
Accreditation Council for Graduate Medical Education
Guide to the
Common Program Requirements
(
Residency)
(Version 4.1; updated March 2024)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
1

Accreditation Council for Graduate Medical Education
ACGME Mission
The Mission of the ACGME is to improve health care and population health by assessing and
enhancing the quality of resident and fellow physicians’ education through advancements in
accreditation and education.
ACGME Vision
We envision a health care system in which the Quadruple Aim* has been realized. We aspire to
advance a transformed system of graduate medical education with global reach that is:
• Compet
ency-based with customized professional development and identity formation for
all physicians;
• Led by inspirational faculty role models overseeing supervised, humanistic, clinical
educational experiences;
• Immersed in evidence-based, data-driven, clinical learning and care environments
defined by excellence in clinical care, safety, cost-effectiveness, professionalism, and
diversity, equity, and inclusion;
• Located in health care delivery systems equitably meeting local and regional community
needs; and,
• Graduating residents and fellows who strive for continuous mastery and altruistic
professionalism throughout their careers, placing the needs of patients and their
communities first.
* The Quad
ruple Aim simultaneously improves patient experience of care, population health,
and health care practitioner work life, while lowering per capita cost.
ACGME Values
• Honesty and Integrity
• Accountability and Transparency
• Equity and Fairness
• Diversity and Inclusion
• Excellence and Innovation
• Stewardship and Service
• Leadership and Collaboration
• Engagement of Stakeholders
©2024 Accreditation Council for Graduate Medical Education (ACGME)
2

Int.A, B and C Introduction 6
I.A. and I.A.1. Oversight and Sponsoring Institution 9
I.B.1. Participating Sites 11
I.B.2. and I.B.3. Program Letters of Agreement with AAMC Template 14
I.B.4. Participating Sites Addition and Deletion 18
I.C. Diversity and Inclusion in Workforce Recruitment and Retention 23
I.D.1. - I.D.3. Resources, Sleep Facilities, References, Security 27
I.E. Presence of Other Learners 30
II.A.1.a) and
II.A.1.a).(1)
Program Director Appointment 33
II.A.1.b) Program Director Continuity of Leadership 37
II.A.2. Program Director Support for Administration of Program 39
II.A.3. and
II.A.3.a) - c)
Qualifications of Program Director 42
II.A.4.a).(1) - (5)
Program Director Responsibilities - Professionalism and
Learning Environment
49
II.A.4.a).(6)
Program Director Responsibilities - Submit Accurate and
Complete Information
55
II.A.4.a).(7) -
(9).(a)
Program Director Responsibilities - Raising Concerns and
Sponsoring Institution Policies
62
II.A.4.a).(10) -
(11)
Program Director Documentation and Verification of Resident
Education/VGMET
65
II.A.4.a).(12) Resident Eligibility for Specialty Board Examination 68
II.B.1. and
II.B.2.a) - f)
Faculty Responsibilities 72
II.B.3.a) - b) Faculty Qualifications 76
II.B.4. Core Faculty 82
II.C. and II.D. Coordinator and Other Personnel 87
III.A.1. – III.A.3. Resident Appointments 91
III.B. Resident Complement 105
III.C. Resident Transfers 108
IV.A.1. – IV.A.5. Educational Program Curriculum 112
IV.B. ACGME Competencies 118
IV.B.1.a) Professionalism 122
IV.B.1.b) Patient Care and Procedural Skills 126
IV.B.1.c) Medical Knowledge 128
IV.B.1.d) Practice-based Learning and Improvement 130
IV.B.1.e) Interpersonal and Communication Skills 133
IV.B.1.f) Systems-based Practice 137
©2024 Accreditation Council for Graduate Medical Education (ACGME)
3
IV.C. Curriculum Organization and Resident Experiences 141
IV.C.2. Pain Management and Substance Use Disorder 143
IV.D.1. Scholarship Program Responsibilities 147
IV.D.2. Faculty Scholarly Activity 151
IV.D.3. Resident Scholarly Activity 159
V.A.1.a) - f) Resident Evaluation 164
V.A.1.d).(2) Resident Individual Learning Plans 168
V.A.1.d).(3) Plans for Residents Failing to Progress 171
V.A.2.a).(1) Milestones and Sharing Externally 178
V.A.2.a).(2) Final Evaluation 180
V.A.3.a) - b) Clinical Competency Committee Composition and Role 182
V.B.1. - 3. Faculty Evaluation 184
V.C.1. The Program Evaluation Committee 188
V.C.2. Self-Study 197
V.C.3.a) - f) Board Pass Rates and Ultimate Board Certification 199
VI.A.1.a).(1) – (3) Patient Safety and Quality Metrics 205
VI.A.2. Supervision and Accountability 209
VI.B. Professionalism 215
VI.C. Well-Being 222
VI.D. Fatigue Mitigation 226
VI.E. Clinical Responsibilities, Teamwork, and Transitions of Care 229
VI.F. Clinical Experience and Education 232
©2024 Accreditation Council for Graduate Medical Education (ACGME)
4

Guide to the Common Program Requirements
(Residency)
The Guide to the Common Program Requirements is a living document that will be updated as
the Common Program Requirements change. In addition to this Residency version, the ACGME
has developed a Fellowship version.
This gui
de is available as a downloadable PDF version that can be printed. If referring to a
printed version, periodically check the website for any version updates.
The Guide
should serve as a resource, and the content within it is designed to serve as helpful
guidance and not to be interpreted as additional requirements. It is also not meant to be read
cover to cover in one sitting, but to be referenced as needed throughout the academic year.
If t
here are any conflicts between the Guide and the Common Program Requirements, as
interpreted and implemented by the Review Committees, the interpretation and
implementation of the Review Committees shall control.
Note:
Every set of specialty-specific Program Requirements includes content specific and
unique to the specialty. Specialty Program Requirements are not addressed in this Guide. The
specialty-specific FAQs and other resource documents provided by the respective Review
Committee should be consulted; these are available on the respective specialty section of the
ACGME website. Contact Review Committee staff members with specific questions.
Format
• Requirement text is included on the pages with a blue background.
o Italicized text provides philosophical background; these statements are not Program
Requirements and, therefore, are not citable by Review Committees.
o Text in boxes provides Background and Intent and is also not citable.
o Review Committees may further specify additional Program Requirements only
where bracketed notes indicate that the Review Committee may/must further specify.
• Guidance for understanding and applying individual Program Requirements is included
on the pages with a white background.
• Each entry in the Table of Contents is a link that can be used to jump to a specific topic
area in the Guide.
• The search function allows users to enter key words to quickly locate information.
• Where appropriate, screenshots of what data entry looks like within the ACGME’s
Accreditation Data System (ADS) are included. ADS screenshots may change as
system enhancements are made every month. The Guide will be updated periodically as
these changes occur.
The ACG
ME encourages feedback, comments, and questions about the Guide via this survey.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
5

COMMON PROGRAM REQUIREMENTS
Where applicable, text in italics describes the underlying philosophy of the requirements
in that section. These philosophic statements are not program requirements and are
therefore not citable.
Note: Review Committees may further specify only where indicated by “The Review
Committee may/must further specify.”
Intr
oduction
Int.A
.
Definition of Graduate Medical Education
Graduate medical education is the crucial step of professional
development between medical school and autonomous clinical practice. It
is in this vital phase of the continuum of medical education that residents
learn to provide optimal patient care under the supervision of faculty
members who not only instruct, but serve as role models of excellence,
compassion, cultural sensitivity, professionalism, and scholarship.
Gradua
te medical education transforms medical students into physician
scholars who care for the patient, patient’s family, and a diverse
community; create and integrate new knowledge into practice; and educate
future generations of physicians to serve the public. Practice patterns
established during graduate medical education persist many years later.
Gradua
te medical education has as a core tenet the graded authority and
responsibility for patient care. The care of patients is undertaken with
appropriate faculty supervision and conditional independence, allowing
residents to attain the knowledge, skills, attitudes, judgement, and empathy
required for autonomous practice. Graduate medical education develops
physicians who focus on excellence in delivery of safe, equitable,
affordable, quality care; and the health of the populations they serve.
Graduate medical education values the strength that a diverse group of
physicians brings to medical care, and the importance of inclusive and
psychologically safe learning environments
Graduate medical education occurs in clinical settings that establish the
foundation for practice-based and lifelong learning. The professional
development of the physician, begun in medical school, continues through
faculty modeling of the effacement of self-interest in a humanistic
environment that emphasizes joy in curiosity, problem-solving, academic
rigor, and discovery. This transformation is often physically, emotionally,
©2024 Accreditation Council for Graduate Medical Education (ACGME)
6

and intellectually demanding and occurs in a variety of clinical learning
environments committed to graduate medical education and the well-being
of patients, residents, fellows, faculty members, students, and all members
of the health care team.
Int.B
. Definition of Specialty
[The
Review Committee must further specify]
Int.C
. Length of educational program
[The
Review Committee must further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
7

GUIDANCE
Introduction A (Int.A.) is not a requirement but is a philosophic statement that embodies the
meaning and purpose of graduate medical education (GME). It describes why GME is important
and why programs must ensure that residents are provided with the best education possible.
Introduction B (Int.B.) and Introduction C (Int.C.) address the definition of a specialty and the
length of the educational program for that specialty. These requirements must be further
specified in the specialty-specific Program Requirements.
To revi
ew the specialty-specific Program Requirements:
1. Go to
https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the subspecialty Program Requirements currently in effect.
For exam
ple, to locate the Program Requirements for Orthopaedic Surgery:
1. Go to: https://www.acgme.org/specialties/
.
2. Select Orthopaedic Surgery.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Access a P
DF version of the current “Program Requirements for Orthopaedic Surgery”
by selecting the “Program Requirements Effective [current date]” file in the box labeled
“Orthopaedic Surgery.”
As Progr
am Requirements are revised and approved by the ACGME Board of Directors,
Program Requirements that are approved but not yet effective can be found on that same page,
labeled “Future Effective Date.”
Some s
pecialties have also developed an FAQ document, which complements the specialty
Program Requirements and can be found below the specialty-specific Program Requirements.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
8

COMMON PROGRAM REQUIREMENTS
I. Oversight
I.A. Sponsoring Institution
The Sponsoring Institution is the organization or entity that assumes the
ultimate financial and academic responsibility for a program of graduate
medical education, consistent with the ACGME Institutional Requirements.
When th
e Sponsoring Institution is not a rotation site for the program, the
most commonly utilized site of clinical activity for the program is the
primary clinical site.
Background and Intent: Participating sites will reflect the healthcare needs of the
community and the educational needs of the residents. A wide variety of organizations
may provide a robust educational experience and, thus, Sponsoring Institutions and
participating sites may encompass inpatient and outpatient settings including, but not
limited to a university, a medical school, a teaching hospital, a nursing home, a school
of public health, a health department, a public health agency, an organized health care
delivery system, a medical examiner’s office, an educational consortium, a teaching
health center, a physician group practice, federally qualified health center, or an
educational foundation.
I.A.1
. The program must be sponsored by one ACGME-accredited
Sponsoring Institution.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
9

GUIDANCE
Sponsorship and Sponsoring Institution accreditation
Common Program Requirement I.A.1. corresponds with Institutional Requirement I.A.1.:
“Residency and fellowship programs accredited by the ACGME must function under the ultimate
authority and oversight of one Sponsoring Institution. Oversight of resident/fellow assignments
and of the quality of the learning and working environment by the Sponsoring Institution extends
to all participating sites.”
Sponsor
ship of a program includes responsibility for oversight of the Sponsoring Institution’s
and all accredited programs’ compliance with the applicable ACGME requirements, and the
assurance of the resources necessary for graduate medical education.
The ACG
ME Board of Directors delegates authority for accrediting Sponsoring Institutions to the
Institutional Review Committee. The ACGME’s primary point of contact with each Sponsoring
Institution is the designated institutional official (DIO).
For mor
e information about Sponsoring Institutions, refer to the ACGME Institutional
Requirements and Frequently Asked Questions.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
10

COMMON PROGRAM REQUIREMENTS
I.B. Participating Sites
A participating site is an organization providing educational experiences or
educational assignments/rotations for residents.
I.B.1. The pr
ogram, with approval of its Sponsoring Institution, must designate a
primary clinical site.
(Core)
[The Review Committee may specify which other specialties/programs
must be present at the primary clinical site]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
11

GUIDANCE
I.B.1. Primary clinical site designations and Sponsoring Institution approval
The philosophic statement preceding Common Program Requirement I.A defines a program’s
primary clinical site as “the most commonly utilized site of clinical activity for the program.” A
program should follow its Sponsoring Institution’s methods for identifying the primary clinical
site. Typically, the “most commonly utilized” participating site is that which has the highest count
of resident full-time equivalents (FTEs) in a program over an academic year, assuming a full
and evenly distributed resident complement.
ADS screenshot: primary clinical site
In a program’s Accreditation Data System (ADS) profile, the designated primary clinical site can
be found in the “Sites” tab. It is marked as “Primary” in the list of participating sites (# column), is
shaded in yellow, and appears first on the list.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
12

ADS screenshot: identifying the primary clinical site in applications
In applications for ACGME accreditation, when adding participating sites, programs are directed
to identify one of the participating sites as the primary clinical site. Only one site can be
identified as the primary clinical site.
Part
icipating site information listed in ADS, including the designation of the primary clinical site,
implies the Sponsoring Institution’s approval. The ACGME does not provide a standardized
format for documenting institutional approval of these designations. Refer to
specialty-specific
Program Requirements for additional information.
[The Review Committee may specify which other specialties/programs must be
present at the primary clinical site]
Since Review Committees may specify which other specialties/programs must be present at the
primary clinical site, programs must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
Quest
ions about specialty Program Requirements or expectations for the primary clinical site
should be directed to specialty Review Committee staff members. Programs can also access
the Common Program Requirements FAQs
for additional information on participating sites.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
13

COMMON PROGRAM REQUIREMENTS
I.B. Participating Sites
I.B.2.
T
here must be a program letter of agreement (PLA) between the program
and each participating site that governs the relationship between the
program and the participating site providing a required assignm
ent.
(Core)
I.B.2.a
) The PLA must:
I.B.2.a
).(1) be renewed at least every 10 years; and,
(Core)
I.B.2.a
).(2) be approved by the designated institutional official (DIO).
(Core)
I.B.3. T
he program must monitor the clinical learning and working environment
at all participating sites.
(Core)
I.B.3.a
) At each participating site there must be one faculty member,
designated by the program director as the site director, who is
accountable for resident education at that site, in collaboration with
the program director.
(Core)
Background and Intent: While all residency programs must be sponsored by a single ACGME-
accredited Sponsoring Institution, many programs will utilize other clinical settings to provide
required or elective education and training experiences. At times it is appropriate to utilize
community sites that are not owned by or affiliated with the Sponsoring Institution. Some of
these sites may be remote for geographic, transportation, or communication issues. When
utilizing such sites the program must ensure the quality of the educational experience.
Suggested el
ements to be considered in PLAs will be found in the Guide to the Common
Program Requirements. These include:
• Identifying the faculty members who will assume educational and supervisory
responsibility for residents
• Specifying the responsibilities for teaching, supervision, and formal evaluation of
residents
• Specifying the duration and content of the educational experience
• Stating the policies and procedures that will govern resident education during the
assignment
©2024 Accreditation Council for Graduate Medical Education (ACGME)
14

GUIDANCE
The PLA is a written document that addresses graduate medical education (GME)
responsibilities between a program and a participating site at which residents have required
educational experiences.
The As
sociation of American Medical Colleges (AAMC) has developed a PLA
template whic
h
programs can use and modify according to their specific needs.
Note:
• Program directors are responsible for PLAs. Designated institutional officials (DIOs) are
required to review and approve all PLAs.
• A change in program director or DIO does not require updating a PLA with new
signatures.
• PLAs must be updated and renewed at least every 10 years.
• PLAs are required only for sites providing required educational experiences.
• Although the ACGME does not require PLAs for sites providing elective rotations, an
institution or GME office may require a PLA for those sites.
• PLAs are between a program and the participating site and include all rotations taking
place at that participating site.
• PLAs are not required for participating sites under the governance of the Sponsoring
Institution.
The purpose of a PLA is to ensure a shared understanding of expectations for the educational
experience, the nature of the experience, and the responsibilities of the program and the
participating site.
As specified in the Background and Intent under Common Program Requirement I.B.3.a),
suggested elements for a PLA include:
• identifying the faculty members who will assume educational and supervisory
responsibility for residents;
• specifying the responsibilities for teaching, supervision, and formal evaluation of
residents;
• specifying the duration and content of the educational experience (e.g., rotation name,
educational objectives) and
• stating the policies and procedures that will govern resident education during the
assignment.
Addit
ional considerations for PLAs that may be further clarified in specialty-specific FAQs
include:
• the site director may be the program director in some cases, but the program director is
not usually the site director at all participating sites; and
• if the site is distant, the program should consider providing the residents with
accommodation proximate to the participating site.
The ACG
ME requires copies of PLAs to be uploaded in the Accreditation Data System (ADS)
for new program applications and updated applications. Accreditation Field Staff request copies
of and verify PLAs during site visits for applications, initial accreditation, and other types of site
visits. For programs with a status of Continued Accreditation, the PLA is not requested when a
©2024 Accreditation Council for Graduate Medical Education (ACGME)
15

new
participating site is added in ADS. However, the program must provide confirmation that a
PLA is in place and list the effective date. If the effective date is not available, the signature date
may be documented as the effective date.
ADS screenshot: adding a participating site and PLA details
When entering a new participating site in ADS, programs are asked to confirm that a PLA exists
and provide its effective date.
Examples of rotations that require a PLA
• one-month required rotation in a pediatric inpatient unit in a children’s hospital in a family
medicine program
• one-month required rotation in rheumatology in an internal medicine program
• two-month required rotation in an emergency department with a Level 1 trauma center at
a site that is not the Sponsoring Institution
• required osteopathic neuromusculoskeletal medicine inpatient rotation
• longitudinal required geriatric experience in a long-term care facility in a family medicine
program
• four-week required retina rotation with a community physician who is not a member of
the medical staff of one of the participating sites in an ophthalmology program
Potential areas for improvement (AFIs) or citations
• failure to have a PLA signed by the DIO, the program director, and the site director for
each site at which residents rotate for a required educational experience
• failure to renew a PLA every 10 years
• incorrect/incomplete participating site information in ADS
©2024 Accreditation Council for Graduate Medical Education (ACGME)
16

In addi
tion to the guidance included here, the Common Program Requirements FAQs
address
multiple questions from the GME community about PLAs
Com
mon Program Requirement I.B.3. requires that the program must monitor the clinical
learning and working environment at all participating sites. The Background and Intent further
explains the rationale for this requirement and is worth repeating: “While all residency programs
must be sponsored by a single ACGME-accredited Sponsoring Institution, many programs will
utilize other clinical settings to provide required or elective education and training experiences.
At times it is appropriate to utilize community sites that are not owned by or affiliated with the
Sponsoring Institution. Some of these sites may be remote for geographic, transportation, or
communication issues. When utilizing such sites the program must ensure the quality of the
educational experience.” Examples of how programs can monitor the experience at all
participating sites include but are not limited to:
• resident evaluations of rotations at each participating site;
• participation of the site director in faculty meetings; and
• inclusion of the site director on the Clinical Competency Committee (CCC), and/or on the
Program Evaluation Committee (PEC).
©2024 Accreditation Council for Graduate Medical Education (ACGME)
17

COMMON PROGRAM REQUIREMENTS
I.B. Participating Sites
A participating site is an organization providing educational experiences or
educational assignments/rotations for residents.
I.B.4. The program director must submit any additions or deletions of
participating sites routinely providing an educational experience, required
for all residents, of one month full time equivalent (FTE) or more through
the ACGME’s Accreditation Data System (ADS).
(Core)
[The Review Committee may further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
18

GUIDANCE
The philosophic statement preceding Common Program Requirement I.B. defines a
participating site as “an organization providing educational experiences or educational
assignments/rotations for residents.” In addition to the primary clinical site, per Common
Program Requirement I.B.4. the program director must add all participating sites routinely
providing a required educational experience of one month or more in ADS.
When applying for accreditation or recognition of a new program, or when a change occurs in
the educational structure of a program and a new participating site at which a required
educational experience of one month or more will occur, the program director must add the new
site in ADS. All sites added in ADS will be visible to both the program and the Review
Committee.
Adding participating sites in ADS that provide elective experiences and/or experiences shorter
than one month in length is not required by the ACGME but may be helpful for some specialties.
[The Review Committee may further specify]
Since Review Committees may specify other requirements related to participating sites,
programs must review the specialty-specific Program Requirements:
• Go to https://www.acgme.org/specialties/
.
• Select the applicable specialty.
• Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
• Select the specialty Program Requirements currently in effect.
Questions about specialty-specific Program Requirements related to participating sites should
be directed to specialty Review Committee staff. Programs can also access the
Common
Program Requirements FAQs for additional information on participating sites.
ADS screenshot: adding a participating site
To add a site in ADS, log into the program’s ADS profile, then go to the Sites tab on the top
navigation bar and click the “Add Site” blue button.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
19

ADS screenshot: instructions for adding participating sites
For instructions on the participating sites to add into ADS, on the “Sites” tab, click the arrow on
the “Instructions” blue bar to expand it.
ADS screenshot: participating site definition
For the definition of a participating site, click the arrow on the “Participating Site Definition” blue
bar to expand it. (See accompanying screenshot which follows on the next page.)
ADS screenshot: adding participating site details
On the “Add Site” screen, the program will select a site name from the pre-populated dropdown
menu. If the site is not on the list, contact the designated institutional official to have the site
added. Programs may only enter sites that the Sponsoring Institution has approved and added
to ADS. Complete all other information and click the “Save Site” button. (See accompanying
screenshot which follows on the next page.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
20

NOTE: Programs should complete all requested information. The ACGME may request
additional information from the program if the information submitted is incomplete or inaccurate.
For example:
• Rotation months for each post-graduate year listed for that participating site do not align
with the rotation months on the block diagram.
• The description of the content of the educational experience does not include a rationale
for the addition of the site, faculty coverage, volume/variety of clinical experience, site
support, and/or educational impact.
While copies of Program Letters of Agreement (PLAs) are not required when adding a new
participating site, programs should ensure that a PLA is in place. A copy may be requested by
the ACGME during a site visit or as needed.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
21

ADS screenshot: deleting a participating site
If the program no longer uses a participating site, the site should be removed from their list of
sites in ADS. To remove a site, on the Sites tab hover over the site in the list of participating
sites and click the “X” button.
Once all participating sites have been added to or deleted from ADS, programs should review
the list of participating sites and ensure that they are ordered based on the number of months
residents spend at each site, with the most-used site listed as primary and all other sites listed
in descending order. Programs should also ensure that the number of months for each year of
training totals 12. If the number of months for each year of education and training do not total
12, the “Comments” box should be used to provide an explanation to the Review Committee.
Lastly, programs should ensure that the participating sites listed in ADS match the participating
sites listed on the block diagram, including the number of months residents rotate at each site.
This is a common discrepancy identified by Review Committees.
Review Committee approval of participating site additions and deletions
Once a site is added to or removed from ADS, the Review Committee staff members are
notified of the change. The change is reviewed per the Review Committee process and
programs will receive notification of approval or follow-up from the Review Committee staff.
Common areas for improvement (AFIs) or citations
Some of the most common areas for which programs receive an AFI or citation include:
• the listing of participating sites in ADS does not match information on the block diagram;
• the number of months for each year of education and training listed for each participating
site in ADS is different from the block diagram;
• the number of months for each year of education and training does not total 12 and the
program does not provide an explanation; and
• a site director is not identified or is incorrectly identified on the participating site profile in
ADS and/or the PLA.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
22
COMMON PROGRAM REQUIREMENTS
I.C. Workforce Recruitment and Retention
The program, in partnership with its Sponsoring Institution, must engage in
practices that focus on mission-driven, ongoing, systematic recruitment and
retention of a diverse and inclusive workforce of residents, fellows (if present),
faculty members, senior administrative staff members, and other relevant
members of its academic community.
(Core)
Background and Intent: It is expected that the Sponsoring Institution has, and
programs implement, policies and procedures related to recruitment and retention of
individuals underrepresented in medicine and medical leadership in accordance with
the Sponsoring Institution’s mission and aims.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
23

GUIDANCE
The ACGME is interested in the diversity of the physician workforce because it is essential to
addressing health care access and health equity. While most, if not all, Sponsoring Institutions
have mission statements pertaining to diversity and policies regarding diversity, these serve as
a starting point, and there are aspects of this requirement that may take considerable time to
produce quantifiable results. Common Program Requirement I.C. states that programs must
engage in mission-driven, ongoing, systematic efforts to recruit and retain individuals of diverse
backgrounds as residents, fellows, and faculty. It is important to also consider that the ability to
alter the number of such individuals appreciably will require years of effort to expand the pool of
diverse graduate medical education (GME) applicants. This will require cooperative efforts
among programs within Sponsoring Institutions, cities, and specialties. Therefore, the initial
emphasis is on process, not numerical outcomes.
On June 29, 2023, the United States Supreme Court issued its decisions in Students for Fair
Admissions, Inc. v. President and Fellows of Harvard College, University of North Carolina
addressing the consideration of race-based affirmative action in university admissions. The
ACGME reaffirms its commitment to its requirements as a way to help eliminate health care
inequities and disparities, to assist Sponsoring Institutions and programs in achievement of their
mission, and to develop a diverse physician workforce to provide care that meets the needs of
marginalized patients in particular, and all patients in general. It is important to note that the
ACGME standards do not require race-based affirmative action to achieve diversity, and this
decision does not require programs and institutions to change their resident selection practices.
The definition of diversity is intended to parallel that of the Association of American Medical
Colleges’ (AAMC) philosophy on Underrepresented in Medicine
, which permits flexibility in
defining the target groups for diversity based on the service demographics of the program that is
underrepresented relative to the workforce for a given role. The population of individuals
considered underrepresented in medicine will include racial and ethnic minority individuals
reflective of the program’s service area, but may also include others the program deems
underrepresented in medicine in the service area, or in the discipline in general. As noted in the
Background and Intent section of Common Program Requirement V.C.1.c) data to be
considered for assessment may include workforce diversity as a core element of a program’s
annual evaluation. Evaluation of workforce diversity should include an assessment of the
demographic population in the area served by the program and the program’s efforts to recruit
and retain a diverse workforce of individuals who are underrepresented in medicine, reflective of
the service area population, and in the roles clarified in Common Program Requirement I.C. i.e.,
residents, fellows, faculty members, senior GME administrative staff members, and other
relevant members of the program’s academic community.
Eac
h program is asked to present the demographic information for all GME learners on the
Resident Roster in the ACGME’s Accreditation Data System (ADS). This information provides
important baseline data on the number of individuals as a function of race/ethnicity and gender.
With time, as efforts to enhance the pool of diverse learners lead to improvements, ACGME
assessment may shift to include the actual increase in the number of diverse learners. To
assess meaningful change, it is essential to track these numbers annually to reveal continued
progress.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
24
It i
s important that the best possible data are entered in the Resident Roster. The gold standard
for obtaining the race and ethnicity for each resident is for the program staff to have a
conversation about the subject and to ask directly how each resident would choose to be
represented on the Roster. An alternative approach for obtaining this information is to transfer
the race/ethnicity and gender information from the electronic application used at the time of
residency selection. This is primary data supplied by the residents themselves and transfer of
this information is perhaps the most efficient way of supplying it to the ACGME.
In 2020, the ACGME introduced the Resident/Fellow Portal, providing residents and fellows
access to ADS. During their educational program, individual residents can use the Portal to
input their personal demographic information at their discretion. Access to the Portal is
automatically provided to individuals in specialties using the Case Log System but must be
requested by all other residents. Since not all residents are automatically granted access to the
Portal, the ACGME will continue to ask programs to provide this information on the Resident
Roster.
The demographic categories used by the ACGME reflect race/ethnicity as White, Black or
African American, Asian, Native Hawaiian or Pacific Islander, American Indian or Alaska Native;
and Hispanic, Latino, or of Spanish origin. Programs will select one of these categories. There
are three additional categories: Other, Unknown, and Prefer not to report. Since multiple races
cannot currently be selected, if a resident prefers to identify as multiracial, to the exclusion of a
single race choice, “Other” is the suggested category. If any residents truly do not know their
race/ethnicity (e.g., the resident was adopted or the child of an adopted individual, or the
program was not able to obtain any information pertaining to demographics), only then should
the “Unknown” category be selected.
For gender, the ACGME currently offers four options for programs to report on the Resident
Roster: Male, Female, Non-Binary, and Prefer not to report. For individuals who choose to
identify as male, select Male, and for those who choose to identify as female, select Female.
Those who choose not to identify as solely male or female should select Non-Binary.
Programs are encouraged to describe in detail the specific efforts being made to advance
diversity, equity, and inclusion (DEI) to increase the number of diverse residents and other
individuals participating in the program (e.g., faculty members and administrative personnel),
consistent with existing law. Evidence-based strategies and success stories illustrating these
efforts are strongly recommended. Examples should include affiliated medical schools or
Sponsoring Institution efforts only if done in partnership with the program. This is an opportunity
to describe practices instituted in the program to result in a diverse recruitment and retention
strategy and an inclusive learning environment. Do not simply copy and paste general diversity
policies and statements. Any numerical data supporting the success of these DEI efforts (e.g.,
number of students involved, success of students after participation) should be included. The
goal is for programs to outline the concrete steps they are taking to foster DEI among early
learners, residents, and other individuals participating in the program rather than broad,
philosophical policies.
Furthermore, ACGME asks programs to quantify efforts to increase the diversity of residents
and individuals participating in the program to provide a baseline to determine the effectiveness
of such measures in the future. Common Program Requirement I.C. focuses on ongoing,
systematic recruitment and retention of a diverse workforce. Programs are encouraged to
continue recruiting diverse classes as they currently do, consistent with existing law. The
©2024 Accreditation Council for Graduate Medical Education (ACGME)
25

requi
rement encourages programs and institutions to engage learners earlier and farther
upstream in the career pathway to provide equitable opportunities, such as by developing
programs for early medical students that introduce specialties; providing research, mentoring,
and shadowing for college and post-baccalaureate students; and/or partnering with local STEM
programs to encourage biomedical careers for high school and elementary school students. For
programs with such efforts already in place, the request for numerical impact will provide a
baseline to track progress. Numerical data that supports the success of these efforts can
include, but is not limited to, measures of practical outcomes, numbers of participants in a given
activity or approach, and any metrics that can be determined to measure how well a program is
achieving diversity in the recruitment and retention of residents and other individuals
participating in the program. It is hoped that this will help assess and accelerate the
effectiveness of equitable opportunities and diversity efforts. Programs may wish to include
numerical data on faculty members and other academic individuals in the program in response
to the question on efforts to increase diversity through faculty recruitment and retention as this
information is not collected elsewhere.
The ACGME has designed a new initiative, ACGME Equity Matters
TM
, to assist programs in
enhancing their diversity, equity, and inclusion. Among other resources, it includes a toolkit of
approaches that address many of the barriers diverse individuals face in the GME environment.
Some ideas employed by the most inclusive programs include having a chief diversity officer
position; creating and supporting a diversity committee; and actively engaging minoritized
individuals in the learning environment to help eliminate barriers to success in recruitment and
retention.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
26

COMMON PROGRAM REQUIREMENTS
I.D Resources
I.D.1 The program, in partnership with its Sponsoring Institution, must ensure
the availability of adequate resources for resident education.
(Core)
[The Review Committee must further specify]
I.D.2. The program, in partnership with its Sponsoring Institution, must ensure
healthy and safe learning and working environments that promote resident
well-being and provide for:
(Core)
I.D.2.a) access to food while on duty;
(Core)
I.D.2.b) safe, quiet, clean, and private sleep/rest facilities available and
accessible for residents with proximity appropriate for safe patient
care;
(Core)
Background and Intent: Care of patients within a hospital or health system occurs
continually through the day and night. Such care requires that residents function at
their peak abilities, which requires the work environment to provide them with the
ability to meet their basic needs within proximity of their clinical responsibilities.
Access to food and rest are examples of these basic needs, which must be met while
residents are working. Residents should have access to refrigeration where food may
be stored. Food should be available when residents are required to be in the hospital
overnight. Rest facilities are necessary, even when overnight call is not required, to
accommodate the fatigued resident.
I.D.2.c) clean and private facilities for lactation that have refrigeration capabilities,
with proximity appropriate for safe patient care;
(Core)
Background and Intent: Sites must provide private and clean locations where residents
may lactate and store the milk within a refrigerator. These locations should be in close
proximity to clinical responsibilities. It would be helpful to have additional support
within these locations that may assist the resident with the continued care of patients,
such as a computer and a phone. While space is important, the time required for
lactation is also critical for the well-being of the resident and the resident’s family as
outlined in VI.C.1.d).
I.D.2.d) security and safety measures appropriate to the participating site;
and,
(Core)
I.D.2.e) accommodations for residents with disabilities consistent with the
Sponsoring Institution’s policy.
(Core)
I.D.3. Residents must have ready access to specialty-specific and other
appropriate reference material in print or electronic format. This must
include access to electronic medical literature databases with full text
capabilities.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
27

GUIDANCE
I.D.1. Availability of adequate resources for resident education
[The Review Committee must further specify]
Since Common Program Requirement I.D.1. requires that Review Committees further specify
about the “availability of adequate resources,” programs must review the specialty-specific
Program Requirements:
1. Go to https://www.acgme.org/specialties/
.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
The ACGME monitors compliance with requirements in Common Program Requirements I.D.2.-
I.D.3 in various ways, including:
• questions answered by program leadership as part of an application or during the ADS
Annual Update;
• questions answered by residents and faculty members as part of the annual
Resident/Fellow and Faculty Surveys; and
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
The Resident and Faculty Surveys include several questions that address the Program
Requirements in section I.D. Two resource documents, the Resident/Fellow Survey-Common
Program Requirements Crosswalk and the Faculty Survey-Common Program Requirements
Crosswalk, provide additional information for programs on the key areas addressed by the
survey questions and how they map to the ACGME Common Program Requirements. These
documents can be found at
https://www.acgme.org/data-sys
tems-technical-support/resident-
fellow-and-faculty-surveys/.
I.D.2.a) and I.D.2.b) Access to food and sleep/rest facilities
Programs are expected to partner with their Sponsoring Institutions to ensure residents have
adequate access to food and sleep/rest facilities at all participating sites. Interpretations of the
requirements for space may depend on the attributes of a participating site and the needs of
residents when they are assigned to that site.
Depending on the type of participating site and the type of educational experience (e.g.,
overnight call, outpatient clinic) occurring at that site, there may be differences in the types of
resources provided. Because of site-, program-, and resident-specific factors, the ACGME does
not provide uniform specifications for access to food and the physical space of sleep/rest
facilities beyond the qualities indicated in the requirements and the guidance in the associated
Background and Intent. It is important for Sponsoring Institutions and programs to obtain
resident input when evaluating these aspects of clinical learning environments.
I.D.2.c) Access to lactation facilities
It is critical to acknowledge that the timing of residency often overlaps with the timing of starting
and raising families. Therefore, residents must have access to lactation facilities.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
28

Rooms for lactation must be clean, provide privacy and refrigeration, and be close enough to
the clinical setting to be of use for residents who need them. Simply using a restroom as a
facility for lactation or for medication administration would not meet the standard of cleanliness.
Refrigeration capabilities are essential for storage. In addition, the availability of a computer and
telephone will allow residents, if necessary, to provide continued attention to patient care while
attending to their personal health care needs.
Interpretation of the requirement for “proximity appropriate for safe patient care” is left to the
program and the Sponsoring Institution. The requirements do not dictate a specific distance or a
time element for the resident to get from the lactation facility or room for personal health care
needs to the clinical location. Instead, institutions and programs are urged to consider the
circumstances. For example, a busy, high-intensity clinical location, such as the intensive care
unit, might require that the lactation room is in a location that allows immediate access to the
patient care area, whereas a clinical location that is less busy or intense will not require such
proximity. In addition, it is not necessary for the lactation facility to be solely dedicated to
resident use.
I.D.2.e) Accommodations for residents with disabilities
Programs must work with their Sponsoring Institutions to ensure compliance with institutional
policies related to resident requests for accommodation of disabilities. Common Program
Requirements I.D.2. and I.D.2.e) are companions of Institutional Requirement IV.I.4., which
states, “The Sponsoring Institution must have a policy, not necessarily GME-specific, regarding
accommodations for disabilities consistent with all applicable laws and regulations.”
Laws
and regulations concerning requests for accommodation of disabilities include Title I of the
Americans with Disabilities Act and related enforcement guidance published by the US Equal
Employment Opportunity Commission. Other federal, state, and local laws and regulations may
also apply. It is common for program directors, coordinators, residents, faculty members, and
designated institutional officials to collaborate with their institution’s human resources and legal
departments and/or institutional officers/committees to manage requests for accommodation.
I.D.3. Reference Material
Sponsoring Institutions and programs must ensure that residents have access to medical
literature that supports their clinical and educational work. Common Program Requirement
I.D.3. is parallel to ACGME Institutional Requirement II.E.2., which states, “Faculty members
and residents/fellows must have ready access to electronic medical literature databases and
specialty-/subspecialty-specific and other appropriate full-text reference material in print or
electronic format.”
Rev
iew Committee members are aware that the availability of a computer or mobile device with
internet access alone may provide access to a wide range of relevant reference material. Many
Sponsoring Institutions and programs purchase subscriptions to information resources and
services to supplement open access materials. As with other programmatic resources,
interpretation of the requirement may depend on unique circumstances of participating sites,
programs, faculty members, and residents. Residents and faculty members may provide
valuable input to Sponsoring Institutions and programs regarding the adequacy of available
medical literature resources.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
29

COMMON PROGRAM REQUIREMENTS
I.E. Other Learners and Health Care Personnel
The presence of other learners and other health care personnel, including,
but not limited to residents from other programs, subspecialty fellows, and
advanced practice providers, must not negatively impact the appointed
residents’ education.
(Core)
[The Review Committee may further specify]
Background and Intent: The clinical learning environment has become increasingly
complex and often includes care providers, students, and post-graduate residents and
fellows from multiple disciplines. The presence of these practitioners and their
learners enriches the learning environment. Programs have a responsibility to monitor
the learning environment to ensure that residents’ education is not compromised by
the presence of other providers and learners.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
30

GUIDANCE
Although other learners and other health care personnel can, and frequently do, enhance
resident education, there are certainly circumstances in which they negatively impact that
process. Examples include:
• interference of a subspecialty fellow or another care provider in the communication
between a faculty member and the resident (or resident team) in such a manner that the
resident does not gain the educational benefit of direct communication with the faculty
member;
• a fellow repeatedly performing procedures in which the resident is expected to develop
competence when there is a limited pool of procedures available;
• too many learners for the amount of educational experience or excessive rotators (e.g.,
medical students, residents from other specialties, advanced practice provider students);
• lack of opportunity for peer teaching (e.g., senior resident to junior resident, PGY-1 to
medical student); and
• certified registered nurse anesthetists (CRNAs) or CRNA students interfering with
residents performing and gaining competence in certain procedures.
Situations of this type frequently involve a degree of intra- or inter-departmental disagreement
on educational responsibilities and priorities. In the case of other health care personnel, they
may also impact decisions made by the administration of the clinical site. The designated
institutional official and Graduate Medical Education Committee (GMEC) may be very helpful in
supporting the program(s) and in arriving at equitable and mutually beneficial solutions.
The ACGME monitors compliance with Common Program Requirement I.E. in various ways,
including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by residents and faculty members as part of the annual
Resident/Fellow and Faculty Surveys; and
• questions asked by the Accreditation Field Staff during site visits of the program at
various stages of accreditation.
The Resident/Fellow and Faculty Surveys include several questions that address the Program
Requirements in section I.D. The ACGME has prepared two documents, a Resident/Fellow
Survey-Common Program Requirements Crosswalk and a Faculty Survey-Common Program
Requirements Crosswalk, to provide additional information for programs on the key areas
addressed by the survey questions and how they map to the ACGME Common Program
Requirements. These documents can be found at
https://www.acgme.org/data-systems-
technical-support/resident-fellow-and-faculty-surveys/.
Programs are encouraged to monitor any concerns identified in the Resident/Fellow Survey and
address them proactively in the major changes section in ADS as part of their ADS Annual
Update or in preparation for a site visit.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
31

ADS screenshot: presence of other learners
The question below is part of the program ADS Annual Update Questionnaire.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
32

COMMON PROGRAM REQUIREMENTS
II. Personnel
II.A. Program Director
II.A.1. There must be one faculty member appointed as program director
with authority and accountability for the overall program, including
compliance with all applicable program requirements.
(Core)
.
II.A.1.a) The Sponsoring Institution’s GMEC must approve a change in
program director and must verify the program director’s
licensure and clinical appointment.
(Core)
II.A.1.a).(1) Final approval of the program director resides with the
Review Committee.
(Core)
[For specialties that require Review Committee
approval of the program director, the Review
Committee may further specify.
This requirement will be deleted for those specialties
that do not require Review Committee approval of the
program director.]
Background and Intent: While the ACGME recognizes the value of input from numerous
individuals in the management of a residency, a single individual must be designated as
program director and have overall responsibility for the program. The program
director’s nomination is reviewed and approved by the GMEC.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
33

GUIDANCE
II.A.1. One faculty member must be appointed as program director with authority
and accountability for the overall program.
This requirement specifies that each program must have one faculty member appointed as
program director. The program director is responsible for all aspects of the program and is
accountable for compliance with all applicable program requirements. For new programs, the
program director is identified in the Accreditation Data System (ADS) by the designated
institutional official (DIO). For existing programs, the program director is already designated and
appears first on the faculty roster.
II.A.1.a) The Graduate Medical Education Committee (GMEC) must approve a
program director change and verify the program director’s licensure and clinical
appointment.
A new program director can be designated for a program at any time through a program director
change request initiated by the DIO in ADS. For appointment of a new program director, the
GMEC must verify that the program director meets the qualifications outlined in Common
Program Requirement II.A.3. as well as verify that the program director has an active medical
license and a current clinical appointment and privileges before approving the change.
Following GMEC approval, the DIO will enter the recommendation into ADS via a new program
director request.
ADS steps and screenshots for initiating a new program director request:
The DIO must log into the Sponsoring Institution’s ADS account and complete the following
steps:
1. Select the Sponsored Programs tab and locate the program for which the program
director will change.
2. On the Program tab, select New Program Director.
3. Read the instructions carefully and select one of two options: Choose Program Faculty
or Search/Add New Person.
4. The DIO must complete two key sections: DIO questions and Director Profile
Information, including the rationale for the change. (See accompanying screenshots
which follow on the next page.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
34

