
healthy through habit:
Interventionsforinitiating
& maintaining health
behavior change
Wendy Wood & David T. Neal
abstract
Interventions to change health behaviors have had
limited success to date at establishing enduring healthy
lifestyle habits. Despite successfully increasing people’s
knowledge and favorable intentions to adopt healthy
behaviors, interventions typically induce only short-
term behavior changes. Thus, most weight loss is
temporary, and stepped-up exercise regimens soon
fade. Few health behavior change interventions have
been successful in the longer term. In this article,
we unpack the behavioral science of health-habit
interventions. We outline habit-forming approaches
to promote the repetition of healthy behaviors, along
with habit-breaking approaches to disrupt unhealthy
patterns. We show that this two-pronged approach—
breaking existing unhealthy habits while simultaneously
promoting and establishing healthful ones—is best for
long-term beneficial results. Through specific examples,
we identify multiple intervention components for health
policymakers to use as a framework to bring about
lasting behavioral public health benefits.
re view

a publication of the behavioral science & policy association 71
Healthy through habit:
Interventionsforinitiating &
maintaining health behavior change
Wendy Wood & David T. Neal
abstract. Interventions to change health behaviors have had limited
success to date at establishing enduring healthy lifestyle habits. Despite
successfully increasing people’s knowledge and favorable intentions to
adopt healthy behaviors, interventions typically induce only short-term
behavior changes. Thus, most weight loss is temporary, and stepped-up
exercise regimens soon fade. Few health behavior change interventions
have been successful in the longer term. In this article, we unpack the
behavioral science of health-habit interventions. We outline habit-forming
approaches to promote the repetition of healthy behaviors, along with
habit-breaking approaches to disrupt unhealthy patterns. We show that
this two-pronged approach—breaking existing unhealthy habits while
simultaneously promoting and establishing healthful ones—is best for long-
term beneficial results. Through specific examples, we identify multiple
intervention components for health policymakers to use as a framework to
bring about lasting behavioral public health benefits.
I
n 1991, the National Cancer Institute and industry
partners rolled out a nationwide educational public
health
*******
campaign—the 5 A Day for Better Health
Program—to boost consumption of fruits and vege-
tables. The campaign was remarkably successful in
changing people’s knowledge about what they should
eat: Initially, only 7% of the U.S. population understood
that they should eat at least five servings of fruit and
vegetables per day, whereas by 1997, fully 20% were
Wood, W., & Neal, D. T. (2016). Healthy through habit: Interventions for
initiating & maintaining health behavior change. Behavioral Science &
Policy, 2(1), pp. 71–83.
aware of this recommendation.
1
Unfortunately, actual
fruit and vegetable consumption remained flat. During
the years 1988 to 1994, 11% of U.S. adults met this target
amount of fruit and vegetable consumption, and the
percentage did not shift during 1995–2002.
2
Another
national campaign launched in 2007, called Fruit &
Veggies—More Matters, also failed to move the fruit and
vegetable consumption needle.
3
These failures are not surprising. A body of research
shows that many public health campaigns do success-
fully educate and motivate people, especially in the
short run. However, when push comes to shove, they
often fail at changing actual behaviors and long-term
review

72 behavioral science & policy | volume 2 issue 1 2016
health habits, such as the consumption of optimal
amounts of fruit and vegetables.
4,5
Not all behavior change interventions fail to change
behavior. Often, some behavior change happens, but it
does not maintain over time.
6
To show how this works,
we depicted the results of some of the highest quality
health interventions to date in Figure 1. These studies
all appeared in top scientific journals, used exemplary
methods, and conscientiously assessed long-term
success rates.
7–10
It is easy to see that most participants
in these interventions got healthier in the short term (as
shown by the initially increasing lines). They lost weight,
exercised more, and gave up smoking. However, once
the intervention ended, old patterns reemerged, and
the new, healthy behaviors clearly waned over time (as
shown by the eventually decreasing lines). The overall
trajectory of behavior change can be described as a
triangular relapse pattern.
It is tempting to believe that the failures in main-
taining healthy behaviors depicted in Figure 1 are
D: Mean number of minutes per week of moderate to vigorous physical
exercise during computer-delivered interventions or health program
controls at 6 months of treatment, 12 months of treatment, and 6 months
after end of treatment (Ns = 70 control and 75 computerized treatment at
baseline; N = 61 computerized treatment at 18 months). Data are from
“Exercise Advice by Humans Versus Computers: Maintenance Eects at 18
Months,” by A. C. King, E. B. Hekler, C. M. Castro, M. P. Buman, B. H. Marcus
,
R. H. Friedman, and M. A. Napolitano, 2014, Health Psychology, 33, p. 195,
Figure 1. Copyright 2014 by the American Psychological Association.
Figure 1. The triangular relapse pattern in health behavior change over time
Start
A. Intervention of financial incentives for weight loss B. Intervention of payment for gym visits
C. Intervention of smoking information
and financial incentives to quit
D. Intervention via computer
to encourage physical activity
In these triangular relapse patterns, an initial spike in healthful behaviors during the intervention is followed by a decline following
intervention back toward baseline. Panels A–D show four examples of behavior change interventions following this pattern for
(A) weight loss, (B) gym visits, (C) quitting smoking, and (D) exercise. Mos = months; MVP = moderate to vigorous physical activity.
A: Mean pounds lost following a 4-month intervention of financial incentives
for weight loss and after 3 months of no treatment (N = 57). Data are from
“Financial Incentive–Based Approaches for Weight Loss: A Randomized
Trial,” by K. G. Volpp, L. K. John, A. B. Troxel, L. Norton, J. Fassbender, and
G. Loewenstein, 2008, Journal of the American Medical Association, 300,
p. 2635. Copyright 2008 by the American Medical Association.
B: Mean gym visits per week prior to study (weeks -16 to -2), during 5
intervention weeks of payment for attending, and during 15 no-treatment
weeks (weeks 6–21, N = 99). Data are from “Incentives to Exercise,” by G.
Charness and U. Gneezy, 2009
, Econometrica, 77, p. 921, Figure 2b.
Copyright 2009 by Wiley.
C: Percentage of participants who quit smoking (biochemically verified) at 3
or 6 months and at 15 or 18 months following intervention of information
about smoking cessation programs paired with financial incentives (N =
878). Data are from “A Randomized, Controlled Trial of Financial Incentives
for Smoking Cessation,” by K. G. Volpp, A. B. Troxel, M. V. Pauly, H. A. Glick,
A. Puig, D. A. Asch, . . . J. Audrain-McGovern, 2009, New England Journal
of Medicine, 360, p. 703, Table 2. Copyright 2009 by the Massachusetts
Medical Society.
15
10
5
0
Mean number of pounds lost
End of 4 months’
treatment
7 months
2.5
2
1.5
1
0.5
Mean number gym visits/week
Prior to
intervention
5-week
intervention
Post
intervention
Deposit contract plus lottery
No treatment control
Payment
No payment control
Intervention
25
20
15
10
5
0
Percent sample quit
Quit at 3
or 6 mos
Quit at 15
or 18 mos
190
155
115
75
Mean minutes of MVP/week
Baseline12 mos of
treatment
6 mos
follow-up
Information plus financial incentive
Information only
Computerized physical activity prompts
Control
6 mos of
treatment

a publication of the behavioral science & policy association 73
simply due to people’s limited willpower. Surely many
people struggle to inhibit the short-term gratifications
of fast food and the lure of excessive TV watching and
do not make the eort to stick to a balanced diet and
regular exercise. However, relapse is not inevitable if
behavior change interventions form healthy habits. In
fact, research shows that people who consistently act in
healthy ways in daily life do so out of habit. With heathy
diet and exercise habits, they do not need to struggle
with internal urges to act in unhealthy ways.
11,12
Another
insight comes from the success of policy changes
and health interventions in the last few decades that
drastically reduced smoking rates in the United States.
