
Clin.
exp.
Immunol.
(1987)
68,
215-222
Evaluation
of
the
anti-cardiolipin
antibody
test:
report
of
an
international
workshop
held
4
April
1986
E.
N.
HARRIS,
A.
E.
GHARAVI,
S.
P.
PATEL*
&
G.
R.
V.
HUGHES
The
Lupus
Arthritis
Research
Laboratory,
The
Rayne
Institute,
St
Thomas's
Hospital,
London
and
*
Department
of
Community
Medicine,
St
Thomas's
Hospital,
London
(Acceptedfor
publication
4
November
1986)
SUMMARY
Thirty
laboratories
from
institutions
in
Britain,
France,
Italy,
The
Netherlands,
New
Zealand,
Sweden
and
the
USA
participated
in
a
workshop
to
evaluate
the
anti-cardiolipin
(aCL)
test.
Participants
were
asked
to
measure
IgG
and
IgM
aCL
in
seven
samples
on
each
of
three
separate
days.
The
seven
samples
were
prepared
so
that
IgG
and
IgM
aCL
concentrations
were
known
before
distribution.
Twenty-three
of
30
laboratories
measur-
ing
IgG
aCL
had
significant
regression
slopes
(P<0-001)
when
optical
absorbance
readings
or
counts
per
minute
were
compared
with
IgG
aCL
concentration.
Twenty-four
of
28
laboratories
measuring
IgM
aCL
had
significant
regression
slopes
(P<0001).
Coefficient
of
determination
(R2)
ranged
from
81
1
%
to
98
7%
for
laboratories
with
valid
IgG
aCL
assays
and
from
48
0%
to
96
7%
for
valid
IgM
aCL
assays.
Valid
assays
had
in
common
the
use
of
10%
fetal
calf
or
10%
adult
bovine
serum
in
PBS.
Assays
that
were
not
valid
had
in
common
the
use
of
PBS,
PBS-Tween,
or
0
3%
gelatin
as
diluents.
All
laboratories
with
valid
assays
defined
samples
with
high
and
moderate
aCL
levels
as
positive
but
there
was
no
consensus
about
low
positive
samples.
This
study
shows
that
properly
performed
ELISA
or
SRIA
assays
can
be
used
to
provide
an
accurate,
reproducible,
and
quantitative
measure
of
IgG
and
IgM
aCL
concentration
in
serum
samples.
Keywords
anti-cardiolipin
antibody
thrombosis
ELISA
assay
fetal
loss
INTRODUCTION
Preliminary
studies
have
suggested
that
the
anti-cardiolipin
antibody
(aCL)
test
is
important
clinically
in
identifying
a
group
of
patients
prone
to
episodes
of
recurrent
thrombosis,
fetal
loss,
and/or
thrombocytopenia
(Editorial,
1985;
Harris
et
al.,
1985a).
Since
the
first
published
report
of
a
radioimmunoassay
method
to
detect
anti-cardiolipin
antibodies
(Harris
et
al.,
1983),
many
other
centres
have
reported
data
using
various
modifications
of
this
test
(Koike
et
al.,
1984;
Norberg
et
al.,
1984;
Colaco
&
Male,
1985;
Tincani
et
al.,
1985;
Lockshin
et
al.,
1985;
Loizou
et
al.,
1985;
Meyer
et
al.,
1985;
Gharavi
et
al.,
1987).
Given
the
potential
importance
of
the
test
and
its
relative
'novelty',
we
believe
that
it
has
become
necessary
to
standardize
the
aCL
test
before
its
widespread
adoption
as
a
routine
laboratory
test.
Recent
clinical
reports
have
suggested
that
thrombosis
and
fetal
loss
are
more
frequent
in
patients
with
'high'
compared
to
those
with
'low'
aCL
levels
(Lockshin
et
al.,
1985;
Harris
et
al.,
1986)
and
there
have
been
reports
that
'lowering'
anti-phospholipid
(aPL)
levels
in
women
with
Correspondence:
Dr
E.
N.
Harris,
The
Lupus
Arthritis
Research
Laboratory,
The
Rayne
Institute,
St
Thomas's
Hospital,
London
SE1
7EH,
UK.
215
these
antibodies
and
fetal
loss,
using
steroid
therapy,
may
result
in
live
births
(Lubbe
et
al.,
1984;
Branch
et
al.,
1985).
If
these
clinical
observations
are
to
be
substantiated,
it
will
be
necessary,
as
a
minimal
requirement,
that
laboratories
will
be
able
to
distinguish
correctly
and
reproducibly
between
samples
with
varying
aCL
levels.
It
would
be
helpful,
too,
to
adopt
some
unit
of
measurement
that
would
enable
exchange
of
results
between
laboratories.
In
addition,
for
laboratories
wishing
to
set
up
the
aCL
test,
some
method
should
be
available
for
evaluating
which
of
the
published
assay
methods
give
valid
results.
The
aCL
standardization
workshop
was
designed
to
achieve
some
of
the
objectives
outlined
above.
There
is
some
evidence
to
suggest
that
antibody
isotypes
may
be
important
clinically
(Harris
et
al.,
1986),
hence
the
workshop
was
designed
to
evaluate
measurement
both
of
IgG
and
IgM
aCL.