5. When the DIO submits the change, the old program director’s ADS access will
be immediately disabled and the new program director will receive an email
notification with the username and password (if new to ADS) and a notification
to review the change. The new contact information is immediately reflected in ADS
and on the public ACGME website.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
35

6. Once the new program director logs into ADS, the change request will be
available on the Overview tab toward the bottom of the page for review, completion
of any missing information, and submission. The program director change is not
complete until submitted by the new program director.
NOTE: The new program director or a designee must complete all required fields on
both the “Profile and Certifications” and “CV” tabs associated with the request.
Fields that require information or updates will be marked in red. This action will reduce
the need for ACGME staff members to seek updated information from programs and will
ensure timely review and approval by Review Committees.
7. Once the new program director submits the completed request, an email notification will
be generated in ADS to the ACGME, the DIO, and the institutional coordinator(s).
8. Rev
iew Committee staff members will reach out to programs with questions or requests
for additional information as needed if the new program director change request is
incomplete. Programs will be notified through ADS if a request is denied.
II.A.1.a).(1). Final approval of the program director resides with the Review Committee.
This requirement is included in the specialty Program Requirements only if the Review
Committee with oversight for a particular specialty has elected to establish the approval of
program director changes by the Review Committee as one of its processes. Not all Review
Committees or specialties/subspecialties have the same processes for reviewing program
director changes. Programs should review the resources on the applicable specialty section of
the website for more information, and can contact Review Committee staff members to verify
the program director change process for their specialty.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
36

COMMON PROGRAM REQUIREMENTS
II. Personnel
II.A. Program Director
II.A.1. There must be one faculty member appointed as program director
with authority and accountability for the overall program, including
compliance with all applicable program requirements.
(Core)
II.A.1.b) The program must demonstrate retention of the program
director for a length of time adequate to maintain continuity
of leadership and program stability.
(Core)
[The Review Committee may further specify]
Background and Intent: The success of residency programs is generally enhanced by
continuity in the program director position. The professional activities required of a
program director are unique and complex and take time to master. All programs are
encouraged to undertake succession planning to facilitate program stability when
there is necessary turnover in the program director position.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
37

GUIDANCE
II.A.1.b) Program director retention
The program director has many important responsibilities in a residency program. It can take
years for individuals to understand and reach a level of expertise in the role and develop
effective working relationships with all the individuals they must interact, including the
designated institutional official, program faculty members, faculty members and leaders in
related educational programs, administrators at the clinical sites to which residents rotate,
community leaders, and others. For these reasons, continuity in the program director role is
critical to ensure and maintain program stability and it is often associated with success of the
program.
[The Review Committee may further specify]
Common Program Requirement II.A.1.b) allows specialties to further specify. Currently, only a
few specialties have added a requirement that further specifies the minimum amount of time a
program director should serve in their role. To review the specialty-specific Program
Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
The Background and Intent associated with this requirement encourages programs “to
undertake succession planning to facilitate program stability when there is necessary turnover in
the program director position.” While having a formal succession planning process at the
program or Sponsoring Institution level would be ideal, there are many ways programs can think
about succession planning. In larger programs, having one or more assistant/associate program
directors may be a good option for ensuring continuity of leadership in the program in case of a
program director change. In other cases, having a faculty mentoring process to identify faculty
members with an interest in a graduate medical education leadership career path and
supporting them in achieving various leadership competencies would also be a way to develop
talent for a program director or assistant/associate program director role.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
38

COMMON PROGRAM REQUIREMENTS
II.A. Program Director
II.A.2. The program director and, as applicable, the program’s leadership
team, must be provided with support adequate for administration of
the program based upon its size and configuration.
(Core)
[The Review Committee must further specify minimum dedicated
time for program administration and will determine whether
program leadership refers to the program director or both the
program director and associate/assistant program director(s).]
Background and Intent: To achieve successful graduate medical education, individuals
serving as education and administrative leaders of residency programs, as well as
those significantly engaged in the education, supervision, evaluation, and mentoring
of residents, must have sufficient dedicated professional time to perform the vital
activities required to sustain an accredited program.
The ultimate outcome of graduate medical education is excellence in resident
education and patient care.
The program director and, as applicable, the program leadership team, devote a
portion of their professional effort to the oversight and management of the residency
program, as defined in II.A.4.-II.A.4.a).(16). Both provision of support for the time
required for the leadership effort and flexibility regarding how this support is provided
are important. Programs, in partnership with their Sponsoring Institutions, may
provide support for this time in a variety of ways. Examples of support may include,
but are not limited to, salary support, supplemental compensation, educational value
units, or relief of time from other professional duties.
Program directors and, as applicable, members of the program leadership team who
are new to the role, may need to devote additional time to program oversight and
management initially as they learn and become proficient in administering the
program. It is suggested that during this initial period the support described above be
increased as needed.
In addition, it is important to remember that the dedicated time and support
requirement for ACGME activities is a minimum, recognizing that, depending on the
unique needs of the program, additional support may be warranted. The need to
ensure adequate resources, including adequate support and dedicated time for the
program director is also addressed in Institutional Requirement II.B.1. The amount of
support and dedicated time needed for individual programs will vary based on a
number of factors and may exceed the minimum specified in the applicable specialty
specific program requirements. It is expected that the Sponsoring Institution, in
partnership with its accredited programs, will ensure support for program directors,
core faculty members, and program coordinators to fulfill their program
responsibilities effectively.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
39

GUIDANCE
II.A.2. The program director and, as applicable, the program’s leadership team,
must be provided with support adequate for administration of the program based
upon its size and configuration.
The Background and Intent associated with this requirement further explains the rationale,
provides various examples of what may constitute program director support, and identifies
instances in which minimum support may need to be increased.
It is important to note that Review Committees consider approved resident complement rather
than filled resident complement when assessing program director or program leadership support
for administration of the program.
This requirement is closely linked to Institutional Requirements II.B.-II.B.4
. A Sponsoring
Institution is not necessarily the entity that provides compensation directly to a program director,
and, in many cases, a program director’s employer is not the Sponsoring Institution. However,
each accredited Sponsoring Institution is accountable to the ACGME’s Institutional Review
Committee for ensuring that program directors receive support and dedicated time in substantial
compliance with this requirement.
[The Review Committee must further specify minimum dedicated time for
program administration and will determine whether program leadership refers to
the program director or both the program director and associate/assistant
program director(s).]
Since Review Committees must specify minimum dedicated time for the program director or
program leadership, programs must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of specialty
section.
4. Select the specialty Program Requirements currently in effect.
The Program Leadership Dedicated Time
summary document included as an institutional
resource on the ACGME website also provides a snapshot of program director dedicated time
and support across all ACGME-accredited specialties and subspecialties.
Accr
editation Data System (ADS) screenshot: program director support
The program director must answer or update the following questions as part of the ADS Annual
Update regarding support adequate for the administration of the program based on its size and
configuration. Programs are strongly encouraged to verify the specialty-specific Program
Requirements each year to ensure at least the minimum required level of support is provided.
(See accompanying screenshot which follows on the next page.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
40

©2024 Accreditation Council for Graduate Medical Education (ACGME)
41
COMMON PROGRAM REQUIREMENTS
II.A.3. Qualifications of the program director:
II.A.3.a) must include specialty expertise and at least three years of
documented educational and/or administrative experience, or
qualifications acceptable to the Review Committee;
(Core)
Background and Intent: Leading a program requires knowledge and skills that are
established during residency and subsequently further developed. The time period
from completion of residency until assuming the role of program director allows the
individual to cultivate leadership abilities while becoming professionally established.
The three-year period is intended for the individual's professional maturation.
The broad allowance for educational and/or administrative experience recognizes that
strong leaders arise through diverse pathways. These areas of expertise are important
when identifying and appointing a program director. The choice of a program director
should be informed by the mission of the program and the needs of the community.
In certain circumstances, the program and Sponsoring Institution may propose and the
Review Committee may accept a candidate for program director who fulfills these
goals but does not meet the three-year minimum.
II.A.3.b) must include current certification in the specialty for which
they are the program director by the American Board of _____
or by the American Osteopathic Board of _____, or specialty
qualifications that are acceptable to the Review Committee;
and,
(Core)
[The Review Committee may further specify acceptable
specialty qualifications or that only ABMS and AOA
certification will be considered acceptable]
II.A.3.c) must include ongoing clinical activity.
(Core)
Background and Intent: A program director is a role model for faculty members and
residents. The program director must participate in clinical activity consistent with the
specialty. This activity will allow the program director to role model the Core
Competencies for the faculty members and residents.
[The Review Committee may further specify additional program director
qualifications]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
42
GUIDANCE
II.A.3.a) Specialty expertise and at least three years of documented educational
and/or administrative experience, or qualifications acceptable to the Review
Committee.
The Background and Intent that follows this requirement helps explain the rationale behind the
requirement. Graduate medical education leaders require knowledge and skills that are
established during residency and must be subsequently further developed and cultivated over a
minimum of three years as an individual becomes professionally established. This requirement
also broadly allows for educational and/or administrative experience, recognizing that strong
leaders arise through diverse pathways. Lastly, the requirement acknowledges that the mission
of the program and the needs of its community should inform the selection of a program
director.
The Background and Intent also allows for potential exceptions, in certain circumstances, to the
three-year minimum educational or administrative experience requirement. The program and
Sponsoring Institution may propose, and the Review Committee may accept, a candidate for
program director who fulfills all other qualification requirements but does not meet the three-year
minimum.
Program director education and training, clinical and administrative experience and expertise,
and other demographic information are captured on the program director profile and curriculum
vitae (CV) in the Accreditation Data System (ADS). Programs should complete all required
information when adding a new program director into ADS as part of an application or when
submitting a program director change for an existing program. It is also important to carefully
review and update all the program director information if a profile for that individual already
exists in ADS.
ADS screenshots: program director profile and CV (See accompanying screenshots
on the next pages.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
43

©2024 Accreditation Council for Graduate Medical Education (ACGME)
44

©2024 Accreditation Council for Graduate Medical Education (ACGME)
45

II.A.3.b) Current certification in the specialty for which they are the program
director or specialty qualifications that are acceptable to the Review Committee.
[The Review Committee may further specify acceptable specialty qualifications or
that only ABMS and AOA certification will be considered acceptable]
Some Review Committees will accept only certification in the appropriate specialty by an
American Board of Medical Specialties (ABMS) member board or American Osteopathic
Association (AOA) certifying board for the program director. Other Review Committees will
accept other qualifications for the program director. Programs are encouraged to refer to the
specialty-specific Program Requirements
for more information on t
his requirement.
The ACGME automatically populates data received from the ABMS and the AOA for the
program director on their individual ADS profile page, where data are available. Program
director board certification data will be matched to the ABMS and AOA datasets based on
National Provider Identifier (NPI) number, as well as name, date of birth, and medical school
graduation year. Program directors who are newly entered into ADS will have their certification
information matched and populated within 24 hours.
Programs are only required to provide a manual entry for the program director’s specialty
certification under the following circumstances:
• No ABMS/AOA board certification data is displayed in ADS or it is incorrect. In this case,
a manual entry for “ABMS missing/inaccurate data” or “AOA missing/inaccurate data”
should be added on the program director’s profile with a duration type, initial certification
year, certification name, and an explanation for Review Committee consideration.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
46
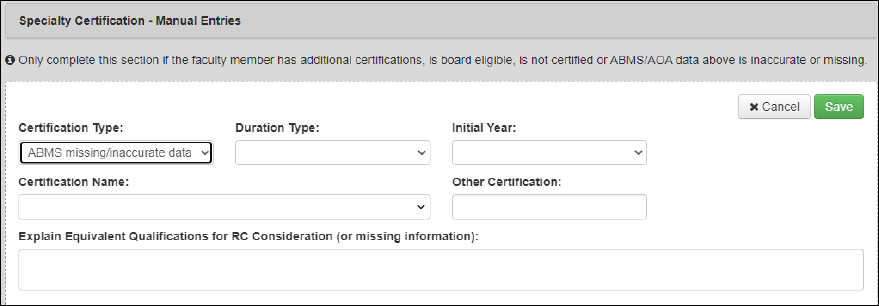
• The program director is not certified by the ABMS/AOA. Add a manual entry of “Not
Board Certified” and an explanation.
• The program director is board eligible but has not yet achieved board certification. Add a
manual entry of “Board eligible” and provide an explanation.
• The program director is certified by another certifying body. Some Review Committees
allow other acceptable specialty qualifications and therefore a manual entry of “Other
Certifying Body” can provide that information.
ADS screenshot: specialty certification – manual entries
Common issues related to the ABMS and AOA data not auto-populating on the program
director’s profile and in the faculty roster include:
• the NPI number in ADS is incorrect or does not match the NPI number in the
ABMS/AOA dataset; and
• a lag in when updated board certification data are received by the ACGME from the
ABMS and AOA.
II.A.3.c).Ongoing clinical activity
This requirement is self explanatory. The expectation is that program directors are clinically
active in their specialty and are involved in working with residents.
Common citations regarding program director qualifications include:
• no or not enough previous experience in the specialty;
• no or not enough previous educational/administrative experience;
• board certifications that are lapsed; and
• no board certification information entered at all.
[The Review Committee may further specify additional program director
qualifications]
The ACGME Review Committees want to help programs succeed. One essential element of
program success is having a qualified individual as program director. Based on years of
cumulative experience with both programs that are successful and those that are not as
successful, many Review Committees have developed minimal qualifications for program
directors in each specialty. Review Committees may specify other requirements related to
additional qualifications and clarifications for appointment, so programs must review the
specialty-specific Program Requirements:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
47

1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
Questions about specialty-specific Program Requirements related to program director
qualifications should be directed to respective specialty Review Committee staff.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
48

COMMON PROGRAM REQUIREMENTS
II.A.4. Program Director Responsibilities
The pr
ogram director must have responsibility, authority, and
accountability for: administration and operations; teaching and scholarly
activity; resident recruitment and selection, evaluation, and promotion of
residents, and disciplinary action; supervision of residents; and resident
education in the context of patient care
. (Core)
II.A.4
.a) The program director must:
II.A.4
.a).(1) be a role model of professionalism;
(Core)
Background and Intent: The program director, as the leader of the program, must serve
as a role model to residents in addition to fulfilling the technical aspects of the role. As
residents are expected to demonstrate compassion, integrity, and respect for others,
they must be able to look to the program director as an exemplar. It is of utmost
importance, therefore, that the program director model outstanding professionalism,
high quality patient care, educational excellence, and a scholarly approach to work.
The program director creates an environment where respectful discussion is welcome,
with the goal of continued improvement of the educational experience.
II.A.4
.a).(2) design and conduct the program in a fashion consistent with
the needs of the community, the mission(s) of the Sponsoring
Institution, and the mission(s) of the program;
(Core)
Background and Intent: The mission of institutions participating in graduate medical
education is to improve the health of the public. Each community has health needs that
vary based upon location and demographics. Programs must understand the structural
and social determinants of health of the populations they serve and incorporate them
in the design and implementation of the program curriculum, with the ultimate goal of
addressing these needs and eliminating health disparities.
II.A.4
.a).(3) administer and maintain a learning environment conducive to
educating the residents in each of the ACGME Competency
domains;
(Core)
Background and Intent: The program director may establish a leadership team to
Assist in the accomplishment of program goals. Residency programs can be highly
complex. In a complex organization, the leader typically has the ability to delegate
authority to others, yet remains accountable. The leadership team may include
physician and non-physician personnel with varying levels of education, training, and
experience.
II.A.4
.a).(4) have the authority to approve or remove physicians and non-
physicians
as faculty members at all participating sites,
including the designation of core faculty members, and must
©2024 Accreditation Council for Graduate Medical Education (ACGME)
49

develop and oversee a process to evaluate candidates prior
to approval;
(Core)
Background and Intent: The provision of optimal and safe patient care requires a team
approach. The education of residents by non-physician educators may enable the
resident to better manage patient care and provides valuable advancement of the
residents’ knowledge. Furthermore, other individuals contribute to the education of
residents in the basic science of the specialty or in research methodology. If the
program director determines that the contribution of a non-physician individual is
significant to the education of the residents, the program director may designate the
individual as a program faculty member or a program core faculty member.
II.A.4.a).(5) have the authority to remove residents from supervising
interactions and/or learning environments that do not meet
the standards of the program;
(Core)
Background and Intent: The program director has the responsibility to ensure that all
who educate residents effectively role model the Core Competencies. Working with a
resident is a privilege that is earned through effective teaching and professional role
modeling. This privilege may be removed by the program director when the standards
of the clinical learning environment are not met.
There may be faculty in a department who are not part of the educational program, and
the program director controls who is teaching the residents.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
50
GUIDANCE
Simply put, the program director is the person who is ultimately responsible for the program.
II.A.4.a).(1) and II.A.4.a).(3) [The program director must:] be a role model of
professionalism; and administer and maintain a learning environment conducive
to educating the residents in each of the ACGME Competency domains.
The purpose of this section is to emphasize the importance of the program director and faculty
leadership as noted in the Background and Intent, including role modeling of professionalism,
high-quality patient care, educational excellence, and scholarly approach to work. While the
guidance below is related to Common Program Requirements II.A.4.a).(1) and II.A.4.a).(3), it
does not constitute actual requirements. Although this section is not tied to a specific
requirement, program directors are urged to consult some or all the references for inspiration
related to mentorship, humanism, and leadership.
Leadership
The concepts of program director and faculty leadership take many forms and are important,
regardless of program size. The designation of faculty leadership can be a formal or informal
process, but what is most important is the composition of such a group. The group can be
composed of physicians and non-physicians who know the residents well, have frequent
interactions with them, and most importantly, can serve as role models in clinical care,
professionalism, and scholarship. In addition, they can serve as a sounding board for the
program director and help in shaping the program.
ACGME President and Chief Executive Officer Dr. Thomas J. Nasca provides the context for
understanding the professionalism that underlies leadership in medicine:
The philosophical roots of professionalism include the Hippocratic tradition of medicine
as a moral enterprise; the transition of medicine from guild to profession with a
commitment to competence, altruism, and public trust; and the responsibility of the
profession to prepare the next generation of physicians to serve the public. (Nasca 2015;
emphasis added)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
51

Nasca 2015
Mentorship
While there are many articles that define and describe mentoring and mentorship, there are
several characteristics that constitute this relationship. Mentorship is a long-term relationship
between a more senior person (mentor) and a less experienced person (mentee). While both
benefit from the relationship, it is generally established for the betterment of the mentee.
According to Sambunjak, Dario, and Marušić (2009), mentorship includes three components:
helping mentees acquire and integrate new learning; managing a personal aspect of transitional
states; and maximizing the mentee’s potential to become a fulfilled and achieving practitioner.
Mentorship therefore helps
physicians uphold the responsibility to educate the next generation
of physicians to serve patients.
Tjan (2017) interviewed scores of leaders and concluded that successful mentors have four
characteristics: 1) they put the relationship before the mentorship; 2) they focus on character
rather than competence and on shaping character, values, self-awareness, empathy, and
capacity for respect; 3) they shout loudly with optimism and keep quiet with cynicism; and 4)
they are more loyal to their mentees than to their companies.
References
• Lacombe, Michael A. 1990. “Recent Advances.” The American Journal of Medicine
88(4), 407–8. https://doi.org/10.1016/0002-9343(90)90497-2
.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
52

• Nasca, Thomas J. 2015. “Professionalism and Its Implications for Governance and
Accountability of Graduate Medical Education in the United States.” JAMA 313(18):
1801. Graphic available at https://doi.org/10.1001/jama.2015.3738
.
• Sambunjak, Dario, Sharon E. Straus, and Ana Marušić. 2006. “Mentoring in Academic
Medicine.” JAMA 296(9): 1103. https://doi.org/10.1001/jama.296.9.1103.
• Sambunjak, Dario, and Ana Marušić. 2009. “Mentoring.” JAMA 302(23): 2591.
https://doi.org/10.1001/jama.2009.1858.
• Tjan, Anthony K. “What the Best Mentors Do.” Harvard Business Review, 2017(2).
https://hbr.org/2017/02/what-the-best-mentors-do.
Humanism
Humanism in health care is characterized by a respectful and compassionate relationship
between physicians and their patients. It reflects attitudes and behaviors that are sensitive to the
values and the cultural and ethnic backgrounds of others. The humanistic health care
professional has two key attributes: altruism and empathy. Chou et al. (2014) stated that
“Humanism in medicine combines scientific knowledge and skills with respectful, compassionate
care that is sensitive to the values, autonomy and cultural backgrounds of patients and their
families.”
Evidence demonstrates that compassion and empathy are critical components of good
medicine. When provided with humanistic care, patients are more likely to adhere to their
treatment regimens, and this adherence makes it more likely that they adhere to preventive
practices and may heal more quickly. Studies indicate that the characteristics of humanism can
be taught. While Chou et al. (2014) acknowledged this fact, they sought to determine how
humanism can be maintained in a world of increasing demands and technologies. They
interviewed faculty members in internal medicine who had been identified by the residents to be
excellent role models for humanism. The authors found three themes: attitudes needed to
sustain humanism included humility, curiosity, standard of behavior (“I treat patients the way I
would want to be treated”), importance for the patient, importance for the physician (joy in caring
for patients), and more than just the disease (“my role is being there with and for the patient”);
habits included self-reflection, seeking a connection with the patients, teaching/role modeling
(“knowing that I’m responsible not just for the patients in front of me, but modeling how my
students and residents are going to treat their patients”), balance, and mindfulness and spiritual
practices; and humanism and maintenance of humanism in medical practice takes effort. Many
of the physicians interviewed noted that humanism takes deliberate, intentional work, and
identified the need for environmental support. While one may conclude that the work that goes
into deliberative practice of humanism imposes additional workload on physicians that leads to
burnout, the physicians in the study believed that humanism, as represented by the joy in caring
for patients and educating residents, actually was a deterrent to burnout.
References
• Chou, Carol M., Katherine Kellom, and Judy A. Shea. 2014. “Attitudes and Habits of
Highly Humanistic Physicians.” Academic Medicine 89(9): 1252–58.
https://doi.org/10.1097/acm.0000000000000405.
• Montgomery, Lynda L., Sana Loue, and Kurt C. Stange. 2017. “Linking the Heart and the
Head: Humanism and Professionalism in Medical Education and Practice.” Family
Medicine 49(5): 378–83. https://www.ncbi.nlm.nih.gov/pubmed/28535319
.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
53
II.A.4.a).(2) [The program director must:] design and conduct the program in a
fashion consistent with the needs of the community, the mission(s) of the
Sponsoring Institution, and the mission(s) of the program.
This requirement is intended to bring intentionality to the development, design, and
implementation of each residency program in consideration of the needs and desires of its
stakeholders. Programs are encouraged to develop and clearly articulate their mission with the
input of the communities they serve, their residents, their Sponsoring Institution, and
participating sites, and others. Although the process may prove to be time consuming,
developing this foundation will likely prove rewarding for all involved. Once developed, the
mission of the program should periodically be re-evaluated for potential improvement, again
incorporating input from stakeholders.
II.A.4.a).(4) [The program director must:] have the authority to approve or remove
faculty for participation in the residency program education at all sites and
oversee a process to evaluate candidates prior to approval.
This requirement applies to faculty members at the primary clinical site and at any participating
sites used by the program. It is important that the faculty members who participate in the
education of residents are interested in and dedicated to the educational program.
The program director must have the authority to approve or remove a faculty member from the
teaching service. For example, if a faculty member is consistently reported as being unable or
refusing to teach, berating the residents, and generally being unavailable for educational
activities, the program director may decide to remove the faculty member from the teaching
service. However, the faculty member may still continue with other clinical and administrative
responsibilities within the department.
II.A.4.a).(5) [The program director must:] have the authority to remove residents
from supervising interactions and/or learning environments that do not meet the
standards of the program.
For example, residents might be assigned to a participating site for a one-month rotation and
residents report that their role is only to provide service. Faculty members at the site do not
provide supervision, evaluation, or education and are not available to the residents. The
program director may choose to discontinue the rotation and have the residents rotate to
another participating site that can provide the appropriate an educational experience.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
54

COMMON PROGRAM REQUIREMENTS
II. Personnel
II.A. Program Director
II.A.4. Program Director Responsibilities
II.A.4.a) The program director must:
II.A.4.a).(6)
submit accurate and complete information required
and requested by the DIO, GMEC, and ACGME;
(Core)
Background and Intent: This includes providing information in the form and format
requested by the ACGME and obtaining requisite sign-off by the DIO.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
55

GUIDANCE
II.A.4.a).(6). It is the responsibility of the program director to submit accurate and
complete information required and requested by the DIO, GMEC, and ACGME.
The submission of incomplete and/or inaccurate information by a program is one of the most
common citations given by the Review Committees. Programs are required to submit specific
information as part of an application, annually during the Accreditation Data System (ADS)
Annual Update process, as part of preparing for a program site visit, or for other types of
requests submitted to the ACGME. The program director is responsible for the accuracy and
completeness of information submitted to the ACGME.
This requirement captures a broad array of information and Review Committees will issue
citations related to this requirement if there are consistent gaps in data submitted to the
ACGME. Some examples include:
• An application or updated application had significant gaps in data required by the
ACGME, the data was submitted in a format that is hard to understand for the Review
Committee, or there are a lot of discrepancies between various parts of the application
or updated application.
• The program’s Annual Update was not completed, not approved by the designated
institutional official (DIO), or has significant gaps in data required by the ACGME.
• For an application or updated application, required attachment documents were not
provided, are missing key information, or do not meet common and specialty-specific
requirements. For example:
o program letter(s) of agreement (PLA) not submitted, outdated, lacking the
appropriate components, or lacking requisite signatures (see I.B.2.a) and I.B.3.);
o block diagram not submitted, does not capture all required clinical experiences, or
includes participating sites that do not align with the participating sites listed in ADS;
o goals and objectives not provided, are not competency based, or are not level- or
rotation-specific; and
o the supervision policy does not reflect appropriate levels of supervision (see
Common Program Requirements VI.A.2.b) through VI.A.2.b).(3)).
• Responses to previous citations were not provided or were inadequate, if applicable.
• Program director and faculty qualifications were missing or outdated
residency/fellowship training, as well as academic appointments, licensure, and board
certification information.
• Program director and faculty curriculum vitae (CV) were incomplete or outdated
scholarly activity was included.
• Faculty and resident scholarly activity information were not submitted as part of the
Annual Update.
• ACGME Case Log or patient numeric data were not submitted or were incomplete.
• The Accreditation Field Staff spent a significant amount of time during the site visit
needing to make clarifications, corrections, and looking for missing information.
The ACGME created three brief videos available here
to help with av
oiding common errors in
the data submitted to the ACGME:
• creating a block diagram (N
OTE: some specialties require a specialty-specific block
diagram, so programs must check ADS for instructions on whether the common block
diagram instructions or specialty-specific instructions apply)
• responding to citations
©2024 Accreditation Council for Graduate Medical Education (ACGME)
56

• providing information on scholarly activity
ADS Annual Update
The ACGME will conduct an annual review of programs that achieve a status of Initial or
Continued Accreditation and provide an accreditation decision. As part of this annual review,
programs must complete the ADS Annual Update process each academic year between July
and September. The exact date varies by specialty. The program director and program
coordinator will receive a notification in ADS with a reminder to perform the required program
ADS Annual Update and a deadline. Program directors are responsible for ensuring that all
program information is updated in ADS, that the Annual Update is submitted by the program’s
due date, and that it is approved by the DIO.
Key data to be reviewed and updated during the ADS Annual Update
• Program information
o program details
o Common Program Requirements questions, clinical and educational work section,
overall evaluations methods section, etc.
o responses to current citations, if applicable
o major changes and other program updates section
o The sites tab and added, deleted, or updated information for each participating site
o current block diagram, if applicable
• Faculty information
o the program director’s profile and CV, if applicable
o all physician and non-physician faculty members’ profiles and CVs (if applicable)
accuracy of all information and dates
number limitations for current professional activities, selected bibliography,
review articles, chapters, and/or textbooks
removal of program director and faculty scholarly activities which occurred more
than five years ago
For the physician and non-physician faculty rosters, accuracy of information,
including board certification, identification of an individual as a core faculty
member, and time spent in the program
o Faculty scholarly activity for the previous academic year
• Resident information
o resident profiles; identification of new residents to the program, confirmation or
updating of PGY level, and identification of graduating residents
o resident ultimate certification status for graduates from seven years prior.
o resident scholarly activity for the previous academic year
ADS screenshot: program annual update checklist
When logging into ADS, on the Program Overview tab, the program director and/or program
coordinator can see a checklist of all information that should be reviewed and updated during
the Annual Update. (See accompanying screenshots which follow on the next page.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
57

Block diagrams
When completing an application for accreditation of a new program in ADS, instructions are
provided for completing a block diagram. Subsequently, the block diagram may need to be
updated during the ADS Annual Update to reflect changes in the program.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
58

ADS screenshot: common block diagram instructions
ADS screenshot: specialty-specific block diagram instructions
Some Review Committees have created specialty-specific block diagrams and do not accept
the common block diagram. For these specialties, the program will not see the sample block
diagram in ADS, but rather a link to the specialty instructions on the ACGME specialty-specific
web page.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
59
Review Committees use block diagrams:
• to review rotation length(s);
• to get a summary of time spent at each participating site; and
• to get a summary of time spent on each rotation type
The block diagram must clearly illustrate the length of rotations in a program. Rotation length
has educational implications since longer rotations provide more opportunities for the educators
on that rotation to observe and assess the residents, providing more accurate evaluations and
increased opportunities to provide feedback. Rotation length also has clinical implications in that
short rotations increase the number of team turnovers. The block diagram also provides a
summary of the types of clinical experiences and the time spent at each participating site. An
accurate block diagram therefore illustrates how much cumulative time a resident spends in a
particular clinical experience or subspecialty area at all of the participating sites used by the
program.
Programs may use the block diagram:
• to ensure that Program Requirements are met (by documenting the participating site and
the program year during which required experiences take place, the block diagram helps
programs ensure that the Program Requirements are being met);
• to ensure that certifying board requirements are met (many certifying boards require that
candidates fulfill certain chronological educational requirements);
• in recruitment of residents (an accurate and complete block diagram may provide
potential applicants a quick yet detailed snapshot of what they can expect each year in
the program); and
• when a program is contemplating or requesting a permanent increase of its resident
complement (block diagrams for each of the years anticipated for the transition to the
new full complement are extremely useful to—and required by—the Review Committee,
allowing the program to ensure that each rotation and participating site will have an
appropriate number of residents at any time during the transition).
NOTE: Rotation schedules for individual residents are important for use by the residents, faculty
members, and other personnel involved in a program, but rotation schedules are NOT block
diagrams, and are not required by the ACGME. A block diagram is not a depiction of the rotation
schedule of an individual resident.
A block diagram:
• depicts the rotations assigned in each program year (a block diagram shows each of the
rotations a resident will typically be assigned in each year of the program, the amount of
time that a resident spends on each of these rotations, and the participating sites the
rotations occur at);
• is flexible in defining rotation lengths (a block diagram can show rotations as short as
one week or as long as several months) and
• provides other important information, such as
o inpatient time on a rotation;
o outpatient time on a rotation;
o research time on a rotation; and
o rotation(s) offering particular required experience(s).
©2024 Accreditation Council for Graduate Medical Education (ACGME)
60
Tips for completing the block diagram
• Show program name and number.
• Clearly identify each clinical site.
• Use participating site numbers from ADS.
• Clearly explain any abbreviations.
• Clearly explain any local jargon.
• Differentiate rotations with the same name.
• Identify rotations for key clinical experience.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
61

COMMON PROGRAM REQUIREMENTS
II. Personnel
II.A Program Director
II.A.4. Program Director Responsibilities
II.A.4.a) The program director must:
II.A.4.a).(7)
provide a learning and working environment in which
residents have the opportunity to raise concerns, report
mistreatment, and provide feedback in a confidential manner
as appropriate, without fear of intimidation or retaliation;
(Core)
II.A.4.a).(8)
ensure the program’s compliance with the Sponsoring
Institution’s policies and procedures related to grievances
and due process, including when action is taken to suspend
or dismiss, or not to promote or renew the appointment of a
resident;
(Core)
Background and Intent: A program does not operate independently of its Sponsoring
Institution. It is expected that the program director will be aware of the Sponsoring
Institution’s policies and procedures and will ensure they are followed by the
program’s leadership, faculty members, support personnel, and residents.
II.A.4.a).(9) ensure the program’s compliance with the Sponsoring
Institution’s policies and procedures on employment and
non-discrimination;
(Core)
II.A.4.a).(9).(a) Residents must not be required to sign a non-
competition guarantee or restrictive covenant.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
62

GUIDANCE
II.A.4.a).(7) Raising concerns, providing feedback, and submitting grievances
There must be both institutional and programmatic processes that support residents in raising
concerns, reporting mistreatment, and providing feedback confidentially and without fear of
retaliation. Residents should first attempt to address concerns within their programs. In some
programs, chief residents, junior faculty members, or administrators facilitate communication
between residents and program leaders by conveying residents’ concerns and feedback in a
confidential manner. Programs may solicit residents’ concerns and feedback confidentially using
program evaluations, rotation evaluations, class or program meetings, and other means.
If attempts to address concerns within the program are ineffective, residents must be able to
raise concerns, report mistreatment, or provide feedback confidentially and without fear of
retaliation through institutional mechanisms (see Institutional Requirement III.A.
), which m
ay
include specific, confidential reporting processes related to patient safety events, supervision
concerns, or professionalism issues. Avenues to raise concerns and provide feedback outside
of the program may involve the designated institutional official (DIO), other institutional officers,
and/or groups, such as resident/fellow forums or the Graduate Medical Education Committee
(GMEC).
As
stated in Institutional Requirement IV.E.: “The S
ponsoring Institution must have a policy that
outlines the procedures for submitting and processing resident/fellow grievances at the program
and institutional level and that minimizes conflicts of interest.” This requirement ensures there
are formal processes through which residents can address concerns about their education or
the clinical learning environment. Sponsoring Institutions and programs must manage conflicts
of interest of individuals or groups who make decisions in grievance processes. Program
directors should contact the DIO if they have questions about the Sponsoring Institution’s or
program’s grievance procedures or policies.
For p
rograms applying or re-applying for accreditation and accredited programs with a status of
Initial Accreditation and Initial Accreditation with Warning, the ACGME includes the following
question in the ADS Annual Update that programs must answer or update annually until they
move to a Continued Accreditation status.
ADS screenshot: Common Program Requirements question regarding the
process of reporting problems and concerns
The ACGME’s Institutional Review Committee and/or the specialty Review Committees may
investigate potential non-compliance with these requirements indicated by the results of the
annual ACGME Resident/Fellow and/or Faculty Surveys or by complaints or concerns submitted
to the ACGME.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
63

II.A.4.a).(8) Actions against residents and due process
(See related Common Program Requirement V.A.1. on feedback and evaluation)
Each program must determine criteria for promotion and/or renewal of a resident’s appointment.
Sponsoring Institutions “must ensure that each [program] provides a resident/fellow with a
written notice of intent when that resident’s/fellow’s agreement [of appointment] will not be
renewed, when that resident/fellow will not be promoted to the next level of training, or when
that resident/fellow will be dismissed.” (Institutional Requirement IV.D.1.a)
)
There must be an institutional policy that provides due process to any resident who is
suspended or dismissed from a program, who is not promoted to the next program year, or
whose residency appointment will not be renewed. Questions about institutional policy should
be directed to the Sponsoring Institution’s DIO. Sponsoring Institutions and programs are not
required to provide due process in the remediation of residents through probation, warning, or
other locally defined disciplinary or academic actions that are not identified in the requirement.
It is common for program directors, coordinators, residents, fellows, faculty members, and DIOs
to collaborate with their local human resources or legal departments, and/or with institutional
officers/committees to ensure compliance with institutional policy related to actions against
residents and the provision of due process.
II.A.4.a).(9) Employment and discrimination
Laws and regulations concerning employment and discrimination include, but are not limited to,
those for which enforcement is overseen by the US Equal Employment Opportunity
Commission. Other federal, state, and local laws and regulations may also apply. It is common
for program directors, coordinators, residents, fellows, faculty members, and DIOs to collaborate
with their local human resources or legal departments and/or with institutional
officers/committees to ensure compliance with institutional policy related to employment and
discrimination. Sponsoring Institutions must have policies and procedures, not necessarily
GME-specific, prohibiting discrimination in employment and in the learning and working
environment, consistent with all applicable laws and regulations (
Institutional Requirement
IV.I.5.).
II.A.4.a).(9).(a) Non-competition guarantees and restrictive covenants
Sponsoring Institutions and programs must not require residents to enter into restrictive
covenants or non-competition guarantees. (See Institutional Requirement IV.M.) The
participation of residents in graduate medical education must not be contingent upon such
contractual provisions, which may limit residents’ professional options after completing their
programs.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
64

COMMON PROGRAM REQUIREMENTS
II. Personnel
II.A. Program Director
II.A.4. Program Director Responsibilities
II.A.4.a) The program director must:
II.A.4.a).(10)
document verification of education for all residents
within 30 days of completion of or departure from the
program; and,
(Core)
II.A.4.a).(11)
provide verification of an individual resident’s
education upon the resident’s request, within 30 days
and,
(Core)
Background and Intent: Primary verification of graduate medical education is
important to credentialing of physicians for further training and practice. Such
verification must be accurate and timely. Sponsoring Institution and program policies
for record retention are important to facilitate timely documentation of residents who
have previously completed the program. Residents who leave the program prior to
completion also require timely documentation of their summative evaluation.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
65

GUIDANCE
It is important to the resident, to the program itself, and to the Sponsoring Institution that
resident education be verified in a timely manner for all residents completing or departing from
the program. Such verification should be provided to residents upon their request, and to other
entities as needed. The ACGME does not specify exactly what must be included in such
verification, nor does it require that any particular format be used for such verification.
The Verification of Graduate Medical Education Training (VGMET) Form
Several organizations have collaborated to develop a Verification of Graduate Medical
Education Training (VGMET) Form that programs can use or adapt to their needs. The VGMET
Form was jointly developed by the American Hospital Association (AHA), the National
Association Medical Staff Services (NAMSS), the Organization of Program Director
Associations (OPDA), and the ACGME. It is designed to satisfy national credentialing
standards, and to be completed once (and only once) by the program director, and then copied
and reused in perpetuity.
Clarification
The VGMET Form was not designed or intended for applications for licensure or certification.
For licensure purposes, use this Federation Credentials Verification Service (FCVS) Form. The
FCVS Form can be used if the physician is using FCVS or is seeking licensure independently.
There i
s no time limit on a program’s obligation to continue providing verifications of residents’
graduate medical education appointments. Programs are accountable for ensuring timely
verifications for graduate medical education regardless of the location and control of the
relevant program records. When making major program changes or transferring program
sponsorship, program directors should work with the designated institutional official and others
to ensure that they are able to continue fulfilling their responsibility for timely verifications.
When a program closes and will no longer be accredited by the ACGME, program directors may
transfer responsibility for verifications to another party, such as the
Federation Credentials
Verification Service (FCVS) of the Federation of State Medical Boards (FSMB).
The verification of training should not be confused with the final evaluation described in the
Common Program Requirements V.A.2., which must include the specific elements outlined in
those requirements. Programs may use one form to meet both the requirement for verification
of training and final evaluation, but they must ensure that the final evaluation includes the
specific elements the ACGME requires.
Milestones information
The verification of training and education requirements do not indicate that programs should
share residents’ Milestones information with certifying bodies.
Milestones can and should be utilized in the determination by a program director that an
individual resident has satisfactorily completed the program and is able to engage in
autonomous practice of the specialty.
(See Common Program Requirement V.A.2.a).(1))
However, a resident’s attainment of a specific level on the Milestones should not be specified in
the program director’s verification of education or program completion. The Milestones were not
designed or intended for use in such high-stakes applications for credentialing, certification, and
©2024 Accreditation Council for Graduate Medical Education (ACGME)
66

licensure. The Milestones are designed as a formative judgment of progress at least twice a
year. Therefore, the ACGME actively discourages specification of Milestones achievement in
verification of education or program completion.
Milestones Resources
Programs are encouraged to visit the Milestones Resources section of the ACGME website to
review additional resources and tools.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
67