Antismoking campaigns have many components,
13
but
the most successful parts targeted cigarette purchase
and smoking habits as opposed to people’s willpower
and self-control. In this article, we use these insights
as a framework to construct interventions that break
unhealthy habits and encourage the adoption of bene-
ficial ones.
Both breaking and creating habits are central to
behavior change. Habits play a significant role in
people’s failure to adopt and stick with what is best
for their health. Eating habits are especially striking.
Research has shown that people habitually consume
food that they neither want nor even like.
14
For example,
movie theater patrons with strong popcorn-eating
habits consumed just as much stale, week-old popcorn
as they did fresh popcorn, despite reporting that they
hated the stale food.
15
Fortunately, just as bad habits impede behavior
change, good habits can promote it. As noted above,
good habits ensure that people continue to act in
healthy ways without constant struggle. For example,
chocolate lovers who had formed a habit to eat carrots
continued to make the healthy carrot choice even when
chocolate became available.
16
Habits represent context–response associations
in memory that develop as people repeat behav-
iors in daily life. For example, after repeatedly eating
hamburgers and pizza for dinner, a person is likely to
find that dinnertime cues such as driving home from
work and watching the evening news automatically acti-
vate thoughts of these foods and not vegetables.
17
From a habit perspective, behavior change interven-
tions are likely to fail unless they account for the ways in
which people form healthy habits and break unhealthy
ones. Although the research literature on behavior
change oers sophisticated understanding of many
intervention features (for example, oering appropriate
incentives, tailoring messages to specific subsets of the
target audience, tracking nonintrusive outcomes such as
credit card charges), little attention has been paid to the
importance of habits in maintaining lifestyle choices.
In the first part of this article, we explain how inter-
ventions create healthy habits. Essentially, healthy habit
creation involves repeated performance of rewarding
actions in stable contexts. The second part of the article
addresses how interventions can break unhealthy habits
by neutralizing the cues that automatically trigger these
responses. Our set of habit-based interventions thus
augments existing tools to promote automated perfor-
mance of desired over undesired responses. Among
existing tools, people are most likely to make a good
choice when decisions are structured to make that
choice easy,
18,19
when other people are making the same
choice,
20,21
and after forming if-then plans.
22,23
Finally,
we explain how habit-based interventions can be incor-
porated into health policies.
Promoting the Formation of New Habits
The three central components of habit formation are
(a)behavioral repetition, (b) associated context cues,
and (c) rewards (see Table 1).
Behavior change interventions form habits by getting
people to act in consistent ways that can be repeated
frequently with little thought. Habits develop gradually
through experience, as people repeat a rewarded action
in a stable place, time, or other context. Through repe-
tition, the context becomes a sort of shorthand cue for
what behavior will be rewarded in that context. People’s
habits essentially recreate what has worked for them in
the past. In this way, habits lock people into a cycle of
automatic repetition.
Once a habit has formed, it tends to guide behavior
even when people might have intended to do some-
thing else.
24
Essentially, habits come to guide behavior
instead of intentions. Early in habit formation, people
might intentionally decide how to respond to achieve
Existing habits are a significant impediment to
people adopting and sticking with healthy behavior

74 behavioral science & policy | volume 2 issue 1 2016
a certain outcome. However, once a habit gains
strength, people tend to habitually respond, for better
or worse.
25
According to a study in the British Journal
of Health Psychology, eating habits were stronger
determinants of food choices than intentions or even
sensitivity to food temptations.
26
When habits are
healthy, outsourcing behavioral control to the environ-
ment in this way is beneficial. People keep on track by
responding habitually when distractions, stress, and dips
in willpower impede decision-making.
27
However, when
habits are unhealthy, the automatic or environmental
control of behavior impedes health and can create a
self-control dilemma.
Next, we expand on the central components of habit
formation and later address unhealthy habits.
The Three Central Habit-Forming Interventions
Behavior Repetition
Habit formation interventions create opportunities
for and encourage frequent repetition of specific
responses, but there is no single formula for success. In
one study, participants chose a new health behavior to
perform once a day in the same context (for example,
eating fruit after dinner).
28
For some behaviors and
some people, only 18 days of repetition were required
for the behavior to become suciently automatic to be
performed without thinking. For other behaviors and
participants, however, over 200 days of repetition were
needed. Another study published in Health Psychology
29
found that people required 5 to 6 weeks of regular gym
workouts to establish new exercise habits.
30
Interventions may encourage repetition by visu-
ally depicting the physical act of repeating the desired
behavior—think of the famous Nike advertisements
advising, “Just Do It,” while showing famous athletes
and others engaged in vigorous exercise. Interven-
tions in schools and other controlled environments
could direct physical practice of the new habit by, for
example, conducting hand-washing drills in bath-
rooms instead of merely teaching hygiene benefits and
setting performance goals.
31
Hospitals and restaurants
can similarly benefit from employees rehearsing best
sanitationpractices.
Longer interventions with frequent repetitions (vs.
shorter interventions, with fewer repetitions) tend to be
most successful because they are most likely to lead
to the formation of strong habits. Such a pattern could
explain the greater success of long-duration weight loss
interventions.
5
Intervention length also might explain
one of the most successful behavioral interventions:
Opower’s multiyear energy conservation programs.
32
These multicomponent interventions, involving smart
meters and feedback about power use, have proved
especially successful at limiting energy use, presumably
because the extended intervention allowed consumers
to form energy-saving habits.
Context Matters: Cues Trigger Habit Formation
Successful habit learning depends not only on repeti-
tion but also on the presence of stable context cues.
Context cues can include times of day, locations, prior
actions in a sequence, or even the presence of other
people (see Table 1). Illustrating the importance of stable
cues, almost 90% of regular exercisers in one study had
a location or time cue to exercise, and exercising was
more automatic for those who were cued by a partic-
ular location, such as running on the beach.
33
Other
research shows that older adults are more compliant
with their drug regimens when pill taking is done in a
particular context in their home (for example, in the
bathroom) or integrated into a daily activity routine.
34
Implementation plans. Intervention programs to
form healthy habits can promote stable habit cues in
Table 1. Three main components of habit
formation interventions and examples
of implementation in practice
Principle Examples in practice
Frequent
repetition
• School hand-washing interventions that
involve practicing actual washing behavior
in the restroom
Recurring
contexts and
associated
context cues
• Public health campaigns linking changing
smoke detector batteries to the start and
end of daylight savings time
• Medical compliance communications
that piggyback medications onto existing
habits such as mealtime
Intermittent
rewards
• Free public transit days scheduled
randomly
• Coupons and discounts for fresh fruits and
vegetables provided on an intermittent or
random basis

a publication of the behavioral science & policy association 75
several ways. People can be encouraged to create plans,
or implementation intentions, to perform a behavior in a
given context (for example, “I will floss in the bathroom
after brushing my teeth”).
18
Forming implementation plans increases the likeli-
hood that people will carry out their intentions.
35
Accord-
ingly, these plans promote performance only for people
who already intend to perform the healthy behavior (for
example, people who want to floss more regularly),
36
and the ecacy of the intervention fades if their inten-
tions change. Even so, implementation intentions may
be a useful stepping stone on the path to creating habits
because, as people act repeatedly on such intentions in
a stable context, behavior may gradually become less
dependent on intentions and gel into habits.
Piggybacking. Intervention programs also create cues
by piggybacking, or tying a new healthy behavior to an
existing habit. The habitual response can then serve as
a cue to trigger performance of the new behavior. For
example, dental-flossing habits were established most
successfully when people practiced flossing immedi-
ately after they brushed their teeth, rather than before.
37
The large number of habits in people’s daily lives
provides many opportunities to connect a new behavior
to an existing habit.
38
Successful examples include
public information campaigns that link the replacement
of smoke alarm batteries to another periodic activity—
changing the clock for daylight savings; and medical
compliance is boosted when a prescribed health prac-
tice (for example, taking pills) is paired with a daily habit
(for example, eating a meal, going to bed).