Seven
samples
were
prepared
in
such
a
way
that
concentrations
of
IgG
and
IgM
aCL
could
be
estimated
in
each
sample
by
measurements
that
were
largely
independent
of
the
ELISA
or
SRIA
techniques
being
evaluated.
This
enabled
an
objective
measure
of
the
accuracy
and
reproducibility
of
assay
methods
used
to
estimate
aCL
in
serum
samples.
We
were
also
able
to
recommend
a
unit
of
measurement
of
aCL
assays
and
to
determine
which
assay
methods
provided
valid
results.
METHODS
Preparation
of
samples.
Six
of
the
seven
samples
were
prepared
by
mixing
various
proportions
of
sera
from
two
patients
and
a
normal
person.
Both
patients
A
and
B
had
the
lupus
anticoagulant
and
histories
of
multiple
thromboses
compatible
with
the
'anti-phospholipid
syndrome'
(Harris
et
al.,
1985a),
but
patient
A
had
high
levels
of
IgG
aCL
alone,
and
patient
B
had
high
levels
of
IgM
aCL
alone.
Preparations
of
affinity
purified
IgG
and
IgM
aCL
antibodies
from
sera
of
patient
A
and
patient
B,
respectively,
were
prepared
(Harris
et
al.,
1985b).
These
affinity-purified
preparations
were
characterized
by
Ouchterlony
and
immunoelectrophoresis
(IEP)
and
antibody
concentrations
determined
by
the
Mancini
method.
Serial
dilutions
of
the
affinity-purified
preparations
were
compared
with
patient
sera
from
which
these
preparations
were
obtained
using
a
modified
aCL
ELISA
technique
(Gharavi
et
al.,
1986).
On
the
basis
of
these
results,
the
concentration
of
IgG
aCL
in
sample
A
was
estimated
to
be
approximately
320
yg/ml
and
the
concentration
of
IgM
aCL
in
sample
B
to
be
approximately
82
pg/ml.
For
the
purpose
of
this
study,
sample
A
was
designated
as
having
an
IgG
aCL
binding
activity
of
320
GPL
units,
where
I
GPL
unit
was
taken
as
the
binding
activity
of
1
yg/ml
IgG
aCL,
affinity-purified
from
sample
A.
Sample
B
was
designated
as
having
82
MPL
units,
where
1
MPL
unit
was
taken
as
the
binding
activity
of
1
,ug/ml
IgM
aCL,
affinity-
purified
from
sample
B.
A
total
of 25
ml
of each
of
seven
test
samples
were
prepared
by
mixing
various
proportions
of
serum
samples
A,
B
and
N.
We
were,
therefore,
able
to
calculate
a
GPL
and
MPL
value
for
each
test
sample
based
on
the
proportion
of
samples
A,
B
and
N
in
that
test
sample.
For
example,
if
in
preparing
a
test
sample,
we
mixed
10
ml
of
sample
A
(320
GPL),
5
ml
of
sample
B
(82
MPL),
and
10
ml
of
sample
N
(zero
GPL,
zero
MPL),
the
concentration
of
IgG
aCL
in
the
test
sample
would
be
10/25
x
320
GPL
units
and
of
IgM
aCL,
5/25
x
82
MPL
units.
Using
this
method,
we
were
able
to