COMMON PROGRAM REQUIREMENTS
II. Personnel
II.A. Program Director
II.A.4 Program Director Responsibilities
II.A.4.a) The program director must:
II.A.4.a).(12)
provide applicants who are offered an interview with
information related to the applicant’s eligibility for the
relevant specialty board examination(s);
(Core)
[This requirement may be omitted at the discretion of the
Review Committee]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
68
GUIDANCE
While the transition to a single graduate medical education (GME) accreditation system that was
outlined in the Memorandum of Understanding among the ACGME, American Osteopathic
Association (AOA), and Association of American Colleges of Osteopathic Medicine (AACOM)
ended June 30, 2020, individuals who entered AOA-approved programs may be affected by the
transition for several years after 2020. Furthermore, the number of individuals completing
ACGME-accredited programs who will be eligible to be certified by AOA boards has increased
considerably. There are now many more permutations and combinations of educational
pathways and board-determined eligibility standards that may be confusing to sort out. The
following is an attempt to delineate some of those educational pathways and their effects on
board eligibility.
NOTE: Eligibility to enter an ACGME-accredited program is under ACGME purview and is
clearly delineated in the ACGME Institutional and Program Requirements. Eligibility for
certification in a specialty or subspecialty is individually determined by more than 40 different
American Board of Medical Specialties (ABMS) and AOA boards and can be changed at any
time by any of those boards. Accordingly, the ACGME cannot provide accurate, up-to-date
criteria for certification. It is the responsibility of the program director to ascertain and convey to
each applicant the pertinent eligibility criteria in any given specialty or subspecialty.
The following general guidance applies:
1. For a resident who enters residency directly from medical school, assuming acceptance
to and completion of the program, the individual should be eligible for specialty
certification.
o Allopathic and osteopathic physicians would be eligible for certification by an
ABMS member board.
o Osteopathic physicians would be eligible for certification by an AOA board.
Allopathic physicians in an ACGME-accredited program with Osteopathic
Recognition in a designated osteopathic position would be eligible for certification by
an AOA board. Allopathic physicians in an ACGME-accredited osteopathic
neuromusculoskeletal medicine program are also eligible for AOA board
certification in neuromusculoskeletal medicine.
2. For a resident who transfers from one program that has been accredited by the ACGME
throughout the resident’s tenure to another ACGME-accredited program, assuming
acceptance to and completion of the program, the individual should be eligible for
specialty certification.
o Allopathic and osteopathic physicians would be eligible for certification by an
ABMS member board.
o Osteopathic physicians would be eligible for certification by an AOA board.
Allopathic physicians in an ACGME-accredited program with Osteopathic
Recognition in a designated osteopathic position would be eligible for certification by
an AOA board. Allopathic physicians in an ACGME-accredited osteopathic
neuromusculoskeletal medicine program are also eligible for AOA board
certification in neuromusculoskeletal medicine.
3. For a
resident who transfers from an AOA-approved program to an ACGME-accredited
program, assuming acceptance to and completion of the program, the individual should
be eligible for specialty certification.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
69
o The individual may be eligible for certification by an ABMS member board. The
program director should check with the applicable ABMS member board to
determine eligibility.
o The individual may be eligible for certification by an AOA board. The program
director should check with the applicable AOA specialty board to determine eligibility.
4. For a resident who transfers from a program that is currently accredited by the ACGME
but that was AOA-approved when the resident entered the program, assuming
acceptance to and completion of the program, the individual should be eligible for
specialty certification.
o The individual may be eligible for certification by an ABMS member board. The
program director should check with the applicable ABMS member board to
determine eligibility.
o The individual may be eligible for certification by an AOA board. The program
director should check with the applicable AOA specialty board to determine eligibility.
Program directors MUST make this clear to all applicants, as required in Common Program
Requirement II.A.4.a).(12): “The program director must provide applicants who are offered an
interview with information related to the applicant’s eligibility for the relevant specialty board
examination(s).” This requirement is closely linked to Common Program Requirement III.A. and
we encourage you to review that section of the guide as well. A sample letter the program
director can provide to applicants to comply with this requirement is provided on the following
page.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
70
SAMPLE LETTER
Eligibility for Board Certification to Applicants to the Program
Date:
To: Residency Applicants
Re: Eligibility for Board Certification
Dear:
As part of your application and interview for a potential residency position in our program, this
letter is to notify you that this program is accredited by the Accreditation Council for Graduate
Medical Education (ACGME) and that you meet the ACGME requirements for matriculation in
our program.
Upon graduating from our program, most of our residency graduates seek board certification
from the American Board of _____ or the American Osteopathic Board of ________. Board
certification is a separate process from residency training and education and has additional
requirements. Some board organizations require that you complete all of your education in an
ACGME-accredited residency. If part of your residency education occurred in a non-ACGME-
accredited program, even if it was approved by the American Osteopathic Association or
accredited by the Royal College of Physicians and Surgeons of Canada, the College of Family
Physicians of Canada, or ACGME International (ACGME-I) with Advanced Specialty
Accreditation, there is a possibility that you may not be eligible for board certification upon
completion of your education.
It is important that you contact the appropriate certifying board to understand your eligibility for
board certification before you accept a position for residency (if offered) at our institution.
Please contact the American Board of _________________ at (website URL) or American
Osteopathic Board of ______________ at (website).
I have read this letter and understand the requirements for board certification.
____________________ ________________________
Applicant Name Applicant Signature/Date
____________________ _________________________
Program Director Name Program Director Signature/Date
©2024 Accreditation Council for Graduate Medical Education (ACGME)
71

COMMON PROGRAM REQUIREMENTS
II.B. Faculty
Faculty members are a foundational element of graduate medical education –
faculty members teach residents how to care for patients. Faculty members
provide an important bridge allowing residents to grow and become practice-
ready, ensuring that patients receive the highest quality of care. They are role
models for future generations of physicians by demonstrating compassion,
commitment to excellence in teaching and patient care, professionalism, and a
dedication to lifelong learning. Faculty members experience the pride and joy of
fostering the growth and development of future colleagues. The care they provide
is enhanced by the opportunity to teach and model exemplary behavior. By
employing a scholarly approach to patient care, faculty members, through the
graduate medical education system, improve the health of the individual and the
population.
Faculty members ensure that patients receive the level of care expected from a
specialist in the field. They recognize and respond to the needs of the patients,
residents, community, and institution. Faculty members provide appropriate
levels of supervision to residents to promote patient safety. Faculty members
create an effective learning environment by acting in a professional manner and
attending to the well-being of the residents and themselves.
Background and Intent: “Faculty” refers to the entire teaching force responsible for
educating residents. The term “faculty,” including “core faculty,” does not imply or
require an academic appointment.
II.B.1.
There must be a sufficient number of faculty members with competence to
instruct and supervise all residents.
(Core)
[The Review Committee may further specify]
II.B.2. Faculty members must:
II.B.2.a) be role models of professionalism;
(Core)
II.B.2.b)
demonstrate commitment to the delivery of safe, equitable, high-
quality, cost-effective, patient-centered care;
(Core)
II.B.2.c)
demonstrate a strong interest in the education of residents including
devoting sufficient time to the educational program to fulfill their
supervisory and teaching responsibilities;
(Core)
Background and Intent: Patients have the right to expect quality, cost-effective care
with patient safety at its core. The foundation for meeting this expectation is formed
during residency and fellowship. Faculty members model these goals and continually
strive for improvement in care and cost, embracing a commitment to the patient and
the community they serve.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
72

II.B.2.d) administer and maintain an educational environment conducive to
educating residents;
(Core)
II.B.2.e) regularly participate in organized clinical discussions, rounds,
journal clubs, and conferences; and,
(Core)
II.B.2.f) pursue faculty development designed to enhance their skills at least
annually:
(Core)
Background and Intent: Faculty development is intended to describe structured
programming developed for the purpose of enhancing transference of knowledge, skill,
and behavior from the educator to the learner. Faculty development may occur in a
variety of configurations (lecture, workshop, etc.) using internal and/or external
resources. Programming is typically needs-based (individual or group) and may be
specific to the institution or the program. Faculty development programming is to be
reported for the residency program faculty in the aggregate.
II.B.2.f).(1)
as educators and evaluators;
(Detail)
II.B.2.f).(2)
in quality improvement, eliminating health inequities, and
patient safety;
(Detail)
II.B.2.f).(3)
in fostering their own and their residents’ well-being; and,
(Detail)
II.B.2.f).(4)
in patient care based on their practice-based learning and
improvement efforts.
(Detail)
Background and Intent: Practice-based learning serves as the foundation for the
practice of medicine. Through a systematic analysis of one’s practice and review of the
literature, one is able to make adjustments that improve patient outcomes and care.
Thoughtful consideration to practice-based analysis improves quality of care, as well
as patient safety. This allows faculty members to serve as role models for residents in
practice-based learning.
[The Review Committee may further specify additional faculty
responsibilities]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
73

GUIDANCE
II.B. Faculty
As a foundational element of graduate medical education, faculty members have numerous
responsibilities in the education of residents. Selection of faculty members should be carefully
considered to ensure they fulfill the stated requirements that follow. In addition to providing
consistently high-quality patient care, faculty members must teach and supervise residents in
the provision of equivalent high-quality care and allow graded supervision that enables residents
to achieve readiness for autonomous practice at the end of their training and education. Non-
clinical faculty members should be similarly capable in their areas of expertise. Faculty
members should be effective in the provision of both formal and informal, written and oral
feedback and participate in faculty development activities to enhance their teaching and
evaluative skills. They should demonstrate a commitment to the education of residents and to
the privilege of training the next generation of physicians.
The Background and Intent for this requirement clarifies that the term “Faculty” refers to the
entire teaching force responsible for educating residents. The term “faculty,” including “core
faculty,” does not imply or require an academic appointment.
II.B.1. Need for a sufficient number of faculty members
The requirement is intended to ensure that there are enough competent faculty members to
teach and supervise residents at all participating sites. Participating sites cannot be selected
solely based on the availability of a specific procedure or a unique patient care experience in the
absence of faculty members with the interest, ability, and commitment to resident education.
[The Review Committee may further specify]
Programs should reference the specialty-specific Program Requirements to ensure they are
compliant with the minimum number of faculty members and/ or faculty-to-resident ratio
requirements of their particular specialty. Programs may also reference the Number of Facult
y
document available on the Institutional Application and Requirements page of the Institutional
Review Committee section of the ACGME website.
II.B.2.a)-c) Faculty Members as role models of professionalism, commitment to
delivery of safe, quality, cost-effective, patient-centered care
In addition to being role models, faculty members must also demonstrate a strong interest in the
education of residents. Residents learned the most about professionalism from observing
faculty member role models. (Brownell, A. Keith W., and Luc Côté. 2001. “Senior Residents’
Views on the Meaning of Professionalism and How They Learn about It.” Academic Medicine
76,(7): 734–37. https://doi.org/10.1097/00001888-200107000-00019
.)
Faculty members must also have sufficient time to fulfill their responsibilities. Some faculty
members may need defined protected time to fulfill their responsibilities, while other faculty
members can supervise and teach within their defined assignments. Sufficient time for resident
education is a shared responsibility of individual faculty members and the department or
institution. Pressure for clinical productivity must not preclude sufficient time to teach and
supervise residents in the program.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
74

II.B.2.d) Faculty members as part of administration and maintenance of an
educational environment conducive to educating residents
An educational environment includes more elements than the provision of patient care. An
environment geared toward resident education allows time for questions and discussions which
support evidence-based medical decision making. There should be appropriate discussions
about the evidence-based references, pathophysiology, and rationale of clinical decisions to a
sufficient degree to maintain an environment of continuous learning.
II.B.2.e) Faculty member participation in organized clinical discussion, rounds,
journal clubs, and conferences
Formal didactic educational activities should include experienced faculty members who can
provide commentary and clinical insights to augment the information being presented. All faculty
members do not need to participate in all didactic activities. However, it is inappropriate for
residents to consistently lead organized didactic experiences without a faculty presence.
II.B.2.f).(1)-(4) Faculty members pursuit of faculty development designed to
enhance skills as an educator, quality improvement and patient safety, well-
being, and patient care
Programs should ensure that there are opportunities for their faculty members to participate in
professional development activities designed to optimize their skills. Faculty members should
participate annually in faculty development activities in one of these four areas: as an educator,
quality improvement and patient safety, fostering their own and their residents’ well-being, and
patient care based on their practice-based learning and improvement efforts. This does not
preclude faculty development in other important areas such as clinical knowledge, leadership,
team building, communications, and patient relationships.
The Background and Intent states that faculty development is intended to describe structured
programming developed for the purpose of enhancing transference of knowledge, skill, and
behavior from the educator to the learner. Faculty development may occur in a variety of
configurations (lecture, workshop, etc.) using internal and/or external resources. Programming
is typically needs based (individual or group) and may be specific to the institution or the
program. Faculty development programming is to be reported for the residency program faculty
in the aggregate.
[The Review Committee may further specify additional faculty responsibilities]
Review Committees may specify other requirements related to additional faculty responsibilities,
so programs must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
Questions about specialty-specific Program Requirements related to program director
qualifications should be directed to specialty Review Committee staff.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
75

COMMON PROGRAM REQUIREMENTS
II.B.3. Faculty Qualifications
II.B.3.a) Faculty members must have appropriate qualifications in their field
and hold appropriate institutional appointments.
(Core)
[The Review Committee may further specify]
II.B.3.b) Physician faculty members must:
II.B.3.b).(1) have current certification in the specialty by the American
Board of _____ or the American Osteopathic Board of _____,
or possess qualifications judged acceptable to the Review
Committee.
(Core)
[The Review Committee may further specify additional qualifications
and/or requirements regarding non-physician faculty]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
76
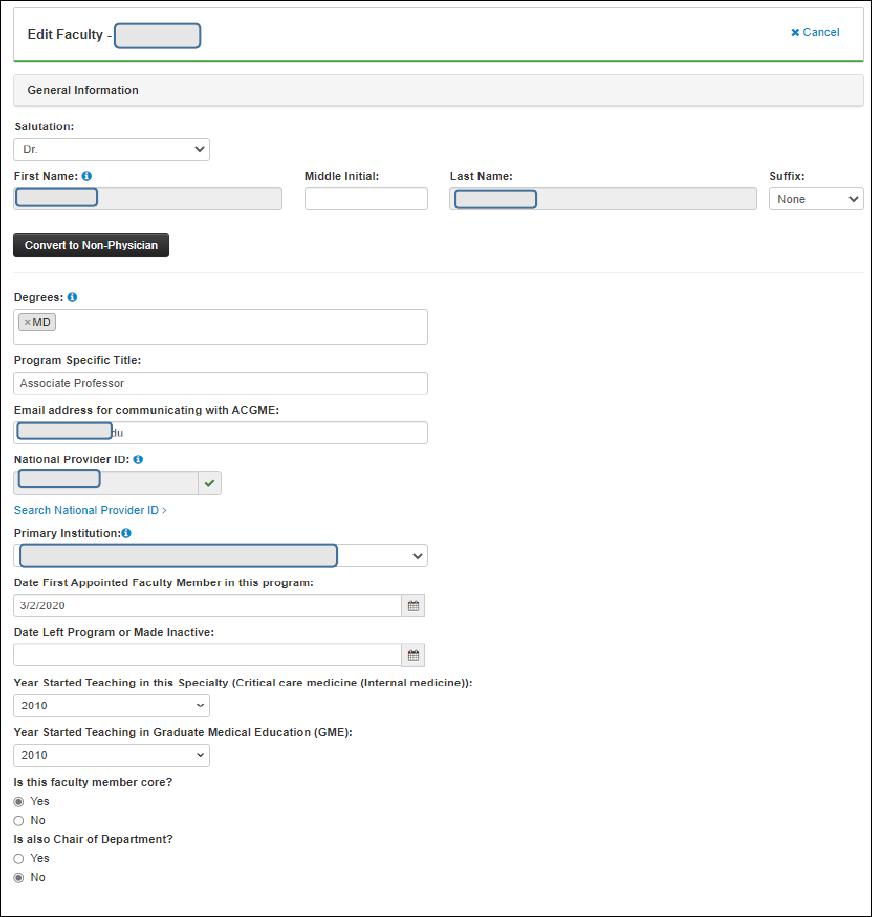
GUIDANCE
II.B.3.a) Faculty members must have appropriate qualifications in their field and
hold appropriate institutional appointments.
Minimum faculty member qualifications include having specialty or subspecialty board
certification, a license to practice, and appropriate institutional appointment. Additional
qualifications include expertise in the field and skills as an educator. Faculty information is
captured in the faculty profile and curriculum vitae (CV) in the Accreditation Data System (ADS).
Programs should complete all required information when adding a new faculty member into
ADS. It is also important to carefully review and update all the faculty information if a profile for
that individual already exists in ADS and you are importing the profile into your program.
ADS screenshots: faculty profile and CV
©2024 Accreditation Council for Graduate Medical Education (ACGME)
77

©2024 Accreditation Council for Graduate Medical Education (ACGME)
78

II.B.3.b) Physician faculty members must have current certification in the
specialty by the ABMS or AOA, or possess qualifications judged acceptable to
the Review Committee.
Some Review Committees will accept only certification in the appropriate specialty by an
American Board of Medical Specialties (ABMS) member board or American Osteopathic
Association (AOA) certifying board for the program director. Other Review Committees will
accept other qualifications for the program director. Programs are encouraged to refer to the
specialty-specific Program Requirements
for more information on this requirement.
The ACGME automatically populates data received from the ABMS and the AOA for all faculty
members on their individual ADS faculty profile page, where data are available. Physician
faculty members’ board certification data will be matched to the ABMS and AOA datasets based
on National Provider Identifier (NPI) number, as well as name, date of birth, and medical school
graduation year. Faculty members who are newly entered into ADS will have their certification
information matched and populated within 24 hours.
Programs are only required to provide a manual entry for faculty members’ specialty certification
if:
• No ABMS/AOA board certification data is displayed in ADS or it is incorrect. In this case,
a manual entry for “ABMS missing/inaccurate data” or “AOA missing/inaccurate data”
should be added on the faculty’s profile with a duration type, initial certification year,
certification name, and an explanation for Review Committee consideration.
• The faculty member is not certified by the ABMS/AOA. Add a manual entry of “Not Board
Certified” and an explanation.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
79

• The faculty member is board eligible but has not yet achieved board certification. Add a
manual entry of “Board eligible” and provide an explanation.
• The faculty member is certified by another certifying body. Some Review Committees
allow other acceptable specialty qualifications and therefore a manual entry of “Other
Certifying Body” can provide that information.
ADS screenshot: specialty certification – manual entries
Common issues related to the ABMS and AOA data not auto-populating on the faculty profile
and in the faculty roster include:
• The NPI number in ADS is incorrect or does not match the NPI number in the
ABMS/AOA dataset.
• A lag in when updated board certification data are received by the ACGME from the
ABMS and AOA.
Non-physicians are often important contributors to programs and warrant appointment to the
faculty. These individuals may bring specialized expertise in public health, patient safety,
laboratory science, pharmacology, basic science, research, a specific procedural skill, or other
important aspects of medicine. Non-physician educators may provide valuable contributions to
the residents’ knowledge and skills. If the program director determines that the contribution of a
non-physician individual is significant to the education of the residents, the program director
may designate the individual as a faculty member or a core faculty member.
ADS screenshot: non-physician faculty qualifications
©2024 Accreditation Council for Graduate Medical Education (ACGME)
80

[The Review Committee may further specify]
Review Committees may specify other requirements related to faculty qualifications, specialty
certification and non-physician faculty, so programs must review the specialty-specific Program
Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
Questions about specialty-specific Program Requirements related to faculty qualifications
should be directed to specialty Review Committee staff.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
81
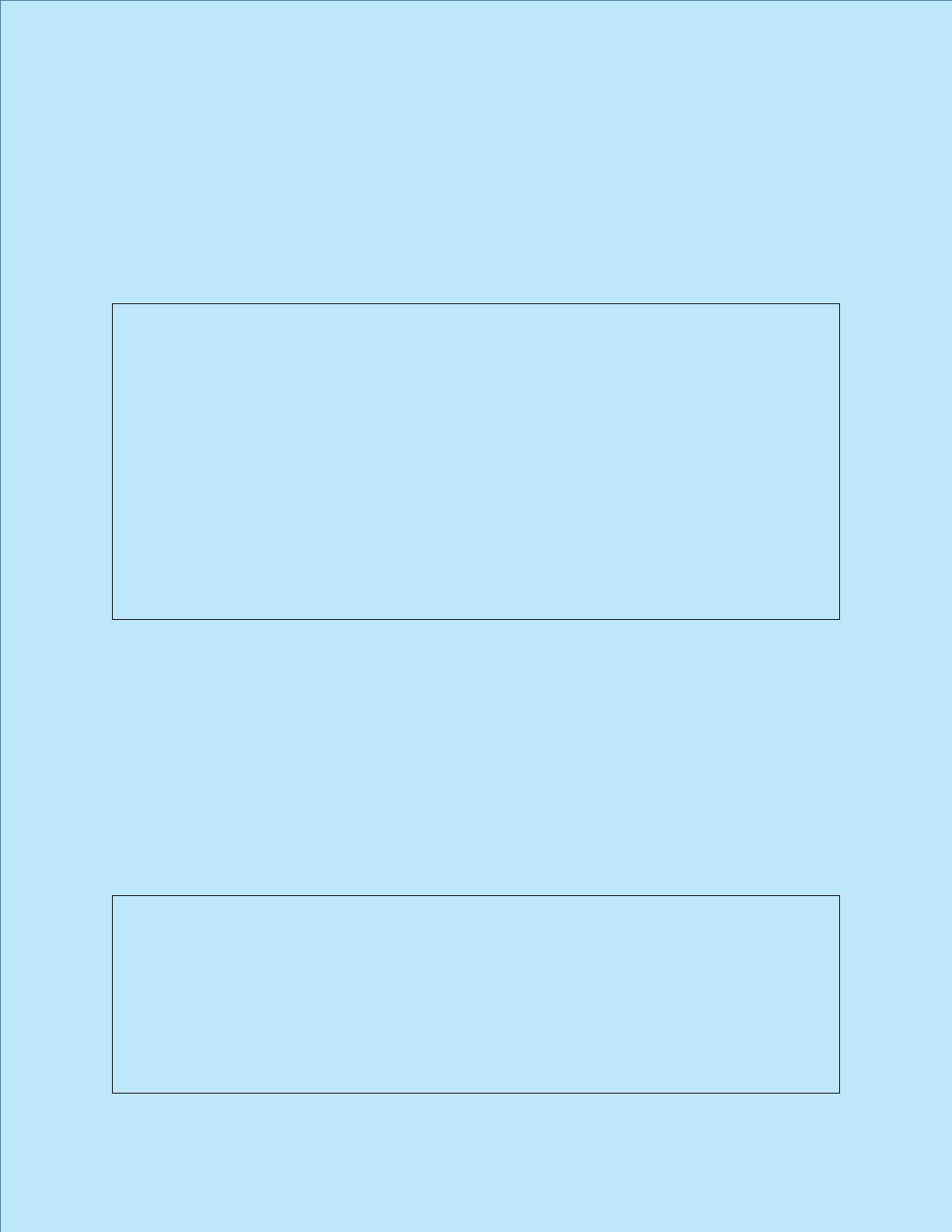
COMMON PROGRAM REQUIREMENTS
II.B.4. Core Faculty
Cor
e faculty members must have a significant role in the education and
supervision of residents and must devote a significant portion of their entire effort
to resident education and/or administration, and must, as a component of their
activities, teach, evaluate, and provide formative feedback to residents.
(Core)
Background and Intent: Core faculty members are critical to the success of resident
education. They support the program leadership in developing, implementing, and
assessing curriculum, mentoring residents, and assessing residents’ progress toward
achievement of competence in and the independent practice of the specialty. Core
faculty members should be selected for their broad knowledge of and involvement in
the program, permitting them to effectively evaluate the program. Core faculty
members may also be selected for their specific expertise and unique contribution to
the program. Core faculty members are engaged in a broad range of activities, which
may vary across programs and specialties. Core faculty members provide clinical
teaching and supervision of residents, and also participate in non-clinical activities
related to resident education and program administration. Examples of these non-
clinical activities include, but are not limited to, interviewing and selecting resident
applicants, providing didactic instruction, mentoring residents, simulation exercises,
completing the annual ACGME Faculty Survey, and participating on the program’s
Clinical Competency Committee, Program Evaluation Committee, and other GME
committees.
II.B
.4.a) Core faculty members must complete the annual ACGME Faculty
Survey.
(Core)
[The Review Committee must specify the minimum number of core
faculty and/or the core faculty-resident ratio]
[The Review Committee may further specify either:
1) requirements regarding dedicated time and support for core
faculty members’ non-clinical responsibilities related to
resident education and/or administration of the program, or]
2) requirements regarding the role and responsibilities of core
faculty members, inclusive of both clinical and non-clinical
activities, and the corresponding time commitment required
to meet those responsibilities.]
If the Review Committee adds requirements as described in number (1) above, the
Review Committee may choose to include background and intent as follows:
Background and Intent: Provision of support for the time required for the core
faculty members’ responsibilities related to resident education and/or
administration of the program, as well as flexibility regarding how this support
is provided, are important. Programs, in partnership with their Sponsoring
Institutions, may provide support for this time in a variety of ways. Examples of
support may include, but are not limited to, salary support, supplemental
compensation, educational value units, or relief of time from other professional
duties.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
82

It is important to remember that the dedicated time and support requirement is a
minimum, recognizing that, depending on the unique needs of the program,
additional support may be warranted. The need to ensure adequate resources,
including adequate support and dedicated time for the core faculty members, is
also addressed in Institutional Requirement II.B.2. The amount of support and
dedicated time needed for individual programs will vary based on a number of
factors and may exceed the minimum specified in the applicable specialty-
/subspecialty-specific Program Requirements.
If the Review Committee adds requirements as described in number (2) above, the
following Background and Intent must be included:
Background and Intent: The core faculty time requirements address the role and
responsibilities of core faculty members, inclusive of both clinical and
nonclinical activities, and the corresponding time to meet those responsibilities.
The requirements do not address how this is accomplished, and do not
mandate dedicated or protected time for these activities. Programs, in
partnership with their Sponsoring Institutions, will determine how compliance
with the requirements is achieved.
[The
Review Committee may specify requirements specific to
associate program director(s)]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
83

GUIDANCE
II.B.4. Core faculty
Core faculty members have responsibilities specific to the educational program. These
individuals may be associate/assistant program directors, participating site directors, conference
organizers, or subspecialty experts responsible for a segment of the curriculum. They may be
members of the Program Evaluation Committee and/or Clinical Competency Committee, have
expertise in medical education, or be health care professionals dedicated to the program who
are developing into future educational leaders.
As the Background and Intent for this requirement states, “Core faculty members are critical to
the success of resident education. They support the program leadership in developing,
implementing, and assessing curriculum, mentoring residents, and assessing residents’
progress toward achievement of competence in and the independent practice of the specialty.”
II.B.4.a) Core faculty members must complete the ACGME Faculty Survey.
Core faculty members are expected to complete the annual ACGME Faculty Survey, which is
one of the instruments used by specialty Review Committees to assess programs. Therefore,
core faculty members should be selected for their broad knowledge of and involvement in the
program, which provides them with the insight necessary to effectively evaluate the program.
[The Review Committee must specify the minimum number of core faculty and/or
the core faculty-resident ratio]
Since Review Committees must specify minimum number of core faculty, programs must review
the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
It is the responsibility of the program director to determine which members of the faculty best
meet the needs of the program and to designate those individuals as core faculty members in
the Accreditation Data System (ADS). As stated in the Background and Intent for this
requirement, “Core faculty members should be selected for their broad knowledge of and
involvement in the program, permitting them to effectively evaluate the program. Core faculty
members may also be selected for their specific expertise and unique contribution to the
program. Core faculty members are engaged in a broad range of activities, which may vary
across programs and specialties. Core faculty members provide clinical teaching and
supervision of residents, and also participate in non-clinical activities related to resident
education and program administration. Examples of these non-clinical activities include, but are
not limited to, interviewing and selecting resident applicants, providing didactic instruction,
mentoring residents, simulation exercises, completing the annual ACGME Faculty Survey, and
participating on the program’s Clinical Competency Committee, Program Evaluation Committee,
and other GME committees.”
©2024 Accreditation Council for Graduate Medical Education (ACGME)
84

ADS screenshots: designating core faculty in ADS
1. Programs can designate individual faculty members as core/non-core.
2. Programs can designate multiple faculty members as core/non-core at the
same time.
[The Review Committee may further specify requirements regarding dedicated
time and support for or the role and responsibilities of core faculty members]
The Core Faculty Dedicated Time summary document included on the ACGME website
provides a snapshot of the core faculty dedicated time and support across all ACGME-
accredited specialties.
ADS Screenshot: program resources – percent of FTE support – core faculty (if
applicable)
As
part of a new a program application as well as the Accreditation Data System (ADS) Annual
Update process, programs must provide the percent of FTE support allocated to core faculty, if
applicable for their specialty.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
85

[The Review Committee may specify requirements specific to associate program
director(s)]
Programs should consult the specialty-specific Program Requirements for further specification.
ADS screenshot: program resources – percent of FTE support – associate
program director(s) (if applicable)
As part of a new program application as well as the Accreditation Data System (ADS) Annual
Update process, programs must provide the percent of FTE support allocated to associate
program director(s), if applicable for their specialty.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
86

COMMON PROGRAM REQUIREMENTS
II.C. Program Coordinator
II.C
.1.
II.C
.2.
There must be a program coordinator.
(Core)
The program coordinator must be provided with dedicated time and
support adequate for administration of the program based upon its size
and configuration.
(Core)
[The Review Committee must further specify minimum dedicated time for
the program coordinator.]
Background and Intent: The requirement does not address the source of funding
required to provide the specified salary support.
Each pr
ogram requires a lead administrative person, frequently referred to as a
program coordinator, administrator, or as otherwise titled by the institution. This
person will frequently manage the day-to-day operations of the program and serve as
an important liaison and facilitator between the learners, faculty and other staff
members, and the ACGME. Individuals serving in this role are recognized as program
coordinators by the ACGME.
The
program coordinator is a key member of the leadership team and is critical to the
success of the program. As such, the program coordinator must possess skills in
leadership and personnel management appropriate to the complexity of the program.
Program coordinators are expected to develop in-depth knowledge of the ACGME and
Program Requirements, including policies and procedures. Program coordinators
assist the program director in meeting accreditation requirements, educational
programming, and support of residents.
Pr
ograms, in partnership with their Sponsoring Institutions, should encourage the
professional development of their program coordinators and avail them of
opportunities for both professional and personal growth. Programs with fewer
residents may not require a full-time coordinator; one coordinator may support more
than one program.
The
minimum required dedicated time and support specified in II.C.2.a) is inclusive of
activities directly related to administration of the accredited program. It is understood
that coordinators often have additional responsibilities, beyond those directly related
to program administration, including, but not limited to, departmental administrative
responsibilities, medical school clerkships, planning lectures that are not solely
intended for the accredited program, and mandatory reporting for entities other than
the ACGME. Assignment of these other responsibilities will necessitate consideration
of allocation of additional support so as not to preclude the coordinator from devoting
the time specified above solely to administrative activities that support the accredited
program.
In addition, it is important to remember that the dedicated time and support
requirement for ACGME activities is a minimum, recognizing that, depending on the
©2024 Accreditation Council for Graduate Medical Education (ACGME)
87
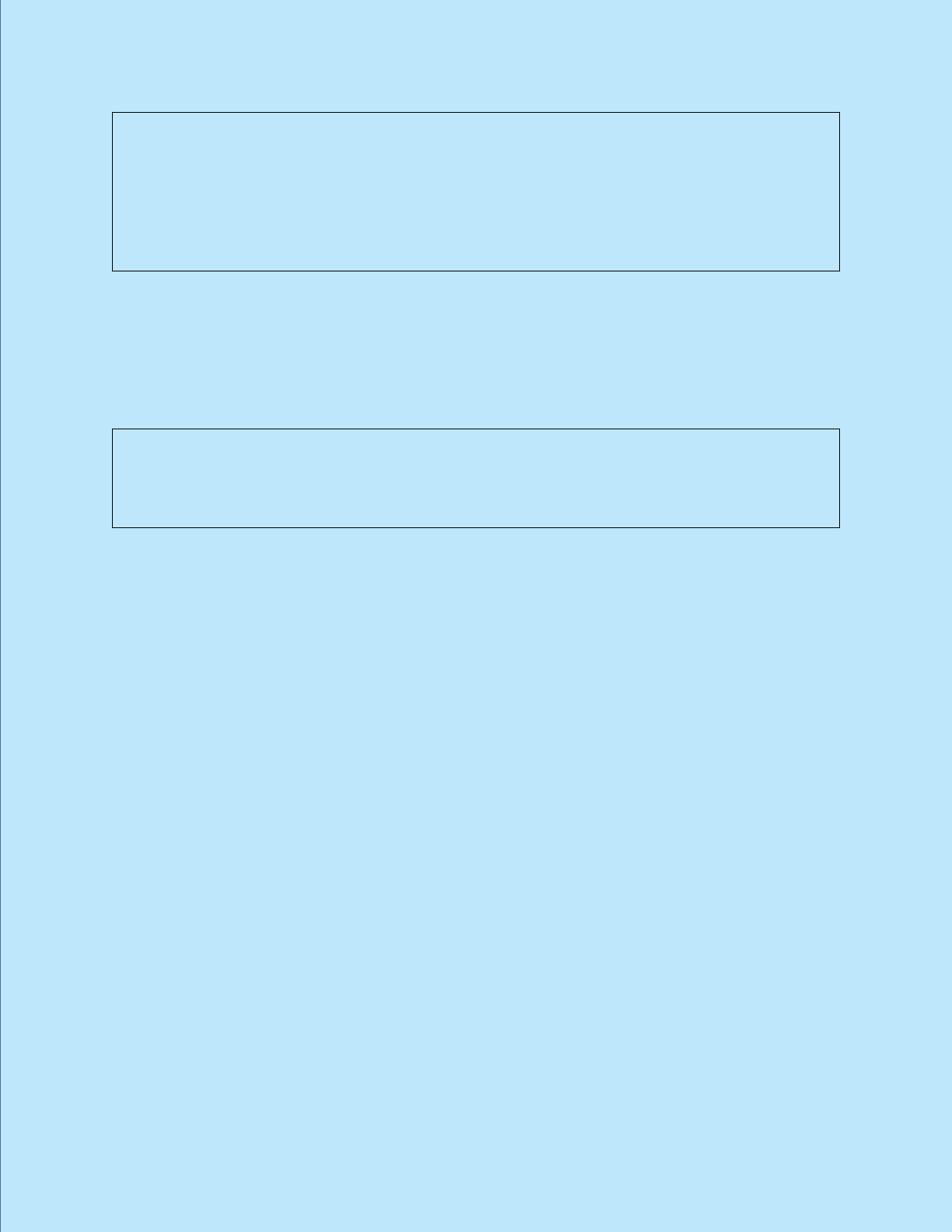
unique needs of the program, additional support may be warranted. The need to
ensure adequate resources, including adequate support and dedicated time for the
program coordinator, is also addressed in Institutional Requirement II.B.4. The amount
of support and dedicated time needed for individual programs will vary based on a
number of factors and may exceed the minimum specified in the applicable
specialty/subspecialty-specific Program Requirements. It is expected that the
Sponsoring Institution, in partnership with its accredited programs, will ensure support
for program coordinators to fulfill their program responsibilities effectively.
II.D. Other Program Personnel
The program, in partnership with its Sponsoring Institution, must jointly ensure
the availability of necessary personnel for the effective administration of the
program.
(Core)
[The Review Committee may further specify]
Background and Intent: Multiple personnel may be required to effectively administer a
program. These may include staff members with clerical skills, project managers,
education experts, and staff members to maintain electronic communication for the
program. These personnel may support more than one program in more than one
discipline.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
88

GUIDANCE
II.C. Program coordinator
Common Program Requirement II.C.1. specifies that each program must have a program
coordinator. Requirement II.C.2. further specifies that the program coordinator must be provided
with dedicated time and support adequate for administration of the program based upon its size
and configuration.
[The Review Committee must further specify minimum dedicated time for the
program coordinator.]
Since Review Committees must specify minimum dedicated time for the program coordinator,
programs must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
The Coordinator Dedicated Time
summary document included as an institutional resource also
provides a snapshot of the program coordinator dedicated time and support across all ACGME-
accredited specialties.
The Bac
kground and Intent for Common Program Requirement II.C. explains that “each
program requires a lead administrative person, frequently referred to as a program coordinator,
administrator, or as otherwise titled by the institution. This person will frequently manage the
day-to-day operations of the program and serve as an important liaison and facilitator between
the learners, faculty and other staff members, and the ACGME. Individuals serving in this role
are recognized as program coordinators by the ACGME.” In that same section, the ACGME also
recognizes that “the program coordinator is a key member of the leadership team and is critical
to the success of the program. As such, the program coordinator must possess skills in
leadership and personnel management appropriate to the complexity of the program. Program
coordinators are expected to develop in-depth knowledge of the ACGME and Program
Requirements, including policies and procedures. Program coordinators assist the program
director in meeting accreditation requirements, educational programming, and support of
residents.”
Other important considerations described in the Background and Intent for this requirement
include the following:
• The source of funding for the specified salary support is not addressed.
• Programs, in partnership with their Sponsoring Institutions, should encourage the
professional development of their program coordinators.
• Programs with fewer residents may not require a full-time coordinator; one coordinator
may support more than one program so long as the individual’s total dedicated time
across programs does not exceed 100 percent FTE.
• The minimum required dedicated time and support specified in Common Program
Requirement II.C.2.a) is inclusive of activities directly related to administration of the
accredited program.
• Assignment of other responsibilities, beyond those directly related to program
administration, will necessitate consideration of allocation of additional support.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
89

• The dedicated time and support requirement for ACGME activities is a minimum,
recognizing that, depending on the unique needs of the program, additional support may
be warranted.
The ACGME monitors compliance with requirements in section II.C. in various ways, including:
• questions answered by program leadership as part of an application or during the ADS
Annual Update; and
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
ADS screenshot: program resources – percent of FTE support – program
coordinators
As part of a new program application as well as the Accreditation Data System (ADS) Annual
Update process, programs must provide the percent of FTE support allocated to the program
coordinator(s).
II.D. Other program personnel
[The Review Committee may further specify]
Programs should review the specialty-specific Program Requirements for further specification, if
applicable.
The Background and Intent for this requirement explains that in addition to program
coordinators, there may be others needed to help in the administration of a program. These
individuals may include project managers, experts in education and/or communication, and
those with clerical skills. These individuals may provide support for more than one program in
more than one specialty.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
90

COMMON PROGRAM REQUIREMENTS
III. Resident Appointments
III.A. Eligibility Requirements
III.A.1. An applicant must meet one of the following qualifications to be
eligible for appointment to an ACGME-accredited program:
(Core)
III.A.1.a) graduation from a medical school in the United States or
Canada, accredited by the Liaison Committee on Medical
Education (LCME) or graduation from a college of
osteopathic medicine in the United States, accredited by the
American Osteopathic Association Commission on
Osteopathic College Accreditation (AOACOCA); or,
(Core)
III.A.1.b) graduation from a medical school outside of the United
States or Canada, and meeting one of the following additional
qualifications:
(Core)
III.A.1.b).(1) holding a currently valid certificate from the
Educational Commission for Foreign Medical
Graduates (ECFMG) prior to appointment; or,
(Core)
III.A.1.b).(2) holding a full and unrestricted license to practice
medicine in the United States licensing jurisdiction in
which the ACGME-accredited program is located.
(Core)
III.A.2. All prerequisite post-graduate clinical education required for initial
entry or transfer into ACGME-accredited residency programs must
be completed in ACGME-accredited residency programs, AOA
approved residency programs, Royal College of Physicians and
Surgeons of Canada (RCPSC)-accredited or College of Family
Physicians of Canada (CFPC)-accredited residency programs
located in Canada, or in residency programs with ACGME
International (ACGME-I) Advanced Specialty Accreditation.
(Core)
III.A.2.a) Residency programs must receive verification of each
resident’s level of competency in the required clinical field
using ACGME, CanMEDS, or ACGME-I Milestones evaluations
from the prior training program upon matriculation.
(Core)
[The Review Committee may further specify prerequisite
postgraduate clinical education]
Background and Intent: Programs with ACGME-I Foundational Accreditation or from
institutions with ACGME-I accreditation do not qualify unless the program has also
achieved ACGME-I Advanced Specialty Accreditation. To ensure entrants into ACGME-
accredited programs from ACGME-I programs have attained the prerequisite
milestones for this training, they must be from programs that have ACGME-I Advanced
Specialty Accreditation.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
91

III.A.3. Resident Eligibility Exception
The Review Committee for ______ will allow the following exception to the
resident eligibility requirements:
(Core)
[Note: A Review Committee may permit the eligibility exception if the
specialty requires completion of a prerequisite residency program prior to
admission. If the specialty-specific Program Requirements define multiple
program formats, the Review Committee may permit the exception only for
the format(s) that require completion of a prerequisite residency program
prior to admission. If this language is not applicable, this section will not
appear in the specialty-specific requirements.]
III.A.4.a) An ACGME-accredited residency program may accept an
exceptionally qualified international graduate applicant who does
not satisfy the eligibility requirements listed in III.A.1. - II.A.2., but
who does meet all of the following additional qualifications and
conditions:
(Core)
III.A.4.a).(1) evaluation by the program director and residency selection
committee of the applicant’s suitability to enter the program,
based on prior training and review of the summative
evaluations of this training; and,
(Core)
III.A.4.a).(2) review and approval of the applicant’s exceptional
qualifications by the GMEC; and,
(Core)
III.A.4.a).(3) verification of Educational Commission for Foreign Medical
Graduates (ECFMG) certification.
(Core)
III.A.4.b) Applicants accepted through this exception must have an evaluation
of their performance by the Clinical Competency Committee within
12 weeks of matriculation.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
92

GUIDANCE
In addition to the Common Program Requirements related to resident eligibility requirements,
program directors must comply with the policies and procedures of the Sponsoring Institution
and the ACGME Institutional Requirements for resident appointment. See Institutional
Requirements IV.B., IV.B.1., and IV.B.2. for additional information.
III.A.1. Eligibility Requirements
The following links provide helpful information about residency eligibility requirements:
• United States Doctor of Medicine (MD) graduates
−
Liaison Committee on Medical
Education (LCME)
• United States Doctor of Osteopathic Medicine (DO) graduates
−
American Osteopathic
Association (AOA) Commission on Osteopathic College Accreditation (AOA-COCA)
• Canada jointly with LCME Doctor of Medicine (MD) graduates
−
Committee on
Accreditation of Canadian Medical Schools (CACMS)
Residents who completed an AOA-approved program that became ACGME accredited during
the transition to a single graduate medical education (GME) accreditation system may be
eligible for American Board of Medical Specialties (ABMS) and/or AOA board certification.
While program accreditation is under the purview of the ACGME, individual board certification is
under the jurisdiction of the individual certifying boards. For individual specialty board qualifying
information, program directors and residents must communicate with the applicable certifying
board.
ADS screenshots: resident eligibility requirements
The ACGME collects information on each resident during the Accreditation Data System (ADS)
Annual Update process when programs input new residents into ADS and update their resident
roster. Information collected includes the type of medical school the resident graduated from,
the graduation date, and the Educational Commission for Foreign Medical Graduates (ECFMG)
certificate where applicable. (See accompanying screenshots which follow on the next pages.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
93

©2024 Accreditation Council for Graduate Medical Education (ACGME)
94

The table below provides definitions of the different resident statuses:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
95

III.A.2. Prerequisite post-graduate clinical education required for initial entry or
transfer into ACGME-accredited residency programs
Prerequisite post-graduate clinical education must be obtained in the following types of
programs:
• ACGME-accredited residency programs
• AOA-approved residency programs
• Royal College of Physicians and Surgeons of Canada (RCPSC)-accredited or College of
Family Physicians of Canada (CFPC)-accredited residency programs located in Canada
• Residency programs with ACGME International (ACGME-I) Advanced Specialty
Accreditation
III.A.2.a) Verification of competence using Milestones evaluations in the required
clinical field
To verify the competence of each matriculating resident, all prerequisite post-graduate clinical
education required for initial entry or transfer into ACGME-accredited residency programs must
be verified by the program director using Milestones evaluations. Any one of the following three
evaluation tools may be used:
• ACGME Milestones evaluations
• ACGME-I Milestones evaluations
• CanMEDS Milestones evaluations
ADS screenshot: retrieving Milestones reports from a previous residency
program
Once a transfer resident is entered in ADS and starts in a new residency program, program
leadership can retrieve the Milestones report for that resident from the previous program by
following these steps:
1. Log into ADS.
2. Go to the Reports tab.
3. Select “Residency Milestones Retrieval” in the Reports section.
4. Select the academic year to view a list of current residents and, if available, the last
Milestone evaluation form completed by their most recent accredited core residency
program.
5. Select the “Summary Report” button for that particular resident.
NOTE: A report may be unavailable if the previous program has not updated that resident's
record in ADS or if the previous training and education could not be matched when entered on
your roster (based on name, date of birth, social security number, medical school, or some
combination of those elements). The resident may also have completed core residency training
and education in a program not accredited by the ACGME or completed training and education
prior to Milestones implementation. For residents that do not have a Milestone report on record,
contact the previous specialty program director to obtain the summative report or email
with questions. (
See accompanying screenshot which follows on the next
page.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
96

