
CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India
ICT India Working Paper #25
Manisha Wadhwa
March 2020

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 2
Table of Contents
Abbreviations ................................................................................................................................................ 4
Abstract ......................................................................................................................................................... 5
Introduction .................................................................................................................................................. 6
Benefits of EHR ............................................................................................................................................. 8
Initiatives by the Government of India ......................................................................................................... 8
EHR Standards ........................................................................................................................................... 8
Goals of EHR Standards ......................................................................................................................... 9
Need for EHR Standards ........................................................................................................................ 9
Other Initiatives ........................................................................................................................................ 9
Electronic Medical Record Adoption Model ............................................................................................... 10
Private Sector Initiatives ............................................................................................................................. 10
Challenges ................................................................................................................................................... 10
International Lessons .................................................................................................................................. 11
EHR and EMR in China ............................................................................................................................ 11
Establishment of Bangladesh National Enterprise Architecture ............................................................ 12
Lifetime Health Record in Malaysia ........................................................................................................ 12
Components & Activities involved in EHR adoption ................................................................................... 12
ICT Infrastructure .................................................................................................................................... 13
Policy & regulations ................................................................................................................................ 13
Standards & interoperability ................................................................................................................... 14
Research, development & education ..................................................................................................... 14
Conclusion ................................................................................................................................................... 14
References .................................................................................................................................................. 14
Annexures ................................................................................................................................................... 16
Annexure 1: Standards at a Glance ......................................................................................................... 16
Annexure 2: List of Supporting / Complimenting Standards .................................................................. 19
Annexure 3: Objectives of National eHealth Authority (NeHA).............................................................. 19

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 3
List of Tables
Table 1: Benefits of EHR ................................................................................................................................ 8
Table 2: Goals of EHR Standards ................................................................................................................... 9
Table 3: Electronic Medical Record Adoption Model (EMRAM) ................................................................. 10
Table 4 : Components and Activities involved in EHR adoption ................................................................. 13
List of Figures
Figure 1: A Simple Electronic Health Record System .................................................................................... 7

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 4
Abbreviations
AHR Automated Health Records
BCC Bangladesh Computer Council
CPR Computer-based Patient Record
DISHA Digital Health Information in Healthcare Security
e-GIF e-Government Interoperability Framework
eHIE electronic health information exchange
EHR Electronic Health Record
EMR Electronic Medical Record
EMRAM Electronic Medical Record Adoption Model
ERNET Education and Research Network
FOSS Free and Open Source
GoB Government of Bangladesh
HIMSS Healthcare Information and Management Systems Society
HISPC Health Information Standards Professional Committee
ICT Information and Communications Technology
IT Information Technology
ITU International Telecommunication Union
LHR Lifetime Health Record
MIS Management Information System
MOH Ministry of Health
MoH&FW Ministry of Health & Family Welfare
NeHA National e-health Authority of India
NITI National Institution for Transforming India
NKN National Knowledge Network
PHR Personal Health Record
SHR Shared Health Record
SN Sankara Nethralaya
WHO World Health Organization

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 5
Abstract
The Information and Communications Technology (ICT) seem to diffuse in almost all the sectors.
ICT has transformed the way the healthcare data is managed. The widespread usage of electronic
devices like computers, tablets, mobile phones along with the availability of high speed internet
have made possible the transition from paper based patient records to electronic records.
Electronic Health Records (EHRs) are real time digital version of patient records. An Electronic
Health Record (EHR) is a comprehensive report of an individual’s overall health. Electronic Health
Records (EHRs) help track patient’s clinical progress, facilitate improved health care decisions and
provide evidence based care.
This is a concept paper based on secondary data from various national and international journals,
government documents, government and private websites. This paper presents a review of
Electronic Health Records (EHRs) and its use in India. The document gives details of initiatives
taken by the government of India in relation to EHRs. Further, the paper discusses the potential
benefits of Electronic Health Records (EHRs). International lessons from other countries like
China, Bangladesh and Malaysia are also discussed. A brief account of Electronic Medical Record
Adoption Model (EMRAM) and private initiatives is also given. Challenges in the way of adoption
of Electronic Health Records (EHRs) in India are discussed in detail. Further, this paper presents
an outline of roadmap for adoption of Electronic Health Records (EHRs) in India.
Keywords: Electronic Health Records, EHR, Information and Communications Technology, ICT,
India

