncology, lung cancer, functional status, supportive care
interventions
Carmen Quatman
The Ohio State University Wexner
Medical Center
Falls, Frailty, Cognitive Impairment, Emergency/Trauma, Fractures
Nancy Schoenborn
Johns Hopkins University
Decision-making; communication; messaging; patient preference;
cancer screening; deprescribing; de-implementation; life expectancy;
Mina Sedrak
UCLA Cancer, Aging, Geroscience, Intervention, Clinical Trials
Melisa Wong
University of California, San Francisco
geriatric oncology, lung cancer, functional status, shared decision
making, clinical prediction
DataBlitz! - Group 6
Thursday, November 16, 3:15 - 5:00 pm
Moderator: Catherine Sarkisian
Co-moderator: Tony Rosen
Room: Puma B
FIRST: LAST:
INSTITUTION: Research Interests
Sandra Aleksic
Albert Einstein College of Medicine Hypothalamus, Endocrine changes in aging, Testosterone
Tim Anderson
University of Pittsburgh
prescribing, hospital medicine, deprescribing, multiple chronic
conditions, hypertension, diabetes
Alexander Chern
Johns Hopkins University
Age-related hearing loss, cognition, epidemiology, qualitative methods,
music perception and enjoyment
Elizabeth Dzeng
University of California, San Francisco
institutional cultures, health policy, equity, structural racism,
community-based participatory research methods, qualitative
Rasheeda Hall
Duke University Medical Center nephrology, deprescribing, geriatric assessment, frailty
Lisa Kilpela
University of Texas Health Science
Center San Antonio
Behavioral health; nutrition pathology; women's health; obesity;
metabolic disturbances; psychological health
Bharati Kochar
Massachusetts General Hospital
inflammatory bowel disease; Crohn's disease, ulcerative colitis,
gastroenterology; frailty; risk stratification; immunosuppression
Carolyn Seib
Stanford University School of Medicine
geriatric surgery, surgical decision-making in older adults, primary
hyperparathyroidism, endocrine disorders

Consultancies
Thursday, November 16 Thursday, November 16
12:15 -1:30 pm 12:15 -1:30 pm
Room: Puma A Room: Puma B
Moderator: Mike Steinman UCSF Moderator: Heather Whitson Duke Medical Center
Co-moderator: Stacey Fischer Colorado Co-moderator Mac Ishii UT Southwestern Medical Center
Group 1 Group 2
Sandra Aleksic Albert Einstein College of Medicine Claire Ankuda Mount Sinai
Miles Berger Duke Katie Buck Ohio State
Biren Kamdar UC San Diego Mikita Fuchita University of Colorado
Rowena McBeath Thomas Jefferson University Miyeon Jung Indiana University School of Medicine
Anaïs Rameau Weill Cornell Medicine Lisa Kilpela UT Health San Antonio
Jason Roh MGH/Harvard Medical School Kei Ouchi Brigham and Women's Hospital
Sachin Shah Massachusetts General Hospital
How a Consultancy Session works:
This is a popular and effective group problem-solving activity known as a “consultancy.” This is structured to enable a set of people with a variety of
knowledge and expertise to provide support, new perspectives, and ideas to one another, particularly around an important or difficult challenge.
Each Scholar will get approximately 10 minutes. Each Scholar will have 2-3 minutes or so to present what he/she views as the major career challenge
he/she are facing (or will soon face). This may include, but is certainly not limited to:
- Time Management
- Balancing Career and Family
- Strategies for promotion
- Balancing research, clinical, teaching and administrative responsibilities
- Issues related to your lab/team members (supervision, quality control, hiring, firing, disciplinary action, etc.)
- Transitioning relationship with your mentor(s).
- Finding/solidifying your niche, area of expertise
Following each Scholar's presentation, the group will ask clarifying questions for the next one-two minutes. For the bulk of the remainder of the
time, the Scholar will receive feedback and advice from the group. In the last minute or so, the Scholar will then have a chance to respond to the
ideas presented.
We will follow a strict timetable, so that each person will have the same opportunity for constructive feedback.
Consultancies
Thursday, November 16
12:15 -1:30 pm
Room: Puma C
Moderator: Steve Austad UAB
Co-moderator: Catherine Sarkisian UCLA
Group 3
Rasheeda Hall Duke University School of Medicine
Bharati Kochar Massachusetts General Hospital
Jenny Portz University of Colorado
Danny Roh Boston University
Katie Schenning Oregon Health & Science University
Carolyn Seib Stanford University School of Medicine
observer
kavita dharmarajan mount sinai
How a Consultancy Session works:
This is a popular and effective group problem-solving activity known as a “consultancy.” This is structured to enable a set of people with a
variety of knowledge and expertise to provide support, new perspectives, and ideas to one another, particularly around an important or
difficult challenge.
Each Scholar will get approximately 10 minutes. Each Scholar will have 2-3 minutes or so to present what he/she views as the major career
challenge he/she are facing (or will soon face). This may include, but is certainly not limited to:
- Time Management
- Balancing Career and Family
- Strategies for promotion
- Balancing research, clinical, teaching and administrative responsibilities
- Issues related to your lab/team members (supervision, quality control, hiring, firing, disciplinary action, etc.)
- Transitioning relationship with your mentor(s).
- Finding/solidifying your niche, area of expertise
Following each Scholar's presentation, the group will ask clarifying questions for the next one-two minutes. For the bulk of the remainder of
the time, the Scholar will receive feedback and advice from the group. In the last minute or so, the Scholar will then have a chance to respond
to the ideas presented.
We will follow a strict timetable, so that each person will have the same opportunity for constructive feedback.

Consultancies
Friday, November 17 Friday, November 17
11:30 - 1:00 pm 11:30 - 1:00 pm
Room: Puma A Room: Puma B
Moderator Amy Jo Kind University of Wisconsin-Madison Moderator Mark Lachs Weill Cornell
Group 1 Group 2
Sikandar Khan Indiana University School of Medicine Charles Brown Johns Hopkins
Carolyn Presley The Ohio State University Jason Falvey University of Maryland School of Medicine
Melisa Wong Kaiser Permanente Northern California/UCSF Felipe Jain Harvard Medical School - MIT
Alexander Chern Johns Hopkins University Elizabeth Dzeng UCSF
Miles Berger Duke Courtney Balentine UW- Madison
Brienne Miner Yale University Kate Callahan Wake Forest University School of Medicine
Miriam Rodriguez Indiana University Bloomington
How a Consultancy Session works:
This is a popular and effective group problem-solving activity known as a “consultancy.” This is structured to enable a set of
people with a variety of knowledge and expertise to provide support, new perspectives, and ideas to one another, particularly
around an important or difficult challenge.
Each Scholar will get approximately 10 minutes. Each Scholar will have 2-3 minutes or so to present what he/she views as the
major career challenge he/she are facing (or will soon face). This may include, but is certainly not limited to:
- Time Management
- Balancing Career and Family
- Strategies for promotion
- Balancing research, clinical, teaching and administrative responsibilities
- Issues related to your lab/team members (supervision, quality control, hiring, firing, disciplinary action, etc.)
- Transitioning relationship with your mentor(s).
- Finding/solidifying your niche, area of expertise
Following each Scholar's presentation, the group will ask clarifying questions for the next one-two minutes. For the bulk of the
remainder of the time, the Scholar will receive feedback and advice from the group. In the last minute or so, the Scholar will then
have a chance to respond to the ideas presented.
We will follow a strict timetable, so that each person will have the same opportunity for constructive feedback.

Thursday, November 16, 2023
12:15-1:30 pm
Aims Page Workshop
Room: Bear A
Group 1
Tim Anderson University of Pittsburgh
ELIZABETH GOLDBERG University of Colorado
Anand Iyer UAB
Sikandar Khan Indiana University School of Medicine
Elissa Kozlov Rutgers School of Public Health
Nancy Schoenborn Johns Hopkins University
Moderators Cathleen Colon-Emeric Duke University
Alex Smith UCSF

Thursday, November 16, 2023
12:15-1:30 pm
Aims Page Workshop
Room: Bear B
Group 2
Charles Brown Johns Hopkins
Parag Goyal
Weill Cornell Medicine
Felipe
Jain Harvard Medical School - MIT
Allison Magnuson University of Rochester
Brienne Miner
Yale University
Melisa
Wong Kaiser Permanente Northern California/UCSF
Moderators George
Kuchel UConn
Molly Wagster NIA

Thursday, November 16, 2023
12:15-1:30 pm
Aims Page Workshop
Room: Elk A
Group 3
Alexander Chern Johns Hopkins University
Mikita Fuchita
University of Colorado
Lauren
Hunt UCSF
Carmen Quatman The Ohio State University
Corey Simon
Duke University
Heidi
Zapata Yale School of Medicine
Moderators Alexis
Bakos NIA
Sean Morrison Mount Sinai

Thursday, November 16, 2023
12:15-1:30 pm
Aims Page Workshop
Room: Elk B
Group 4 Courtney
Balentine UW- Madison
Kate Callahan Wake Forest University School of Medicine
Veerawat Phongtankuel
Weill Cornell Medicine
Carolyn
Presley The Ohio State University
Miriam Rodriguez Indiana University Bloomington
Nadia Sutton
Vanderbilt University Medical Center
Moderators Marcel Salive NIA
Alison Huang
UCSF

Friday, November 17, 2023
11:30 am -1:00 pm
Aims Page Workshop
Room: Bear A
Group 1
Lyndsay
DeGroot University of Colorado School of Medicine
Biren Kamdar UC San Diego
Rowena McBeath Thomas Jefferson University
Jenny Portz
University of Colorado
Jasmine Travers New York University
Moderators Randy Bateman Washington University St. Louis
Shoshana Kahana NIA

PosterSession
Thursday,November16
6:00‐7:00pm
Room:TamayaD
SMALLGROUPPOSTERDISCUSSIONS
Group A 6:00‐6:20pm
JohnNewman
Moderato
r
Poster Presenter
Abstracttitle
1 Chern,A.
TheAssociationofHearingLossandMusicEngagementintheCanadian
LongitudinalStudyofAging
2 Fuchita,M.
InterdisciplinarySimulation‐BasedTrainingonSedationMinimizationinthe
ICU:APilotStudy
3 Kilpela,L.
RecommendationsfromOlderAdultWomenonAge‐TailoringEvidence‐
BasedTreatmentsforBingeEatingDisorder:AMixed‐MethodsApproach
4 Zapata,H.
SingleCellAnalysisofAdiposeTissueintheSettingofHIV‐infectionandAging
How aSmallGroupPosterSessionworks:
Eachposterpresenterwillhaveapproximately3minutestopresenttheirpostertothegroupwith
oneortwominutesoffollowupquestions.Thenthe groupwillmoveto thenextposter.Time
keepingisessentialsoallpostersinthegroupcanbevisitedwithinth
e20minutetimeframe.The
moderatorwillguidethediscussionandmovethegrouptothenextposterattheconclusionofthe
fiveminutes.