prepare
seven
test
samples
whose
concentrations
together
encompassed
the
full
sensitive
range
of
ELISA
and
SRIA
assays
for
IgG
and
IgM
aCL
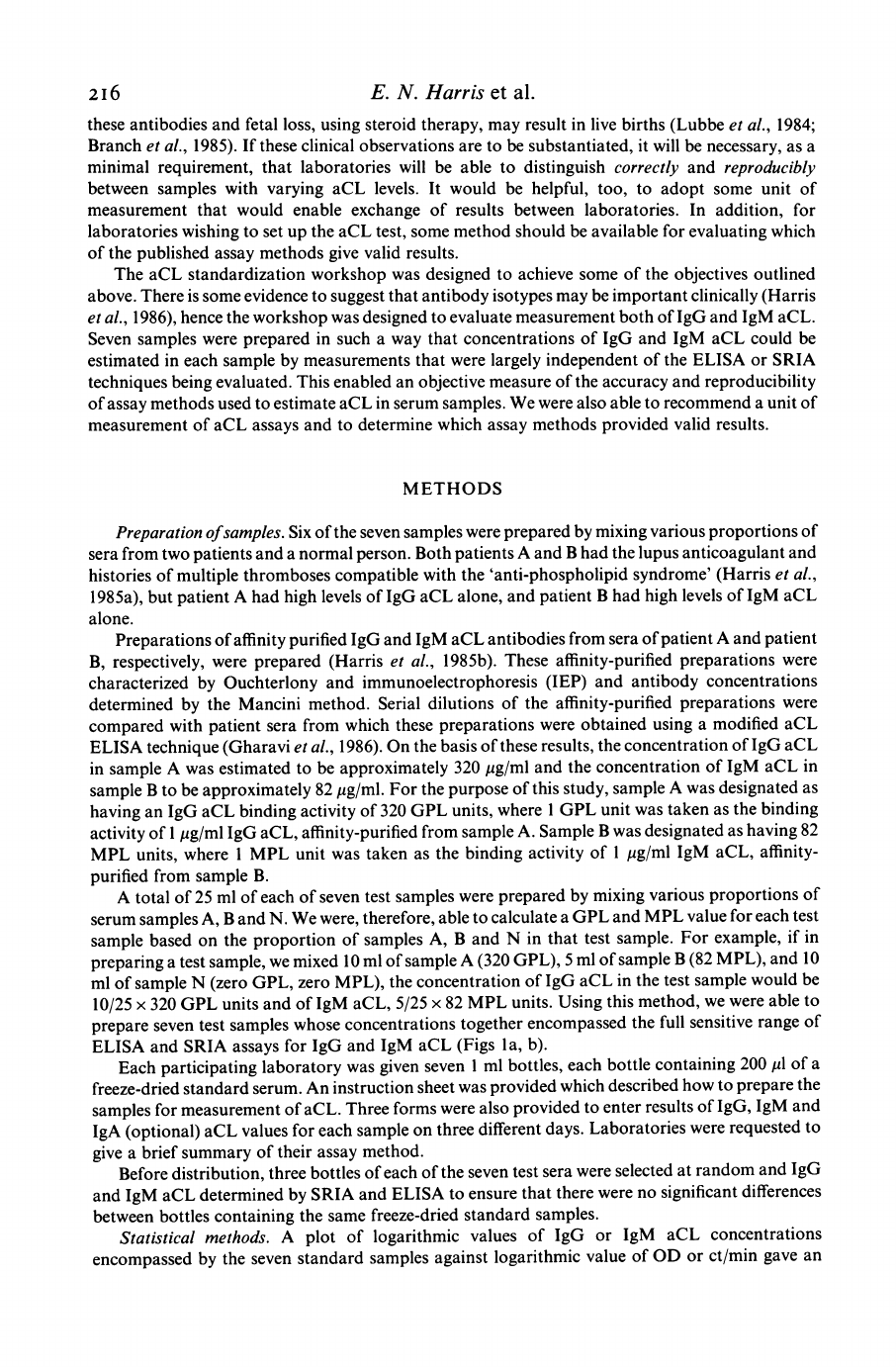
(Figs
la,
b).
Each
participating
laboratory
was
given
seven
1
ml
bottles,
each
bottle
containing
200
p1
of
a
freeze-dried
standard
serum.
An
instruction
sheet
was
provided
which
described
how
to
prepare
the
samples
for
measurement
of
aCL.
Three
forms
were
also
provided
to
enter
results
of
IgG,
IgM
and
IgA
(optional)
aCL
values
for
each
sample
on
three
different
days.
Laboratories
were
requested
to
give
a
brief
summary
of
their
assay
method.
Before
distribution,
three
bottles
of
each
of
the
seven
test
sera
were
selected
at
random
and
IgG
and
IgM
aCL
determined
by
SRIA
and
ELISA
to
ensure
that
there
were
no
significant
differences
between
bottles
containing
the
same
freeze-dried
standard
samples.
Statistical
methods.
A
plot
of
logarithmic
values
of
IgG
or
IgM
aCL
concentrations
encompassed
by
the
seven
standard
samples
against
logarithmic
value
of
OD
or
ct/min
gave
an
2i6
E.
N.
Harris
et
al.

International
workshop
on
anti-cardiolipin
antibody
test
0-
-80
x
a)
0
0
80
160
aCL
concentration
(IgG)
(GPL)
-'~
E
06-
-601
C.
)
Cl)
0.
0
0
10
30
50
aCL
concentration
(IgM)
(MPL)
Fig.
1.
Relationship
between
optical
absorbance
and
IgG
aCL
concentrations
(Fig.
la)
or
IgM
aCL
concentrations
(Fig.
Ilb)
for
five
laboratories,
two
with
solid
phase
radioimmunoassays
(-&,
Lab.
12
1;
*,
Lab.
12)
and
three
with
enzyme-linked
immunosorbent
assays
(a,
Lab.
19;
0,
Lab.
24;
0,
Lab.
50).
approximately
linear
relationship.
A
linear
regression
equation
was
derived
for
each
laboratory
as
shown
below:
Loe(
Y)=
a
+b.
Lo&e
(A)
where
Y
is
OD
reading
or
ct/min;
X
is
IgG
or
IgM
aCL
concentration;
a
is
the
intercept
and
b
is
the
slope.
Analysis
of
variances
for
linear
regression
was
carried
out
on
results
of
each
laboratory
to
test
for
significance
of:
(I)
Linear
regression,
i.e.
to
test
whether
the
common
slope
was
significantly
different
from
zero.
(2)
Between-day
variation,
i.e.
to
test
for
parallelism
of
the
slopes
for
the
different
days,
and
shifts
in
the
position
of
the
regression
line.
Assay
methods
were
defined
as
acceptable
only
if
the
linear
regression
was
statistically
significant
at
the
0-1I%
level.
RESULTS
Seven
test
samples
were
distributed
to
each
of
39
laboratories.
Results
were
obtained
from
30
of
the
39
laboratories.
All
30
laboratories
measured
IgG
aCL
in
the
seven
test
sera
and
28/30
measured
IgM
aCL.