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 6
Introduction
Information and Communications Technology (ICT) has created a paradigm shift in the way
patient clinical data is captured, stored, used and disseminated. Evidently, there has been a
gradual shift from paper based records to electronic records. A number of terms have been used
to describe the move from paper based records to electronic records. Some of these terms are:
Automated Health Records (AHR), Computer-based Patient Record (CPR), Electronic Medical
Record (EMR), and Electronic Health Record (EHR).
Automated Health Records (AHR)
Automated Health Records was the term used for a set of health records stored in the form of
images into a computer(World Health Organization and Regional Office for the Western Pacific
2006). This type of health records were used in early 1990’s when data was stored in the form of
images on optical disk. This helped address problems like those of space and access related to
the traditional paper based records.
Computer-based Patient Record (CPR)
The Computer-based Patient Record (CPR) was used to define a collection of health information
for a single patient, either for a single episode or for extended period of care and this was linked
by a patient identifier(World Health Organization and Regional Office for the Western Pacific
2006). The Computer-based Patient Record (CPR) focused on functions like alerts, orders for
medication and providing integrated patient information from various departments like
pharmacy, laboratory, radiology etc. However, the exchange of information was limited to
inpatient facilities.
Electronic Medical Record (EMR)
The term Electronic Medical Record was used to define an electronic record system used by the
general practitioners to record patient clinical information like identification, prescription,
laboratory test results etc.(World Health Organization and Regional Office for the Western Pacific
2006).
Electronic Health Record (EHR)
Electronic Health Records were first introduced in 1960s. However, it is in the year 2009 when
the “Health Information Technology for Economic and Clinical Health Act” was passed and
around $30 billion was allocated for the adoption of the Electronic Health Records and its
implementation on a large scale.
“An Electronic Health Record (EHR) is defined as a collection of various medical records that get
generated during any clinical encounter or events”(Vikaspedia 2019). In USA EHR is defined as:
“The electronic health record includes all information contained in a traditional health record
including a patient’s health profile, behavioural and environmental information. As well as
content the EHR also includes the dimension of time, which allows for the inclusion of information

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 7
across multiple episodes and providers, which will ultimately evolve into a lifetime record”(World
Health Organization and Regional Office for the Western Pacific 2006).
EHR refers to a real time, unique longitudinal health record of a single individual containing his
or her entire personal health information including medical details like history, medical
examination, diagnosis, laboratory results, allergies, details of immunization, treatment etc. in a
digital format. The information is entered electronically by the healthcare providers over the
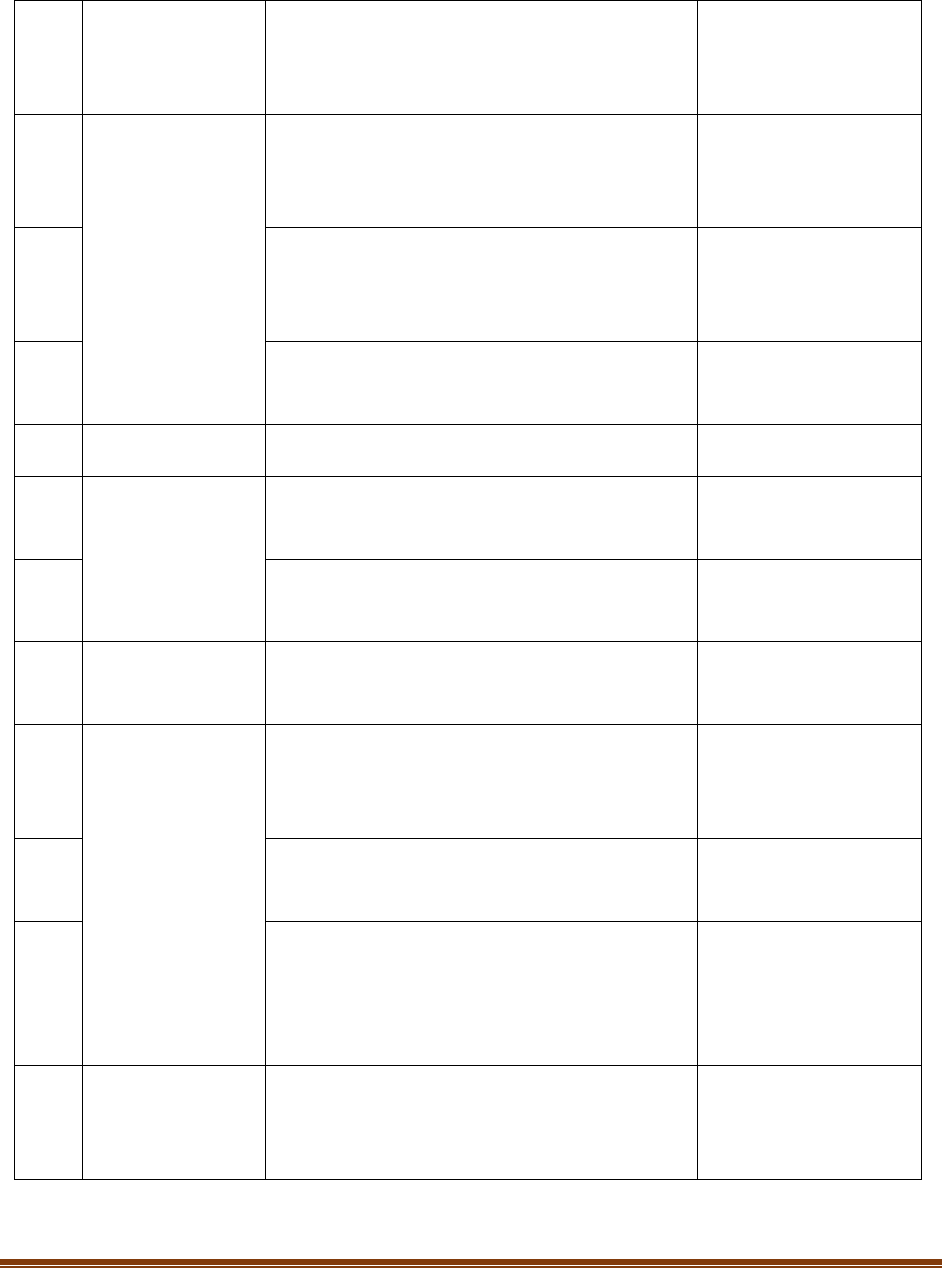
course of his/her lifetime. A simple Electronic Health Record System is shown in the Figure
1(World Health Organization and Regional Office for the Western Pacific 2006). This includes
details from some departments within the Institution. Depending on the scope of the EHR system
patient details from other departments can also be included.
Figure 1: A Simple Electronic Health Record System
Source: Electronic Health Records: A Manual for Developing Countries by WHO
It is important to note that Electronic Health Records differ from Electronic Medical Records.
Electronic Medical Record is a digital version of paper record related to patient’s medical history
recorded in a clinician’s office. Electronic Medical Records are not designed to be shared outside
EHR
Patient ID
and
Registration
details
Lab/Haem/
Pathology/
Biochem/
Radiology
Scanned
documents
/previous
medical
records
Disease
Classification
and
Indexing
Clinical data
treatment
orders/result
OPD visits

