
The George Washington University
School of Medicine and Health Sciences
“Guide to the 4
th
Year”
(Transition to Advanced Clinical Practice)
Everything You Need to Know about Senior Year and Successful Residency Matching
Prepared for the Class of 2025 by
The Offices of Student Affairs & Curricular Affairs
Table
of
Contents
Introduction ................................................................................. 4
Timetable ..................................................................................... 5
Career Decision-Making ............................................................. 7
What Should I be Doing/Thinking? ........................................................................................................... 7
Considerations in Specialty Choice ............................................................................................................ 7
Changing Residencies ................................................................................................................................ 8
Planning the Fourth Year ............................................................ 9
Goals ........................................................................................................................................................... 9
Scheduling................................................................................................................................................... 9
Graduation Requirements ........................................................................................................................... 9
Independent Study ..................................................................................................................................... 10
Electives ..................................................................................................................................................... 10
On-Campus Electives ................................................................................................................................ 10
Off-Campus Electives (“away” or “extramural”) ......................................................................................... 11
Visiting Student Learning Opportunities (VSLO) ...................................................................................... 11
Advantages and Disadvantages of Off-Campus (Away/Extramural) Electives........................................ 12
Timetable for Arranging Off-Campus Electives ........................................................................................ 12
Off-Campus Living Arrangements ............................................................................................................ 12
Arranging Away Electives .......................................................................................................................... 12
Documents Required for Away Electives (in order) .................................................................................. 13
International Electives ............................................................................................................................... 14
Military Active Duty Tours ........................................................................................................................ 14
Electives at The National Institutes of Health .......................................................................................... 14
USMLE STEP-2 Overview ........................................................................................................................ 15
Exam Failure and Consequences .............................................................................................................. 15
Exam Format ............................................................................................................................................. 15
USMLE Exam Scheduling ........................................................................................................................ 15
Faculty Advisors ......................................................................................................................................... 16
Letters of Recommendation ...................................................................................................................... 16
Applying for Residency .............................................................. 17
How do programs select residents? ........................................................................................................... 17
How to decide and where to apply ............................................................................................................ 17
How do you know if you are competitive? ................................................................................................. 18
Competitiveness: Strategies to Protect Yourself ........................................................................................ 21
The Application Process ............................................................................................................................ 21
The Electronic Residency Application Service (ERAS) ............................................................................22
Interviewing ...............................................................................................................................................22
How to Assess a Program During your Interview? ...................................................................................23
Supporting Materials ..................................................................................................................................24
New Trends in the Application Process ....................................................................................................25

The Match .................................................................................. 27
The National Residency Matching Program ............................................................................................. 27
Types of Programs ..................................................................................................................................... 28
Alternative Matching Possibilities in the NRMP ...................................................................................... 28
The Military Match .................................................................................................................................... 28
Canadian Students ..................................................................................................................................... 29
Specifics of Planning your Fourth Year ...................................... 31
Lottery ........................................................................................................................................................ 31
Consultation with your career advisory dean ............................................................................................. 31
Specific Scheduling Issues ......................................................................................................................... 31
Appendix A: Fourth Year Calendar 2024-25 ............................... 34
Appendix B: Interview Tips for the Residency Process ............. 35
Advance Planning: ..................................................................................................................................... 35
The Interview Day ..................................................................................................................................... 36
After the Interview...................................................................................................................................... 37
Appendix C: Residency Program Evaluation ............................ 43
Inpatient Experiences ................................................................................................................................ 43
Ambulatory Experiences ............................................................................................................................ 43
Special Educational Opportunities ............................................................................................................ 43
Residency Outcomes ................................................................................................................................. 44
Miscellaneous ............................................................................................................................................. 44
GUT CHECK (circle one) ......................................................................................................................... 44
Appendix D: Tips for Career Selection during Year III ............. 45
Overview .................................................................................................................................................... 45
Tips for Career Selection ............................................................................................................................ 45
Appendix E: Prior NRMP Match Data (LINK) ........................... 46
Appendix F: Writing a Curriculum Vitae ................................... 51
Writing a Curriculum Vitae (CV) ............................................................................................................... 51
CV Components ......................................................................................................................................... 51
Appendix G: Sample Curriculum Vitae ...................................... 53
Appendix H: Previous Residency Matchlist .............................. 56
Appendix I: Saving Money ....................................................... 70
Saving Money on Residency Travels ....................................................................................................... 70
Saving Money on Housing during Interviews .......................................................................................... 70
Guide to the Transition to Advanced Clinical Practice | 4
Introduction
Most of you have already started to think about what your career as a physician will entail. During the next several
months, you will begin to make important choices about specialty selection, residency training, and beyond. The
process of making these decisions is exciting and challenging, and this manual can help guide you. The guide is by
no means an exhaustive source of information. There are many sources of more specific information, and you
should take advantage of everything available to you. The time and attention that you invest in this process has
invaluable dividends. Get organized early, make note of important dates and deadlines and keep an eye on your
email inbox!

Guide to the Transition to Advanced Clinical Practice | 5
Timetable
It is critical for you to understand the timetable involved in planning residency applications. The schedule below
should serve as a guide as you plan your approach to the process. Please note that many of the websites mentioned
will update information for the upcoming residency application cycle in the next several months, so visit the sites
often. Students interested in Plastic Surgery, Ophthalmology, and Urology should note that the match process for
these specialties occurs early. Additionally, students in the Military Health Professions Scholarship Program
participate in an early match.
Third Year
Winter
Break
1. Reflect on clinical experiences and interactions with faculty and residents during the clerkships as
you begin the process of specialty selection.
2. Revisit the Careers in Medicine website (link) hosted by the AAMC (Use your AAMC ID to
login).
3. Review FREIDA online (link).
This is a searchable electronic database of all residency and fellowship programs in the U.S.
Review the Roadmap to Residency Site (link).
Review and complete the Google Portfolio Form, which will be utilized through the 2024 Match
Cycle.
4. Review the National Resident Matching Program publication, Charting Outcomes in the Match
(link).
This report casts light on how applicant qualifications affect match success.
5. Military Students: Start planning Active Duty Tours (Military Away Rotations) (link)
•
Army Students should review the information at:
http://www.goarmy.com/amedd/education.html
•
Navy Students should review the information at:
Graduate Medical Education (navy.mil)
•
Air Force Students should review the information at:
Application Instructions (af.mil) and 2022 Checklist (af.mil)
Military Residency Catalog:
http
s://www.usuaoa.org/program-previews
January
2024
1. Be sure to attend specialty night events with faculty in the areas of your interest. This may
include faculty at other institutions. Connect with current fourth year students in the areas of
your interest; they have completed applications, are on the interview trail, and have lots of
valuable information to share.
2. Review the Clinical Course Catalog (link) and plan your fourth year schedule. Use this guide and
the “Self-Assessment” scheduling guide in the Appendix. It may help to discuss this with your
Career Advisory Dean or a specialty advisor early in the process.
3. Enter your fourth year schedule requests into the web-based lottery system.
4. Consider fourth year electives at outside institutions and investigate deadlines for these
applications. Many medical schools will use the Visiting Student Learning Opportunities
website (link). Become familiar with the process.
5.
VSLO Authorizations are issued by the Deans Office.
February
2024
1. Select an official GW Faculty Advisor from the list provided by the
dean’s office (you can have more than one if you are considering multiple specialties).
2. Lottery results emailed to students
3.
Students begin to meet individually with Career Advisory Dean to review and modify schedules.
You will be assigned a time and date for this required meeting.
Guide to the Transition to Advanced Clinical Practice | 6
March-April
2024
Register for USMLE-2 to be taken by mid August
May 2024
Complete your Google Roadmap to Residency Longitudinal Questionnaire and personal statement
draft.
June
2024
Electronic Residency Application Service (ERAS) opens. Review the ERAS website (link) and
take note of all deadlines.
Situational judgment exams for Altus (if required/requested) should be scheduled by July 1
st
for select
specialties and programs.
Fourth Year
July
2024
Early Match (Ophthalmology and Urology) begins registration.
See Ophthalmology Match timeline here. See Urology timeline here.
August
2024
1. Complete application materials
2. Review transcripts for accuracy
3. Target date for Ophthalmology applications: August 15
4. Military students complete application
September
2024
1.
Students submit ERAS Supplemental Applications and register for NRMP Sept 15-19. All
students participating in NRMP match should register without delay once NRMP registration opens
2.
Students submit ERAS Application by Sept 28. MSPE, Transcript, LORs uploaded by Sept 29.
October
2024
1. Interviews for students participating in the NRMP, SF Match, and Urology Match begin.
2. Many specialties batch interview offers on uniform release dates.
Sept -
November
2024
Complete the weekly Student Affairs Interview Questionnaire
December
2024
Military Match complete
January
2025
San Francisco Match (Ophthalmology) and Urology matches complete
NRMP Registration deadline
February
2025
NRMP Rank lists due
March
2025
1. SOAP (Supplemental Offer and Acceptance Program) for unmatched students
2. NRMP Match Day

Guide to the Transition to Advanced Clinical Practice | 7
Career Decision-Making
What Should I be Doing/Thinking?
It is difficult to plan a fourth-year schedule effectively without having a fair amount of the third year under your belt
and some sense of your ultimate career direction. By January, you should begin to think about your career direction.
While it is premature to try to identify formal advisors in January (they’re still busy with fourth year students) there
is no harm, and it is very helpful, to talk with the more senior physicians with whom you work (residents,
attendings, etc.) about their career decision process. How did these people choose their specialty? What did the
residents and seniors do as electives? What really helped? Many third-year students feel confused with regard to
career selection. Next year by this time, almost all of you will have a very firm grasp of where you are and where you
are going. Those of you who already “know” ought to be a bit concerned: Have you come to a conclusion
prematurely and without reviewing all of the options? The Roadmap to Residency series can be your comprehensive
guide for career planning.
Considerations in Specialty Choice
Role of Core Rotations: While you are beginning to talk with people about career choices, you must firmly keep in mind
that your third-year rotations will give you an exposure to predominantly hospital-based medical practices. You can
certainly get some sense of a specialty by looking at what you see in our hospital clerkships, but you have to be very
careful not to assume that the life of the practitioner is similar to that of a third year clerk, the resident staff, or even
the full-time faculty on that service in the hospital. Also, remember that most residents primarily have experience
with in-hospital medicine. While it is appropriate and important to talk with senior students and residents - they are
closest to you and closest to having made career decisions -- practitioners are a more reliable and valid source of
information.
Therefore, it is important to talk with experienced physicians, particularly those in practice, to get some idea of what
the various generalists/specialists do in the “real” world. Don’t hesitate to stop attendings whom you know (and
even some you don’t know!) and ask questions. Talk to as many people as possible. Most of them will understand
your quandary and be delighted to share their points of view with you. While the primary care clerkship is not a
perfect representation of office experience, it is much closer to routine medical care than what you see in a hospital.
(Recall that only about 5% of an average physician’s patients have problems needing hospitalization in a given year,
much less in some specialties.) Keep your ambulatory experiences in mind!
Stereotypes and Biases: Stereotypes of practitioners in the various specialties must be recognized as having some real
basis, but many exceptions exist. For example, it is possible to be a very patient and long-term care oriented
surgeon, and conversely, a procedure-oriented and intensivist internal medicine physician. The kinds of people with
whom you feel most comfortable are likely to be the people with whom you will be most happy training with for
long and grueling hours. If you think you love a specialty but hate the physicians practicing it, you had better be
careful; the process of socialization throughout residency training is incredibly powerful. You need to consider the
duration of training: Are you able to postpone goal achievement sufficiently to tolerate a seven-year residency?
Lifestyle and Income: Many of you may want to consider the practice style and income of practitioners in various
specialties: Academicians tend to be paid less than private practitioners, pediatricians usually make much less than
surgeons. How important are these considerations to you to your spouse? All doctors work fairly hard and most of
you when applying to medical school said one of the attractions was that medicine was not in the “9 to 5” mentality.
Have you changed? Are you willing to make sacrifices for the needs of your patients? How much control of your
time do you demand? Are you willing to limit your practice to a certain patient population or age group (e.g.,
childbearing women, children, adults) or do you want to care for all people?
Personal Development: Another facet of this conundrum that you need to keep in mind is that we change over time!
Many students and residents enjoy being at the “cutting edge” of their field. Many like intensive/critical situations.
Guide to the Transition to Advanced Clinical Practice | 8
However, many physicians will tell you that their substantial joys during mid- practice years come from being of
service and making a difference in the lives of their patients. How can you know how you will feel in 15 years? You
probably can’t but you ought to be aware of this common change in older physicians.
Steps to Determine Final Choice: Finally, if you have narrowed your choice down to two or three options but don’t
seem to be getting any further, try a little exercise. Decide on one choice (“I’m going to be an obstetrician”) and live
with that choice for a week. See how you like being an obstetrician. How does your spouse like it, your family and
friends? During the day and evening try to picture how you would be spending your time, what your patients would
be like. After a week, try another choice (“I’m going to be a neurologist”) and live with that for a week. This will
help you focus on one at a time rather than having to constantly weigh one against another. In addition, scheduling
early experiences in your fourth year in a variety of specialties may give you further insight that will help you narrow
down your options. An early visit to one of the deans may also be helpful if you are in a particular quandary.
There are numerous written sources of information on choosing a specialty. Many of these are mentioned above in
the timeline table. In addition, we will hold another “Specialty Night” in January when you can meet faculty or
program directors from most of the major specialty areas.
Like all important decisions, your specialty choice will require you to spend many hours thinking, reading, and
discussing your options. Your advisors and the deans are an important resource that you should take advantage of.
Changing Residencies
Once you have made a decision about a career path and started a residency, it may be challenging to switch to
another specialty. This is largely a result of the way residency positions are funded. It is important that you be aware
of the way Medicare reimburses medical centers for postgraduate training.
Historically, Medicare paid each medical center around $30-50,000 each year for each resident. This varies
substantially from specialty to specialty, since it is determined by complicated formulas based on the Medicare
population served by that institution. Thus, for some programs it will be very high, while for others it may be much
lower. This subsidy is designed to offset the expenses of training residents (faculty, learning resources, etc.).
Medicare will only support residents for fixed periods of time linked to their specialty training (for instance, 3 years
for internal medicine, 5 years for general surgery, etc.). If you stay in residency beyond that time period, the medical
center only receives half of the original training subsidy (i.e. you essentially become fiscal red ink to the medical
center!).
The problem is not so much that you will stay longer in your original residency choice, but that this makes it
difficult to change residency programs in mid-stream. If you do two years in medicine and decide to switch
specialties, you will have only one full year of financing left. Therefore, any surgery program that wants to take you
will have to forfeit four years of full support. As you may imagine, this puts you at a disadvantage relative to freshly
minted graduates who have not used up any of their eligibility. This is making it more difficult to change residency
training once you have started. This means that you need to be as certain as possible about your plans at the time of
your original match.

Guide to the Transition to Advanced Clinical Practice | 9
Planning the Fourth Year
Goals
The fourth year comprises one quarter of your medical education. It is especially important because it is the crucial
time for you to solidify and broaden the foundation you have built in the first three years. In addition, it has
importance beyond your immediate educational needs: It is the time to better understand your residency options
and enhance your opportunities for the transition to your postgraduate years.
The goals then for the fourth year are:
Primary
To broaden your medical education (especially through your required courses)
To deepen your medical education (through your skillful selection of pertinent electives)
To solidify areas of weakness
Secondary
To gain more experience in areas of medicine to help you make a career choice.
To improve your chances for a successful match by: working hard and doing well in your fourth year
courses; working closely with faculty who might write your letters of recommendation; working in outside
hospitals to see if you would like being a resident there.
Scheduling
In January of your third year, we will use a “lottery” system for you to schedule your fourth year similar to that used
for scheduling your third year. In brief, you will initially choose courses both within and outside the GW system. We
have a fairly sophisticated computer algorithm to help you get your preferred schedule. After the lottery, your
Career Advisory Dean will meet with each of you and review the first draft of your schedule. During that time, we
will make all the appropriate modifications. A period of grace will follow during which you will be able to make
additional changes and finalize electives before the ADD/DROP procedure (LINK) goes into effect.
The purpose of this entire process is to get you your optimal schedule and simultaneously to allow our faculty
sufficient time to arrange for students from other medical schools to participate in our elective programs. (Note: we
will not accommodate outside students until your first scheduling deadline has passed.) In addition, the rising third
year class will select their preferences after you have selected yours.
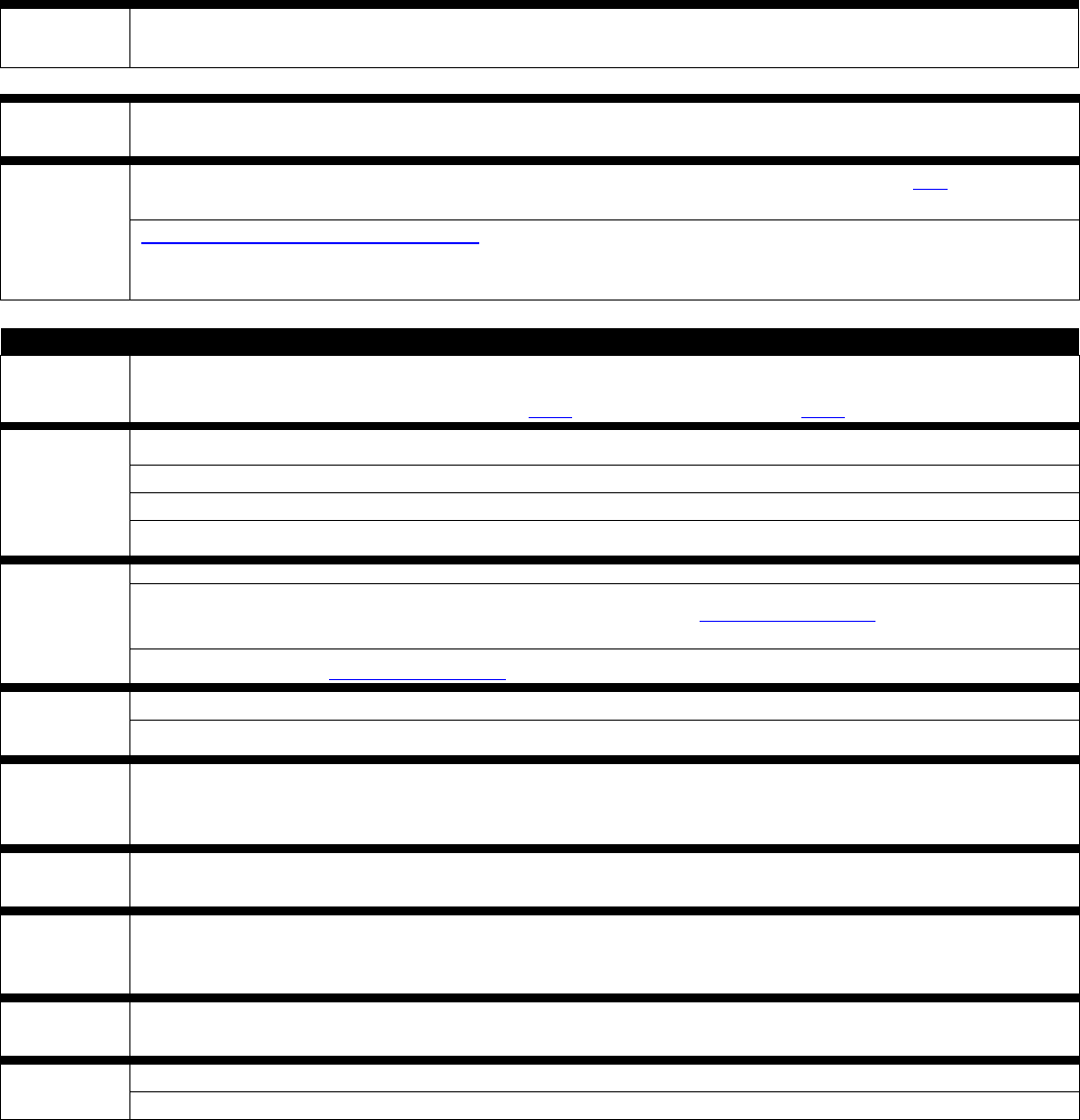
Graduation Requirements*
Course Name Duration Comments
Intersession IV
7 days
Intersession IV occurs Monday through Friday during week 44 at the start
of your 4
th
year
Acting Internship
4 weeks
Any one of the following satisfies this requirement: An Acting Internship
in Medicine or Pediatrics or General Surgery or Critical
Care/Anesthesiology (GW Hospital Intensive Care Unit), inpatient
Family Medicine (IDIS 390 extramurally), or Pediatric Intensive Care.