Twenty
of
the
30
laboratories
measured
IgG
aCL,
and
20/28
laboratories
measured
IgM
aCL
in
all
samples
on
three
different
days.
Seven
laboratories
measured
IgG
aCL
and
five
laboratories
measured
IgM
aCL
on
two
different
days.
Three
laboratories
measured
IgG
aCL
and
IgM
aCL
on
one
day
only.
Twenty-six
of
the
30
laboratories
used
an
ELISA
technique,
three
laboratories
used
a
solid
phase
radioimmunoassay
technique,
and
one
laboratory
used
a
diagnostic
kit
(Cheshire
Diagnostics,
Cheshire,
UK),
based
on
an
ELISA
technique.
Regression
significance
and
coefficient
of
determination.
A
laboratory
was
defined
as
having
a
217

218
E.
N.
Harris
et
al.
5-4
-
(a)
G)
0
4-7
_
.0
0
40
Cal
0
1-1
2-2
Log
aCL
concentration
(IgG)
0.
0
0-0
-(b)
0'7
-J3
o
(
1.1
22
Log
aCL
concentration
(IgG)
Fig.
2.
Example
of
approximate
linear
relationship
between
logarithmic
values
of
optical
absorbance
and
logarithmic
values
of
IgG
aCL
concentrations
encompassed
by
the
seven
standard
samples
for
(a)
a
laboratory
with
a
valid
assay
and
(b)
a
laboratory
with
an
assay
that
was
not
valid.
(a)
(0)
Day
1,
(0)
day
2,
(0)
day
3;
R2
=
98
7%,
F
regression
=
1731
(P
<
0
001),
Fbetween
day
=
NS,
loge
Y=
3
047
+
0
828
x
log,
(X).
(b)
(e)
Day
1,
(0)
day
2,
(11)
day
3;
R2=
20
6%,
Fregression
=NS,
Fbetween
day
=NS,
log,
Y=
-
1365
+0-071
x
log,
(X).
valid
assay
only
if
the
linear
regression
was
statistically
significant
at
the
0-1I%
level.
There
were
no
laboratories
where
the
linear
regression
was
significant
between
5
%
and
0-1I%
level.
Twenty-three
of
the
30
participating
laboratories
measuring
IgG
aCL
and
24
of
the
28
laboratories
measuring
IgM
aCL
were
valid
according
to
the
above
criteria.
All
23
laboratories
with
a
valid
test
for
IgG
aCL
had
coefficients
of
determination,
R
2,
ranging
from
81
-1%
to
98
7%
(Fig.
2a).
The
six
laboratories
with
non-valid
IgG
aCL
assays
had
coefficients
of
determination,
RI,
ranging
from
0
03%
to
34
0%
(Fig.
2b).
Coefficients
of
determination,
R
,
for
IgM
aCL
varied
from
48
0%
to
96
7%
for
laboratories
with
valid
assays,
and,
0
0%
to
0-2%,
for
laboratories
with
non-
valid
assays.
All
23
laboratories
with
significant
linear
regression
values
of
IgG
aCL
had
slopes
greater
than
0
20
(Fig.
2a),
and
all
seven
laboratories
with
linear
regression
values
which
were
not
statistically
significant
had
slopes
less
than
0-
10
(Fig.
2b).
For
IgM
aCL,
the
24
laboratories
with
valid
tests
had
slopes
greater
than
0
2,
and
all
four
laboratories
with
non-valid
tests
had
slopes
less
than
0-05.
Between-day
variations.
Only
six
of
the
20
laboratories
measuring
IgG
aCL
on
more
than
one
day
and
4/24
laboratories
measuring
IgM
aCL
had
significant
variations
in
'between-day'
readings.
No
laboratory
had
a
significant
difference
in
the
slopes
between
different
days.
Significant
between-
day
variations
need
not
invalidate
an
assay
method
and
usually
reflects
the
fact
that
OD
readings
may
vary
from
day
to
day
because
of
slight
variations
in
experimental
conditions.
Despite
these
variations,
the
relationship
between
OD
readings
and
aCL
concentrations
remained
relatively
constant.
Determination
of
level
of
positivity.
The
seven
test
samples
could
be
ranked
according
to
their
IgG
aCL
(Table
1)
or
IgM
aCL
concentrations
(Table
2).
Sample
No.
62,
which
consisted
entirely
of
serum
from
a
healthy
patient,
was
assumed
to
have
no
IgG
or
IgM
aCL.
For
IgG
aCL,
one
of
the
23
laboratories
with
valid
assays
did
not
indicate
which
of
the
seven
samples
werhere
he
linr
on
w
remaining
22
laboratories
listed
samples
35
(160
GPL),
71
(80
GPL)
and
17
(20
GPL)
as
positive.
Twenty
of
the
22
laboratories
considered
sample
26
(15
GPL)
as
positive
and
one
each
of
the
remaining
laboratories
took
this
sample
as
'doubtful
positive'

International
workshop
on
anti-cardiolipin
antibody
test
Table
1.
The
seven
test
samples
ranked
according
to
IgG
aCL
concentration
and
number
of
laboratories
defining
each
of
the
seven
samples
as
positive,
doubtful
positive,
or
negative
IgG
No.