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 8
an individual clinical practice. On the other hand, an Electronic Health Record is a comprehensive
report of an individual’s overall health. Electronic Health Records is a collection of various medical
records. It is designed with an intention to be shared outside the healthcare organization.
However, some people still use the terms “Electronic Medical Record (EMR)” and “Electronic
Health Record (EHR)” interchangeably.
Benefits of EHR
The benefits of EHRs are manifold. Some of them are given in Table1.
Table 1: Benefits of EHR
1
EHRs ensure that patient records are easily accessible from anywhere and at any time
2
EHRs can be stored easily, in less space and for indefinite time
3
Being in electronic format, it reduces the number of records lost
4
EHRs improves the quality of patient records and are cost-effective
5
EHRs help track patient’s clinical progress and improve patient compliance
6
EHR gives a summary report of the various clinical encounters in a person’s lifetime
7
EHRs help improve the accuracy and speed of diagnosis, and avoid repeating unnecessary
tests
8
EHRs can be transferred easily within and across healthcare facilities
9
EHRs are easy to update and can be made available to be used by multiple users at single
point of time
10
EHRs allow keeping back up of patient records at a very low cost
11
EHRs facilitate improved health care decisions and provide evidence based care
12
EHRs can be used for research purposes
Initiatives by the Government of India
EHR Standards
The Ministry of Health & Family Welfare (MoH&FW) first came out with standards for Electronic
Health Record (EHR) for India in Sept 2013. These were based on the recommendations made
by the EMR Standards Committee constituted under the Ministry of Health & Family Welfare
(MoH&FW)(Ozair et al. 2015). The document contained recommendations for developing a
uniform system for EHRs creation and maintenance by healthcare providers. These standards
were revised and were notified in December 2016(Mantri 2016). See Annexure 1 for a quick
reference to the MoH&FW EHR Standards Version 2016. List of supporting/complimenting
standards is given in Annexure 2.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 9
Goals of EHR Standards
The goals of EHR Standards are enlisted in Table2(Mantri 2016; Vikaspedia 2019).
Table 2: Goals of EHR Standards
1
Promote interoperability and where necessary be specific about certain content exchange
and vocabulary standards to establish a path forward toward semantic interoperability
2
Support the evolution and timely maintenance of adopted standards
3
Promote technical innovation using adopted standards
4
Encourage participation and adoption by all vendors and stakeholders
5
Keep implementation costs as low as reasonably possible
6
Consider best practices, experiences, policies and frameworks
7
To the extent possible, adopt standards that are modular and not interdependent.
Need for EHR Standards
➢ Without standards, a lifelong interoperable medical record is hardly interoperable(Mantri 2016)
Other Initiatives
The following are some of the other steps taken by the Government of India:
➢ National e-health Authority of India (NeHA) was proposed be set up in the year 2015 under the
Ministry of Health & Family Welfare (MoH&FW) with the goal to establish the e-Health ecosystem
in India(Ministry of Health and Family Welfare, Government of India 2017). One of the objectives
of the NeHA is “To lay down data management, privacy and security policies, guidelines and health
records of patients in accordance with statutory provisions”(Ministry of Health and Family
Welfare, Government of India 2017). All the objectives of NeHA are outlined in the Annexure 3.
➢ The Ministry of Health & Family Welfare (MoH&FW) have put forward a draft for the
establishment of an Act called Digital Health Information in Healthcare Security (DISHA) of
parliament as a statutory body for promotion or adoption of e-Health standards(Bhavaraju 2018).
Digital Health Information in Healthcare Security Act (2018) is “An Act to provide for
establishment of National and State eHealth Authorities and Health Information Exchanges; to
standardize and regulate the processes related to collection, storing, transmission and use of
digital health data; and to ensure reliability, data privacy, confidentiality and security of digital
health data and such other matters related and incidental thereto”(Ministry of Health & Family
Welfare, and Government of India 2018).
➢ “National Health Stack” a visionary digital framework is proposed by the National Institution for
Transforming India (NITI Aayog) with an aim to create digital health records for all the citizens of
India by the year 2022(NITI Aayog 2018).