PosterSession
Thursday,November16
6:00‐7:00pm
Room:TamayaD
SMALLGROUPPOSTERDISCUSSIONS
GroupC 6:40‐7:00pm
DukeHan
Moderato
r
Poster Presenter
Abstracttitle
5 Rodriguez,M.
TechnologycaregiverinterventionforAlzheimer’sdisease(I‐CARE):Feasibility
andpreliminaryefficacyofBrainCareNotes
6 Seib,C.
Effectofparathyroidectomywithnewdiagnosisofdepressionamongadults
withprimaryhyperparathyroidism
7 Quatman,C.
ProjectADOPT(AgileDeploymentofPatientTechnology)
How aSmallGroupPosterSessionworks:
Eachposterpresenterwillhaveapproximately3minutestopresenttheirpostertothegroupwith
oneortwominutesoffollowupquestions.Thenthe groupwillmoveto thenextposter.Timekeeping
isessentialsoallpostersinthegroupcanbevisitedwithinth
e20minutetimeframe.Themoderator
willguidethediscussionandmovethegrouptothenextposterattheconclusionofthefiveminutes.

PosterSession
Thursday,November16
6:00‐7:00pm
Room:TamayaD
SMALLGROUPPOSTERDISCUSSIONS
Group B 6:20‐6:40pm
LouiseWalter
Moderator
Poster Presenter
Abstracttitle
8 DeGroot,L.
TheOverlapofPalliativeCareNeedsandPhysicalFrailtyInfluenceClinicalOutcomesin
Community‐DwellingPeoplewithHeartFailure
9 Goldberg,E.
Feasibilityofobtainingdigitalassessmentofcognitiveandphysicalfunctioninolder
adultspresentingtotheemergencydepartmentforfallsusingwearable
accelerometersandsmartphonesintheGAPcareIIstudy
10 Phongtankuel
,
Assessingthefeasibility,acceptability,andpreliminaryefficacyofanovelsymptom
managementcaredeliveryinterventionforcaregiversreceivinghomehospicecare.
11 Shah,S.
MultidimensionalRepresentativenessofOlderAdultswithAtrialFibrillationin
RandomizedControlledTrials:ComparingParticipantsof12OralAnticoagulantRCTsto
aNationallyRepresentativeUSCohort
How aSmallGroupPosterSessionworks:
Eachposterpresenterwillhaveapproximately3minutestopresenttheirpostertothegroupwithoneortwo
minutesoffollowupquestions.Thenthe groupwillmovetothenextposter.Timekeepingisessentialsoall
postersinthegroupcanbevisitedwithinthe20mi
nutetimeframe.Themoderatorwillguidethediscussion
andmovethegrouptothenextposterattheconclusionofthefiveminutes.
Ti
tle: The Association of Hearing Loss and Music Engagement in the Canadian Longitudinal
Study of Aging
Alexander Chern, MD
1,2*
; Srishti Nayak
3*
, PhD; Peyton L. Coleman
3
, BS; Reyna Gordon, PhD
3
1
Department of Otolaryngology—HNS, Columbia University Vagelos College of Physicians and
Surgeons and Columbia University Irving Medical Center/NewYork-Presbyterian Hospital, New York,
NY
2
Department of Otolaryngology—HNS, Weill Cornell Medical College and NewYork-Presbyterian
Hospital, New York, NY
3
Department of Otolaryngology—HNS, Vanderbilt University Medical Center, Nashville, TN
*indicates co-first authors
Keywords: music engagement, music enjoyment, hearing loss, epidemiology, quality of life
Objective: Music engagement has been associated with increased quality of life, health, and well-being. However,
individuals with HL may not be able to perceive, appreciate, or engage with music as much as their normal hearing (NH)
peers. However, studies investigating music engagement and its relationship with hearing loss (HL) have been limited to
small samples, heterogeneous outcome variables, and inconsistent results. Our objective was to examine the association of
HL with music engagement on a population level.
Study D
esign: Cross-sectional analysis of prospective, epidemiologic cohort study
Setting: Canadian Longitudinal Study of Aging
Patients: 26,236 adults ≥45 years old
Int
erventions: none
Mai
n Outcome Measures:
The exposure was HL, measured by better hearing ear pure tone average (PTA). The outcome
was music engagement, measured by frequency of singing or playing a musical instrument (1=every day, 2=several
times/week, 3=several times/month, 4=several times/year, 5=once/year or less) or having played a musical instrument,
listened to radio/music, or participated in a musical program in the past 7 days. Multivariable linear/logistic regressions were
performed to assess associations between music engagement and HL, adjusting for age, sex, socioeconomic status, and
hearing aid usage.
Results:
Mean (SD) age was 62.7 (10.1) years; 51% were women. Mean (SD) better ear PTA was 17.6 (10.9) dB; 5.2%
were hearing aid users. Multivariable regression demonstrated a significant association between increased severity of HL and
decreased active music engagement. For every 10-dB worsening in better ear PTA, there was a 0.051-point decrease in
frequency of singing or playing a musical instrument (95% CI 0.035-0.068, p<0.0001).
Co
nclusions:
Using population-level analyses, increased severity of HL was independently associated with reduced active
music engagement. Our findings align with behavioral studies demonstrating decreased music appreciation in individuals
with HL. Given the known association of HL of neuropsychiatric disorders of the elderly including isolation, loneliness,
depression, cognitive decline, and dementia, our findings may drive future studies examining the complex interplay of
hearing, music engagement, and cognition.
Poster 1

Abstract Title: Interdisciplinary Simulation-Based Training on Sedation Minimization in the ICU: A Pilot
Study
Presenting Author: Mikita Fuchita, MD
Co-Authors: Lorel Huber, MD; Anuj B. Mehta, MD, MS; Dan Matlock, MD, MPH; Ryan Good, MD
This work was conducted at the University of Colorado Anschutz Medical Campus, Aurora, CO (12401
East 17
th
Avenue, 7
th
Floor, Aurora, CO, USA).
Purpose: To evaluate the feasibility of interprofessional simulation-based training focused on promoting
sedation minimization in the intensive care unit (ICU) using the Spontaneous Awakening Trial (SAT).
Material and Methods: In this pilot before-and-after study, a 90-minute simulation-based training was
provided to interdisciplinary ICU clinicians to 1) improve the accuracy of Richmond Agitation Sedation
Scale (RASS) assessment, and 2) promote attitudes towards sedation minimization, non-pharmacologic
delirium management, and early mobilization. Kirkpatrick’s framework for training program evaluation was
used to develop survey instruments to measure the participants’ reactions to the training and their
acquisition of skills and attitudes.
Results: Sixteen clinicians representing different disciplines participated. After the training, participant’s
RASS assessment skills improved (p=0.003). The training resulted in significantly more participants
feeling comfortable performing an SAT on a patient with acute respiratory distress syndrome (31% pre-
training vs. 100% post-training, p<0.001) and repeating an SAT 4 hours after a failed SAT (62% vs.
100%, p=0.02). Most participants strongly agreed that the training was realistic, relevant, important, and
would improve their performance in real clinical settings.
Conclusions: Our study demonstrated the feasibility of using interdisciplinary simulation-based training
to promote ICU clinicians’ skills and attitudes necessary to minimize sedation in the ICU. Future studies
should evaluate the impact of simulation-based training on clinicians’ bedside behaviors and patient
outcomes, including delirium, long-term cognitive function, and mortality.
Key Words: delirium; early mobilization; interdisciplinary care; patient-centered care; sedation; simulation
training
Poster 2
Recommendations from Older Adult Women on Age-Tailoring Evidence-Based Treatments for
Binge Eating Disorder: A Mixed-Methods Approach
Introduction
Binge eating disorder (BED) is defined as averaging one objective binge episode
(consuming unusually large amounts of food in one sitting while feeling out of control) per week
for the past three months. Older adult women experience high rates of binge eating yet are
understudied in eating disorders research. While cognitive behavioral therapy is an evidence-
based treatment for BED, in 58 eating disorders randomized control trials, only 3 allowed
participants age ≥65; none were designed for older adults (Burnette et al., 2022). Thus, no
guidelines exist for the treatment of BED in older women. The current study is a concurrent
nested mixed-methods study that gathered and integrated quantitative and qualitative feedback
from older women (ages 60+), with current BED, on existing treatments for binge eating. The
goal is to use this feedback to tailor a BED intervention for older women.
Participants (N = 18, ages 60-76), provided feedback on six existing evidence-based
intervention approaches: Nutrition Guidance, Emotion Regulation skills, Acceptance and
Commitment Therapy (ACT), Appetite Awareness Training (AAT), Cognitive-Behavioral
Therapy-Enhanced (CBT-E), and positive Body Image. Participants viewed intervention
materials and provided quantitative feedback before attending focus groups. During focus
groups, we collected qualitative data regarding intervention material content, presentation, and
logistical considerations for program implementation.
Quantitative data indicated that participants rated AAT, ACT, and Emotion Regulation
skills as strategies they were “most likely to try;” Nutrition Guidance and Body Image activities
were rated as “least likely to try.” Different themes in qualitative data explained these findings.
Emotion Regulation was most frequently rated as “most likely to try” as participants reported
emotions were the core of the problem, while ACT was favored for its focus on values.
Participants also liked aspects of AAT, such as focusing on how to eat mindfully to stop at
moderate fullness (versus feeling “stuffed”). Other themes included Nutritional Guidance as
repetitive and insufficient to incite behavior change, CBT-E food tracking as redundant and
unhelpful, and Body Image exercises as too difficult. Age-specific themes included social
isolation with age, adapting to life transitions (e.g., empty nest, retirement), and loss/grief.
Regarding program logistics, themes included: 1) forms/language simple and easy to digest, 2)
small groups are preferred for social support, and 3) concerns regarding sustainability of
behavior change after a program ends. More in depth information and exemplar quotes will be
included on the poster.
Overall, older women with BED want effective treatments that bring a different approach
to healthy eating and that are tailored for their age group. Preferred treatments align with
emotion regulation and acceptance strategies; both social support and interactive learning were
emphasized. Future clinical trials of age-tailored BED treatments for older adults are needed.
Poster 3