Sample
Concentration
No.
doubtful
No.
no.
(GPL
units)
positive
positive
negative
1
160
22
0
0
2
80
22
0
0
3
20
22
0
0
4
15
20
1
1
5
10
15
5
2
6
5
11
4
7
7
0
2
0
20
Table
2.
The
seven
standard
samples
ranked
according
to
IgM
aCL
concentration
and
number
of
laboratories
defining
each
of
the
seven
samples
as
positive,
doubtful
positive
or
negative
IgM
No.
Sample
concentration
No.
doubtful
No.
no.
(MPL
units)
positive
positive
negative
1
52
21
0
0
2
26
21
0
0
3
13
20
1
0
4
65
18
1
2
5
3.2
14
3
4
6
16
9
4
8
7
0
0
0
21
and
negative.
The
remaining
results
are
summarized
in
Table
1.
Of
note
was
the
fact
that
20/22
laboratories
considered
sample
62
(0
GPL)
as
negative.
For
IgM
aCL,
21
of
the
24
laboratories
with
valid
assays
indicated
which
of
the
seven
samples
were
considered
positive.
All
21
laboratories
listed
samples
17
(52
MPL)
and
71
(26
MPL)
as
positive
(Table
2).
Twenty
of
the
21
laboratories
considered
sample
26
(13
MPL)
as
positive
and
the
remaining
laboratory
considered
the
sample
as
'doubtful
positive'.
Other
results
are
summarized
in
Table
2.
All
21
laboratories
agreed
that
sample
62
(0
MPL)
was
negative.
The
differences
between
laboratories
in
assigning
positivity
to
samples
with
low
aCL
concentrations
illustrate
the
difficulty
in
determining
a
mutually
agreeable
'cut-off'
point
and
may
explain
why
there
may
be
quite
wide
variations
in
reports
of
percentages
of
patients
'positive'
for
the
aCL
test.
Evaluation
of
materials
and
methods
used
by
participating
laboratories.
There
was
no
single
computed
measurement
that
enabled
us
to
determine
whether
one
given
assay
method
was
better
than
the
other.
Assays
best
able
to
measure
IgG
and
IgM
aCL
concentrations
over
the
range
of
concentrations
encompassed
by
the
seven
standard
samples
had
the
following
features
in
common:
a
coefficient
of
determination,
R2,
of
85
0%
or
greater,
and
a
linear
regression
equation
with
a
slope
greater
than
0
35.
A
summary
of
the
various
assay
methods
that
achieved
these
goals
is
shown
in
Table
3.
All
assay
methods
that
were
not
valid
had
the
following
features
in
common:
the
use
of
phosphate
buffered
saline
(PBS)
alone,
PBS/Tween,
or
0
3%
gelatin/PBS
as
diluent
of
serum
219

Table
3.
Summary
of
assay
conditions
used
by
laboratories
with
valid
assays
Materials
and
methods
used
in
assays
considered
satisfactory
Plates
coated
with
cardiolipin
Plates
blocked
Patient
serum
Anti-human
antibody
(enzyme-labelled
in
ELISA
I-labelled
in
SRIA)
2nd
antibody
Source
Concentration
Solvent
evaporation
Blocking
materials
Time
Dilution
Diluent
Incubation
time
Material
Incubation
time
usually
Sigma.
12
-
100
pg/ml;
25-40
pl/well.
under
nitrogen;
under
vacuum;
4
C
overnight.
10%
fetal
calf
serum
(FCS)/PBS
10/oo
adult
bovine
(or
ox)
serum
(ABS)/PBS;
1%
bovine
serum
albumin
(BSA)/PBS;
15%
BSA/0
300
gelatin/PBS.
1
-
4
h
at
room
temperature.
1/50
and
below
(dilutions
less
than
1/50,
e.g.
1/25
appeared
less
reliable).
10%
FCS;
10%
ABS;
0.10%
BSA;
0.750%
BSA/0
3%
gelatin.
1
-
4
h
(overnight
with
0O
%
BSA
in
one
instance)
at
room
temperature.
usually
a.p.
goat
or
a.p.
rabbit
anti-human
IgG
or
anti-human
IgM
in
the
same
diluent
as
used
for
serum.
Laboratories
using
BSA/gelatin
for
patient
serum
dilution
used
l%
BSA
as
diluent
here.
1
h
to
overnight
(SRIA
used
overnight
incubation)
at
room
temperature.
Some
laboratories
had
an
additional
step,
first
using
a.p.
goat
anti-human
IgG
or
IgM
in
the
previous
step
and
then
going
to
a
second
step
using
enzyme
labelled
a.p.
sheep
or
rabbit
anti-goat
IgG.
Subsequent
procedures
are
the
same
for
any
ELISA
or
SRIA
technique
a.p.,
affinity
purified.
samples,
and
of
anti-human
antibody
preparations.
The
source
of
antigen
did
not
appear
to
affect
results.
Two
of
the
assays
that
did
not
work
either
used
phospholipid
micelles
or
a
mixture
of
phospholipids
to
coat
microtitre
plates,
but
our
experience
suggests
that
these
procedures
alone
should
not
have
caused
these
assays
to
fail,
and
reasons
for
failure
appear
to
have been
the
use
of
gelatin
both
as
diluent
of standard
sera
and
of
anti-human
antibody
preparations,
and/or
incubations
of
plates
at
370C.