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 10
Electronic Medical Record Adoption Model
Electronic Medical Record Adoption Model (EMRAM) was created in the year 2005 by Healthcare
Information and Management Systems Society (HIMSS)
1
(HIMSS Analytics 2017). EMRAM is an
eight stage (0-7) model which measures the level of adoption and utilization of electronic medical
record (EMR) functions in any healthcare organization. This tool helps healthcare organizations
to measure their progress in EMR adoption compared to other healthcare organizations in the
world. Electronic Medical Record Adoption Model (EMRAM) is shown in Table 3. For details see
Annexure 4.
Table 3: Electronic Medical Record Adoption Model (EMRAM)
Stage 7
Complete EMR; External HIE; Data Analytics, Governance, Disaster Recovery,
Privacy And Security
Stage 6
Technology Enabled Medication, Blood Products, And Human Milk
Administration; Risk Reporting; Full CDS
Stage 5
Physician Documentation Using Structured Templates; Intrusion/ Device
Protection
Stage 4
CPOE With CDS; Nursing And Allied Health Documentation; Basic Business
Continuity
Stage 3
Nursing And Allied Health Documentation; EMAR; Role-Based Security
Stage 2
CDR; Internal Interoperability; Basic Security
Stage 1
Ancillaries - Laboratory, Pharmacy, And Radiology/ Cardiology Information
Systems; PACS; Digital Non-DICOM Image Management
Stage 0
All Three Ancillaries (Laboratory, Pharmacy, And Radiology) Not Installed
Private Sector Initiatives
Electronic Health Records have been implemented by some of the private hospitals in India. Max
Healthcare initiated adoption of EHRs in the year 2009 and has achieved Stage 6 level of EMR
adoption model. Max Healthcare in East Wing and West Wing, Saket in New Delhi achieved
recognition award for this in the year 2012(Srivastava 2016). Apollo group of Hospitals have also
implemented EHR and have achieved stage 6 in four hospitals located in Chennai, Aynambakkam,
Nandanam, and Jubilee Hills in Hyderabad(Srivastava 2016). Other Hospitals like Sankara
Nethralaya (SN), Fortis etc. have also implemented EHRs. Though, private sector hospitals seem
to adopt EHRs system, but the information is hardly exchanged between hospitals.
Challenges
The development and implementation of EHRs involve lots of challenges. It requires adequate
funding, sufficient and well trained manpower including experts from different areas like doctors,
1
HIMSS Analytics® is a global healthcare IT market intelligence, research and standards organization
assisting clientele in both healthcare delivery and healthcare technology solutions business
development to make lasting improvements in efficiency and performance.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 11
IT experts, health consultants, educators etc. Keeping patient records secure is one of the key
challenges in the implementation of EHRs. There are concerns related to the misuse of the
database and threat to the cyber-security. In order to ensure the privacy and confidentiality of
the patient’s record, access to data should be given only to the authorized users. Some of the
measures like password protected data, cloud storage and encryption can address issues related
to security of the EHRs. For data integrity, security measures like antivirus software, firewalls etc.
should be incorporated in use.
Designing a user friendly interface is another challenging task. Poorly designed interface may lead
to reduced time efficiency, poor quality of health care delivery and can become a threat to the
patient’s safety as well. Acceptance of EHR by the doctors is also perceived as a barrier. This is
due to the extra time that doctor spends in entering data electronically which otherwise they can
spend in treating the patients. The idea of introducing accountability by the use of EHRs, financial
and administrative liabilities are some of the other things being resisted by the doctors.
Theft of Medical Identity is also becoming a growing concern. A person may access and use
someone else identifiable information illegally to get the medical services for the ailment. Lack
of computer literacy among the healthcare professionals, lack of uniformity in the EHR Software,
infrastructural demands, lack of synergy among the health care providers to use the EHR system,
poor management practices, lack of awareness of protocols related to security of health
information, lack of common understanding between the software development team and the
healthcare team, communication silos within the healthcare system, and electronic monitor of
data not being a mandatory requirement are some of the other challenges in the way of
successful deployment of EHRs in India.
International Lessons
EHR and EMR in China
Though regional EHR systems began to develop in China in the year 2002, the major efforts
started in the year 2005(Gao et al. 2013). In 2005, the 16th Communist Party Central Committee
made recommendation for the 11th Five-Year Plan12, directing the establishment of EHR and
EMR systems in the country. In 2006, Health Information Standards Professional Committee
(HISPC) was established under the Ministry of Health (MOH), China for creating standards related
to EHR and EMR. In 2009, MOH, China published first series of standards and specifications
related to Health Records. By the year 2011, 120 EHR systems were successfully established
across the country. For the establishment of EHR and EMR systems, China learnt from the
experiences of United States and Australia. China adopted US HL7 Standard for the establishment
of EMR systems. To establish a national EHR System, China follows Australia’s three stage
approach (pilot stage, regional EHR systems, National EHR system). “The Minister of MOH
declared on Feb 27, 2012 that 900 million residents had created their health records, accounting
for 66% of the national population, and more than 50% of residents had created their ehealth
records”(Gao et al. 2013). In the year 2014, 50% tertiary hospitals, 30% Community Health