Single Cell Analysis of Adipose Tissue in the Setting of HIV-infection and Aging
Zapat
a, Heidi, Yale University
Every individual has a distinct immune signature that may determine if they will develop co-morbidities
such as metabolic syndrome or develop severe infections. This unique immune signature is likely
influenced by inflammatory factors that are secreted from fat tissue. This project aims to understand how
fat tissue contributes to the inflammation that is seen with increased age, and HIV-infection.
A
dipose tissue is a complex community of cells that includes non-immune cells and innate immune
cells such as macrophages, dendritic cells, and monocytes. As one of the largest organs in the body
there is strong evidence that it is a significant source of inflammatory mediators, such as IL-6 (a
cytokine strongly associated with age-associated chronic inflammation). As a source of inflammatory
mediators, adipose tissue likely contributes to systemic inflammation. Both aging and HIV-infection are
associated with pro-inflammatory environments that are characterized by elevated levels of cytokines,
acute phase reactants, and clotting factors. However, the mechanisms underlying how adipose tissue
contributes to systemic inflammation in the setting of aging, and HIV-infection are incompletely
understood. The overall objective of this proposal is to determine how adipose tissue
contributes to the pro-inflammatory environment seen in Aging, and HIV-infection. To achieve
this objective, we will characterize innate immune pathways in both immune and non-immune cells of
adipose tissue and evaluate their interactions at the single-cell level in uninfected and HIV-infected
cohorts of young and old patients. Our central hypothesis is that increased age, and HIV-infection will
lead to the dysregulation of innate immune pathways, including the NLRP3 inflammasome, in both
immune and non-immune cells within adipose tissue, and thus contribute to systemic inflammation. In
Specific Aim 1 fat pad biopsies will be collected from HIV-positive, and HIV-negative adults in the
following age groups (21-35) and (≥ 60 years). Multicolor flow cytometry and single cell RNA seq
(including nuclear-seq) will be used to characterize both immune (macrophages, dendritic cells,
monocytes) and non-immune cell populations within adipose tissue by evaluation of innate immune
pathways, such as the NLRP3 inflammasome, cytokines (IL-1β, IL-18, IL-6, TNF-α, IL-10 etc.), and
transcriptomics of specific cells to evaluate cellular signaling networks and identify new cell
populations. Specific Aim 2 seeks to characterize both gene and protein expression in the context of
adipose tissue architecture by using spatial transcriptomics (DBiT-seq). Clinical characteristics (e.g.,
BMI) and co-morbidities (e.g., diabetes) will be evaluated in conjunction with the experimental data.
The rationale for the proposed research is that by discovering how innate immune signaling and cell-
cell interactions become dysregulated in adipose tissue with age and HIV-infection, we will identify
novel therapeutic targets in adipose tissue that could be used to control systemic inflammation in these
growing patient populations.
Poster 4
Technology caregiver intervention for Alzheimer’s disease (I-CARE): Feasibility and
preliminary efficacy of Brain CareNotes
M
iriam Jocelyn Rodriguez, PhD
1,
Vanessa M. (Martinez) Kercher, PhD
1
, Evan J. Jordan,
PhD
1
, April Savoy, PhD
2
,, Jordan R. Hill, PhD
1
, Nicole Werner, PhD
1
, Arthur Owora, PhD
1
, Pete
Castelluccio, PhD
3
, Malaz A. Boustani, MD
3
& Richard J. Holden, PhD
1
1
Indiana University Bloomington,
2
Purdue School of Engineering and Technology, Indiana
University-Purdue University Indianapolis
3
Indiana University School of Medicine
P
resenter: Miriam Jocelyn Rodriguez, PhD.
Indiana University-Bloomington
School of Public Health
1025 E. 7th Street
Bloomington, IN 47405
K
ey Words: ADRD Caregivers, Caregiver intervention, Technology, Behavioral and
Psychological Symptoms of Dementia (BPSD).
BACKGROUND: The primary aim of the current pilot study was to examine enrollment rate,
data completion, usability, acceptance and use of a mobile telehealth application, Brain
CareNotes. A secondary aim was to estimate the application’s effect in reducing caregiver
burden and behavioral and psychological symptoms related to dementia (BPSD). METHODS:
Patient-caregiver dyads (n = 53) were recruited and randomized to intervention and control
groups. Assessment of usability, acceptance, BPSD symptoms, and caregiver burden were
collected at baseline, 3- and 6-month follow-up. RESULTS: The enrollment rate was acceptable
despite pandemic related challenges (53/60 target recruitment sample). Among randomized
individuals, there was a retention rate of 85% and data completion was attained for 81.5% of
those allocated to usual care and 88.5% of those allocated to Brain CareNotes. Mean caregiver-
reported app usability at 6 months was 72.5 (IQR 70.0-90.0) on the System Usability Scale—
considered “Good to Excellent”—and user acceptance was reasonable as indicated by 85-90%
of caregivers reporting they would intend to use the app to some degree in the next 6 months, if
able. Regarding intervention effect, although differences in outcome measures between the
groups were not statistically significant, compared to baseline, we found a reduction of caregiver
burden (NPI-Caregiver Distress) of 1.0 at 3 months and 0.7 at 6 months for those in the
intervention group. BPSD (NPI Total Score) was also reduced from baseline by 4.0 at 3 months
and by 0.5 at 6 months. CONCLUSIONS: Brain CareNotes is a highly scalable, usable and
acceptable mobile caregiver intervention. Future studies will focus on testing Brain CareNotes
on a larger sample size to examine efficacy of reducing caregiver burden and BPSD and
culturally adapting the intervention for effective use among Hispanic ADRD caregivers.
Poster 5
Effect of parathyroidectomy with new diagnosis of depression among adults with
primary hyperparathyroidism
Presenter: Carolyn D. Seib MD MAS
Institution: Stanford University School of Medicine, 300 Pasteur Dr, Stanford, CA 94035
Co-Authors: Lia Delaney MD MS; Adam Furst MS; Robin M. Cisco MD, Electron Kebebew MD;
Maria E. Montez-Rath PhD MS; Manjula Kurella Tamura MD MPH
O
bjective: To determine the effect of early parathyroidectomy on the incidence of new
depression among adults with primary hyperparathyroidism (PHPT).
Background: PHPT is a common disorder of aging and is associated with neuropsychiatric
symptoms. Parathyroidectomy is the only definitive treatment for PHPT and has been
associated with improvement of pre-existing depression. The effect of parathyroidectomy on the
subsequent development of depression among adults with PHPT has not been studied.
Methods: Observational data of adults within the Veterans Health Administration with a new
diagnosis of PHPT from 2000-2019 was analyzed using target trial emulation. A new diagnosis
of depression was compared between patients treated with early parathyroidectomy (within 1
year of PHPT diagnosis) vs. non-operative management using an extended Cox model with
time-varying inverse probability censoring weighting, adjusted for patient demographics,
comorbidities, and depression risk factors.
R
esults: A total of 40,231 adults with PHPT and no history of depression were identified, of
whom 3,294 (8.2%) underwent early parathyroidectomy. The weighted cumulative incidence of
depression was 11% at 5 years and 18% at 10 years among parathyroidectomy patients,
compared with 9% and 18%, respectively, among non-operative patients (Figure 1). Using
target trial emulation, PHPT patients treated with parathyroidectomy experienced no difference
in the adjusted rate of new depression (HR 1.06, 95%CI 0.94-1.18).
Conclusions: Among adults with PHPT, there was no difference in the incidence of new
depression between those treated with parathyroidectomy and non-operative management,
which is relevant to preoperative discussions about the benefits and risks of operative
treatment.
K
ey words: Primary hyperparathyroidism; geriatric surgery; target trial emulation
Poster 6

Project ADOPT (Agile Deployment of Patient Technology)
ELH Fellow: Carmen E. Quatman, MD, PhD
Institution: The Ohio State University College of Medicine and Wexner Medical Center
Co-Authors: Jennifer Dauer, BA, Geoffrey Beecher, MBA, Thomas Bentley, RN, MS, Ryan Haley MBOE,
Carol Bradford, MD, MS
Background: Innovative technologies are created worldwide daily that can transform healthcare. Yet,
implementation and scaling new technology to impact patient care at the bedside at most healthcare
centers is often complex, inefficient, and expensive.1 Many medical centers have minimal strategy
and/or infrastructure devoted to translation of medical technologies to the patients (bench to bedside).
A healthcare critical gap at is a seamless process that facilitates identification, approval, deployment,
scale, and monitoring of equipment.
Goal: Evaluate the current state and design a future approach to adoption of patient technology.
Methods: An agile implementation framework to design and pilot an evidence-based healthcare
solution for a rapid, efficient, scalable, and sustainable workflow for adoption of patient technology. A
mixed-methods needs assessment consisting of semi-structured multi-stakeholder qualitative interviews
and faculty survey was used to create implementation strategy.
Results: 17% (2/12) department faculty council representatives know how to get new patient
technology to bedside. Faculty projected time to new technology at bedside 2 months-10 yrs but
described ideal time as 1 month- 2 yrs. Faculty thoughts on need for IRB research approval to deploy
technology (25% no; 58% sometimes, 8% always). Barriers identified included unclear processes,
financial, multiple layers of bureaucracy, timeline to approval, getting stuck in multiple places to get to
get to final approval and entire implementation process transparency is lacking. Central themes:
1) Clarity of approval to implementation processes are lacking.
2) Unclear whether a process map exists.
3) “Wicked” yet important problem in healthcare.
4) Regulatory and approval processes feel “insurmountable” and several have stopped tryin
g
P
ilot of technology process demonstrated a prolonged timeline 15 months to achieve approvals, with
projected further physician championing through IT and patient implementation sprints, prior to further
scaling up of technology across enterprise (estimated 12 to 18 more months). Barriers: approval
process, document gathering, financial projections, funding dependent on physician champion.
Significant redundancy in approval processes and no clear transparency on the process to follow.
Conclusion: New patient technology has the potential to transform healthcare. However, the journey
from needs assessment of technology to bedside implementation is complex, expensive and time
consuming. Results from Project ADOPT support a rapid, agile implementation process to that facilitates
identification, approval, deployment, scale, and monitoring of innovative healthcare technologies.
REFERENCES: [1] Clark D, Dean G, et al. The technology adoption pathway in healthcare. Health and
Technology. 2020 [2] Marwaha JS, Landman AB, et al. Deploying digital health tools within large,
complex health systems: Nature Partner Journal: Digital Medicine. 2022.[3] Boustani M, Azar J, Solid C.
Agile Implementation. New York: Morgan James Publishing; 2020.[4] Rodriguez Santana, I., Mason, et al.
Need, demand, supply in health care. 2023.
Poster 7