Guide to the Transition to Advanced Clinical Practice | 10
Anesthesiology (may be
completed in the third
year)
2 weeks
ANES 380 or ANES 302 satisfies this requirement. If taking the 4-week
ANES 380 Sub-I, this counts for 2 weeks anesthesia requirement and 2
weeks free choice electives.
Emergency Medicine 4 weeks
Adult (EMED 302) or Pediatric Emergency Medicine (PED 405) satisfies
this requirement.
Neuroscience (may be
completed in the third
year)
4 weeks
All students register for NEUR 380. This may be taken in the third or
fourth year, but must be completed at GW/affiliates. Students will be
assigned to various local sites according to a lottery system and will
receive
information via email about the site lottery about one month prior to the
block. Choices will include adult and pediatric neurology and
neurosurgery
sites, and will include both outpatient and inpatient experiences.
Transition to Residency
4 weeks
Taught weeks 36, 37, 38 and 39, coinciding with Match Day. All
graduating seniors are required to attend this course at GW. No other
course work can be scheduled at this time.
Free Choice Electives
in MS3 + MS4 years
26 weeks
minimum
These 26 weeks include any electives completed for credit during the third
year. On-campus electives are listed in the online course catalog. Off-
campus “away” or “extramural” electives may be arranged by the student
with the approval of the appropriate GW department and the dean’s
office. (more on this later)** may be impacted by COVID.
Independent Study
14 weeks
maximum
This is flexible time to be used for USMLE study, interviews, making up
missed clerkship time, etc. This does not count towards your elective 26
week elective requirement.
*in addition to completing all seven core clerkships. See Coursework Requirements for Class of
2025: LINK
Independent Study
You will have 14 weeks of independent study time that you are free to include in your schedule at any time.
Remember that in addition to time for relaxation, you will use independent study weeks to study for step 2, make up
any missed clerkship time, and to interview for residency. In addition, students have a mandatory additional vacation
week 1, June 27 – July 3, 2022 plus winter break (weeks 26 and 27) that is not counted in the 18 weeks. Remember
that during the Transitions to Advanced Clinical Practice phase there are NO guaranteed holidays off
(see duty hour policy) Any third year clerkship make-up time or any non-credit accruing academic work in year 4 is
deducted from your Independent Study time.
Electives
While we want you to use your fourth year to help you find a residency, we need to assure the broad educational
value of the year. We have accordingly employed a policy that restricts the amount of time a student can spend in a
specialty area to 12 weeks. This applies to individual specialties, not broad specialty areas. For instance, you could
take 6 weeks of general surgery, 4 weeks of trauma surgery, and 4 weeks of colorectal surgery without violating the
rule. However, 14 weeks of general surgery would not be permitted. Likewise, a mixture of medical, pediatric

Guide to the Transition to Advanced Clinical Practice | 11
surgical subspecialties are permissible, but you are not permitted to do more than 12 weeks of cardiology for
instance. Note: you can spend more than 12 weeks in a specialty area, but anything above 12 will not count towards
your course requirements and will be deducted from your vacation time.
On-Campus Elective
Any elective controlled by the GW elective registration system will be listed in our online Clinical Course Catalog,
and is considered on-campus. Any elective not listed in the catalog is considered off-campus.
Off-Campus Electives (“away” or “extramural”)
What are the Purposes for Doing Electives “away” from the Medical Center?
First, there is very little available outside of GW that one could not arrange to do within our system. For financial
and personal reasons, many of you will not be able to take electives away from the school. This is not a problem or a
liability for most specialties. However, some specialties may strongly encourage applicants to complete an
extramural "audition" elective in the summer months of the early MS4 year. (Please be sure to talk with your
specialty advisor regarding the utility of doing an away rotation.) Please be reminded that no additional financial
aid can be awarded to cover the extra costs of spending time on off-campus electives unless the rotation is outside
of the U.S., is credit bearing, and is taken as part of the Global Health Scholarly Concentration.)
Pre-COVID, about 30% of students took no away electives, 40% did one month away, and 30% did two or more
months off-campus. It is difficult to assess whether these rotations substantially helped students get their desired
residencies. Most students do not match to residency programs at which they did an extramural elective (excluding
military scholarship students). Visiting the program is no guarantee that it will remain top on your list, nor an
assurance of matching there. Given the timing of residency applications and interviews in the senior year it is VERY
DIFFICULT to do more than two extramural electives in your specialty of choice. Since most of you will apply to
20-50 residency programs it is obvious that you will only be able to do an away elective at a tiny fraction of the
programs that you are interested in. Therefore, if you choose to do this, you will have to pick a program(s) that you
are convinced may be the right place for you. See below for advantages and disadvantages of away electives.
Visiting Student Learning Opportunities (VSLO) / Visiting Student Application Service
(VSAS)
Visiting Student Learning Opportunities (VSLO), also referred to as the “Visiting Student Application Service”
(VSAS) (link) is an AAMC service designed to streamline the application process for senior “away” electives at other
U.S. LCME accredited medical schools, including in-person away electives as well as virtual experiences. Students
submit just one application for all participating schools, effectively reducing paperwork, miscommunication, and
time. VSAS also provides a centralized location for managing offers and tracking decisions. You will use VSAS if
you are applying for senior away electives at any of the host schools listed on the VSAS website. When applying for
electives at schools that are not using VSAS, you will need multiple documents. Different schools require different
combinations of these documents. The table below lists the various documents and where/how to get them
completed.
Other medical schools keep course directories online at their websites along with instructions and forms for
applications. These directories will be the most valuable source of information about off-campus electives and
application procedures. It is your obligation to be sure that the elective you are investigating outside of GW is at
least as good as the elective available within our own program. Senior students can be useful resources on these
issues. Also if you are interested in a particular hospital or program you might stop by the Dean’s office and review
lists of recent graduates and the programs to which they matched. It is often very useful to contact GW graduates
working at hospitals of interest, and ask them to recommend the best electives, the best teachers, etc. If we can help
with this, let us know.
Guide to the Transition to Advanced Clinical Practice | 12
Finally, most medical schools and many residencies now have very informative websites where you can find
important information. Students with prior academic difficulty must meet with one of the deans to determine if in-
person off-campus electives are permissible.
Advantages and Disadvantages of Off-Campus (Away/Extramural) In-Person Electives
There are some good reasons to take electives at other institutions:
Allows you to compare GW to other medical schools and yourself to other students.
Allows you to see if you will be comfortable with the geography and culture of the areas in which you are
thinking of practicing or training.
May be a good way to get a feel for the specialty.
May help your residency chances at that program. If you will be aiming high and you perform well, you may
make a more vivid impression at a prestigious program by taking an elective there.
May gain you a letter of recommendation from someone outside of GW. Such a letter may be viewed as more
objective than a letter from a GW faculty member (who has a vested interest in seeing GW graduates do well).
However, many of you will find the process of locating and scheduling extramural electives to be bothersome
and time consuming. It may be difficult to get the elective you want. Notification of acceptance to such electives
can be delayed into the summer or fall. Away or “audition” electives can be a double-edged sword. You may
look good, perform well, and impress, but you can also look flat and disoriented at new facilities in unfamiliar
surroundings. Know yourself!
There are also some risks in spending a substantial portion of the fourth year away. If you are planning on going
into a clinical residency, letters of evaluation are crucial to your success in matching. The evaluative comments that
are most important tend to be those written by clinicians. It is sometimes difficult for faculty to get to know you
(and for you to know them!) during your third year. Accordingly, some students use the early part of the fourth year
to know and be known by our faculty -- the group most interested in getting you a top residency. Many letters of
recommendation are written by members of our faculty with whom you work in the summer and early fall of your
fourth year. There are other disadvantages to away electives. Historically, we have done very well in terms of
advising and helping students match to good postgraduate programs. That advising does not readily take place long
distance. Our faculty is often willing to contact friends at other institutions, to put in a good word for students they
know. That does not happen when you have been away for the entire fall. Taking care of the details that are so
important to this whole process can be difficult from a long distance.
Timetable for Arranging In-Person Off-Campus Electives
Plan to begin submitting applications for away rotations by the start of February of your MS3 year (February 2024).
Most medical centers with active elective programs will not begin signing-up an outside student until early spring.
They may accept applications as early as December 2023, but they will rarely commit to a specific course schedule
until sometime in February-April 2024. Many schools will be unable to accommodate requests to complete an away
elective during the end of the 3rd year (May, June).
Many of you, although early on inclined toward a particular medical field, will make substantial changes in your
timetable during the remainder of this year. Therefore 1) don’t get yourself locked into one or a set of programs that
may have no bearing or meaning to your ultimate training plans; 2) don’t commit yourself to programs without
complete and careful discussion of your options and opportunities here, as well as away, with at least one advisor;
and 3) don’t get yourself or GW a bad reputation at hospitals for signing-up but then reneging on a prematurely
arranged elective!
Off-Campus Living Arrangements
You will usually have to arrange your own housing at any extramural site that you attend.
Arranging Away Electives

Guide to the Transition to Advanced Clinical Practice | 13
All students taking off-campus electives must get prior approval to participate in these courses. You must have a
“Permission to take Extramural elective” form on file in the dean’s office before going to any off-campus rotation.
Permission to take an off campus elective is granted by a course director in the department that coincides with
your requested elective. For example, if you want to do an away elective in general surgery at Georgetown, you must
get permission from the GW General Surgery clerkship director. This permission form is found electronically on
the GW SMHS website (Current Students->Forms). All students must have a GW Uniform Clinical Evaluation
Form completed for their away rotations, which is then sent back to our registrar. Students are also required to
complete an evaluation of the off-campus elective experience.
Documents Required for In-Person Away Electives*
Document
Provided by
Comments
Affiliation Agreement for
all non-VSLO institutions
Dean’s office (Sherry
Brody)
Budget at least 3-6-months for an affiliation agreement to be
ratified by both GW SMHS and host institution. Note: it is
possible that an agreement cannot ultimately be reached.
You
may not rotate at an institution without a signed
agreement
in place. [This is not necessary if you apply
through VSLO.]
Application Form from
the
host institution (non-
VSLO
institutions)
Dean’s office (Registrar,
Career advisory dean)
Generally
these require a section to be completed by your
career advisory dean, signed and sealed with the official
school seal. Turnaround time: 1
-2 business days
Curriculum Vitae
Student
See Appendices F & G
Profile Photo
Student
Criminal Background
Check/Drug Testing
Dean’s office
(Vendor: Certiphi®)
Most schools will accept your previous results obtained
dur
ing your second year in preparation for your clinical
clerkship
rotation. Some schools will require that you have
this done again (possibly at your expense) prior to the
rotation;
the school can provide information on vendors to
have this completed.
Official Transcript
Student Center
Most
VSLO participants will accept unofficial transcripts
uploaded by the dean’s office. Official transcripts are
handled by the University Registrar.
HIPAA Certification
Office of Medical
Education
Completion of HIPAA modules is currently a requirement
for successful completion of POM. Documentation of
successful completion of HIPAA is provided as part of the
General
Letter of Good Standing. If the institution requires
additional information, please contact OSA for assis
tance
Immunization Record
MedHub, Student,
Employee Health
Most VSLO participants require the AAMC Standardized
Immunization
Form (link). Some schools have their own
immu
nization forms. Students should complete these
forms in conjunction with Employee Health or their
primary care provider.
Proof of Health Insurance Student
Photocopy
of your insurance card (front and back)
Basic Life Support (BLS)
Certification
Tel: 202-741-2958
Email: gwtrainingcenter@
mfa.gwu.edu
Photocopy
of your BLS card (front and back)

Guide to the Transition to Advanced Clinical Practice | 14
Proof of Malpractice
Insurance (aka Certificate
of Insurance / COI)
Dean’s office (Sherry
Brody)
$2
Million (Each Claim)
$3
Million (Aggregate)
Mask Fit
GW Health & Emergency
Management Services
Tel: 202-994-8425
Email: [email protected]
Letter of Good Standing
(LOGS)
Dean’s office
Submit your request to the Dean’s office administrators
using
the LOGS request form found on the website (Letter
of Good Standing/Recommendation Request (gwu.edu)
).
Completed
letters are generally available for pick up within
24- 48 hours.
Official School Seal
Dean’s office (Registrar)
Upon acceptance,
complete
“Permission to Take Off-
Campus Elective
Form” (Permission to take
Extramural elective)
GW Clerkship Director in
the specialty area you are
requesting to do your away
elective.
For
example, if you want to do an away surgery elective you
must have permission from the surgery clerkship director.
This
ensures that our students are steered to programs with
the most educational value. Turn
completed forms into the
dean’s office
*Virtual electives may require only a portion of these required elements.
International Electives
There are specific and legitimate reasons for some students to study abroad. Students with a strong interest in
differing health administration systems have spent time in countries with different health care systems. Others have
gone abroad because of an interest in Global Health or participation in the Scholarly Concentration Program.
Others, usually strong and very independent students, have done a primary care experience in a third world country.
These electives may need to be planned a year in advance.
GW has several formal programs and exchanges with international programs and schools. For information about
the location, timing, and application procedures refer to details in the online Course Catalog, or contact the Office
of International Medicine Programs. All medical students participating in international clinical electives or summer
internships, regardless of whether they are in the Global Health Scholarly Concentration or not, must register and
apply through the International Medicine Programs (IMP) office and obtain permission from their career advisory
dean. Also see the school policy on international electives Students interested in international electives at non-
affiliated sites must inquire with and obtain permission at least three months in advance of the elective from the
Office of International Medicine Programs.
Military Active Duty Tours
Those of you in the military should make contact with your program office in the fall/winter of your third year to
arrange for active duty tours in the early summer. If at all possible, it will work to your advantage if you are able to
identify the specialty of your ultimate interest, and the hospital in which you are most interested in working by
winter break of your third year.
Electives at The National Institutes of Health
Another valuable elective experience is at the NIH which offers both clinical and research electives. Additional
information may be available through the Scholarly Concentration in Clinical and Translational Research or OSPE.

Guide to the Transition to Advanced Clinical Practice | 15
USMLE STEP-2 Overview
Most residency programs are placing increased value on the USMLE Step 2 score when determining which
applicants to interview and subsequently rank. Virtually all programs want a USMLE Step 2 score before offering
interviews to applicants. and, nearly all programs require a Step 2 score prior to ranking applicants Consequently,
it is imperative that you allocate the proper amount of study time in preparation for taking USMLE Step 2.
Common errors that lead to suboptimal scores include:
Taking less than 4 weeks to prepare for USMLE Step 2
Failure to schedule a meeting with Dean Goldberg if you’ve had repeated difficulties with standardized tests
in the past or a marginal performance on Step 1
Preparing for the exam while doing other activities (electives, family obligations, interviews, etc.)
Exam Failure and Consequences
Failure of a USMLE examination can adversely affect your chances of successfully matching. Failure of step-2
though has its own unique challenges:
Step-2 is focused on clinical knowledge. Consequently, some programs consider it more predictive of
your ability to function as a resident, and they will be less forgiving of a step-2 failure.
Depending on when you initially scheduled the exam you may have limited time to study and retake it
before residency programs beginning offering interviews in late Summer/Autumn.
Exam Format
The USMLE-2 exam will be administered at Prometric Technology Centers throughout the US. There are nine
centers within a one hour drive of GW, and additional centers throughout the US. The CS exam was previously
administered at five regional centers, the closest location is in Philadelphia, Pennsylvania.
Scheduling
When you apply for the Step 2 examination, you will designate a three-month window in which you would like to
take it. Once your application has been processed (about 6 weeks), you will receive certification allowing you to call
Prometric or the NBME in order to schedule a testing date at the center of your choice. Scheduling can be done
starting 6 months before the date of the exam. Please visit www.nbme.org for the most current information on
application procedures, costs, and deadlines.
We recommend that you complete the scheduling process for USMLE Step 2 no later than the beginning
There is no fee to change dates if done more than 14 calendar days in advance. If
you wait until the summer, you may have trouble scheduling the exams. Remember you are required to complete
both components of the exam by November 1 of your fourth year. If you have not passed the exams by
graduation, you will not receive a diploma. If you do not receive a diploma at graduation, the University will not
issue a diploma until June 30 or later! Consequently, you may not be able to start your residency rotation on time.
of March of your third year.

Guide to the Transition to Advanced Clinical Practice | 16
More and more residency program directors want to see your Step 2 scores BEFORE they begin to offer
interviews in October - November. The military programs have historically required that scholarship students sit for
Step 2 by the end of August or September. For the rest of you, there are a number of considerations. First, many
residency programs like to see your Step 2 scores during the residency application process (particularly programs
in more competitive training fields; you must have it by September for OB/GYN). Second, if you performed
marginally on Step 1, a good score on Step 2 may help your application significantly.
Our fourth year overview is now complete. In the next few chapters we will discuss advisors, applying for
residencies, and the Match, and then finish with two chapters on the specifics of how to design your fourth year.
Advisors
Advisors are guides, sources of information, and sources of contact with the “outside” for the remainder of your
stay at GW. Ideally, an advisor should be knowledgeable about the elective programs available here and elsewhere,
knowledgeable about residency programs over the whole country, willing to find out more about you and your
abilities, able to make you feel comfortable and able to get things done! In the real world, however, no one person
can do all these things well. Try to select an advisor that suits your specific needs best. It is particularly important to
select a person with whom you feel comfortable talking honestly. If your advisor is not well versed in a particular
area, seek out other people who are. Many specialties have designated a faculty member to serve as the key advising
figure for all students applying in their specialty (often a Residency Director, Clerkship Director or Department Chair).
(Link to faculty advisor guide)
Your official advisor may be your main source of advice but do not let that stop you from filling in the gaps by
talking with many other faculty. Students who have had difficulty with the match have typically not connected with
a good advisor.
Advisors and Letters of Recommendation
Your advisor is someone you should be able to talk with candidly. You should feel comfortable bringing up your
doubts, fears, career decision angst, weaknesses as well as triumphs. Some students have their advisor also prepare a
letter of recommendation; though some students choose to have other faculty write their letters (you will need three
letters of recommendation in total).
Mechanics of Selecting an Advisor
While you cannot formally choose an advisor yet, there is great benefit in starting to think about advisors and
meeting with potential advisors early. We will provide you with an updated list of advisors in each department. Ask
the fourth year students who the really good advisors are! Talk with as many attendings and consultants as you can.
The major reason you are not permitted to choose an advisor until February is that up to that time they are still very
involved with their 4th year advisees. Your advisor will also work with you on refining your fourth year schedule.
Guide to the Transition to Advanced Clinical Practice | 17
Applying for Residency
How do programs select residents?
There is little question that program directors look at your performance in medical school as the prime
consideration. Grades, your letters of recommendation, what you say about yourself in your application and/or
personal statement, your research experience, your community service, and extracurricular activities are all
important. Most programs look at National Board scores. For most programs, the most important factor is their
assessment of your stability, reliability, and teachability through your academic record, letters of recommendation,
and the interview.
For more information about what factors program directors consider important in considering an applicant, review
the results of the NRMP Program Director Survey. https://www.nrmp.org/wp-content/uploads/2022/09/PD-
Survey-Report-2022_FINALrev.pdf
How to decide and where to apply
Types of Hospitals
There are numerous ways of classifying hospitals. In general, the primary training hospital of an academic medical
center (e.g., the GW University Hospital) often is very different from one not on the main campus. Some
unaffiliated hospitals may be community-based and vary in their focus on education.
If there is a possibility that you will be considering postgraduate training in the form of specialty fellowships, post-
doctoral research fellowships, etc., you are more likely to be accepted to these programs if your residency was done
in a university-based training program, less likely in an affiliated hospital, least likely from an unaffiliated program.
(There are, however, certainly exceptions to this rule.) Accordingly, many seniors consider seeking university-based
programs as a means of keeping their options open. This fact tends to make these programs more competitive than
others.
Another basis for classifying hospitals is the public versus private continuum. While there can be great educational
emphasis in both public and private institutions, the major difference between these is the degree of responsibility
given directly to residents and the (often inversely related) quality of support services. At private hospitals, the final
word is always in the hands of the private physicians who admitted the patient. At public hospitals, while there is
always an attending responsible, care and management decisions are usually considered by the residents and then
checked and confirmed with the attending. In these situations, residents usually feel more responsible for decisions.
Programs with very strong fellowship programs and programs in hospitals that segregate patients by specialty
(thereby allowing a stronger presence of specialty fellows) tend to keep their early trainees in less critical roles.
Responsibility and opportunity to make decisions is available to trainees at these hospitals later in their postgraduate
training. For some, this is ideal; for others, it is at best an annoyance, and sometimes a significant hindrance to
learning.
Private institutions generally have more of the amenities, whereas public institutions often are more barebones.
Your own experiences at places like Holy Cross versus the V.A. Hospital, will likely give you some sense of this.
Location
It will come as no surprise that some areas of the country are considered more desirable than others! Because
competition is stiffer in geographically desirable locations, you are more likely to match at a better quality residency
in a less popular location. Also, as increasing numbers of physicians locate in highly desirable locations, finding jobs
in those areas can be difficult. Past studies have shown that 70 percent of physicians practice within a one-hundred
mile radius of the hospital in which they did their last years of residency training. If you are interested in doing a