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 12
Centres in Urban areas and 20% hospitals in rural areas successfully established their own EHR
system in China(Parikh 2015). It is expected that by the year 2020, 80% tertiary hospitals, 50%
Community Health Centres in Urban areas and 50% hospitals in rural areas would established
their own EHR system in China(Parikh 2015). Governments at all the levels in China are working
on sharing data and clinical services among communities which are geographically dispersed
through Regional Healthcare Information Networks (RHINs) by utilizing data centres and
telecommunication networks. Efforts are under way to link EMR Systems with EHR systems
through Health Cards.
Establishment of Bangladesh National Enterprise Architecture
To realize the vision and mission of establishing “Digital Bangladesh” by the year 2021 through
establishment of transparent, efficient and citizen centric public services, termed as “e-services”
through ICT, "National Enterprise Architecture" and “e-Government Interoperability Framework
(e-GIF)” has been one of the key projects undertaken by the Government of Bangladesh
(GoB)(International Telecommunication Union (ITU) 2016). The project objective was to develop
systems, structures, technologies, strategies and provide an enabling environment across the
Government via improved management of asset, increased interoperability and reduced risks
and procurement costs. The goal of the system is to improve the quality of service delivery by
health care providers. The rural citizens, who form majority (around 76%) of the Bangladesh’
population were first to be included in the system(Zishan et al. 2019). The project initiated in the
year 2014 and was completed by the year 2016. It was implemented by the Bangladesh Computer
Council (BCC), an apex body of the GoB. The government of Bangladesh uses three types of
softwares, namely DHIS-2 for public health services through health facilities all over the country,
OpenMRS for hospital services and HRM for human resource management(Additional Director
General and Director of Management Information System (MIS), DGHS 2015). The government
plans to develop electronic shared health records (SHR) systems which will integrate DHIS-2,
OpenMRS and HRM in national level eHealth enterprise architecture (eHEA), to exchange data
via eHIE (electronic health information exchange)(Additional Director General and Director of
Management Information System (MIS), DGHS 2015).
Lifetime Health Record in Malaysia
Lifetime Health Record (LHR) and Services is an initiative by the Government of Malaysia(Zishan
et al. 2019). Under this plan, records for each individual will be maintained throughout his life
time, starting from the time of his/her first consultation with the service provider until each time
he/she visits the service provider.
Components & Activities involved in EHR adoption
Srivastava in his paper on “Adoption of Electronic Health Records: A Roadmap for India” clearly
outlines four key components that are needed to adopt EHR at the national level (Srivastava
2016). Table 4 enlist these components and the underlying activities in each.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 13
Table 4 : Components and Activities involved in EHR adoption
S.No.
Component
Activities
1
ICT Infrastructure
Creation of basic ICT Infrastructure
Creation of national secure health net
Creation of storage and exchange infrastructure
Use of free and open source software
Use of personal health record system
2
Policy & regulations
National Health IT Policy
Protection of Privacy
Sharing of health information
Use of health information
Liability of technical failures
3
Standards & interoperability
Establishment of agency for health IT standards
Use of unique patient identity
Conformation of testing facility
Support for adoption of standards
Guidelines for health IT solutions
4
Research, development &
education
Research & development in health IT
Human resource development
Development of online courseware
Dissemination of best practices
International collaboration
ICT Infrastructure
In order to establish EHR system at the national level, the first pre-requisite is to have appropriate
ICT infrastructure in place. At present, only major hospitals in India have ICT infrastructure for
the delivery of healthcare services. It is needed that all the public healthcare facilities across the
nation have basic ICT equipments in place. Also, to ensure that information exchange is secure
and reliable, appropriate communication networks should be established using the existing ones
like NKN, ERNET etc. Further, it is required to take an approach of establishing free and open
source (FOSS) EMR system. This will ensure that private healthcare facilities which handle a huge
burden of patients can provide relevant inputs and support. Also, establishing a personal health
record (PHR) system can facilitate easy adoption of EHR. PHR system will help doctors an easy
access to the basic patient information like demographics, medical history etc.
Policy & regulations
A National Health IT policy needs to be formulated which will ensure that efforts are not
duplicated and systems are interoperable. Regulations to protect the confidentiality of the
patient data are also needed. Laws are required to ensure that information shared electronically
by the healthcare providers is in the interest of patients. A well-defined procedure must be
defined under the legislation to use the clinical information of the patients for decision making
purposes. Regulations should define the responsibilities of all the stakeholders involved to ensure