[The Review Committee may further specify prerequisite postgraduate clinical
education]
Since Review Committees may specify other requirements related to prerequisite postgraduate
clinical education, programs must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
Questions about specialty-specific Program Requirements should be directed to specialty
Review Committee staff.
Common Program Requirement III.A.3 describes exceptions to the general requirement in
Common Program Requirement III.A.2. It applies only to an individual who has graduated from
a residency in the same specialty. Residents should expect to enter at the PGY-1 level, but if
©2024 Accreditation Council for Graduate Medical Education (ACGME)
97

they are performing at a higher level that can be demonstrated through the Milestone
evaluation, they can be advanced to the PGY-2 level.
III.A.3. Resident eligibility exception
The Review Committee for ______ will allow the following exception to the
resident eligibility requirements:
(Core)
[NOTE: A Review Committee may permit the eligibility exception if the specialty
requires completion of a prerequisite residency program prior to admission. If
this language is not applicable, this section will not appear in the specialty-
specific requirements.]
Some specialties will allow exceptions to resident eligibility requirements. Review the
information in the document ACGME Review Committee Eligibility Decisions or refe
r to the
specialty-specific Program Requirements. Review Committees that allow exceptions require
completion of a prerequisite residency program prior to admission. Programs can also access
the Common Program Requirements FAQs for additional information on resident eligibility.
See the table below for information on eligibility for specialty certification by ABMS
member boards and AOA member boards during and following the transition period to a
single GME accreditation system based on training and program accreditation status.
Refer to the ABMS and AOA websites for most current information.
The A
OA provides a pathway for osteopathic physicians (whether they were educated in AOA-
approved or ACGME-accredited programs) to sit for AOA board examinations in the areas the
AOA certifies. Allopathic physicians who complete an ACGME-accredited program with
Osteopathic Recognition in a designated osteopathic position are also eligible for AOA board
certification. Allopathic physicians who complete an ACGME-accredited osteopathic
neuromusculoskeletal medicine program are eligible for AOA board certification in
neuromusculoskeletal medicine. For AOA programs that achieved ACGME accreditation during
the transition, all osteopathic residents in the program at the time it achieved ACGME
accreditation will receive AOA approval following completion of the program, which will satisfy
the AOA board eligibility requirements.
ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
Allergy and
Immunology
American Board of Allergy and
Immunology (ABAI)
Two full years in an ACGME-
accredited allergy and immunology
program AND must be eligible to
take the certifying examination for
either the American Board of
Internal Medicine or the American
Board of Pediatrics. In 2016, the
Allergy and Immunology -
Joint Examination
Completed an AOA-
approved or ACGME-
accredited program
©2024 Accreditation Council for Graduate Medical Education (ACGME)
98
ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
ACGME approved allergy and
immunology programs accredited
by the American Osteopathic
Association to be approved for dual
accreditation. Graduates of a dually
accredited program are now eligible
to apply for admission to the ABAI
Certification Examination in Allergy
and Immunology. Therefore,
candidates with one year of training
in an AOA-accredited program and
one year of training in an ACGME-
accredited program may be
considered for admission to the
allergy and immunology
examination. Candidates who
submit appropriate documentation
will be reviewed by the ABAI Ethics
and Professionalism Committee to
ensure their training meets the
requirements for admission to the
examination.
Anesthesiology
American Board of
Anesthesiology (ABA)
All three years of clinical anesthesia
(CA 1-3) training must occur in
programs that are accredited by the
ACGME for the entire period of
training. All physicians who
graduate from an AOA-approved
anesthesiology residency program
on or after the date the program
receives full ACGME accreditation
will receive ABA credit for the CA 1-
3 years of satisfactory training in
the newly accredited program.
American Osteopathic
Board of Anesthesiology
Completed an AOA-
approved or ACGME-
accredited program
Colon and Rectal
Surgery
American Board of Colon and
Rectal Surgery
Not applicable. There are no AOA-
approved programs.
N/A
Dermatology
American Board of Dermatology
Program must achieve ACGME
accreditation prior to completion.
American Osteopathic
Board of Dermatology
©2024 Accreditation Council for Graduate Medical Education (ACGME)
99

ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
Completed an AOA-
approved or ACGME-
accredited program
Emergency Medicine
American Board of Emergency
Medicine
Program must achieve ACGME
accreditation prior to completion.
American Osteopathic
Board of Emergency
Medicine
Completed an AOA-
approved or ACGME-
accredited program
Family Medicine
American Board of Family
Medicine (ABFM)
A time-limited exemption during the
transition period will be offered to
allow osteopathic family physicians
who have completed three years of
an AOA-approved family medicine
residency program to be eligible for
ABFM specialty certification.
American Osteopathic
Board of Family
Physicians
Completed an AOA-
approved or ACGME-
accredited program
Internal Medicine
American Board of Internal
Medicine (ABIM)
Program must achieve ACGME
accreditation prior to resident’s
completion of the program. In
addition, the program director must
be certified by ABIM, or other
ABMS member board if applicable,
by the completion of the transition
period (2016-2023) to a single GME
accreditation system in order to
attest to ABIM initial eligibility
criteria. Beginning in 2024, only
graduates of programs with
program directors certified by ABIM,
or other ABMS board if applicable,
will be eligible for certification by
ABIM.
American Osteopathic
Board of Internal Medicine
Completed an AOA-
approved or ACGME-
accredited program
Medical Genetics and
Genomics
American Board of Medical
Genetics and Genomics
There are no AOA-approved
residency programs in medical
genetics and genomics. A minimum
of one year of GME training in
either an ACGME-accredited
program or a program in the
ACGME pre-accreditation phase
N/A
©2024 Accreditation Council for Graduate Medical Education (ACGME)
100
ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
with 12 months of direct patient
care is required prior to beginning
the medical genetics and genomics
residency.
Neuromusculoskeletal
Medicine
N/A
American Osteopathic
Board of
Neuromusculoskeletal
Medicine
Completed an AOA-
approved or ACGME-
accredited program
Neurological Surgery
American Board of Neurological
Surgery (ABNS)
Neurological surgery training is 84
months in total. There are 54
months of “core" neurological
surgery training which must be
completed in an ACGME-accredited
program. For the 30 months of
research or elective time, there is
flexibility depending upon the
quality of the clinical or research
experience. It is not necessary for
this experience to be in an ACGME-
accredited program. However,
written approval from the ABNS is
required for any off-site elective
experiences. The ABNS works
collaboratively with the ACGME
when questions arise to ensure
high-quality training and education.
American Osteopathic
Board of Surgery:
Neurological Surgery
Completed an AOA-
approved or ACGME-
accredited program
Nuclear Medicine
American Board of Nuclear
Medicine
Not applicable. There are no AOA-
approved nuclear medicine
programs.
American Osteopathic
Board of Nuclear Medicine
Completed an AOA-
approved or ACGME-
accredited program
Obstetrics and
Gynecology
American Board of Obstetrics
and Gynecology
Program must have achieved
ACGME accreditation prior to
completion.
American Osteopathic
Board of Obstetrics and
Gynecology
Completed an AOA-
approved or ACGME-
accredited program
©2024 Accreditation Council for Graduate Medical Education (ACGME)
101

ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
Ophthalmology
American Board of
Ophthalmology
All training must be in an ACGME-
accredited program.
American Osteopathic
Board of Ophthalmology
and Otolaryngology
Completed an AOA-
approved or ACGME-
accredited program
Orthopaedic Surgery
American Board of Orthopaedic
Surgery
All training must be in an ACGME-
accredited program.
American Osteopathic
Board of Orthopedic
Surgery
Completed an AOA-
approved or ACGME-
accredited program
Otolaryngology –
Head and Neck
Surgery
American Board of
Otolaryngology – Head and Neck
Surgery (ABOHNS)
All training must be in an ACGME-
accredited program.
Based on the timing of AOA-
approved residencies transitioning
to ACGME accreditation, ABOHNS
started seeing some applicants
from the traditional AOA-approved
residencies in 2021. This transition
will be completed with all residents
in newly ACGME-accredited
residency programs by 2025.
American Osteopathic
Board of Ophthalmology
and Otolaryngology
Completed an AOA-
approved or ACGME-
accredited program
Pathology
American Board of Pathology
Not applicable. There are no AOA-
approved programs in pathology.
American Osteopathic
Board of Pathology
Completed an AOA-
approved or ACGME-
accredited program
Pediatrics
American Board of Pediatrics
All residency training must be
completed in an ACGME- or
RCPSC-accredited program.
American Osteopathic
Board of Pediatrics
Completed an AOA-
approved or ACGME-
accredited program
Physical Medicine and
Rehabilitation
American Board of Physical
Medicine and Rehabilitation
(ABPMR)
Through June 30, 2020, the
ABPMR will recognize AOA-
approved training as acceptable
toward PGY-1-level physical
American Osteopathic
Board of Physical
Medicine and
Rehabilitation
©2024 Accreditation Council for Graduate Medical Education (ACGME)
102

ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
medicine and rehabilitation
residency training. Due to the
impact of the transition to a single
GME accreditation system, the
ABPMR will recognize physicians
who completed at least 36 months
of AOA-approved physical medicine
and rehabilitation training as eligible
for certification in circumstances
where ACGME accreditation was
granted by the time of program
completion. Program completion
must have occurred July 1, 2015,
and forward to coincide with the
transition to a single GME
accreditation system.
Completed an AOA-
approved or ACGME-
accredited program
Plastic Surgery
American Board of Plastic
Surgery
All training must be in an ACGME-
accredited program.
American Osteopathic
Board of Surgery: Plastic
and Reconstructive
Surgery
Completed an AOA-
approved or ACGME-
accredited program
Preventive Medicine
American Board of Preventive
Medicine
PGY-1 year can take place in an
AOA-approved program. Years 2
and 3 must be in an ACGME-
accredited program.
American Osteopathic
Board of
Preventive Medicine
Completed an AOA-
approved or ACGME-
accredited program
Psychiatry and
Neurology
American Board of Psychiatry
and Neurology
Program must achieve ACGME
accreditation prior to completion.
American Osteopathic
Board of Neurology and
Psychiatry
Completed an AOA-
approved or ACGME-
accredited program
Radiology
American Board of Radiology
All residency training must be
completed in an ACGME- or
RCPSC-accredited program.
American Osteopathic
Board of Radiology
Completed an AOA-
approved or ACGME-
accredited program
Surgery
American Board of Surgery
The final three years of the basic
five-year surgery residency must be
in an ACGME-accredited program.
American Osteopathic
Board of Surgery
Completed an AOA-
approved or ACGME-
accredited program
©2024 Accreditation Council for Graduate Medical Education (ACGME)
103

ABMS Board Certification
Requirements
AOA Board Certification
Requirements
Specialty
ABMS Member Board and
Training and Program
Accreditation Status
AOA Member Board and
Training Eligibility Criteria
for Specialty Certification
Thoracic Surgery
American Board of Thoracic
Surgery
The last three years of a surgical
residency (PGY 3-5) must be
completed in an ACGME-accredited
program followed by completion of
an ACGME-accredited thoracic
surgical residency.
American Osteopathic
Board of Surgery:
Thoracic and
Cardiovascular Surgery
Completed an AOA-
approved or ACGME-
accredited program
Urology
American Board of Urology
All training must be in an ACGME-
or RCPSC-accredited program.
American Osteopathic
Board of Surgery:
Urological Surgery
Completed an AOA-
approved or ACGME-
accredited program
©2024 Accreditation Council for Graduate Medical Education (ACGME)
104

COMMON PROGRAM REQUIREMENTS
III. Resident Appointments
III.B. Resident Complement
The program director must not appoint more residents than approved by
the Review Committee.
(Core)
[The Review Committee may further specify minimum complement
numbers]
Background and Intent: Programs are required to request approval of all complement
changes, whether temporary or permanent, by the Review Committee through ADS.
Permanent increases require prior approval from the Review Committee and temporary
increases may also require approval. Specialty-specific instructions for requesting a
complement increase are found in the “Documents and Resources” page of the applicable
specialty section of the ACGME website.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
105

GUIDANCE
III.B. Resident complement
Review Committees approve resident complement for a program at the time of an application
and the program director must not appoint more residents than approved by the Review
Committee. Some Review Committees approve complement by total while others approve
complement by both total and program year.
Complement increases can be permanent or temporary.
Permanent complement change requests
A program may request a permanent complement increase to expand its size. Programs can
also request a decrease in permanent complement if they need to decrease the size of the
program below the approved complement. All permanent complement increase requests must
be submitted through the Accreditation Data System (ADS) and require approval by the Review
Committee. Review Committees assess all requests for permanent complement increases
thoroughly, considering the clinical, educational, and other resources available to the program.
Additional information or a site visit may be requested for a permanent complement change
request, depending on the details of the request. Review Committees review permanent
increase requests at their scheduled meetings and therefore programs should check posted
meeting agenda closing dates on the applicable specialty
page of the ACGME website and plan
accordingly before submitting a request.
Te
mporary complement change requests
A program may request a temporary complement increase for many reasons, including
remediation, resident well-being needs, medical, parental, or caregiver leave, and a resident
beginning the program off-cycle. Temporary complement increase requests of greater than 90
days must be submitted through ADS and require approval by the Review Committee, although
the submission and approval process differ by Review Committee and programs must consult
specialty-specific guidance referenced below in this document. All Review Committees allow
extensions of education and training of up to 90 days for residents in all specialties except one-
year programs without the need to submit a temporary complement increase request. This
change was implemented to reduce burden for the graduate medical education community and
better align with the Institutional Requirements related to Leaves of Absence (IV.H.1.a)).
Program directors are strongly encouraged to contact their graduate medical education office
and the applicable specialty certifying board for guidance on extending a resident’s education
and training, as the impact and requirements vary from one certifying board to another.
To initiate a request to change the program’s approved complement:
1. The program director must:
b. Log into ADS.
c. Under the “Program” tab, select “Complement Change” from the right panel
under “Requests.”
d. Select either “Temporary” or “Permanent” request.
e. Complete all required information and submit.
2. Once submitted, the request will be forwarded to the designated institutional official
(DIO) for approval.
3. Once approved by the DIO, the request will be forwarded to the specialty Review
Committee.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
106

4. ACGME staff will notify the program of the Review Committee’s decision. The
notification time may vary based on the type of request and whether it needs to be
reviewed during a Review Committee meeting.
ADS screenshot: complement change requests
[The Review Committee may further specify minimum complement numbers]
For more information on resident complement and whether your specialty Review Committee
specifies minimum complement numbers, programs must review the specialty-specific Program
Requirements.
1. Go to https://www.acgme.org/specialties/
.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
Each Review Committee also provides additional information on the specialty-specific process
to request a complement change in the Documents and Resources section of their specialty-
specific web page or in the specialty FAQs. Questions about specialty-specific Program
Requirements related to resident complement should be directed to specialty Review
Committee staff.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
107
COMMON PROGRAM REQUIREMENTS
III. Resident Appointments
III.C. Resident Transfers
The program must obtain verification of previous educational experiences
and a summative competency-based performance evaluation prior to
acceptance of a transferring resident, and Milestones evaluations upon
matriculation.
(Core)
[The Review Committee may further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
108
GUIDANCE
III.C. Resident Transfers
Residents are considered transfer residents under several conditions, including:
• when moving from one program to another within the same or to a different Sponsoring
Institution;
• when moving from one program to another within the same or different specialty; and
• when entering as a PGY-2 in a program requiring a preliminary year, regardless of
whether the resident was accepted to the preliminary year and the specialty program as
part of the match (i.e., accepted to both the preliminary program and the specialty
program upon graduation from medical school).
The term does not apply to a resident who has successfully completed a residency and then is
accepted into a subsequent residency or fellowship program.
Before accepting a transferring resident, the “receiving” program director must obtain written or
electronic verification of prior educational experiences and performance by the program from
which the resident is seeking to transfer.
Documentation includes evaluations, rotations completed, procedural/operative
experience/Case Logs if applicable, and a summative competency-based performance
evaluation.
While a Milestones evaluation cannot be used in the decision to accept a transferring resident, a
Milestones evaluation must be obtained upon matriculation.
The ACGME monitors compliance with this requirement in various ways, including:
• resident-level questions answered by program leadership as part of an application or
during the Accreditation Data System (ADS) Annual Update when entering/updating
their resident roster; and
• questions asked and documentation reviewed by Accreditation Field Staff during site
visits of the program at various stages of accreditation.
ADS screenshot: identifying transfer residents
During the ADS Annual Update, programs update their resident roster and information on each
resident. On the resident Profile page, under the Resident Details section, programs are asked
to answer several questions regarding a transferring resident and confirm that documentation of
prior training and education has been obtained for a transfer resident(s). (See accompanying
screenshot which follows on the next page.)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
109

ADS screenshot: retrieving Milestones reports from previous residency program
Once a transfer resident starts in a new residency program, program leadership can retrieve the
Milestones report for that resident from the previous program by following these steps:
1. Log into ADS.
2. Go to the Reports tab.
3. Select “Residency Milestones Retrieval” in the Reports section.
4. Select the academic year to view a list of current residents and, if available, the last
Milestone evaluation form completed by their most recent accredited core residency
program.
5. Select the “Summary Report” button for that particular resident.
NOTE: A report may be unavailable if the previous program has not updated that resident's
record in ADS or if the previous training and education could not be matched when entered on
that resident’s roster (based on name, date of birth, social security number, medical school, or
some combination of those elements). The resident may also have completed core residency
training and education in a program not accredited by the ACGME or completed training and
education prior to Milestones implementation. For residents that do not have a Milestone report
on record, contact the previous specialty program director to obtain the summative report or
email ADS@acgme.org
with questions.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
110

[The Review Committee may further specify]
Since Review Committees may specify other requirements related to resident transfers,
programs must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the currently in effect specialty Program Requirements currently in effect.
Quest
ions about specialty-specific Program Requirements related to resident transfers should
be directed to specialty Review Committee staff.
Programs can also access the Common Program Requirements FAQs for additional information
on resident transfers and Milestones retrieval.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
111

COMMON PROGRAM REQUIREMENTS
IV. Educational Program
The ACG
ME accreditation system is designed to encourage excellence and
innovation in graduate medical education regardless of the organizational
affiliation, size, or location of the program.
The educational
program must support the development of knowledgeable, skillful
physicians who provide compassionate care.
It is
recognized that programs may place different emphasis on research,
leadership, public health, etc. It is expected that the program aims will reflect the
nuanced program-specific goals for it and its graduates; for example, it is
expected that a program aiming to prepare physician-scientists will have a
different curriculum from one focusing on community health.
IV.A
.
Educational Components
The cur
riculum must contain the following educational components:
IV.A
.1.
a set of program aims consistent with the Sponsoring Institution’s
mi
ssion, the needs of the community it serves, and the desired
distinctive capabilities of its graduates, which must be made
available to program applicants, residents, and faculty members;
(Core)
IV.A
.2. competency-based goal
s and objectives for each educational
experience designed to promote progress on a trajectory to
independent practice. These must be distributed, reviewed, and
available to residents and faculty members;
(Core)
Background and Intent: The trajectory to autonomous practice is documented by
Milestones evaluations. Milestones are considered formative and should be used to
identify learning needs. Milestones data may lead to focused or general curricular
revision in any given program or to individualized learning plans for any specific
resident.
IV.A
.3. delineation of resident responsibilities for patient care, progressive
responsibility for patient management, and graded supervision;
(Core)
Background and Intent: These responsibilities may generally be described by PGY
level and specifically by Milestones progress as determined by the Clinical
Competency Committee. This approach encourages the transition to competency-
based education. An advanced learner may be granted more responsibility
independent of PGY level and a learner needing more time to accomplish a certain task
may do so in a focused rather than global manner.
IV.A
.4. a broad range of structured didactic activities; and,
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
112

IV.A.4.a) Residents must be provided with protected time to participate
in core didactic activities.
(Core)
Background and Intent: It is intended that residents will participate in structured
didactic activities. It is recognized that there may be circumstances in which this is not
possible. Programs should define core didactic activities for which time is protected
and the circumstances in which residents may be excused from these didactic
activities. Didactic activities may include, but are not limited to, lectures, conferences,
courses, labs, asynchronous learning, simulations, drills, case discussions, grand
rounds, didactic teaching, and education in critical appraisal of medical evidence.
IV.A
.5. formal educational activities that promote patient safety-rel
ated
goals, tools, and techniques.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
113
GUIDANCE
The Common Program Requirements do not list detailed curricular elements for each specialty.
The overarching intent of the Common Program Requirements related to the educational
program is to ensure that programs provide a framework for:
• a comprehensive education for residents pertinent to the specific mission and aims of
the Sponsoring Institution, the program, and the community served; and
• the development of knowledgeable, skilled, and compassionate physicians capable of
autonomous practice.
IV.A.1. Program aims
Programs must develop aims to add context to the program’s expectations and focus on
aspects such as:
• tyles of residents being educated by the program
• residents’ future roles in the community
Having aims allows the program to construct curricular elements that address career options
(e.g., clinical practice, research, primary care, or health policy and advocacy). For example, a
program in a rural community might focus its resident education on issues relevant to that
community, while a program in an institution with a goal to produce physician-scientists might
want to provide more education in research. The Program Evaluation Committee (PEC) should
play a central role in the development of program aims and should ensure that the program is
working toward these aims.
Program aims should be vetted with program and institutional leaders, and in some institutions,
setting aims will be an institution-level initiative. In setting aims, programs should generally take
a longer-term strategic view. However, aims may change over time. Factors such as a shift in
program focus initiated by institutional or department leadership, changes in local or national
demand for a resident workforce with certain capabilities, or new opportunities to train and
educate residents in a different setting may prompt revision of program aims.
It bears re-emphasizing that while Common Program Requirement IV.A.1. requires that the
program develop a set of program aims consistent with its mission and the community it serves,
the Review Committees will not evaluate the specifics of the program aims for accreditation
purposes. What Review Committees will evaluate is that a program has defined its program
aims and that it has a process to share them with applicants to the program, residents, and
faculty members.
New programs submitting an application for accreditation and programs with a status of Initial
Accreditation or Initial Accreditation with Warning must provide or update their program aims in
the Accreditation Data System (ADS) as part of an application or the ADS Annual Update.
Accreditation Field Staff also verify that a program has identified program aims and that it has a
process in place to share those with program applicants, residents, and faculty members.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
114

ADS screenshot: program aims
IV.A.2. Goals and objectives
The program must design competency-based, level-specific goals and objectives for each
educational experience/rotation to promote progress on a trajectory to autonomous practice in
its subspecialty. These goals and objectives must be distributed, reviewed, and available to
residents and faculty members.
Defining goals and objectives
• A goal is an overarching principle that guides decision making.
• Objectives are specific, measurable steps that can be taken to meet a goal.
Developing goals and objectives
While the ACGME and the Review Committees do not endorse any single method for
developing goals and objectives, a number of resources are available to guide those entrusted
with constructing residency curricula. For example, among the most widely known approaches
is the “Theory of Bloom’s Taxonomy of Measurable Verbs.” (Bloom, 1956) Bloom based his
taxonomy on the premise that observable action levels can help explicitly define what a student
must do to demonstrate learning. He organized these action levels by using measurable verbs
to describe observable knowledge, skills, attitudes, behaviors, and abilities. In developing
residency curricula, these categories can be used to identify residents’ learning needs for each
rotation. Many iterations of the taxonomy are easily accessible on a variety of educational
websites.
Another
tool for guiding the development of goals and objectives is the SMART mnemonic
developed by Doran (1981). He simply states that goals and objectives should be:
• S − Specific
• M − Measurable
• A − Attainable
• R − Relevant
• T −Time-bound
Common mistakes in creating goals and objectives
• Using vague verbs and phrases that cannot be measured
a. words to avoid
• believe
• comprehend
• know
• perceive
• recognize
• understand
©2024 Accreditation Council for Graduate Medical Education (ACGME)
115

b. phrases to avoid
• appreciation for
• capable of
• familiar with
• knowledge of
2. Creating goals and objectives that are not level-specific and/or competency-based
Goals
and objectives must be competency-based and level-specific. For example, a PGY-1
resident must demonstrate the ability to independently perform a complete history and physical
examination as part of the Patient Care Competency. As part of the same competency, a PGY-3
resident in a three-year program must demonstrate the ability to guide and supervise a PGY-1
resident in obtaining a complete history and physical examination and take an active role in the
formulation of diagnostic and treatment plans.
Goals
and objectives must be distributed, reviewed, and available to residents and faculty
members to ensure an understanding of learning expectations. New programs submitting an
application for accreditation and programs with a status of Initial Accreditation or Initial
Accreditation with Warning must answer the question shown in the screenshot below in ADS as
part of the application or during the ADS Annual Update process. Finally, Accreditation Field
Staff also verify during a site visit that the program has a process in place for informing
residents about goals and objectives for all educational assignments.
ADS screenshot: goals and objectives
IV.A.3. Resident responsibilities and graded supervision
Common Program Requirement IV.A.3. is closely related to the Common Program
Requirements in section VI.A.2. focused on supervision and accountability. Programs are
encouraged to review those requirements and associated guidance as well. The responsibilities
and supervision of residents must be clearly delineated. The ACGME assesses compliance with
this requirement in multiple ways, including:
• review of the supervision policy and answers to the question shown below for programs
submitting an application or during the Initial Accreditation stage; and
• verification of information Accreditation Field Staff related to this requirement during
accreditation site visits.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
116
ADS screenshot: resident progressive authority and responsibilities in patient
care
Milestones evaluations can be helpful to Clinical Competency Committees which should review
them, be educated in Milestones assessment, and use this knowledge to delineate resident
responsibilities and determine levels of graded supervision in the program.
IV.A.4. Structured didactic activities
There are many forms of didactic activities, including lectures, workshops, courses, simulation
with feedback, case discussions, grand rounds, board review, and journal club. Faculty
members’ presence, participation, and leadership is key. In addition, residents must have the
opportunity to participate in didactic activities. While residents may occasionally miss didactic
activities because of priorities related to patient care, it is important that the program provide
protected time to allow their attendance. Residents on rotations at a distant site should be given
the opportunity to participate in didactic activities online, via recorded conferences, and through
other means as applicable.
Program l
eaders should conduct periodic reviews of the program’s curriculum to determine if
adjustments need to be made (e.g., new treatment protocols or concepts may need to be
incorporated). If Milestones evaluation and in-training examination results consistently indicate a
significant portion of residents are not performing well in a particular area, program leaders
should address that knowledge deficiency in the didactic curriculum.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
117

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
Background and Intent: The Competencies provide a conceptual framework describing
the required domains for a trusted physician to enter autonomous practice. These
Competencies are core to the practice of all physicians, although the specifics are
further defined by each specialty. The developmental trajectories in each of the
Competencies are articulated through the Milestones for each specialty.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
118

GUIDANCE
The ACGME and the American Board of Medical Specialties developed the six Core
Competencies necessary for a practicing physician:
• Patient Care and Procedural Skills
• Medical Knowledge
• Practice-Based Learning and Improvement
• Interpersonal and Communication Skills
• Professionalism
• Systems-Based Practice
The Core C
ompetencies provide a systematic framework to think about both curriculum and
assessment in medical education. Each specialty was tasked with crafting specific
milestones within each Competency.
The Mil
estones in graduate medical education (GME) provide narrative descriptions of the
Competencies and subcompetencies along a developmental continuum with varying degrees of
granularity. Simply stated, the Milestones describe performance levels residents are expected to
demonstrate for skills, knowledge, and behaviors in the six Core Competency domains. The
Milestones lay out a framework of observable behaviors and other attributes associated with a
resident’s development as a physician.
It i
s essential to recognize that milestones, based on the concept of stages of professional
development, are designed to be criterion-based and agnostic to the actual PGY level of the
resident. Programs should judge each resident based on the actual level of performance as
described in the Milestones, not in relation to peers or others.
The Mil
estones describe the learning trajectory within a subcompetency that takes the resident
from a beginner in the specialty to a highly proficient resident or resident expert. The Milestones
are different from many other assessments because there is an opportunity for the learner to
demonstrate the attainment of aspirational levels of the subcompetency. The Level 4 milestones
are designed as the graduation target but do not represent a graduation requirement. Making
decisions about readiness for graduation is the purview of the residency program director. (See
the Milestones FAQs
for further discussion of this issue: “Can a resident/fellow graduate if he or
she does not reach all of the milestones?”) The Milestones allow for a shared understanding of
the expectations for the learner.
It i
s also important to recognize what the Milestones are not. First and foremost, they do not
describe or represent a complete description of a clinical discipline. They represent the core of a
discipline, but programs will need to use good judgment to fill in the gaps in curriculum and
assessment. It is essential that the Milestones do not serve as curricula in and of themselves,
but rather guide a thoughtful analysis of curricula to identify strengths and gaps. Second, they
are not tools designed to affect program accreditation, and therefore Review Committees do not
see or review any individual resident Milestones ratings or aggregated Milestones data for a
particular program. The Milestones are intended for formative purposes to help learners, faculty
members, and programs.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
119

General description of Milestone levels related to stage of education
Example of the basic Anatomy of a milestone
Several key aspects about the use of the Milestones deserve special attention. First, the
Milestones reported to the ACGME were not designed to be used as evaluation forms for
specific rotations or experiences. The Milestones are designed as a formative judgment of
progress at least twice a year. The language from the Milestones may be helpful as part of a
mapping exercise to determine which subcompetencies are best covered in specific rotations
and curricular experiences. The Milestones can also be used for guided self-assessment and
reflection by the resident in preparation for feedback sessions and in creating individual learning
plans. Residents should use the Milestones for self-assessment with input and feedback from a
faculty advisor, mentor, or program director. Residents should not judge themselves on the
Milestones in isolation. Milestones feedback is most effective when performed in dialogue
between a learner and a faculty advisor. The Milestones can be useful in faculty development
by helping faculty members recognize performance expectations of learners, more explicitly
assess the trajectory of skill progression in their specialty, and discern how to ideally assess a
©2024 Accreditation Council for Graduate Medical Education (ACGME)
120

learner’s perf
ormance. Finally, it is imperative that programs remember that the Milestones are
not inclusive of the broader curriculum and that limiting assessments to the Milestones could
leave many topics without proper and essential assessment and evaluation.
The Supplemental Guides are a tool to aid in the development of a shared mental model of the
Milestones for each specialty. The Milestones Supplemental Guide for each specialty includes
the overall intent of each subcompetency, examples for each individual milestone, ideas for
assessment methods, and other resources. An editable version of each Supplemental Guide is
available so that each program can identify what it expects to see at each level. It can also be
used to aid in mapping to curricula, rotations, and assessments. Many of the Supplemental
Guides include a map from Milestones 1.0 to 2.0 to show topics that were carried over and
those that were deleted or added. It is recommended that the Supplemental Guide be shared
with all learners and faculty. Milestones Supplemental Guides can be found on the Milestones
section of each specialty
section of the ACGME website.
Other Milestones resources
The ACGME provides many resources for residents, faculty members, and
program administration and leadership, and new resources are developed regularly.
The Milestones section of the ACGME website provides access to available resources and
tools at https://www.acgme.org/milestones/resources/.
The ACGME also offers courses designed to help faculty members and leaders achieve the
goals of competency-based assessment in graduate medical education. Visit the Developing
Faculty Competencies in Assessment course page for information on dates, fees, and
registration availability.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
121

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
Background and Intent: The Competencies provide a conceptual framework describing
the required domains for a trusted physician to enter autonomous practice. These
Competencies are core to the practice of all physicians, although the specifics are
further defined by each specialty. The developmental trajectories in each of the
Competencies are articulated through the Milestones for each specialty.
IV.B.1. T
he program must integrate the following ACGME Competencies
into the curriculum:
(Core)
IV.B.1.a
) Professionalism
Residents
must demonstrate a commitment to
professionalism and an adherence to ethical principles.
(Core)
IV.B.1.a
).(1) Residents must demonstrate competence in:
IV.B.1.a
).(1).(a) compassion, integrity, and respect for others;
(Core)
IV.B.1.a
).(1).(b) responsiveness to patient needs that
supersedes self-interest;
(Core)
IV.B.1.a
).(1).(c) cultural humility;
(Core)
IV.B.1.a
).(1).(d) respect for patient privacy and autonomy;
(Core)
IV.B.1.a
).(1).(e) accountability to patients, society, and the
profession;
(Core)
IV.B.1.a
).(1).(f) respect and responsiveness to diverse patient
populations, including but not limited to
diversity in gender, age, culture, race, religion,
disabilities, national origin, socioeconomic
status, and sexual orientation;
(Core)
IV.B.1.a
).(1).(g) ability to recognize and develop a plan for one’s
own personal and professional well-being; and,
(Core)
IV.B.1.a
).(1).(h) appropriately disclosing and addressing
confli
ct or duality of interest.
(Core)
Background and Intent: This includes the recognition that under certain
circumstances, the interests of the patient may be best served by transitioning care to
another practitioner. Examples include fatigue, conflict or duality of interest, not
connecting well with a patient, or when another physician would be better for the
situation based on skill set or knowledge base.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
122

GUIDANCE
Professionalism is at the core of being a physician, yet, teaching it can be difficult, and
evaluation of professionalism presents significant challenges. There are many factors that
influence the erosion of professionalism, including state control, corporate demands, and
overemphasis on income and power. Some argue that the loss of ethics and morals underlies
this erosion, and therefore propose that medical professionalism cannot be taught separately
from ethical principles, morality, and emotional intelligence.
ACGME President and Chief Executive Officer Thomas J. Nasca, MD, MACP uses the following
chart to summarize the traditions contributing to the American concept of professionalism.
Dr. Na
sca (2015) states: “The philosophical roots of professionalism include the Hippocratic
tradition of medicine as a moral enterprise; the transition of medicine from guild to profession
with a commitment to competence, altruism, and public trust; and the responsibility of the
profession to prepare the next generation of physicians to serve the public.” Often neglected in
this equation is physician well-being. A physician who is unwell may not be able to provide good
care to patients.
Element
s of professionalism must be addressed in the program curriculum. Programs have
reported more success with simulation, workshops, and case discussions. Some programs have
incorporated education on professionalism into morbidity and mortality conferences and other
case review conferences. More importantly, repeated sessions throughout the educational
program provide reminders of the elements of professionalism and keep residents on track to
Nasca 2015
©2024 Accreditation Council for Graduate Medical Education (ACGME)
123
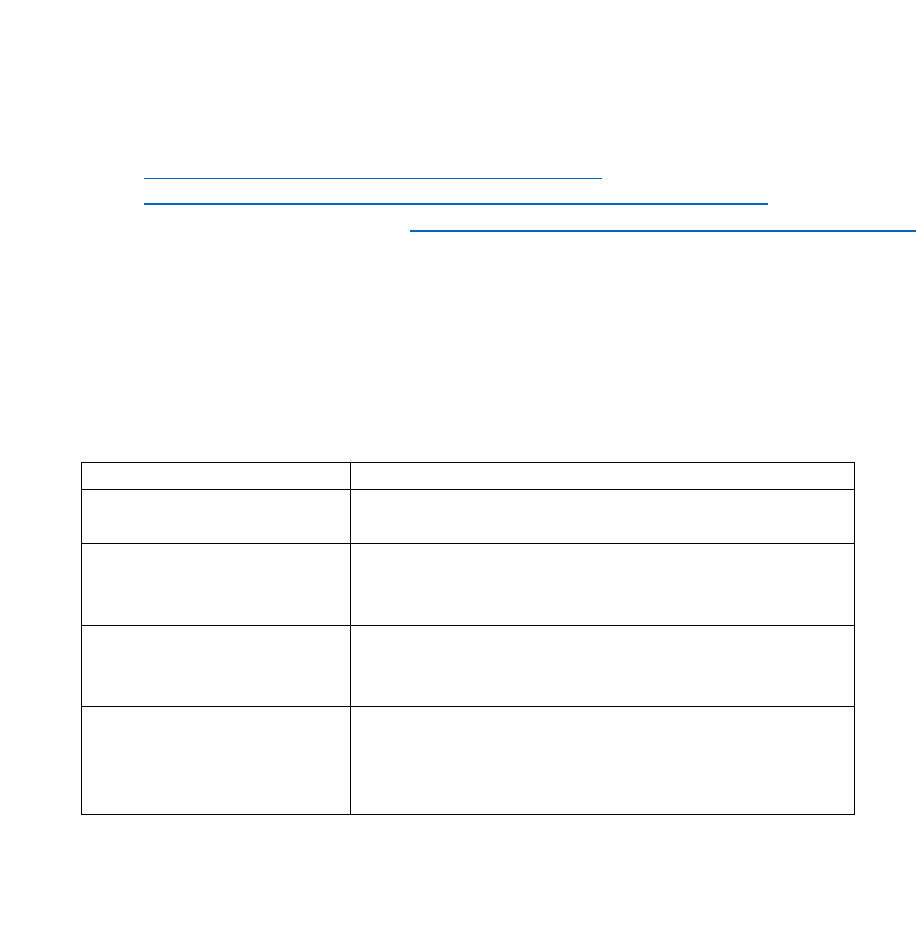
develop a lifelong commitment to this critical aspect of being a physician. Since role modeling of
professionalism by faculty members is key to the professional behavior of residents, it is
important to incorporate professionalism into faculty development sessions. While good role
models and mentors are essential for the education of residents and fellows, there is no way to
guarantee their presence. In addition, role modeling as a method of teaching professionalism
has been criticized as imprecise and lacking structure.
References/Resources
• Nasca, Thomas J. 2015. “Professionalism and its Implications for Governance and
Accountability of Graduate Medical Education in the United States.” JAMA 313(18):
1801-1802. doi:10.1001/jama.2015.3738.
• The American Medical Association (AMA) and the American Osteopathic Association
(AO
A) have defined rules and guidelines for physician professional responsibility and
conduct; those resources are provided below:
o AMA Declaration of Professional Responsibility
o AOA Rules and Guidelines on Physicians’ Professional Conduct
• The May 12, 2015 issue of JAMA (https://jamanetwork.com/journals/jama/issue/313/18)
is a great resource for programs and takes a deep dive into professionalism, including
Viewpoints from scholars and academic leaders about the responsibility and
accountability of medicine to self-govern, self-regulate, and ensure the highest degree of
professionalism.
Related Requirements: II.A.4.a) and II.A.4.a).(1): The program director must be a
role model of professionalism.
Examples of linking professionalism values to specific behaviors:
Values
Behaviors
Responsibility
• Follows through on tasks
• Arrives on time
Maturity
• Accepts blame for failure
• Does not make inappropriate demands
• Is not abusive and critical in times of stress
Communication Skills
• Listens well
• Is not hostile, derogatory, sarcastic
• Is not loud or disruptive
Respect
• Maintains patient confidentiality
• Is patient
• Is sensitive to physical/emotional needs
• Is not biased/discriminatory
Reference
Kirk, Lynne M. 2007. “Professionalism in Medicine: Definitions and Considerations for
Teaching.” Proceedings (Baylor University. Medical Center) 20(1):13-16.
doi:10.1080/08998280.2007.11928225
©2024 Accreditation Council for Graduate Medical Education (ACGME)
124

To review specialty-specific Requirements for Professionalism:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
In addit
ion, the Milestones are used to assess the progression of a resident in specific
competencies and subcompetencies. To access a specialty’s Milestones:
1. Go to https://www.acgme.org/specialties
/.
2. Select the applicable specialty.
3. Select “Milestones” at the top of the specialty section.
4. Select from the list of applicable Milestones.
Below
is an example of an Internal Medicine Milestones evaluation of Professionalism:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
125

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
IV.B.1. The program must integrate the following ACGME Competencies
into the curriculum:
(Core)
IV.B.1.b) Patient Care and Procedural Skills
Background and Intent: Quality patient care is safe, effective, timely, efficient, patient-
centered, equitable, and designed to improve population health, while reducing per
capita costs. In addition, there should be a focus on improving the clinician’s well-
being as a means to improve patient care and reduce burnout among residents,
fellows, and practicing physicians.
IV.B.1.b).(1)
Residents must be able to provide patient care that is
patient- and family-centered is compassionate,
equitable, appropriate, and effective for the treatment
of health problems and the promotion of health.
(Core)
[The Review Committee must further specify]
IV.B.1.b).(2) Residents must be able to perform all medical,
diagnostic, and surgical procedures considered
essential for the area of practice.
(Core)
[The Review Committee may further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
126

GUIDANCE
To review the specialty-specific Program Requirements for Patient Care and Procedural Skills:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
In addit
ion, Milestones are used to assess the progression of a resident in specific
competencies and subcompetencies. To access a specialty’s Milestones:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select the “Milestones” at the top of the specialty section.
4. Select from the list of applicable Milestones.
Below
is an example of an Internal Medicine Milestones evaluation of Patient Care and
Procedural Skills:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
127

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
IV.B.1
. The program must integrate the following ACGME Competencies
into the curriculum:
(Core)
IV.B.1
.c) Medical Knowledge
Resident
s must demonstrate knowledge of established and
evolving biomedical, clinical, epidemiological and social-
behavioral sciences, including scientific inquiry, as well as
the application of this knowledge to patient care.
(Core)
[The Review Committee must further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
128

GUIDANCE
To review the specialty-specific Program Requirements for Medical Knowledge:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” tab at the top of the
specialty section.
4. Select the specialty Program Requirements currently in effect.
In addit
ion, Milestones are used to assess the progression of a resident in specific
competencies and subcompetencies. To access a subspecialty’s Milestones:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Milestones” at the top of the specialty section.
4. Select from the list of applicable Milestones.
Below is an example of a Surgery Milestones evaluation of Medical Knowledge:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
129