The Overlap of Palliative Care Needs and Physical Frailty Influence Clinical Outcomes in
Community-Dwelling People with Heart Failure
Lyndsay DeGroot, PhD, RN, CNE
1
, Noelle Pavlovic, PhD, MSN, RN,
Nancy Perrin, PhD, MA, Nisha
A. Gilotra, M.D., Hailey Miller, PhD, RN, Quin E. Denfeld PhD, RN, FAHA, FAAN, FHFSA, Colleen
K. McIlvennan, PhD, DNP, ANP, Sydney M. Dy, M.D., Patricia M. Davidson, PhD, MEd, RN, FAAN,
Sarah L. Szanton, PhD, MSN, FAAN, ANP, Martha Abshire Saylor, PhD, RN
1
Johns Hopkins University School of Nursing , 525 N. Wolfe Street Baltimore, MD 21205
Introduction: Patients with HF often experience fragmented care, severe physical and
psychological symptoms, existential distress, increased caregiving needs, and complex end of
life decisions. Palliative care (PC) is well-suited to address these complex PC needs and improve
quality of life (QOL), especially for physically frail people at risk for poor outcomes. The purpose
of this study was to examine unmet PC needs and their associations with health related QOL in
physically frail persons with HF.
Methods: We recruited a convenience sample of persons with HF from an urban hospital
system who were: >50 years old and had hospitalization in the last year. We excluded patients
who: had moderate/severe cognitive impairment, hospice, or non-English speaking. We
measured frailty using the FRAIL scale (0-5: 0 = robust, 1-2 = pre-frail, 3-5 = frail), PC needs
using the Integrated Palliative Outcome Scale (score 0-68; higher score = higher PC needs), and
health related QOL using the Kansas City Cardiomyopathy Questionnaire (0-100; higher scores =
better QOL). We performed multiple linear regression to test the relationships between
physical frailty, PC needs, and QOL and a subgroup analysis of four PC needs/frailty groups (high
PC needs/frail, high PC needs/robust, low PC needs/frail, low PC needs/robust).
Results: We enrolled 320 people, 292 completed surveys. Mean age was 68 (SD 9.8), 37% were
female (n=108), 28% identified as Black/African American (n=83), and 33% reported financial
strain (n=96). Participants averaged 2 hospitalizations per year. Only 5% of participants had a
documented PC consultation at any point during their illness trajectory. Most participants were
physically frail (44%, n=127) or pre-frail (41%, n=120). Mean PC needs score was 19.7 and frail
participants had a significantly higher mean PC needs score than pre-frail or robust participants.
Mean QOL score was 59.8 (range 17.5 to 91.7). For each 1 unit increase in palliative care needs,
quality of life decreased by 1.12 units (p<0.001), adjusting for covariates (age, comorbidities,
financial strain, education, race, gender, ejection fraction, and employment). Compared to
robust participants, physically frail participants (beta= -28.8, p<0.001) and pre-frail participants
(beta = -11.7, p<0.001) had significantly lower quality of life scores. In a subgroup analysis of 4
frailty/PC needs groups, physically frail participants with high PC needs had the lowest quality
of life score (beta = -28.6, p<0.001).
Conclusion: Physically frail and pre-frail people with HF have higher unmet PC needs and lower
QOL than robust people with HF. Physical frailty and PC needs screening in clinical settings may
improve identification of patients at highest risk for poor QOL amenable to PC intervention.
Poster 8

Feasibility of obtaining digital assessment of cognitive and physical function in older adults
presenting to the emergency department for falls using wearable accelerometers and
smartphones in the GAPcare II study
Elizabeth M. Goldberg, Roland C. Merchant, Linda J. Resnik, Sarah D. Berry, Samantha Roberts,
Vincent Mor, Andrew Leroux
Background: Digital assessment of cognitive and physical function using wearable sensors
and/or smartphones are increasingly deployed in studies of older adults. However, their use in
emergency departments (EDs) for patients presenting with falls has thus far been limited.
Measures derived from digital assessment have been shown to be highly predictive of health
outcomes in older adults, and evaluation in the ED may provide useful clinical insights into post-
fall outcomes. Our objective was to determine the feasibility of obtaining these measures in
older ED patients and their association with demographic data and validated assessments of
cognition and function.
Methods: Patients presenting in the ED for a fall were assessed for cognitive (Stroop, trail
making, and reaction time tests) and physical function (gait and balance, and timed walk).
Completion rates and outcomes for each test with valid data were examined marginally and
associated with age, demographic data (sex, educational attainment), cognitive impairment (Six
Item Screener), and functional independence (modified Barthel index), using a series of additive
logistic and linear regression models.
Results: Of 167 participants, comparatively more women were recruited than men (32.9%);
mean age of 78.5 (standard deviation = 7.7). Most participants reported at least some college
education (62.3%) and falling within the last 3 months (52.4%). Ten percent had cognitive
impairment (six item screener <= 4, 10.1%), and most reported some measure of dependence
(modified Barthel Index < 20, 69.9%). Completion rates for cognitive assessment tests were
moderately high (55-68%) and did not vary by age or demographic variables, but did vary by
cognitive impairment (p < 0.05, Stroop and trail making tests) or independence as measured by
the modified Barthel index (p < 0.05, reaction time). Completion rates for physical function
tests were substantially lower (16-18%), largely due to reluctance to mobilize after injury. Rates
did not vary by age, demographics, or cognitive impairment, but were significantly higher in
participants with functional independence (modified Barthel index of 20, p<0.01, gait and
balance, and timed walk tests). Associations of cognitive test results largely did not vary with
age or demographic variables, apart from education (p < 0.05) and longer time to complete the
trail making test among the oldest individuals in the sample (nonlinear association, p < 0.01).
Conclusions: Digital assessment of cognitive function using publicly available tools is feasible in
studies of older adults presenting to the ED for falls. Collection of physical function measures
presents more challenges. Future research should investigate whether such data, including the
ability and willingness to perform both cognitive and physical function tests, are independent
predictors of patient outcomes.
Poster 9
Title: Assessing the feasibility, acceptability, and preliminary efficacy of a novel
symptom management care delivery intervention for caregivers receiving home hospice
care.
V
eerawat Phongtankuel
a
, Taeyoung Park, Sara Czaja, Ritchell Dignam, Ronald Adelman, M.C.
Reid
D
ivision of Geriatrics and Palliative Medicine, Department of Medicine, Weill Cornell Medicine,
525 E 68th St Box 39, New York, NY, USA
B
ackground: Terminally ill patients experience high symptom burden at the end of life (EoL),
even when receiving hospice care. In the U.S., family caregivers play a critical role in managing
symptoms experienced by patients receiving home hospice services. Yet, most caregivers don’t
receive sufficient support or formal training in symptom management. Therefore, providing
additional visits and education to caregivers could potentially improve outcomes for both patient
and caregiver. In response, we developed the Improving Home hospice Management of End-of-
life issues through technology (I-HoME) intervention, a program designed for family caregivers
of home hospice patients. This paper describes the intervention, study design, and protocol
used to evaluate the intervention.
Methods: The I-HoME study is a pilot randomized controlled trial aimed at reducing patient
symptom burden through weekly tele-visits and education videos to benefit the patient’s family
caregiver. One hundred caregivers will be randomized to hospice care with (n=50) or without
(n=50) the I-HoME intervention. Primary outcomes include intervention feasibility (e.g., accrual,
attrition, use of the intervention) and acceptability (e.g., caregivers’ comfort accessing the tele-
visits and satisfaction). We will also examine preliminary efficacy using patient symptom burden
(as reported by the caregiver) and caregiver outcome measures (i.e., burden, depression,
anxiety, satisfaction).
C
onclusion: The trial is evaluating a novel symptom management intervention that supports
caregivers of patients receiving home hospice services. The intervention employs a multi-
pronged approach that provides needed services at a time when close contact and support is
crucial. This research could lead to advances in how care gets delivered in the home hospice
setting.
K
eywords: Hospice, caregivers, symptom management, technology, education
Poster 10

Multidimensional Representativeness of Older Adults with Atrial Fibrillation in Randomized Controlled Trials:
Comparing Participants of 12 Oral Anticoagulant RCTs to a Nationally Representative US Cohort
Sachin J Shah, MD, MPH (1); Timothy S. Anderson, MD, MAS (2); David Cheng, Ph.D. (1); Joseph S. Ross, MD, MHS
(3); FD Richard Hobbs, FMedSci (4); Stuart Connolly, MD (5);
Michael Ezekowitz MB, ChB, DPhil (6); Carl van Walraven, MD, MSc (7);
Daniel E. Singer, MD (1)
(1) Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
(2) Department of Medicine, Beth Israel Deaconess Medical Hospital, Boston, MA, USA
(3) Department of Medicine, Yale School of Medicine, New Haven, CT, USA
(4) Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford UK
(5) Population Health Research Institute, McMaster University, Hamilton, ON, Canada
(6) Department of Medicine, Thomas Jefferson University, Philadelphia, PA, USA and Cardiovascular
Medicine, Lankenau Institute for Medical Research, Wynnewood, PA, USA
(7) Departments of Medicine and Epidemiology & Community Medicine, University of Ottawa, Ottawa, ON,
CA
B
ackground: Anticoagulant RCTs are thought to have enrolled younger and less comorbid patients with atrial
fibrillation (AF) compared to the general population. We developed a representation score summarizing patient
characteristics to describe how well RCT participants with AF reflect a nationally representative cohort.
M
ethods: We studied adults >=65 years old with AF by harmonizing 2 data sources: (1) patient-level data from 12
landmark RCTs testing anticoagulants vs. placebo or antiplatelets from the Atrial Fibrillation Investigators (AFI)
consortium and (2) the Health and Retirement Study AF cohort (HRS-AF), a representative cohort of older adults
with AF in the U.S. We fit a logistic regression model to estimate the probability of inclusion in the HRS-AF cohort
in the pooled sample using age, height, weight, gender, heart failure, hypertension, diabetes, prior stroke, and
prior myocardial infarction. This estimate, the Trial Benchmark Score, reflected the probability of belonging to the
HRS-AF cohort and ranged from 0 to 1, with higher scores reflecting a greater likelihood of belonging to the HRS-AF
cohort. We plotted the distribution of scores for HRS-AF and AFI participants and compared the mean scores using
a t-test.
Res
ults: Compared to the HRS-AF cohort (n=3542), AFI participants (n=7933) were younger (72 vs. 76yrs,
standardized mean difference [SMD] -0.7), more frequently male (64% vs. 46%, SMD 0.3), and had a lower
likelihood of prior stroke (19% vs. 23%, SMD -0.4). The mean Trial Benchmark Score differed significantly between
the two cohorts (HRS-AF mean 0.47 vs. AFI mean 0.23, p<0.001) (Figure). 52% of HRS-AF participants and 12% of
AFI participants had a score >0.47 (the HRS-AF mean score).
C
onclusion: Differences in the Trial Benchmark Scores distributions indicate a substantial difference in the
distribution of observable characteristics and that RCT participants were not fully representative of the benchmark
population.
Poster 11
Dinner, Thursday, November 16, 2023, 7:00 – 9:00 pm, Cottonwoods
Table assignments by Cohort
Table 1 – 2023 Scholars and Travel Awardees
Table 2 – 2022 Scholars
Table 3 – 2021 and 2022 Scholars
Table 4 – 2020 and 2021 Scholars
Table 5 – 2019 Scholars
Table 6 – 2018 Scholars
Table 7 – 2016 and 2017 Scholars
Table 8 – 2010, 2011, 2012, 2014, 2015 Scholars
Table 9 – 2005, 2006, 2007, 2008 Scholars
Table 10 – 1995, 1998, 1999, 2000, 2001, 2004 Scholars
Table 11 – NIA, AFAR, Clin-STAR, speakers, etc.
Table 12 – NIA, AFAR, Clin-STAR, speakers, etc.
Each table is set for 10, some cohorts are larger than 10, some smaller. If you can’t
recall your cohort, see the table on the next page. Enjoy!