39
Rewards Promote Habit Formation
People tend to repeat behaviors that produce positive
consequences or reduce negative ones (see Table 1).
Positive consequences include the intrinsic payo of a
behavior, for instance, the taste of a sweet dessert or the
feeling of accomplishment that comes from eectively
meeting health goals.
40
Positive consequences also
include extrinsic rewards, such as monetary incentives
or others’ approval. Avoiding negative consequences
is illustrated by contingency contracts, such as when
people agree to pay money for every swear word they
utter or experience other negative consequences for
failing to meet a goal.
41
Habits form most readily when specific behaviors are
rewarded. Especially during the initial stages of habit
formation, specific incentives can increase people’s
motivation to do things they might typically avoid,
such as exercising or giving up ice cream. In this sense,
rewards can oset the loss of enjoyable activities in
order to start a healthful behavior.
Other rewards are less successful at habit formation
because they are too broad to promote specific habits.
Overly general rewards include symbolic trophies,
prizes that recognize strong performance, or temporal
landmarks such as birthdays or the kicko of a new
calendar year. Only rewards that promote the repetition
of specific actions contribute to habit formation.
Many decades of laboratory research have shown
what kinds of rewards are most likely to motivate
habits. Surprisingly, habits form best when rewards are
powerful enough to motivate behavior but are uncertain
in the sense that they do not always occur.
42
Uncertain
rewards powerfully motivate repetition and habit forma-
tion. In learning theory terminology, such rewards are
given on random-interval schedules.
Slot machines are a good example of uncertain
rewards. People keep paying money into the machines
because sometimes they win, sometimes they don’t.
This reward system is so powerful that slot machines are
sometimes described as the crack cocaine of gambling.
E-mail and social networking sites have similar eects:
people keep checking on them because sometimes they
are rewarded with interesting communications, but other
times they get only junk. The key is that rewards are
received probabilistically, meaning not for every behavior.
To date, few health interventions have used uncer-
tain rewards.
43
Instead, most health interventions oer
consistent, predicable rewards, such as payments
received each time program participants go to the gym.
Such rewards eectively drive short-term behavior
changes, but they do not establish habits. When the
rewards stop, people usually quit the behavior.
6
In part,
people quit because predictable rewards can signal
that a behavior is dicult, undesirable, and not worth
performing without the reward.
44
Behavior change interventions should give rewards
in the way a slot machine does—at uncertain intervals
Uncertain rewards are most eective
76 behavioral science & policy | volume 2 issue 1 2016
but often enough to suciently motivate people to
perform the target healthy behavior. For example,
discounts on fresh fruits and vegetables at grocery
stores can be provided intermittently to encourage
habitual produce purchases. The structure and routines
of school and work environments are particularly well
suited to providing uncertain rewards. School policies,
especially in elementary schools, could be structured
to provide occasional monitoring and reinforcements
for healthy behaviors such as hand washing after using
the restroom or fruit and vegetable consumption during
school lunches.
The Three Main Habit-Change Interventions
Work Best in Combination.
Only a few health interventions with the general popu-
lation have incorporated all three components of habit
formation: response repetition, stable cues, and uncer-
tain rewards. Yet, the few existing habit-based inter-
ventions that have bundled two or all three of these
components have yielded promising results for weight
loss
45
and consumption of healthy food in families.
46
In one study, for example, overweight participants
were instructed to (a) develop predictable and sustain-
able weight loss routines, (b) modify their home envi-
ronments to increase cues to eat healthy foods and
engage in exercise, and (c) have immediate positive
rewards for weight-loss behaviors.
47
Participants also
were instructed on how to disrupt existing habits by
removing cues that triggered them along with making
unhealthy behaviors less reinforcing (for example,
increasing the preparation time and eort for unhealthy
snacks). As depicted in Figure 2A, participants under-
going this multifaceted habit formation and disruption
treatment continued to lose weight during several
months following the end of the intervention, whereas
participants using a more standard weight-loss program
relapsed over time.
A very dierent habit formation intervention used
an electronic monitoring device to promote weight
loss among overweight adolescents.
48
This interven-
tion targeted a specific behavior: the amount and
speed of eating. Cues to eating were standardized by
having participants undergo monitoring by a device
while eating dinner at a table. The device delivered
feedback about success and failure in hitting predeter-
mined goals. As shown in Figure 2B, after 12 months,
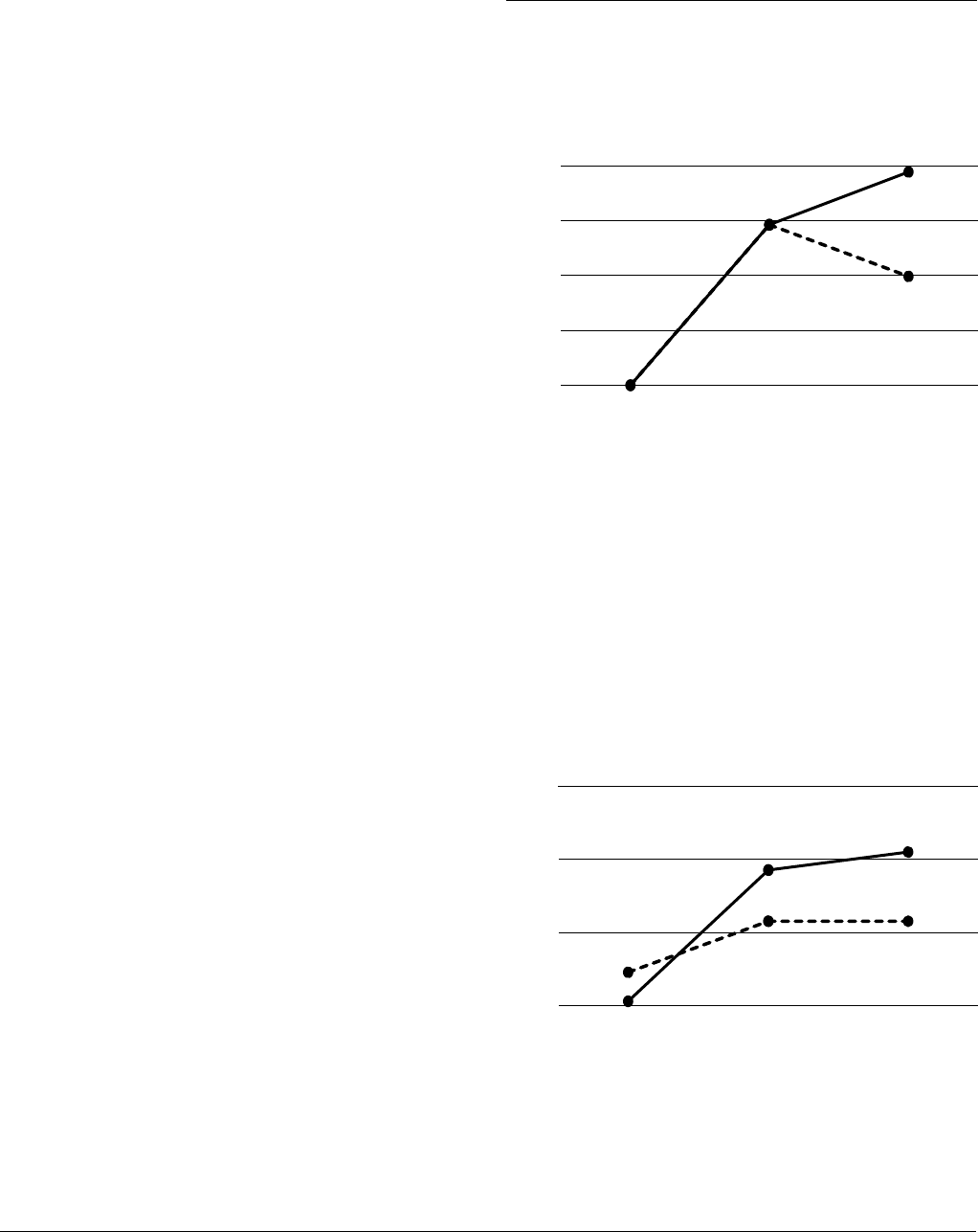
Figure 2. Interventions specifically targeting
habits can create enduring behavior change
over tim
e
Baseline
A. Multifaceted habit formation and disruption
weight loss program vs. standard weight loss program
B. Electronic monitoring device to promote control
of eating vs. standard weight loss program
In behavior change in
terventions that target habit formation
and
change, more enduring behavior change is possible.