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
IV.B.1
. The program must integrate the following ACGME Competencies
into the curriculum:
(Core)
IV.B.1
.d) Practice-based Learning and Improvement
Resident
s must demonstrate the ability to investigate and
evaluate their care of patients, to appraise and assimilate
scientific evidence, and to continuously improve patient care
based on constant self-evaluation and lifelong learning.
(Core)
IV.B.1
.d).(1) Residents must demonstrate competence in:
IV.B.1.d).(1).(a) identifying strengths, deficiencies, and limits in
one’s knowledge and expertise;
(Core)
IV.B.1.d).(1).(b) setting learning and improvement goals;
(Core)
IV.B.1
.d).(1).(c) identifying and performing appropriate learning
activities;
(Core)
IV.B.1
.d).(1).(d)
systematically analyzing practice using quality
impr
ovement methods, including activities
aimed at reducing health care disparities, and
implementing changes with the goal of practice
improvement;
(Core)
IV.B.1
.d).(1).(e) incorporating feedback and formative
evaluation into daily practice; and,
(Core)
IV.B.1
.d).(1).(f) locating, appraising, and assimilating evidence
from scientific studies related to their patients’
health problems.
(Core)
[The
Review Committee may further specify by adding to the
list of sub-competencies]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
130

GUIDANCE
Practice-based Learning and Improvement is best developed in an environment that provides
residents with enough information to investigate and evaluate the care of their patients. The
environment needs to support open and honest attempts to improve, and not punish errors or
mistakes as personal weakness.
To identi
fy strengths, deficiencies, and limitations, residents should learn to self-reflect to
answer the question: How can I improve care for my patients? This may include single patients,
such as at a case conference during which residents present individual patients they have cared
for and reflect on how they may improve on that care for a similar patient in the future. A more
systematic approach provides residents with information about the outcomes of their care for a
larger sample of their patients. This information may demonstrate a resident’s compliance with a
specific protocol or clinical guideline for a defined group of patients. Examples include the
number of patients who receive key elements of care in a sepsis bundle or the complication rate
for a certain procedure. It is not required that each resident have an individual project. Some
outcome measures will require institutional assistance to link the activity to a broader
departmental goal.
Learning and i
mprovement goals can be formulated after a resident determines what to improve
and may follow a deliberate process such as a “Plan-Do-Study-Act” cycle under the guidance of
a faculty member to systematically analyze the resident’s practice. This may be performed in
conjunction with the ongoing quality improvement efforts of the Sponsoring Institution.
Residents constantly receive feedback and suggestions. They may wish to target a certain
behavior for improvement, or try out suggestions for improvement, and consider how to analyze
and incorporate these improvements into practice.
Locati
ng and assimilating evidence may occur while a resident is preparing for upcoming case
presentations or during the actual care of a patient using a Cochrane Review or a PubMed
search or other clinical references. A resident may need to learn how an individual patient’s
circumstances fit into the larger knowledge base, and how to use published literature to fit the
scenario. This may incorporate activities such as literature review for case conferences or
journal club where a critical review of the literature is demonstrated and learned.
To revi
ew the specialty-specific Program Requirements for Practice-based Learning and
Improvement:
• Go to https://www.acgme.org/specialties/
.
• Select the applicable specialty.
• Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
• Select the subspecialty Program Requirements currently in effect.
In addit
ion, Milestones are used to assess the progression of a resident in specific
competencies and subcompetencies. To access a subspecialty’s Milestones:
1. Go to https://www.acgme.org/specialties
/.
2. Select the applicable specialty.
3. Select “Milestones” at the top of the specialty section.
4. Select from the list of applicable Milestones.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
131

Below is an example of a Pediatrics Milestones evaluation of Practice-Based Learning and
Improvement:
References
1. Bernabeo, Elizabeth, Sarah Hood, William Iobst, Eric Holmboe, and Kelly Caverzagie.
2013. “Optimizing the Implementation of Practice Improvement Modules in Training:
Lessons from Educators.” Journal of Graduate Medical Education 5(1): 74–80.
https://doi.org/10.4300/jgme-d-11-00281.1.
2. “Practice-Based Learning and Improvement: ACGME Core Competencies.” 2016. NEJM
Knowledge+. November 18. https://knowledgeplus.nejm.org/blog/practice-based-
learning-and-improvement/.
A description of why practice-based learning is important and how it fits into lifelong
learning.
3. “Practice-Based Learning - ACGME Competencies.” n.d. University of Maryland Medical
Center.
https://www.umms.org/ummc/pros/gme/acgme-com
petencies/practice-based-
learning.
Resources
An example of the resources compiled at one institution to address key components of Practice-
Based Learning and Improvement:
• life-long learning and practice improvement (self-reflection)
• appraisal and assimilation of scientific literature (EBM)
• ability to implement quality improvement
• actively participate in the education of others
©2024 Accreditation Council for Graduate Medical Education (ACGME)
132

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
IV.B.1
. The program must integrate the following ACGME Competencies
into the curriculum:
(Core)
IV.B.1
.e) Interpersonal and Communication Skills
Resident
s must demonstrate interpersonal and
communication skills that result in the effective exchange of
information and collaboration with patients, their families,
and health professionals.
(Core)
IV.B.1
.e).(1) Residents must demonstrate competence in:
IV.B.1.e).(1).(a)
communicating effectively with patients and
pati
ents’ families, as appropriate, across a
broad range of socioeconomic circumstances,
cultural backgrounds, and language
capabilities, learning to engage interpretive
services as required to provide appropriate care
to each patient;
(Core)
IV.B.1
.e).(1).(b) communicating effectively with physicians,
other health professionals, and health-related
agencies;
(Core)
IV.B.1
.e).(1).(c) working effectively as a member or leader of a
health care team or other professional group;
(Core)
IV.B.1
.e).(1).(d) educating patients, patients’ fami
lies, students,
other residents, and other health professionals;
(Core)
IV.B.1
.e).(1).(e)
acting in a consultative role to other physicians
and health pr
ofessionals;
(Core)
IV.B.1
.e).(1).(f) maintaining comprehensive, timely, and legible
health
care records, if applicable.
(Core)
IV.B.1
.e).(2) Residents must learn to communicate with patients
and patient
s’ families to partner with them to assess
their care goals, including, when appropriate, end-of-
life goals.
(Core)
[The
Review Committee may further specify by adding to the
list of sub-competencies]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
133
GUIDANCE
The ability to communicate is one of the basic tenets of the physician-patient relationship, and
an important component of professionalism. Yet education related to communication skills is
frequently neglected. Apart from medical knowledge and the ability to provide good patient care,
physicians need communication skills in many aspects of their practice. Examples include:
• The physi
cian and the patient:
o history taking and physical examination — ability to elicit pertinent information, and
the capacity to listen attentively to what a patient/family member has to say
o explaining medical information, such as diagnosis, complications, and treatment
(surgical and medical)
o shared decision making regarding diagnostic and therapeutic interventions
o Instructions related to prescriptions — patients often take medications incorrectly
because of inadequate instructions
o delivering bad news
o discharge instructions
o sensitivity to different cultural and socioeconomic backgrounds
o respect for privacy and confidentiality
o obtaining informed consent for procedures or study participation
o end-of-life decisions
• Physician to physician or other health care providers:
o consultations
o sign-outs
o patient transfers
o leading and participating in team-based medical care
• Written and other communication
o medical records
o procedure notes
o consults
o transfers
o lectures and presentations
It i
s well known that good communication skills improve patient satisfaction and treatment
adherence and reduce medication errors. Modalities of communication skills include:
• skills-based − word usage, approach to patients and families;
• content-based − patient interviewing, obtaining informed consent;
• advanced encounters − delivering bad news, disclosing errors, shared decision making;
and
• interaction-focused − physician-patient and/or physician-family, interprofessional.
Techniques used to teach interpersonal and communication skills include:
• role play;
• standardized patients;
• simulation; and
• real-life experiences, such as during morbidity and mortality conference.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
134

References
1. Bragard, Isabelle, Isabelle Merckaert, Yves Libert, Nicole Delvaux, Anne-Marie Etienne,
Serge Marchal, Christine Reynaert, et. al. 2012. “Communication Skills Training for
Residents: Which Variables Predict Learning of Skills?” Open J Med Psychol 1:68-75.
2. Peterson, Eleanor B., Kimberly A. Boland, Kristina A. Bryant, Tara F. McKinley, Melissa
B. Porter, Katherine E. Potter, and Aaron W. Calhoun. 2016. “Development of a
Comprehensive Communication Skills Curriculum for Pediatrics Residents.” Journal of
Graduate Medical Education 8(5): 739–46. https://doi.org/10.4300/jgme-d-15-00485.1
.
3. Sullivan, Amy M., Laura K. Rock, Nina M. Gadmer, Diana E. Norwich, and Richard M.
Schwartzstein. 2016. “The Impact of Resident Training on Communication with Families
in the ICU: Resident and Family Outcomes.” Annals of the American Thoracic Society.
https://doi.org/10.1513/annalsats.201508-495oc
.
4. Wild, Dorothea, Haq Nawaz, Saif Ullah, Christina Via, William Vance, and Paul Petraro.
2018. “Teaching Residents to Put Patients First: Creation and Evaluation of a
Comprehensive Curriculum in Patient-Centered Communication.” BMC Medical
Education 18(1). https://doi.org/10.1186/s12909-018-1371-3
.
Whil
e many of the efforts in teaching communication skills are successful, there is evidence that
success also depends on human variables. The ability to develop effective communication skills
is dependent on a number of human factors, including:
• individual characteristics, such as sociodemographics, professional and personal
experiences, health, burnout, depersonalization, ability to cope, psychological
characteristics, and technological demands;
• contextual characteristics, such as professional and personal environments; and
• pre-training communication skills.
Some ex
amples of patient comments regarding negative communication experiences include:
• “I wish he would face me instead of the computer.”
• “She seemed in a hurry and did not have time to listen to my fears about the surgery.”
• “He seemed to be hiding something when he told me about the medication mistake.”
• “I felt like I did not matter, my concerns were ignored.”
• “He seemed in a hurry to pull the plug on my dad so he could get on to the next task.”
To revi
ew the specialty-specific Program Requirements for Interpersonal and Communication
Skills:
• Go to https://www.acgme.org/specialties/
.
• Select the applicable specialty.
• Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
• Select the specialty Program Requirements currently in effect.
In addit
ion, Milestones are used to assess the progression of a resident in specific
competencies and subcompetencies. To access a specialty’s Milestones:
1. Go to https://www.acgme.org/specialties/
.
2. Select the applicable specialty.
3. Select “Milestones” at the top of the specialty section.
4. Select from the list of applicable Milestones.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
135

Below is an example of an Obstetrics and Gynecology Milestones evaluation of Interpersonal
and Communication Skills:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
136

COMMON PROGRAM REQUIREMENTS
IV.B. ACGME Competencies
IV.B.1
. The program must integrate the following ACGME Competencies
into the curriculum:
(Core)
IV.B.1
.f) Systems-based Practice
Resident
s must demonstrate an awareness of and
responsiveness to the larger context and system of health
care, including the structural and social determinants of
health, as well as the ability to call effectively on other
resources to provide optimal health care.
(Core)
Background and Intent: Medical practice occurs in the context of an increasingly
complex clinical care environment where optimal patient care requires attention to
compliance with external and internal administrative and regulatory requirements.
IV.B.1
.f).(1) Residents must demonstrate competence in:
IV.B.1.f).(1).(a) working effectively in various health care
delivery settings and systems relevant to their
clinical specialty;
(Core)
IV.B.1
.f).(1).(b) coordinating patient care across the health care
continuum and beyond as relevant to their
clinical specialty;
(Core)
Background and Intent: Every patient deserves to be treated as a whole person.
Therefore it is recognized that any one component of the health care system does not
meet the totality of the patient's needs. An appropriate transition plan requires
coordination and forethought by an interdisciplinary team. The patient benefits from
proper care and the system benefits from proper use of resources.
IV.B.1
.f).(1).(c) advocating for quality patient care and optimal
patien
t care systems;
(Core)
IV.B.1
.f).(1).(d) participating in identifying system errors and
implementing potential systems solutions;
(Core)
IV.B.1
.f).(1).(e) incorporating considerations of value, eq
uity,
cost awareness, delivery and payment, and
risk-benefit analysis in patient and/or
population-based care as appropriate; and,
(Core)
IV.B.1.f).(1).(f) understanding health care finances and its
impact on individual patients’ health decisions.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
137

V.B.1.f).(1).(g) using tools and techniques that promote patient
safety and disclosure of patient safety events
(real or simulated).
(Detail)
IV.B.1
.f).(2) Residents must learn to advocate for patients within
the heal
th care system to achieve the patient's and
patient’s family's care goals, including, when
appropriate, end-of-life goals.
(Core)
[The
Review Committee may further specify by adding to the
list of sub-competencies]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
138

GUIDANCE
Physicians are increasingly dependent on the health care system to support their patients. At
the same time, they can significantly influence the health care system to ensure appropriate
support for patients and their families. Most residents work passively in these settings, but the
curriculum must provide education on how residents can actively and positively have such an
impact on the system in their future practice. Their education and training should prepare
residents to answer the question: How can I help to improve the system of care?
There are many ways residents can participate in specialty-specific didactics or discussions
regarding their practice environment through institution-wide, multi-specialty, or multi-
disciplinary discussions. Residents may participate in one or more institutional or program
committees seeking to address health care system issues. These learning activities can be
longitudinal or part of regularly scheduled workshops.
References/Resources
1. Johnson, Julie K., Stephen H. Miller, and Sheldon D. Horowitz. 2008. “Systems-Based
Practice: Improving the Safety and Quality of Patient Care by Recognizing and
Improving the Systems in Which We Work.” In Advances in Patient Safety: New
Directions and Alternative Approaches (Vol. 2: Culture and Redesign). Vol. 2. Rockville,
MD: Agency for Healthcare Research and Quality (US).
https://www.ncbi.nlm.nih.gov/books/NBK43731/#_ncbi_dlg_citbx_NBK43731
.
2. Nabors, Christopher, Stephen J. Peterson, Roger Weems, Leanne Forman, Arif
Mumtaz, Randy Goldberg, Kausik Kar, et.al. 2011. “A Multidisciplinary Approach for
Teaching Systems-Based Practice to Internal Medicine Residents.” Journal of Graduate
Medical Education 3(1): 75-80. https://doi.org/10.4300/JGME-D-10-00037.1
.
3. “Systems-Based Practice: ACGME Core Competencies (Part 4 of 7).” 2016. NEJM
Knowledge. November 18. https://knowledgeplus.nejm.org/blog/acgme-core-
competencies-systems-based-practice/.
4. Wachtel, Ruth E. and Franklin Dexter. 2010. “Curriculum Providing Cognitive Knowledge
and Problem-Solving Skills for Anesthesia Systems-Based Practice.” Journal of
Graduate Medical Education 2(4): 624-632. https://doi.org/10.4300/JGME-D-10-00064.1.
To review the specialty-specific Program Requirements for Systems-based Practice
Competency,
1. Go to https://www.acgme.org/specialties.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
4. Select the specialty Program Requirements currently in effect.
In addit
ion, the Milestones are used to assess the progression of a resident in specific
competencies and subcompetencies. To access a specialty’s or subspecialty’s Milestones:
1. Go to https://www.acgme.org/specialties
.
2. Select the specialty.
3. Select “Milestones” at the top of the specialty section.
4. Select from the list of applicable Milestones.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
139

Below is an example of an Emergency Medicine Milestones evaluation of Systems-based
Practice:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
140

COMMON PROGRAM REQUIREMENTS
IV.C. Curriculum Organization and Resident Experiences
IV.C.1
.
The curriculum must be structured to optimize resident educational
experi
ences, the length of the experiences, and the supervisory
continuity. These educational experiences include an appropriate
blend of supervised patient care responsibilities, clinical teaching,
and didactic educational events.
(Core)
[The Review Committee must further specify]
Background and Intent: In some specialties, frequent rotational transitions, inadequate
continuity of faculty member supervision, and dispersed patient locations within the
hospital have adversely affected optimal resident education and effective team-based
care. The need for patient care continuity varies from specialty to specialty and by
clinical situation, and may be addressed by the individual Review Committee.
[The
Review Committee may specify required didactic and clinical
experiences]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
141

GUIDANCE
[The Review Committee must further specify]
Common Program Requirement IV.C.1. requires programs to optimize all educational
experiences, the length of the experiences, and supervision continuity. Review Committees
must further specify additional requirements, therefore programs must review the specialty-
specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
• Select the applicable specialty.
• Select “Program Requirements and FAQs and Applications” at the top of the specialty
section.
• Select the specialty Program Requirements currently in effect.
Quest
ions about specialty requirements should be directed to specialty Review Committee staff
members.
[The Review Committee may specify required didactic and clinical experiences]
Common Program Requirement IV.C. allows Review Committees to specify required didactic
and clinical experiences, so programs should consult the specialty-specific Program
Requirements for additional information.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
142

COMMON PROGRAM REQUIREMENTS
IV. Educational Program
IV.C. C
urriculum Organization and Resident Experiences
IV.C.2. The program must provide instruction and experience in pain
management if applicable for the specialty, including recognition of
the signs of substance use disorder.
(Core)
[The Review Committee may further specify]
[The
Review Committee may specify required didactic and clinical
experiences]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
143

GUIDANCE
Common Program Requirement IV.C.2. directs programs to develop evidence-based
educational interventions to effectively teach residents how to:
• prevent substance use disorder wherever possible while effectively treating pain;
• recognize substance use disorder in its earliest stages;
• function effectively in systems of care for effective pain relief and substance use
disorder;
• use non-pharmacologic means wherever possible; and
• participate in clinical trials of new non-opioid pain relief customized to the needs of the
clinical disorders of the populations they serve.
The ACGM
E expects that the education of residents and faculty members regarding prescribing
opioids be integrated into graduate medical education and professional development, including,
but not limited to, didactic lectures, specific learning modules, chart reviews, and small-group
discussions about difficult patients.
Review Co
mmittees monitor compliance with Common Program Requirement IV.C.2. in various
ways, including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by residents and faculty members as part of the annual ACGME
Resident/Fellow and Faculty Surveys; and
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
ADS screenshot: ADS Annual Update Common Program Requirements question
for applications and programs with statuses of Initial and Continued
Accreditation
The Resident/Fellow and Faculty Surveys include several questions that address the
requirements in Common Program Requirement IV.C.2. Two resource documents, the
“Resident/Fellow Survey-Common Program Requirements Crosswalk” and the “Faculty Survey-
Common Program Requirements Crosswalk,” provide additional information for programs on the
key areas addressed by the survey questions and how they map to the ACGME Common
©2024 Accreditation Council for Graduate Medical Education (ACGME)
144

Program Requirements. These documents can be found at https://www.acgme.org/data-
systems-technical-support/resident-fellow-and-faculty-surveys/.
GME Stakeholder Congress on Preparing Residents and Fellows to Manage Pain
and Substance Use Disorder
On March 30-31, 2021, the ACGME hosted a virtual graduate medical education (GME)
Stakeholder Congress on Preparing Residents and Fellows to Manage Pain and Substance Use
Disorder. The Congress brought together experts from across the medical education spectrum
with the goal of supporting programs in implementing Common Program Requirement IV.C.2.
by developing considerations for general and specialty-specific elements of a foundational
curriculum for the recognition and treatment of pain and substance use disorder. More
information about the Congress and a variety of resources are available on the ACGME website
at https://www.acgme.org/meetings-and-educational-activities/opioid-use-disorder/
.
National Academy of Medicine (NAM) Action Collaborative on Countering the US
Opioid Epidemic
The ACGME participates in and supports the NAM Action Collaborative on Countering the US
Opioid Epidemic.
Centers for Disease Control and Prevention (CDC) Guideline for Prescribing
Opioids for Chronic Pain
Improving the way opioids are prescribed through clinical practice guidelines can ensure
patients have access to safer, more effective chronic pain treatment while reducing the number
of people who misuse or overdose from these drugs.
The CDC developed and published the CDC Guideline for Prescribing Opioids for Chronic Pain
to provide recommendations for the prescribing of opioid pain medication for patients 18 and
older in primary care settings. Recommendations focus on the use of opioids in treating chronic
pain outside of active cancer treatment, palliative care, and end-of-life care.
The CDC has
also provided a number of Opioid Prescribing Guideline Resources that
complement and supplement the guideline, including clinical tools, practitioner FAQs, web-
based training for practitioner, and public educational videos.
Additional resources for pain management and substance use disorder
The following resources can be used to help programs and institutions identify solutions to meet
local needs. The ACGME does not endorse the use of any specific tool or resource.
• The ACGME-accredited multidisciplinary subspecialty of addiction medicine: The
ACGME Program Requirements for Addiction Medicine
(subspecialty) provide detailed
curricular elements related to medical knowledge and patient care that might be useful in
defining curricular and didactic substance use disorder experiences for residents and
fellows.
• ACP Pain Management Learning Series: The American College of Physicians provides
interactive modules, case studies, and videos supporting patient-centered pain
management, OUD identification, and OUD treatment. Content stresses communication
techniques and interdisciplinary team care. Modules can be viewed in a linear fashion or
independently. An X-Express buprenorphine waiver video supports implementation for
limited waiver applicants.
• FDA caution to avoid abrupt decrease or discontinuation of prescribed opioids: The US
©2024 Accreditation Council for Graduate Medical Education (ACGME)
145

Food and Drug Administration (FDA) identifies harm reported from sudden
discontinuation of opioid pain medicines, and requires label changes to guide
prescribers on gradual, individualized tapering. April 9, 2019.
• MAT Waivered Prescriber Support Initiative Presents: Medications for Opioid Use
Disorder: The purpose of this online training is to provide participants with a detailed
overview of medications that have been shown to be effective as a component of the
treatment of opioid use disorder.
• Medication-ass
isted treatment waiver training: Medication assisted treatment (MAT) of
substance use disorders involves a combination of medications that target the brain, and
psychosocial interventions (e.g., counseling, skills development) aimed at improving
treatment outcomes. Research shows that medications and therapy together may be
more successful than either treatment method alone.
• Medications for Opioid Use Disorder. Treatment Improvement Protocol (TIP) 63.
SAMHSA: This guide provides a comprehensive overview and guidance on issues
related to Opioid Use Disorder: signs and symptoms; diagnostic criteria; co-occurrence
with other substance use disorders; and prevention and treatment, including opioid
withdrawal techniques, pharmacotherapies, tapering opioids, and non-pharmacologic
interventions.
• New England Journal of Medicine Knowledge + Pain Management and Opioids learning
module: The New England Journal of Medicine, in partnership with Boston University
School of Medicine’s SCOPE of Pain and Area9 Lyceum, has instated a learning module
to assist in furthering education regarding pain management, opioid prescribing, and
Opioid Use Disorder (OUD).
• References of par
ticular interest:
o Lembke, Anna, Keith Humphreys, and Jordan Newmark. “Weighing the Risks and
Benefits of Chronic Opioid Therapy.” American Family Physician 93, no. 12 (June 16,
2016): 982-90. https://www.ncbi.nlm.nih.gov/pubmed/27304767
.
o Salsitz, Edwin A. “Chronic Pain, Chronic Opioid Addiction: a Complex
Nexus.” Journal of Medical Toxicology 12, no. 1 (2015): 54-57.
https://doi.org/10.1007/s13181-015-0521-9.
What does this mean for GME?
• Current residents and fellows will prescribe opioids for the next 40 years.
• Everyone involved in GME must be part of the solution.
• Clinical learning environments must use protocols and procedures that are:
o evidence-based;
o customized to the needs of the clinical disorders of the populations served; and
o effective in teaching residents how to:
treat pain while preventing substance use disorder;
recognize substance use disorder in its earliest stages;
function effectively in systems of care for effective pain relief and substance use
disorder treatment;
use non-pharmacologic means wherever possible; and
participate in clinical trials of new non-opioid pain relief.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
146

COMMON PROGRAM REQUIREMENTS
IV.D. Scholarship
Medic
ine is both an art and a science. The physician is a humanistic
scientist who cares for patients. This requires the ability to think critically,
evaluate the literature, appropriately assimilate new knowledge, and
practice lifelong learning. The program and faculty must create an
environment that fosters the acquisition of such skills through resident
participation in scholarly activities. Scholarly activities may include
discovery, integration, application, and teaching.
The ACG
ME recognizes the diversity of residencies and anticipates that
programs prepare physicians for a variety of roles, including clinicians,
scientists, and educators. It is expected that the program’s scholarship will
reflect its mission(s) and aims, and the needs of the community it serves.
For example, some programs may concentrate their scholarly activity on
quality improvement, population health, and/or teaching, while other
programs might choose to utilize more classic forms of biomedical
research as the focus for scholarship.
IV.D.1
. Program Responsibilities
IV.D.1
.a) The program must demonstrate evidence of scholarly
activities consistent with its mission(s) and aims.
(Core)
IV.D.1.b) The program, in partnership with its Sponsoring Institution,
must allocate adequate resources to facilitate resident and
faculty involvement in scholarly activities.
(Core)
[The Review Committee may further specify]
IV.D.1
.c) The program must advance residents’ knowledge and
practice of the scholarly approach to evidence-based patient
care.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
147
GUIDANCE
IV.D.1. Program responsibilities related to scholarship
This section focuses on requirements for program responsibilities related to scholarship and is
closely linked to both Common Program Requirements IV.D.2. — faculty scholarly activity —
and IV.D.3. — resident scholarly activity. As the italicized philosophy states, physicians require
“the ability to think critically, evaluate the literature, appropriately assimilate new knowledge, and
practice lifelong learning. The program and faculty must create an environment that fosters the
acquisition of such skills through resident participation in scholarly activities. Scholarly activities
may include discovery, integration, application, and teaching.”
IV.D.1.a) The program must demonstrate evidence of scholarly activities
consistent with its mission(s) and aims.
As the italicized philosophy states, “the ACGME recognizes the diversity of residencies and
anticipates that programs prepare physicians for a variety of roles, including clinicians,
scientists, and educators. It is expected that the program’s scholarship will reflect its mission(s)
and aims, and the needs of the community it serves.” For example, a program located in a rural
environment may want to focus on meeting the needs of the community, and advance scholarly
efforts on quality improvement measures or projects that would benefit the people it serves,
while a large cancer center in an urban institution may want to recruit faculty members and
residents whose primary research focus is basic science.
IV.D.1.b) The program, in partnership with its Sponsoring Institution, must
allocate adequate resources to facilitate resident and faculty involvement in
scholarly activities.
Depending on the mission and aims of each program, the resources needed to support resident
and faculty involvement in scholarly activities may vary greatly. The work taking place in a basic
science laboratory or the conduct of large clinical trials may require significant personnel,
laboratory, and other resources. There are many other scholarly activities that may not require
such resources. A key universal resource requirement for scholarly activities is time. Faculty
members and residents may need protected time away from clinical activities to successfully
engage in and perform scholarly activity.
IV.D.1.c) The program must advance residents’ knowledge and practice of the
scholarly approach to evidence-based patient care.
The scholarly approach can be defined as a synthesis of teaching, learning, and research with
the aim of encouraging curiosity and critical thinking based on an understanding of physiology,
pathophysiology, differential diagnosis, treatments, treatment alternatives, efficiency of care,
and patient safety. While some faculty members are responsible for fulfilling the traditional
elements of scholarship through research, integration, and teaching, all faculty members are
responsible for advancing residents’ scholarly approach to patient care.
Elements of a scholarly approach to patient care include:
• asking meaningful questions to stimulate residents to utilize learning resources to create
a differential diagnosis, diagnostic algorithm, and treatment plan;
• challenging the evidence that the residents use to reach their medical decisions so that
they understand the benefits and limits of the medical literature;
©2024 Accreditation Council for Graduate Medical Education (ACGME)
148
• when appropriate, disseminating scholarly learning in a peer-reviewed manner
(publication or presentation); and,
• improving residents’ learning by encouraging them to teach using a scholarly approach.
The scholarly approach to patient care begins with curiosity, is grounded in the principles of
evidence-based medicine, expands the knowledge base through dissemination, and develops
the habits of lifelong learning by encouraging residents to be scholarly teachers.
The intent
is to create an environment of scholarship to encourage critical thinking in providing
patient care, e.g., discussing the rationale for a new and expensive therapeutic option;
discontinuing a “popular” treatment option based on evidence that it provides no benefits;
adapting an approach to early discontinuation of central venous catheters or bladder catheters
when these devices are no longer essential for the care of the patient; or the judicious use of
antibiotics. These scholarly approaches are all designed to instill curiosity and critical thinking in
patient care. There is evidence that fostering this mindset in residents during residency implants
lifelong habits that continue decades after graduation.
• An envi
ronment of scholarship:
o leads to the creation of new knowledge;
o encourages lifelong learning;
o creates a mindset of inquiry that
might reduce “jumping on any bandwagon that comes along;” and
develops mindful practice habits, e.g., antibiotic stewardship, infection control,
and careful consideration of new (and expensive) drugs before use.
• Boyer’s (1990) Models of Scholarship:
o The scholarship of DISCOVERY
Traditional definition: research
Search for new knowledge
Discovery of new information and new models
Sharing discoveries through scholarly publication
o The scholarship of INTEGRATION
integrates knowledge from different sources
presents overview of findings in a resource topic
brings findings together from different disciplines to discover convergence
Identifies trends and sees knowledge in new ways
o examples: professional development workshops, literature reviews, meta-
analysis, quality improvement projects
o The scholarship of APPLICATION
discovers ways that new knowledge can be used to solve real-world problems
identifies new intellectual problems that can arise out of the very act of
application
examples: translational research, development of community activities that link
with academic work, development of centers for study or service, quality
improvement projects
o The scholarship of TEACHING
searches for innovative approaches and best practices to develop skills and
disseminate knowledge
examples: courses; innovative teaching materials; educational research;
instructional activities; publication of books or other teaching materials; quality
©2024 Accreditation Council for Graduate Medical Education (ACGME)
149
improvement projects; digital scholarship, including open education resources
(Massive Open Online Courses (MOOCs), Khan Academy, digital publishing, and
providing courses in Blackboard
®
, Bridge
®
, and Moodle
®
)
There are many ways to provide these curricular elements. Programs may wish to cover specific
topics at monthly sessions over a one-year period. These sessions do not need to be taught by
the program director; this is an opportunity for collaboration, where experts in the topic can be
invited to speak. There are many web-based curricula for teaching these topics as well.
Key t
o this process is faculty mentorship. While there may be some residents who begin the
program with specific research plans, many do not. They need guidance from faculty mentors
who can help them design and conduct a study, gather and analyze data, and write up results
for presentation or publication. Faculty members also need to be involved in, or even lead,
journal club and other scholarly activities.
An envi
ronment of scholarship is essential to ensuring residents continue applying the methods
of the scholarly approach in their own practice after completion of the program.
Reference
Boyer, Ernest L., 1990. Scholarship reconsidered: priorities of the professoriate, A
special report. The Carnegie Foundation for the Advancement of Teaching, Princeton
University Press.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
150

COMMON PROGRAM REQUIREMENTS
IV. Educational Program
IV.D. Scholarship
Medicine is both an art and a science. The physician is a humanistic
scientist who cares for patients. This requires the ability to think critically,
evaluate the literature, appropriately assimilate new knowledge, and
practice lifelong learning. The program and faculty must create an
environment that fosters the acquisition of such skills through resident
participation in scholarly activities. Scholarly activities may include
discovery, integration, application, and teaching.
The ACG
ME recognizes the diversity of residencies and anticipates that
programs prepare physicians for a variety of roles, including clinicians,
scientists, and educators. It is expected that the program’s scholarship will
reflect its mission(s) and aims, and the needs of the community it serves.
For example, some programs may concentrate their scholarly activity on
quality improvement, population health, and/or teaching, while other
programs might choose to utilize more classic forms of biomedical
research as the focus for scholarship.
IV.D.2. Faculty Scholarly Activity
IV.D.2
.a) Among their scholarly activity, programs must demonstrate
accomplishments in at least three of the following domains:
(Core)
• Research i
n basic science, education, translational
science, patient care, or population health
• Peer-reviewed grants
• Quality improvement and/or patient safety initiatives
• Systematic reviews, meta-analyses, review articles,
chapters in medical textbooks, or case reports
• Creation of curricula, evaluation tools, didactic
educational activities, or electronic educational
materials
• Contribution to professional committees, educational
organizations, or editorial boards
• Innovations in education
IV.D.2.b) The program must demonstrate dissemination of scholarly
activity within and external to the program by the following
methods:
[Revi
ew Committee will choose to require either IV.D.2.b).(1)
or both IV.D.2.b).(1) and IV.D.2.b).(2)]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
151

Background and Intent: For the purposes of education, metrics of scholarly activity
represent one of the surrogates for the program’s effectiveness in the creation of an
environment of inquiry that advances the residents’ scholarly approach to patient care.
The Review Committee will evaluate the dissemination of scholarship for the program
as a whole, not for individual faculty members, for a five-year interval, for both core
and non-core faculty members, with the goal of assessing the effectiveness of the
creation of such an environment. The ACGME recognizes that there may be differences
in scholarship requirements between different specialties and between residencies and
fellowships in the same specialty.
IV.D.2
.b).(1) faculty participation in grand rounds, posters,
workshops, quality improvement presentations,
podium presentations, grant leadership, non-peer-
reviewed print/electronic resources, articles or
publications, book chapters, textbooks, webinars,
service on professional committees, or serving as a
journal reviewer, journal editorial board member, or
editor;
(Outcome)
IV.D.2
.b).(2) peer-reviewed publication.
(Outcome)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
152
GUIDANCE
The requirements for faculty scholarship in Common Program Requirement IV.D.2. are closely
linked to the program responsibility of ensuring that residents and faculty members are provided
with a scholarly environment as specified in Common Program Requirement IV.D.1. and
resident scholarly activity as specified in IV.D.3.
Facult
y scholarly activity demonstrates to the Review Committees that:
• Faculty members have the skills to analyze and utilize new knowledge.
• The program has the ability to teach those skills to residents.
• An environment of scholarship exists in the program.
While
the value of scholarly activity is undeniable, such as the publication of peer-reviewed
journal articles and the presentation of basic science research at national conferences, other
activities are equally valuable. Scholarship is not done only for its own sake, but also serves as
a proxy for the creation of a clinical learning environment that encourages an environment of
inquiry and an evidence-based, scholarly approach to patient care.
The phil
osophical statement associated with section IV.D. of the Common Program
Requirement on the previous page, bears repeating:
Medic
ine is both an art and a science. The physician is a humanistic scientist who cares for
patients. This requires the ability to think critically, evaluate the literature, appropriately
assimilate new knowledge, and practice lifelong learning. The program and faculty must
create an environment that fosters the acquisition of such skills through resident
participation in scholarly activities.
and
It is expected that the program’s scholarship will reflect its mission(s) and aims, and
the needs of the community it serves. For example, some programs may concentrate
their scholarly activity on quality improvement, population health, and/or teaching, while
others might use more classic forms of biomedical research as the focus for scholarship.
There is
wide variability in programs and the communities they serve. For example, a program
in a remote, rural community might focus on primary care education and training, and may not
want or have the resources to put together a million-dollar laboratory to study some
characteristics of a murine model of disease. Instead, it may emphasize improving vaccination
rates, increasing compliance with diabetes care, or determining how to deal with an opioid
epidemic in the community.
IV.D.2.a) Among their [faculty] scholarly activity, programs must demonstrate
accomplishments in at least three of the following domains:
• research in basic science, education, translational science, patient care, or population
health;
• peer-reviewed grants;
• quality improvement and/or patient safety initiatives;
• systematic reviews, meta-analyses, review articles, chapters in medical textbooks, or
case reports;
©2024 Accreditation Council for Graduate Medical Education (ACGME)
153

• creation of curricula, evaluation tools, didactic educational activities, or electronic
educational materials;
• contribution to professional committees, educational organizations, or editorial boards;
and
• innovations in education.
The program will be reviewed in aggregate. This requirement does not mean that each faculty
member must have activity in three domains.
IV.D.2.b) The program must demonstrate dissemination of scholarly activity
within and external to the program by the following methods:
IV.D.2.b).(1) faculty participation in grand rounds, posters, workshops, quality
improvement presentations, podium presentations, grant leadership, non-
peer-reviewed print/electronic resources, articles or publications, book
chapters, textbooks, webinars, service on professional committees, or
serving as a journal reviewer, journal editorial board member, or editor;
IV.D.2.b).(2) peer-reviewed publication.
The Review Committee will choose to require either Common Program Requirement
IV.D.2.b).(1) or both IV.D.2.b).(1) and IV.D.2.b).(2), so programs are encouraged to reference
the specialty-specific Program Requirements. This
ACGME Review Committee Faculty
Scholarly Activity Decisions document provides a synopsis of the faculty scholarly activity
requirement across all specialties and subspecialties. Some Review Committees also provide
further information on their interpretation of these requirements in associated specialty-specific
FAQs. These documents, for specialties that provide them, can be found on the Program
Requirements and FAQs and Applications section of the
specialty-specific w
eb pages.
Accreditation Data System (ADS) screenshots: faculty scholarly activity
instructions and data entry screens (see below)
1. Faculty scholarly activity instructions
2. The “Download Scholarly Activity Template” button in the screenshot
above will pull up an Excel spreadsheet to enter information. The purpose of
the spreadsheet is for programs to disseminate it to program faculty members to aid in
the collection of accurate scholarly activity data. The spreadsheet includes definitions of
the different types of scholarly activities.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
154

3. The faculty scholarly activity summary provides a list of all faculty
members in the program and allows programs to update scholarly activity
information for each individual faculty member by adding it, copying
information another program has entered, or reporting “no activity.”
4. The columns on the faculty scholarly activity data entry screen have an
“information” button that expands to provide a more specific definition of
each type of scholarly activity. Those definitions are also provided in the
downloadable Excel template, and are included below.
• PubMed IDs (PMIDs)
The PMID is a unique number assigned to each PubMed record. This is
generally an eight-digit number. Enter up to four PMIDs (assigned by PubMed)
for articles published during the previous academic year. The PubMed Central
reference number (PMCID) is different from the PubMed reference number
(PMID). PubMed Central is an index of full-text papers, while PubMed is an index
of abstracts.
If this faculty is a designated osteopathic faculty, use the
checkboxes (if applicable) to indicate if an article integrated the application of
Osteopathic Principles and Practice (OPP).
• Non-PMI
D Peer Review Publications: Number of peer-reviewed publications
without a PMID, which are not recognized by the National Library of Medicine
during the previous academic year.
• Other Publications: Number of other articles/publications without PMIDs and
not peer reviewed. Examples include editorials, online magazines, or other
©2024 Accreditation Council for Graduate Medical Education (ACGME)
155

activities related to item-writing (e.g., board examination questions) during the
previous academic year.
• Conference Presentations: Number of abstracts, posters, and presentations at
international, national, state, or regional meetings during the previous academic
year.
• Other Presentations: Number of other presentations (e.g., grand rounds, invited
professorships), materials developed (e.g., computer-based modules) during the
previous academic year.
• Chapters/Textbooks: Number of chapters or textbooks published during the
previous academic year.
• Grant Leadership: Number of grants for which faculty member had a leadership
role (e.g., principal investigator [PI], co-PI, or site director) during the previous
academic year.
• Leadership or Peer-Review Role: Active leadership role (such as serving on
committees or governing boards) in international, national, state, or regional
medical organizations or served as reviewer or editorial board member for a
peer-reviewed journal during the previous academic year.
• Formal Courses: Responsible for seminars, conference series, or course
coordination (e.g., arrangement of presentations and speakers, organization of
materials). This includes developing training modules for medical students,
residents, fellows, and other health professionals (e.g., simulation). Program
didactics and/or conferences are not considered formal courses.
5. The legend at the bottom of the faculty scholarly activity data entry screen
provides the key domains for scholarly activity. These domains are also
available in the Excel template and on the individual faculty scholarly activity
entry screen.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
156

6. The screenshots below depict the individual faculty scholarly activity data
entry.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
157

Resources
The following presentation is available on the ACGME website and provides helpful tips for
entering scholarly activity in ADS as part of the ADS Annual Update and avoiding common
citations.
• Video: Av
oiding Common Errors in the ADS Annual Update - Entering Scholarly Activity
into ADS
©2024 Accreditation Council for Graduate Medical Education (ACGME)
158

COMMON PROGRAM REQUIREMENTS
IV. Educational Program
IV.D. Scholarship
Medicine is both an art and a science. The physician is a humanistic
scientist who cares for patients. This requires the ability to think critically,
evaluate the literature, appropriately assimilate new knowledge, and
practice lifelong learning. The program and faculty must create an
environment that fosters the acquisition of such skills through resident
participation in scholarly activities. Scholarly activities may include
discovery, integration, application, and teaching.
The ACG
ME recognizes the diversity of residencies and anticipates that
programs prepare physicians for a variety of roles, including clinicians,
scientists, and educators. It is expected that the program’s scholarship will
reflect its mission(s) and aims, and the needs of the community it serves.
For example, some programs may concentrate their scholarly activity on
quality improvement, population health, and/or teaching, while other
programs might choose to utilize more classic forms of biomedical
research as the focus for scholarship.
IV.D.3
. Resident Scholarly Activity
IV.D.3
.a) Residents must participate in scholarship
(Core)
[The Review Committee may further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
159

GUIDANCE
The requirement for resident participation in scholarship in Common Program Requirement
IV.D.3.a) is closely linked to the program responsibility of ensuring that the faculty members and
residents are provided with a scholarly environment as specified in Common Program
Requirement IV.D.1. and faculty scholarly activity as specified in Common Program
Requirement IV.D.2.
Resi
dent scholarly activity demonstrates to the Review Committees that the program can teach
scholarship skills to residents and that an environment of scholarship exists in the program.
[The Review Committee may further specify]
Since Review Committees may specify requirements for resident scholarly activity, programs
must review the specialty-specific Program Requirements:
1. Go to https://www.acgme.org/specialties/.
2. Select the applicable specialty.
3. Select “Program Requirements and FAQs and Applications” at the top of the specialty
page.
4. Select the specialty Program Requirements currently in effect.
Quest
ions about subspecialty Program Requirements related to resident scholarly activity
should be directed to specialty Review Committee staff members.
Review Committees consider the wide variability in programs and the communities they serve
when evaluating programs. For example, a program in a remote, rural community might focus
on primary care education and training and may not want or have the resources to put together
a million-dollar laboratory to study some characteristics of a murine model of disease. Instead, it
may emphasize improving vaccination rates, increasing compliance with diabetes care, or
determining how to deal with an opioid epidemic in the community.
Accreditation Data System (ADS) screenshots: resident scholarly activity
instructions and data entry screens
1. Resident scholarly activity instructions
©2024 Accreditation Council for Graduate Medical Education (ACGME)
160