Guide to the Transition to Advanced Clinical Practice | 18
residency and settling in a desirable location (e.g., states of California, Washington, Oregon; cities of New York and
Boston), you have a good chance of doing so (our students from California in particular have been doing well
matching to West Coast programs). However, you may have an even better chance in some of the superb
institutions of the south and the midwest. We urge you to test the waters.
Duration of Training
Two or three states allow a physician to be licensed to practice after graduation; most require a minimum of one
year of postgraduate training. Virtually no U.S. physicians follow these pathways. Most do at least three years of
training. When you match into a categorical residency program, the program expects that you will complete their
entire curriculum. For instance, if you are an applicant to a pediatrics training program, the program assumes you
are applying for year one, but will stay on for years two and three. NRMP matches you in a legally binding manner
for your first year. Unless you and the program have a major issue, you will be offered a contract for Year 2 usually
around November.
How do you know if you are competitive?
You need to consider two components: 1) How competitive is the specialty to which I am applying? 2) How do I
stack-up against the other applicants? There is considerable variation in competitiveness between specialties. A
useful technique to assess this is to look at the percentage of applicants who matched to a specific specialty. The
chart in the appendix shows the percentages of U.S. seniors and independent applicants who matched to their
preference specialty.
For a comprehensive look at the NRMP match results you may review the AAMC publication, Charting Outcomes
in the Match: Characteristics of Applicants Who Matched to their Preferred Specialty in the 2023 NRMP Main
Residency Match.
Once you are committed to a specialty, how do you evaluate your competitiveness within the field? In general,
advisors’ recommendations and thoughts can give you some sense of your level of competitiveness. The better
advisors are pretty good at predicting where students are safe.
A more general way of assessing competitiveness is to look at the current residents of each program. How many are
members of Alpha Omega Alpha, the medical honor society? How many are foreign trained? How many of our
students have been accepted to that program in recent years? How are the GW alumni, who have worked in that
hospital, perceived?
If you happen to do an elective at an outside hospital, evaluate the competence of the interns (and other fourth-year
students). Our students usually come back feeling at least as competent as their peers from other schools, if not
more so. It is of note, however, that many seniors do not match to programs they felt comfortable in when they
took an elective there.
You will also have access to the Texas STAR database that includes self-reported student data from most medical
schools in the country for the past several years. This database has a lot of data (that can be overwhelming at times),
but it’s handy to see where applicants similar to you got interviews and where they eventually matched. Don’t forget
to pay it forward by completing the Texas STAR Match Survey on Match Day to provide data for your little sibs.
More Information on Competitiveness – Grouped by Specialty
Medicine Programs
Guide to the Transition to Advanced Clinical Practice | 19
There is a wide range of competitiveness in medicine programs and a large number of good programs available.
Larger programs, especially those affiliated with medical centers, are commonly offering two separate tracks
within the Department of Medicine: one for people who plan a subspecialty career in medicine or who at least
want some subspecialty training, and the other (by cooperating with other departments) in a more general or
primary care program with more experience in ambulatory internal medicine practice. Many medicine programs
also offer a preliminary as well as a complete categorical program. In the complete program, the expectation is
that if you do a reasonable job, you will stay on and complete your three years of training in that program. If
you select a preliminary program, the program makes a commitment to you for only one year. If you do well,
many programs will try to make room for you for the second year. For some of you who have a strong interest
in a particular hospital, you may want to consider applying to both their three-year program, and, to increase
your chances, to their one-year program as well. In outstanding hospitals, one year programs may not fill, while
the 3 year programs almost always fill. Due to recent changes in medicine and the support for postgraduate
training some programs are cutting back on preliminary positions, making these programs more competitive.
Medicine programs use the NRMP to match applicants.
Pediatrics Programs
Pediatrics is a 3 year residency and has historically had a favorable match rate for students. GW graduates have
done very well. Virtually all of our pediatric applicants match, if they complete their rank list reasonably.
Pediatrics programs use the NRMP to match applicants. There are some programs that have special tracks in
addition to categorical tracks, like those that are focused on community health or advocacy/social justice,
primary care, or research. When discussing with your advisor, consider your interests in free standing children’s
hospitals, academic pediatrics or community programs, geography, and intern class size, in addition to special
features (i.e. global health, advocacy, medical education, research, etc).
Medicine/Pediatrics and Other Combined Programs
A growing phenomenon is the emergence of combined programs. The oldest is Medicine/Pediatrics (a 4 year,
double board eligible program). These are of interest to those who want a broad age spectrum of patients, and
who don’t want to do OB and surgery (i.e. family practice). Because all the combination programs are relatively
new and small in number, there are only a few advisors who know much about these options. There are several
faculty members in pediatrics who trained at med-peds programs. Otherwise, you will need to talk to one of the
deans and other advisors in individual specialty areas to discuss whether a combined program is right for your
needs. To get more information, you might call a couple of programs and talk with a few residents.
Other combined programs include: Medicine-Emergency Medicine, Medicine- Family Practice, Medicine-
Neurology, Medicine-PM&R, Medicine-Preventive Medicine, Medicine-Psychiatry, Pediatrics-Emergency
Medicine, Pediatrics-PM&R, Pediatrics- Psychiatry-Child Psychiatry, Psychiatry-Child Psychiatry, Psychiatry-
Family Practice, and Psychiatry-Neurology. Most of these combined programs use the NRMP to match
applicants.
Family Medicine Programs
Family medicine has been a specialty for many decades. It is a reasonably popular choice for American medical
school graduates (about 10% of whom choose FP for their PGY-1 program). A general theme in family
medicine selection seems to be “How do we know that you really want to be a family practitioner?” In the past,
many of our students have felt at a disadvantage answering such questions because we don’t have a Department
of Family Medicine (although now we do have a division of family medicine under the Department of
Emergency Medicine.) It is reasonable to point out to interviewers, that GW was one of the first medical
schools to require an ambulatory (primary care) clerkship for all students during the third year when students
still have some career flexibility. Many of you worked with family practitioners while on that rotation. For those
who didn’t, many programs would like to see that an applicant has done a clerkship with a family practitioner or
in an established family medicine program. Your advisor or one of the deans should be of assistance in helping
you decide if you want to do a clerkship off-campus. Dr. Andrea Anderson serves as the main family medicine
advisor for our students. Many of the established family medicine programs are becoming traditional: They are
increasingly looking more heavily at grades, board scores, and the like. Generally, however, family medicine
Guide to the Transition to Advanced Clinical Practice | 20
programs place very great emphasis on the kind of person you are, your aspirations, your experience working in
more rural or underserved environments, and where you intend to practice. The style and “interviewability” of
the applicant appear to be very important to most FM programs. Family Medicine programs use the NRMP to
match applicants.
Psychiatry Programs
Psychiatry has seen a greater than 10% increase in the number of matched applicants from 2015-2019. Given
the recent national level push towards population health and integrated health care have increased the interest in
this field. Psychiatry is now considered a moderately completive field with a 99% program fill rate over the past
two years. This fill rate is higher than pediatrics, internal medicine, and anesthesiology. Many applicants have
good traditional academic metrics, so students who have shown a sustained interest in mental health care are
particularly sought out by psychiatric residency program directors. Historically our students have always done
well in psychiatry, frequently matching to some of the most popular training programs. Psychiatry programs
match via the NRMP system.
Obstetrics/Gynecology Programs
Obstetrics and Gynecology has historically been a moderately to highly competitive field. Our Department of
Obstetrics has an aggressive and very successful approach to getting our graduates matched into good
programs. In this department particularly, it is imperative that you keep the department well informed of your
interests. Obstetrics/Gynecology programs use the NRMP to match applicants.
Surgery and Surgical Subspecialties
General surgery is usually a five-year or six-year program and has become increasingly more competitive over
the past years.
Most of the surgical subspecialty programs allow you to apply via NRMP for Year-1 and automatically track into
your final destination. Other programs require that you find your first one or two years of general surgical
training, but simultaneously (as seniors in medical school) complete applications for your subspecialty surgical
training program as well. A large percentage of orthopedic, urology, neurosurgery, plastics, and ENT programs
have joined with the general surgery programs in their institutions to form a complete program. Matching to
such a program will guarantee the first one or, in some situations, two years of general surgical training prior to
the essentially automatic admission to that department’s surgical specialty training program. Ophthalmology
programs almost always require you to find your preliminary year separately through the NRMP process.
There is an independent (non-NRMP) match that handles the ophthalmology match. The urologists have yet
another match for candidates who intend to start urology training. You can go to the
https://www.sfmatch.org/ (ophthalmology) or the https://www.auanet.org/education/urology-and- specialty-
matches.cfm (urology) web sites for full information and registration information about these matches.
Right now orthopedics, urology, neurosurgery, ophthalmology, dermatology, otolaryngology, and plastic surgery
are VERY competitive. If you are considering one of these specialties you should meet with that department
early and realistically assess your chances. Any student who has not done truly outstanding work thus far must
consider some type of back-up plan.
Emergency Medicine Programs
EM programs match via NRMP for either complete (three or four years) or advanced (PGY-2 placement)
programs. Review the web site at SAEM.org and click on the “medical student section” for more information.
Your advisor can help you choose among the program options for a best fit. EM is moderately competitive, so
be sure to coordinate carefully with your advisor to maximize your chances of matching.
Radiology Programs
Radiology is an average competitive specialty. In most cases you will have to match to your preliminary year
separately from the Radiology program. Radiology programs use the NRMP to match applicants.
Guide to the Transition to Advanced Clinical Practice | 21
Dermatology Programs
Those of you interested in dermatology will need to match for your PGY2 position and a preliminary year.
Dermatology remains the most highly competitive field, nearly a quarter of all applicants go unmatched to a
position each year. Every student interested in dermatology should consider a back-up plan. Dermatology
programs use the NRMP to match applicants.
Anesthesiology Programs
In the past several years, GW students have done extremely well in the anesthesiology match. However, this
specialty has become more competitive recently. Most programs require a preliminary/ transitional year before
the anesthesiology residency and some programs include this year as part of the categorical program. You will
be applying to both through the NRMP match.
Physical Medicine and Rehabilitation Programs
This is a field that is becoming more attractive every year, and GW students have done very well in this match.
PM&R programs use the NRMP to match applicants.
Competitiveness: Strategies to Protect Yourself
Competing for residencies in competitive fields is obviously difficult; nonetheless, GW students have a fine track
record: most of our students in the Military Scholarship programs get their first or second choice of training site and
‘path’ (e.g. categorical military training, preliminary military training followed by GMO service, or civilian
deferments (deferments tend to be much less predictable, but many of our students who have requested deferments
have been successful). Our students applying in ‘early’ match specialties have also done well; although a number of
less competitive students fail to match in some of these specialties almost every year. Overall, from year to year only
about 3-6% of GW seniors fail to match to a residency program.
Those of you applying to the more competitive specialties (orthopedics, otolaryngology, urology, ophthalmology,
plastics, neurosurgery, and dermatology) must exercise great caution. The first question you need to ask is, “How
much do I want this field?” If you are convinced only “x” will satisfy you, then you absolutely should give it a try.
However, if you see attractions in other areas, we suggest you look at them again, and carefully.
Students applying to such highly competitive specialties must carefully consider back up plans regardless of the
strength of their academic records. Students with average or weak academic records absolutely must have a firm and
rational back-up plan in the event that they go unmatched. Viable back-up plans include:
Applying to one or more alternative specialties
Applying to preliminary positions in surgery or medicine (although preliminary programs are becoming
more competitive especially in medicine)
Taking a year off after graduation and reapplying
Taking a year off between third and fourth year to do research in the specialty area you are considering
All these strategies have advantages and disadvantages, and you should carefully discuss them with your faculty
advisors and with the deans.
The Application Process
Settling on a group of residency programs that you would like to apply to is a complicated but achievable goal.
However, it will require a lot of “leg work” on your part. Unfortunately, there is no single resource that attempts to
describe individual residency programs or compare their quality or competitiveness. This will be frustrating to many
of you. You will need to access as many resources as possible to find out about programs. Although many programs
sustain their reputations for quality training and competitiveness from year to year, as you may expect, many
programs will fluctuate quite widely in these characteristics over even relatively short time spans.

Guide to the Transition to Advanced Clinical Practice | 22
For instance, changes in the residency director or other key faculty can raise or lower a residency program’s status
very dramatically overnight! In addition, changes in the nature of the hospital(s) or ambulatory training facilities
affiliated with each program may affect the quality of the program significantly [particularly in these days of rapid
and unpredictable change in health care. Consequently, what a recent graduate or faculty member may “know”
about a program could become inaccurate very quickly. In addition, faculty that have spent a great deal of time at
GW (and those who did their residency training more years ago than they would like to admit!) may have very
limited insight into the current status of any particular training program. You will need to ask around quite a bit to
find faculty who may be knowledgeable about residencies outside of the immediate Washington, DC area or their
own residency training program. Here are a few quick tips for identifying residency training programs:
Pick a specialty (or maybe more than on if you are still deciding!)
Pick some geographic regions in which you think you might like (or need!) to be.
Warning: Those of you applying to very competitive specialties should not be too picky about geography;
you will need to apply broadly! Regardless of your specialty choice, very narrow geographic preferences (like
“I have to be in Washington, DC”) are extremely risky and are the source of many of our recent matching
failures. Unless you are among the most outstanding members of the class, you’d better consider more than
a single very isolated geographic area. The application process isn’t the time to be picky. You can always
turn down an interview if offered.
Make a list of potential programs in those geographic areas using FREIDA
Narrow your list. This is the hardest part, but here are some suggestions:
1. How competitive are you as an applicant? (ask your advisor(s), or one of the deans)
2. What kind of program do you want (university, university-affiliate, community)?
3. What kind of program are you competitive at (the answer to this question may or not be the same as
your answer to the prior question, and will vary by specialty choice)?
4. Visit program websites for detailed information
5. Check to determine if we have any recent graduates at the programs you are considering (see Appendix)
6. Determine if we have any faculty members who trained or served as faculty at any of the programs (this
requires you asking around).
7. Do an audition rotation at the program (an away elective, usually set up in the spring or summer of your
third year)
The Electronic Residency Application Service (ERAS)
ERAS is an application service that is run by the Association of American Medical Colleges. Except for early match
programs, virtually all specialties use ERAS.
ERAS makes your life immeasurably easier. Through this system everything related to the application process is
done online. Next summer, those of you using ERAS will receive all the necessary instructions. You will complete
your application online, and designate letters of recommendation that are to be sent to programs. Your letter of
recommendation writers will upload their letters directly into ERAS. The Dean’s office will upload your transcript
and your MSPE into ERAS.
Most residency programs will utilize ERAS though you will still need to double check to make sure that all the
programs to which you would like to apply are participating in the electronic system. If you are interested, visit the
ERAS web site at: www.aamc.org.
Interviewing
Programs use different strategies to determine who they will interview. Most will require a completed application
including letters of recommendation and the MSPE before considering your application. Others will make their first
round of decisions about interviews based solely on academic performance gleaned from the transcript. It is to your
Guide to the Transition to Advanced Clinical Practice | 23
advantage to submit all documents to ERAS in a timely fashion. Remember the MSPE is released on or around
October 1 for all students (the date varies by year according to the ERAS calendar). This includes military students and
those participating in early match programs. This is a nationwide release date set by the Association of American
Medical Colleges and no exceptions are permitted.
Since many programs will contact you through email, you absolutely must check your email regularly (several times a
day). We have heard of several students who opened an email with an interview invitation a few hours late, when
they called the program, found out that all the interview spots were filled and they were ‘waitlisted’ for an interview.
Due to COVID-19, the class of 2022’s interview season was completely virtual. This is a great cost-savings but also
requires different considerations in terms of lighting and ensuring appropriate technology/sound. It is unclear
whether your class will have strictly virtual interviews, in-person interviews, or options to do either. See
Interviewing Tips in the Appendix for additional guidance and advice on conducting virtual or in-person interviews.
The timing of interviews has grown more complex. The majority of programs still allow applicants a choice of dates
for their visit. Increasingly, however, programs are identifying specific days (e.g., every Tuesday or the first Monday
of each month, or specific dates) and restrict interviews to those times. Most interviews will be scheduled in mid to
late November, December, and January. Most military interviews are in August and September and occur while
students are doing their active duty tours. Early matches will interview earlier, sometimes as early as September or
October. By and large, you should not plan on formally interviewing at more than one program per day, whether in-
person or virtual. For in-person preferred programs, you may even want to arrive a full day ahead of your interview
to get a better sense of the program (to be particularly sharp and knowledgeable in your interview) and attend the
optional dinner the night before. Accordingly, we strongly recommend you plan to reserve a full four weeks of
vacation time to complete your interviews. For those of you applying to PGY-2 programs and therefore also having
to apply for a preliminary position, six weeks is not too much time. On occasion, programs will insist that you
interview when you are on an elective rotation. In this occurrence, our faculty (except for those responsible for the
acting internships, Neuroscience, Anesthesia and Emergency Medicine) is usually quite adaptable. Attempts to do this
frequently, however, can cause substantial difficulties. Remember you cannot graduate with incomplete or failing
grades on your record.
Interviews can take many forms: Some programs actually quiz students on their field. A more common ploy is to
ask the student to present a case, and then the interviewer discusses that case and its ramifications with the
applicant. Most programs simply try to assess your interest in their program, your apparent ability to get along with
strangers, your general philosophic approach (e.g. research-oriented, primary care-oriented), etc. Obviously, be
yourself, although it is a good idea to have thought about a couple of cases before embarking on your visits.
Remember also, an interview is a two-way street-you are interviewing them as well as they, you. Be knowledgeable
about their program and have well-thought-out questions ready to ask. A list of interviewing tips is attached in the
Appendix. Your career advisory deans are available for mock interviews and we encourage you to take advantage of
this.
How to Assess a Program During your Interview?
Statistics regarding the number of hospital admissions, the number of outpatient visits, the number of surgical
procedures, etc., can give you a start on assessing the nature of the program before visiting it. The program’s
website, social media accounts, and discussions with residents and advisors will give you additional information.
Virtually all students agree that they derive considerable information from interviewing and visiting a program and
its hospital(s). This makes assessing a program solely by virtual means a bit more challenging. As usual, the best
sources of information about a program are the people in that program. Seek out a few residents and ask them
about their gripes as well as their pleasures. A good tack is to try to identify G.W. alumni: in general, they are very
helpful and tend to be more willing to open up and make comparative statements.
Most students are particularly interested in the teaching qualities of the programs that they are considering. A good
way to at least get a “snap shot” of the program is to attend a conference, virtually or in-person, to ask multiple
Guide to the Transition to Advanced Clinical Practice | 24
house officers about the teaching strengths, or to ask to attend resident’s report ) if that’ is not preplanned as a routine
part of your visit).
If your visit is in-person and you are touring the hospital with one of its housestaff, you can get some sense of the
orientation of the program by visiting a general ward or ambulatory practice. Another aspect to investigate is the
degree of housestaff responsibility. Is the program intern-oriented, or dominated by upper echelon housestaff? Who
takes primary (not legal) responsibility for patient care?
Certainly one of the most commonly used assessment instruments is to ask, “Are the residents happy?” Visits to the
program generally help you assess this. Don’t forget that you will have sampling problems, so talk with more than
one house officer. Finally, very few interns are “happy.” Don’t only ask PGY-1s if they are happy, but check on
PGY-2s and 3s as well.
Each of you must decide what’s important for you. For some, outstanding housestaff and excellent teaching faculty
will more than make up for lots of hassles with radiology, laboratory, the nursing staff, and/or a tough schedule.
For others, a reasonably-guided experience in a comfortable place will be sufficient and productive. Before you
convince yourself that you know the answer to this question now, however, plan on trying to visit a couple of
different types of programs: Exposing yourself to your various options may have considerable impact on your
outlook and change your position from the one you expected.
It’s very important to keep detailed information about each program during and after your interview. The appendix
has one suggested form that you can use to keep track of important program information. Feel free to copy this
form, adapt it to your needs, or make your own form. Trust us, after your 15th interview; everything will seem to be
a blur if you haven’t kept careful notes about each program and your overall impressions.
Revisiting a program after the interview for what has been termed a “second look” has become more popular over
the past several years and is recommended by some as an opportunity to show heightened interest and potentially
improve your chances of matching. We discourage this practice and encourage you to speak with one of the deans
to discuss this if you are considering second looks. Second looks are costly and unlikely to strengthen your match
success.
Supporting Materials
Letters of Recommendation
Most PGY 1 programs request at least three letters of recommendation, (in addition to your MSPE, see below).
Some departments will prepare a Department Letter for you summarizing all your work in that department and
signed by the chairperson or their designee (or both). A Department Letter usually “counts” as one of your three
letters. In general, whether you have a Department Letter or not, it is usually best that at least one of your letters
comes from a GW faculty member in your specialty field of interest. Your additional letters can come from
physicians in your specialty field, though it is usually more important that the recommender can report close
personal experience with your clinical or research skills than whether or not they are in your specific field of
interest. Letters from “senior” more well-known faculty are usually preferable, but detailed, believable letters from
junior faculty are usually given more weight than vague, impersonal letters from a Nobel laureate who met you for
30 minutes in their office one day! Even though they may know you in more detail than faculty, letters from
residents and fellows are worse than useless (program directors may interpret a lack of faculty support as a very
strong negative factor!). Some programs will not limit the number of letters that you can send; but it is usually not
wise to send more than 3 unless the additional letter(s) add something unique and substantive that cannot be
gleaned from your “top three” recommenders. Letters from non-GW faculty are certainly acceptable and may be
particularly helpful in some fields, but except in unique circumstances no more than one of your letters should be
from outside faculty.
Don’t forget the general rule: When asking individuals for a recommendation, it’s a good idea to ask,
“Do you feel you can write a strong letter of recommendation on my behalf?” This gives the faculty member the

Guide to the Transition to Advanced Clinical Practice | 25
opportunity to say, “Gee, maybe you ought to turn elsewhere,” and decreases the chance that a fairly negative letter
will go forth. Also realize that you must keep on top of whether or not the letter has actually been written and sent.
Several students have been surprised by deadlines passing without letters having been sent. Once you designate
letters of recommendation to be sent via ERAS, you can check the ERAS website to see if the letter has actually
been uploaded to the program.
Medical Student Performance Evaluation: The MSPE (Dean’s Letter)
The MSPE is a detailed letter prepared by your career advisory dean. The letter begins with a “Noteworthy
Characteristics” section that will include three brief bullet points (each bullet point can be two sentences long),
which highlights your unique experiences, skills, or path to medical school. It also includes your academic history,
including explanation for any time off, and it will list any below passing grades. Most of the letter will provide
detailed information about your clinical performance during the third year clerkships and place that performance in
the context of the entire class. You will have a chance to review and (within limits) edit your letter. However, this is
a letter of evaluation not recommendation, and therefore it will contain a balanced description of your strengths and
weaknesses. The Dean’s Office holds ultimate editorial control over the contents of the letter.
The formal clerkship evaluations written and submitted to the Dean’s Office at the end of each clerkship will be the
basis for a substantial portion of your MSPE. If you are concerned about comments made in the narrative
summaries of your clerkship evaluations, it can be useful to meet with the clerkship director as soon as possible
after its receipt and discuss the evaluation. Your narratives will also be important for other writers of
recommendations and also for your advisor. You should consider giving your letter writers a copy of your grades
and your clinical narratives to help them when writing your letter.
Transcripts
Most programs request transcripts. The Dean’s Office uploads all transcripts for ERAS applications. These
transcripts are then directly downloaded by the corresponding programs. The Dean’s Office cannot directly send
you official transcripts. For non- ERAS applications you must obtain them directly from the University Registrar at
the Marvin Center. Those of you who took some medical school courses elsewhere (for example, transfers from
U.S. schools), should request these additional transcripts be sent directly to the dean’s office to be uploaded to
ERAS or sent directly if you are using a non-ERAS application.
Board Scores
Students who participate in ERAS can have their NBME scores directly transferred to ERAS participating residency
programs. Students whom are not participating in ERAS must contact the NBME directly to request an official
report of scores be sent directly to the programs.
New Trends in the Application Process
Some specialties have added special features to the application process. As of this writing some of these may or may
not be incorporated to the upcoming application cycle so stay tuned into the specialty of your choice so you know
what is expected. Recent examples include:
Emergency Medicine: The specialty requires completion of the Standard Letter of Evaluation (SLOE) Form, with
ideally two forms submitted (typically from 1 home and 1 away rotation.). Emergency medicine had piloted the
AAMC Standardized Video Interview for the 2020 and 2021 seasons, but has decided to NOT continue this pilot
for your 2022 interview cycle. You may find this medical student advising guide from Council of Residency
Directors in Emergency Medicine and Emergency Medicine Residents’ Association helpful:
https://www.cordem.org/resources/education--curricula/advisingguide/.
Orthopaedic Surgery: The American Orthopaedic Association’s Council of Orthopaedic Residency Directors (CORD)
has introduced a Electronic Standardized Letter of Recommendation (eSLOR) - American Orthopaedic
Association (aoassn.org)for applicants applying to Orthopaedics.