F
igure A: Mean pounds lost after 3 months (mos) of habit-based or
standa
rd weight loss interventions (N = 59 at baseline, N = 35 at 6 months).
Th
e habit-based intervention emphasized (a) developing and maintaining
heal
thy habits and disrupting unhealthy habits, (b) creating a personal food
an
d exercise environment that increased exposure to healthy eating and
ph
ysical activity and encouraged automatic responding to goal-related
cu
es, and (c) facilitating weight loss motivation. The standard weight loss
pr
ogram involved examining attitudes toward food, body, and weight, such
as
improving body acceptance and understanding social stereotypes. Data
ar
e from “A Randomized Trial Comparing Two Approaches to Weight Loss:
Di
erences in Weight Loss Maintenance,” by R. A. Carels, J. M. Burmeister,
A.
M. Koball, M. W. Oehlhof, N. Hinman, M. LeRoy, . . . A. Gumble, 2014,
Journal
of Health Psychology, 19, p. 304, Figure 2. Copyright 2014 by Sage.
F
igure B: Mean children’s age- and sex-adjusted body mass index (BMI)
af
ter a yearlong intervention using a monitoring device to reduce the
amount
and speed of eating, plus a 6-month follow-up (N = 106 at baseline
an
d 12 months, N = 87 at the 18-month assessment). Data are from
“T
reatment of Childhood Obesity by Retraining Eating Behaviour:
Randomise
d Controlled Trial,” by A. L. Ford, C. Bergh, P. Södersten, M. A.
Sabi
n, S. Hollinghurst, L. P. Hunt, and J. P. Shield, 2010, British Medical
Journal
, 340, Article b5388, Table 2. Copyright 2010 by BMJ.
20
15
10
5
0
Mean pounds lost
3 months 6 months
Habit change program
Control program
Baseline
2.7
2.9
3.1
3.3
Mean BMI, sex and weight adjusted
End of 12 mos
intervention
6 mos after
intervention
Eating training
Standard treatment

a publication of the behavioral science & policy association 77
monitored participants not only ate smaller meals than
participants in a control group did, but they had lost
significant amounts of weight and kept it o 6 months
after the intervention ended.
Breaking Unhealthy Habits
Because habits are represented in memory in a relatively
separate manner from goals and conscious intentions,
existing habits do not readily change when people
adopt new goals. Thus, recognizing the health value of
five servings of fruits and vegetables per day does not,
by itself, remove the cues that trigger consumption of
other less healthful foods. Similarly, incentive programs
to break habits will not necessarily alter the memory
trace underlying the behavior. Familiar contexts and
routines still will bring unhealthy habits to mind, leaving
people at risk of lapsing into old patterns.
49
Even after
new habits have been formed, the existing memory
traces are not necessarily replaced but instead remain
dormant and can be reactivated relatively easily with a
memory cue.
50
Changing unhealthy habits, much like forming
healthy ones, requires an understanding of the
psychology behind habits. Specifically, ridding oneself
of unhealthy habits requires neutralizing the context
cues that automatically trigger habit performance.
The Three Main Habit-Breaking Interventions
Health interventions can incorporate three strategies to
reduce the impact of existing bad cues: (a) cue disrup-
tion, (b) environmental reengineering, and (c) vigilant
monitoring or inhibition (see Table 2). Experiments
show that habit performance is readily disrupted when
contexts have shifted.
50,51
Cue Disruption
Interventions can take advantage of naturally occur-
ring life events—such as moving to a new house,
beginning a new job, or having a child—that reduce or
eliminate exposure to the familiar cues that automat-
ically trigger habit performance (see Table 2). People
are most successful at changing their behavior in daily
life when they capitalize on such life events. In a study
in which people reported their attempts to change
some unwanted behavior, moving to a new location
was mentioned in 36% of successful behavior change
attempts but only in 13% of unsuccessful ones.
52
In
addition, 13% of successful changers indicated that,
to support the change, they altered the environment
where a prior habit was performed, whereas none of the
unsuccessful ones mentioned this.
Habit discontinuity interventions capitalize on this
window of opportunity in which people are no longer
exposed to cues that trigger old habits.
53
For example,
an intervention that provided a free transit pass to car
commuters increased the use of transit only among
those who changed their residence or workplace in the
prior 3 months.
54
Apparently, the move from a familiar
environment disrupted cues to driving a car, enabling
participants to act on the incentive to use transit instead
of falling back on their car-driving habit. Another
study showed that students’ TV-watching habits were
disrupted when they transferred to a new university, but
only if cues specific to this behavior changed, such as
their new residence no longer having a screen in the
living room.
55
Without the old cue to trigger their TV
habits, students only watched TV at the new university if
they intended to.
Many dierent health interventions can be applied
during the window of opportunity provided by life tran-
sitions. For example, new residents could be messaged,
via text or mailers, with incentives to perform healthy
behaviors related to their recent move. These could
include reminders of the public transit options in the
new neighborhood, notices that registration is open
for community fitness classes, and invitations to local
farmers’ markets. Similarly, new employees could be
informed about workplace-related health options
such as employer-sponsored health classes. Also,
reduced insurance rates could be oered if employees
quit smoking or adopt other healthy behaviors. First-
time parents could be engaged by interventions that
encourage the preparation of healthy meals when
cooking at home or that promote enrollment in child-
and-parent exercise classes.
Environmental Reengineering
The impact of unhealthy habit cues also can be reduced
by altering performance environments, or the place
where the unhealthy habit regularly occurs (see Table
2). Although environmental reengineering often involves
cue disruption (as described above), it additionally

78 behavioral science & policy | volume 2 issue 1 2016
introduces new or altered environmental features to
support the healthy behavior. The basic psychological
process involves adding behavioral friction to unhealthy
options and reducing behavioral friction for healthy
ones to lubricate their adoption.
Adding friction. Large-scale social policies can intro-
duce friction into an environment, making it harder for
people to perform unhealthy habits. Smoking bans in
English pubs, for instance, made it more dicult for
people with strong smoking habits to light up while
drinking.
56
Having to leave the pub to smoke creates
friction, so smoking bans have generally increased
quit rates.
57
Bans on visible retail displays of cigarettes
also add friction by forcing potential purchasers to
remember to request cigarettes.
58
Such bans are espe-
cially likely to reduce impulsive tobacco purchases
59
by
removing environmental smoking cues.
60
Another way of adding friction to unhealthy options
is being tested in several cities in Switzerland. Policy-
makers are providing citizens with free electric bikes or
free ride-share schemes, but only after they hand over
their car keys for a few weeks. The idea is to add fric-
tion to existing car-use habits.
61
If successful, blocking
the automatic response of car driving will encourage
the use of other forms of transit that, in turn, may
becomehabitual.
Reducing friction. A variety of existing policies
successfully alter physical environments to promote
frictionless accessibility to healthy behaviors over
unhealthy ones. These include the availability of recre-
ational facilities, opportunities to walk and cycle, and
accessibility of stores selling fresh foods. The eective-
ness of such friction-easing interventions is clear: U.S.
residents with access to parks closer to home engage in
more leisure-time physical activity and have lower rates
of obesity.