DISCUSSION
The
primary
finding
of
this
co-operative
study
was
that
a
variety
of
ELISA
or
SRIA
methods
can
provide
an
accurate
and
reproducible
measure
of
IgG
aCL
and
IgM
aCL,
over
a
concentration
range
of
about
100
GPL
units
to
approximately
5
GPL
units
for
IgG,
and
from
50
MPL
units
to
approximately
1-6
MPL
units
for
IgM
aCL.
Although
OD
or
ct/min
readings
for
individual
samples
may
vary
from
day
to
day,
the
essentially
linear
relationship
between
logarithm
of
OD
(or
ct/min)
and
logarithm
of
aCL
concentrations
does
not
change
significantly
over
the
range
of
concentrations
encompassed
by
the
seven
standard
samples.
Thus,
by
using
four
to
six
standard
samples
on
each
assay
plate
which
together
cover
a
wide
range
of
IgG
and
IgM
aCL
concentrations,
and
by
assigning
some
'unit'
of
measurement
to
these
standard
samples
related
to
aCL
concentration,
aCL
assays
can
be
standardized
so
that
they
provide
an
estimate
of
aCL
concentration
in
unknown
serum
samples.
Major
stages
of
anti-cardiolipin
assay
E.
N.
Harris
et
al.
220

International
workshop
on
anti-cardiolipin
antibody
test
Determination
of
which
of
the
seven
test
samples
were
positive
was
difficult
only
at
low
IgG
and
IgM
concentrations.
Instead
of
defining
a
'cut-off
point
we
suggest
that
sample
results
be
reported
as
'high',
'medium',
or
'low'
positive.
We
suggest
that
an
IgG
aCL
value
above
80
GPL
units
be
defined
as
'high'
positive.
The
range
15-80
GPL
units
over
which
the
majority
of
valid
assays
were
most
sensitive,
can
be
defined
as
'medium'
positive,
and
levels
below
15
GPL
units
be
defined
as
'low'
positive
(Fig.
la).
For
the
IgM
aCL,
we
suggest
that
levels
above
50
MPL
units
be
defined
'high'
positive,
those
levels
between
6-0
and
50
MPL
units
be
defined
as
'medium'
positive
and
those
with
levels
less
than
6-0
MPL
be
defined
as
'low'
positive
(Fig.
I
b).
This
method
of
reporting
results,
although
vague,
provides
some
objective
means
of
exchanging
information.
The
results
of
this
study
suggest
that
all
laboratories
with
valid
assays
can
correctly
identify
the
'high'
positive
and
'medium'
positive
aCL
samples
and
significant
differences
only
arise
in
reporting
'low'
positive
results.
Although
unable
to
determine
with
accuracy
why
some
assays
seemed
to
provide
'better
results'
than
others,
this
study
was
able
to
pin-point
certain
common
problems
to
assays
that
were
not
valid.
The
use
of
PBS
alone,
PBS-Tween,
or
0-3%
gelatin
as
diluent
of
both
serum
samples
and
anti-
human
antibody,
as
well
as
warming
plates
to
37
C,
were
features
only
of
assays
that
were
not
valid.
Most
laboratories
with
valid
assays
used
10%
fetal
calf
serum
or
10%
adult
bovine
serum
for
blocking
plates,
as
diluent
of
serum
samples
and
as
diluent
of
enzyme-labelled
or
'25l-labelled
antihuman
antibody.
Other
variables
such
as
incubation
time
and
choice
of
anti-human
antibody
may
also
have
affected
the
quality
of
results.
If,
as
some
investigators
currently
believe
(Harris
et
al.,
1985a),
anti-cardiolipin
antibodies
include
sub-populations
of
antiphospholipid
antibodies
with
lupus
anticoagulant
activity,
then
a
standardized
aCL
test
will
be
a
better
instrument
for
detecting
and
measuring
anti-phospholipid
antibodies
than
the
lupus
anticoagulant
(LA)
test.
Significant
variations
in
the
tests
used
to
detect
the
lupus
anticoagulant
make
standardization
and
reliable
quantification
of
results
difficult
(Green
et
al.,
1983).
We
suggest
that
the
method
outlined
in
this
report
for
evaluation
of
the
aCL
test
can,
in
theory,
be
applied
to
evaluation
and
standardization
procedures
for
other
auto-antibody
tests
which
utilize
ELISA
or
SRIA
techniques.
We
wish
to
acknowledge
the
assistance
given
by
Mr
Thomas
Patterson
in
preparing
standard
samples
and
data
processing.
We
wish
to
thank
Mrs
Pauleen
Moss
for
secretarial
assistance.
This
work
was
supported
in
part
by
the
Arthritis
and
Rheumatism
Council
and
by
the
British
SLE
Aid
Group.
PARTICIPANTS
Dr
Vincent
Agnello
and
Dr
Cindy
White
Lahey
Clinic
Medical
Center,
Burlington,
Massachussets,
USA;
Dr
R.
M.
R.
Barnes
and
Dr
P.