Guide to the Transition to Advanced Clinical Practice | 26
Otolaryngology: The Otolaryngology Program Directors Organization (OPDO) has reported that inclusion of a
program-specific paragraph at the conclusion of the applicant’s personal statement is optional (It was mandatory in
2016). Programs still requiring a program-specific paragraph will alert the applicant of this fact. The telephone-based
assessment in which the applicant records responses to a series of questions is also optional. No data collected from
the completed assessment will be released to the programs until after the Match process. This past year (for class of
2021), ENT piloted a signaling program where each applicant had 5 “signals” to give to programs that they were
most interested in. Data from this pilot is pending and it is unclear how and if this program will continue for your
class.
Plastic Surgery: Plastic Surgery introduced a new application portal, the “Plastic Surgery Common Application” also
called the “Central Application”, during the 2022-2023 application season, which can be accessed here. The
program directors group in Plastic Surgery has standard letter of recommendation form for applicants applying in
Plastic Surgery. A copy of the Plastic Surgery Residency Recommendation Form can be obtained at the following
link as well as other helpful resources for students can be found on the American Council of Academic Plastic
Surgeons website: https://acaplasticsurgeons.org/Resources/#residents.
Anesthesiology: A small number of Anesthesiology residency training programs are now asking applicants to register
for supplementary testing to assess personal and professional characteristics that might predict success in residency
through commercial products such as Altus (takealtus.com). During the 2022 application cycle, 13 Anesthesiology
residency programs required Altus testing between early August - October.
Obstetrics & Gynecology: A small number of OB/GYN residency training programs are now asking applicants to
register for supplementary testing to assess personal and professional characteristics that might predict success in
residency through commercial products such as Altus (takealtus.com) During the 2022 application cycle, 7 OB/GYN
residency programs required Altus testing between early August – October. OB/GYN has recently announced
intentions of migrating the application process away from ERAS and to a third-party platform (similar to
Ophthalmology and Plastic Surgery) in 2024.
Guide to the Transition to Advanced Clinical Practice | 27
The Match
The vast majority of positions for graduate medical training are filled using one of four matching programs.
Most students will apply using ERAS and match to a residency using the National Resident Matching Program
(NRMP).
Military students will apply and match to a residency using the special Military Match System, MODS. (Note that all
military students should register for the NRMP and apply to civilian programs through ERAS in case you are
deferred to a civilian residency.) The exact process can change from year to year.
Students interested in Ophthalmology will apply to a PGY-2 residency position in Ophthalmology using the
Centralized Application Service (CAS) and match to residency using the ophthalmology matching program, San
Francisco Match. Note that all students applying to ophthalmology will also use ERAS to apply for a preliminary
(PGY-1) position and the NRMP to match to a preliminary position.
Generally, students interested in Urology will apply using ERAS (some programs don’t use ERAS and you will need
to contact them directly) and match to residency using the American Urological Association Match. Note that you
may also need to register for the NRMP match for the general training which is required prior to beginning
urological training.
After reading the above information, it is obvious that all students will need to register for the NRMP. The
following NRMP information is therefore applicable to all students.
The National Residency Matching Program
The National Residency Matching Program was developed in the 1950’s to try to bring order into what was then an
absolutely chaotic system. It has succeeded magnificently, and seems to be getting better organized and stronger.
Virtually all U.S. medical school graduates who are seeking postgraduate training participate in the NRMP. Signing
the agreement form for participating in the NRMP makes explicit (legally binding) that: 1) the hospital will accept
the student who matches to its program, and 2) the student will accept the program to which he/she is matched
(i.e., neither of you can change your minds after the Match), for the PGY1 year.
Essentially, the NRMP sets a timetable for students and program directors to evaluate and then rank order each
other. Students submit a rank order list (ROL) of the programs to which they are applying; program directors rank
order all the applicants to their programs. A computer algorithm matches you to that hospital which is highest on
your list and which has ranked you highly as well. The matching program allows students to list their hospitals in
priority order. If your first five choices are very competitive and ultimately have no position for you, but your sixth
hospital has you highly ranked, there is no less chance of your matching to that sixth hospital if it is in the sixth
position, or the first or, in fact, the 15th. Please keep this fact in mind: A number of students (and advisors) around
matching time fear that highly ranking their out of range choices will have a negative impact on the other programs
on their list. This is a misconception. How many programs you rank depends upon the competitiveness of the
programs to which you are applying.
As a general rule, most students should rank all acceptable programs at which they interviewed. You should apply to
enough programs at the right level of competitiveness to garner 10-15 interviews. For some of you this is 10-15
programs, for some 50-60, and perhaps many more. It is very rare for a student with 10 programs on their final
ROL to go unmatched. In general, list every program at which you interviewed unless you think you would prefer
not matching to attending that program.
The independent matches (San Francisco Matching Program and the American Urologic Association Matching
Program) will again match programs in ophthalmology and urology. Information about these programs is found at
SFMATCH.org or AUA.org.
Guide to the Transition to Advanced Clinical Practice | 28
Types of Programs
There are three types of first-year programs: categorical, preliminary, and transitional (flexible) programs.
Categorical programs are full and complete training programs in a specialty, e.g. medicine, general surgery,
orthopaedics. While you match through NRMP for the first year, the assumption is you will be continuing and
completing the specialty program in that hospital.
Preliminary programs exist in medicine and surgery and are one year in duration. While this preliminary year is
usually identical to that hospital’s “categorical” program, the program is not committed to you beyond your first
year of training. These programs are typically selected by people going into another kind of program after the first
year. e.g., urology, dermatology, ophthalmology, or radiology. Sometimes they are chosen by people who have not
yet made a final career decision. They tend to be good places to learn general skills applicable to many fields.
Transitional programs are the so-called “rotating” internships. They usually consist of a year that allows a student to
spend a few months in most major departments of the hospital and are not a part of a complete residency. Only a
small portion (if any) of the transitional program year can subsequently be applied to meet a specialty board’s
requirements. Thus, if you subsequently decide to go into medicine, it may take you a year longer (than someone
who began in medicine) to complete the program.
Alternative Matching Possibilities in the NRMP
Ninety-five percent of you will use the common and straightforward system for matching: You seek a full time, one-
year program via NRMP; you submit your rank order of desired programs. However, there are a couple of other
alternatives, noted here in decreasing order of use:
Couples (no legal definitions are used) can fill out a couples rank order form that links the choices of two
people. The computer tries to match the couple to their highest pair of programs and thereby allows people
who want to be together to organize their rank order lists (ROLs) in tandem.
Another available option through NRMP is for two people to be identified under one NRMP student
number. This pre-formed pair would apply to all programs and implies that the two students would share
equally in one program. In the first year, both members of the pair would get six months of credit and do
their internship over a two-year period.
If any of you are interested in the couples or pair matches, please contact your career advisory dean to discuss these
options in detail.
The Military Match
Students in the Military HPSP programs (Navy, Army, and Air Force) have three potential pathways in the Military
Matching Program. You can match to a categorical (straight) program at one of the Military Consortium Hospitals;
or to a preliminary or transitional military internship, followed by a tour of duty as a General Medical Officer
(GMO); or receive a deferral to match to a civilian residency program. You owe the military a year for each year of
your scholarship. Residency training in the military does not count towards your pay-back. However, years spent as
a GMO or as a board eligible/certified physician (after residency) do count towards your scholarship pay-back.
Deciding which of these pathways to request can be complicated. The military training programs are very good, and
students applying in fields that are highly competitive in the civilian world may find it easier to match to such fields
in the military. In addition, scholarship students who complete GMO duties in the military are given high priority
for military residency positions, thus offering another avenue to enter competitive training programs that you may
not be able to enter in the civilian match. Requesting a deferral to civilian residency training offers the advantage of
many more programs to which you can apply in a wider geographic area. However, the number of deferrals can vary
dramatically from year to year. In other words, you can request deferral in order to train in a civilian program, but
you may not get it. Unfortunately, every year the military elects to defer one or more students who did not request a
deferment. Needless to say, this can be problematic. Therefore, every military scholarship student must register with
Guide to the Transition to Advanced Clinical Practice | 29
the NRMP and apply to some civilian programs so that they are positioned to interview at and match to a civilian
program if they get “bad” news from the military in mid- December. You can put off interviews until after you hear
from the military and withdraw applications if you match within the military, but you can’t wait till mid-December
to apply to programs.
All of the military services want student application forms completed by August. They tend to make selections in
November and announce their decisions in mid-December. In the past, our students have done extremely well in
the military match. Indeed, many students get their first choices. This likely relates to the military’s confidence in
GW graduates, and also to their resident selection process. It is important to recognize that this selection process is
very different from that used in the civilian area. Military programs don’t participate in the NRMP. In the military,
who you know and who knows you is very important. Because of this, most of you are planning to spend an early
period (between May-October) in electives at military programs. If you do a clerkship and haven’t met the
Department Chairperson, ask your attending to introduce you. If your ADT clerkship is not with the department to
which you are applying for residency, make an appointment and meet the senior members of that department. Also,
many of the military docs know their peers at other military hospitals. It is reasonable to ask them to call a friend at
another program and put in a “good word” for you. Finally, it is wise for you to interview at a few of the hospitals
where you won’t have done an ADT by phone, Skype, or in person!
Canadian Students
Students from Canada will need to decide early in the application process if they are staying in the US for residency
training or if they wish to return to Canada. There are various advantages and disadvantages with either choice and
Canadian students are advised to speak with their advisory dean at the start of the third year regarding these options.
A full discussion of the Canadian match process is beyond the scope of this guide and only a general overview of
the visa options and applying to Canada through CaRMS will be presented.
Staying in the US: Visas for Residency
To stay in the US, residencies will have to grant the Canadian student a visa. Some programs do not offer any
visas and therefore not worth applying to. There is information about visas on FREIDA, however it is not up-
to-date or trustworthy consequently, student should email each program they are interested in directly and ask if
they sponsor or support visas for Canadians. In this email, the student should mention they are a US medical
student and are Canadian.
Basics on the Visas:
F1- OPT: F1 is the student visa we get from GW. We can extend it for 12 months as “Optional Professional
Training” for the first year of residency.
H1B: This is a green card eligible work visa – the student can potentially stay at the end of residency. Programs
have to legally prove an American could not fill the position and it costs the hospitals money; consequently only
a few schools offer this type of visa.
J1: This is a training visa. At the end of residency the student must return to Canada for two years. Student
should look up the Royal College accreditation requirements for their specialty to make sure they can practice
when they return to Canada.
To get a J1, Health Canada must issue you a “Statement of Need”. Health Canada is limiting the number of
SONs it will issue. http://www.hc-sc.gc.ca/hcs-sss/hhr-rhs/postgrad-postdoc/cat_b-list-liste-eng.php
Some schools “sponsor” a J1, others say they will “accept applications from individuals with a J1”. The second
means that the student goes to an organization called the ECFMG to sponsor their visa.
Applying To Canada
Students apply to the Canadian Match through the Canadian Resident Matching Service (CaRMS). Like the
NRMP, CaRMS uses an algorithm to match students to their desired residencies. Students who are seriously
considering residency training in a Canadian program are highly advised to familiarize themselves with the
Guide to the Transition to Advanced Clinical Practice | 30
CaRMS application, and to meet with an advisory dean in January of their third year. The general timeline of the
CaRMS application process is outlined below:
1. August – Register for the match, GW verifies attendance with a letter of good standing
2. September – Application opens
3. October – All documents need to be mailed in or uploaded
4. November – Application is submitted
5. December – Interview invites sent out
6. January -Feb – CaRMS interview season
7. Mid-February – Rank lists due
8. First Wednesday of March – CaRMS Match
There are several important differences between the CaRMS process and NRMP process. Key differences between
the matches are highlighted below:
Residency Positions: In America everyone competes for the same residency positions regardless of where
you graduated. In Canada they have separate residency positions for CMGs and IMGs so that they are not
in direct competition. A Canadian USMG applies for the CMG positions.
The NRMP has the Match and SOAP process. In CaRMS this is replaced with 1st and 2nd Iterations
process. If you go unmatched for the 1st iteration you have the option of applying to the 2nd iteration.
The vast majority of Canadian medical students apply to two specialties. The statistics are the same as the
US in that one should rank 10-12 programs to feel safe(r) about matching,
Interviews in Canada are more intense than the US. There are more MMI interviews, ethical questions,
behavioral questions etc.

Guide to the Transition to Advanced Clinical Practice | 31
Specifics of Planning your Fourth Year
Now that we have discussed advisor, career, residency, and match issues, you have much of the background needed
to put together the best possible fourth year schedule for you. To maximize your chance of getting your ideal
schedule (yet ensure that everyone gets a fair chance at the most popular electives), we utilize a computer matching
system. In your fourth year, the faculty wants you to have a strong general medical education. Remember, there is a
twelve-week limit on subspecialty experiences.
There are four steps to producing a schedule:
1. Information gathering
2. Review the Course Catalog; evaluations of electives by students from the graduating class are available to
review in the dean’s office.
3. Consultation with your advisors
4. You can meet with your specialty advisor or your Career Advisory Dean to discuss your schedule choices.
Lottery
To access the lottery program, once open for you to select your fourth year schedule preferences:
https://portal.smhs.gwu.edu/MDStudentWeb and enter the GW Net ID and Password that is used to access your
GW email.
Consultation with your Career Advisory Dean
Each student will meet individually with their career advisory dean to review and revise your schedule. Students will
be selected randomly and notified by email of the date and time of your meeting during February-March of your
third year. You can modify your schedule later on if you choose.
Specific Scheduling Issues
Independent Study: You will have 18 weeks of independent study time that you are free to include in your schedule at
any time. Remember that in addition to time for relaxation, you will use independent study weeks to study for Step
2 and to interview for residency. This does not include the mandatory vacation week (week 1) nor the two weeks
of winter break (weeks 26 and 27). Remember that during the Transitions to Advanced Clinical Practice phase,
there are NO guaranteed holidays with the exception of winter break (see duty hour policy)! Any third year
clerkship make-up time or any non-credit accruing academic work in year 4 is deducted from your Independent
Study time.
Interviewing Time: Set aside at least 6 weeks for interviewing. A rough guideline to follow is to allow three interviews
per week. The best times are late November, December, and early January (except for the early matches, October
and November are best). Consult your advisor regarding when you should schedule your independent study time
for interviewing based on historical data.
Students on military scholarships should also leave time for civilian interviewing in the event that their service
defers them. Most of the services inform their students of the military match results by mid-December.
Accordingly, some time (at least two weeks) in December or January should be set aside in case you need to
interview for civilian programs. If you don’t need to interview, you can always add a course.
Away Electives: As soon as you receive acceptance to do an away elective and a detailed description from the away
elective, you will need to obtain approval to take the elective from the appropriate GW department and from the
Dean’s Office. Please note that before you start the elective, the Dean’s Office must have a “Permission to take
Extramural elective stating your schedule, location of the elective, course title, preceptors name, and the approval
signature of a GW departmental course director. You will be covered by the GW malpractice insurance

Guide to the Transition to Advanced Clinical Practice | 32
policy only when you are taking an approved elective off-campus. In order to be covered by this insurance,
however, the elective must be approved by the departmental designee, and the Deans office, and a copy of the
approval form be present in your folder prior to the beginning of the course. Failure to meet these requirements
could result in canceling the course and will be grounds for disapproving all subsequent off-campus electives. If the
institution you would like to rotate with in-person does not use VSLO, there is an extra step involved to ensure an
affiliation agreement between institutions is in place. Because new affiliation agreements can take weeks to months
to set-up between legal counsels, you will need sufficient lead time, and it is your responsibility to track this process.
If a necessary affiliation agreement is not signed by the time your rotation starts, you will not be able to rotate at the
outside institution. For non-VSAS institutions requiring a new affiliation agreement, please contact your advisory
dean with the institution and your rotation dates at least 4 months prior to your rotation start date.
Third Year Courses: Some of you have third-year work to complete. We do our best to add the delayed clerkship when
you wish to take it, but placement depends on overall enrollment numbers. Remember that as a fourth year student,
you do not have site priority if taking with the rising class. Anyone taking a third-year course who has had any
academic problem during the third year should complete the requirement prior to January 1 of the 4th year.
Step 1: If you still need to take Step 1, you will likely wish to schedule this after you complete all third-year
clerkships. Consider budgeting no more than 4-8 weeks for this exam in order to accomplish the other goals for
fourth year prior to submitting your applications. You will likely want to see the results on your exam (3-5 weeks)
and take a break prior to studying and taking Step 2. As long as you take Step 2 by early-mid August, you should
have your score by the time applications are due for most specialties.
Advanced Electives: Most students will want to do an advanced elective in the specialty they are interested in. For some
specialties, these must be scheduled in advance, directly with the department. If you are interested in careers in one
of the specialties below, you must contact the clerkship coordinator when the fourth year lottery is open to reserve a
space for your advanced elective early during your senior year. Use the “390” course code in your schedule to hold a
space until you meet with one of the deans. For instance, if you have arranged with the Department of Orthopaedics
to do an orthopaedic sub-internship during weeks 6-9, you would enter the code ORTH 390 during weeks 6-9. After
all individual scheduling meetings in February/March, the 390 course code will be changed to reflect the actual
course that you have reserved with the department.
Anesthesia
Contact the course coordinator when the lottery opens to reserve a spot in ANES 380, the four-week sub-
internship. Use the ANES 390 code in the lottery during the block you have reserved. The two-week ANES 302
elective will be available in the lottery.
Emergency Medicine
Emergency Medicine requires advanced reservations during May-September (weeks 45-13). Contact the course
coordinator to reserve a block and enter EMED 390 in the lottery during the block you have reserved. During the
remaining months, EMED 302 is available through the lottery directly.
Orthopaedics
The orthopaedics advanced elective is a one-month preceptorship that virtually all students considering orthopaedics
as a career select. The department must operate an unusual schedule. They therefore require that any student
interested in a one-month preceptorship contact Yolanda Porter at 202 741-3311 in January during the open lottery
period. Hold a space in your schedule using ORTH 390.
Surgery Acting Internships
Students who are interested in a General Surgery residency are strongly encouraged to complete a Surgery AI. When
the lottery opens in January, please contact the surgery coordinator to communicate your preferences for team
placement at GWUH and to schedule your AI. Use SURG390 to hold your reserved space until you meet with the

Guide to the Transition to Advanced Clinical Practice | 33
Deans to finalize your schedule.
Ophthalmology
Students interested in ophthalmology should contact the department coordinator in January during the open lottery
period to schedule elective time early in the year. Hold a space in your schedule using OPHT 390.
Dermatology
Students interested in Dermatology should contact the dermatology coordinator in January during the open lottery
period. Dermatology requires departmental permission for all elective scheduling. Use DERM390 to hold the
relevant spot in your schedule.
Radiology
Students interested in Radiology should contact the department coordinator in January during the open lottery
period to schedule electives. You can reserve a space in your schedule using RAD 390.

Appendix A
Fourth Year Calendar 2024-25 for Class of 2025
Week 44
Apr 22–Apr 28 2024
INTERSESSION IV Mon thru Fri only
Week 45
Apr 29 - May 5, 2024
Week 46
May 6 – May 12, 2024
Week 47
May 13 - May 19, 2024
Week 48
May 20 – May 26, 2024
Week 49
May 27 - June 2, 2024
Week 50
June 3 – June 9, 2024
Week 51
June 10 – June 16, 2024
Week 52
June 17 – June 23, 2024
Week 1
June 24 - Jun 30, 2024
Vacation/”Spring Break”
Week 2
July 1 - July 7, 2024
Week 3
July 8 - July 14, 2024
Week 4
July 15 - July 21, 2024
Week 5
July 22 - July 28, 2024
Week 6
July 29 – Aug 4, 2024
Week 7
Aug 5- Aug 11, 2024
Week 8
Aug 12 – Aug 18, 2024
Week 9
Aug 19 – Aug 25, 2024
Week 10
Aug 26 – Sept 1, 2024
Week 11
Sept 2 – Sept 8, 2024
Week 12
Sept 9 - Sept 15, 2024
Week 13
Sept 16 -Sept 22, 2024
Week 14
Sept 23 – Sept 29, 2024
Week 15
Sept 30 - Oct 6, 2024
Week 16
Oct 7 – Oct 13, 2024
Week 17
Oct 14 – Oct 20, 2024
Week 18
Oct 21- Oct 27, 2024
Week 19
Oct 28 – Nov 3, 2024
Week 20
Nov 4 – Nov 10, 2024
Week 21
Nov 11 – Nov 17, 2024
Week 22
Nov 18 – Nov 24, 2024
Week 23
Nov 25 – Dec 1, 2024
Week 24
Dec 2 – Dec 8 2024
Week 25
Dec 9 – Dec 15, 2024
Week 26
Dec 16 – Dec 22, 2024
VACATION/”Winter Break”
Week 27
Dec 23 – Dec 29, 2024
VACATION/”Winter Break”
x
Dec 30 – Jan 5, 2025
VACATION/”Winter Break”
Week 28
Jan 6 – Jan 12, 2025
Week 29
Jan 13 – Jan 19, 2025
Week 30
Jan 20 – Jan 26, 2025
Week 31
Jan 27 – Feb 2, 2025
Week 32
Feb 3 – Feb 9 2025
Week 33
Feb 10 – Feb 16, 2025
Week 34
Feb 17 – Feb 23, 2025
Week 35
Feb 24 – Mar 2, 2025
Week 36
Mar 3 -Mar 9, 2025
Transitions to Residency
Week 37
Mar 10 – Mar 16, 2025
Transitions to Residency
Week 38
Mar 17 – Mar 23, 2025
Transitions – Match Day 3/21/25
Week 39
Mar 24 – Mar 30, 2025
Transitions to Residency
Week 40
Mar 31 -Apr 6, 2025
Week 41
Apr 7 – Apr 13, 2025
Week 42
Apr 14 – Apr 20, 2025
Week 43
Apr 21 – Apr 27, 2025
Week 44
Apr 28 – May 4, 2025
Week 45
May 5 – May 11 2025
GRADUATION
Sunday May 18, 2025
Guide to the Transition to Advanced Clinical Practice | 34
APPENDIX B
INTERVIEW TIPS FOR THE
RESIDENCY PROCESS
With Virtual Interview Updates for Class of 2021 and 2022
Advance Planning:
● Always carry several copies of all your application materials (copies of ERAS or CAS
applications, CV, personal statement, etc.) -->Have application materials on hand in
case you need to refer to them.
● Know your CV, personal statement, and MSPE thoroughly. You will be asked questions
about things that appear in these documents.
● Try to find out from the interview coordinator as much detail about the interview day as
you can (when to arrive; who you will meet with; opportunities to meet with residents,
tour facilities, attend conferences, etc.; are there ‘informal’ parts of the interview
process such as dinner with residents) -->Know the schedule for the day and all options
to interact with residents
● Try to find out as much about the program as you can.
○ Who are key faculty (program director, etc.) and what are their
interests/specialty/research (can try a literature search by their name to find out
their research interests or other published work).
○ Contact friends or previous GW grads who are familiar with the program (the
legendary Guide to the Fourth Year has a list of match results for the past several
years that can help you identify a GW grad at a particular program if we have
one).
○ Read every scrap of literature about the program (websites, social media
accounts etc.).
○ Follow residency social media accounts. Many have Twitter, Instagram or
Facebook presences. This can be a venue for potential interactions with the
program and a source of information about upcoming events, and for you to get
a glimpse of the culture. Importantly, make sure your social media profiles are
accurate reflections of you that you are comfortable sharing.
○ Prepare a series of questions to ask during your interviews (it’s very poor form to
get to the end of an interview and have no questions for the interviewer!). Ask
faculty about big program issues (curriculum, conferences, research, teaching,
Guide to the Transition to Advanced Clinical Practice | 35
special opportunities, program/institution stability, where previous residents
completing the program have gone for practice/fellowships, etc.). Ask residents
about the nitty-gritty details (schedule, perks, morale, ancillary support, teaching
quality of the faculty, life outside the residency) and the big issues (see my
proposed residency checklist at the end of this summary for examples of things
to inquire about)
○ Be prepared to present/discuss an interesting clinical case (it’s best to pick one in
the area of your specialty interest)
○ Be prepared to answer the commonly encountered questions (see the list of
common questions prepared by graduating students from prior years, attached)
○ Cancel or reschedule interviews well in advance if you can’t make it. Even if you
don’t want to go to that program, one of your GW classmates or a future grad
may want to, so don’t sour the program on GW..
The Interview Day:
● Get there early! Go to the bathroom. Eat something so you don’t pass out. Avoid too
much coffee/soda/water in case you have a long interview or few breaks! → Have a
snack and water on hand in case you need it. Use the bathroom first. Have a good
breakfast beforehand.
● Look sharp. Dress conservatively. Bring some casual clothes as well in case there are
opportunities to meet with residents or faculty after hours.--> Wear pants, dress
professionally from head to toe.
● Treat everybody from the janitor to the program director as if they are your best friend.
Assume that everybody could have impact on your ranking at the program. Don’t ever
get on the wrong side of an interview coordinator, program administrator, or program
director; it’s the kiss of death to your application. -->Same with IT/coordinators on your
zoom, etc. Be kind and respectful in ALL interactions.
● Take any/every opportunity to meet with residents, tour the facility, go to conferences,
etc. Don’t schedule your arrivals and departures so tightly that you have to bail out on
important parts of the interview day. You may miss important details and you may give
the impression of disinterest in the program. -->Attend any get-to-know-you events as
your schedule allows. Do not let them interfere with other formal interview days
though.
Guide to the Transition to Advanced Clinical Practice | 36