62
Also, a bike-share program instituted in
London increased exercise rates.
63
Furthermore, in U.S.
metropolitan areas, fruit and vegetable consumption
was greater and obesity rates were lower among people
living closer to a supermarket with fresh foods.
64
The broad success of environmental reengineering
policies and changes to the physical environment makes
these prime strategies for large-scale habit change.
Nonetheless, these initiatives require political and citizen
support for healthy policies, tax codes, and zoning. We
suspect that such support will increase in the future,
given increasing recognition of lifestyle eects on
health.
65
To illustrate this potential, we note that building
Table 2. Three main components of habit-breaking interventions
and examples of implementation in practice
Principle Examples in practice
Cue disruption • Target recent movers with public transit price reductions
• Target new employees with health and wellness programs
• Reduce salience of cues to unhealthy choices; increase salience of healthy choices
(forexample, redesign cafeterias to show healthy items first)
Environmental reengineering Add friction to unhealthy behaviors
• Banning smoking in public places
• Banning visual reminders of cigarettes at point of purchase
• Changing building design regulations to increase prominence of stairways
• Explaining through public health communications how to alter personal environments to
reduce the salience of unhealthy foods
Remove friction from healthy behaviors
• Starting bike-share programs
• Bundling healthy food items in fast food menu selections (for example, apple slices as default
side item)
• Adding a fast check-out line in cafeterias for those purchasing healthy items only
Vigilant monitoring • Food labeling regulations that require visual cues on packaging to show serving sizes
• GPS technology triggers in smartphones and wearable devices that deliver nudges to adopt
healthful behaviors (for example, based on time to and location of fast food restaurants,
sending “don’t go” alerts or “order this not that” messaging)

a publication of the behavioral science & policy association 79
codes could make healthy options the default choice
by applying friction to elevator use so that stairways are
readily accessible and elevators less apparent. In addi-
tion, to add friction to unhealthy food choices and to
automate healthy ones, restaurants could provide food
bundles (for example, value meals) with healthy default
options (for example, apple slices instead of French
fries), and manufacturers could switch to packaging
formats that do not minimize apparent food quantity but
enable people to accurately assess the amount they are
eating.
66
To simplify consumer understanding of healthy
choices, restaurants and food companies could be rated
for health performance, much as they currently are
forsanitation.
67
Finally, on a more immediate, personal level, behavior
change interventions can provide individuals with the
knowledge and ability to reengineer their own personal
environments. The potential benefits of change in
microenvironments have been demonstrated clearly
with respect to healthy eating: People with a lower body
mass index were likely to have fruit available on their
kitchen counters, whereas those weighing more were
likely to have candy, sugary cereal, and nondiet soft
drinks.
68
And demonstrating that food choice is based in
part on high visibility, studies that have directly manipu-
lated the visibility and convenience of foods reveal that
people tend to consume easily accessible, frictionless
options rather than inaccessible, high-friction choices.
69
Another approach to reduce the friction to healthy
choices is allowing people to preorder food, enabling
them to make healthier choices outside of the influence
of the evocative smells and visual temptations of school
or work cafeterias.
70
In summary, it is sound policy to
empower individuals to reengineer their immediate
environments to increase access to contexts promoting
healthy behaviors and avoid contexts of unhealthy ones.
Vigilant Monitoring
Inhibition of habits through vigilant monitoring is a final
habit-breaking strategy that increases awareness of the
cues that trigger unhealthy habits and provides oppor-
tunities to inhibit them (see Table 2). Unlike cue disrup-
tion and environmental reengineering, which focus
primarily on harnessing automatic processes, vigilant
monitoring combines conscious thoughts of control
with automatic processes. This works as a sort of cogni-
tive override process.
Vigilant monitoring is the strategy that people are
most likely to use to control unwanted habits in daily
life.
71
By thinking, “Don’t do it,” and monitoring carefully
for slipups, participants in several studies were more
eective at curbing bad habits such as eating junk food,
smoking, and drinking too much than when they used
other strategies (for example, distracting themselves).
These researchers subsequently brought this strategy
into the lab to study it under controlled conditions using
a word-pair task. Vigilant monitoring proved to control
habits by heightening inhibitory cognitive control
processes at critical times when bad habits were most
likely—that is, by helping people combat their automatic
responses before they happened.
Vigilance may be most eective when paired with
strategies that also make healthy options cognitively
accessible, so the desired action is salient in contexts
in which people have an unhealthy habit. Thus, after
people formed implementation intentions to eat apples
or another healthy snack in a context in which they
typically ate unhealthy ones like candy bars, the healthy
behavior automatically came to mind when that context
was encountered in the future.
23
Facilitating vigilant monitoring for individuals.
Because vigilant inhibition is eortful to sustain, it could
be facilitated by GPS technology in smartphones and
wearable devices that enable reminders or nudges, to
be delivered on the basis of physical proximity to loca-
tions linked with unwanted habits (for example, fast
food restaurants). Given that these sensor devices can
detect daily activities such as eating and watching TV,
72
they could potentially deliver response-timed elec-
tronic prompts at just the right time to inhibit acting on
unhealthy habits.
In policy applications, vigilant monitoring of
unwanted behaviors can be adapted into interventions
through reminders to control unwanted habits. These
could be conveyed indirectly with simple changes to
product packaging, such as pictures illustrating the
amount of a single-serving portion on a bag of Oreos.
Or serving cues could be embedded within the food
itself, perhaps by inserting a dierent-colored cookie
at a certain point in the package to trigger a “stop here”
response.
73
More directly, point-of-choice prompts
involving signs or other reminders of desired actions
might be used in situations where people usually
respond in other ways. For example, signs to promote
stair climbing over elevator and escalator use in public

80 behavioral science & policy | volume 2 issue 1 2016
settings have shown modest but consistent success.
74
Because such reminders may become less eective
over time, except among people who perform the
behavior suciently often so that it becomes habitual,
75
it may be necessary to diversify such visual cues over
time to help retrigger vigilance.
Framework for Policymakers
Habit-based interventions are tailored to the mecha-
nisms of action, ensuring that the patterning of behavior
is optimal to create healthy habits and impede unhealthy
ones. The principles and tactics outlined here can be
applied at varying levels of scale, with some best suited
to individual self-change, others to community health
interventions, and still others to state and national poli-
cies. So, which of the ideas we have discussed in this
article scale best for public policy?
For Habit Formation
Public policy regulations can eectively make healthy
responses salient (for example, funding bike paths and
bike-share programs) and tie desired behaviors to stable
contexts (for example, public health communications
that link reminders to change smoke detector batteries
to the start and end of daylight savings time, medical
compliance communications that piggyback medication
intake onto an existing habit). At its core, habit forma-
tion is promoted through the various public policies
that incentivize repeated healthy responses in stable
contexts (for example, free public transit days; Supple-
mental Nutrition Assistance Program benefits limited to
the purchase of high nutrition, low-energy-dense foods
such as spinach and carrots).
For Habit Disruption
Policymakers can initiate legislation to reduce the pres-
ence of unhealthy habit cues (for example, funding the
reengineering of school cafeterias) and can also harness
context disruption (for example, free public transit
programs for recent movers). The success of anti-
smoking campaigns provides a model for how this can
work. Among the many dierent policies used to control
tobacco, the most successful were the ones that added
friction to smoking, such as increasing tobacco prices,
instituting smoking bans in public places, and removing
tobacco and advertising from point-of-purchase
displays.
9
As would be anticipated given the habitual,
addictive nature of smoking, warning labels on packets
have limited impact,
65
and mass media campaigns have
generally only been eective in conjunction with the
more friction-inducing interventions listed above.
76,77
Traditional policy tools such as tax breaks are a
generally useful tool for health behavior change. Linking
tax breaks for health insurers to policyholders’ health
habits can create incentives for companies and other
large institutions to apply habit-change principles in
more localized ways. Tax policies can also drive habit
change by adding friction to unhealthy consumer
choices (for example, taxes on sugared soft drinks,
tobacco, and fast food).