Kenton
Royal
Liverpool
Hospital,
Liverpool,
UK;
Dr
Stefano
Bombardieri,
Dr
A.
d'Ascunio
and
Dr
R.
Neri
Istituto
di
Patologia
Medica,
Pisa,
Italy;
Mr
David
Clarke
North
Staffordshire
Royal
Infirmary,
Stoke
on
Trent,
UK;
Dr
Ian
Collins
and
Dr
R.
B.
Clague
University
of
Manchester
Medical
School,
Manchester,
UK;
Dr
Susan
Cowchock
Jefferson
Medical
College,
Philadelphia,
USA;
Dr
L.
Cyna
and
Dr
0.
Meyer
Hopital
Lariboiosiere,
Paris,
France;
Dr
R.
H.
W.
M.
Derksen,
Dr
P.
Hasselaar,
Dr
L.
Blockryl
and
Dr
P.
G.
De
Groot
Academisch
Ziekenhuis,
Utrecht,
Holland;
Dr
Anat
El-Roeiy
Mount
Sinai
Hospital,
Chicago,
Illinois,
USA;
Dr
T.
Exner
and
Dr
Narelle
Taylor
Westmead
Hospital,
Sydney,
Australia;
Dr
Geoffrey
Frampton
Guy's
Hospital,
London,
UK;
Dr
Jennifer
Faux
and
Dr
Margaret
Byron
John
Radcliffe
Hospital,
Oxford,
UK;
Dr
A.
E.
Gharavi
and
Mr
T.
Patterson
Lupus
Research
Laboratory,
St
Thomas's
Hospital,
London,
UK;
Dr
H.
J.
Heine
and
Dr
Sandor
Shapiro
Cardeza
Foundation
for
Hematologic
Research,
Philadelphia,
USA;
Dr
Hilary
Joyce
Dudley
Road
Hospital,
Birmingham,
UK;
Dr
A.
W.
L.
Joss
and
Dr
Malcolm
Steven
Raigmore
Hospital,
Inverness,
UK;
Or
Michael
Lockshin
and
Dr
Tasneem
Qamar
Hospitalfor
Special
Surgery,
New
York,
USA;
Mr
Sozos
Loizou
Hammersmith
Hospital;
London,
UK;
Dr
W.
Lucassen
and
Dr
R.
Smeenk
Department
of
Autoimmune
Diseases,
Central
Laboratory
of
Netherlands,
Amsterdam,
The
Netherlands;
Dr
M.
N.
Madhat
and
Mr
N.
Amos
University
Hospital
of
Wales,
Cardiff,
Wales,
UK;
Dr
Pier
Luigi
Meroni
221

222
E.
N.
Harris
et
al.
and
Dr
Antonio
Brucato
Istituto
Clinica
Medica
II,
Ospedale
Policlinico,
Milan,
Italy;
Dr
J.
Maymo
and
Dr
P.
J.
Maddison
Royal
National
Hospital
for
Rheumatic
Diseases,
Bath,
UK;
Dr
M.
N.
Manoussakis,
Dr
A.
G.
Tzioufas
and
Dr
H.
M.
Moutsopoulos
Department
of
Medicine,
University
of
Ioannina,
Greece;
Dr
Renee
Norberg
The
National
Bacteriological
Laboratory,
Stockholm,
Sweden;
Dr
Angelo
Passaleva
and
Dr
Graziella
Massai
Cattedra
di
Immunologia
Clinica,
Policlinico
di
Careggi,
Firenze,
Italy;
Dr
Eng
Tan
and
Dr
Carol
A.
Penning
Scripps
Clinic
and
Research
Foundation,
La
Jolla,
California,
USA;
Dr
Angela
Tincani,
Dr
Flavio
Allegri,
Dr
Genesio
Balestrieri
and
Dr
Roberto
Cattaneo
Spedali
Civili,
Brescia,
Italy;
Dr
Pamela
Taylor
Department
of
Obstetrics,
University
of
Leeds,
Leeds,
UK,
Dr
Guido
Valesini,
Dr
Mirella
Falco
and
Dr
Rosella
Pastora
Immunogia,
Clinica
Medica
I,
Universita
di
Roma,
Rome,
Italy;
Dr
Wendell
Wilson,
Dr
Myriam
Perez
and
Dr
J.
Michalski
Louisiana
State
University
Medical
Center,
New?
Orleans,
USA.
REFERENCES
BRANCH,
D.W.,
SCOTT,
J.R.,
KODENOUR,
N.K.
&
HERSHGOLD,
E.
(1985)
Obstetric
complications
associated
with
the
lupus
anticoagulant.
New
Engl.
J.
Med.
313,
1322.
COLACO,
C.B.
&
MALE,
D.K.
(1985)
Anti-phospholi-
pid
antibodies
in
syphilis
and
a
thrombotic
subset
of
SLE:
distinct
profiles
of
epitope
specificity.
Clin.
exp.
Immunol.
59,
449.
EDITORIAL
(1985)
Anticardiolipin
antibodies:
a
risk
factor
for
venous
and
arterial
thrombosis.
Lancet
i,
912.
GHARAVI,
A.E.,
HARRIS,
E.N.,
ASHERSON,
R.A.