Guide to the Transition to Advanced Clinical Practice | 37
● Consider taking your spouse/significant other if living conditions/geography are
important issues. Leave your parents at home, please, you’re a grown-up now. → For
places/programs you are really interested in, consider taking a safe drive/trip with your
S.O. to check it out separately.
● Be prepared to ask about these key issues:
○ What was the result of the program’s last RRC (Residency Review Committee)
site visit? Was the program fully accredited, cited for any deficiencies, or put on
probation (they must tell you this information if you ask)?
○ How is the academic medical center/hospital doing? Is it financially sound? If
not, what is being done about it? Are key faculty leaving/coming?
○ How is the program adjusting to changes in resident work hours? How is this
working out?
○ Talk to other students who are interviewing with you. What do they know about
the program/other programs that you may interview at? The grapevine can be
very valuable.
○ If you are unfamiliar with the town/city, you may want to plan some extra time
to tour about and see if you like it.
After the Interview:
● Consider writing thank you messages to interviewers, as long as the program does not
have post-interview communication prohibitions. If you really like the program, tell
them. You needn’t/shouldn’t commit yourself to any particular ranking of a program,
although it’s fair to say “I plan to rank your program highly.”
● Get names of residents/and or faculty who may be willing to talk to you later if you think
of other questions or want a second opportunity to talk about the program.
● If you really want to check up on a program again, you may be able to arrange a ‘second
look’ visit. These are absolutely not required. That is, you shouldn’t feel compelled to
return to a program just to convince them that you are interested. In fact, many
programs will actively discourage ‘second looks’. Only spend the time and effort to go
back if you think it will really help you make a decision.
● Don’t ever believe anything that a program director tells you (this is advice from a
program director!)! Programs are not supposed to tell you specifics about where they
plan to rank you, though they too can say things like, “We plan to rank you highly.”
They will tell you all kinds of things; just nod and smile and thank them. If they pressure
you inappropriately about how you are going to rank them, just tell them whatever you

Guide to the Transition to Advanced Clinical Practice | 38
are comfortable with. Remember, it is to your advantage to rank programs in your
exact order of preference, regardless of how likely you think it is that you will get into
any individual program. Likewise, it is to the program director’s advantage to rank all
applicants in the exact order of their preference for you. The match guarantees you
that you will not match to a lower program on your list, unless all positions at higher
programs are already filled by higher ranked candidates. Therefore, the length of your
match list has no influence on where you match. In fact, statistical analyses prove only
one thing: the shorter your match list, the more likely you are to go unmatched!
General Interviewing Tips
The length and format of residency interviews varies significantly across specialties and
individual faculty interviewers.
Here are some general tips to prepare:
●
Think about what are your key strengths/takeaways (2-4) that you want to make sure
your interviewer knows about you by the end of the interview. Use these to guide your
approach to the interview. You will want to make sure you touch upon these in your
opening answer to “Tell me about yourself” or similar.
●
Some interviews ONLY involve having you ask questions to the interviewer about the
program, so make sure you have specific questions in mind for every interview.
●
Behavioral interview questions are becoming popular in many specialties. These are
questions that have you explain how you handled various scenarios that reflect
important competencies in medicine: challenges, conflicts, ethical dilemmas,
professionalism, interpersonal communication, etc.
One approach to answering behavioral interview questions
1.
Situation: Describe the situation in detail
2.
Action: What action did you take?
3.
Result: What was the result?
Examples:
○
Tell me about a time you worked effectively under pressure.
○
Tell me about a stressful situation you experienced in medical school and how
you handled it.
○
Tell me about a time you made a mistake and had to tell a resident or attending.
○
Tell me how you would you deal with a resident who wasn’t doing his share of
the work.

Guide to the Transition to Advanced Clinical Practice | 39
○
Tell me about a time that you had a conflict with a team member and how you
handled it.
○
Tell me about a time when you were disappointed in your performance.
○
Tell me about a time you had to build a relationship with someone you didn’t like.
○
Tell me about a difficult decision you’ve made in the last year.
○
Tell me about a time you when you tried to accomplish something and failed.
●
It’s helpful to have a couple of patient cases in mind - an interesting patient that you took
care of and one where something went wrong. Be able to concisely tell the case and
what you learned from it.
●
Tailor your questions and answers to the program you are interviewing with. Be sure to
communicate why you would strongly consider going to their program. Include if you
have any specific ties to the location/city, etc.
●
Be yourself! You want to match at a program that is a great fit. Be honest and authentic
about your passions and goals.
Sample Interview Questions
(*some of these are the standard questions, others are more strange and interesting questions
that students were asked, we thought it would be best to be comprehensive, but questions are
the common, straight forward ones)
Common Interview Questions:
1. Do you have any questions for us? – Be aware that in some interviews this will be the only
question you are asked so be prepared!
2. Why do you want to be a ?
3. What are your strengths and weaknesses?
4. How do you describe yourself?
5. How would your friends describe you?
6. Where do you see yourself in 15 years?
7. Why are you interested in coming to this particular program?
8. Why are you interested in coming to this particular city? Are you willing to move to this city
for the length of your residency?
9. Tell me about yourself.
10. What are your interests outside of medicine?
11. Tell me about the last book you read.
12. What research have you done while in medical school?
13. For more competitive specialties – What will you do if you don’t match?
14. Tell me about an interesting patient you saw.
Guide to the Transition to Advanced Clinical Practice | 40
15. Give me an example of a situation in which you had to be a good leader.
16. Who is your role model?
17. If you could not be a doctor, what would you be?
18. What other programs are you looking at? What are their strengths and weaknesses?
19. Where did you do an away rotation? Why did you rotate there? What service were you on?
20. If you took any time off between college and medical school, what did you do with that
time?
21. What is the most risky thing you have ever done?
22. What can you bring to this program?
23. Describe a situation in which you failed.
24. Describe a situation in which you made a mistake. What did you do to remedy the
situation?
25. If you were trapped on an island and could only bring three things, what would they be?
26. What are your feelings on the Iraq war?
27. Tell me about the last movie you saw.
28. Please explain the criticism written about you in your dean’s letter.
29. Of all the competitive applicants we are interviewing, what about you should make me
want to rank you at
the top of our list?
30. Where do you see this specialty going in the next 10 years?
31. Tell me about a conflict you had in medical school and how you resolved it.
32. Specifically for peds – If you are in clinic and you see a mother spank her child, what would
you do?
33. Who are you? Where have you been? Where do you see yourself in the future?
34. If you could not do the specialty you are applying for, which other specialty would you
choose?
35. What does your family think of you applying here?
36. Tell me about a time that you took on a leadership role.
37. What will you specifically add to the intern class at this program?
38. Tell me about a time when you failed and how did you handle it.
39. Tell me about a time when you saw someone do something you felt was wrong, and how
did you handle it.
40. Make me laugh (funny story, joke, anything).
41. Tell me the characteristics you have liked and not liked in other programs.
42. Where did you do (virtual) away rotations? What did you like/not like about them? How do
those programs compare to ours?
43. If you were a residency program director and could design a program from scratch, what
would it consist of?
Guide to the Transition to Advanced Clinical Practice | 41
44. Why would you want to live in this city?
45. Why don’t you want to stay at your home institution for residency?
“Interesting” interview questions
1.
Tell me about the state where I am from...
2.
What is your favorite movie and why?
3.
Be prepared for personal, non-medicine questions i.e. favorite or most recent books read,
movies seen, hobbies, etc...
4.
"Tell me about an ethical dilemma you had involving patient care.
5.
Tell me about a case that challenged you. How did you handle it and what did you learn from
that experience.
6.
Tell me about your most interesting patient.
7.
"Give a case presentation in 5 minutes in the form of a discharge summary. (Scripps Mercy in
San Diego, Internal Medicine)
8.
I was asked to teach my interviewer something I had learned from research I had done at
Johns Hopkins.
9.
if you were a car that represented you what would it be?
10.
Tell me a joke
11.
What do you think about universal health care vs. fee for service?
12.
Can religion and science coexist?"
13.
Interviews for Internal Medicine are generally relaxed and conversational. Programs want to
get to know you and see how personable you are. Although I did not get any awful questions,
there were some trickier ones:
a. Tell me where else you applied (and they will often not settle for vague
answers)?
b. Why should we choose you?
c. Why are you interested in our program?
d. Tell me where you see yourself in 10 years.
e. Tell me about your research.
f. What do you think will be most challenging for you in residency?
g. Tell me about a time you failed.
h. Tell me about an interesting case you encountered.
i. What have you found most difficult about medical school?
j. What are you most proud of?
k. Who is your role model?
l. Why do you want to enter this field?
14.
Most programs want to know any reasons you would not consider coming to their program.
15.
. I was asked on one interview what three people I would want to go to lunch with (historical
or current)
16.
I was asked to reveal one interesting fact about myself on my NYU medicine interview in
front of the entire room of applicants.
17.
Describe an ethical situation that you encountered as a medical student while on the wards.
18.
Tell me about a time that you made a medical error. What did you do to fix the situation?
19.
Always have an interesting patient case in mind to refer to if needed. The majority of
interviews are just a meet and greet, but they occasionally ask for lessons learned from
patients.
20.
Are you the first person in your family to go to college? (When my grandfathers went to law
school at Yale...)
21.
Tell me about Mississippi.
22.
What is your favorite movie and why?
23.
When was the last time that you laughed out loud?
24.
If you were an organ system, what would you be and why?
25.
If you were a tree, what type would you be and why?
26.
Did you enjoy high school?
27.
Who is Thelodius Monk? He is a famous pianist.
28.
When was first xray?
29.
What are 3 top medical advances?
30.
Please present a case in discharge summary format in 5 minutes or less. Then asked
questions on case.
31.
Name a situation in which you disagreed with a colleague/superior and how you dealt with
it (got asked this probably 10 times..)
32.
What kind of learner are you?
33.
How do you deal with situations in which you don't know the solution?
34.
How is the interview trail going? (seems easy, but it's all too easy to just blurt out ""good""
and then just stare blankly... use this chance to drop a quick hint into what kinds of things you
like/want/noticed in a program)
35.
Why would you come here as opposed to some other neighboring programs?
36.
Can you apply the general research concept used in your other research project to a specific
research topic within radiology?
37.
If you could be a car, what would it be? What would your plate read?
38.
What is the overall meaning of your life? What is your grand goal in life?
39.
What values did your family raise you with?
Guide to the Transition to Advanced Clinical Practice | 42

Guide to the Transition to Advanced Clinical Practice | 43
Appendix C: Residency Program Evaluation
Suggested program evaluation form that you can use to keep track of key information regarding residency programs
at which you interview. Feel free to add your own personal criteria as you see fit.
Program name
Type of Program: university university-affiliated community
Number of Residents:
Quality of Residents (circle one): outstanding|bright|solid|questionable
Resident Morale (circle one): very happy|happy|satisfied|unhappy
Quality of Teaching (circle one): outstanding|very good|good|poor
Quality of Faculty (circle one): outstanding|very good|good|poor
Quality of Resident Report (circle one): outstanding|very good|good|poor|NA
Quality of Teaching Conferences (circle one): outstanding|very good|good|poor
Quality of Library Facilities (circle one): outstanding|very good|good|poor
Quality of Informatics Resources (circle one): outstanding|very good|good|poor
Inpatient Experiences:
Number of months of inpatient experience each year
Frequency of call
Number of patients admitted per call day
Size of teams
Quality of supervision
Availability of “cutting edge” technology
Variety of patient conditions
Opportunity for ;earning/performing procedures
Quality of facilities
Quality of conferences/morning/intern report
Quality of ancillary services (phlebotomy, iv team, etc.)
Quality of social services/discharge planning
Quality of call rooms
Availability of food
Ambulatory Experiences:
Number of months of ambulatory experiences or frequency of clinic practice
Number of patient encounters per session
Quality of facilities
Quality of supervision/teaching
Quality of ancillary services/social services
Variety of patients/conditions
Opportunity to learn/perform office procedures
Quality of teaching conferences
Continuity of care
Special Educational Opportunities:

Guide to the Transition to Advanced Clinical Practice | 44
Number of elective opportunities
Variety of elective opportunities
Availability of research opportunities
Availability of teaching opportunities
Availability of community service opportunities
Availability of special skills training (teaching, research, practice management, etc.)
Residency Outcomes:
Where do residents go (write down percentage): private practice % fellowship % research %
teaching %
How many residents who start program finish program:
How easy is it for graduates to get jobs (write numbers): local area anywhere
Quality of local job opportunities (circle one): outstanding|very good|good|poor
Miscellaneous:
Quality of living conditions (circle one): within reasonable|commute
Expense of living conditions (circle one): within reasonable|commute
Quality of commute to work (circle one): car|public transportation|walking
Extracurricular opportunities:
Cultural?
Sports?
Outdoors?
GUT CHECK (circle one)
Outstanding Program|Great Program|Good Program|Satisfactory Program|Would rather not match
Guide to the Transition to Advanced Clinical Practice | 45
Appendix D: Tips for Career Selection during Year III
Overview:
One of the most important tasks of third year is to begin the process of choosing a specialty. Although many of you
came to medical school with an idea of what sort of physician you would like to be, studies show that three-quarters
of you will ultimately pick a different specialty by the time you reach your senior year. Firming up your original ideas
or finding a new specialty that perhaps you weren’t considering before are processes that occur most commonly
during the third year and the early part of fourth year.
Don’t leave your specialty choice decision, which will determine your activities and career satisfaction for the next
40 years, to serendipity or chance. Unless you carefully assess all the options beginning on day one of your third
year, you may arrive at the fall of your senior year without a good feeling for your career choice or, almost as bad, a
career selection based on incomplete and misleading information and perceptions! Be vigilant, and utilize the “tips”
below as you work on this critical decision.
Tips for Career Selection:
Enter each clerkship with an open mind. Try to leave your preconceptions behind (they may be inaccurate!).
Enter each clerkship as if it might be the career for you. Imagine yourself practicing in that specialty field during
the time that you are on the clerkship.
Try not to be over-influenced by “positive” or “negative” experiences with individual faculty members or
residents. Focus on the intellectual content of the specialty, the types of patients, the sorts of activities, and the
“life” of the attending physicians. Are these the sorts of things that you like?
Remember, attending physicians, particularly those at an academic medical center, may have careers that differ
substantially from physicians in the community. Try to get a feel for both settings. Most clerkships will expose
you to both academic medicine and community medicine. Pay attention!
Remember, you will only be a resident for a few years. It’s generally not a good idea to be too heavily influenced
by your observations of residency. Yes, you have to make it through a residency, but that is usually only a
relatively brief period compared to the rest of your medical career! Even the “toughest” residencies are “fun” if
you really love the specialty you are training in!
Keep track of your perceptions during the year. Use the Careers in Medicine website to track your ideas and
investigate specialties throughout the year (aamc.org/students/cim)
There are a number of “smaller” specialties that you may not directly experience during your third year (for
instance, some surgical specialties, anesthesiology, emergency medicine, radiology, etc.). However, you will be
spending a great deal of time in the emergency room, the operating room, radiology, and pathology. Pay
attention to what is going on. Observe the attendings and residents in these fields. If your patients go to
specialty clinics for referrals or are seen by other specialists during a hospital stay, go observe what happens
when they are evaluated or treated by these specialists. There are literally hundreds of opportunities to see other
fields during your third year if you just pay attention and take advantage of them when they arise.
Talk to everybody you meet about their careers. What do they do? How do they like it?
What are the strengths and weaknesses of the career? What are the career opportunities like? How is the job
market? Don’t be shy!

Guide to the Transition to Advanced Clinical Practice | 46
Table 14 A
APPENDIX E
Table 14
Tables 14A and 14B present data on applicants who ranked each specialty as their only choice in the 2022 Match.
Table 14A, reflects outcomes for U.S. MD and DO seniors, and the same categories are presented in Table
14B for
U.S. IMGs and non-U.S. IMGs. Prior to 2012, Table 14 and Figure 6 reported Match results by specialty groups
that included the combined specialties. In this report, results are aggregated by specialty instead of specialty group.
Preliminary positions are reported separately.
Internal Medicine, Family Medicine, and Pediatrics had large numbers of matched U.S. MD seniors and DO
seniors. Overall, 3,038 (61.8 percent) of matched U.S. DO seniors who ranked only one specialty (n=4,914)
matched to a primary care specialty compared to 6,437 (42.6 percent) of matched U.S. MD seniors who
ranked only one specialty(n=15,123). In contrast, 75.4 percent (1,368 of 1,815) matched U.S. citizen IMGs
who ranked only one specialty matched in primary care along with 79.1 percent (2,468 of 3,119) of non-U.S.
citizen IMGs.
As seen in Figure 6, higher proportions of unmatched U.S. MD seniors and DO seniors have been observed in
traditionally competitive specialties like Orthopedic Surgery, Neurological Surgery, Plastic Surgery,
Otolaryngology, Dermatology, and General Surgery.
Match Results for U.S. MD Seniors and U.S. DO Seniors ApplicantsWho
Ranked Each Specialty as Their Only Choice, 2022
Matched Unmatched Total
Percent
Matched
Percent
Unmatched
Specialty
MD
DO
MD DO
MD DO
MD DO
MD DO
Anesthesiology
901
135
53
40
954
175
6.0
2.7
5.6
22.9
Child Neurology
77
12
0
0
77
12
0.5
0.2
0.0
0.0
Dermatology
106
10
27
4
133
14
0.7
0.2
20.3
28.6
Emergency Medicine
1,454
611
16
19
1,470
630
9.6
12.4
1.1
3.0
Family Medicine
1,386
1,228
23
43
1,409
1,271
9.2
25.0
1.6
3.4
Internal Medicine
3,443
1,305
48
48
3,491
1,353
22.8
26.6
1.4
3.5
Internal Medicine (Prelim)
210
4
4
0
214
4
1.4
0.1
1.9
0.0
Internal Medicine/Emergency Medicine
0
0
0
0
0
0
0.0
0.0
0.0
0.0
Internal Medicine/Pediatrics
242
18
5
0
247
18
1.6
0.4
2.0
0.0
Internal Medicine/Psychiatry
0
0
1
0
1
0
0.0
0.0
100.0
0.0
Interventional Radiology
4
0
0
0
4
0
0.0
0.0
0.0
0.0
Neurological Surgery
196
5
44
4
240
9
1.3
0.1
18.3
44.4
Neurology
494
111
7
4
501
115
3.3
2.3
1.4
3.5
Obstetrics and Gynecology
975
179
148
71
1,123
250
6.4
3.6
13.2
28.4
Orthopaedic Surgery
658
91
281
56
939
147
4.4
1.9
29.9
38.1
Osteopathic Neuromusculoskeletal
0
3
0
0
0
3
0.0
0.1
0.0
0.0
Medicine
Otolaryngology
275
7
100
0
375
7
1.8
0.1
26.7
0.0
Pathology-Anatomic and Clinical
210
70
5
5
215
75
1.4
1.4
2.3
6.7
Pediatrics
1,608
505
18
6
1,626
511
10.6
10.3
1.1
1.2
Pediatrics (Prelim)
0
0
0
0
0
0
0.0
0.0
0.0
0.0
Pediatrics/Medical Genetics
3
0
0
0
3
0
0.0
0.0
0.0
0.0
Pediatrics/Psychiatry/Child and Adolescent
0
0
0
0
0
0
0.0
0.0
0.0
0.0
Psychiatry
Physical Medicine and Rehabilitation
180
111
22
26
202
137
1.2
2.3
10.9
19.0
Plastic Surgery
138
0
35
1
173
1
0.9
0.0
20.2
100.0
Psychiatry
1,105
275
78
24
1,183
299
7.3
5.6
6.6
8.0
Radiation Oncology
80
3
1
0
81
3
0.5
0.1
1.2
0.0
Radiology-Diagnostic
444
68
58
21
502
89
2.9
1.4
11.6
23.6
Surgery-General
775
146
114
56
889
202
5.1
3.0
12.8
27.7
Surgery-General (Prelim)
66
7
9
1
75
8
0.4
0.1
12.0
12.5
Thoracic Surgery
0
0
1
0
1
0
0.0
0.0
100.0
0.0