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 14
timely delivery of services. This will also help in addressing liabilities in case of technical issues
and failure.
Standards & interoperability
Though the Ministry of Health & Family Welfare (MoH&FW) has put forward the EHR standards,
but there is a need of an agency to regularly update these standards and to extend necessary
technical support needed for its implementation. It is recommended to use unique ID like
Aadhaar number for each patient’s identification and for tracking his/her clinical progress. The
government should put forward an agency to verify and ensure that the IT solutions developed
are interoperable. Guidelines should be developed for providing solutions in cases where it is not
possible to follow the EHR standards.
Research, development & education
Research & Development related to use of EHRs should be promoted. This is needed to
continuously improve the quality of EHRs, reduce its deployment cost and also to facilitate
innovations. A well trained human resource in the field of Health IT should be prepared.
Developing e-courses to facilitate learning related to EHRs will be helpful. An agency is needed
to collect and share information related to EHRs. Further, International collaborations and their
expertise can be useful for the deployment of EHRs in India.
Conclusion
To conclude, the development and implementation of Electronic Health Records in India are still
in the fragmented stages. It is important to focus on following broad issues if this initiative have
to succeed on scale: 1) proper training of doctors and other healthcare professionals to use EHR
effectively; 2) a much higher level of public-private partnerships is needed; 3) appropriate ICT
infrastructure should be in place; 4) working towards standardizing EHRs; 5) a National Health IT
policy needs to be formulated; 6) an efficient management structure to deploy EHR should be in
place; 7) efforts should be made to sensitize healthcare workers related to the importance of
EHRs; 8) synergy between software development team and healthcare delivery team is required;
9) incorporating voice-based and writing based inputs into the EHR System should be explored;
and 10) research & development related to the use of EHRs should be promoted.
References
Additional Director General and Director of Management Information System (MIS), DGHS.
2015. “Health Sector Demonstrates the Incredible Power of the System.” 2015.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 15
https://www.thedailystar.net/supplements/24th-anniversary-the-daily-star-part-2/health-
sector-demonstrates-the-incredible-power.
Bhavaraju, RS. 2018. “From Subconscious to Conscious to Artificial Intelligence: A Focus on
Electronic Health Records” 66 (5): 1270–75.
Gao, Xiangzhu, Jun Xu, Golam Sorwar, and Peter Croll. 2013. “Implementation of E-Health
Record Systems and E-Medical Record Systems in China.” The International Technology
Management Review 3 (2): 127. https://doi.org/10.2991/itmr.2013.3.2.6.
HIMSS Analytics. 2017. “Electronic Medical Record Adoption Model.” 2017.
https://www.himssanalytics.org/emram.
International Telecommunication Union (ITU). 2016. “Establishment of Bangladesh National
Enterprise Architecture.” 2016.
https://www.itu.int/net4/wsis/archive/stocktaking/Project/Details?projectId=1515593078.
Mantri, Manisha. 2016. “Electronic Health Record (EHR) Standards for India (2016),” 57.
Ministry of Health & Family Welfare, and Government of India. 2018. “Digital Information
Security in Healthcare, Act [Draft for Public Consultation].”
https://www.nhp.gov.in/NHPfiles/R_4179_1521627488625_0.pdf.
Ministry of Health and Family Welfare, Government of India. 2017. “National EHealth Authority
(NeHA).” 2017. https://www.nhp.gov.in/national_eHealth_authority_neha_mtl.
NITI Aayog. 2018. “National Health Stack -Strategy and Approach.”
http://niti.gov.in/writereaddata/files/document_publication/NHS-Strategy-and-Approach-
Document-for-consultation.pdf.
Ozair, FF, N Jamshed, A Sharma, and P Aggarwal. 2015. “Ethical Issues in Electronic Health
Records: A General Overview.” Perspect Clin Res 6 (2): 73–76.
Parikh, Harsh. 2015. “Overview Of EHR Systems In BRIC Nations.” 2015.
https://www.clinicalleader.com/doc/overview-of-ehr-systems-in-bric-nations-0001.
Srivastava, Sunil Kumar. 2016. “Adoption of Electronic Health Records: A Roadmap for India.”
Healthcare Informatics Research 22 (4): 261. https://doi.org/10.4258/hir.2016.22.4.261.
Vikaspedia. 2019. “Electronic Health Record Standards for India.” 2019.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 16
http://vikaspedia.in/health/nrhm/national-health-policies/electronic-health-record-standards-
for-india.
World Health Organization, and Regional Office for the Western Pacific. 2006. Electronic Health
Records: A Manual for Developing Countries. Manila: World Health Organization Western
Pacific Region. http://books.google.com/books?id=6UchAQAAMAAJ.
Zishan, Saniat Rahman, Chowdhury Akram Hossain, Mohamad Afendee Mohamed, and
Maryam Sharun. 2019. “The Scenario of E-Health Systems in Developing Countries (Bangladesh
and Malaysia)” 8 (1): 6.
Annexures
Annexure 1: Standards at a Glance
S.No.
Type
Standard Name
Intended Purpose
1
Identification &
Demographics
ISO/TS 22220:2011 Health Informatics –
Identification of Subjects of Health Care
Basic identity details
of patient
2
MDDS – Demographic (Person Identification
and Land Region Codification) version 1.1
Complete
demographic for
interoperability with
E-Governance systems
3
Patient Identifiers
UIDAI Aadhaar
Preferable identifier
where available
4
Local Identifier
Identifier given within
institution / clinic /lab
5
Government Issued Photo Identity Card
Number
Identifier used in
conjunction with local
in absence of Aadhaar
6
Architecture
Requirements
ISO 18308:2011 Health Informatics –
Requirements for an Electronic Health Record
Architecture
System architectural
Requirements
CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 17
7
Functional
Requirements
ISO/HL7 10781:2015 Health Informatics - HL7
Electronic Health Records-System Functional
Model Release 2 (EHR FM)
System functional
requirements
8
Reference Model
and Composition
ISO 13940 Health informatics - System of
Concepts to Support Continuity of Care
Concepts for care,
actors, activities,
processes, etc.
9
ISO 13606 Health informatics - Electronic
Health Record Communication (Part 1
through 3)
Information model
architecture and
communication
10
openEHR Foundation Models Release 1.0.2
Structural definition
and composition
11
Terminology
SNOMED Clinical Terms (SNOMED CT)
Primary terminology
12
Coding System
Logical Observation Identifiers Names and
Codes (LOINC)
Test, measurement,
observations
13
WHO Family of International Classifications
(WHOFIC) including ICD, ICF, ICHI, ICD-O
Classification and
reporting
14
Imaging
Digital Imaging and Communications in
Medicine (DICOM) PS3.0-2015
Image, waveform,
audio/video
15
Scanned or
Captured Records
JPEG lossy (or lossless) with size and
resolution not less than 1024px x 768px at
300dpi
Image capture format
16
ISO/IEC 14496 - Coding of Audio-Visual
Objects
Audio/Video capture
format
17
ISO 19005-2 Document Management –
Electronic Document File Format for Long-
Term Preservation - Part 2: Use of ISO 32000-
1 (PDF/A-2)
Scanned documents
format
18
Data Exchange
ANSI/HL7 V2.8.2-2015 HL7 Standard Version
2.8.2 - An Application Protocol for Electronic
Data Exchange in Healthcare Environments
Event/Message
exchange