Dinner‐Thursday,November16,2023
7:00‐9:00pm,Cottonwoods
Name Last Year/affiliation Name Last Year/affiliation
Sandra Aleksic 2023 George Kuchel Clin‐STAR
Tim Anderson 2022 Mark Lachs 1995
Steven Austad AFAR Eleni Linos 2016
Alexis Bakos NIA Allison Magnuson 2019
Courtney Balentine 2021 Dan Matlock 2011
Robin Barr guest Meghan Mattos 2022
Randall Bateman 2007 Donovan Maust 2014
L.Michelle Bennett guest Rowena McBeath 2019
Miles Berger 2017 Brienne Miner 2021
Malaz Boustani 2005 Lona Mody Clin‐STAR
Charles Brown 2017 sean morrison 2000
Rebecca Brown 2018 John Newman 2014
Katie Buck 2022 Kei Ouchi 2020
Kate Callahan 2018 Veerawat Phongtankuel 2019
Alexander Chern TravelAwardee Hannah Polau
f
AFAR
Sevdenur Cizgine
r
2022 Jenny Portz 2018
Andrew Cohen 2018 Carolyn Presley 2021
Harvey Cohen Clin‐STAR Elizabeth Pritchett‐Montavon AFAR
Cathleen Colon‐Emeric 2004 Carmem Quatman 2021
ken covinsk
y
1999 Anais Rameau 2022
William Dale 2004 Miriam Rodriguez TravelAwardee
Lyndsay DeGroot TravelAwardee Jason Roh 2019
Kavita Dharmarajan 2021 Daniel Roh 2023
Elizabeth Dzeng 2022 Tony Rosen 2016
Nahed ElKassar NIA Catherine Sarkisian 2004
Sara Espinoza Clin‐STAR Katie Schenning 2022
Jason Falvey 2021 Nancy Schoenborn 2018
Lauren Ferrante 2017 Matthew Schrag 2019
Emily Finlayson 2006 Mina Sedrak 2022
Stacy Fischer 2006 Carolyn Seib 2021
Mikita Fuchita TravelAwardee Manish Shah 2006
ELIZABETH GOLDBERG 2019 Sachin Shah 2021
Parag Goyal 2020 Andrea Sherman AFAR
Meredith Greene 2019 Corey Simon 2022
Rasheeda Hall 2018 Indranil Sinha 2018
Duke Han 2012 Alex Smith 2012
Hattie Herman AFAR Leigh Smith TravelAwardee
Alison Huang 2011 Mike Steinman 2008
Lauren Hunt 2021 Caroline Stephens 2017
Makoto Ishii 2015 Nadia Sutton 2020
Anand Iyer 2020 Andrew Teich 2016
Felipe Jain 2020 Jasmine Travers 2021
Angela Jefferson 2007 Odette VanDerWilli
k
AFAR
Miyeon Jung 2022 Jennifer Vincenzo 2022
Shoshana Kahana NIA Molly Wagster NIA
Biren Kamdar 2018 Louise Walter Clin‐STAR
Sikandar Khan 2022 Heather Whitson 2008
Lisa Kilpela 2019 Melisa Wong 2019
Dae Kim 2015 kristine yaffe 2001
Amy Kind 2010 Raymond Yung 1998
Bharati Kochar 2023 Heidi Zapata 2019
ELISSA KOZLOV 2021 Susan Zieman NIA
Assignments by Mentor
Speed Mentoring
Friday, November 17, 8:00 - 9:00 am
Steve Austad - 1 Randy Bateman - 2 Malaz Boustani - 3 Harvey Cohen - 4 Cathleen Colon-Emeric - 5
8:00-8:20
Danny Roh Courtney Balentine Felipe Jain Sikandar Khan
Alexander Chern
8:20-8:40 Sandra Aleksic Meredith Greene Lauren Hunt Mina Sedrak Rowena McBeath
8:40-9:00 Rowena McBeath Jenny Portz
Vee Phongtankuel Danny Roh Sevde Cizginer
Ken Covinsky 6 William Dale - 7 Stacy Fischer - 8 Duke Han - 9 Alison Huang - 10
8:00-8:20 Jennifer Vincnzo Rasheeda Hall Lauren Hunt
Anand Iyer
Sachin Shah
8:20-8:40 kavita dharmarajan Matthew Schrag Carmen Quatman Brienne Miner Anais Rameau
8:40-9:00 Anand Iyer Miriam Rodriguez
Allison Magnuson Sachin Shah Matthew Schrag
Mac Ishii - 11 Dae Kim - 12 Amy Kind - 13 George Kuchel - 14 Mark Lachs - 15
8:00-8:20 Anais Rameau Meredith Greene Elizabeth Dzeng
Jason Roh
Miriam Rodriguez
8:20-8:40 Sachin Shah Biren Kamdar Jenny Portz Bharati Kochar Felipe Jain
8:40-9:00 Nancy Schoenborn Jennifer Vincenzo
Elissa Kozlov Sandra Aleksic Bharati Kochar
Eleni Linos - 16 Hillary Lum - 17 Lona Mody - 18 Alison Moore - 19 Sean Morrison - 20
8:00-8:20 Allison Magnuson kavita dharmarajan Mina Sedrak
Cevdenur Cizginer
Katie Schenning
8:20-8:40 Jennifer Vincenzo Nancy Schoenborn Miriam Rodriguez Carolyn Seib Alexander Chern
8:40-9:00 Elizabeth Dzeng Carmen Quatman Rasheeda Hall Katie Schenning Carolyn Seib
John Newman - 21 Tony Rosen - 22
Alex Smith -23 Caroline Stephens - 24
Louise Walter - 25
8:00-8:20 Sandra Aleksic Elissa Kozlov Biren Kamdar Vee Phongtankuel Bharati Kochar
8:20-8:40 Danny Roh Courtney Balentine Sevde Cizginer Rasheeda Hall Kate Callahan
8:40-9:00 Jason Roh Sikandar Khan Brienne Miner Alexander Chern Anais Rameau
Heather Whitson - 26 Ray Yung - 27
8:00-8:20 Brienne Miner
Kate Callahan
8:20-8:40 Katie Schenning
Elizabeth Dzeng
8:40-9:00 Meredith Greene Mina Sedrak
*Mentors, please sit at the assigned table number. We have scheduled 20 min for each session, but it will be ~17 minutes
of discussion, allowing 3 minutes for mentees to move to the next mentor.

Assignments by Mentee
Mentee
8:00 - 8:20 am
8:20 - 8:40 am 8:40 - 9:00 am
Sandra Aleksic John Newman - 21
Steve Austad - 1 George Kuchel - 14
Courtney
Balentine
Randy Bateman - 2 Tony Rosen - 22
Kate Callahan Ray Yung - 27 Louise Walter - 25
Alexander Chern Cathleen Colon-Emeric - 5 Sean Morrison - 20 Caroline Stephens - 24
Sevdenur Cizginer Alison Moore - 19
Alex Smith -23 Cathleen Colon-Emeric - 5
kavita dharmarajan Hillary Lum - 17
Ken Covinsky 6
Elizabeth
Dzeng Amy Kind - 13 Ray Yung - 27 Eleni Linos - 16
Meredith
Greene Dae Kim - 12 Randy Bateman - 2 Heather Whitson - 26
Rasheeda Hall
William Dale - 7 Caroline Stephens - 24 Lona Mody - 18
Lauren Hunt Stacy Fischer - 8 Malaz Boustani - 3
Anand Iyer Duke Han - 9 Ken Covinsky 6
Felipe Jain Malaz Boustani - 3 Mark Lachs - 15
Biren
Kamdar Alex Smith -23 Dae Kim - 12
Sikandar Khan Harvey Cohen - 4 Tony Rosen - 22
Bharati Kochar Louise Walter - 25
George Kuchel - 14 Mark Lachs - 15
Elissa Kozlov Tony Rosen - 22 Amy Kind - 13
Allison Magnuson Eleni Linos - 16 Stacy Fischer - 8
Rowena McBeath Cathleen Colon-Emeric - 5 Steve Austad - 1
Brienne Miner Heather Whitson - 26 Duke Han - 9 Alex Smith -23
Veerawat
Phongtankuel Caroline Stephens - 24 Malaz Boustani - 3
Jenny Portz Amy Kind - 13 Randy Bateman - 2
Carmen Quatman Stacy Fischer - 8 Hillary Lum - 17
Anaïs Rameau Mac Ishii - 11 Alison Huang - 10 Louise Walter - 25
Miriam Rodriguez Mark Lachs - 15 Lona Mody - 18 William Dale - 7
Danny Roh Steve Austad - 1 John Newman - 21 Harvey Cohen - 4
Jason Roh George Kuchel - 14 John Newman - 21
Katie Schenning
Sean Morrison - 20 Heather Whitson - 26 Alison Moore - 19
Nancy Schoenborn Hillary Lum - 17 Mac Ishii - 11
Matthew Schrag William Dale - 7 Alison Huang - 10
Mina Sedrak
Lona Mody - 18 Harvey Cohen - 4 Ray Yung - 27
Carolyn Seib Alison Moore - 19 Sean Morrison - 20
Sachin Shah Alison Huang - 10 Mac Ishii - 11 Duke Han - 9
Jennifer Vincenzo Ken Covinsky 6 Eleni Linos - 16 Dae Kim - 12

Sandra Aleksic, MD
Assistant Professor, Einstein College of Medicine
The Role of Hypothalamic Dysfunction in Accelerating Aging in Humans
Lindsay Hampson, MD, MAS
Associate Professor of Urology,
University of California, San Francisco
Improving Patient-Centered Decision-Making for
Stress Urinary Incontinence Treatment in Older Men