For many everyday health challenges, people are
likely to benefit from both forming healthy habits and
disrupting unhealthy ones. Thus, multicomponent
interventions that include distinct elements designed
to break existing habits and support the initiation
and maintenance of new ones will be needed. For
example, an intervention to increase fruit and vegetable
consumption among students in a school cafeteria
could simultaneously reengineer the choice environ-
ment to disrupt their existing habits to eat processed
snacks (for example, by moving such snacks to the
back of displays and fruit to the front) and to form new
habits (for example, by providing discounts to incen-
tivize the selection and consumption of healthful foods,
or express checkout lanes for people making healthy
purchases). However, habit disruption is, of course,
irrelevant in shifting, changing environments and for
people who do not have a history of acting in a given
domain or circumstance. Thus, habit interruptions have
more limited use than the broadly applicable habit
formationprinciples.
Conclusion
Strategies that accelerate habit formation and promote
maintenance are especially important for health inter-
ventions, given that many benefits of healthy behaviors
are not evident immediately but instead accrue gradually
with repetition. Thus, interventions that are successful
at promoting short spurts of exercise or a sporadi-
cally healthful diet will provide little protection against
the risks of lifestyle diseases associated with inactivity
and overeating. The habit-based strategies outlined in

a publication of the behavioral science & policy association 81
this article provide policymakers and behavior change
specialists with important insights into the mecha-
nisms by which people can create sustainable healthy
lifestyles.
author aliation
Wood, Dornsife Department of Psychology and Marshall
School of Business, University of Southern California;
Neal, Catalyst Behavioral Sciences and Center for
Advanced Hindsight, Duke University. Corresponding
author’s e-mail: wendy[email protected]
author note
Preparation of this article was supported by a grant to
Wendy Wood from the John Templeton Foundation.
The opinions expressed in this article are those of the
authors and do not necessarily reflect the views of the
John Templeton Foundation. The authors thank Hei
Yeung Lam and Drew Kogon for their help with the
references.
References
1. Stables, G. J., Subar, A. F., Patterson, B. H., Dodd, K.,
Heimendinger, J., Van Duyn, M. A. S., & Nebeling, L. (2002).
Changes in vegetable and fruit consumption and awareness
among US adults: Results of the 1991 and 1997 5 A Day for
Better Health Program surveys. Journal of the American
Dietetic Association, 102, 809–817. http://dx.doi.org/10.1016/
S0002-8223(02)90181-1
2. Casagrande, S. S., Wang, Y., Anderson, C., & Gary, T. L. (2007).
Have Americans increased their fruit and vegetable intake?
The trends between 1988 and 2002. American Journal of
Preventive Medicine, 32, 257–263. http://dx.doi.org/10.1016/j.
amepre.2006.12.002
3. Moore, L. V., & Thompson, F. E. (2015, July 10). Adults meeting
fruit and vegetable intake recommendations—United States,
2013. Morbity and Mortality Weekly Report, 64, 709–713.
http://www.cdc.gov/MMWR/preview/mmwrhtml/mm6426a1.
htm
4. Vandelanotte, C., Spathonis, K. M., Eakin, E. G., & Owen, N.
(2007). Website-delivered physical activity interventions:
A review of the literature. American Journal of Preventive
Medicine, 33, 54–64. http://dx.doi.org/10.1016/j.
amepre.2007.02.041
5. Fjeldsoe, B., Neuhaus, M., Winkler, E., & Eakin, E. (2011).
Systematic review of maintenance of behavior change
following physical activity and dietary interventions. Health
Psychology, 30, 99–109. http://dx.doi.org/10.1037/a0021974
6. Mantzari, E., Vogt, F., Shemilt, I., Wei, Y., Higgins, J. P., &
Marteau, T. M. (2015). Personal financial incentives for
changing habitual health-related behaviors: A systematic
review and meta-analysis. Preventive Medicine, 75, 75-85.
http://dx.doi.org/10.1016/j.ypmed.2015.03.001
7. Volpp, K. G., John, L. K., Troxel, A. B., Norton, L., Fassbender,
J., & Loewenstein, G. (2008). Financial incentive–based
approaches for weight loss: A randomized trial. Journal of the
American Medical Association, 300, 2631–2637. http://dx.doi.
org/10.1001/jama.2008.804
8. Charness, G., & Gneezy, U. (2009). Incentives to exercise.
Econometrica, 77, 909–931. http://dx.doi.org/10.3982/
ECTA7416
9. Volpp, K. G., Troxel, A. B., Pauly, M. V., Glick, H. A., Puig, A.,
Asch, D. A., . . . Audrain-McGovern, J. (2009). A randomized,
controlled trial of financial incentives for smoking cessation.
New England Journal of Medicine, 360, 699–709. http://dx.doi.
org/10.1056/NEJMsa0806819
10. King, A. C., Hekler, E. B., Castro, C. M., Buman, M. P., Marcus,
B. H., Friedman, R. H., & Napolitano, M. A. (2014). Exercise
advice by humans versus computers: Maintenance eects
at 18 months. Health Psychology, 33, 192–196. http://dx.doi.
org/10.1037/a0030646
11. Adriaanse, M. A., Kroese, F. M., Gillebaart, M., & De Ridder,
D. T. (2014). Eortless inhibition: Habit mediates the relation
between self-control and unhealthy snack consumption.
Frontiers in Psychology, 5, Article 444. http://dx.doi.
org/10.3389/fpsyg.2014.00444
12. Galla, B. M., & Duckworth, A. L. (2015). More than resisting
temptation: Beneficial habits mediate the relationship
between self-control and positive life outcomes. Journal of
Personality and Social Psychology, 109, 508–525. http://dx.doi.
org/10.1037/pspp0000026
13. Wilson, L. M., Tang, E. A., Chander, G., Hutton, H. E., Odelola, O.
A., Elf, J. L., . . . Apelberg, B. J. (2012). Impact of tobacco control
interventions on smoking initiation, cessation, and prevalence: A
systematic review. Journal of Environmental and Public Health,
2012, Article 961724. http://dx.doi.org/10.1155/2012/961724
14. Tricomi, E., Balleine, B. W., & O’Doherty, J. P. (2009). A specific
role for posterior dorsolateral striatum in human habit learning.
European Journal of Neuroscience, 29, 2225–2232. http://
dx.doi.org/10.1111/j.1460-9568.2009.06796.x
15. Neal, D. T., Wood, W., Wu, M., & Kurlander, D. (2011). The
pull of the past: When do habits persist despite conflict with
motives? Personality and Social Psychology Bulletin, 37, 1428–
1437. http://dx.doi.org/10.1177/0146167211419863
16. Lin, P.-Y., Wood, W., & Monterosso, J. (2016). Healthy eating
habits protect against temptations. Appetite, 103, 432–440.
http://dx.doi.org/10.1016/j.appet.2015.11.011
17. Neal, D. T., Wood, W., Labrecque, J. S., & Lally, P. (2012). How
do habits guide behavior? Perceived and actual triggers of
habits in daily life. Journal of Experimental Social Psychology,
48, 492–498. http://dx.doi.org/10.1016/j.jesp.2011.10.011
18. Thaler, R. H., Sunstein, C. R., & Balz, J. P. (2012). Choice
architecture. In E. Shafir (Ed.), The behavioral foundations
of public policy (pp. 428–439). Princeton, NJ: Princeton
University Press. http://dx.doi.org/10.2139/ssrn.2536504
19. Johnson, E. J., Shu, S. B., Dellaert, B. G. C., Fox, C., Goldstein,
D. G., Häubl, G., . . . Weber, E. U. (2012). Beyond nudges: Tools
of a choice architecture. Marketing Letters, 23, 487–504.
http://dx.doi.org/10.1007/s11002-012-9186-1
20. Sherif, M. (1936). The psychology of social norms. Oxford,
England: Harper.