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 18
19
ASTM/HL7 CCD Release 1 (basis standard
ISO/HL7 27932:2009)
Summary Records
exchange
20
ISO 13606-5:2010 Health informatics –
Electronic Health Record Communication -
Part 5: Interface Specification
EHR archetypes
exchange [Also, refer
to openEHR Service
Model specification]
21
DICOM PS3.0-2015 (using DIMSE services &
Part-10 media/files)
Imaging/Waveform
Exchange
22
Other Relevant
Standards
Bureau of Indian Standards and its MHD-17
Committee
Standards
Development
Organizations (SDOs)
23
ISO TC 215 set of standards
24
IEEE/NEMA/CE standards for physical systems
and interfaces
25
Discharge/
Treatment
Summary
Medical Council of India (MCI) under
regulation 3.1 of Ethics
Composition as
prescribed
26
E-Prescription
Pharmacy Practice Regulations, 2015
Notification No. 14-148/ 2012- PCI as
specified by Pharmacy Council of India
Composition as
prescribed
27
Personal
Healthcare and
medical Device
Interface
IEEE 11073 health informatics standards and
related ISO standards for medical devices
Device interfacing
28
Data Privacy and
Security
ISO/TS 14441:2013 Health Informatics –
Security & Privacy Requirements of EHR
Systems for Use in Conformity Assessment
Basis security and
privacy requirements
29
Information
Security
Management
ISO/DIS 27799 Health informatics –
Information Security Management in Health
using ISO/IEC 27002
Overall information
security management
30
Privilege
Management
ISO 22600:2014 Health informatics – Privilege
Management and Access Control (Part 1
through 3)
Access control

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 19
and Access
Control
31
Audit Trail and
Logs
ISO 27789:2013 Health informatics - Audit
trails for Electronic Health Records
Audit trail
32
Data Integrity
Secure Hash Algorithm (SHA) used must be
SHA-256 or higher
Data Hashing
33
Data Encryption
Minimum 256-bits key length
Encryption key
34
HTTPS, SSL v3.0, and TLS v1.2
Encrypted connection
35
Digital Certificate
ISO 17090 Health informatics - Public Key
Infrastructure (Part 1 through 5)
Digital certificates use
and management
Annexure 2: List of Supporting / Complimenting Standards
S.No.
Standard
Description
1
ISO 12967:2009
Health Informatics - Service Architecture (Parts 1 - 3)
2
ISO 13972:2015
Health Informatics - Detailed Clinical Models, Characteristics
and Processes
3
ISO 20301:2014
Health Informatics - Health Cards - General Characteristics
4
ISO 21090:2011
Health Informatics - Harmonized Data Types for Information
Interchange
5
ISO 8601:2004
Data elements and Interchange Formats - Information
Interchange -Representation of Dates and Times
6
ISO 13119:2012
Health Informatics - Clinical Knowledge Resources - Metadata
7
ISO 22857:2013
Health Informatics – Guidelines on Data Protection to
Facilitate Trans-Border Flows of Personal Health Data
8
ISO 21549-1:2013
Health Informatics — Patient Healthcard Data — Part 1:
General Structure
9
ISO TS 14265:2011
Classification of Purposes for Processing Personal Health
Information
10
ISO TS 27527:2010
Health Informatics – Provider Identification
Annexure 3: Objectives of National eHealth Authority (NeHA)
S.No.
Objectives
1
To formulate “National eHealth Policy and Strategy” for coordinated eHealth adoption in
the country

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 20
2
To oversee orderly evolution of eHealth initiatives (state and nationwide) and to guide
adoption of eHealth at various levels and in different geographical and health system areas
3
To promote setting up of state health records repositories and health information
exchanges (HIEs) to facilitate interoperability
4
To formulate and manage all health informatics standards for India
5
To lay down data management, privacy and security policies, guidelines and health records
of patients in accordance with statutory provisions
6
To enforce the laws and regulations relating to the privacy, confidentiality, and security of
the patient's health information and records
7
To coordinate efforts across departments and ministries, and liaise with other related
policy/regulatory groups to ensure consistency and coherence
8
To help enable ecosystem that involves stakeholders to improve care delivery and health
outcomes
9
To map continuous evolution of the eHealth landscape and take on new functions as
needed
Annexure 4: Electronic Medical Record Adoption Model (EMRAM)
Stage 7
Complete EMR; External HIE;
Data Analytics, Governance,
Disaster Recovery, Privacy And
Security
The hospital no longer uses paper charts to
deliver and manage patient care and has a
mixture of discrete data, document images,
and medical images within its EMR
environment.
Data warehousing is being used to analyze
patterns of clinical data to improve quality of
care, patient safety, and care delivery
efficiency.
Clinical information can be readily shared via
standardized electronic transactions (i.e.,
CCD) with all entities that are authorized to
treat the patient, or a health information
exchange (i.e., other non-associated
hospitals, outpatient clinics, sub-acute
environments, employers, payers and
patients in a data sharing environment).
The hospital demonstrates
summary data continuity for all hospital
services (e.g., inpatient, outpatient, ED, and
with any owned or managed outpatient
clinics).
Physician documentation and CPOE has
reached 90% (excluding the ED), and the
closed-loop processes have reached 95%
(excluding the ED).