Bharati Kochar, MD, MS
Assistant Professor of Medicine,
Massachusetts General Hospital
Incorporating Geriatric Constructs into Management of
Inflammatory Bowel Diseases in Older Adults
Daniel Roh, MD, PhD
Assistant Professor of Surgery, Boston University
Chobanian & Avedisian School of Medicine
Targeting Senescence to Improve Wound Healing in Aging

| 2023 BEESON TRAVEL AWARDEES |
Alexander Chern, MD
Fellow, Johns Hopkins University
Lyndsay DeGroot, PhD, RN, CNE
Postdoctoral Fellow, University of Colorado School of Medicine
Mikita Fuchita, MD
Assistant Professor, University of Colorado
Miriam Rodriguez, PhD
Associate Professor, Indiana University School of Public Health
Lauren Leigh Smith, MD, MAS
Assistant Professor, University of Maryland School of Medicine
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST: LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Leah Acker
Duke University GEMSSTAR
Delirium, Cognitive Neuroscience, Resilience, Attention,
Neuromodulation, Neuroimmunology
Sandra Aleksic
Einstein College of Medicine Beeson Scholar sandra.aleksic@einsteinmed.edu
hypothalamus, MRI, endocrine system, cognitive aging,
frailty, human, proteome
Timothy Anderson
University of Pittsburgh Beeson Scholar tsander@pitt.edu
pharmacoepidemiology, deprescribing, transitions of care,
hospital medicine, primary care
Claire Ankuda
Icahn School of Medicine at Mount
Sinai
Beeson Scholar claire.ankuda@mssm.edu Palliative care, Medicare, Medicare Advantage
Andrew Artz
City of Hope Clin-STAR aartz@coh.org
Hematology, Transplantation, Geriatric Assessment, Multi-
disciplinary Teams, Older Adults
Steven Austad
University of Alabama at Birmingham Staff [email protected]du
Laura Baehr
Temple University College of Public
Health Dept Health Rehabilitation
Health Equity
Scholar
laura.baehr@temple.edu
spinal cord injury; physical activity; self-efficacy; digital
health
Alexis Bakos
National Institute on Aging NIA alexis.bakos@nih.gov Palliative care/symptom science; health disparities
Courtney Balentine
University of Wisconsin Madison Beeson Scholar
balentine@surgery.wisc.edu surgery, implementation science, clinical trials
Ayomide Bankole
UNC Chapel Hill
Health Equity
Scholar
Abankole@unc.edu
aging in place; home-based care; transitional care; shared
decision making; health equity; multiple chronic conditions
Robin Barr
Geeontological Society of America Honorary Staff robmattles@gmail.com Aging, of course
Randall Bateman
Washington University Sch. of Med.
Beeson alumni batemanr@neuro.wustl.edu
Michelle Bennett
Roger Schwarz & Associates SPEAKER LMBen[email protected]
Miles Berger
Anesthetic pharmacology, delirium, perioperative
neurocognitive disorders, Alzheimer’s disease, APOE4
Marie Bernard
National Institutes of Health SPEAKER
marie.bernard@nih.gov
Tasce Bongiovanni
UCSF
Health Equity
Scholar
tasce.bongiovanni@ucsf.edu surgery, postoperative care, pain management
Malaz Boustani
Indiana Univ. Sch. of Med./Regenstrief
Inst., Inc.
Clin-STAR; Beeson
alumn
Jennifer Brach
Univ. of Pittsburgh School of Health
and Rehabilitation Sciences
Clin-STAR; Beeson
alumn
Charles Brown
Johns Hopkins University Beeson Scholar cbrownv@jhmi.edu anesthesia, delirium, POCD, surgery
Rebecca Brown
University of Pennsylvania Beeson Scholar rebecca.brown@pennmedicine.upenn.edu
Functional status, housing, marginalized populations,
epidemiology, implementation science, housing-based
Katherine Buck
The Ohio State University Beeson Scholar Katherine.Buck@osumc.edu emergency medicine, pneumonia, diagnostics
Kathryn Callahan
Wake Forest School of Medicine Beeson Scholar kecallah@wakehealth.edu frailty, function, implementation science
Anne Cappola
Perelman Sch. of Med. at the Univ. of
Pennsylvania
Clin-STAR acappola@pennmedicine.upenn.edu Hormones, frailty, women's health
Christopher Carpenter
Mayo Clinic Rochester Clin-STAR carpenter.christopher@mayo.edu
Implementation Science, Emergency Medicine, diagnostics,
clinical practice guidelines, EQUATOR Network
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Stephanie Cham
University of California San Francisco
Clin-STAR Travel
Awardee
stephanie.cham@ucsf.edu
Gynecologic oncology, surgery, oncology, frailty, functional
recovery, patient centered outcomes
Anita Chary
Baylor College of Medicine GEMSSTAR anita.chary@bcm.edu
emergency care, delirium, dementia, cognitive impairment,
geriatric screening, implementation science, qualitative
Po-Jung Chen
University of Nebraska Medical Center GEMSSTAR pchen@unmc.edu
Alexander Chern
Johns Hopkins University
Beeson Travel
Awardee
achern1@jh.edu
Age-related hearing loss, cognition, epidemiology, qualitative
methods, music perception and enjoyment
Sevdenur Cizginer Konuk
Massachusetts General Hospital Beeson Scholar scizgin[email protected]rvard.edu
Geriatric surgery, Colorectal surgery, Qualitative research
Andrew Cohen
Yale University
Beeson Scholar;
Clin-STAR speaker;
Andrew.b.cohen@yale.edu
Medical decision-making for persons with dementia,
surrogate decision-making, unrepresented ("unbefriended")
Harvey Cohen
Center For The Study Of Aging Clin-STAR [email protected]
Cancer and Aging, Functional Status, resilience, aging and
function biomarkers.
Cathleen Colon-Emeric
Duke University Medical Center Beeson alumni colon001@mc.duke.edu
fracture, osteoporosis, nursing home, injurious falls,
resilience
Kenneth Covinsky
Univ. of California, San Francisco
School of Medicine
Beeson alumni
covinsky@medicine.ucsf.edu Disability; prognosis; dementia
William Dale
City of Hope Beeson alumni
#Cancer #Aging #Medical Decision Making #Geriatric
Assessment #Supportive Care
William Deardorff
skilled nursing facility, post-acute care, long-term care,
prediction model, prognosis
Lyndsay DeGroot
University of Colorado School of
Medicine
Beeson Travel
Awardee
lyndsay.degroot@cuanschutz.edu Palliative care, heart failure, aging, nursing
Arjune Dhanekula
University of Washington
Clin-STAR Travel
Awardee
adhaneku@uw.edu
Aortic surgery, cardiac surgery, aging, aortic aneurysm, aortic
dissection, aortic disease, cardiology
Kavita Dharmarajan
Icahn School of Medicine at Mount
Sinai
Beeson Scholar kavita.dharmarajan@mountsinai.org palliative care, geriatric oncology
Pamela Dunlap
University of Pittsburgh Clin-STAR
dunlappm@pitt.edu
Rehabilitation, Physical Therapy, Vestibular, Implementation
Science
Elizabeth Dzeng
University of California, San Francisco
Beeson Scholar;
Clin-STAR
liz.dz[email protected]du
institutional cultures, health policy, equity, structural racism,
community-based participatory research methods,
Nahed El Kassar
National Institute on Aging, NIH NIA nahed.elkassar@nih.gov
Sara Espinoza
Cedars-Sinai Medical Center Clin-STAR sara.espi[email protected] frailty, geroscience, clinical trials
Hina Faisal
Houston Methodist Academic Institute GEMSSTAR hfaisal@houstonmethodist.org Delirium, Digital technology, virtual/augmented reality
Jason Falvey
University of Maryland School of
Medicine
Beeson Scholar JFalvey@som.umaryland.edu
Traumatic injury, neighborhood socioeconomic
disadvantage; community mobility; rehabilitation; falls;
Adam Faye
NYU Grossman School of Medicine GEMSSTAR adam.faye@nyulangone.org
Inflammatory bowel disease, Preoperative care, Frailty,
Sarcopenia
Lauren Ferrante
Yale School of Medicine Beeson Scholar [email protected] critical illness, functional outcomes, disability, post-ICU
Emily Finlayson
Univ. of California, San Francisco Committee Emily.Finlayson@ucsf.edu surgery; prehabilitation
Stacy Fischer
Univ. of Colorado Denver Beeson alumni [email protected]
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Terri Fried
Yale University School of Medicine
Clin-STAR; Beeson
alumn
Ari Friedman
University of Pennsylvania GEMSSTAR ari.friedman@pennmedicine.upenn.edu
geriatric emergency medicine, health economics, cognitive
frailty
David Friedmann
New York University GEMSSTAR David.Friedmann@nyulangone.org Hearing loss
Mikita Fuchita
University of Colorado
Beeson Travel
Awardee
mikita.fuchita@cuanschutz.edu
Sedation, delirium, and early mobility in the ICU; post-
intensive care syndrome; patient-centered care;
Elizabeth Goldberg
University of Colorado Beeson Scholar elizabeth.goldberg@cuanschutz.edu
fall prevention, digital health, clinical trials
Parag Goyal
Weill Cornell Medicine Beeson Scholar pag9051@med.cornell.edu cardiology, heart failure, polypharmacy, deprescribing
Meredith Greene
Matthew Growdon
University of California, San Francisco GEMSSTAR matthew.growdon@ucsf.edu
Dementia
Prescribing quality and deprescribing
Rasheeda Hall
Duke University Medical Center Beeson Scholar
S. Duke Han
USC Keck School of Medicine Beeson alumni
dukehan@usc.edu
cognition, decision making, Alzheimer's
Hattie Herman
AFAR Staff hattie@afar.org
Alison Huang
University of California, San Francisco
Beeson alumni Alison.Huang@ucsf.edu
urinary incontinence, menopause, genitourinary aging,
women's health, clinical trials
Megan Huisingh-Scheetz
University of Chicago School of
Medicine
Clin-STAR megan.huisingh-scheetz@uchospitals.edu
frailty, technology, exercise, social engagement,
accelerometry, voice-activated devices, older adult-care
Lauren Hunt
University of California, San Francisco Beeson Scholar Lauren.Hunt@ucsf.edu hospice, dementia, policy and health services research
Angela Ingraham
University of Wisconsin-Madison GEMSSTAR
Dina Ioffe
Fox Chase Cancer Center Clin-STAR
dina.ioff[email protected]u
Gastrointestinal cancers, geriatric oncology, health disparities
Makoto Ishii
UT Southwestern Medical Center Beeson alumni Makoto.Ishii@UTSouthwestern.edu
Alzheimer's disease, hypothalamus, mouse models,
biomarker, metabolism
Anand Iyer
University of Alabama at Birmingham Beeson Scholar aiyer@uabmc.edu
implementation science, intervention development, COPD,
geriatrics, palliative care, behavioral research
Snigdha Jain
Yale University School of Medicine GEMSSTAR Snigdha.Jain@yale.edu
Digital Health, Exercise Interventions, Functional Recovery,
Critical Illness, Patient-Centered Outcomes
Felipe Jain
Harvard Medical School and
Massachusetts General Hospital
Beeson Scholar felipe.jain@mgh.harvard.edu
family caregivers, digital phenotyping, mHealth,
neuroimaging, dementia, depression, stress, mindfulness,
Dejan Jakimovski
University at Buffalo Clin-STAR dejanjak@buffalo.edu aging in neurology, imaging in aging, multiple sclerosis
Angela Jefferson
Vanderbilt University Medical Center
Clin-STAR; Beeson
Committee
angela.jefferson@vumc.org neuropsychology, Alzheimer’s disease, vascular risk factors
Elizabeth Joe
Teresa Jones
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Miyeon Jung
Indiana University School of Medicine Beeson Scholar
miyjung@iu.edu
Cognitive interventions, virtual reality, clinical trials, mild
cognitive impairment, heart failure
Shoshana Kahana
National Institute on Aging, NIH NIA shoshana.kahan@nih.gov
Biren Kamdar
University of California, San Diego
School of Medicine
Beeson Scholar kamdar@ucsd.edu
critical care, delirium, sleep-wake rhythms, implementation
science
Hadiza Kazaure
DUKE UNIVERSITY GEMSSTAR hadiza.kazaure@duke.edu surgery, outcomes, cognition
Sikandar Khan
Indiana University School of Medicine Beeson Scholar sikhan@iu.edu
critical illness, delirium, acute respiratory failure, post-
intensive care syndrome, post-ICU aging, oxidative stress
Lisa Kilpela
University of Texas Health Science
Center San Antonio
Beeson Scholar kilpela@uthscsa.edu
women's health; nutrition pathology; health behavior
change; mental health
Dae Hyun Kim
Harvard Medical School Beeson alumni dhk000@mail.harvard.edu
Frailty, Medicare Data, Pharmacoepidemiology, Health
Services Research
Amy Jo Kind
University of Wisconsin-Madison Beeson alumni ajk@medicine.wisc.edu
Health Disparities; Social Exposome; Alzheimer's Disease;
Area Deprivation Index (ADI) and Neighborhood Atlas;
Bharati Kochar
Massachusetts General Hospital Beeson Scholar
bkochar@mgh.harvard.edu
inflammatory bowel disease; Crohn's disease, ulcerative
colitis, gastroenterology; frailty; risk stratification;
Elissa Kozlov
Rutgers School of Public Health Beeson Scholar
Elissa.Kozlov@rutgers.edu
Mental Health, Dyads, Caregiving, serious illness, palliative
care
George Kuchel
Univ. of Connecticut Health Center Clin-STAR kuchel@uchc.edu Geroscience; Geriatric Syndromes; Immunology; Vaccines
Mark Lachs
Weill Med. Col. of Cornell University
Alumni Committee mslachs@med.cornell.edu elder abuse
Kenneth Lam
University of California, San Francisco GEMSSTAR kenneth.lam@cuanschutz.edu
Long-term care, post-acute care, mixed methods, functional
measures, disability
Emily Largent
University of Pennsylvania Clin-STAR speaker elargent@pennmedicine.upenn.edu Ethics, health policy, digital health, biomarkers
Andrea Levine
UNIVERSITY OF MARYLAND
BALTIMORE
GEMSSTAR
Andrea.Levine@som.umaryland.edu
Acute Respitory Distress Syndrome (ARDS), inflammatory
biomarkers, subphenotypes of ARDS, inflammaging
Lingsheng Li
UCSF
Health Equity
Scholar
Lingsheng.Li@ucsf.edu
Advance care planning
Asian American Pacific Islander Older Adults
Sarah Lieber
Hospital for Special Surgery GEMSSTAR liebers@HSS.EDU Systemic lupus erythematosus; aging; physical activity; frailty
Eleni Linos
Stanford University Beeson alumni linos@stanford.edu
Rachel Litke
Mount Sinai Dept Neuroscience GEMSSTAR Rachel.li[email protected]
Alzheimer's disease, C. elegans, pharmaco-epidemiology,