21. Salmon, S. J., Fennis, B. M., de Ridder, D. T., Adriaanse, M. A.,
& de Vet, E. (2014). Health on impulse: When low self-control
promotes healthy food choices. Health Psychology, 33,
103–109. http://dx.doi.org/10.1037/a0031785
22. Gollwitzer, P. M. (1999). Implementation intentions: Strong
eects of simple plans. American Psychologist, 54, 493–503.
http://dx.doi.org/10.1037/0003-066X.54.7.493
23. Adriaanse, M. A., Gollwitzer, P. M., de Ridder, D. T. D., de
Wit, J. B. F., & Kroese, F. M. (2011). Breaking habits with
implementation intentions: A test of underlying processes.
Personality and Social Psychology Bulletin, 37, 502–513. http://
dx.doi.org/10.1177/0146167211399102

82 behavioral science & policy | volume 2 issue 1 2016
24. Wood, W., & Rünger, D. (2016). The psychology of habit.
Annual Review of Psychology, 67, 289–314. http://dx.doi.
org/10.1146/annurev-psych-122414-033417
25. Ji, M. F., & Wood, W. (2007). Purchase and consumption
habits: Not necessarily what you intend. Journal of Consumer
Psychology, 17, 261–276. http://dx.doi.org/10.1016/
S1057-7408(07)70037-2
26. Verhoeven, A. A. C., Adriaanse, M. A., Evers, C., & de Ridder,
D. T. D. (2012). The power of habits: Unhealthy snacking
behaviour is primarily predicted by habit strength. British
Journal of Health Psychology, 17, 758–770. http://dx.doi.
org/10.1111/j.2044-8287.2012.02070.x
27. Neal, D. T., Wood, W., & Drolet, A. (2013). How do people
adhere to goals when willpower is low? The profits (and
pitfalls) of strong habits. Journal of Personality and Social
Psychology, 104, 959–975. http://dx.doi.org/10.1037/a0032626
28. Lally, P., van Jaarsveld, C. H. M., Potts, H. W. W., & Wardle, J.
(2010). How are habits formed: Modelling habit formation in
the real world. European Journal of Social Psychology, 40,
998–1009. http://dx.doi.org/10.1002/ejsp.674
29. Armitage, C. J. (2005). Can the theory of planned
behavior predict the maintenance of physical activity?
Health Psychology, 24, 235–245. http://dx.doi.
org/10.1037/0278-6133.24.3.235
30. Kaushal, N., & Rhodes, R. E. (2015). Exercise habit formation
in new gym members: A longitudinal study. Journal of
Behavioral Medicine, 38, 652–663. http://dx.doi.org/10.1007/
s10865-015-9640-7
31. Neal, D. T., Vujcic, J., Hernandez, O., & Wood, W. (2015).
Creating hand-washing habits: Six principles for creating
disruptive and sticky behavior change for hand washing with
soap. Unpublished manuscript, Catalyst Behavioral Science,
Miami, FL.
32. Allcott, H., & Rogers, T. (2014). The short-run and long-run
eects of behavioral interventions: Experimental evidence
from energy conservation. American Economic Review, 104,
3003–3037. http://dx.doi.org/10.1257/aer.104.10.3003
33. Tappe, K., Tarves, E., Oltarzewski, J., & Frum, D. (2013). Habit
formation among regular exercisers at fitness centers: An
exploratory study. Journal of Physical Activity & Health, 10,
607–613.
34. Brooks, T. L., Leventhal, H., Wolf, M. S., O’Conor, R.,
Morillo, J., Martynenko, M., Wisnivesky, J. P., & Federman,
A. D. (2014). Strategies used by older adults with asthma for
adherence toinhaled corticosteroids. Journal of General
Internal Medicine, 29, 1506–1512. http://dx.doi.org/10.1007/
s11606-014-2940-8
35. Rogers, T., Milkman, K. L., John, L. K., & Norton, M. I. (2015).
Beyond good intentions: Prompting people to make plans
improves follow-through on important tasks. Behavioral
Science & Policy, 1(2), 33–41.
36. Orbell, S., & Verplanken, B. (2010). The automatic component
of habit in health behavior: Habit as cue-contingent
automaticity. Health Psychology, 29, 374–383. http://dx.doi.
org/10.1037/a0019596
37. Judah, G., Gardner, B., & Aunger, R. (2013). Forming a flossing
habit: An exploratory study of the psychological determinants
of habit formation. British Journal of Health Psychology, 18,
338–353. http://dx.doi.org/10.1111/j.2044-8287.2012.02086.x
38. Labrecque, J. S., Wood, W., Neal, D. T., & Harrington, N.
(2016). Habit slips: When consumers unintentionally resist
new products. Journal of the Academy of Marketing Science.
Advance online publication. http://dx.doi.org/10.1007/
s11747-016-0482-9
39. Phillips, A. L., Leventhal, H., & Leventhal, E. A. (2013). Assessing
theoretical predictors of long-term medication adherence:
Patients’ treatment-related beliefs, experiential feedback and
habit development. Psychology & Health, 28, 1135–1151.
http://dx.doi.org/10.1080/08870446.2013.793798
40. Lally, P., & Gardner, B. (2013). Promoting habit formation.
Health Psychology Review, 7(Suppl. 1), S137–S158. http://
dx.doi.org/10.1080/17437199.2011.603640
41. Fishbach, A., & Trope, Y. (2005). The substitutability of
external control and self-control. Journal of Experimental
Social Psychology, 41, 256–270. http://dx.doi.org/10.1016/j.
jesp.2004.07.002
42. DeRusso, A. L., Fan, D., Gupta, J., Shelest, O., Costa, R. M., &
Yin, H. H. (2010). Instrumental uncertainty as a determinant of
behavior under interval schedules of reinforcement. Frontiers
in Integrative Neuroscience, 4, Article 17. http://dx.doi.
org/10.3389/fnint.2010.00017
43. Burns, R. J., Donovan, A. S., Ackermann, R. T., Finch, E. A.,
Rothman, A. J., & Jeery, R. W. (2012). A theoretically grounded
systematic review of material incentives for weight loss:
Implications for interventions. Annals of Behavioral Medicine,
44, 375–388. http://dx.doi.org/10.1007/s12160-012-9403-4
44. Gneezy, U., Meier, S., & Rey-Biel, P. (2011). When and why
incentives (don’t) work to modify behavior. The Journal of
Economic Perspectives, 25, 191–209. http://dx.doi.org/10.1257/
jep.25.4.191
45. Lally, P., Chipperfield, A., & Wardle, J. (2008). Healthy habits:
Ecacy of simple advice on weight control based on a
habit-formation model. International Journal of Obesity, 32,
700–707. http://dx.doi.org/10.1038/sj.ijo.0803771
46. Gardner, B., Sheals, K., Wardle, J., & McGowan, L. (2014).
Putting habit into practice, and practice into habit: A process
evaluation and exploration of the acceptability of a habit-based
dietary behaviour change intervention. International Journal of
Behavioral Nutrition and Physical Activity, 11, Article 135. http://
dx.doi.org/10.1186/s12966-014-0135-7
47. Carels, R. A., Burmeister, J. M., Koball, A. M., Oehlhof, M. W.,
Hinman, N., LeRoy, M., . . . Gumble, A. (2014). A randomized
trial comparing two approaches to weight loss: Dierences in
weight loss maintenance. Journal of Health Psychology, 19,
296–311. http://dx.doi.org/10.1177/1359105312470156
48. Ford, A. L., Bergh, C., Södersten, P., Sabin, M. A., Hollinghurst,
S., Hunt, L. P., & Shield, J. P. (2010). Treatment of childhood
obesity by retraining eating behaviour: Randomised controlled
trial. British Medical Journal, 340, Article b5388. http://dx.doi.
org/10.1136/bmj.b5388
49. Walker, I., Thomas, G. O., & Verplanken, B. (2015). Old habits
die hard: Travel habit formation and decay during an oce
relocation. Environment Behavior, 47, 1089–1106. http://dx.doi.
org/10.1177/0013916514549619
50. Bouton, M. E., Todd, T. P., Vurbic, D., & Winterbauer, N. E.
(2011). Renewal after the extinction of free operant behavior.