2. The “Download Scholarly Activity Template” button in the screenshot
above will pull up an Excel spreadsheet to enter information. The purpose of
the spreadsheet is for programs to disseminate it to residents to aid in the collection of
accurate scholarly activity data. The spreadsheet includes definitions of the different
types of scholarly activities.
3. The resident scholarly activity summary provides a list of all residents in
the program and allows programs to update scholarly activity information
for each individual resident. NOTE: The information requested is for the previous
academic year only. First-year residents in the program will not appear on the list.
4. The columns on the resident scholarly activity data entry screen have an
“information” button that expands to provide a more specific definition of
each type of scholarly activity. Those definitions are also provided in the
downloadable Excel template and are included below.
• PubMed IDs (PMIDs):
The PMID is a unique number assigned to each PubMed record. This is generally an
eight-digit number. Enter up to four PMIDs
(assigned by PubMed) for articles
published during the previous academic year. The PubMed Central reference
number (PMCID) is different from the PubMed reference number (PMID). PubMed
Central is an index of full-text papers, while PubMed is an index of abstracts. If this
resident is a designated osteopathic resident, use the checkboxes (if applicable) to
©2024 Accreditation Council for Graduate Medical Education (ACGME)
161

indicate if an article integrated the application of Osteopathic Principles and Practice
(OPP).
• Other Publications: Number of articles without PMIDs, non-peer-reviewed
publications, peer-reviewed publications which are not recognized by the National
Library of Medicine, and activities related to item-writing (e.g., board examination
questions) during the previous academic year.
• Conference Presentations: Number of abstracts, posters, and presentations given
at international, national, or regional meetings during the previous academic year.
• Chapters/Textbooks: Number of chapters or textbooks published during the
previous academic year.
• Participated in Research: Participated in funded or non-funded basic science or
clinical outcomes research project during the previous academic year.
• Teaching Presentations: Lecture or presentation (such as grand rounds or case
presentations) of at least 30-minute duration within the Sponsoring Institution or
program during the previous academic year.
5. The screenshots below depict the individual resident scholarly activity data
entry.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
162

If a program sends its residents to a one-month rotation at a participating site where faculty
members produce a large amount of scholarly activity, it would be improper for the program to
list all the scholarly activities at that participating site. Doing so does not meet substantial
compliance with the requirement to create an environment of scholarship. The idea behind this
requirement is that residents be “immersed” in an environment of scholarship and inquiry
throughout their educational programs.
Resources:
The following presentation is available on the ACGME website and provides helpful tips for
entering scholarly activity in ADS as part of the ADS Annual Update and avoiding common
citations.
• Video: Av
oiding Common Errors in the ADS Annual Update - Entering Scholarly Activity
into ADS
©2024 Accreditation Council for Graduate Medical Education (ACGME)
163

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.A. Resident Evaluation
V.A.1. Feedback and Evaluation
Background and Intent: Feedback is ongoing information provided regarding aspects of one’s
performance, knowledge, or understanding. The faculty empower residents to provide much
of that feedback themselves in a spirit of continuous learning and self-reflection. Feedback
from faculty members in the context of routine clinical care should be frequent, and need not
always be formally documented.
Formative and summative evaluation have distinct definitions. Formative evaluation is
monitoring resident learning and providing ongoing feedback that can be used by residents
to improve their learning in the context of provision of patient care or other educational
opportunities. More specifically, formative evaluations help:
• residents identify their strengths and weaknesses and target areas that need work
• program directors and faculty members recognize where residents are struggling and
address problems immediately
Summative evaluation is evaluating a resident’s learning by comparing the residents against
the goals and objectives of the rotation and program, respectively. Summative evaluation is
utilized to make decisions about promotion to the next level of training, or program
completion.
End-of-rotation and end-of-year evaluations have both summative and formative components.
Information from a summative evaluation can be used formatively when residents or faculty
members use it to guide their efforts and activities in subsequent rotations and to
successfully complete the residency program.
Feedback, formative evaluation, and summative evaluation compare intentions with
accomplishments, enabling the transformation of a neophyte physician to one with growing
expertise.
V.A.1.a) Faculty members must directly observe, evaluate, and frequently
provide feedback on resident performance during each rotation or
similar educational assignment.
(Core)
Background and Intent: Faculty members should provide feedback frequently throughout the
course of each rotation. Residents require feedback from faculty members to reinforce well-
performed duties and tasks, as well as to correct deficiencies. This feedback will allow for the
development of the learner as they strive to achieve the Milestones. More frequent feedback is
strongly encouraged for residents who have deficiencies that may result in a poor final
rotation evaluation.
V.A.1.b) Evaluation must be documented at the completion of the
assignment.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
164

V.A.1.b).(1) For block rotations of greater than three months in duration,
evaluation must be documented at least every three months.
(Core)
V.A.1.b).(2) Longitudinal experiences, such as continuity clinic in the
context of other clinical responsibilities, must be evaluated at
least every three months and at completion.
(Core)
V.A.1.c) The program must provide an objective performance evaluation
based on the Competencies and the specialty-specific Milestones,
and must:
(Core)
V.A.1.c).(1) use multiple evaluators (e.g., faculty members, peers,
patients, self, and other professional staff members); and,
(Core)
V.A.1.c).(2) provide that information to the Clinical Competency
Committee for its synthesis of progressive resident
performance and improvement toward unsupervised practice.
(Core)
V.A.1.d) The program director or their designee, with input from the Clinical
Competency Committee, must:
V.A.1.d).(1) meet with and review with each resident their
documented semi-annual evaluation of performance,
including progress along the specialty-specific
Milestones;
(Core)
V.A.1.e) At least annually, there must be a summative evaluation of each
resident that includes their readiness to progress to the next year of
the program, if applicable.
(Core)
V.A.1.f) The evaluations of a resident’s performance must be accessible for
review by the resident.
(Core)
[The Review Committee may further specify under any requirement in
V.A.1.-V.A.1.f)]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
165

GUIDANCE
The requirements included in this section are generally self-explanatory, including descriptions
of evaluation frequency and when they should be performed.
V.A.1.a) Faculty members must directly observe, evaluate, and frequently provide
feedback on resident performance during each rotation or similar educational
assignment.
Common Program Requirements V.A.1.a) is unequivocal in stating that direct observation is key
to the evaluation of resident performance and progress. The Background and Intent box further
emphasizes that “faculty members should provide feedback frequently throughout the course of
each rotation. Residents require feedback from faculty members to reinforce well-performed
duties and tasks, as well as to correct deficiencies. [This feedback will allow for development of
learners as they strive to achieve the Milestones.] More frequent feedback is strongly
encouraged for residents who have deficiencies that may result in a poor final rotation
evaluation.”
Evaluation and feedback can be provided during the provision of clinical care for any of the six
required Competency areas. Faculty members have many responsibilities that sometimes
require short clinical rotations of five days or less. It is important to note that continuity of
observation is just as important; even in short rotations, continuity allows faculty members to
know the resident and for the resident to observe the faculty members.
V.A.1.b) Evaluation must be documented at the completion of the assignment.
Timely faculty member completion of resident evaluation following completion of an assignment
is crucial to a resident’s development. Evaluation must address strengths and areas for
improvement. Requirements V.A.1.b).(1) and (2) further specify that for block rotations or
continuity experiences that are longer than three months in duration, an evaluation must be
documented at least every three months.
ADS screenshots: overall evaluation methods
Either as part of an application for accreditation or annually, as part of the ADS Annual Update,
the program director must answer or update the following question regarding end of rotation
evaluations.
V.A.1.c) The program must provide an objective performance evaluation based on
the Competencies and the specialty-specific Milestones, and must:
(Core)
V.A.1.c).(1) use multiple evaluators (e.g., faculty members, peers, patients, self,
and other professional staff members); and,
In addition to faculty members, residents interact with many other health providers, including
nurses, physician assistants, other physicians, residents, fellows, peers, and patients. The input
of the relevant individuals or groups is needed to provide an overall picture of resident
performance. Notably, residents asked to provide a self-evaluation using the Milestones have
been shown to develop a better perspective of their own performance.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
166

V.A.1.c).(2) provide that information to the Clinical Competency Committee for its
synthesis of progressive resident performance and improvement toward
unsupervised practice.
V.A.1.d) The program director or their designee, with input from the Clinical
Competency Committee, must:
V.A.1.d).(1) meet with and review with each resident their documented semi-
annual evaluation of performance, including progress along the specialty-specific
Milestones;
(Core)
Although this requirement is self-explanatory, it is critical to note that the semi-annual evaluation
of performance must include a review of the resident’s progress on the specialty-specific
milestones. As the Background and Intent further states, “Learning is an active process that
requires effort from the teacher and the learner. Faculty members evaluate a resident's
performance at least at the end of each rotation. The program director or their designee will
review those evaluations, including their progress on the Milestones, at a minimum of every six
months. Residents should be encouraged to reflect upon the evaluation, using the information to
reinforce well-performed tasks or knowledge or to modify deficiencies in knowledge or practice.
Working together with the faculty members, residents should develop an individualized learning
plan.”
Accreditation Data System (ADS) screenshot: semi-annual evaluation
The program director must answer or update the following question as part of the ADS Annual
Update to acknowledge meeting with the residents to review their documented semi-annual
evaluation of performance, including progress along the specialty-specific milestones.
V.A.1.e) At least annually, there must be a summative evaluation of each resident
that includes their readiness to progress to the next year of the program, if
applicable.
The end-of-year, summative evaluation of each resident must include a specific statement about
the resident’s readiness to progress to the next year of the program and it should be discussed
by the Clinical Competency Committee.
V.A.1.f) The evaluations of a resident’s performance must be accessible for
review by the resident.
Residents must be able to access their performance evaluations, which could be in
electronic or hard copy format, depending on the system used by each program.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
167

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.A. R
esident Evaluation
V.A.1. Feedback and Evaluation
Background and Intent: Feedback is ongoing information provided regarding aspects
of one’s performance, knowledge, or understanding. The faculty empower residents to
provide much of that feedback themselves in a spirit of continuous learning and self-
reflection. Feedback from faculty members in the context of routine clinical care
should be frequent, and need not always be formally documented. Formative and
summative evaluation have distinct definitions. Formative evaluation is monitoring
resident learning and providing ongoing feedback that can be used by residents to
improve their learning in the context of provision of patient care or other educational
opportunities. More specifically, formative evaluations help:
• residents identify their strengths and weaknesses and target areas that need
work
• program directors and faculty members recognize where residents are
struggling and address problems immediately
Summative evaluation is evaluating a resident’s learning by comparing the residents
against the goals and objectives of the rotation and program, respectively. Summative
evaluation is utilized to make decisions about promotion to the next level of training, or
program completion. End-of-rotation and end-of-year evaluations have both summative
and formative components. Information from a summative evaluation can be used
formatively when residents or faculty members use it to guide their efforts and
activities in subsequent rotations and to successfully complete the residency program.
Feedback, formative evaluation, and summative evaluation compare intentions with
accomplishments, enabling the transformation of a neophyte physician to one with
growing expertise.
V.A.1
.d).(2) assist residents in developing individualized learning plans to
capitalize on their strengths and identify areas for growth;
and
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
168

GUIDANCE
Common Program Requirement V.A.1.d).(2) was written with the intention of ensuring that the
program director and faculty members help residents to develop individualized learning plans
(ILPs) that capitalize on their strengths and identify any areas that need additional support or
effort.
General
ly, ILPs include self-assessment and reflection, career goals, development of plans to
achieve the goal(s), assessment of progress toward the goal(s), and revising/generating new
goals. An ILP is a living document that must be reviewed to ensure progress and refocus as
needed. Goals can be short term and/or long term. ILPs help residents learn the concepts of
lifelong learning and practice-based learning and improvement.
Barr
iers to successful implementation of an ILP (identified by residents)
• difficulty with self-reflection
• environmental strain: fatigue, time constraints
• competing demands: personal and work
• difficulty with goal generation
Dif
ficulties in developing a plan and plan implementation
• not seeing the patient population needed for clinical goals
• not having time to consistently review the plan with a mentor
• Lack of objective measures when goals that were created goals cannot be tracked
The ACGME has developed several resources for programs that include more information on
ILPs, including components of an ILP and what ILPs are and what they are not. The Clinical
Competency Committee Guidebook provides more insight on this requirement and ILPs.
Component
s of an ILP (Li and Burke, 2010)
• reflection on goals and self-assessment of strengths and weaknesses
• generation of specific learning goals and/or objectives
• specific plans or strategies to achieve each goal focused on what the learner will do to
improve
• mutual agreement on how the assessment of progress on each goal will be determined
• eventual revision of goals or creation of new goals based on performance
• expected timeline
ILPs are:
• formulated by the individual (resident/fellow) – made by the learner, for the learner;
• guided by a facilitator (faculty member, advisor, coach, or program director);
• an exercise in self-assessment and self-reflection;
• iterative;
• an ACGME core requirement; and
• an indicator of insight and ability to become an independent lifelong learner.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
169

ILPs are not:
• set in stone – they can and should be revisited by both the learner and the facilitator;
• a portfolio;
• evaluations; or
• The sole or major responsibility of the program director (or faculty) or the program.
References/Resources
1. Li, Su-Ting T., and Ann E. Burke. 2010. “Individualized Learning Plans: Basics and
Beyond.” Academic Pediatrics 10(5): 289–92.
https://doi.org/10.1016/j.acap.2010.08.002.
2. Li, Su-Ting T., Debora A. Paterniti, John Patrick T. Co, and Daniel C. West. 2010.
“Successful Self-Directed Lifelong Learning in Medicine: A Conceptual Model Derived
From Qualitative Analysis of a National Survey of Pediatric Residents.” Academic
Medicine 85(7): 1229–36. https://doi.org/10.1097/acm.0b013e3181e1931c.
3. Li, Su-Ting T., Debora A. Paterniti, Daniel J. Tancredi, John Patrick T. Co, and Daniel C.
West. 2011. “Is Residents' Progress on Individualized Learning Plans Related to the
Type of Learning Goal Set?” Academic Medicine 86(10): 1293-1299.
doi:10.1097/ACM.0b013e31822be22b.
4. University of Washington Graduate Medical Education. “Resident and Fellow Education:
Individualized Learning Plan (ILP).” https://sites.uw.edu/uwgme/resident-evaluation/#ilp.
Accessed 2023.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
170

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.A. R
esident Evaluation
V.A.1. Feedback and Evaluation
Background and Intent: Feedback is ongoing information provided regarding aspects
of one’s performance, knowledge, or understanding. The faculty empower residents to
provide much of that feedback themselves in a spirit of continuous learning and self-
reflection. Feedback from faculty members in the context of routine clinical care
should be frequent, and need not always be formally documented.
Format
ive and summative evaluation have distinct definitions. Formative evaluation is
monitoring resident learning and providing ongoing feedback that can be used by
residents to improve their learning in the context of provision of patient care or other
educational opportunities. More specifically, formative evaluations help:
• resident
s identify their strengths and weaknesses and target areas that need
work
• program directors and faculty members recognize where residents are
struggling and address problems immediately
Summ
ative evaluation is evaluating a resident’s learning by comparing the residents
against the goals and objectives of the rotation and program, respectively. Summative
evaluation is utilized to make decisions about promotion to the next level of training, or
program completion.
End-of-rot
ation and end-of-year evaluations have both summative and formative
components. Information from a summative evaluation can be used formatively when
residents or faculty members use it to guide their efforts and activities in subsequent
rotations and to successfully complete the residency program.
Feedback, formative evaluation, and summative evaluation compare intentions with
accomplishments, enabling the transformation of a neophyte physician to one with
growing expertise.
V.A.1
.d) The program director or their designee, with input from the Clinical
Competency Committee, must:
V.A.1.d).(3) develop plans for residents failing to progress, following
institutional policies and procedures.
(Core)
Background and Intent: Learning is an active process that requires effort from the
teacher and the learner. Faculty members evaluate a resident's performance at least at
the end of each rotation. The program director or their designee will review those
evaluations, including their progress on the Milestones, at a minimum of every six
months. Residents should be encouraged to reflect upon the evaluation, using the
information to reinforce well-performed tasks or knowledge or to modify deficiencies in
©2024 Accreditation Council for Graduate Medical Education (ACGME)
171

knowledge or practice. Working together with the faculty members, residents should
develop an individualized learning plan.
Residents who are experiencing difficulties with achieving progress along the
Milestones may require intervention to address specific deficiencies. Such intervention,
documented in an individual remediation plan developed by the program director or a
faculty mentor and the resident, will take a variety of forms based on the specific
learning needs of the resident. However, the ACGME recognizes that there are
situations which require more significant intervention that may alter the time course of
resident progression. To ensure due process, it is essential that the program director
follow institutional policies and procedures.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
172

GUIDANCE
V.A.1.d). and V.A.1.d).(3). The program director or their designee, with input from
the Clinical Competency Committee, must develop plans for residents failing to
progress, following institutional policies and procedures.
The Background and Intent reinforces the importance of institutional policies and procedures in
this process: “To ensure due process, it is essential that the program director follow institutional
policies and procedures.” It is, therefore, strongly encouraged that program directors work
closely with the designated institutional official (DIO) to ensure all applicable policies and
procedures are followed and the appropriate institutional departments are engaged in the
process of addressing residents failing to progress at the appropriate time. The goal of these
processes is to help residents in difficulty to succeed while also ensuring appropriate
documentation of resident performance and due process.
Mil
estones assessments and evaluations by the Clinical Competency Committee (CCC) are
essential to the early identification of residents in difficulty.
To assi
st with fulfilling this responsibility, the ACGME has developed a Remediation Toolkit
authored by experts from across the country. This free course consists of 11 modules covering
a range of essential topics related to remediation. These modules will equip educators and
administrators with a solid foundation for addressing the needs of struggling learners,
implementing effective remediation strategies, and fostering a supportive and conducive
learning environment in GME. The toolkit is available in
Learn at ACGME and is part of a suite
of materials to aid in faculty development, including the Improving Assessment Using Direct
Observation Toolkit and the Developing Faculty Competencies in Assessment Course.
The st
udies listed below address the issue of residents failing to progress.
1. Cosco, Dominique, Denise Dupras, Maggie So, Eugene Lee, Jason Schneider, and
Randall Edson. 2014. “Look on the Bright Side: Case Studies in Successful
Remediation of Problem Learners. Tools for Faculty and Staff/Remediation.”
Academic Medicine Insight 12(3): 8-11.
Cosco et al. studied cases in which remediation of problem learners was successful and
identified some key steps
o identification of the issue (competency-based)
o multiple sources of learner assessment
o early feedback and intervention
o resident reflection with buy-in
o specific remediation goals with outlined consequences for failure to meet goals
o frequent follow-up
o group effort
o thorough documentation
©2024 Accreditation Council for Graduate Medical Education (ACGME)
173

2. Dupras, Denise M., Randall S. Edson, Andrew J. Halvorsen, Robert H. Hopkins, and
Furman S. McDonald. 2012. “‘Problem Residents’: Prevalence, Problems and
Remediation in the Era of Core Competencies.” The American Journal of Medicine
125,(4): 421–25. https://doi.org/10.1016/j.amjmed.2011.12.008
.
The authors studied the prevalence of residents in difficulty, and the problems associated
with placing a resident in remediation. They suggested a change of terms from “problem
residents” to “residents in difficulty” (RID).
The authors conducted a survey of members of the Association of Program Directors in
Internal Medicine:
o 372 program directors were surveyed (97.1% of 383 US categorical internal
medicine programs).
o 268 program directors (72%) completed the survey.
o 197 program directors reported RID.
o 3.5% of residents were identified as RID (532 of 15,031 total residents with a mean
of 2.9 RIDs per program).
They noted
that factors that correlated with subsequent need for probation/remediation
included low scores on the Internal Medicine In-Training Examination and the US Medical
Licensing Examination Step 3.
Resi
dents in difficulty were most frequently identified by faculty member (#1). They were
also identified by supervising/chief residents, program directors, fellows, and nurses.
The most
common deficiencies of residents in difficulty identified in this study included:
o patient care (53%);
o medical knowledge (48%;)
o organization/prioritization, communication (40%;)
o professionalism (41%); and
o the majority (77%) had MULTIPLE deficiencies.
The most
common contributing factors to residents having difficulty in the study were:
o depression
o anxiety
o personality disorders
Less common contributing factors to residents having difficulty included:
o learning disability
o illness
o substance use disorder
o divorce
In t
his study, the authors noted that actions taken by program directors to address residents
in difficulty included:
o remediation (including repeating a rotation or an entire year)
o disciplinary action
o probation
o dismissal
In t
his study, only 34.5% of program directors retrospectively identified warning signs.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
174

Conclusions:
o The majority of residents in difficulty have deficiencies in multiple competencies.
o Medical knowledge and patient care deficiencies are much easier to remediate.
o Deficiencies in professionalism are common (41%).
o Residents respond poorly to remediation.
o There is a concern that unprofessional behavior in residents is predictive of future
disciplinary action by specialty boards.
3. Lefebvre,
Cedric, Kelly Williamson, Peter Moffett, Angela Cummings, Beth
Gianopulos, Elizabeth Winters, and Mitchell Sokolosky. 2018. “Legal Considerations
in the Remediation and Dismissal of Graduate Medical Trainees.” Journal of Graduate
Medical Education 10,(3): 253–57. https://doi.org/10.4300/jgme-d-17-00813.1
.
Lefebvre et al. reviewed the legal considerations in placing residents in remediation or
dismissing them from the program, and have the following summary points:
o Sponsoring Institutions and their programs must provide residents with due process
in cases of contract non-renewal, non-promotion, suspension, or dismissal.
Adherence to remediation policy, use of consistent remediation language, and
documentation of all phases of remediation are important to optimize outcomes
and limit legal liability when dismissal occurs.
Programs are generally on solid legal ground when they exercise due process for
the remediated resident, when they take actions based on educational standards
and patient safety, and when they only disclose educational records to inquiring
parties in good faith.
Courts have consistently declined to consider the tort of educational malpractice.
4. Papadakis,
Maxine A., Gerald K. Arnold, Linda L. Blank, Eric S. Holmboe, and
Rebecca S. Lipner. 2008. “Performance during Internal Medicine Residency Training
and Subsequent Disciplinary Action by State Licensing Boards.” Annals of Internal
Medicine 148,(11): 869. https://doi.org/10.7326/0003-4819-148-11-200806030-00009
.
Papadakis et al. evaluated the incidence of subsequent disciplinary action by state licensing
boards according to performance during residency and concluded that poor performance on
behavioral and cognitive measures during residency is associated with greater risk for state
licensing board actions against practicing physicians at every point on a performance
continuum. These findings support the ACGME standards for professionalism and cognitive
performance and the development of best practices to remediate these deficiencies.
5. Smith, Jessica, Monica Lypson, Mark Silverberg, Moshe Weizberg, Tiffany Murano,
Michael Lukela, and Sally Santen. 2017 “Defining Uniform Processes for Remediation,
Probation and Termination in Residency Training.” Western Journal of Emergency
Medicine 18,(1): 110–13. https://doi.org/10.5811/westjem.2016.10.31483
.
The authors state that: “It is important that residency programs identify trainees who
progress appropriately, as well as identify residents who fail to achieve educational
milestones as expected so they may be remediated. The process of remediation varies
greatly across training programs, due in part to the lack of standardized definitions for good
standing, remediation, probation and termination.”
The author
s provided standardized definitions for terms used in remediation, probation, and
termination related to residency education as listed below:
©2024 Accreditation Council for Graduate Medical Education (ACGME)
175
Informal Remediation: The first step in the process when warning signs of problems exist but
are not so significant that formal remediation is warranted. This is a critical time to start
documentation of the process to determine if there is an eventual need to escalate to a
formal remediation process. Many programs have developed documentation templates or
standard language, and completed forms or email notifications to the resident are placed in
the resident’s file. Some create confidential notes placed in “shadow files,” which are
destroyed once the remediation process is completed successfully.
It i
s important to engage the program director, CCC, and resident at this stage.
Formal
Remediation: The next step in the management of residents in difficulty. This step is
implemented when the resident fails to correct identified deficiencies during informal
remediation or when the deficiencies are so significant that the step of informal remediation
is skipped.
o Components of formal remediation:
Document the need for formal remediation and inform the resident in writing. It is
important that the resident read and sign a formal document. The document must
also be signed by the program director.
Provide the resident with program and institutional grievance and due process
policies.
Determine the length of time of formal remediation, decided by the program
director and the CCC. Do not leave the date open-ended — there must be a
target date.
Create a correction plan with expected outcomes — there must be specific
targets based on the deficiencies.
Include a time frame for reassessment and the consequences of not meeting the
expected outcome within the time frame.
Place all documentation in the resident’s file.
Notify the graduate medical education (GME) office, including the DIO.
Probat
ion: Probation is initiated when a resident fails to correct deficiencies identified during
formal remediation. The program director and the CCC may place a resident on immediate
probation if major problems occur.
Some p
rograms set a limit of six months to the period of formal remediation. If there is no or
not enough improvement after six months of formal remediation, the resident is then placed
on probation.
Notes
related to probation:
o The period of probation must be definite, not open-ended.
o The program must follow due process, especially if non-renewal or termination is
being considered.
o The same points listed in formal remediation need to be followed: dates, target
outcome, consequences of not meeting the requirements, and documentation.
o The GME office must be involved. Other participants in the probation process include
the program director, the CCC, the department chair, and faculty members assigned
to remediate the resident.
o The legal department must be involved.
o Probation must be disclosed in the final Verification of Graduate Medical Education
Training (VGMET) Form, employment letters, and letters of references.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
176
o If the resident does not meet the requirements outlined in the letter of probation, the
program may choose non-renewal of contract, or termination.
Termi
nation: A resident may be terminated if that resident fails to meet the terms of
probation. In some instances, a resident may be terminated immediately if the problem is
severe enough.
o Those involved in the process of probation must be involved in the termination
process. In addition, if there is a house officer/resident union, a representative of the
union needs to be involved.
o Termination must be disclosed in the final VGMET Form, employment letters, and
letters of references.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
177

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.A. R
esident Evaluation
V.A.2. Final Evaluation
V.A.2.a) T
he program director must provide a final evaluation for each
resident upon completion of the program.
(Core)
V.A.2
.a).(1) The specialty-specific Milestones, and when
applicable, the specialty-specific Case Logs, must be
used as tools to ensure residents are able to engage in
autonomous practice upon completion of the program.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
178

GUIDANCE
As Com
mon Program Requirement V.A.2.a).(1) specifies, the program director must use the
specialty-specific Milestones, and when applicable, the specialty-specific Case Logs as tools to
ensure residents are able to engage in autonomous practice upon completion of the program.
However, the program director should consider a number of other items to make the
determination about a resident’s ability to engage in autonomous practice (e.g., semi-annual
and summative evaluations; recommendations from the Clinical Competency Committee).
Milestones
Milestones evaluation is an educational and formative assessment methodology designed to
help promote improvement in every specialty and subspecialty graduate medical education
(GME) program in the United States. The Milestones were not designed or intended for use by
external entities, such as state medical licensing boards or credentialing entities, to inform or to
make high-stakes decisions. The ACGME is concerned that GME programs may artificially
inflate individual Milestones assessment data if the Milestones are used for high-stakes
decisions. Their value would risk being lost as an honest and valuable assessment tool for
continuous improvement and professional development.
The Milestones are designed only for use in evaluation of residents in the context of their
participation in ACGME-accredited programs. The Milestones provide a framework for the
assessment of the development of the resident in key dimensions of the elements of physician
competence in a specialty. They neither represent the entirety of the dimensions of the six Core
Competency domains, nor are they designed to be relevant in any other context.
The Level 4 milestones are designed as the graduation target but do not represent a graduation
requirement. Making decisions about readiness for graduation is the purview of the residency
program director. (See the Milestones FAQs for further discussion of this issue: “Can a
resident/fellow graduate if he or she does not reach every milestone?”).
NOTE: Program directors are urged to read the following article regarding appropriate use of the
Milestones (located under the Other Resources heading):
• Use of Individual Milestones Data by External Entities for High Stakes Decisions - A
Function for Which they Are not Designed or Intended
Milestones resources
The ACGME provides many resources for residents, faculty members, and
program administration and leadership, and new resources are developed regularly.
Visit the Milestones/Resources section of the ACGME website to review available resources
and tools.
ACGME Case Log System
When applicable, Case Logs must also be used by the program director to determine if
residents are able to engage in independent practice upon completion of their educational
program. The program director should monitor residents’ Case Logs throughout their training to
ensure they are able to meet Case Log minima for their specialty, if applicable, and to achieve
competence in key procedures.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
179

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.A. R
esident Evaluation
V.A.2. Final Evaluation
V.A.2.a) T
he program director must provide a final evaluation for each
resident upon completion of the program.
(Core)
V.A.2
.a).(2) The final evaluation must:
V.A
.2.a).(2).(a) become part of the resident’s permanent record
maintained by the institution, and must be
accessible for review by the resident in
accordance with institutional policy;
(Core)
V.A.2
.a).(2).(b) verify that the resident has demonstrated the
knowledge, skills, and behaviors necessary to
enter autonomous practice; and,
(Core)
V.A
.2.a).(2).(c) be shared with the resident upon completion of
the program.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
180

GUIDANCE
It is important to note that the final evaluation requirement specified in Common Program
Requirement V.A.2.a).(2) is different from the verification of training and education specified in
Common Program Requirement II.A.4.a).(10). Program directors may use one form to meet
both the requirement for final evaluation and verification of training and education, but they must
ensure that the final evaluation includes the specific elements identified below as well as in
Common Program Requirement V.A.2.a).(1). Some of the most common elements that are
missed by programs and are cited by Review Committees when programs use the same form
for verification of training and final evaluation relate to:
• the specific language around readiness for autonomous practice; and,
• review of milestones and, as applicable, Case Log System data.
The Verification of Graduate Medical Education Training (VGMET) Form, which programs
can use or adapt to their needs, was jointly developed by several organizations: the American
Hospital Association (AHA), the National Association Medical Staff Services (NAMSS), the
Organization of Program Director Associations (OPDA), and the ACGME. It is designed to
satisfy national credentialing standards, and to be completed once (and only once) by the
program director, and then copied and re-used in perpetuity.
V.A.2.a).(2).(a) [The final evaluation must:] become part of the resident’s
permanent record maintained by the institution, and must be accessible for
review by the resident in accordance with institutional policy.
This requirement is self-explanatory.
V.A.2.a).(2).(b) [The final evaluation must:] verify that the resident has
demonstrated the knowledge, skills, and behaviors necessary to enter
autonomous practice.
It is important for the program director to affirmatively state in the final evaluation, “Dr. [resident
name] has demonstrated the knowledge, skills, and behaviors necessary to enter autonomous
practice.” It is also desirable to add the specialty or subspecialty, i.e., “…to enter autonomous
practice of [specialty].” This is a frequently missed and cited requirement and therefore, program
directors are strongly encouraged to ensure that this language is included in the final evaluation.
Whil
e Milestones assessments and Case Logs must be used in the determination of an
individual resident’s ability to practice autonomously, the achievement of specific milestones by
an individual resident or the number of procedures performed do not need to be documented in
the final evaluation. See Common Program Requirement V.A.2.a).(1) for additional information.
V.A.2.a).(2).(c) [The final evaluation must:] be shared with the resident upon
completion of the program.
This requirement is self-explanatory.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
181

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.A. Resident Evaluation
V.A.3. A Clinical Competency Committee must be appointed by the program
director.
(Core)
V.A.3.a) At a minimum, the Clinical Competency Committee must
include three members of the program faculty, at least one of
whom is a core faculty member.
(Core)
V.A.3.a).(1) Additional members must be faculty members from
the same program or other programs, or other health
professionals who have extensive contact and
experience with the program’s residents.
(Core)
Background and Intent: The requirements regarding the Clinical Competency
Committee do not preclude or limit a program director’s participation on the Clinical
Competency Committee. The intent is to have flexibility for each program to decide the
best structure for its own circumstances, but a program should consider: Its program
director’s other roles as resident advocate, advisor, and confidante; the impact of the
program director’s presence on the other Clinical Competency Committee members’
discussions and decisions; the size of the program faculty; and other program-relevant
factors. Inclusivity is an important consideration in the appointment of Clinical
Competency Committee members, allowing for diverse participation to ensure fair
evaluation. The program director has final responsibility for resident evaluation and
promotion decisions.
Program faculty may include more than the physician faculty members, such as other
physicians and non-physicians who teach and evaluate the program’s residents.
There may be additional members of the Clinical Competency Committee. Chief
residents who have completed core residency programs in their specialty may be
members of the Clinical Competency Committee.
V.A.3.b) The Clinical Competency Committee must:
V.A.3.b).(1) review all resident evaluations at least semi-annually;
(Core)
V.A.3.b).(2) determine each resident’s progress on achievement of
the specialty-specific Milestones; and,
(Core)
V.A.3.b).(3) meet prior to the residents’ semi-annual evaluations
and advise the program director regarding each
resident’s progress.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
182
GUIDANCE
The membership of the Clinical Competency Committee (CCC) and the roles of the program
director, physician and non-physician faculty members, and chief residents are outlined in the
Background and Intent section preceding these requirements. The requirements are
purposefully stated in general terms to allow programs flexibility to include individuals who are
most appropriate locally, and to structure their meetings according to their specific needs. Note
that the role of the chief resident on the CCC is clarified. Chief residents who have completed
specialty or core residency programs can be members of the CCC. For example, someone who
has completed an internal medicine or pediatrics residency program and is then appointed as
chief resident would qualify for membership. However, chief residents in surgery are in their fifth
year of the educational program and are residents, and therefore cannot serve on the CCC.
Program coordinators are essential in the CCC process through their involvement with many, if
not all, aspects of the program, and their knowledge of the residents. Program coordinators may
attend CCC meetings in an administrative role at the discretion of the program director.
However, the program coordinator cannot be a CCC member, or make judgments in or after the
meeting regarding resident performance. Program coordinators should provide assessment and
feedback through the program’s assessment system, such as by participating in multisource
assessment instruments.
Accreditation Data System (ADS) screenshot: Clinical Comptency Committee
membership
All programs are expected to provide the membership of the CCC as part of a new application
or during the ADS Annual Update. This question is located on the Program Tab > Overall
Evaluation Methods – CCC Membership.
V.A.3.b).(1): If there is a disagreement in assessment between the program director and the
CCC, note V.A.2. and V.A.2.a) The program director must provide a final evaluation for
each resident upon completion of the program.
(Core)
Common Program Requirements V.A.3.b).(1) - (3) articulate three critical responsibilities of the
CCC. The CCC must review all resident evaluations at least semi-annually. Based on the size
and structure of the program, this expectation may be insufficient to assess all residents and
some programs may have CCCs that meet quarterly or monthly. The CCC is also responsible
for reviewing each resident’s progress on the specialty-specific Milestones. Finally, the CCC
must meet prior to the residents’ semi-annual evaluations and advise the program director about
each resident’s progress.
Resources
Online resources related to CCCs and the Milestones can be found at
https://www.acgme.org/milestones/resources/.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
183

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.B. Faculty
Evaluation
V.B.1. The program must have a process to evaluate each faculty
member’s performance as it relates to the educational program at
least annually.
(Core)
Background and Intent: The program director is responsible for the educational program and
all educators While the term “faculty” may be applied to physicians within a given institution
for other reasons, it is applied to residency program faculty members only through approval
by a program director. The development of the faculty improves the education, clinical, and
research aspects of a program. Faculty members have a strong commitment to the resident
and desire to provide optimal education and work opportunities. Faculty members must be
provided feedback on their contribution to the mission of the program. All faculty members
who interact with residents desire feedback on their education, clinical care, and research. If
a faculty member does not interact with residents, feedback is not required. With regard to
the diverse operating environments and configurations, the residency program director may
need to work with others to determine the effectiveness of the program’s faculty
performance with regard to their role in the educational program. All teaching faculty
members should have their educational efforts evaluated by the residents in a confidential
and anonymous manner. Other aspects for the feedback may include research or clinical
productivity, review of patient outcomes, or peer review of scholarly activity. The process
should reflect the local environment and identify the necessary information. The feedback
from the various sources should be should be summarized and provided to the faculty on an
annual basis by a member of the leadership team of the program.
V.B.1
.a) This evaluation must include a review of the faculty member’s
clinical teaching abilities, engagement with the educational
program, participation in faculty development related to their
skills as an educator, clinical performance, professionalism,
and scholarly activities.
(Core)
V.B.1
.b) This evaluation must include written, anonymous, and
confidential evaluations by the residents.
(Core)
V.B.2
. Faculty members must receive feedback on their evaluations at least
annually.
(Core)
V.B.3
. Results of the faculty educational evaluations should be
incorporated into program-wide faculty development plans.
(Core)
Background and Intent: The quality of the faculty’s teaching and clinical care is a
determinant of the quality of the program and the quality of the residents’ future clinical care.
Therefore, the program has the responsibility to evaluate and improve the program faculty
members’ teaching, scholarship, professionalism, and quality care. This section mandates
annual review of the program’s faculty members for this purpose, and can be used as input
into the Annual Program Evaluation.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
184
GUIDANCE
The section of the Common Program Requirements addressing faculty evaluation has several
components:
1. who to evaluate;
2. what to evaluate − clinical teaching abilities, engagement with the educational program,
participation in faculty development related to their skills as an educator, clinical
performance, professionalism and scholarly activities;
3. when to evaluate − faculty members’ feedback on their evaluations at least annually; and
4. how to use evaluations − results of faculty educational evaluations incorporated into
faculty development plans
Who to evaluate
As stated in the Background and Intent, all teaching faculty members who have significant
interactions with the residents must receive feedback.
What to evaluate
Faculty members should be evaluated based on their role in resident education, including
clinical care, teaching, and research, in aspects such as clinical productivity, review of patient
outcomes, or peer review of scholarly activity. Sometimes, the program director may need to
work with others to determine the effectiveness of faculty members’ performance regarding their
role in the educational program. The process should reflect the local environment and identify
the necessary information.
As not
ed in the Background and Intent, assessment of faculty members is an important part of
improving the teaching program. Feedback is important to help individual faculty members
measure and increase their contribution to the mission of the program and improve their
individual effectiveness as teachers. It is suggested that assessment include research and
scholarly activity, clinical work, and educational activities. The specific requirement for written
and confidential evaluations of faculty members is intended to collect the most honest feedback
from the residents, which requires minimizing any possibility for fear of retaliation or intimidation
of the residents resulting from comments made.
V.B.1.b) This evaluation must include written, anonymous, and confidential
evaluations by the residents.
Programs with a small number of residents often struggle to maintain the confidentiality of a
resident’s evaluation. For a confidential evaluation, the reviewer is not known by the individual
being evaluated, but the identity of the evaluator might be known by someone such as the
program director or departmental chair. For an anonymous evaluation, the evaluator is not
known by anyone, offering a higher level of security. Frequently, feedback from multiple
anonymous evaluations is aggregated so that it is impossible to guess the individual source.
The advantage
of a confidential evaluation is that someone can respond if needed to an
egregious situation if it is reported or that a residency program director or departmental chair
can place the information in better context. Confidential evaluations only work if the residents
trust their identity will be kept secret, which requires they must have a high degree of trust in the
individual who knows their identity. The trusted individual may be the program coordinator who
is collecting the evaluations or the program director or department chair who oversees the
faculty member. However, these individuals may be intimidating to a resident because of their
supervisory relationship. In this instance, the trusted individual must be someone else,
©2024 Accreditation Council for Graduate Medical Education (ACGME)
185

particularly when the resident is evaluating the program director and the department chair.
Another scenario has the trusted individual being someone outside of the program, such as the
designated institutional official (DIO) or an individual who reports to a different department.
The advantage
of an anonymous evaluation is that it is the most reassuring to the resident.
Anonymous evaluations may be accomplished by collecting them via a system that does not
identify an individual resident. Because it might be possible for faculty members to guess the
identity by timing when the evaluation appears, the individual comments might be collected
throughout the year and batched feedback might be best given at the end of the year or even
over two years for very small programs. Another option is to batch resident feedback across
multiple programs with which the faculty member is associated.
Confi
dentiality is at risk when the written evaluation contains details that might identify a specific
patient, case, or resident interaction that the faculty member can recall and attribute to the
specific individual resident.
Confi
dential faculty evaluations are a critical piece of information to help improve the program,
but they are a special challenge in small programs. Some of the strategies above may help to
collect that information while preserving confidentiality.
The ACG
ME monitors compliance with Common Program Requirements V.B.1.- 3. in various
ways, including:
• questions answered by program leadership as part of an application or during the ADS
Annual Update;
• documents submitted by programs as part of an application or site visit (e.g., sample
evaluation forms);
• questions answered by residents and faculty members as part of the annual
Resident/Fellow and Faculty Surveys; and
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
The Resident
/Fellow and Faculty Surveys include several questions that address the
requirements in section V.B.1.-3. The ACGME has prepared two documents, a “Resident/Fellow
Survey−Common Program Requirements Crosswalk” and a “Faculty Survey−Common Program
Requirements Crosswalk,” to provide additional information for programs on the key areas
addressed by the survey questions and how they map to the ACGME Common Program
Requirements. These documents can be found at
https://www.acgme.org/data-systems-
technical-support/resident-fellow-and-faculty-surveys.
Many i
nstitutions have “home-grown” versions of faculty evaluation forms. In addition,
departments may have annual evaluation forms that address clinical performance, role in
education, and scholarship. Some examples of these efforts are included below:
1. Kassis,
Karyn, Rebecca Wallihan, Larry Hurtubise, Sara Goode, Margaret Chase, and
John Mahan. 2017. “Milestone-Based Tool for Learner Evaluation of Faculty Clinical
Teaching.” MedEdPORTAL Publications 13.
https://doi.org/10.15766/mep_2374-
8265.10626.
Created a 10-question evaluation tool to assess clinical teaching skills with descriptive
Milestones behavior anchors using a combination of the Stanford Faculty Development
Clinical Teaching Model and annual ACGME Resident/Fellow Survey questions.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
186