Guide to the Transition to Advanced Clinical Practice | 47
Vascular Surgery
45
0
5
2
50
2
0.3
0.0
10.0
100.0
TOTAL*
15,123 4,914 1,111 439 16,234 5,353
100.0 100.0
6.8 8.2
Note: Specialties with fewer than 20 total positions are not displayed on this table. Transitional Year is excluded.
* The TOTAL row includes all positions in all specialties.
Results and Data 2022 Main Residency Match®
35

Results and Data 2022 Main Residency Match®
Table 14 B
Match Results for U.S. IMG and Non-U.S. IMG ApplicantsWho
Ranked Each Specialty as Their Only Choice, 2022
Percent Percent
Matched Unmatched Total Matched Unmatched
Specialty
Anesthesiology
35
39
42
57
77
96
1.9
1.3
54.5
59.4
Child Neurology
5
7
3
7
8
14
0.3
0.2
37.5
50.0
Dermatology
7
7
10
9
17
16
0.4
0.2
58.8
56.3
Emergency Medicine
92
24
21
10
113
34
5.1
0.8
18.6
29.4
Family Medicine
478
265
322
299
800
564
26.3
8.5
40.3
53.0
Internal Medicine
726
1,955
434
1,278
1,160
3,233
40.0
62.7
37.4
39.5
Internal Medicine (Prelim)
4
11
8
14
12
25
0.2
0.4
66.7
56.0
Internal Medicine/Emergency Medicine
0
0
0
0
0
0
0.0
0.0
0.0
0.0
Internal Medicine/Pediatrics
1
2
4
4
5
6
0.1
0.1
80.0
66.7
Internal Medicine/Psychiatry
0
0
1
1
1
1
0.0
0.0
100.0
100.0
Interventional Radiology
0
0
0
1
0
1
0.0
0.0
0.0
100.0
Neurological Surgery
2
13
4
15
6
28
0.1
0.4
66.7
53.6
Neurology
37
122
28
99
65
221
2.0
3.9
43.1
44.8
Obstetrics and Gynecology
19
18
35
41
54
59
1.0
0.6
64.8
69.5
Orthopaedic Surgery
6
11
13
6
19
17
0.3
0.4
68.4
35.3
Osteopathic Neuromusculoskeletal
1
0
0
0
1
0
0.1
0.0
0.0
0.0
Medicine
Otolaryngology
1
1
1
6
2
7
0.1
0.0
50.0
85.7
Pathology-Anatomic and Clinical
48
185
52
120
100
305
2.6
5.9
52.0
39.3
Pediatrics
164
248
47
157
211
405
9.0
8.0
22.3
38.8
Pediatrics (Prelim)
0
0
0
0
0
0
0.0
0.0
0.0
0.0
Pediatrics/Medical Genetics
0
1
0
1
0
2
0.0
0.0
0.0
50.0
Pediatrics/Psychiatry/Child and Adolescent
0
0
0
0
0
0
0.0
0.0
0.0
0.0
Psychiatry
Physical Medicine and Rehabilitation
5
6
13
10
18
16
0.3
0.2
72.2
62.5
Plastic Surgery
2
3
4
3
6
6
0.1
0.1
66.7
50.0
Psychiatry
112
101
133
122
245
223
6.2
3.2
54.3
54.7
Radiation Oncology
7
9
2
7
9
16
0.4
0.3
22.2
43.8
Radiology-Diagnostic
13
24
17
31
30
55
0.7
0.8
56.7
56.4
Surgery-General
33
32
63
78
96
110
1.8
1.0
65.6
70.9
Surgery-General (Prelim)
5
28
7
38
12
66
0.3
0.9
58.3
57.6
Thoracic Surgery
0
1
0
3
0
4
0.0
0.0
0.0
75.0
Vascular Surgery
0
1
0
4
0
5
0.0
0.0
0.0
80.0
TOTAL*
1,815 3,119 1,302 2,451 3,117 5,570
100.0 100.0
41.8 44.0
Note: Specialties with fewer than 20 total positions are not displayed on this table. Transitional Year is excluded.
* The TOTAL row includes all positions in all specialties.
U.S.IMG IM
U.S.
IMG
IM
U.S.
IMG IM
U.S. IMG IMG
U.S. IMG IMG
G
G
G

Results and Data 2022 Main Residency Match®
0.0%
Percentages of Unmatched MD Seniors and DO Seniors Who
Ranked Each Specialty as Their Only Choice, 2022
Orthopaedic Surgery
29.9%
38.1%
Otolaryngology
Dermatology
Plastic Surgery
Neurological Surgery
Transitional Year
26.7%
0.0%
20.3%
28.6%
20.2%
18.3%
14.3%
44.4%
44.4%
100.0%
Obstetrics and Gynecology
S
urgery-
G
enera
l
Surgery-General (Prelim)
13.
2%
12.8%
12.0%
12.5%
28.4%
27.7%
Radiology-Diagnostic
Physical Medicine and Rehabilitation
Vascular Surgery
Psychiatry
11.6%
23.6%
10.9%
19.0%
10.0%
6.6%
8.0%
100.0%
Anesthesiology
Pathology-Anatomic and Clinical
Internal Medicine/Pediatrics
Internal Medicine (Prelim)
Family Medicine
Neurology
Internal Medicine
Radiation Oncology
Emergency Medicine
Pediatrics
Child Neurology
5.6%
2.3%
6.7%
2.0%
0.0%
1.9%
1.6%
3.4%
1.4%
3.5%
1.4%
3.5%
1.2%
0.0%
1.1%
3.0%
1.1%
1.2%
0.0%
22.9%
Figure 6

Results and Data 2021 Main Residency Match®
50
0.0%
0.0% 20.0%
40.0%
60.0%
80.0%
100.0%
Unmatched MD Seniors Unmatched DO Seniors
Note: Specialties with fewer than 20 matched applicants are excluded from this figure. Transitional Year is excluded.
Table 14
Guide to the Transition to Advanced Clinical Practice | 51
Appendix F: Writing a Curriculum Vitae
Writing a Curriculum Vitae (CV)
The first of many supporting documents you will want for the residency application process is a curriculum vitae
(CV). A CV is concise summary of relevant information about your background and accomplishments, particularly
relating to your academic and work experience. You will use your CV throughout your career to communicate your
skills and qualifications. It will help potential employers know whether you would be a suitable candidate for a job,
including your job as a resident physician.
In the residency application process, you will you use your CV to complete ERAS, you will provide it to faculty
members who will write your letters of recommendation, and your advisory deans will review it to help write your
Medical School Performance Evaluation (MSPE or “Dean’s Letter”).
CV Components
When considering information to include in your CV, ask yourself:
Does this help? Will this piece of information help select me for a residency interview?
If I were reading this for the first time and without knowledge of myself as an applicant, would this
information be useful?
If you answer “no” to either of these questions, leave the information out. If you’re unsure, consult your advisor
and/or a specialty contact for advice. The basic categories that your CV should contain are listed below. Not all of
these elements may be relevant to you, so choose what will work best for your background and experience.
Formatting and Production
1. You want your CV to have a clean, distinctive appearance that attracts attention. The final product should
be well organized, look professional, and be easy to read.
2. Keep margins at 0.5 - 1 inches.
3. One page is standard length at this point in your career, but don’t reduce the font size, change your margins,
or leave important info out just to crowd it onto one page.
4. 12-point font is preferable, but 11-point is acceptable.
5. Stick with one font, or two similar fonts (one for headings, the other for everything else) - use only
conservative, common fonts.
6. Headings should be consistent in style, size, and formatting.
7. Use bold, italics, capitalization, and bullets to organize your CV - but use sparingly.
8. Check text for misspellings and poor grammar - have someone help you proofread.
9. Keep sentences short and succinct while using active verbs and vivid, precise language.
Contact and Personal Information
Give your formal legal name (no nicknames) and your complete and current contact information. Make sure
you can be reached easily at the address, email and telephone number that you list. You can include other
personal information such as birth date, marital status, names/ages of children but these are optional. While
federal law prohibits employers from discriminating on the basis of age, sex, religion, national origin and
disability status, providing personal information may invite bias so it is up to you whether or not you choose to
provide it. You may elect to include it if you feel it is pertinent to your candidacy for the position.
Education
List all colleges/universities you have attended with the most recent first. Include name and location of
institution, degree sought or completed, and the dates of attendance, including dates of expected completion if
in progress, and major/minor field of study. Include medical school, graduate and undergraduate education. If
you do not have an Honors section on your CV, you may include that information here. If you completed a
Guide to the Transition to Advanced Clinical Practice | 52
thesis or dissertation as part of one of your degree programs, you may wish to add this distinction along with
the title of the paper, particularly if it is relevant to health care or science. As you move forward in your
professional life, you will add further achievements including postgraduate training (residencies and fellowships),
academic appointments, and certification and licensure. No high school information, please.
Honors and Awards
Include any awards and/or scholarships received during medical school (election to AOA, biochemistry prize,
etc.) If you did well in medical school or on the boards, list your honors and board scores. Include only the
most important awards and scholarships from undergraduate or other programs. If you have numerous items,
you may want to separate them into subsections: undergraduate and medical school. Keep in mind how
relevant and useful each item will be, and cut any that may not be valued by the person reading your CV.
Work Experience
List your work experience in reverse chronological order. List all major or medically related work experiences.
Include position title, name of employer, location, and dates. For medically related work, add a brief description
of your responsibilities, achievements, and competencies gained. Be specific, skill-focused and relevant. Include
volunteer experience while in medical school and any leadership experiences. If there are gaps of time in your
history, make sure to include ANY work experience, medical or non-medical, which accounts for your time out
of school (e.g. time between undergraduate studies and medical school).
Research
List research projects you have worked on. For each entry, include a sentence or title describing research.
Include mentor (including professional title), institution, department, and dates. Include your title, if applicable;
e.g., research assistant, fellow. List skills you used/learned.
Professional Memberships
List any professional organizations of which you are a member (dates optional). Include any leadership positions
you may have held. This section may be combined or redefined to include student organization involvement.
Extracurricular Activities
Include the most important long-term activities you were involved in during medical school, including
committee work, community service projects, and student organization involvement with dates. Include
activities from before medical school only if they are extraordinary or applicable to health care.
Publications
Include all published articles you’ve authored. If an article has been accepted for publication but not yet
published, use the notation “in press” instead of year of publication. Use medical bibliographic reference style
and be consistent throughout your CV.
Presentations
Include any research, professional, or poster presentations conducted at conferences, lectures, symposiums,
specialty association meetings, etc. List the title of the presentation, authors, audience, and any other relevant
details. This section may be easily combined with publications to create a single, more attractive section.
Hobbies and Outside Interests
Include a list of your outside interests or extracurricular activities. You may be surprised at how often you will
be asked about these items - interviewers frequently use them as a means to keep an interview conversational so
be prepared to talk about any hobby or interest that you put here. This section is optional and should be brief.
See Suggested Template for CV (Appendix G)
Guide to the Transition to Advanced Clinical Practice | 53
Appendix G: Sample Curriculum Vitae
FULL LEGAL NAME
Phone Number
Email address
Current Address
Permanent Address
EDUCATION
Name of Medical School
City, State
M.D.
2015-2019 (Anticipated)
Name of Graduate School
City,
State
Degree Type
Dates of attendance
Name of Undergraduate School
City,
State
Degree Type
Dates of attendance
EXPERIENCE
TALKS:Teaching and Learning Knowledge and Skills Senior Elective July 2018- Present
•
Serve as an instructor for first year medical students in Physical Diagnosis section
•
Prepare lessons for six different Physical Diagnosis classes, each focusing on different parts of the physical exam,
with an emphasis on clinical relevance and skill development.
•
Provide students with regular feedback regarding their performance in the physical diagnosis class in a manner
that mimics the feedback they will receive from residents and attending during their clinical years.
•
Participate in workshops on adult learning theory, evaluation of student performance, providing feedback, and
effective teaching techniques, with special focus on teaching clinical skills.
•
Evaluate students during their performance on standardized patient exams.
The HEALing Clinic, George Washington University’s Student Run Clinic Oct 2015-Present
Training Chair Jan 2016-Dec 2016
•
Developed and implement a novel biannual training conference for all HEALing Clinic volunteers to teach history
taking, physical exam, and cultural competency skills.
•
Instructed a course for preclinical students on performing a well woman examine, including pelvic exam, Pap
test, and breast exam.
•
Organized and ran monthly orientation sessions for the new volunteers serving at the HEALing Clinic in the
upcoming month.
Co-Director Jan 2016-Dec 2016
•
Managed a Steering Committee of 30 members who oversaw all aspects of clinic management, operations,
fundraising, research, and recruitment.
•
Responsible for strategic planning and development of educational and clinical programs.
•
Presented at alumni and faculty meetings to build support, secure funding, and recruit volunteer attending
physicians.
•
Attended a national conference for Student Run Clinics to study various clinic models, network with other clinic
directors, and explore areas for future research and development.
Guide to the Transition to Advanced Clinical Practice | 54
Clinic Manager July 2018-present
• Oversee clinic flow and all activities of the weekly student run clinic in Ward 8, Washington DC’s most
• underserved ward.
• Coordinate the schedules of medical, physician assistant, and public health students with attending physicians to ensure
optimal patient service staffing and educational support.
• Supervise all student volunteers each week in an effort to maximize efficient patient management.
• Facilitate weekly teaching and debrief session after each clinic night.
Medical Education Scholarly Concentration Nov 2015-present
• Explored the topics of teaching methods, medical education research, and adult learning theory through a series of
interactive classes.
• Learned and applied methods for teaching clinical skills through a series of workshops and projects.
• Will mentor first year medical students and teach physical exam skills in the physical diagnosis course.
• Will complete an in-depth research project in the field of Medical Education.
Curriculum Committee Jan 2016 – present
•
Selected by the Student Council to be a member of GW’s curriculum development committee, which is
responsible for analyzing and reconstructing the current curriculum to ensure that LCME accreditation
standards are met and surpassed.
•
Personally responsible for methodically gathering objective data from the third year medical student class on
their attitudes towards the current curriculum and class structure.
•
Will compile and analyze the data in order to build a new curriculum that will meet student’s goals as well as
national educational standards.
Office of Admissions Sept 2015-Dec 2017
Prospective Medical Student Interviewer
• Interviewed 4-5 prospective medical students each month regarding their experience, values, goals, and commitment to
the field of medicine.
• Wrote detailed reports on all candidates outlining their strengths and weaknesses, as well as their potential contributions
to the George Washington medical community.
• Advised prospective students regarding life as a GW medical student, the benefits of learning the practice of medicine in
Washington DC, and the application process.
GW Community Service Day August 2016
Student Chair
• Nominated and selected by classmates to serve as student chair for GW’s annual Community Service Day, when the entire
school of medicine and health sciences travel to various sites in Washington, DC to volunteer.
• Trained and transported an interdisciplinary group of 10 students and faculty members to a food bank at Bread for the
City in northeast DC.
• Educated fellow students on the importance of community involvement.
Anatomy Laboratory Curriculum Development June 2016-July 2016
•
Researched interactive methods of teaching Gross Anatomy in an effort to better understand what motivates
students to learn and allows them to understand the relevance of anatomy to clinical medicine.
•
Developed a series of cases in which students explore anatomy in the cadaver lab by identifying the landmarks
and functionality of various anatomical structures and performing the physical exam maneuvers relevant to
realistic clinical scenarios.
Guide to the Transition to Advanced Clinical Practice | 55
Omni Eye Specialists, Washington, DC February 2013- July 2014
Patient Services Manager
•
Managed the patient services department and acted as team leader to all reception, medical
records, and insurance personnel.
•
Coordinated office visits and consultations based on individual patient needs, insurance status
and physician availability.
•
Utilized an extensive working knowledge of various insurance plans to assist patients and verify
benefit information for billing purposes.
•
Maintained positive relationships with referring doctors’ offices in an effort to increase new patient
volumes.
RESEARCH
Department of Medicine, George Washington University June 2016-Sept 2017
“Participation in Student-Run Free Clinics and Empathy in Medical Students”
Mentor: Dr. W. Scott Schroth
•
Compared students who participated in GW’s HEALing clinic with students who applied but were not selected in
the areas of empathy, professionalism, and commitment to working with underserved populations using a series
of validated scales as well as student’s grades.
•
Will analyze the data and submit for publication to various medical education journals in the upcoming months.
HONORS
Gold Humanism Honor Society Member 2018
•
Nominated by peers and selected by faculty to be a member of this prestigious society which honors students
and faculty who demonstrate exemplary humanistic qualities of patient care.

Guide to the Transition to Advanced Clinical Practice | 56
Appendix H
CLASS OF 2023 RESIDENCY MATCH LIST
Last Name
First Name
Institution Name
Program Name
Duval
Margaret
NYP Hosp-Weill Cornell Med Ctr-NY
Anesthesiology
Ejiofor
Beverly
Brown Univ/Rhode Island Hosp
Anesthesiology
Galvin
Meredith
B I Deaconess Med Ctr-MA
Anesthesiology
Giang
Brian
Cedars-Sinai Med Ctr-CA
Anesthesiology
Gupta
Puneet
George Washington Univ-DC
Anesthesiology
Mallon
John
U Maryland Med Ctr
Anesthesiology
Marcinkowski
Bridget
Brigham & Womens Hosp-MA
Anesthesiology
Sherwood
Ian
Penn State Hershey Med Ctr-PA
Anesthesiology
Stewart
Caitlyn
U Florida COM-Shands Hosp
Anesthesiology
Dick
Alexander
Childrens Hosp-Philadelphia-PA
Child Neurology
McNett
Sienna
TJU/Nemours Childrens Health-PA
Child Neurology
Ali
Rowanne
Emory Univ SOM-GA
Dermatology
Nussbaum
Dillon
George Washington Univ-DC
Dermatology
Omar
Deega
UC San Francisco-CA
Dermatology
Parthasarathy
Varsha
Johns Hopkins Hosp-MD
Dermatology
Yeroushalmi
Samuel
NYP Hosp-Weill Cornell Med Ctr-NY
Dermatology
Authelet
Kayla
Alameda Health Sys-Highland Hosp-CA
Emergency Medicine
Barton
Jordan
San Antonio Military Medical Center-Army
Emergency Medicine
Braswell
Morgan
U Wisconsin Hospital and Clinics
Emergency Medicine
Dave
Pooja
Albert Einstein Medical Center-PA
Emergency Medicine
Klein
Andrea
Carilion Clinic- Virginia Tech Carilion SOM
Emergency Medicine
Metri
Samer
Kaiser Permanente-San Diego-CA
Emergency Medicine
Newton
Sophia
U Cincinnati Med Ctr-OH
Emergency Medicine
Patella
Margaret
Brown Univ/Rhode Island Hosp
Emergency Medicine
Rao
Krithika
UCLA Med Ctr-CA
Emergency Medicine
Sjaarda
Alexandra
Albert Einstein Med Ctr-PA
Emergency Medicine
Sweetser
Peter
George Washington Univ-DC
Emergency Medicine
Thirunagaru
Sreenidhi
Thomas Jefferson Univ-PA
Emergency Medicine
Tovar
Matthew
Navy Hospital Portsmouth
Emergency Medicine
Wend
Christopher
Johns Hopkins Hosp-MD
Emergency Medicine
Corrado
Colleen
Camp Lejeune- Navy
Family Medicine
Huh
Jung
VCU-Shenandoah Valley-VA
Family Medicine
Swint
Alysia
Sutter Med Ctr of Santa Rosa-CA
Family Medicine
Weston
Christopher
Eisenhower Army Medical
Family Medicine
Yan
Tong
Grtr Lawrence Fam Hlth Ctr-MA
Family Medicine
Yu
Katherine
Contra Costa Reg Med Ctr-CA
Family Medicine
Arnautovic
Alisa
Emory Univ SOM-GA
General Surgery
Clark
Elizabeth
Carolinas Med Ctr-NC
General Surgery
Doan
Tina
ISMMS Mount Sinai Hospital-NY
General Surgery
Esmailian
Gabriel
Indiana University SOM
General Surgery
Ganguli
Sangrag
Univ of Chicago Med Ctr-IL
General Surgery
Leighton
Nicolas
U Southern California
General Surgery
Zollinger
Benjamin
Inova Fairfax Hospital-VA
General Surgery
Horiuchi
Sakura
Creighton University-AZ
General Surgery/Valleywise