geriatric endocrinology, diabetes technology
Melissa (Kah Poh) Loh
University of Rochester Medical
Center
GEMSSTAR kahpoh_loh@urmc.rochester.edu
geriatric hematology, digital health, epigenetics, supportive
care and behavioral interventions, shared decision making,
Hillary Lum
University of Colorado, Denver and VA
Eastern Colorado GRECC
Beeson alumni hillary.lum@cuanschutz.edu
dementia, caregiving research, advance care planning,
geriatric palliative care, implementation science, mHealth,
Nancy Lundebjerg
American Geriatrics Society Clin-STAR nlundebjerg@americangeriatrics.org governance; caregiving; fundraising; communications;
John Mafi
University of California, Los Angeles Beeson Scholar jmafi@mednet.ucla.edu
Access, quality, and costs of medical care, health policy, low-
value care
Allison Magnuson
University of Rochester Beeson Scholar allison_magnuson@urmc.rochester.edu Geriatric Oncology
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Edward Manning
Yale University and the VA GEMSSTAR
edward.manning@yale.edu Vasculature, Pulmonary, Right Ventricle, Senescence
Maria Marquine
Duke University Clin-STAR maria.marquine@duke.edu DEIA
Daniel Matlock
University of Colorado Denver Committee daniel.matlock@ucdenver.edu Shared Decision Making, Implementation Science
Meghan Mattos
University of Virginia Beeson Scholar ms2bv@virginia.edu
Dementia, Alzheimer’s disease, sleep, digital health,
intervention
Donovan Maust
University of Michigan
Committee;
Beeson alumni
maustd@umich.edu
dementia, psychotropic, deprescribing, Medicare, VA
Rowena McBeath
Jefferson University Beeson Scholar rowena.mcbeath@gmail.com
tendinosis, hypoxia, senescence, RhoA small GTPase, Rac1
GTPase, HIF1alpha
Shannon McCurdy
University of Pennsylvania GEMSSTAR shannon.mccurdy@pennmedicine.upenn.edu
Frailty, Allogeneic Transplantation, Post-transplant
cyclophosphamide
Brienne Miner
Yale University Beeson Scholar brienn[email protected] sleep, aging, Alzheimer's disease, patient-centered outcomes
Lona Mody
University of Michigan Clin-STAR
lonamody@med.umich.edu
Infection and Aging, translational research, mentorship,
women in medicine
Alison Moore
University of California, San Diego
Clin-STAR; Beeson
alumn
alisonmoor[email protected]
aging, substance use, disparities, mentorship, age-friendly
health systems, technology and aging, healthy aging
R. Sean Morrison
Icahn School of Medicine at Mount
Sinai
Beeson alumni sean.mo[email protected]u
Christopher Mosher
Duke University
GEMSSTAR christopher.mosher@duke.edu exercise, rehabilitation, immunology, COPD
Anand Naik
University of Texas Health Science
Center at Houston (UTHealth Houston)
Clin-STAR speaker aanand.naik@uth.tmc.edu
Multiple Morbidities; Patient-Centered Care; Patient-Clinician
Encounter; Population Health Systems
John Newman
Buck Institute for Research on Aging Beeson alumni jnewman@buckinstitute.org
Geroscience, metabolism, delirium, ketone, frailty,
translational
An Nguyen
Cedars-Sinai; GW University
Health Equity
Scholar
an.nguyen@cshs.org
occupational therapy, telehealth, implementation science,
transitions of care, Alzheimer's disease and related
Lolita Nidadavolu
JHMI GEMSSTAR lnidada1@jhmi.edu
Inflammation, mild cognitive impairment, biomarkers,
microglia
Unwanaobong Nseyo
Weill Cornell Medicine
Clin-STAR Travel
Awardee
unn2001@med.cornell.edu
overactive bladder, urinary UI, racial/ethnic minority, health
disparities, barriers/access to care
Kei Ouchi
Brigham and Women's Hospital and
Harvard Medical School
Beeson Scholar kouchi@bwh.harvard.edu
emergency medicine, palliative care, serious illness
communication, advance care planning
Deborah Oyeyemi Walton
University of California Los Angeles
Clin-STAR Travel
Awardee
doyeyemiwalton@mednet.ucla.edu
Alzheimer's Disease, Dementia, Assistance Networks, Aging-
in-Place, Caregiving, Health Disparities
Krishna Patel
ICAHN SCHOOL OF MEDICINE AT
MOUNT SINAI
GEMSSTAR Krishna.Patel5@mountsinai.org
Ischemic heart disease, cardiac imaging, frailty, decision
support
Darina Petrovsky
Rutgers School of Nursing
Health Equity
Scholar
darina.petrovsky@rutgers.edu
caregiving, music, nonpharmacological interventions,
dementia, clinical trials
Veerawat Phongtankuel
Joan & Sanford I. Weill Medical College
of Cornell University
Beeson Scholar vep9012@med.cornell.edu Hospice, caregiving, symptom management, palliative care
Hannah Polauf
AFAR Staff [email protected]g
Jennifer Portz
University of Colorado Beeson Scholar jennifer.portz@cuanschutz.edu social work, palliative care, caregivers, digital health
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Carolyn Presley
The Ohio State University
Comprehensive Cancer Center
Beeson Scholar
carolyn.presley@osumc.edu
geriatric and thoracic oncology; supportive care
interventions; lung cancer survivorship; IPE programmatic
Suzanne Prevost
University of Alabama at Birmingham Clin-STAR [email protected] Pain, Palliative Care, Nursing Education
Elizabeth Pritchett-Montavon
AFAR Staff elizabet[email protected]g
Sarah Psutka
University of Washington GEMSSTAR spsutka@uw.edu
Geriatric Assessment, Frailty, Resilience, Bladder Cancer,
Kidney Cancer, Surgical Risk, Functional Decline
Carmen Quatman
The Ohio State University Wexner
Medical Center
Beeson Scholar carmen.quatman@osumc.edu
Falls, Frailty, Cognitive Impairment, Emergency/Trauma,
Fractures
Anais Rameau
Weill Cornell Medicine Beeson Scholar anr2783@med.cornell.edu swallowing, dysphagia, voice
Elizabeth Regan
University of South Carolina
Clin-STAR Travel
Awardee
eregan@mailbox.sc.edu
exercise, physical activity, mobility impairments, community
research
Raele Robison
University of Wisconsin-Madison
Health Equity
Scholar
rrobison@wisc.edu Dysphagia, Health Equity, Dementia
Miriam Rodriguez
Indiana University
Beeson Travel
Awardee
mijrodri@iu.edu
Health disparities in Alzheimer's disease and related
dementias (ADRD), Hispanic/Latino ADRD patients and
Nicole Rogus-Pulia
University of Wisconsin-Madison Beeson Scholar
npulia@wisc.edu
Swallowing, Dysphagia, Alzheimer's Disease, Rehabilitation,
Speech-Language Pathology, Frailty
Jason Roh
Massachusetts General Hospital Beeson Scholar jroh@mgh.harvard.edu Wound healing, senescence, tissue repair
Daniel Roh
Boston University Chobanian &
Avedisian School of Medicine
Beeson Scholar [email protected] Cardiovascular aging, geroscience, heart failure
Karen Rose
The Ohio State University Clin-STAR rose.1482@osu.edu
dementia
caregiving
Anthony Rosen
Weill Cornell Medical College Beeson alumni aer2006@med.cornell.edu
elder abuse; elder mistreatment' geriatric emergency
medicine
Jessica Rove
University of Colorado
Clin-STAR Travel
Awardee
Daniel Rubin
University of Chicago GEMSSTAR drubin@dacc.uchicago.edu
physical activity, walking cadence, smartphones,
accelerometers, prehabilitation
Marcel Salive
multimorbidity, comparative effectiveness, Alzheimer's
disease, medical decision-making;
Catherine Sarkisian
UCLA Beeson alumni csarkisian@mednet.ucla.edu
reducing low-value care, health system science, pragmatic
trials, health disparities research
Nandini Sarma
Oregon Health and Science University
Health Equity
Scholar
sarma@ohsu.edu Health equity, disparities, critical care
Katie Schenning
Oregon Health & Science University Beeson Scholar malcore@ohsu.edu
postoperative neurocognitive disorders, frailty, delirium,
surgery, anesthesiology
Nancy Schoenborn
Johns Hopkins University Beeson Scholar nancyli@jhmi.edu
Decision-making; communication; messaging; de-
implementation; prognosis; cancer screening; deprescribing
Matthew Schrag
Vanderbilt University School of
Medicine
Beeson Scholar matthew.schrag@vanderbilt.edu Alzheimer's disease, cerebral amyloid angiopathy
Margaret Schwarze
University of Wisconsin-Madison Clin-STAR schwarze@surgery.wisc.edu
surgical decision making, informed consent, advance
directives and end-of-life care
Mina Sedrak
UCLA Beeson Scholar MSedrak@mednet.ucla.edu Cancer, Aging, Geroscience
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Carolyn Seib
Stanford University School of Medicine Beeson Scholar
cseib@stanford.edu
Geriatric surgery, surgical decision support, endocrine
disorders of aging
Benjamin Seligman
UCLA GEMSSTAR BSeligman@mednet.ucla.edu
Frailty, Vaccination, Social Determinants of Health,
Geroscience
Manish Shah
University of Wisconsin School of
Medicine & Public Health
Clin-STAR; Beeson
Committee
mnshah@medicine.wisc.edu emergency medicine, aging, community paramedicine
Sachin Shah
Massachusetts General Hospital Beeson Scholar sshah@mgh.harvard.edu
high risk/high reward clinical decisions, anticoagulants, atrial
fibrillation, lecanemab, generalizability of clinical trials to
Kerry Sheets
Hennepin Healthcare
Clin-STAR Travel
Awardee
kerry.[email protected]
Dementia, Functional decline, Health equity, HIV and aging
Andrea Sherman
AFAR Staff andrea@afar.org
Sandra Shi
Hebrew Senior Life GEMSSTAR sandras[email protected]d.edu
Frailty, Post-acute care, Skilled Nursing Facilities,
Rehabilitation
Corey Simon
Duke University Beeson Scholar corey.simon@duke.edu pain, inflammation, stress
Namrata Singh
UNIVERSITY OF WASHINGTON GEMSSTAR
nasingh@medicine.washington.edu Rheumatoid arthritis, Frailty, Sarcopenia, Cancer outcomes
Indranil Sinha
Harvard Medical School/ Brigham and
Women's Hospital
Beeson Scholar
isinha@bwh.harvard.edu
Rachel Skains
UABMC GEMSSTAR rskains@uabmc.edu
geriatric emergency medicine, delirium, cognitive
impairment, risk factors, prevention, medication safety
Lauren Leigh Smith
University of Maryland School of
Medicine
Beeson Travel
Awardee
[email protected]maryland.edu
infection control and prevention, nursing facilities, multi drug
resistant organisms
Alexander Smith
Univ. of California, San Francisco Beeson alumni aksmith@ucsf.edu
Palliative Care, JAGS, Bioethics, Hospice, Disability, Dementia,
Mentoring, Podcasting, Campfire sing alongs.
Sarah Smith
Wash U GEMSSTAR [email protected]u
postoperative delirium, circadian rhythms, anesthesia, critical
care
Germine Soliman
University of Connecticut Center on
Aging
Clin-STAR Travel
Awardee
soliman@uchc.edu Geroscience, cellular senescence, senolytics, palliative care.
Michael Steinman
University of California, San Francisco
School of Medicine
Beeson alumni mike.steinman@ucsf.edu
medication appropriateness, improving prescribing quality,
pharmacoepidemiology, multimorbidity
Caroline Stephens
University of Utah College of Nursing Beeson alumni Caroline.Stephens@nurs.utah.edu
nursing home, palliative care, telehealth, caregiving,
population science,
Brocha Stern
Icahn School of Medicine at Mount
Sinai
Clin-STAR Travel
Awardee
brocha.stern@mountsinai.org
Perioperative care; Occupational therapy; Orthopedics;
Patient-reported outcome measures
Nadia Sutton
Vanderbilt University Medical Center Beeson Scholar nadia.sutton@vumc.org vascular aging
Andrew Teich
Columbia University Beeson alumni [email protected]mbia.edu Alzheimer's disease, neuropathology
Roland Thorpe
Johns Hopkins University Clin-STAR; speaker rthorpe@jhu.edu
gerontology, social epidemiology, minority aging, men’s
health, and place-based disparities
Jasmine Travers
New York University Rory Meyers
College of Nursing
Beeson Scholar jt129@nyu.edu
long-term care, nursing homes, workforce issues, equity, care
quality
Odette Van Der Willik
American Federation for Aging
Research
Staff odette@afar.org
Jennifer Vincenzo
University of Arkansas for Medical
Sciences
Beeson Scholar;
Clin-STAR
jlvincenzo@uams.edu
implementation science, rehabilitation, fall prevention,
health promotion
2023 Clin-STAR and Beeson Meetings
Contact List
FIRST:
LAST:
INSTITUTION: ROLE E-MAIL:
research insterest key words
Elena Volpi
University of Texas Medical Branch Clin-STAR
evolpi@UTMB.EDU N/A
Molly Wagster
National Institute on Aging NIA wagsterm@nia.nih.gov
Aging Brain
Cognitive Neuroscience
Louise Walter
University of California, San Francisco
and San Francisco VA Health Care
Clin-STAR Lou[email protected].edu
cancer screening in older adults, prognostication, geriatric
oncology
Heather Whitson
Duke University School of Medicine Beeson alumni heather.whit[email protected]du Alzheimer's disease, sensory health, resilience
Melisa Wong
University of California, San Francisco Beeson Scholar melisa.wo[email protected]rg
geriatric oncology, lung cancer, functional status, shared
decision making, clinical prediction
Kristine Yaffe
Univ. of California, San Francisco
Clin-STAR; Beeson
Committee
Raymond Yung
University of Michigan Medical School Beeson alumni ryung@umich.edu Rheumatology, inflammation, geroscience
Heidi Zapata
Yale School of Medicine Beeson Scholar heidi.zapata@yale.edu HIV and Aging, Innate Immune System,
Johnson (Qiang) Zhang
University of Iowa GEMSSTAR
qiang-zhang@uiowa.edu
multiple sclerosis, biological aging, immunosenescence,
frailty, MRI
Yinan Zhang
Ohio State University GEMSSTAR
yinan.zhang@osumc.edu
Alzheimer's disease, Glycolysis, Terazosin, ATP,
metabolomics, Transgenic mouse model
Audrey Zhang
Duke University School of Medicine
Clin-STAR Travel
Awardee
audrey.d.zhang@gmail.com
Improving quality of care for older adults with multiple
chronic conditions, with a focus on improving prescribing and
Susan Zieman
National Institute on Aging/ NIH
NIA susan.ziema[email protected]ov
Cardiovascular aging, vascular aging, heart failure with
preserved function, aging/geriatrics research in medical and