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 21
Stage 6
Technology Enabled Medication,
Blood Products, And Human Milk
Administration; Risk Reporting;
Full CDS
Technology is used to achieve a closed-loop
process for administering medications, blood
products, and human milk, and for blood
specimen collection and tracking. These
closed-loop processes are fully implemented
in 50 percent of the hospital. Capability must
be in use in the ED, but ED is excluded from
50% rule.
The eMAR and technology in use are
implemented and integrated with CPOE,
pharmacy, and laboratory systems to
maximize safe point-of-care processes and
results.
A more advanced level of CDS provides for
the “five rights” of medication
administration and other 'rights' for blood
product, and human milk administrations
and blood specimen processing.
At least one example of a more advanced
level of CDS provides guidance triggered by
physician documentation related to
protocols and outcomes in the form of
variance and compliance alerts (e.g., VTE risk
assessment triggers the appropriate VTE
protocol recommendation).
Mobile/portable device security policy and
practices are applied to user-owned devices.
Hospital conducts annual security risk
assessments and report is provided to a
governing authority for action.
Stage 5
Physician Documentation Using
Structured Templates; Intrusion/
Device Protection
Full physician documentation (e.g., progress
notes, consult notes, discharge summaries,
problem/diagnosis list, etc.) with structured
templates and discrete data is implemented
for at least 50 percent of the hospital.
Capability must be in use in the ED, but ED is
excluded from 50% rule.
Hospital can track and report on the
timeliness of nurse order/task completion.
Intrusion prevention system is in use to not
only detect possible intrusions, but also
prevent intrusions. Hospital-owned portable
devices are recognized and properly
authorized to operate on the network, and
can be wiped remotely if lost or stolen.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 22
Stage 4
CPOE With CDS; Nursing And
Allied Health Documentation;
Basic Business Continuity
50 percent of all medical orders are placed
using Computerized Practitioner Order Entry
(CPOE) by any clinician licensed to create
orders. CPOE is supported by a clinical
decision support (CDS) rules engine for
rudimentary conflict checking, and orders
are added to the nursing and CDR
environment.
CPOE is in use in the Emergency
Department, but not counted in the 50%
rule.
Nursing/allied health professional
documentation has reached 90% (excluding
the ED).
Where publicly available, clinicians have
access to a national or regional patient
database to support decision making (e.g.,
medications, images, immunizations, lab
results, etc.).
During EMR downtimes, clinicians have
access to patient allergies, problem/
diagnosis list, medications, and lab results.
Network intrusion detection system in place
to detect possible network intrusions.
Nurses are supported by a second level of
CDS capabilities related to evidence-based
medicine protocols (e.g., risk assessment
scores trigger recommended nursing tasks).
Stage 3
Nursing And Allied Health
Documentation; EMAR; Role-
Based Security
50 percent of nursing/allied health
professional documentation (e.g., vital signs,
flowsheets, nursing notes, nursing tasks,
care plans) is implemented and integrated
with the CDR (hospital defines formula).
Capability must be in use in the ED, but ED is
excluded from 50% rule. The Electronic
Medication Administration Record
application (eMAR) is implemented.
Role-based access control (RBAC) is
implemented.
Stage 2
CDR; Internal Interoperability;
Basic Security
Major ancillary clinical systems are enabled
with internal interoperability feeding data to
a single clinical data repository (CDR) or fully
integrated data stores that provide seamless
clinician access from a single user interface
for reviewing all orders, results, and radiology
and cardiology images.

CSD Working Paper Series: Towards a New Indian Model of Information and Communications
Technology-Led Growth and Development
Electronic Health Records in India Page 23
The CDR/data stores contain a controlled
medical vocabulary and order verification is
supported by a clinical decision support (CDS)
rules engine for rudimentary conflict
checking.
Information from document imaging systems
may be linked to the CDR at this stage
Basic security policies and capabilities
addressing physical access, acceptable use,
mobile security, encryption, antivirus/anti-
malware, and data destruction.
Stage 1
Ancillaries - Laboratory,
Pharmacy, And Radiology/
Cardiology Information Systems;
PACS; Digital Non-DICOM Image
Management
All three major ancillary clinical systems are
installed (i.e., pharmacy, laboratory, and
radiology).
A full complement of radiology and
cardiology PACS systems provides medical
images to physicians via an intranet and
displaces all film-based images. Patient-
centric storage of non-DICOM images is also
available.
Stage 0
All Three Ancillaries Not Installed
The organization has not installed all of the
three key ancillary department systems
(laboratory, pharmacy, and radiology).