Guide to the Transition to Advanced Clinical Practice | 57
Adams-Mardi
Cyrus
George Washington Univ-DC
Internal Medicine
Attia
Monica
UC Davis Med Ctr-CA
Internal Medicine
Barsoum
Julia
NYU Grossman School Of Medicine-NY
Internal Medicine
Burke
Morgan
U Southern California
Internal Medicine
Cohen
Austin
George Washington Univ-DC
Internal Medicine
Diamond
Ethan
MedStar Georgetown Univ Hosp-DC
Internal Medicine
Dobbs
John
Johns Hopkins Hosp-MD
Internal Medicine
Falk
Zachary
NYP Hosp-Weill Cornell Med Ctr-NY
Internal Medicine
Foltz-Davis
Colin
Tulane Univ SOM-LA
Internal Medicine
Friedman
Nicolette
Univ of Vermont Medical Center
Internal Medicine
Gupta
Vrinda
Johns Hopkins Hosp-MD
Internal Medicine
Hamilton
Colleen
Harbor-UCLA Med Ctr-CA
Internal Medicine
Jaber
Diana
Northwestern McGaw/NMH/VA-IL
Internal Medicine
Kennedy
Charles
U Texas Southwestern Med Sch-Dallas
Internal Medicine
Maddali
Aditya
George Washington Univ-DC
Internal Medicine
Menezes
Shannon
Kaiser Permanente Mid-Atlantic-MD
Internal Medicine
Min
Kyung
Kaiser Permanente-SF-CA
Internal Medicine
Muller
Daniel
U Michigan Hosps-Ann Arbor
Internal Medicine
Naatey
Ahumah
Monica
Case Western/Univ Hosps Cleveland Med Ctr-
OH
Internal Medicine
Ong
Justin
U Southern California
Internal Medicine
Pradhan
Nicholas
Univ of Chicago Med Ctr-IL
Internal Medicine
Rizk Salib
Monika
U Maryland Med Ctr
Internal Medicine
Schwartz
Mollie
Montefiore Med Ctr/Einstein-NY
Internal Medicine
Shancer
Zoe
Duke Univ Med Ctr-NC
Internal Medicine
Srinivasa
Nandan
University of Virginia
Internal Medicine
Surana
Pallavi
Montefiore Med Ctr/Einstein-NY
Internal Medicine
Cho
Kevin
Brown Univ/Rhode Island Hosp
Interventional Radiology
(Integ)
Gutti
Subhash
Rush University Med Ctr-IL
Interventional Radiology
(Integ)
Dazelle
Wayde
Ohio State University Med Ctr
Medicine-Pediatrics
Ali
Rowanne
Sinai Hospital of Baltimore-MD
Medicine-Preliminary
Anderson
Alyssa
St Mary Med Ctr-Long Beach-CA
Medicine-Preliminary
Brown
Lauryn
MedStar Washington Hosp Ctr-DC
Medicine-Preliminary
Calabria
Emily
Morristown Med Ctr-NJ
Medicine-Preliminary
Ejiofor
Beverly
St Vincent Hosp-Worcester-MA
Medicine-Preliminary
Marcinkowski
Bridget
George Washington Univ-DC
Medicine-Preliminary
Mortman
Ryan
MedStar Washington Hosp Ctr-DC
Medicine-Preliminary
Olivares
Philip
Eastern Virginia Med School
Medicine-Preliminary
Omar
Deega
George Washington Univ-DC
Medicine-Preliminary
Parthasarathy
Varsha
MedStar Washington Hosp Ctr-DC
Medicine-Preliminary
Rahimi
Murwarit
George Washington Univ-DC
Medicine-Preliminary
Vaziri
Tina
MedStar Washington Hosp Ctr-DC
Medicine-Preliminary
Yeroushalmi
Samuel
MedStar Washington Hosp Ctr-DC
Medicine-Preliminary
Zarabian
Kimia
Sinai Hospital of Baltimore-MD
Medicine-Preliminary
Thomasian
Julie
George Washington Univ-DC
Medicine-
Preliminary/Ophthalmology
Haag
Alejandro
George Washington Univ-DC
Medicine-Primary
Trivedi
Charmi
Brown Univ/Rhode Island Hosp
Medicine-Primary
Nussbaum
Dillon
George Washington Univ-DC
Med-Prelim/Dermatology

Guide to the Transition to Advanced Clinical Practice | 58
Mishra
Shelly
Sinai Hospital of Baltimore-MD
Med-Prelim/KEI
Kallik
Christina
NYU Grossman School Of Medicine-NY
Med-Prelim/Neurology NYU
Man
McHarg
Matthew
CA Pacific Med Center
Med-Prelim/Ophthalmology
Chalif
Eric
Brigham & Womens Hosp-MA
Neurological Surgery
Kedda
Jayanidhi
George Washington Univ-DC
Neurological Surgery
Hilger
Joseph
Loyola Univ Med Ctr-IL
Neurology
Mandel
Alexandra
U Michigan Hosps-Ann Arbor
Neurology
Movva
Sriya
MedStar Georgetown Univ Hosp-DC
Neurology
Pertsovskaya
Vera
NYP Hosp-Weill Cornell Med Ctr-NY
Neurology
Wannon
Avi
MedStar Georgetown Univ Hosp-DC
Neurology
Weiner
Julia
Case Western/Univ Hosps Cleveland Med Ctr-
OH
Neurology
Kallik
Christina
NYU Grossman School Of Medicine-NY
Neurology/NYU Man
Bryan
Katherine
SUNY Upstate Med University
Obstetrics-Gynecology
Caraballo
Graciela
Stanford Health Care-CA
Obstetrics-Gynecology
Dafilou
Caleb
Montefiore Med Ctr/Einstein-NY
Obstetrics-Gynecology
Diab
Noor
Rutgers-Newark Beth Israel Med Ctr-NJ
Obstetrics-Gynecology
Ebner
Megan
SUNY HSC Brooklyn-NY
Obstetrics-Gynecology
Hasan
Mai
Summa Health/NEOMED-OH
Obstetrics-Gynecology
Keegan
Emma
Pennsylvania Hospital
Obstetrics-Gynecology
Khan
Sophia
St Joseph Hospital SCL Health-CO
Obstetrics-Gynecology
Khosravian
Kiana
Kaiser Permanente-Santa Clara-CA
Obstetrics-Gynecology
Kolodner
Rebecca
UC San Diego Med Ctr-CA
Obstetrics-Gynecology
Mattson
Anna
Kaiser Permanente-Santa Clara-CA
Obstetrics-Gynecology
Neira Gesteira
Andrea
Ochsner Clinic Foundation-LA
Obstetrics-Gynecology
Patel
Akshat
ISMMS Mount Sinai Hospital-NY
Obstetrics-Gynecology
Pelsang
Rachel
Medical College of Georgia
Obstetrics-Gynecology
Rao
Maya
George Washington Univ-DC
Obstetrics-Gynecology
Shwe
Wendy
Montefiore Med Ctr/Einstein-NY
Obstetrics-Gynecology
Wood
Elizabeth
Naval Medical Center San Diego
Obstetrics-Gynecology
Jeong
Go Eun
Georgetown U/Wash Hosp
Ophthalmology
Rosenberg
Sedona
U Virginia
Ophthalmology
Barajas
Juan
Atlanta Med Ctr-GA
Orthopaedic Surgery
Fuller
Samuel
University at Buffalo SOM-NY
Orthopaedic Surgery
Quan
Theodore
George Washington Univ-DC
Orthopaedic Surgery
Shah
Aribah
George Washington Univ-DC
Orthopaedic Surgery
El Shatanofy
Muhammad
U Miami/Jackson Health System-FL
Otolaryngology
Gorelik
Daniel
Methodist Hospital-Houston-TX
Otolaryngology
Youner
Emily
Case Western/Univ Hosps Cleveland Med Ctr-
OH
Otolaryngology
Carlson
David
University of Virginia
Pathology
Jett
David
Duke Univ Med Ctr-NC
Pathology
Ahmed
Bilal
Zucker SOM-Northwell Cohen Childrens-NY
Pediatrics
Anderson
Lauren
Univ of Chicago Med Ctr-IL
Pediatrics
Baldwin
Joshua
SUNY Upstate Med University
Pediatrics
Bamfo
Adwoa
Eastern Virginia Med School
Pediatrics
Bullen
Theresa
UPMC Medical Education-PA
Pediatrics
Dow
Serena
Nationwide Childrens Hosp-OH
Pediatrics
Fimmel
Fiona
Cincinnati Childrens Hosp Med Ctr-OH
Pediatrics

Guide to the Transition to Advanced Clinical Practice | 59
Gutierrez
Gloria
Childrens Hosp-Philadelphia-PA
Pediatrics
Henriques
Jane
Childrens National Med Ctr-DC
Pediatrics
Leon
Andrea
U Miami/Jackson Health System-FL
Pediatrics
Liu
Grace
U Colorado SOM-Denver
Pediatrics
Mijares
Joseph
Childrens National Med Ctr-DC
Pediatrics
Milki
Anthony
NYP Hosp-Columbia Univ Med Ctr-NY
Pediatrics
Reilly
Curran
Childrens Hosp-Philadelphia-PA
Pediatrics
Sallander
Kayla
Walter Reed- Army
Pediatrics
Sankar
Mathavi
Childrens Hosp-Philadelphia-PA
Pediatrics
Schmitt
Sarah
NYU Grossman School Of Medicine-NY
Pediatrics
Shalkevich
Jacob
Phoenix Childrens Hospital-AZ
Pediatrics
Torroella
Kristin
Johns Hopkins Hosp-MD
Pediatrics
Phan
Megan
U Washington Affil Hosps
Pediatrics/Health Equity
Uppal
Prayerna
U Washington Affil Hosps
Pediatrics/Health Equity
Davis
Elisabeth
Childrens National Med Ctr-DC
Pediatrics/LAUnCH
Community Hlth
Ipe
Abraham
Childrens National Med Ctr-DC
Pediatrics/LAUnCH
Community Hlth
Moore
Brenna
UC Irvine Med Ctr-CA
Pediatrics/UCI-CHOC
Emamzadeh
Emily
TJU/Nemours Childrens Health-PA
Pediatrics-PM&R
Broadbent
Geoffrey
Childrens National Med Ctr-DC
Pediatrics-Primary
Eng
Jared
U Washington Affil Hosps
Phys Medicine & Rehab
Jain
Esha
MedStar National Rehab Hosp-DC
Phys Medicine & Rehab
Mortman
Ryan
UPMC Medical Education-PA
Phys Medicine & Rehab
Zarabian
Kimia
U Washington Affil Hosps
Phys Medicine & Rehab
Anderson
Alyssa
VA Greater LA Hlth Sys-CA
Phys Medicine &
Rehab/UCLA
Martinez
Paul
MedStar Georgetown Univ Hosp-DC
Plastic Surgery (Integrated)
Schwartz
Rachel
Carilion Clinic-Virginia Tech Carilion SOM
Plastic Surgery (Integrated)
Dasher
Kegan
ISMMS Mount Sinai Hospital-NY
Psychiatry
Duffy
Samuel
MedStar Georgetown Univ Hosp-DC
Psychiatry
Elnasseh
Abdelrhman
Duke Univ Med Ctr-NC
Psychiatry
Galla
Jonathan
MedStar Georgetown Univ Hosp-DC
Psychiatry
Hovsepian
Gary
George Washington Univ-DC
Psychiatry
Kalsi
Simran
Thomas Jefferson Univ-PA
Psychiatry
Mehta
Varun
ISMMS Mount Sinai Beth Israel-NY
Psychiatry
Seo
Veri
Cambridge Health Alliance-MA
Psychiatry
Sevier
Justin
George Washington Univ-DC
Psychiatry
Silva
Olivia
NYU Grossman School Of Medicine-NY
Psychiatry
Wang
Yixue
University of Virginia
Psychiatry
Yadgar
Ramsin
George Washington Univ-DC
Psychiatry
Ritter
Rebecca
Indiana University SOM
Psychiatry/Merrillville
Jacobs
Lauren
ISMMS Mount Sinai Hospital-NY
Radiation Oncology
Vaziri
Tina
Johns Hopkins Hosp-MD
Radiation Oncology
Brown
Lauryn
U Washington Affil Hosps
Radiology-Diagnostic
Calabria
Emily
Boston Univ Med Ctr-MA
Radiology-Diagnostic
Herman
Sean
Virginia Commonwealth U Hlth Sys
Radiology-Diagnostic
Olivares
Philip
Eastern Virginia Med School
Radiology-Diagnostic
Rahimi
Murwarit
U Texas Med Sch-Houston
Radiology-Diagnostic
Bonitto
Stephano
Ochsner Clinic Foundation-LA
Surgery-Preliminary

Guide to the Transition to Advanced Clinical Practice | 60
McSweeney
Benjamin
Wake Forest Baptist Med Ctr-NC
Surgery-Preliminary
Nasser
Jacob
ISMMS Mount Sinai Hospital-NY
Surgery-Preliminary
Panahi
Armon
NYMC-Metropolitan Hosp Ctr-NY
Surgery-Preliminary
Cho
Kevin
Riverside Reg Med Ctr-VA
Transitional
Herman
Sean
Geisinger Health System-PA
Transitional
Acosta
Christian
Nassau Univ Med Ctr-NY
Transitional
Jacobs
Lauren
Zucker SOM-Northwell South Shore-NY
Transitional
Nemirovsky
Daniel
Creighton University
Urology
Wynne
Michael
George Washington Univ-DC
Urology
Saini
Prashant
Zucker SOM-Northwell Lenox Hill Hosp-NY
Vascular Surgery
CLASS OF 2022 RESIDENCY MATCH LIST
Last Name
First Name
Institution Name
Program Name
Chemtob
Erica
George Washington Univ-DC
Anesthesiology
Danielson
Madalyn
UC San Diego Med Ctr-CA
Anesthesiology
DeFreitas
Cory
George Washington Univ-DC
Anesthesiology
Garcia
Andrew
Harbor-UCLA Med Ctr-CA
Anesthesiology
Hu
Nina
B I Deaconess Med Ctr-MA
Anesthesiology
Ip
Alexander
Brown Univ/Rhode Island Hosp
Anesthesiology
McKiernan
Brianna
U Maryland Med Ctr
Anesthesiology
Mortimer
Nakita
Montefiore Med Ctr/Einstein-NY
Anesthesiology
Nguyen
Connie
NYP Hosp-Columbia Univ Med Ctr-NY
Anesthesiology
Sun
Emily
Thomas Jefferson Univ-PA
Anesthesiology
Weinshel
Talya
Tufts Medical Center-MA
Anesthesiology
Ome Irondi
Obinna
U Washington Affil Hosps
Anesthesiology/Clin Base Yr
Mehta
Nikita
NYU Grossman School Of Medicine-NY
Anesthesiology/NYU Man
Greaves
Tori
Northwestern McGaw/Lurie Childrens-IL
Child Neurology
Adusumilli
Nagasai
George Washington Univ-DC
Dermatology
Millan
Sarah
MedStar Washington Hosp Ctr-DC
Dermatology
Shah
Nidhi
George Washington Univ-DC
Dermatology
Barshay
Allison
Brown Univ/Rhode Island Hosp
Emergency Medicine
Chan
Bill
UC San Diego Med Ctr-CA
Emergency Medicine
Haridasa
Naeha
Univ of Chicago Med Ctr-IL
Emergency Medicine
Herrera
Rachael
Temple Univ Hosp-PA
Emergency Medicine
Hodgson
Ryan
NYP Hosp-Columbia & Cornell-NY
Emergency Medicine
Jacobs
Erica
NYU Grossman School Of Medicine-NY
Emergency Medicine
Keswani
Meghana
University of Virginia
Emergency Medicine
Kotil
Michael
St Lukes Hosp-Anderson-PA
Emergency Medicine
Larsen
Victoria
George Washington Univ-DC
Emergency Medicine
Markin
Katherine
George Washington Univ-DC
Emergency Medicine
Mullings
Jordan
Alameda Health Sys-Highland Hosp-CA
Emergency Medicine
Munday
Adam
Nassau Univ Med Ctr-NY
Emergency Medicine
Parekh
Neil
St Johns Riverside Hospital-NY
Emergency Medicine
Pradarelli
Brad
ISMMS Mount Sinai Morningside-West-NY
Emergency Medicine
Ravishankar
Veda
Cook County Health and Hosps Sys-IL
Emergency Medicine
Rego
Angelica
University of Virginia
Emergency Medicine
Felton
Erin
Sutter Med Ctr of Santa Rosa-CA
Family Medicine
Kerrigan
Michael
Inova Fairfax Hospital-VA
Family Medicine
Kovacs
Mitch
Penn Highlands Healthcare-PA
Family Medicine

Guide to the Transition to Advanced Clinical Practice | 61
Vincent
Kathryn
Inova Fairfax Hospital-VA
Family Medicine
Wang
Elaine
UC San Francisco-CA
Family Medicine
Mehta
Esha
Institute for Family Health-NY
Family Medicine/Harlem-Mt Sinai
Cavallo
Kathryn
George Washington Univ-DC
General Surgery
Cohn
Ellen
Univ of Chicago Med Ctr-IL
General Surgery
Helbing
Alexandra
Parkview Health-IN
General Surgery
Kelley
Devon
Rutgers-R W Johnson Medical School-NJ
General Surgery
McClanahan
Megan
Methodist Hospital-Houston-TX
General Surgery
Perkins
Molly
LSU SOM-New Orleans-LA
General Surgery
Kapani
Nisha
Creighton University-AZ
General Surgery/Valleywise
Ghandakly
Elizabeth
Cleveland Clinic Fdn-OH
Internal Med/Clin Ed
Asif
Usman
Stony Brook Teach Hosps-NY
Internal Med/Southampton
Adeshoga
Kathleen
Kaiser Permanente Mid-Atlantic-MD
Internal Medicine
Agronin
Jacob
Temple Univ Hosp-PA
Internal Medicine
Bergstrom
Annika
UC San Diego Med Ctr-CA
Internal Medicine
Bernstein
Andrew
Thomas Jefferson Univ-PA
Internal Medicine
Bush
Haley
Duke Univ Med Ctr-NC
Internal Medicine
Chhabra
Kabir
U Maryland Med Ctr
Internal Medicine
Distler
Allison
U South Florida Morsani COM-Tampa
Internal Medicine
Gerhard
Eleanor
NYP Hosp-Weill Cornell Med Ctr-NY
Internal Medicine
Gurijala
Nyshidha
Boston Univ Med Ctr-MA
Internal Medicine
Halaseh
Rami
Kaiser Permanente-SF-CA
Internal Medicine
Lum
Nicole
Univ of Chicago Med Ctr-IL
Internal Medicine
Miller
Christian
NYU Grossman School Of Medicine-NY
Internal Medicine
Mirda
Danielle
Hosp of the Univ of PA
Internal Medicine
Moalem
Kamilia
U Miami/Jackson Health System-FL
Internal Medicine
Okezue
Chisom
Westchester Medical Ctr-NY
Internal Medicine
Ortiz
Adriem
CMSRU/Cooper University Hospital-NJ
Internal Medicine
Osman
Kareem
UCLA Med Ctr-CA
Internal Medicine
Pelaez
Guido
Barnes-Jewish Hosp-MO
Internal Medicine
Schonman
Ian
Johns Hopkins Hosp-MD
Internal Medicine
Shincovich
Christina
Massachusetts Gen Hosp
Internal Medicine
Soriano
Rachelle
U Texas at Austin Dell Medical School
Internal Medicine
Stein
Jason
Anne Arundel Med Ctr-MD
Internal Medicine
Vemu
Prasantha
U Washington Affil Hosps
Internal Medicine
Zegarra
Diego
ISMMS Mount Sinai Hospital-NY
Internal Medicine
Syed
Fahim
Trident Medical Center-SC
Internal Medicine
Gowda
Nikhil
George Washington Univ-DC
Interventional Radiology (Integ)
Bernstein
Brittany
Temple Univ Hosp-PA
Medicine-Preliminary
Chan
Christabel
George Washington Univ-DC
Medicine-Preliminary
Gowda
Nikhil
Montefiore-New Rochelle/Einstein-NY
Medicine-Preliminary
Mangera
Linda
Zucker SOM-Northwell Lenox Hill Hosp-NY
Medicine-Preliminary
Mehta
Nikita
George Washington Univ-DC
Medicine-Preliminary
Millan
Sarah
George Washington Univ-DC
Medicine-Preliminary
Vaynberg
Idelle
Greenwich Hospital-CT
Medicine-Preliminary
Weinshel
Talya
St Elizabeths Med Ctr-MA
Medicine-Preliminary
Gopinath
Charlotte
George Washington Univ-DC
Medicine-Primary
Rehman
Muhammad
Advocate Health Care-IL
Med-Prelim/ALGH
Chernet
Sofia
Northwestern McGaw/NMH/VA-IL
Med-Prelim/Neurology
Martin
Gwen
Virginia Commonwealth U Hlth Sys
Med-Prelim/Ophthalmology
Mark
Veronica
Indiana University SOM
Med-Prelim/SW Indiana
Ratnaseelan
Aarane
UPMC Medical Education-PA
Neurodevelopmental Disabilities
Chernet
Sofia
Northwestern McGaw/NMH/VA-IL
Neurology
MacKenzie
Isobel
Barnes-Jewish Hosp-MO
Neurology
Newman
Matthew
George Washington Univ-DC
Neurology

Guide to the Transition to Advanced Clinical Practice | 62
Polyakov
Diane
HCA Medical City Healthcare-TX
Ob-Gyn/Arlington
Akin-Olugbade
Olamide
Northwestern McGaw/NMH/VA-IL
Obstetrics-Gynecology
Bhatnagar
Gauri
Mercy St Vincent Med Ctr-OH
Obstetrics-Gynecology
Dzienny
Alexa
Yale-New Haven Hosp-CT
Obstetrics-Gynecology
Goldstein
Naomi
Ohio State University Med Ctr
Obstetrics-Gynecology
Kripalani
Shawn
ISMMS Mount Sinai Hospital-NY
Obstetrics-Gynecology
Nair
Isabel
Sinai Hospital of Baltimore-MD
Obstetrics-Gynecology
Rossi
Cecilia
Case Western/Univ Hosps Cleveland Med Ctr-OH
Obstetrics-Gynecology
Saleeb
Monica
U Connecticut School of Medicine
Obstetrics-Gynecology
Scanlon
Natalie
Penn State Hershey Med Ctr-PA
Obstetrics-Gynecology
Serpas
Andrea
Anne Arundel Med Ctr-MD
Obstetrics-Gynecology
Skjoldager
Kara
UPMC Medical Education-PA
Obstetrics-Gynecology
Gatens
Heather
Virtua-NJ
Obstetrics-Gynecology
Bernstein
Brittany
Temple Univ Hosp-PA
Ophthalmology
Chan
Christabel
George Washington Univ-DC
Ophthalmology
Sandler
Alexis
William Beaumont Army Medical Center
Orthopaedic
McDaniel
Lea
U Arizona COM-Phoenix
Orthopaedic Surgery
Whiting
Zachariah
Case Western/Univ Hosps Cleveland Med Ctr-OH
Orthopaedic Surgery
Chillakuru
Yeshwant
NYU Grossman School Of Medicine-NY
Otolaryngology
Crowder
Hannah
Duke Univ Med Ctr-NC
Otolaryngology
Terhaar
Samantha
SUNY Upstate Med University
Otolaryngology
Marchak
Alexander
U Louisville SOM-KY
Pathology
Andretti
Olivia
Childrens Hosp-Philadelphia-PA
Pediatrics
Arocha
Rebeca
U Miami/Jackson Health System-FL
Pediatrics
Batoon
Dale Andrew
U Washington Affil Hosps
Pediatrics
Chen
Leon
Montefiore Med Ctr/Einstein-NY
Pediatrics
Desai
Sajani
Montefiore Med Ctr/Einstein-NY
Pediatrics
Johnson
Margot
U Colorado SOM-Denver
Pediatrics
Knapp
Kelsi
Vanderbilt Univ Med Ctr-TN
Pediatrics
Kuipers
Connor
Spectrum Health/Michigan State Univ
Pediatrics
Nolan
Abigail
Childrens National Med Ctr-DC
Pediatrics
Nwasike
Chukwunonso
Baylor Coll Med-Houston-TX
Pediatrics
Partridge
Marie-Claire
Childrens Hosp-Philadelphia-PA
Pediatrics
Pettit
Elizabeth
Childrens National Med Ctr-DC
Pediatrics
Poranki
Menitha
Childrens Hospital-Oakland-CA
Pediatrics
Sandhu
Pavneet
Nicklaus Childrens Hospital-Miami-FL
Pediatrics
Schreiner
Katherine
Childrens Hosp-Philadelphia-PA
Pediatrics
Vanmali
Bobby
Kaiser Permanente-Los Angeles-CA
Pediatrics
Ray
Randall
Childrens Hospital-Boston-MA
Pediatrics-Medical Genetics
Vij
Abhya
Childrens Hospital-Boston-MA
Peds/Childrens Hosp
Vaynberg
Idelle
NYP Hosp-Columbia & Cornell-NY
Phys Medicine & Rehab
Aledort
Emily
ISMMS Mount Sinai Morningside-West-NY
Psychiatry
Clark
Martin
George Washington Univ-DC
Psychiatry
DeSilva
Samantha
U North Carolina Hospitals
Psychiatry
Edouna Obama
Levi Brice
Emory Univ SOM-GA
Psychiatry
Kupsky
Genevieve
Rush University Med Ctr-IL
Psychiatry
Mohyuddin
Hira
George Washington Univ-DC
Psychiatry
Qadir
Sarah
Thomas Jefferson Univ-PA
Psychiatry
Schlager
Samuel
Navy Medical Center, San Diego
Psychiatry
Smith
Kirklin
U Texas at Austin Dell Medical School
Psychiatry
Tillery
Shannon
U Washington Affil Hosps
Psychiatry
Vemulapalli
Keerthi
U Texas at Austin Dell Medical School
Psychiatry