&
HUGHES,
G.R.V.
(1987)
Anti-cardiolipin
(aCL)
isotypes:
a
study
of
their
clinical
relevance.
Ann.
Rheum.
Dis.
(in
press).
GREEN,
D.,
HOUGHIE,
C.,
KAZMIER,
F.J.,
et
al.,
(1983)
A
report
of
the
working
party
on
acquired
inhibi-
tors
of
coagulation:
studies
of
the
lupus
anticoagu-
lant.
Thromb.
Haemostas.
49,
144.
HARRIS,
E.N.,
GHARAVI,
A.E.M.,
BOEY,
M.L.,
PATEL,
B.M.,
MACKWORTH-YOUNG,
C.G.,
Lolzou,
S.
&
HUGHES,
G.R.V.
(1983)
Anti-cardiolipin
anti-
bodies:
detection
by
radioimmunoassay
and
associ-
ation
with
thrombosis
in
systemic
lupus
erythema-
tosus.
Lancet
ii,
1211.
HARRIS,
E.N.,
GHARAVI,
A.E.
&
HUGHES,
G.R.V.
(1985a)
Anti-phospholipid
antibodies.
Clin.
rheum.
Dis.
11,
591.
HARRIS,
E.N.,
GHARAVI,
A.E.,
TINCANI,
A.,
CHAN,
J.K.H.,
ENGLERT,
H.,
MANTELLI,
P.,
ALLEGRO,
F.,
BALESTRIERI,
G.
&
HUGHES,
G.R.V.
(1985b)
Affi-
nity
purified
anti-cardiolipin
and
anti-DNA
anti-
bodies
J.
clin.
Lab.
Immunol.
17,
155.
HARRIS,
E.N.,
CHAN,
J.K.H.,
ASHERSON,
R.A.,
ABER,
V.R.,
GHARAVI,
A.E.
&
HUGHES,
G.R.V.
(1986)
Thrombosis,
recurrent
fetal
loss,
thrombocytope-
nia:
predictive
value
of
IgG
anti-cardiolipin
anti-
bodies.
Arch.
int.
Med.
(in
press).
HAMSTEN,
A.,
NORBERG,
R.,
BJORKHOLM.,
DE
FAIRE,
U.
&
HOLM,
G.
(1986)
Antibodies
to
cardiolipin
in
young
survivors
of
myocardial
infarction:
an
association
with
recurrent
cardiovascular
events.
Lancet
i,
113.
KOIKE,
T.,
SUEISHI,
M.,
FUNAKI,
H.,
TOMIOKA,
H.
&
YOSHIDA,
S.
(1984)
Anti-phospholipid
antibodies
and
biological
false
positive
serological
tests
for
syphilis
in
patients
with
systemic
lupus
erythemato-
sus.
Clin.
exp.
Immunol.
56,
193.
LOCKSHIN,
M.D.,
DRUZIN,
M.L.,
GOEI,
S.,
QAMAR,
T.,
MAGID,
M.S.,
JOVANOVICv,
L.
&
FERENC,
M.
(1985)
Antibody
to
cardiolipin
as
a
predictor
of
fetal
distress
or
death
in
pregnant
patients
with
systemic
lupus
erythematosus.
New
Engl.
J.
Med.
313,
152.
Loizou,
S.,
MCCREA,
J.D.,
RUDGE,
A.C.,
REYNOLDS,
R.,
BOYLE,
C.C.
&
HARRIS,
E.N.
(1985)
Measure-
ment
of
anti-cardiolipin
antibodies
by
an
enzyme-
linked
immunosorbent
assay
(ELISA).
Standardis-
ation
and
quantitation
of
results.
Clin.
exp.
Immu-
nol.
62,
738.
LUBBE,
W.E.,
BUTLER,
W.S.,
PALMER,
S.J.
&
LIGGINS,
G.C.
(1984)
Lupus
anticoagulant
in
pregnancy.
Br.
J.
Obstet.
Gynaecol.
91,
357.
MEYER,
O.,
CYNA,
L.,
BORDA-IRIARTE,
O.,
JUNGERS,
P.,
PIETTE,
J.C.,
DAUTZENBERG,
M.D.,
DUPUY,
E.
&
RYCKEWAERT,
A.
(1985)
Anticorps
anti-phospholi-
pides,
thromboses
et
maladie
luique:
interet
du
dosage
des
anticorps
anti-cardiolipine
par
la
meth-
ode
ELISA.
Rev.
du
Rheum.
52,
297.
NORBERG,
R.,
GARDLUND,
B.,
THORSTENSSON,
R.,
LIDMAN,
K.
(1984)
Further
immunological
studies
of
sera
containing
anti-mitochondrial
antibodies,
type
MS.
Clin.
exp.
Immunol.
58,
639.
TINCANI,
A.,
MERONI,
P.L.,
BRUCATO,
A.,
ZANUSSI,
C.,
ALLEGRO,
F.,
MANTELLI,
P.,
CATTANCO,
R.
&
BALESTRIERI,
G.
(1985).
Anti-phospholipid
and
anti-mitochrondrial
type
M5
antibodies
in
systemic
lupus
erythematosus.
J.
clin.
exp.
Rheumatol.
3,
321.