Zoom Instructions
• Make sure your Zoom application is up to date https://support.zoom.us/hc/en-
us/articles/201362233-Upgrading-Zoom-to-the-latest-version
• Clin-STAR and Beeson plenary sessions can be accessed through Zoom using this link
(same for all days):
https://us02web.zoom.us/j/86471125703?pwd=NmlRLzY1ZVVrZk9sR0E2azdpR3gzZz09
• Use this link to download and import the following iCalendar (.ics) files to your calendar
system:
https://us02web.zoom.us/webinar/tZIpcOiprD4tGtcXis9n_jAp7P04CoxDM5u1/ics?icsToken=98t
yKuGuqjwrG9aQtxmERpwABo_Cd-vzpiVajbdepBb2Wi5saCLmYdISZpFwCPz9
• When: Nov 15, 2023 08:30 AM Mountain Time (US and Canada)
Nov 16, 2023 09:00 AM
Nov 17, 2023 08:30 AM
Please note the calendar invites will cover from the beginning of the first virtual session
to the end of the final virtual session each day. There is not a way to specify each
session on each day.
• Additional Zoom dial-in details: Please click the link below to join the webinar:
https://us02web.zoom.us/j/86471125703?pwd=NmlRLzY1ZVVrZk9sR0E2azdpR3gzZz09
Passcode: 305453
Or One tap mobile :
+16469313860,,86471125703#,,,,*305453# US
+16465588656,,86471125703#,,,,*305453# US (New York)
Or Telephone:
Dial(for higher quality, dial a number based on your current location):
Or Telephone:
Dial(for higher quality, dial a number based on your current location):
US: +1 646 931 3860 or +1 646 558 8656 or +1 309 205 3325 or +1 312 626 6799 or
+1 301 715 8592 or +1 564 217 2000 or +1 669 444 9171 or +1 669 900 9128 or +1 689
278 1000 or +1 719 359 4580 or +1 253 215 8782 or +1 346 248 7799 or +1 360 209
5623 or +1 386 347 5053 or +1 507 473 4847
Webinar ID: 864 7112 5703
Passcode: 305453
International numbers available: https://us02web.zoom.us/u/kbyxKQwOtI