Learning & Behavior, 39, 57–67. http://dx.doi.org/10.3758/
s13420-011-0018-6
51. Thrailkill, E. A., & Bouton, M. E. (2015). Extinction of chained
instrumental behaviors: Eects of procurement extinction on
consumption responding. Journal of Experimental Psychology:
Animal Learning and Cognition, 41, 232–246. http://dx.doi.
org/10.1037/xan0000064
52. Heatherton, T. F., & Nichols, P. A. (1994). Personal accounts
of successful versus failed attempts at life change. Personality
and Social Psychology Bulletin, 20, 664–675. http://dx.doi.
org/10.1177/0146167294206005
53. Verplanken, B., Walker, I., Davis, A., & Jurasek, M. (2008).
Context change and travel mode choice: Combining the
habit discontinuity and self-activation hypotheses. Journal
of Environmental Psychology, 28, 121–127. http://dx.doi.
org/10.1016/j.jenvp.2007.10.005
54. Thøgersen, J. (2012). The importance of timing for breaking
commuters’ car driving habits. Collegium: Studies Across

a publication of the behavioral science & policy association 83
Disciplines in the Humanities and Social Sciences, 12,
130–140. Retrieved from https://helda.helsinki.fi/bitstream/
handle/10138/34227/12_08_thogersen.pdf?sequence=1
55. Wood, W., Tam, L., & Witt, M. G. (2005). Changing circumstances,
disrupting habits. Journal of Personality and Social Psychology,
88, 918–933. http://dx.doi.org/10.1037/0022-3514.88.6.918
56. Orbell, S., & Verplanken, B. (2010). The automatic component
of habit in health behavior: Habit as cue-contingent
automaticity. Health Psychology, 29, 374–383. http://dx.doi.
org/10.1037/a0019596
57. Lemmens, V., Oenema, A., Knut, I. K., & Brug, J. (2008).
Eectiveness of smoking cessation interventions among
adults: A systematic review of reviews. European Journal of
Cancer Prevention, 17, 535–544. http://dx.doi.org/10.1097/
CEJ.0b013e3282f75e48
58. Wakefield, M., Germain, D., & Henriksen, L. (2008).
The eect of retail cigarette pack displays on impulse
purchase. Addiction, 103, 322–328. http://dx.doi.
org/10.1111/j.1360-0443.2007.02062.x
59. Robertson, L., McGee, R., Marsh, L., & Hoek, J. (2014). A
systematic review on the impact of point-of-sale tobacco
promotion on smoking. Nicotine & Tobacco Research, 17, 2–17.
http://dx.doi.org/10.1093/ntr/ntu168
60. Kirchner, T. R., Cantrell, J., Anesetti-Rothermel, A., Ganz, O.,
Vallone, D. M., & Abrams, D. B. (2013). Geospatial exposure
to point-of-sale tobacco: Real-time craving and smoking-
cessation outcomes. American Journal of Preventive Medicine,
45, 379–385. http://dx.doi.org/10.1016/j.amepre.2013.05.016
61. Lourenço, J. S., Ciriolo, E., Almeida, S. R., & Troussard, X.
(2016). Behavioural insights applied to policy: European
Report 2016 (Report No. EUR 27726 EN). http://dx.doi.
org/10.2760/903938
62. Roubal, A. M., Jovaag, A., Park, H., & Gennuso, K. P. (2015).
Development of a nationally representative built environment
measure of access to exercise opportunities. Preventing
Chronic Disease, 12, Article 140378. http://dx.doi.org/10.5888/
pcd12.140378
63. Woodcock, J., Tainio, M., Cheshire, J., O’Brien, O., &
Goodman, A. (2014). Health eects of the London bicycle
sharing system: Health impact modelling study. British Medical
Journal, 348, Article g425. http://dx.doi.org/10.1136/bmj.g425
64. Michimi, A., & Wimberly, M. C. (2010). Associations of
supermarket accessibility with obesity and fruit and vegetable
consumption in the conterminous United States. International
Journal of Health Geographics, 9, Article 49. http://dx.doi.
org/10.1186/1476-072X-9-49
65. Kohl, H. W., Craig, C. L., Lambert, E. V., Inoue, S., Alkandari, J.
R., Leetongin, G., . . . Lancet Physical Activity Series Working
Group. (2012). The pandemic of physical inactivity: Global
action for public health. The Lancet, 380, 294–305. http://
dx.doi.org/10.1016/S0140-6736(12)60898-8
66. Krishna, A. (2006). Interaction of senses: The eect of vision
versus touch on the elongation bias. Journal of Consumer
Research, 32, 557–566.
67. Cohen, D., Bhatia, R., Story, M. T., Wootan, M., Economos,
C. D., Van Horn, L., . . . Williams, J. D. (2013). Performance
standards for restaurants: A new approach to addressing the
obesity epidemic. Retrieved from http://www.rand.org/pubs/
conf_proceedings/CF313.html
68. Wansink, B., Hanks, A. S., & Kaipainen, K. (2015). Slim by
design: Kitchen counter correlates of obesity. Health Education
& Behavior. Advance online publication. http://dx.doi.
org/10.1177/1090198115610571
69. Rozin, P., Scott, S., Dingley, M., Urbanek, J. K., Jiang, H., &
Kaltenbach, M. (2011). Nudge to nobesity I: Minor changes in
accessibility decrease food intake. Judgment and Decision
Making, 6, 323–332.
70. Hanks, A. S., Just, D. R., & Wansink, B. (2013). Preordering
school lunch encourages better food choices by children.
JAMA Pediatrics, 167, 673–674. http://dx.doi.org/10.1001/
jamapediatrics.2013.82
71. Quinn, J. M., Pascoe, A., Wood, W., & Neal, D. T. (2010).
Can’t control yourself? Monitor those bad habits. Personality
and Social Psychology Bulletin, 36, 499–511. http://dx.doi.
org/10.1177/0146167209360665
72. Chen, G., Ding, X., Huang, K., Ye, X., & Zhang, C. (2015,
February). Changing health behaviors through social
and physical context awareness. Paper presented at the
International Conference on Computing, Networking, and
Communications, Anaheim, CA.
73. Geier, A., Wansink, B., & Rozin, P. (2012). Red potato chips:
Segmentation cues substantially decrease food intake. Health
Psychology, 31, 398–401.
74. Soler, R. E., Leeks, K. D., Buchanan, L. R., Brownson, R. C.,
Heath, G. W., Hopkins, D. H., & Task Force on Community
Preventive Services. (2010). Point-of-decision prompts to
increase stair use. American Journal of Preventive Medicine,
38(2, Suppl.), S292–S300. http://dx.doi.org/10.1016/j.
amepre.2009.10.028
75. Tobias, R. (2009). Changing behavior by memory aids:
Asocialpsychological model of prospective memory
and habitdevelopment tested with dynamic field data.
Psychological Review, 116, 408–438. http://dx.doi.org/
10.1037/a0015512
76. Bala, M., Strzeszynski, L., & Cahill, K. (2008). Mass media
interventions for smoking cessation in adults. Cochrane
Database of Systematic Reviews, 2013(6), Article CD004704.
http://dx.doi.org/10.1002/14651858.CD004704.pub3
77. Levy, D. T., Chaloupka, F., & Gitchell, J. (2004). The eects of
tobacco control policies on smoking rates: A tobacco control
scorecard. Journal of Public Health Management and Practice,
10, 338–353.