Guide to the Transition to Advanced Clinical Practice | 63
Zurlo
Jessica
Prisma Health-U of SC SOM Columbia
Psychiatry
Messing
Ian
Hosp of the Univ of PA
Radiation Oncology
Thomas
Rehema
U Texas MD Anderson Cancer Ctr
Radiation Oncology
Arsenault
Lauren
Rush University Med Ctr-IL
Radiology-Diagnostic
Goncalves
Tiffany
U Southern California
Radiology-Diagnostic
Kauffman
David
Yale-New Haven Hosp-CT
Radiology-Diagnostic
Liu
Matthew
MedStar Georgetown Univ Hosp-DC
Radiology-Diagnostic
Mangera
Linda
ISMMS Mount Sinai Morningside-West-NY
Radiology-Diagnostic
Osorio
Andrew
Duke Univ Med Ctr-NC
Radiology-Diagnostic
Rehman
Muhammad
U Florida COM-Shands Hosp
Radiology-Diagnostic
Boulos
Sameh
Zucker SOM-Northwell NS/LIJ-NY
Surgery-Preliminary
Lee
Grace
Riverside University Health Sys-CA
Surgery-Preliminary
Lee
Ryan
Rutgers-New Jersey Medical School
Surgery-Preliminary
Liu
Matthew
B I Deaconess Med Ctr-MA
Surgery-Preliminary
Palosaari
Andrew
ISMMS Mount Sinai Hospital-NY
Surgery-Preliminary
Ip
Alexander
MedStar Georgetown Univ Hosp-DC
Surg-Prelim/Georgetown-WHC
Adusumilli
Nagasai
Ascension St Vincent Hosp-IN
Transitional
Arsenault
Lauren
Mountain AHEC-NC
Transitional
Kauffman
David
St Lukes Hosp-Bethlehem-PA
Transitional
Osorio
Andrew
Northside Hospital Gwinnett-GA
Transitional
Shah
Nidhi
Riverside Reg Med Ctr-VA
Transitional
Subramani
Dhanusha
Navy Medical Center, San Diego
Transitional
Thomas
Rehema
Memorial Sloan-Kettering-NY
Transitional
Walker
Ian
NCC-Walter Reed National Military
Transitional
Goncalves
Tiffany
UHS So California Med Ed Consortium
Transitional Year
Danielson
Madalyn
Scripps Mercy Hosp-San Diego-CA
Transitional/Anesthesia
Cruz-Bendezu
Alanna
George Washington Univ-DC
Urology
Dadashian
Eman
Cedars-Sinai Medical Center
Urology
Fu
Melinda
Rutgers-R W Johnson Medical School-NJ
Urology
Nguyen
Andrew
Cooper University Hospital
Urology
Reddy
Akshay
Massachusetts Gen Hosp
Urology
Mangipudi
Sowmya
UC San Francisco-CA
Vascular Surgery
Rodriguez
Stephanie
Medical University of SC
Vascular Surgery

Guide to the Transition to Advanced Clinical Practice | 64
CLASS OF 2021 RESIDENCY MATCH LIST
Applicant Name
Institution Name
Program Name
Gougelet, Jonathan
Univ of Vermont Medical Center
Anesthesiology
Dunn, Patrick
U Texas Med Branch-Galveston
Anesthesiology
Powell, Alva
NYP Hosp-Columbia Univ Med Ctr-NY
Anesthesiology
Yao, Caylynn MedStar Georgetown Univ Hosp-DC Anesthesiology
Dominah, Gifty
Johns Hopkins Hosp-MD
Anesthesiology
Hebenstreit, Trevor
George Washington Univ-DC
Anesthesiology
Richards, Stephen George Washington Univ-DC Anesthesiology
Vilardo, Lauren
Childrens National Med Ctr-DC
Child Neurology
Chung, Stacey
U North Carolina Hospitals
Child Neurology
Aizman, Leora
Johns Hopkins Hosp-MD
Dermatology
Baruffi, Francesca
West Virginia University SOM
Emergency Medicine
Whiteside, Tess
Wellspan Health York Hosp-PA
Emergency Medicine
Croskey, Annabelle
UPMC Medical Education-PA
Emergency Medicine
Lee, Paulyne
UC San Diego Med Ctr-CA
Emergency Medicine
Hollister, Nathaniel
U Nevada Las Vegas SOM
Emergency Medicine
Rapp, Abigail
U Illinois COM-Peoria OSF
Emergency Medicine
Sobelman, Samantha
Stanford Univ Progs-CA
Emergency Medicine
Aly, Iman
St Johns Riverside Hospital-NY
Emergency Medicine
Kuppanda, Nitin
St Johns Riverside Hospital-NY
Emergency Medicine
Van Nispen, Christiaan
San Antonio Military Medical Center
Emergency Medicine
Kaul, Pranav
Northwestern McGaw/NMH/VA-IL
Emergency Medicine
Alsamman, Marya
ISMMS Mount Sinai Hospital-NY
Emergency Medicine
Hartley, Charles
ISMMS Mount Sinai Hospital-NY
Emergency Medicine
Thomas, Daniel
ISMMS Mount Sinai Hospital-NY
Emergency Medicine
Rahman, Md Mostafizur HCA Healthcare/USF Morsani GME-Brandon Emergency Medicine
Akhtar, Aslam
Harbor-UCLA Med Ctr-CA
Emergency Medicine
Hussain, Arman
George Washington Univ-DC
Emergency Medicine
Gordon, Brittney
Emory Univ SOM-GA
Emergency Medicine
Wahrenbrock, Taylor
Cook County Health and Hosps Sys-IL
Emergency Medicine
Tronnier, Amy
Brown Univ/Rhode Island Hosp
Emergency Medicine
McClintock, Kime
Swedish Med Ctr-WA
Family Med/Ballard
Howard, Louisa
U Michigan Hosps-Ann Arbor
Family Med/Ypsilanti
Knowles, Jessenia
UC Irvine Med Ctr-CA
Family Medicine
Hung, Chen-min
PeaceHealth Southwest Med Ctr-WA
Family Medicine
Emamian, Sara
Oregon Health & Science Univ
Family Medicine
Greenblatt, Melissa
Kaiser Permanente-San Diego-CA
Family Medicine
Mangini, Marissa
Inova Fairfax Hospital-VA
Family Medicine
Rao, Madhuri
Cambridge Health Alliance-MA
Family Medicine/Tufts
Rosseau, Natalie MedStar Georgetown Univ Hosp-DC
Gen Surgery/Georgetown-
WHC
Aivaz, Marudeen
Zucker SOM-Northwell NS/LIJ-NY
General Surgery
Barq, Rabab Virginia Commonwealth U Hlth Sys General Surgery
Ichiuji, Brynne
U Southern California
General Surgery
Marsden, Daniel
Nassau Univ Med Ctr-NY
General Surgery
Berger, Peter
Mt Sinai Med Ctr-Miami-FL
General Surgery

Guide to the Transition to Advanced Clinical Practice | 65
Habboosh, Noor
Montefiore Med Ctr/Einstein-NY
General Surgery
Potarazu, Deepika
Inova Fairfax Hospital-VA
General Surgery
Lin, Ryan
George Washington Univ-DC
General Surgery

Matecki, Mary
George Washington Univ-DC
General Surgery
Ong, Paulina
NYU Grossman School Of Medicine-NY
Int Med/NYU-Tisch-Kimmel
Mire, Muhammad
Univ of Chicago Med Ctr-IL
Internal Medicine
Abraham, Tsion UC San Francisco-CA Internal Medicine
Agdashian, David
UC San Diego Med Ctr-CA
Internal Medicine
Kubendran, Sindhu
UC San Diego Med Ctr-CA
Internal Medicine
Hayrapetian, Laurie
U Southern California
Internal Medicine
Hoffman, Eric
U Southern California
Internal Medicine
Hand, Taylor
U Minnesota Med School
Internal Medicine
Rao, Sanjana
U Miami/Jackson Health System-FL
Internal Medicine
Kaji, Raina
U Maryland Med Ctr
Internal Medicine
Roman, Aida
U Connecticut School of Medicine
Internal Medicine
Khludenev, George
U Arizona COM-Tucson
Internal Medicine
Houle, Matthew
Tulane Univ SOM-LA
Internal Medicine
Finau, Melesilika Portsmouth Naval Medical Center Internal Medicine
Panda, Arjun
Oregon Health & Science Univ
Internal Medicine
Mandler, Ari
NYP Hosp-Weill Cornell Med Ctr-NY
Internal Medicine
Onyilofor, Chinelo
NYP Hosp-Columbia Univ Med Ctr-NY
Internal Medicine
Atienza, Matthew
Montefiore Med Ctr/Einstein-NY
Internal Medicine
Varghese, Reshma
MedStar Georgetown Univ Hosp-DC
Internal Medicine
Moazzami, Mitra
Mayo Clinic School of Grad Med Educ-MN
Internal Medicine
Mai, William
Mayo Clinic School of Grad Med Educ-FL
Internal Medicine
Clark, Christina
Maine Med Ctr
Internal Medicine
Zafar, Nadia
Maine Med Ctr
Internal Medicine
Haley, Mairin
Lankenau Med Ctr-PA
Internal Medicine
Aquino, Gabrielle
ISMMS Mount Sinai Hospital-NY
Internal Medicine
Darwish, Christina
ISMMS Mount Sinai Hospital-NY
Internal Medicine
Dharia, Ishaan
ISMMS Mount Sinai Hospital-NY
Internal Medicine
Al Shabeeb, Reem Inova Fairfax Hospital-VA Internal Medicine
Roche, Kyle
George Washington Univ-DC
Internal Medicine
Chan, Emily
Family Health Ctrs at NYU Langone-NY
Internal Medicine
Chan, Melissa
Family Health Ctrs at NYU Langone-NY
Internal Medicine
Hennessey, Megan
Dartmouth-Hitchcock Med Ctr-NH
Internal Medicine
Makonnen, Tirsit
CMSRU/Cooper University Hospital-NJ
Internal Medicine
Gupta, Simran
Brown Univ/Rhode Island Hosp
Internal Medicine
Cerezo, Maria Abigail Boston Univ Med Ctr-MA Internal Medicine
Zepp, Molly
B I Deaconess Med Ctr-MA
Internal Medicine
Imtiaz, Danish
UPMC Medical Education-PA
Interventional Radiology (Integ)
Zemel, Rachel
MedStar Georgetown Univ Hosp-DC
Medicine-Pediatrics
Osei, Kendrah
St Agnes Hospital-MD
Medicine-Preliminary
Nguyen, Chantal
Santa Clara Valley Med Ctr-CA
Medicine-Preliminary
Aizman, Leora
MedStar Washington Hosp Ctr-DC
Medicine-Preliminary
McCullum, Catherine George Washington Univ-DC Medicine-Preliminary
Guide to the Transition to Advanced Clinical Practice | 66

Richards, Stephen
George Washington Univ-DC
Medicine-Preliminary
Sohal, Preet
George Washington Univ-DC
Medicine-Preliminary
Duggal, Neel
HCA Healthcare/USF Morsani GME-Trinity
Medicine-Preliminary
Pugliese, Christina NYP Hosp-Weill Cornell Med Ctr-NY Medicine-Primary
Pashai, Erika
George Washington Univ-DC
Medicine-Primary
Ormond, Jelyca
Kaiser Permanente-Santa Clara-CA
Medicine-Primary/CHOICE
Dominah, Gifty
MedStar Union Memorial Hosp-MD
Med-Prelim/Anesthesiology-JHU
Rokni, Alex
U Illinois COM-Chicago
Med-Prelim/UIH
Almeida, Neil
University at Buffalo SOM-NY
Neurological Surgery
Archuleta, Christine
Virginia Commonwealth U Hlth Sys
Obstetrics-Gynecology
Georgakopoulos, Bianca
U Kentucky Med Ctr
Obstetrics-Gynecology
Konigkramer, Megan
U Illinois COM-Chicago
Obstetrics-Gynecology
Thirunagaru, Koumudi
St Lukes Hosp-Bethlehem-PA
Obstetrics-Gynecology
Hynds, Elaine
Pennsylvania Hospital
Obstetrics-Gynecology
Fuerst, Megan Oregon Health & Science Univ Obstetrics-Gynecology
Milando, Rose
ISMMS Mount Sinai Morningside-West-NY
Obstetrics-Gynecology
Sadeghi, Noushine
Christiana Care-DE
Obstetrics-Gynecology
Tsaturian, Mary
Arrowhead Reg Med Ctr-CA
Obstetrics-Gynecology
Walker, Taniya Brigham & Womens Hosp-MA
Obstetrics-Gynecology/BWH-
MGH
Aneja, Prabhleen
Beaumont Health-MI
Obstetrics-Gynecology/Royal Oak
Baker, Dara
Illinois Eye and Ear Infirmary
Ophthalmology
Sohal, Preet
George Washington Univ-DC
Ophthalmology
Kartalias, Katina
Walter Reed National Medical Center
Orthopaedic Surgery
Rodenhouse, Thomas
U Rochester/Strong Memorial-NY
Orthopaedic Surgery
Ward, Caitlin
Rush University Med Ctr-IL
Orthopaedic Surgery
Ramamurti, Pradip
University of Virginia
Orthopaedic Surgery/5 Yr
Bestourous, Daniel
University of Utah Health
Otolaryngology
Straughan, Alexander
U Minnesota Med School
Otolaryngology
Shim, Timothy
Stony Brook Teach Hosps-NY
Otolaryngology
Mamidi, Ishwarya LSU SOM-New Orleans-LA Otolaryngology
Nogues, Juan
ISMMS Mount Sinai Hospital-NY
Otolaryngology
Michel, Margaret
Cleveland Clinic Fdn-OH
Otolaryngology
Photavath, Jai
Westchester Medical Ctr-NY
Pediatrics
Kafashzadeh, Dariush UCLA Med Ctr-CA Pediatrics
Lipsitz, Joshua
U Texas Southwestern Med Sch-Dallas
Pediatrics
Chun, Camille
U Colorado SOM-Denver
Pediatrics
Bakizada, Zayna
Oregon Health & Science Univ
Pediatrics
Pudalov, Natalie
Medical University of SC
Pediatrics
Patrick, Kristin
Cincinnati Childrens Hosp Med Ctr-OH
Pediatrics
Rashidi, Ghazal
Cincinnati Childrens Hosp Med Ctr-OH
Pediatrics
Brown, Ciara Childrens National Med Ctr-DC Pediatrics
Chase, Hannah
Childrens National Med Ctr-DC
Pediatrics
Guide to the Transition to Advanced Clinical Practice | 67

Considine, Colleen
Childrens National Med Ctr-DC
Pediatrics
Ben-Maimon, Sivan
Childrens Hosp-Philadelphia-PA
Pediatrics
Marwah, Harleen
Childrens Hosp-Philadelphia-PA
Pediatrics
Nishikawa, Moena Childrens Hospital-Oakland-CA Pediatrics
Burkholder, Joshua
U Nevada Las Vegas SOM
Pediatrics
Johnson, Sheryl
Rutgers-Newark Beth Israel Med Ctr-NJ
Pediatrics
Ceneri, Nicolle
Childrens National Med Ctr-DC
Pediatrics-Research
Summerlin, Maxwell
U Colorado SOM-Denver
Peds/Med Genetics & Genomics
Nguyen, Chantal
Stanford Univ Progs-CA
Phys Medicine & Rehab
Satin, Zachary
MedStar National Rehab Hosp-DC
Phys Medicine & Rehab
Gable, Brenda
Ohio State University Med Ctr
Psychiatry
Keshavarz, Samaneh
MedStar Georgetown Univ Hosp-DC
Psychiatry
Taylor, Benjamin
MedStar Georgetown Univ Hosp-DC
Psychiatry
Guide to the Transition to Advanced Clinical Practice | 68

Peace, Melissa
Medical University of SC
Psychiatry
Siddiqi, Tulha
Johns Hopkins Hosp-MD
Psychiatry
Quinn, Margot
ISMMS Mount Sinai Hospital-NY
Psychiatry
Islam, Celia U Maryland Med Ctr Psychiatry/Sheppard Pratt
Momeni, Kimia
U Maryland Med Ctr
Psychiatry/Sheppard Pratt
Pepin, Abigail
Hosp of the Univ of PA
Radiation Oncology
Osei, Kendrah
Johns Hopkins Hosp-MD
Radiology-Diagnostic
Imtiaz, Danish
Swedish Med Ctr-WA
Surgery-Preliminary
Maghsoudi, Taneen
Carilion Clinic-Virginia Tech Carilion SOM
Surgery-Preliminary
Brodsky, Spencer
Weiss Memorial Hospital-IL
Transitional
Osman, Omer
LewisGale Medical Center
Transitional
Elovic, Andres
Mount Sinai Medical Center
Urology
Shoen, Ezra
Mount Sinai Medical Center
Urology
Guide to the Transition to Advanced Clinical Practice | 69

Appendix I: Saving Money
Saving Money on Residency Travels
Federal Student Loans: These may be used for travel to residency interview locations. For reference, the allowance in
the Cost of Attendance was $3,200 for the 2018-2019 academic year. Should you require additional funding, visit
the Office of Financial Aid’s website and complete the fourth year travel allowance form and the travel expense
worksheet.
Institutional Loans for Canadian students: Canadian Students traveling for residency interviews in the U.S. may obtain up
to $2000 in institutional loan funding through the Medical School Consolidated Loan Program. The interest rate on
these loans is 0% through six months after graduation and then the rate changes to 6%. The loan must be paid back
through quarterly payments within 10 years.
Private Loans: The maximum amount of federal or private loan funding a student can take out during a school year
cannot exceed the cost of attendance. However, cost of attendance cannot include expenses associated with
relocating to a residency program after graduation. If you need additional loan funding to cover these expenses you
can consider a “residency and relocation loan” offered by a private bank. Usually, these loans can be repaid after
residency (just like educational loans), but the amount is sent to the student and not the school.
More information about these can be found on www.finaid.org. Make sure to look only at loans that mention
“residency” or “relocation” in their title or description, since another private loan may be denied if you are already
receiving funding that equals your cost of attendance. Due to our code of conduct we are unable to recommend any
private loan lenders. However, the Office of Financial Aid staff would be happy to meet with you to discuss the
terms of any loans you decide to pursue.
Although exact terms vary depending on the residency and relocation loan lender, it seems that as with everything
else, a good credit score helps. The amount can be up to $20,000, rates of interest vary, although terms may be
harsh. Usually all you need to apply is proof of applying to residency (like a letter from the Dean’s office) and proof
of interviewing (invite letter). It sounds like the turnaround time is quick (few weeks from application until money
in your account), and you can apply anytime as a fourth year student up until six months into residency.
Tax Deductions: We have not found any final word on whether interview expenses qualify for tax deductions or not.
These may help figure it out: http://www.irs.gov/publications/p529/ar02.html and http://www.irs.gov/pub/irs-
pdf/p4128.pdf. Remember to keep all of your moving receipts and review IRS publication 521 for more
information about the effects of moving on your federal taxes.
Credit Cards: Using a card that gives you airline miles or discounts on rental cars can help offset some of the travel
expenses
AMA membership: Helps with getting discounts on car rentals. More information available under the benefits section
on their website.
Others: Research the programs to which you are applying by checking their websites to see if they can fund your
interview. For example, the Wisconsin Academy of Family Physicians provides funding support to MS4s who
interview at four or more FM residency programs in Wisconsin.
Saving Money on Housing during Interviews
Rarely, programs will offer to cover the cost of your hotel stay. Others may be able to obtain a discounted rate for
you. If you feel comfortable, ask the residency coordinator if he/she can provide you with suggestions as to where
other applicants have stayed in the past.
Guide to the Transition to Advanced Clinical Practice | 70

Some GW Alumni offer to host interviewing students coming to their local area. For more information on the GW
Medical Alumni Connect (GWMAC) Program please visit: https://smhs.gwu.edu/alumni/volunteer/GW-Med-
Alumni-Connect/student-information. You may fill out the GWMAC student registration form here:
https://docs.google.com/forms/d/e/1FAIpQLSf7JPjgVrWKdwA79U3P5AXDdu16G7Nh0_rX9B3MRvAOpq7S
fw/viewform.
For help in finding local housing during your interviews, you can also call the American Medical
Association. The AMA Alliance, in partnership with the AMA Resident and Fellow and Medical Student
Sections, runs the Community Welcoming Program -- which finds on-site hosts for fourth- year medical
students and their families as they interview for residency. This helps medical students minimize travel costs
while keeping them connected with organized medicine. More information about the Community
Welcoming Program, including how to request housing and how to become a host is available on the AMA
Alliance Website.
Guide to the Transition to Advanced Clinical Practice | 71