Conclusion: The tool provided faculty members with more meaningful teaching evaluations
and feedback.
Domains:
• Milestone 1: Establishes positive learning domain
• Milestone 2: Maintains control of educational session
• Milestone 3: Establishes learning goals
• Milestone 4: Promotes understanding and retention of knowledge and skills
• Milestone 5: Provides formative feedback
• Milestone 6: Promotes clinical reasoning
• Milestone 7: Promotes evidence-based medicine
• Milestone 8: Promotes self-directed learning in learners
• Milestone 9: Balances supervision and autonomy
• Milestone 10: Displays professionalism
2. Mintz, Marcy, Danielle A. Southern, William A. Ghali, and Irene W. Y. Ma. 2015.
“Validation of the 25-Item Stanford Faculty Development Program Tool on Clinical
Teaching Effectiveness.” Teaching and Learning in Medicine 27(2): 174–81.
https://doi.org/10.1080/10401334.2015.1011645
.
Domains:
• Learning climate
• Control of session
• Communication of goals
• Promotes understanding and retention
• Evaluation
• Feedback
Promotes self-directed learning
3. Williams, Brent C., Debra K. Litzelman, Stewart F. Babbott, Robert M. Lubitz, and Tim
P. Hofer. 2002. “Validation of a Global Measure of Facultyʼs Clinical Teaching
Performance.” Academic Medicine 77(2): 177–80.
https://doi.org/10.1097/00001888-
200202000-00020.
Created a Global Rating Scale (GRS) – a single-item, five-point global measure of faculty
members’ clinical teaching performance previously known to be reliable.
Evaluation completed by 98 senior medical residents from four academic institutions; also
completed the 26-item Stanford Faculty Development questionnaire for 10 faculty members
with whom they had teaching contact during residency.
The GRS correlated highly with measures of seven specific aspects of teaching
effectiveness. The scale is reportedly simple to use, readily administered as part of an
incentive or reward program, or for review in promotion decisions.
V.B.2.-V.B.3 Faculty members must receive feedback on their evaluations at least
annually; results of faculty educational evaluations should be incorporated into
program-wide faculty development plans.
The feedback should include strengths and opportunities for improvement, and be considered in
planning for faculty development sessions and tracked as part of the Annual Program
Evaluation. For example, if residents’ evaluations of faculty members consistently show that
faculty members’ evaluations are not constructive and do not provide information to help the
residents improve, there might be a need to provide faculty development on resident evaluation.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
187

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.C. P
rogram Evaluation and Improvement
V.C.1. The program director must appoint the Program Evaluation
Committee to conduct and document the Annual Program
Evaluation as part of the program’s continuous improvement
process.
V.C.1
.a) The Program Evaluation Committee must be composed of at
least two program faculty members, at least one of whom is a
core faculty member, and at least one resident.
(Core)
V.C.1
.b) Program Evaluation Committee responsibilities must include:
V.C.1.b).(1) review of the program’s self-determined goals and
progress toward meeting them;
(Core)
V.C.1
.b).(2) guiding ongoing program improvement, including
development of new goals, based upon outcomes;
and,
(Core)
V.C.1
.b).(3) review of the current operating environment to identify
strengths, challenges, opportunities, and threats as
related to the program’s mission and aims.
(Core)
Background and Intent: To achieve its mission and educate and train quality
physicians, a program must evaluate its performance and plan for improvement in the
Annual Program Evaluation. Performance of residents and faculty members is a
reflection of program quality, and can use metrics that reflect the goals that a program
has set for itself. The Program Evaluation Committee utilizes outcome parameters and
other data to assess the program’s progress toward achievement of its goals and aims.
The Program Evaluation Committee advises the program director through program
oversight.
V.C.1
.c) The Program Evaluation Committee should consider the
outcomes from prior Annual Program Evaluation(s),
aggregate resident and faculty written evaluations of the
program, and other relevant data in its assessment of the
program.
(Core)
Background and Intent: Other data to be considered for assessment include:
• Curriculum
• ACGME letters of notification, including citations, Areas for Improvement, and
comments
• Quality and safety of patient care
• Aggregate resident and faculty well-being; recruitment and retention; workforce
diversity, including graduate medical education staff and other relevant
©2024 Accreditation Council for Graduate Medical Education (ACGME)
188

academic community members; engagement in quality improvement and patient
safety; and scholarly activity
• ACGME Resident and Faculty Survey results
• Aggregate resident Milestones evaluations, and achievement on in-training
examinations (where applicable), board pass and certification rates, and
graduate performance.
1. Aggregate faculty evaluation and professional development
V.C.1
.d) The Program Evaluation Committee must evaluate the
program’s mission and aims, strengths, areas for
improvement, and threats.
(Core)
V.C.1
.e) The Annual Program Evaluation, including the action plan,
must be distributed to and discussed with the residents and
the members of the teaching faculty, and be submitted to the
DIO.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
189
GUIDANCE
As the Background and Intent outlines, programs must evaluate their performance and plan for
improvement in the Annual Program Evaluation. Common Program Requirement V.C.1.
requires that each program must have a Program Evaluation Committee (PEC) appointed by
the program director to advise the program director through program oversight and conduct and
document the Annual Program Evaluation.
V.C.1.a) Composition of the PEC
The PEC must include at least two program faculty members, at least one of whom is a core
faculty member, and at least one resident. Members of the PEC should know the program well
and be invested in program improvement and success. Resident members are important
because they “live and work” within the context of the program.
Accreditation Data System (ADS) screenshot: composition of the PEC
Programs must provide the membership of the PEC in ADS when submitting a new application
or as part of the ADS Annual Update.
V.C.1.b) PEC responsibilities
The PEC has three key responsibilities as outlined in Common Program Requirements
V.C.1.b).(1)-(3):
1. review of the program’s goals and progress toward meeting them;
2. guiding ongoing program improvement, including development of new goals, based
upon outcomes; and
3. review of the current operating environment to identify strengths, challenges,
opportunities, and threats as related to the program’s mission and aims.
V.C.1.c) Data to be considered for the Annual Program Evaluation
This requirement outlines three key elements the PEC must consider for the Annual Program
evaluation:
1. outcomes from prior Annual Program Evaluation(s);
2. aggregate resident and faculty written evaluations of the program; and
3. other relevant data.
The Back
ground and Intent provides further specification as to other relevant data the PEC can
consider:
• curriculum
• ACGME letters of notification, including citations, Areas for Improvement, and
Comments;
• quality and safety of patient care;
• aggregate resident and faculty well-being; recruitment and retention; and
• workforce diversity, including graduate medical education staff and other relevant
academic community members;
• engagement in quality improvement and patient safety;
©2024 Accreditation Council for Graduate Medical Education (ACGME)
190
• scholarly activity;
• ACGME Resident and Faculty Survey results;
• aggregate resident Milestones evaluations, and achievement on in-training examinations
(where applicable), board pass and certification rates, and graduate performance; and
• aggregate faculty evaluation and professional development.
This r
equirement permits flexibility to identify data and indicators that are feasible to measure
and relevant to an individual program’s aims.
Some Sponsoring Institutions have standardized
elements of Annual Program Evaluations and programs should consult with their designated
institutional official (DIO).
V.C.1.e) Dissemination of the Annual Program Evaluation and submission to the
DIO
While it is important that programs conduct and document an Annual Program Evaluation, this
requirement emphasizes the need to review and discuss the Annual Program Evaluation with
faculty members and residents and also share it with the (DIO. The Sponsoring Institution’s DIO
and Graduate Medical Education Committee (GMEC) are responsible for overseeing Annual
Program Evaluations. The DIO and GMEC may expect programs to submit Annual Program
Evaluation information in a specific format. The DIO should be contacted with any questions
about how to submit an annual review and action plan.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
191

Suggested template for internal program use in the Annual Program Evaluation. Note
that this is a sample template and the ACGME does not require its use.
SAM
PLE Template – Annual Program Evaluation
(For Internal PROGRAM Use Only)
Program:
Date:
Academic Year:
Progr
am Evaluation Committee Membership:
Faculty Members:
1. _____________________________
2. _____________________________
3. _____________________________
Resi
dents:
1. _____________________________
2. _____________________________
Resident Complement
Year 1
Year 2
Year 3
Year 4
Year 5
Year 6
Year 7
Positions
Approved
Current
Complement
Accred
itation Status of the Program
□ Continued Accreditation
□ Initial Accreditation
□ Continued Accreditation with Warning
□ Initial Accreditation with Warning
□ Probationary Accreditation
□ Continued Accreditation without Outcomes
Curr
ent Program Citations
Insert Text from ACGME
Letter of Notification (LON)
Current Program Response to Citation
1.
2.
3.
Curr
ent Areas for Improvement (AFIs)
Insert Text from ACGME LON
Program Actions to Address
Areas for Improvement (AFIs)
1.
2.
3.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
192

Program Aims
Aim(s)
Met (M)/Unmet (U)
Plans f
or Unmet Goals
1. ___________________________________________________________________
2. ___________________________________________________________________
3. ___________________________________________________________________
Str
engths of the Program
1. ___________________________________________________________________
2. ___________________________________________________________________
3. ___________________________________________________________________
Challenges/Threats to the Program
1. ___________________________________________________________________
2. ___________________________________________________________________
3. ___________________________________________________________________
Opportunities for the Program
1. ___________________________________________________________________
2. ___________________________________________________________________
3. ___________________________________________________________________
Progr
am Curriculum
Curricular Element
Action: Modify (M),
Add (A) or Delete (D)
Steps Taken
Timeline for
Completion
Quali
ty Improvement (QI) and Patient Safety (PS)
QI/PS Activity
Active Role
Faculty (F) or
Resident
Has QI/PS
Improved in the
Past Year?
(Yes/No)
Describe
Improvement,
Including Efforts to
Include Faculty
Member(s) and
Residents
Describe QI/PS
Activities that
Can be Added or
Improved
©2024 Accreditation Council for Graduate Medical Education (ACGME)
193

Well-Being and Diversity
Activity
Successes
Needs Improvement
Well-being
Diversity
Recruitment
Retention
Scholar
ship
Resident/Faculty Scholarly
Activities
(append lists here)
If applicable, list efforts to increase scholarship
ACG
ME Annual Resident Survey
Areas with Improvement Areas with Deterioration
Plans to Address Areas of
Deterioration if Applicable
ACG
ME Annual Faculty Survey
Areas with Improvement Areas with Deterioration
Plans to Address Areas of
Deterioration if applicable
Wri
tten Evaluations of the Program
Who provides written evaluations of the program?
Residents in this program
Other hospital/clinic/facility personnel
Residents/fellows in other programs
Faculty members in other programs
Faculty members in this program
Areas Identified for Program Improvement
Plans for Program Improvement/Target Date
©2024 Accreditation Council for Graduate Medical Education (ACGME)
194

Aggregate Resident Achievement of Milestones
Exceeded National Means Below National Means
Plans to Improve
Milestones Achievement
Aggrega
te Resident Performance on In-Training Examinations (if Applicable)
Performance of Cohort this
Year Compared to Prior Year
Subject Areas where Cohort
Fell Short of Program
Expectations
Plans to Improve
Performance on the
In-Training Examination
Aggrega
te Performance of Residents and Graduates on Board Certification Examinations
in the Specialty/Subspecialty Program
Number Eligible to Take
Number Eligible Who Took
the Written Examination
How Many of Those Who
Took the Exam Passed?
If appli
cable, how does the program plan to improve resident/graduate performance on
the examinations in the board certification process over the next year?
_________________________________________________________________
Perf
ormance of Program Graduates
In what ways does the program monitor the performance of program graduates?
Surveys of the graduates
Surveys of the partners of the graduates
Surveys of the employers of the graduates
Surveys of the practice sites (hospitals, clinics, etc.) of the graduates
Monitoring of the continuing board certification of the graduates
Monitoring of state licensing board actions against graduates
Monitoring of medicolegal actions against graduates
Program does not monitor program graduates’ performance
Areas for Improvement for Performance of
Graduates
Plans to Address Areas Identified
as Needing Improvement
©2024 Accreditation Council for Graduate Medical Education (ACGME)
195
Faculty Evaluation
By whom are the faculty members in this program evaluated (for their contributions to the
educational program)?
Medical students
Residents in this program
Residents in other programs
Peer faculty members in this program
Peer faculty members in other programs
Areas for Improvement Identified for Faculty
Member Contributions to the Program
Plans to Address Areas Identified
as Needing Improvement
Faculty
Development Activities
List Faculty Development
Activities Available in the
Past Year
Percent Faculty Participation
If Applicable, How Does the
Program Plan to Increase
Participation in Faculty
Development Activities?
©2024 Accreditation Council for Graduate Medical Education (ACGME)
196

COMMON PROGRAM REQUIREMENTS
V.C.2. The program must complete a Self-Study and submit it to the DIO.
(Core)
Background and Intent: Outcomes of the documented Annual Program Evaluation can
be integrated into the Accreditation Self-Study process. The Self-Study is an objective,
comprehensive evaluation of the residency program, with the aim of improving it.
Underlying the Accreditation Self-Study is this longitudinal evaluation of the program
and its learning environment, facilitated through sequential Annual Program
Evaluations that focus on the required components, with an emphasis on program
strengths and self-identified areas for improvement. Details regarding the timing and
expectations for the Accreditation Self-Study are provided in the ACGME Manual of
Policies and Procedures. Additionally, a description of the
Self-Study process is
available on the ACGME website.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
197

GUIDANCE
NOTE: The ACGME Program Self-Study was unlinked from the former 10-Year Accreditation
Site Visit. Click here for more information regarding the Program Self-Study.
Sponsor
ing Institution Self-Studies and 10-year Accreditation Site Visits are proceeding
according to the Institutional Review Committee’s announced plan.
Self-Study Description
The ACGME Program Self-Study was established as a key component of the ACGME’s current
accreditation model. With the goal of conducting an objective and comprehensive review of the
program, the Self-Study is a tool for program self-reflection and strategic planning that uses the
Annual Program Evaluation as a foundation on which to build the in-depth, multi-year program
evaluation.
Two conc
epts are fundamental in the development of the Self-Study:
1. determination of the program’s aims and mission; and
2. critical assessment of the institutional, local, regional, and even national environment
(context) in which the program operates.
These c
oncepts lead to a thoughtful analysis of program strengths, weaknesses, opportunities,
and threats that will allow a program to distinguish itself from other programs in the specialty
(e.g., highlighting differences between community and urban programs). Ultimately, the goal of
the Self-Study is to provide a platform for a forward-thinking and systematic approach to making
program improvements.
Progr
ams are encouraged to include a broad array of participants in the Self-Study process,
including program leaders, residents, faculty members, and other stakeholders, such as
program graduates, institutional and quality improvement personnel, leaders from related
programs, or nursing and other health care personnel who interact closely with the residents in
the program.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
198

COMMON PROGRAM REQUIREMENTS
V. Evaluation
V.C.
Program Evaluation and Improvement
V.C.3. One goal of ACGME-accredited education is to educate physicians who
seek and achieve board certification. One measure of the effectiveness of
the educational program is the ultimate pass rate.
The progra
m director should encourage all eligible program graduates to
take the certifying examination offered by the applicable American Board of
Medical Specialties (ABMS) member board or American Osteopathic
Association (AOA) certifying board. [If certification in the specialty is not
offered by the ABMS and/or the AOA, V.C.3.a)-V.C.3.f) will be omitted.]
V.C.3
.a) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) an annual written exam, in the preceding
three years, the program’s aggregate pass rate of those taking the
examination for the first time must be higher than the bottom fifth
percentile of programs in that specialty.
(Outcome)
V.C.3
.b) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) a biennial written exam, in the preceding six
years, the program’s aggregate pass rate of those taking the
examination for the first time must be higher than the bottom fifth
percentile of programs in that specialty.
(Outcome)
V.C.3
.c) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) an annual oral exam, in the preceding three
years, the program’s aggregate pass rate of those taking the
examination for the first time must be higher than the bottom fifth
percentile of programs in that specialty.
(Outcome)
V.C.3
.d) For specialties in which the ABMS member board and/or AOA
certifying board offer(s) a biennial oral exam, in the preceding six
years, the program’s aggregate pass rate of those taking the
examination for the first time must be higher than the bottom fifth
percentile of programs in that specialty.
(Outcome)
V.C.3
.e) For each of the exams referenced in V.C.3.a)-d), any program whose
graduates over the time period specified in the requirement have
achieved an 80 percent pass rate will have met this requirement, no
matter the percentile rank of the program for pass rate in that
specialty.
(Outcome)
Background and Intent: Setting a single standard for pass rate that works across
specialties is not supportable based on the heterogeneity of the psychometrics of
different examinations. By using a percentile rank, the performance of the lower five
©2024 Accreditation Council for Graduate Medical Education (ACGME)
199

percent (fifth percentile) of programs can be identified and set on a path to curricular
and test preparation reform.
There are specialties where there is a very high board pass rate that could leave
successful programs in the bottom five percent (fifth percentile) despite admirable
performance. These high-performing programs should not be cited, and V.C.3.e) is
designed to address this.
V.C.3
.f) Programs must report, in ADS, board certification status annually
for the cohort of board-eligible residents that graduated seven years
earlier.
(Core)
Background and Intent: It is essential that residency programs demonstrate knowledge
and skill transfer to their residents. One measure of that is the qualifying or initial
certification exam pass rate. Another important parameter of the success of the
program is the ultimate board certification rate of its graduates. Graduates are eligible
for up to seven years from residency graduation for initial certification. The ACGME
will calculate a rolling three-year average of the ultimate board certification rate at
seven years post-graduation, and the Review Committees will monitor it.
The R
eview Committees will track the rolling seven-year certification rate as an
indicator of program quality. Programs are encouraged to monitor their graduates’
performance on board certification examinations.
In the future, the ACGME may establish parameters related to ultimate board
certification rates.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
200

GUIDANCE
V.C.3. Program Aggregate Board Pass Rate
Board pass rate is one outcome that can demonstrate how well a program prepares its
graduates for independent practice. Review Committees consider variability from year to year in
a program’s board pass rate during program review (especially in small programs). While one
resident failing the board exam(s) in a small program may have a relatively larger negative
impact on the pass rate, the opposite is also true; one resident passing the board exam(s) will
also have a greater positive impact and may provide the opportunity for program improvement
to occur more easily.
V.C.3.a) Annual written board examination pass rate
In specialties that offer an annual written board examination, the three-year rolling
average for first-time takers passing the written board examination will be calculated for
each program and ranked against other programs in the specialty. Those programs
above the fifth percentile in that ranking will not be cited by the Review Committee for
failure to meet the required standard for this program outcome measure.
V.C.3.b) Biennial written board examination pass rate
In specialties that offer a written board examination only on a biennial basis, the six-year
rolling average for first-time takers passing the written board examination will be
calculated for each program and ranked against other programs in the specialty. Those
programs above the fifth percentile in that ranking will not be cited by the Review
Committee for failure to meet the required standard for this program outcome measure.
V.C.3.c) Annual Oral Board Examination Pass Rate
In specialties that offer an annual oral board examination, the three-year rolling average
for first-time takers passing the oral board examination will be calculated for each
program and ranked against other programs in the specialty. Those programs above the
fifth percentile in that ranking will not be cited by the Review Committee for failure to
meet the required standard for this program outcome measure.
V.C.3.d) Biennial oral board examination pass rate
In specialties that offer an oral board examination only on a biennial basis, the six-year
rolling average for first-time takers passing the oral board examination will be calculated
for each program and ranked against other programs in the specialty. Those programs
above the fifth percentile in that ranking will not be cited by the Review Committee for
failure to meet the required standard for this program outcome measure.
V.C.3.e) 80 percent pass rate
Only programs meeting both of the following conditions will receive a citation for this
requirement:
1. the p
rogram must be in the lowest five percent of all programs in the specialty for board
pass rate; and,
2. the program must have a board pass rate below 80 percent.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
201
In other words, if there are 100 programs in a specialty, approximately five programs could
receive that citation, but only if their individual board pass rate for graduates is below 80
percent.
The board pas
s rate for first-time takers will count those who pass in the numerator and those
who are taking the exam for the first time in the denominator. Residency graduates who do not
take the exam, or those who are taking it for the second time or more, do not count in the
denominator. A resident who delays taking the examination will be counted in the year that the
resident takes the exam.
The board pas
s rate for each program is reported to the ACGME directly from the ABMS
member board and the AOA board in the specialty. No names or other individual identifiers are
reported to the ACGME.
If board pass rates are an area of concern for a program, programs are strongly encouraged to
provide the Review Committee with an update on their efforts to improve this metric in the Major
Changes section of the Accreditation Data System (ADS) during the ADS Annual update. The
following list identifies strategies which programs may use to investigate and address concerns
related to board pass rates:
1. The program may evaluate its didactic curriculum to identify weaknesses and make
efforts to improve.
2. The annual in-training examination results can be helpful in identifying content area(s)
where residents did not perform well. In addition, the in-training examination helps
identify those residents who are underperforming in comparison to their peers.
3. A structured certifying board examination review can be implemented, addressing
content specifications of the specialty board.
4. Some residents may benefit from a more structured plan outlined in an individualized
learning plan (see Common Program Requirement V.A.1.d).(2)).
5. The Program Evaluation Committee should include board certification data and in-
training examination performance as part of the Annual Program Review. This review
could determine whether program changes such as changes in the didactic curriculum
and the establishment of conferences to address curricular weaknesses might be
needed.
V.C.3.f) Ultimate Board Pass Rate
The ultimate board pass rate of a program’s graduates is an important program outcome in
addition to the rolling average first-time pass rate noted in Common Program Requirements
V.C.3.a)-e). Neither should be considered in isolation. Note that most member boards of the
ABMS and AOA certifying Boards allow up to seven years for a candidate to achieve board
certification.
Whil
e the most recent three-year rolling average board pass rate may best reflect the
preparation of the most recent graduates, the ultimate certification rates likely reflect the
ultimate goal of the program: to produce graduates who can practice independently and achieve
board certification. This requirement is intended to allow the ACGME to gather data on this
outcome and determine its best use. The Program Evaluation Committee may also find this
information valuable in assessing the program aims and goals. A screenshot of the summary
data the ACGME provides to programs on ultimate resident board certification status can be
found below.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
202
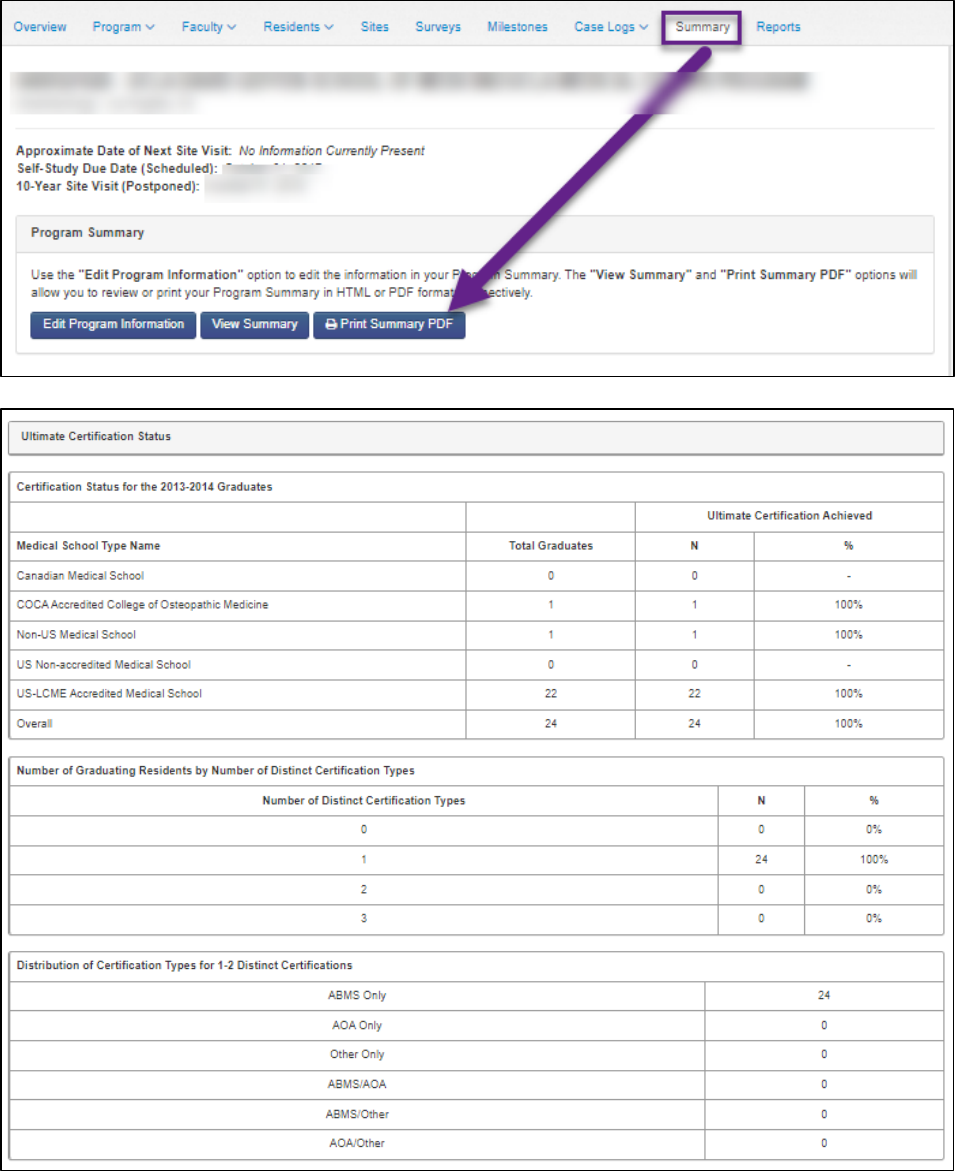
The requir
ement does not specify a minimum for the ultimate certification rate, and programs
will not currently be cited based on the requirement unless they fail to confirm the data provided
by the ABMS and AOA and populated in ADS for their residents on a yearly basis. Programs
©2024 Accreditation Council for Graduate Medical Education (ACGME)
203

cannot edit the graduate list, but they can edit the certification if incorrect, add a certification if it
is not displayed, or confirm that the program was not accredited or there were no graduates for
the specific reporting year. Data for the current reporting year can be edited as part of the
Annual ADS Update or through the end of the academic year. Once the rollover to a new
academic year occurs, the graduate data will be “View Only” and no edits can be made.
Accreditation Data System (ADS) screenshot: The screenshot below shows the
resident board certification data imported from the ABMS and AOA and which
programs must verify during the ADS Annual Update.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
204

COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
Residenc
y education must occur in the context of a learning and working
environment that emphasizes the following principles:
• Excell
ence in the safety and quality of care rendered to patients by fellows
today
• Excell
ence in the safety and quality of care rendered to patients by today’s
fellows in their future practice
• Excellence in professionalism
• Appreci
ation for the privilege of providing care for patients
• Comm
itment to the well-being of the students, residents, fellows, faculty
members, and all members of the health care team
VI.A. Patient Safety, Quality Improvement, Supervision, and Accountability
VI.A
.1. Patient Safety and Quality Improvement
VI.A.1.a) Patient Safety
VI.A
.1.a).(1) Culture of Safety
A cult
ure of safety requires continuous identification
of vulnerabilities and a willingness to transparently
deal with them. An effective organization has formal
mechanisms to assess the knowledge, skills, and
attitudes of its personnel toward safety in order to
identify areas for improvement.
VI.A
.1.a).(1).(a) The program, its faculty, residents, and fellows
must actively participate in patient safety
systems and contribute to a culture of safety.
(Core)
VI.A
.1.a).(2) Patient Safety Events
Report
ing, investigation, and follow-up of safety
events, near misses, and unsafe conditions are pivotal
mechanisms for improving patient safety, and are
essential for the success of any patient safety
program. Feedback and experiential learning are
essential to developing true competence in the ability
to identify causes and institute sustainable systems-
©2024 Accreditation Council for Graduate Medical Education (ACGME)
205

based changes to ameliorate patient safety
vulnerabilities.
VI.A
.1.a).(2).(a) Residents, fellows, faculty members, and other
clinical staff members must:
VI.A
.1.a).(2).(a).(i) know their responsibilities in reporting
patient safety events and unsafe
conditions at the clinical site, including
how to report such events; and,
(Core)
VI.A.1.a).(2).(a).(ii) be provided with summary information
of their institution’s patient safety
reports
. (Core)
*VI.
A.1.a).(2).(b) Residents must participate as team members in
real and/or simulated interprofessional clinical
patient safety and quality improvement
activities, such as root cause analyses or other
activities that include analysis, as well as
formulation and implementation of actions.
(Core)
VI.A.1.a).(3) Quality Metrics
Access to da
ta is essential to prioritizing activities for
care improvement and evaluating success of
improvement efforts.
VI.A
.1.a).(3).(a) Residents and faculty members must receive
data on quality metrics and benchmarks related
to their patient populations.
(Core)
[The Review Committee may further specify]
©2024 Accreditation Council for Graduate Medical Education (ACGME)
206

GUIDANCE
A number of studies prove why it so important to teach residents and fellows safe patient care
and quality improvement. The examples provided below demonstrate what residents and
fellows learn during their education and training stays with them and affects their practice for
many years to come: the 32-year-old fellow today has the potential to be practicing beyond
2054.
1. Asch,
David A. 2009. “Evaluating Obstetrical Residency Programs Using Patient
Outcomes.” JAMA 302(12): 1277. https://doi.org/10.1001/jama.2009.1356
.
Asch et al. studied 4,906,169 deliveries by 4,124 physicians from 107 US obstetrics and
gynecology residency programs. The programs were ranked based on FLEX, NBME Parts I,
II, III, and USMLE Steps 1, 2, 3 scores. The study found that women treated by obstetricians
in the bottom quintile of programs had one-third higher complication rates than those from
the top quintile, and that the effect was durable through 15-17 years after residency.
2. Chen, C
andice, Stephen Petterson, Robert Phillips, Andrew Bazemore, and Fitzhugh
Mullan. 2014. “Spending Patterns in Region of Residency Training and Subsequent
Expenditures for Care Provided by Practicing Physicians for Medicare Beneficiaries.”
JAMA 312(22): 2385. https://doi.org/10.1001/jama.2014.15973
.
Chen et al evaluated spending patterns in regions of residency education and training and
graduates’ subsequent expenditures in practice based on multilevel, multivariable analysis
of 2011 Medicare claims data from family medicine and internal medicine residents
completing residency between 1992 and 2010. The Hospital Referral Regions (HRR) were
classified based on expenditures as low-, average-, and high-spending. The table below
documents that spending levels during residency were associated with the same pattern of
expenditures for subsequent care provided by graduates.
3. Sirovich, Brenda E., Rebecca S. Lipner, Mary Johnston, and Eric S. Holmboe.
2014. “The Association between Residency Training and Internists’ Ability to
Practice Conservatively.” JAMA Internal Medicine 174(10): 1640.
https://doi.org/10.1001/jamainternmed.2014.3337.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
207

Sirovich et al. evaluated the association between residency education and training and
internists’ ability to practice conservatively following graduation, assessing the responses of
6,639 first-time takers of the American Board of Internal Medicine certifying exam (357
programs). They divided the management options according to Appropriately Conservative
Management (ACM) and Appropriately Aggressive Management (AAM) subscales. They
defined the correct response as the least or most aggressive management strategy, and
found that regardless of overall medical knowledge, internists trained in HRRs (Hospital
Referral Regions) with lower-intensity medical practice were more likely to recognize when
conservative management was appropriate and, more importantly, were capable of
choosing an aggressive approach when indicated.
Additional references
• Chan, David K., Thomas H. Gallagher, Richard Reznick, and Wendy Levinson. 2005.
“How Surgeons Disclose Medical Errors to Patients: A Study Using Standardized
Patients.” Surgery 138(5): 851–58. https://doi.org/10.1016/j.surg.2005.04.015
.
• Gallagher, Thomas H. 2003. “Patients’ and Physicians’ Attitudes Regarding the
Disclosure of Medical Errors.” JAMA 289(8): 1001.
https://doi.org/10.1001/jama.289.8.1001.
• Gallagher, Thomas H., Jane M. Garbutt, Amy D. Waterman, David R. Flum, Eric B.
Larson, Brian M. Waterman, W. Claiborne Dunagan, Victoria J. Fraser, and Wendy
Levinson. 2006. “Choosing Your Words Carefully.” Archives of Internal Medicine
166(15): 1585. https://doi.org/10.1001/archinte.166.15.1585
.
• Kessler, David A. 1993. “Introducing MEDWatch. A New Approach to Reporting
Medication and Device Adverse Effects and Product Problems.” JAMA 269(21): 2765–
68. https://doi.org/10.1001/jama.1993.03500210065033
.
• Leape, Lucian L. 2002. “Reporting of Adverse Events.” New England Journal of
Medicine 347(20): 1633–38. https://doi.org/10.1056/nejmnejmhpr011493.
• Nebeker, Jonathan R., Paul Barach, and Matthew H. Samore. 2004. “Clarifying Adverse
Drug Events: A Clinician’s Guide to Terminology, Documentation, and Reporting.”
Annals of Internal Medicine 140(10): 795.
https://doi.org/10.7326/0003-4819-140
-10-
200405180-00009.
• White, Andrew A., Thomas H. Gallagher, Melissa J. Krauss, Jane Garbutt, et al. 2008.
“The Attitudes and Experiences of Trainees Regarding Disclosing Medical Errors to
Patients.” Academic Medicine 83(3): 250–56.
https://doi.org/10.1097/acm.0b013e3181636e96
.
Clinical Learning Environment Review (CLER) findings for graduate medical
education in patient safety
The ACGME established the CLER Program to provide formative assessment and feedback to
participating sites of ACGME-accredited Sponsoring Institutions. CLER findings and other
information contained in CLER National Reports are not linked to ACGME Program
Requirements but may provide useful insights for programs. Actions taken in response to CLER
findings should not be interpreted as fulfilling Program Requirements.
Findings o
f CLER site visits for creating an environment for safe patient care and quality
improvement are summarized in CLER Issue Brief No. 2 (2016) and CLER Issue Brief No. 3
(2016), which can be found on the Resources and Documents
page of the CLER section of the
ACGME website.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
208

COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
VI.A
.2. Supervision and Accountability
VI.A.2.a) Although the attending physician is ultimately responsible for
the care of the patient, every physician shares in the
responsibility and accountability for their efforts in the
provision of care. Effective programs, in partnership with
their Sponsoring Institutions, define, widely communicate,
and monitor a structured chain of responsibility and
accountability as it relates to the supervision of all patient
care.
Supervi
sion in the setting of graduate medical education
provides safe and effective care to patients; ensures each
resident’s development of the skills, knowledge, and attitudes
required to enter the unsupervised practice of medicine; and
establishes a foundation for continued professional growth.
VI.A
.2.a).(1) Residents and faculty members must inform each
patient of their respective roles in that patient’s care
when providing direct patient care.
(Core)
VI.A.2.a).(1).(a) This information must be available to residents,
faculty members, other members of the health
care team, and patients.
(Core)
Background and Intent: Each patient will have an identifiable and appropriately
credentialed and privileged attending physician (or licensed independent practitioner
as specified by the applicable Review Committee) who is responsible and accountable
for the patient’s care.
VI.A
.2.a).(2) The program must demonstrate that the appropriate
level of supervision in place for all residents is based
on each resident’s level of training and ability, as well
as patient complexity and acuity. Supervision may be
exercised through a variety of methods, as appropriate
to the situation.
(Core)
[The Review Committee may specify which activities
require different levels of supervision.]
Background and Intent: Appropriate supervision is essential for patient safety and high-
quality teaching. Supervision is also contextual. There is tremendous diversity of resident-
patient interactions, education and training locations, and resident skills and abilities, even at
the same level of the educational program. The degree of supervision for a resident is
expected to evolve progressively as the resident gains more experience, even with the same
patient condition or procedure. The level of supervision for each resident is commensurate
with that resident’s level of independence in practice; this level of supervision may be
©2024 Accreditation Council for Graduate Medical Education (ACGME)
209

enhanced based on factors such as patient safety, complexity, acuity, urgency, risk of serious
safety events, or other pertinent variables.
VI.A.2.b) Levels of Supervision
To pr
omote appropriate resident supervision while providing
for graded authority and responsibility, the program must use
the following classification of supervision:
(Core)
VI.A
.2.b).(1) Direct Supervision:
VI.A
.2.b).(1).(a) the supervising physician is physically present
with the resident during the key portions of
the patient interaction; or,
(Core)
[The Review Committee may further specify]
VI.A
.2.b).(1).(a).(i) PGY-1 residents must initially be
supervised directly, only as described in
VI.A.2.c).(1).(a).
(Core)
[The
Review Committee may describe
the condition under which PGY-1
residents progress to be supervised
indirectly]
VI.A
.2.b).(1).(b) the supervising physician and/or patient is not
physically present with the resident and the
supervising physician is concurrently
monitoring the patient care through appropriate
telecommunication technology.
(Core)
[The Review Committee may choose not to
permit this requirement. The Review Committee
may further specify]
VI.A
.2.b).(2) Indirect Supervision: the supervising physician is not
providing physical or concurrent visual or audio
supervision but is immediately available to the
resident for guidance and is available to provide
appropriate direct supervision.
(Core)
VI.A
.2.b).(3) Oversight - the supervising physician is available to
provide review of procedures/encounters with
feedback provided after care is delivered.
(Core)
VI.A
.2.c) The program must define when physical presence of a
supervising physician is required.
(Core)
VI.A
.2.d) The privilege of progressive authority and responsibility,
conditional independence, and a supervisory role in patient
care delegated to each resident must be assigned by the
program director and faculty members.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
210

VI.A.2.d).(1) The program director must evaluate each resident’s
abilities based on specific criteria, guided by the
Milestones
. (Core)
VI.A
.2.d).(2) Faculty members functioning as supervising
physicians must delegate portions of care to residents
based on the needs of the patient and the skills of
each resident.
(Core)
VI.A
.2.d).(3) Senior residents or fellows should serve in a
supervisory role to junior residents in recognition of
their progress toward independence, based on the
needs of each patient and the skills of the individual
resident or fellow.
(Detail)
VI.A
.2.e) Programs must set guidelines for circumstances and events
in which residents must communicate with the supervising
faculty member(s).
(Core)
VI.A
.2.e).(1) Each resident must know the limits of their scope of
authority, and the circumstances under which the
resident is permitted to act with conditional
independence.
(Outcome)
Background and Intent: The ACGME Glossary of Terms defines conditional
independence as: Graded, progressive responsibility for patient care with defined
oversight.
VI.A.2.f) Faculty supervision assignments must be of sufficient
duration to assess the knowledge and skills of each resident
and to delegate to the resident the appropriate level of patient
care authority and responsibility.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
211
GUIDANCE
The Common Program Requirements in VI.A.2. are closely linked with Common Program
Requirement IV.A.3., which addresses resident responsibilities and graded supervision.
The respons
ibilities and supervision of the residents must be clearly delineated. As stated in
VI.A.2.a).(1).(a)-(b), each resident must have an identifiable and appropriately credentialed and
privileged attending physician who is responsible and accountable for a patient’s care. These
responsible attending physicians along with their contact must be made available to residents,
faculty members, and other members of the health care team.
As s
tated in Common Program Requirement VI.A.2.a).(2), the program must demonstrate that
the level of supervision in place for each resident is based on the individual resident’s level of
education and ability, as well as patient complexity and acuity. Progressive authority and
conditional independence are a privilege and must be assigned by the program director and
faculty members. The Clinical Competency Committee (CCC) is key in helping the program
director assign progressive authority based on criteria established by the program and through
Milestones assessments. In addition, during each rotation, supervising faculty members can
help assess the skills of each resident.
Superv
ision may be exercised through a variety of methods. For many aspects of patient care,
the supervising physician may be a more advanced resident or fellow. Other portions of care
provided by the resident can be adequately supervised by the immediate availability of the
supervising faculty member, fellow, or senior resident physician, either on site or by means of
telephonic and/or electronic modalities. Some activities require the physical presence of the
supervising faculty member. In some circumstances, supervision may include post-hoc review
of resident-delivered care with feedback.
Telemedi
cine provides an additional method of supervision. Various models of telemedicine
such as tele-stroke, tele-psychiatry, tele-dermatology, and tele-ophthalmology have increased in
recent years. The use of telemedicine is increasingly adopted by institutions because of added
patient satisfaction, ability to provide care and follow-up in remote areas, significant cost
reduction, and in response to pandemic conditions, as was seen during the COVID-19
pandemic. Recognizing this trend and in this context, Review Committees have the option to
allow use of telesupervision and may also choose to further specify aspects of such use.
Distinct levels of supervision detailed in Common Program Requirement VI.A.2.b) include
Direct, Indirect, and Oversight. While supervision is critical to a resident’s professional
development, there is also such a thing as “over-supervision,” which occurs when more
advanced residents, though deemed capable, are not allowed to make independent decisions
and provide autonomous care. This is detrimental to the development of the skills, knowledge,
and attitudes required to enter the unsupervised practice of medicine.
An additional dimension to supervision is continuity in faculty assignments. Because of multiple
constraints, faculty members are increasingly adopting shorter assignments. One-week faculty
rotations are common, with some even taking assignments that last only two or three days.
Such brief supervision assignments provide insufficient time for faculty members to get to know
residents to determine their knowledge and skills, and therefore should be avoided, if possible.
Bernabeo, et al. (2011) have demonstrated that short faculty supervision assignments are,
indeed, detrimental to patient care.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
212

At
present, the ACGME monitors compliance with the requirements in section VI.A.2. in various
ways, including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by residents and faculty members as part of the annual
Resident/Fellow and Faculty Surveys; and
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
Reference
Bernabeo, Elizabeth C., Matthew C. Holtman, Shiphra Ginsburg, Julie R. Rosenbaum, and
Eric S. Holmboe. 2011. “Lost in Transition: The Experience and Impact of Frequent
Changes in the Inpatient Learning Environment.” Academic Medicine 86(5): 591–98.
https://doi.org/10.1097/acm.0b013e318212c2c9.
ADS Screenshots: ADS questions regarding back-up systems for applications
and programs at all accreditation statuses
The Resident
/Fellow and Faculty Surveys include several questions that address the
requirements in section VI.A.2. The ACGME has prepared two documents, a “Resident/Fellow
Survey-Common Program Requirements Crosswalk” and a “Faculty Survey-Common Program
Requirements Crosswalk” to provide additional information for program on the key areas
addressed by the survey questions and how they map to the ACGME Common Program
Requirements. These documents can be found at
https://www.acgme.org/data-systems-
technical-support/resident-fellow-and-faculty-surveys/.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
213

Clinical Learning Environment Review (CLER) Program findings for graduate
medical education in supervision
The ACG
ME established the CLER Program to provide formative assessment and feedback to
participating sites of ACGME-accredited Sponsoring Institutions. CLER Program findings and
other information contained in CLER National Reports are not linked to ACGME Program
Requirements but may provide useful insights for programs. Actions taken in response to CLER
Program findings should not be interpreted as fulfilling requirements.
Findings of the ACGME’s Clinical Learning Environment Review (CLER) Program regarding
supervision are reported in CLER Issue Brief No. 6 (2016), which can be found on the
Resources and Documents
page of the CLER Program section of the ACGME website.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
214

COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
VI.B. P
rofessionalism
VI.B.1.
Programs, in partnership with their Sponsoring Institutions, must
educate
residents and faculty members concerning the professional
and ethical responsibilities of physicians, including but not limited
to their obligation to be appropriately rested and fit to provide the
care required by their patients.
(Core)
Background and Intent: This requirement emphasizes the professional responsibility
of residents and faculty members to arrive for work adequately rested and ready to
care for patients. It is also the responsibility of residents, faculty members, and other
members of the care team to be observant, to intervene, and/or to escalate their
concern about resident and faculty member fitness for work, depending on the
situation, and in accordance with institutional policies. This includes recognition of
impairment, including from illness, fatigue, and substance use, in themselves, their
peers, and other members of the health care team, and the recognition that under
certain circumstances, the best interests of the patient may be served by transitioning
that patient’s care to another qualified and rested practitioner.
VI.B.2
. The learning objectives of the program must:
VI.B.2
.a) be accomplished without excessive reliance on residents to
fulfill non-physician obligations;
(Core)
Background and Intent: Routine reliance on residents to fulfill non-physician
obligations increases work compression for residents and does not provide an optimal
educational experience. Non-physician obligations are those duties which in most
institutions are performed by nursing and allied health professionals, transport
services, or clerical staff. Examples of such obligations include transport of patients
from the wards or units for procedures elsewhere in the hospital; routine blood
drawing for laboratory tests; routine monitoring of patients when off the ward; and
clerical duties, such as scheduling. While it is understood that residents may be
expected to do any of these things on occasion when the need arises, these activities
should not be performed by residents routinely and must be kept to a minimum to
optimize resident education.
VI.B.2
.b) ensure manageable patient care responsibilities; and,
(Core)
[The Review Committee may further specify]
Background and Intent: The Common Program Requirements do not define
“manageable patient care responsibilities” as this is variable by specialty and PGY
level. Review Committees will provide further detail regarding patient care
responsibilities in the applicable specialty-specific Program Requirements and
accompanying FAQs. However, all programs, regardless of specialty, should carefully
©2024 Accreditation Council for Graduate Medical Education (ACGME)
215

assess how the assignment of patient care responsibilities can affect work
compression, especially at the PGY-1 level.
VI.B.2
.c) include efforts to enhance the meaning that each resident
finds in the experience of being a physician, including
protecting time with patients, providing administrative
support, promoting progressive independence and flexibility,
and enhancing professional relationships.
(Core)
VI.B.3
. The program director, in partnership with the Sponsoring Institution,
must provide a culture of professionalism that supports patient
safety and personal responsibility.
(Core)
Background and Intent: The accurate reporting of clinical and educational work hours,
patient outcomes, and clinical experience data are the responsibility of the program
leadership, residents, and faculty.
VI.B.4
. Residents and faculty members must demonstrate an understanding
of their personal role in the safety and welfare of patients entrusted
to their care, including the ability to report unsafe conditions and
safety events.
(Core)
VI.B.
5. Programs, in partnership with their Sponsoring Institutions, must
provide a professional, equitable, respectful, and civil environment
that psychologically safe and that
is free from discrimination, sexual
and other forms of harassment, mistreatment, abuse, or coercion of
students, residents, faculty, and staff.
(Core)
Background and Intent: Psychological safety is defined as an environment of trust and
respect that allows individuals to feel able to ask for help, admit mistakes, raise
concerns, suggest ideas, and challenge ways of working and the ideas of others on the
team, including the ideas of those in authority, without fear of humiliation, and the
knowledge
that mistakes will be handled justly and fairly.
The A
CGME is unable to adjudicate disputes between individuals, including residents,
faculty members, and staff members. However, information that suggests a pattern of
behavior that violates the requirement above will trigger a careful review and, if
deemed appropriate, action by the Review Committee and/or ACGME, in accordance
with ACGME Policies and Procedures.
VI.B.
6. Programs, in partnership with their Sponsoring Institutions, should
have a process for education of residents and faculty regarding
unprofessional behavior and a confidential process for reporting,
investigating, and addressing such concerns.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
216
GUIDANCE
The Common Program Requirements in VI.B. are central to the mission of every residency
program, to instill in residents an understanding of and ability to meet the professional and
ethical responsibilities inherent in being a physician. In addition to elements described in
Section II of the Common Program Requirements regarding the responsibility of the program
director as a model of professionalism and Section IV regarding the educational program and
the Core Competencies, professionalism as detailed in Section VI addresses other components
of the program’s obligation with regard to how expectations for demonstrating professionalism
must be addressed.
VI.B.1. Programs, in partnership with their Sponsoring Institutions, must educate
residents and faculty members concerning the professional responsibilities of
physicians, including their obligation to be appropriately rested and fit to provide
the care required by their patients.
The Background and Intent associated with this requirement provides additional context for this
requirement. “This requirement emphasizes the professional responsibility of residents and
faculty members to arrive for work adequately rested and ready to care for patients. It is also the
responsibility of residents, faculty members, and other members of the care team to be
observant, to intervene, and/or to escalate their concern about resident and faculty member
fitness for work, depending on the situation, and in accordance with institutional policies. This
includes recognition of impairment, including from illness, fatigue, and substance use, in
themselves, their peers, and other members of the health care team, and the recognition that
under certain circumstances, the best interests of the patient may be served by transitioning that
patient’s care to another qualified and rested practitioner.”
VI.B.2.a) [The learning objectives of the program must:] be accomplished without
excessive reliance on fellows to fulfill non-physician obligations.
The Background and Intent associated with this requirement provides further context and
examples of “non-physician obligations. “Routine reliance on residents to fulfill non-physician
obligations increases work compression for fellows and does not provide an optimal educational
experience. Non-physician obligations are those duties which in most institutions are performed
by nursing and allied health professionals, transport services, or clerical staff. Examples of such
obligations include transport of patients from the wards or units for procedures elsewhere in the
hospital; routine blood drawing for laboratory tests; routine monitoring of patients when off the
ward; and clerical duties, such as scheduling. While it is understood that residents may be
expected to do any of these things on occasion when the need arises, these activities should
not be performed by residents routinely and must be kept to a minimum to optimize resident
education.”
VI.B.2.b) [The learning objectives of the program must:] ensure manageable
patient care responsibilities.
The Background and Intent associated with this requirement acknowledges that “The Common
Program Requirements do not define ’manageable patient care responsibilities‘ as this is
variable by specialty/subspecialty and PGY level. Review Committees will provide further detail
regarding patient care responsibilities in the applicable specialty- and subspecialty-specific
Program Requirements and accompanying FAQs. However, all programs, regardless of
specialty/subspecialty, should carefully assess how the assignment of patient care
responsibilities can affect work compression.”
©2024 Accreditation Council for Graduate Medical Education (ACGME)
217

For spec
ific requirements pertaining to patient number caps and other patient care
responsibilities, refer to the specialty-specific Program Requirements, which can be accessed
from the applicable specialty section of the ACGME website: https://www.acgme.org/specialties
.
VI.B.2.c) [The learning objectives of the program must:] include efforts to
enhance the meaning that each resident finds in the experience of being a
physician, including protecting time with patients, providing administrative
support, promoting progressive independence and flexibility, and enhancing
professional relationships.
VI.B.3. The program director, in partnership with the Sponsoring Institution, must
provide a culture of professionalism that supports patient safety and personal
responsibility.
This r
equirement is closely linked to the professionalism competencies in Common Program
Requirements IV.B.1.(a).(1).(a)-(g).
Prof
essionalism includes an understanding of one’s personal role in the management of
patients as relates to the safety and welfare of patients entrusted to the physician’s care. This
encompasses the ability to report unsafe conditions and adverse events. Physicians must also
take responsibility to ensure they are fit for work. This requirement emphasizes the professional
responsibility of faculty members and residents to arrive for work adequately rested and ready
to care for patients. It is also the responsibility of faculty members, residents, and other
members of the care team to be observant, to intervene, and/or to escalate their concern about
other residents’ or faculty members’ fitness for work, depending on the situation, and in
accordance with institutional policies. These responsibilities include:
• management of time before, during, and after clinical assignments;
• Recognition of impairment (illness, fatigue, substance use) in themselves, their peers,
and other members of the health care team;
• Commitment to lifelong learning;
• monitoring patient care performance; and
• accurate reporting of clinical and educational work hours, patient outcomes, and clinical
experience data
©2024 Accreditation Council for Graduate Medical Education (ACGME)
218

Accreditation Data System (ADS) screenshots: ADS Common Program
Requirements questions
NOTE: Some of the questions only apply to applications while others apply to
programs at all accreditation statuses
©2024 Accreditation Council for Graduate Medical Education (ACGME)
219

VI.B.4. Residents and faculty members must demonstrate an understanding of
their personal role in the safety and welfare of patients entrusted to their care,
including the ability to report unsafe conditions and safety events.
Education alone on the role of residents and faculty in providing safe patient care is not
sufficient. This requirement emphasizes that residents must also demonstrate an understanding
of their role in the safety and welfare of patients and reporting unsafe conditions and safety
events.
VI.B.5. Programs, in partnership with their Sponsoring Institutions, must provide
a professional, equitable, respectful, and civil environment that psychologically
safe and that is free from discrimination, sexual and other forms of harassment,
mistreatment, abuse, or coercion of students, residents, faculty, and staff.
VI.B.6. Programs, in partnership with their Sponsoring Institutions, must provide
a professional, equitable, respectful, and civil environment that is free from
discrimination, sexual and other forms of harassment, mistreatment, abuse, or
coercion of students, residents, faculty members, and staff members
A prof
essional, equitable, respectful, and civil environment that is psychologically safe and free
from discrimination, sexual and other forms of harassment, mistreatment, abuse, or coercion of
students, residents, faculty members, and staff members is a comprehensive way of expressing
the idea that inclusiveness and belonging are essential to fostering an effective learning
environment for all. Professionalism refers to the way in which individuals are handled in a
professional manner within and outside the learning environment. This implies that the
standards, practices, and motivations of the profession are used to fulfill the social contract
between medicine and society. It further implies that elements of evaluation are evidence-based
and fairly administered and includes the ability to recognize and not penalize differences as lack
of professionalism while taking into consideration that professionalism should not be centered
on identities of privilege and power. Professionalism demands that honesty, integrity, and
accountability of the individuals and the organization are foundational to the process. An
equitable environment refers to ensuring that resources are provided according to need in the
learning environment and that all individuals are treated in a fair manner. Respectful means that
individuals in the learning environment are all encouraged to treat one another with dignity and
humility such that the supposition of dominant cultural norms is exchanged for sensitivity,
listening, acceptance, welcoming, and fostering a sense of belonging. Civility refers to a wide
©2024 Accreditation Council for Graduate Medical Education (ACGME)
220
range of behaviors, from emotional to physical, and should employ courtesy and politeness
between individuals who share the learning environment.
The ACG
ME recently clarified that the naming of offenses including mistreatment, abuse,
harassment including sexual harassment, and coercion is based on the principle that even a
single resident who is the victim of these behaviors has standing to complain about violations of
this requirement and can lead to an investigation.
ADS screenshot: ADS Common Program Requirement question for applications
and the ADS Annual Update for programs at initial accreditation
Clinical Learning Environment Review (CLER) Program for graduate medical
education in professionalism
The ACGME established the CLER Program to provide formative assessment and feedback to
participating sites of ACGME-accredited Sponsoring Institutions. CLER findings and other
information contained in CLER National Reports are not linked to ACGME Program
Requirements but may provide useful insights for programs. Actions taken in response to CLER
findings should not be interpreted as fulfilling requirements.
Findings of CLER site visits on professionalism are reported in Issue Brief No. 8 (2016), which
can be found on the Resources and Documents page of the CLER section of the ACG
ME
website.
The Milestones
Online resources related to the Milestones and assessment of professionalism can be found at
https://www.acgme.org/milestones/resources/.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
221

COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
VI.C. W
ell-Being
Psychological, emotional, and physical well-being are critical in the
development of the competent, caring, and resilient physician and require
proactive attention to life inside and outside of medicine. Well-being
requires that physicians retain the joy in medicine while managing their
own real-life stresses. Self-care and responsibility to support other
members of the health care team are important components of
professionalism; they are also skills that must be modeled, learned, and
nurtured in the context of other aspects of residency training.
Resident
s and faculty members are at risk for burnout and depression.
Programs, in partnership with their Sponsoring Institutions, have the same
responsibility to address well-being as other aspects of resident
competence. Physicians and all members of the health care team share
responsibility for the well-being of each other. A positive culture in a
clinical learning environment models constructive behaviors, and prepares
residents with the skills and attitudes needed to thrive throughout their
careers.
VI.C.1.
The responsibility of the program, in partnership with the
Sponsor
ing Institution, must include:
VI.C.1.a) attention to scheduling, work intensity, and work
compression that impacts resident well-being;
(Core)
VI.C.1
.b) evaluating workplace safety data and addressing the safety of
residents and faculty members;
(Core)
Background and Intent: This requirement emphasizes the responsibility shared by the
Sponsoring Institution and its programs to gather information and utilize systems that
monitor and enhance resident and faculty member safety, including physical safety.
Issues to be addressed include, but are not limited to, monitoring of workplace
injuries, physical or emotional violence, vehicle collisions, and emotional well-being
after safety events.
VI.C.1
.c) policies and programs that encourage optimal resident and
faculty member well-being; and,
(Core)
Background and Intent: Well-being includes having time away from work to engage
with family and friends, as well as to attend to personal needs and to one’s own health,
including adequate rest, healthy diet, and regular exercise. The intent of this
requirement is to ensure that residents have the opportunity to access medical and
dental care, including mental health care, at times that are appropriate to their
individual circumstances. Residents must be provided with time away from the
©2024 Accreditation Council for Graduate Medical Education (ACGME)
222

program as needed to access care, including appointments scheduled during their
working hours.
VI.C.1.c).(1) Residents must be given the opportunity to attend
medical, mental health, and dental care appointments,
including those scheduled during their working hours.
(Core)
VI.C.1.d) education of residents and faculty members in:
VI.C.1.d).(1) identification of the symptoms of burnout, depression, and
substance use disorders, suicidal ideation, or potential for
violence, including means to assist those who experience
these conditions;
(Core)
VI.C.1.d).(2) recognition of these symptoms in themselves and how to
seek appropriate care; and,
(Core)
VI.C.1.d).(3) access to appropriate tools for self-screening.
(Core)
Background and Intent: Programs and Sponsoring Institutions are encouraged to
review materials in order to create systems for identification of burnout, depression,
and substance use disorders. Materials and more information are available in Learn at
ACGME (https://dl.acgme.org/pages/well-being-tools-resources).
Individuals experiencing burnout, depression, a substance use disorder, and/or
suicidal ideation are often reluctant to reach out for help due to the stigma associated
with these conditions and may be concerned that seeking help may have a negative
impact on their career. Recognizing that physicians are at increased risk in these
areas, it is essential that residents and faculty members are able to report their
concerns when another resident or faculty member displays signs of any of these
conditions, so that the program director or other designated personnel, such as the
department chair, may assess the situation and intervene as necessary to facilitate
access to appropriate care. Residents and faculty members must know which
personnel, in addition to the program director, have been designated with this
responsibility; those personnel and the program director should be familiar with the
institution’s impaired physician policy and any employee health, employee assistance,
and/or wellness/well-being programs within the institution. In cases of physician
impairment, the program director or designated personnel should follow the policies of
their institution for reporting.
VI.C.1.e)
providing access to confidential, affordable mental health
assessment, counseling, and treatment, including access to
urgent and emergent care 24 hours a day, seven days a week.
(Core)
Background and Intent: The intent of this requirement is to ensure that residents have
immediate access at all times to a mental health professional (psychiatrist,
psychologist, Licensed Clinical Social Worker, Primary Mental Health Nurse
Practitioner, or Licensed Professional Counselor) for urgent or emergent mental health
©2024 Accreditation Council for Graduate Medical Education (ACGME)
223
issues. In-person, telemedicine, or telephonic means may be utilized to satisfy this
requirement. Care in the Emergency Department may be necessary in some cases, but
not as the primary or sole means to meet the requirement.
The reference to affordable counseling is intended to require that financial cost not be
a barrier to obtaining care.
VI.C.2
. There are circumstances in which residents may be unable to attend
wor
k, including but not limited to fatigue, illness, family
emergencies, and medical, parental, or caregiver leave. Each
program must allow an appropriate length of absence for residents
unable to perform their patient care responsibilities.
(Core)
VI.C.2
.a) The program must have policies and procedures in place to
ensure coverage
of patient care and ensure continuity of
patient care.
(Core)
VI.C.2
.b) These policies must be implemented without fear of negative
consequences for the resident who is or was unable to
provide the clinical work.
(Core)
Background and Intent: Residents may need to extend their length of training
depending on length of absence and specialty board eligibility requirements.
Teammates should assist colleagues in need and equitably reintegrate them upon
return.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
224

GUIDANCE
Tools and resources for institutions and programs to support physician well-being are located at:
https://www.acgme.org/meetings-and-educational-activities/physician-well-being/.
The ACG
ME monitors compliance with the Common Program Requirements in section VI.C. in
various ways, including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by fellows and faculty members as part of the annual
Resident/Fellow and Faculty Surveys;
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation; and,
• documentation provided as part of an application or during Initial Accreditation.
ADS Screenshots: ADS Annual Update Common Program Requirements
questions
The Resident
/Fellow and Faculty Surveys include several questions that address the
requirements in section VI.C. The ACGME has prepared two documents, a “Resident/Fellow
Requirements Crosswalk” and a “Faculty Survey-Common Program Requirements Crosswalk,”
to provide additional information for programs on the key areas addressed by the survey
questions and how they map to the ACGME Common Program Requirements. These
documents can be found at
https://www.acgme.org/data-syst
ems-technical-support/resident-
fellow-and-faculty-surveys.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
225
COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
VI.D. Fat
igue Mitigation
VI.D.1.
Programs must educat
e all residents and faculty members in
recognition of the signs of fatigue and sleep deprivation, alertness
management, and fatigue mitigation processes.
(Detail)
Background and Intent: Providing medical care to patients is physically and mentally
demanding. Night shifts, even for those who have had enough rest, cause fatigue.
Experiencing fatigue in a supervised environment during training prepares fellows for
managing fatigue in practice. It is expected that programs adopt fatigue mitigation
processes and ensure that there are no negative consequences and/or stigma for using
fatigue mitigation strategies.
Str
ategies that may be used include, but are not limited to, strategic napping; the judicious
use of caffeine; availability of other caregivers; time management to maximize sleep off-
duty; learning to recognize the signs of fatigue, and self-monitoring performance and/or
asking others to monitor performance; remaining active to promote alertness; maintaining a
healthy diet; using relaxation techniques to fall asleep; maintaining a consistent sleep
routine; exercising regularly; increasing sleep time before and after call; and ensuring
sufficient sleep recovery periods.
VI.D.3
. The program, in partnership with its Sponsoring Institution, must
ensure adequate sleep facilities and safe transportation options for
fellows who may be too fatigued to safely return home.
(Core)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
226

GUIDANCE
The ACGME monitors compliance with the requirements in section VI.D. in various ways,
including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by fellows and faculty members answer as part of the annual
Resident/Fellow and Faculty Surveys; and,
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
ADS Screenshots: ADS questions related to fatigue mitigation
The Resident
/Fellow and Faculty Surveys include several questions that address the
requirements in section VI.D. The ACGME has prepared two documents, a “Resident/Fellow
Survey-Common Program Requirements Crosswalk” and a “Faculty Survey-Common Program
Requirements Crosswalk” to provide additional information for programs on the key areas
addressed by the survey questions and how they map to the ACGME Common Program
Requirements. These documents can be found at
https://www.acgme.org/data-systems-
technical-support/resident-fellow-and-faculty-surveys/.
Clinical Learning Environment Review (CLER) Program findings for graduate
medical education (GME) in fatigue management, mitigation and duty hours
©2024 Accreditation Council for Graduate Medical Education (ACGME)
227

The ACGME established the CLER Program to provide formative assessment and feedback to
participating sites of ACGME-accredited Sponsoring Institutions. CLER findings and other
information contained in CLER National Reports are not linked to ACGME Program
Requirements but may provide useful insights for programs. Actions taken in response to CLER
findings should not be interpreted as fulfilling requirements.
Findings of
CLER site visits relating to fatigue management, mitigation, and clinical work and
education hours are summarized in CLER Issue Brief No. 7 (2017), which can be found on the
Resources and Documents
page of the CLER section of the ACGME website.
Additional Resources
1. Fatigue mitigation: https://sites.duke.edu/thelifecurriculum/2014/05/08/the-life-curriculum/
2. Well-being:
https://gmewellness.upmc.com/?_ga=2.214765521.794333632.1657210383-
1973063117.1654787161
©2024 Accreditation Council for Graduate Medical Education (ACGME)
228

COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
VI.E. C
linical Responsibilities, Teamwork, and Transitions of Care
VI.E.1
. Clinical Responsibilities
The cl
inical responsibilities for each resident must be based on PGY
level, patient safety, resident ability, severity and complexity of
patient illness/condition, and available support services.
(Core)
[Optimal clinical workload may be further specified by each Review
Committee]
Background and Intent: The changing clinical care environment of medicine has meant
that work compression due to high complexity has increased stress on residents.
Faculty members and program directors need to make sure residents function in an
environment that has safe patient care and a sense of resident well-being. It is an
essential responsibility of the program director to monitor resident workload.
Workload should be distributed among the resident team and interdisciplinary teams
to minimize work compression.
VI.E.2
. Teamwork
Resident
s must care for patients in an environment that maximizes
communication and promotes safe, interprofessional, team-based
care in the specialty and larger health system.
(Core)
[The Review Committee may further specify]
Background and Intent: Effective programs will have a structure that promotes safe,
interprofessional, team-based care. Optimal patient safety occurs in the setting of a
coordinated interprofessional learning and working environment.
VI.E.3
. Transitions of Care
VI.E.3
.a) Programs must design clinical assignments to optimize transitions
in patient care, including their safety, frequency, and structure.
(Core)
VI.E.3
.b) Programs, in partnership with their Sponsoring Institutions, must
ensure and monitor effective, structured hand-over processes to
facilitate both continuity of care and patient safety.
(Core)
VI.E.3
.c) Programs must ensure that residents are competent in
communicating with team members in the hand-over process.
(Outcome)
©2024 Accreditation Council for Graduate Medical Education (ACGME)
229

GUIDANCE
Common Program Requirements, VI.E., Clinical Responsibilities, Teamwork, and Transitions of
Care, focus on team-based care and transitions of care.
At
present, he ACGME monitors compliance with the requirements in section VI.E. in various
ways, including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by fellows and faculty members as part of the annual
Resident/Fellow and Faculty Surveys; and,
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
ADS Screenshot: ADS Annual Update question regarding hand-off for
applications and programs with Initial Accreditation
The Resident/Fellow and Faculty Surveys include several questions that address the
requirements in section VI.E. The ACGME has prepared two documents, a “Resident/Fellow
Survey-Common Program Requirements Crosswalk” and a “Faculty Survey-Common Program
Requirements Crosswalk,” to provide additional information for programs on the key areas
addressed by the survey questions and how they map to the ACGME Common Program
Requirements. These documents can be found at
https://acgme.org/data-syst
ems-technical-
support/resident-fellow-and-faculty-surveys/.
Clinical Learning Environment Review (CLER) Program findings for graduate
medical education in care transitions
The ACGME established the CLER Program to provide formative assessment and feedback to
participating sites of ACGME-accredited Sponsoring Institutions. CLER findings and other
information contained in CLER National Reports are not linked to ACGME Program
Requirements but may provide useful insights for programs. Actions taken in response to CLER
findings should not be interpreted as fulfilling requirements.
CLER
Issue Brief No. 5 (2016) addresses care transitions, and can be found on the
Resources
and Documents page of the CLER section of the ACGME website.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
230

As w
ith all of the CLER Issue Briefs, this section is preceded by a narrative. In this instance, a
chief resident expresses frustration over a nursing home transfer of a critically ill patient with an
acute abdomen about whose very complicated prior medical and surgical history she had
absolutely no information. This lack of knowledge by the receiving physician posed significant
risks to the care of the patient. This narrative highlights the risks of communication failure when
patients are transferred from one service to another, or from one institution to another.
The following is a list of elements that should be common to all hand-offs, as noted in CLER
Issue Brief No. 5:
1. creation of “to-do” lists;
2. use of “if-then” statements;
3. ability and expectation for the receiver of information to ask questions;
4. “read-back” at the end of a patient hand-off; and
5. setting of expectations for when it is essential to move the hand-off to the patient’s
bedside.
References
1. Abraham, Joanna, Thomas G. Kannampallil, and Vimla L. Patel. 2008. “Bridging Gaps in
Handoffs: A Continuity of Care Based Approach.” Journal of Surgical Education 65(6):
476-485. https://pubmed.ncbi.nlm.nih.gov/22094355/.
2. Cohen, Michael D., Brian Hilligoss, and André Kajdacsy-Balla Amaral. 2011. “A Handoff
Is Not a Telegram: an Understanding of the Patient Is Co-Constructed.” Critical
Care 16(1): 303. https://doi.org/10.1186/cc10536.
3. Solet, Darrell J., J. Michael Norvell, Gale H. Rutan, and Richard M. Frankel. 2005. “Lost
in Translation: Challenges and Opportunities in Physician-to-Physician Communication
During Patient Handoffs.” Academic Medicine 80(12): 1094–99.
https://doi.org/10.1097/00001888-200512000-00005.
4. Wohlauer, Max V., Vineet M. Arora, Leora I. Horwitz, Ellen J. Bass, Sean E. Mahar, and
Ingrid Philibert. 2012. “The Patient Handoff.” Academic Medicine 87(4): 411–18.
https://doi.org/10.1097/acm.0b013e318248e766.
Resources
Inadequate hand-offs can result in a real potential for patient harm, from minor to severe. There
are numerous efforts across specialties, institutions, and regulatory organizations to improve
hand-offs. The following links provide examples and information related to hand-offs:
5. Agency for Healthcare Research and Quality:
https://psnet.ahrq.gov/primers/primer/9/Handoffs-and-
Signouts
6. The American College of Obstetricians and Gynecologists provided a committee opinion
on communication strategies for patient hand-offs:
https://www.acog.org/clinical/clinical-guidance/
committee-
opinion/articles/2012/02/communication-strategies-for-patient-handoffs
7. Standardization of Inpatient Handoff Communication – from the American Academy of
Pediatrics Committee on Hospital Care
https://pediatrics.aappublications.org/content/138/5/e20162681
©2024 Accreditation Council for Graduate Medical Education (ACGME)
231

COMMON PROGRAM REQUIREMENTS
VI. The Learning and Working Environment
VI.F. C
linical Experience and Education
Programs, in partnership with their Sponsoring Institutions, must design
an effective program structure that is configured to provide residents with
educational and clinical experience opportunities, as well as reasonable
opportunities for rest and personal activities.
Background and Intent: The terms “clinical experience and education,” “clinical and
educational work,” and “clinical and educational work hours” replace the terms “duty
hours,” “duty periods,” and “duty.” These terms are used in response to concerns that
the previous use of the term “duty” in reference to number of hours worked may have
led some to conclude that residents’ duty to “clock out” on time superseded their duty
to their patients.
VI.F.1
. Maximum Hours of Clinical and Educational Work per Week
Cli
nical and educational work hours must be limited to no more than
80 hours per week, averaged over a four-week period, inclusive of all
in-house clinical and educational activities, clinical work done from
home, and all moonlighting.
(Core)
Background and Intent: Programs and residents have a shared responsibility to ensure
that the 80-hour maximum weekly limit is not exceeded. While the requirement has
been written with the intent of allowing residents to remain beyond their scheduled
work periods to care for a patient or participate in an educational activity, these
additional hours must be accounted for in the allocated 80 hours when averaged over
four weeks.
Work f
rom Home
While the requirement specifies that clinical work done from home must be counted
toward the 80-hour maximum weekly limit, the expectation remains that scheduling be
structured so that residents are able to complete most work on site during scheduled
clinical work hours without requiring them to take work home. The new requirements
acknowledge the changing landscape of medicine, including electronic health records,
and the resulting increase in the amount of work residents choose to do from home.
The requirement provides flexibility for residents to do this while ensuring that the time
spent by residents completing clinical work from home is accomplished within the 80-
hour weekly maximum. Types of work from home that must be counted include using
an electronic health record and taking calls from home. Reading done in preparation
for the following day’s cases, studying, and research done from home do not count
toward the 80 hours. Resident decisions to leave the hospital before their clinical work
has been completed and to finish that work later from home should be made in
consultation with the resident’s supervisor. In such circumstances, residents should
be mindful of their professional responsibility to complete work in a timely manner and
to maintain patient confidentiality.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
232

Residents are to track the time they spend on clinical work from home and to report
that time to the program. Decisions regarding whether to report infrequent phone calls
of very short duration will be left to the individual resident. Programs will need to
factor in time residents are spending on clinical work at home when schedules are
developed to ensure that residents are not working in excess of 80 hours per week,
averaged over four weeks. There is no requirement that programs assume
responsibility for documenting this time. Rather, the program’s responsibility is
ensuring that residents report their time from home and that schedules are structured
to ensure that residents are not working in excess of 80 hours per week, averaged over
four weeks.
VI.F.2
. Mandatory Time Free of Clinical Work and Education
VI.F.2.a) Residents should have eight hours off between scheduled
clinical work and education periods.
(Detail)
Background and Intent: There may be circumstances when residents choose to stay to
care for their patients or return to the hospital with fewer than eight hours free of
clinical experience and education. This occurs within the context of the 80-hour and
the one-day-off-in-seven requirements While it is expected that resident schedules will
be structured to ensure that residents are provided with a minimum of eight hours off
between scheduled work periods, it is recognized that residents may choose to remain
beyond their scheduled time, or return to the clinical site during this time-off period, to
care for a patient. The requirement preserves the flexibility for residents to make those
choices. It is also noted that the 80-hour weekly limit (averaged over four weeks) is a
deterrent for scheduling fewer than eight hours off between clinical and education
work periods, as it would be difficult for a program to design a schedule that provides
fewer than eight hours off without violating the 80-hour rule.
VI.F.2
.b) Residents must have at least 14 hours free of clinical work
and education after 24 hours of in-house call.
(Core)
Background and Intent: Residents have a responsibility to return to work rested, and
thus are expected to use this time away from work to get adequate rest. In support of
this goal, residents are encouraged to prioritize sleep over other discretionary
activities.
VI.F.2
.c) Residents must be scheduled for a minimum of one day in
seven free of clinical work and required education (when
averaged over four weeks). At-home call cannot be assigned
on these free days.
(Core)
Background and Intent: The requirement provides flexibility for programs to distribute
days off in a manner that meets program and resident needs. It is strongly
recommended that residents’ preference regarding how their days off are distributed
be considered as schedules are developed. It is desirable that days off be distributed
throughout the month, but some residents may prefer to group their days off to have a
“golden weekend,” meaning a consecutive Saturday and Sunday free from work. The
requirement for one free day in seven should not be interpreted as precluding a golden
©2024 Accreditation Council for Graduate Medical Education (ACGME)
233

weekend. Where feasible, schedules may be designed to provide residents with a
weekend, or two consecutive days, free of work. The applicable Review Committee will
evaluate the number of consecutive days of work and determine whether they meet
educational objectives. Programs are encouraged to distribute days off in a fashion
that optimizes resident well-being, and educational and personal goals. It is noted that
a day off is defined in the ACGME Glossary of Terms as “one (1) continuous 24-hour
period free from all administrative, clinical, and educational activities.”
VI.F.3
. Maximum Clinical Work and Education Period Length
VI.F.3
.a) Clinical and educational work periods for residents must not
exceed 24 hours of continuous scheduled clinical
assignments.
(Core)
VI.F.3
.a).(1) Up to four hours of additional time may be used for
activ
ities related to patient safety, such as providing
effective transitions of care, and/or resident education.
Additional patient care responsibilities must not be
assigned to a resident during this time
.
(Core)
Background and Intent: The additional time referenced in VI.F.3.a).(1) should not be
used for the care of new patients. It is essential that the resident continue to function
as a member of the team in an environment where other members of the team can
assess resident fatigue, and that supervision for post-call residents is provided. This
24 hours and up to an additional four hours must occur within the context of 80-hour
weekly limit, averaged over four weeks.
VI.F.4
. Clinical and Educational Work Hour Exceptions
VI.F.4.a)
In rare circumstances, after handing off all other
responsibi
lities, a resident, on their own initiative, may elect
to remain or return to the clinical site in the following
circumstances: to continue to provide care to a single
severely ill or unstable patient; to give humanistic attention to
the needs of a patient or patient’s family; or to attend unique
educational events.
(Detail)
VI.F.4
.b) These additional hours of care or education must be counted
toward the 80-hour weekly limit.
(Detail)
Background and Intent: This requirement is intended to provide residents with some
control over their schedules by providing the flexibility to voluntarily remain beyond
the scheduled responsibilities under the circumstances described above. It is
important to note that a resident may remain to attend a conference, or return for a
conference later in the day, only if the decision is made voluntarily. Residents must not
be required to stay. Programs allowing residents to remain or return beyond the
scheduled work and clinical education period must ensure that the decision to remain
is initiated by the resident and that residents are not coerced. This additional time
must be counted toward the 80-hour maximum weekly limit.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
234

VI.F.4.c) A Review Committee may grant rotation-specific exceptions
for up to 10 percent or a maximum of 88 clinical and
educational work hours to individual programs based on a
sound educational rationale.
VI.F.4
.c).(1)
In preparing a request for an exception, the program
direct
or must follow the clinical and educational work
hour exception policy from the ACGME Manual of
Policies and Procedures.
(Detail)
Background and Intent: Exceptions may be granted for specific rotations if the
program can justify the increase based on criteria specified by the Review Committee.
Review Committees may opt not to permit exceptions. The underlying philosophy for
this requirement is that while it is expected that all residents should be able to train
within an 80-hour work week, it is recognized that some programs may include
rotations with alternate structures based on the nature of the specialty. DIO/GMEC
approval is required before the request will be considered by the Review Committee.
VI.F.5
. Moonlighting
VI.F.5
.a) Moonlighting must not interfere with the ability of the resident
to achieve the goals and objectives of the educational
program, and must not interfere with the resident’s fitness for
work nor compromise patient safety.
(Core)
VI.F.5
.b) Time spent by residents in internal and external moonlighting
(as defined in the ACGME Glossary of Terms) must be
counted toward the 80-hour maximum weekly limit.
(Core)
VI.F.5
.c) PGY-1 residents are not permitted to moonlight.
(Core)
Background and Intent: For additional clarification of the expectations related to
moonlighting, please refer to the Common Program Requirement FAQs (available at
http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements).
VI.F.6
. In-House Night Float
Night
float must occur within the context of the 80-hour and one-
day-off-in-seven requirements.
(Core)
[The maximum number of consecutive weeks of night float, and
maximum number of months of night float per year may be further
specified by the Review Committee.]
VI.F.7
. Maximum In-House On-Call Frequency
Residents must be scheduled for in-house call no more frequently than
every third night (when averaged over a four-week period).
(Core)
VI.F.8
. At-Home Call
©2024 Accreditation Council for Graduate Medical Education (ACGME)
235

VI.F.8.a) Time spent on patient care activities by residents on at-home
call must count toward the 80-hour maximum weekly limit.
The frequency of at-home call is not subject to the every-
third-night limitation, but must satisfy the requirement for one
day in seven free of clinical work and education, when
averaged over four weeks.
(Core)
VI.F.8
.a).(1) At-home call must not be so frequent or taxing as to
preclude rest or reasonable personal time for each
resident.
(Core)
[The
Review Committee may further specify under any requirement in VI.F. –
VI.F.8.a).(1)]
Background and Intent: As noted in VI.F.1., clinical work done from home when a
resident is taking at-home call must count toward the 80-hour maximum weekly limit.
This change acknowledges the often significant amount of time residents devote to
clinical activities when taking at-home call, and ensures that taking at-home call does
not result in residents routinely working more than 80 hours per week. At-home call
activities that must be counted include responding to phone calls and other forms of
communication, as well as documentation, such as entering notes in an electronic
health record. Activities such as reading about the next day’s case, studying, or
research activities do not count toward the 80-hour weekly limit.
In their evaluation of residency/fellowship programs, Review Committees will look at
the overall impact of at-home call on resident/fellow rest and personal time.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
236

GUIDANCE
Section VI.F. of the Common Program Requirements addresses clinical experience and
education. As the Background and Intent box clarifies, the terms “clinical experience and
education,” “clinical and educational work,” and “clinical and educational work hours” replace the
terms “duty hours,” “duty periods,” and “duty.” These changes were made in response to
concerns that use of the term “duty” in reference to number of hours worked may have led some
to conclude that residents’ duty to “clock out” on time superseded their duty to their patients.
The goal of the earliest standards regarding clinical and educational work hours to the most
recent refinements of these standards has remained the same. Through these standards,
ACGME has continually sought to ensure that “conditions conducive to resident learning,
socialization to the medical profession, and safe and effective patient care consistently occur.
(Nasca and Philibert, 2008).
At
present, the ACGME monitors compliance with the requirements in section VI.F. in various
ways including:
• questions answered by program leadership as part of an application or during the
Accreditation Data System (ADS) Annual Update;
• questions answered by fellows and faculty members answer as part of the annual
Resident/Fellow and Faculty Surveys; and
• questions asked by Accreditation Field Staff during site visits of the program at various
stages of accreditation.
The Resi
dent/Fellow and Faculty Surveys include several questions that address the
requirements in section VI.F. The ACGME has prepared two documents, a “Resident/Fellow
Survey-Common Program Requirements Crosswalk” and a “Faculty Survey-Common Program
Requirements Crosswalk,” to provide additional information for programs on the key areas
addressed by the survey questions and how they map to the ACGME Common Program
Requirements. These documents, along with the Common Program Requirements FAQs
address multiple questions from the graduate medical education community and can be found
at https://www.acgme.org/data-syst
ems-technical-support/resident-fellow-and-faculty-surveys/.
VI.
F.1. Maximum Hours of Clinical and Educational Work per Week
The language in the requirements bears repeating: Clinical and educational work hours must be
limited to no more than 80 hours per week, averaged over a four-week period, inclusive of all in-
house clinical and educational activities, clinical work done from home, and all moonlighting.
ADS Screenshot: As part of a program application or for the ADS Annual Update
for a program on Initial Accreditation, the program director must attest that
resident rotation schedules meet the 80-hour work week requirement.
Programs that regularly schedule residents to work 80 hours per week and still permit them to
remain beyond their scheduled work period will undoubtedly exceed the 80-hour maximum,
which would mean they are not in substantial compliance with the requirement.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
237

The ACGME Review Committees strictly monitor and enforce compliance with the 80-hour
requirement. Where violations of the 80-hour requirement are identified, programs are subject to
citation and are at risk for an adverse accreditation action.
References
• Desai, Sanjay V., David A. Asch, Lisa M. Bellini, Krisda H. Chaiyachati, Manqing Liu,
Alice L. Sternberg, James Tonascia, et al. 2018. “Education Outcomes in a Duty-Hour
Flexibility Trial in Internal Medicine.” New England Journal of Medicine 378(16): 1494–
1508. https://doi.org/10.1056/nejmoa1800965
.)
• Nasca, Thomas J, Philibert, Ingrid. 2008. “Resident Duty-Hour Limits.” Health
Affairs. 27(5):1484.
• Ouyang, David, Jonathan H. Chen, Gomathi Krishnan, Jason Hom, Ronald Witteles, and
Jeffrey Chi. 2016. “Patient Outcomes When Housestaff Exceed 80 Hours per
Week.” The American Journal of Medicine 129(9).
https://doi.org/10.1016/j.amjmed.2016.
03.023.
VI.F.2. Mandatory time free of clinical work and education
While the expectation is that schedules will be structured to ensure resdients are provided with
a minimum of eight hours off between scheduled work periods, the requirement recognizes that
residents may choose to remain beyond their scheduled time or return to the clinical site during
this time-off period to care for a patient preserves the flexibility for residents to make those
choices. The 80-hour weekly limit (averaged over four weeks) is also a deterrent for scheduling
fewer than eight hours off between clinical and educational work periods; it would be difficult for
a program to design a schedule that provides fewer than eight hours off without violating the 80-
hour rule.
The follo
wing requirements in this category are self-explanatory:
• VI.F.2.a) Residents should have eight hours off between scheduled clinical work
and education periods.
• VI.F.2.b) Res
idents must have at least 14 hours free of clinical work and
education after 24 hours of in-house call.
• VI.F.2.c) Residents must be scheduled for a minimum of one day in seven free of
clinical work and required education (when averaged over four weeks). At-home
call cannot be assigned on these free days.
ADS Screenshot: As part of a program application or for the ADS Annual Update
for a program on Initial Accreditation, the program director must attest that
residents will have one full day out of seven free from educational and clinical
responsibilities.
VI.F. 3. Maximum clinical work and education period length
VI.F.3.a) Clinical and educational work periods for residents must not exceed 24 hours of
continuous scheduled clinical assignments.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
238

VI.F.4. Clinical and educational work hour exceptions
The exceptions delineated in this requirement are intended to provide residents with some
control over their schedules by providing the flexibility to voluntarily remain beyond the
scheduled responsibilities under the circumstances described in VI.F.4.a). It is important to note
that a resident may remain to attend a conference, or return for a conference later in the day,
only if the decision is made voluntarily. Residents must not be required to stay. Programs
allowing residents to remain or return beyond the scheduled work and clinical education period
must ensure that the decision to remain is initiated by the resident and that residents are not
coerced. This additional time must be counted toward the 80-hour maximum weekly limit.
• VI.F.4.a) In rare circumstances, after handing off all other responsibilities, a
fellow, on their own initiative, may elect to remain or return to the clinical site in
the following circumstances: to continue to provide care to a single severely ill or
unstable patient; to give humanistic attention to the needs of a patient or patient’s family;
or to attend unique educational events.
• VI.F.4.b) These additional hours of care or education must be counted toward the 80-
hour weekly limit.
• VI.F.4.c) A Review Committee may grant rotation-spec
ific exceptions for up to 10
percent or a maximum of 88 clinical and educational work hours to individual programs
based on a sound educational rationale.
• VI.F.4.c).(1) In preparing a request for an exception, the program director must follow the
clinical and educational work hour exception policy from the ACGME Manual of Policies
and Procedures.
The provision for exceptions for up to 88 hours per week specifies that exceptions may be
granted for particular rotations if the program can justify the increase based on criteria specified
by the Review Committee. Currently, the only Review Committee that allows exceptions to the
80-hour weekly limit is the Review Committee for Neurological Surgery. The underlying
philosophy for this requirement is that while it is expected that all residents should be able to
learn and train within an 80-hour work week, it is recognized that some programs may include
rotations with alternate structures based on the nature of the specialty.
VI.F.7. In-House call
Residents must be scheduled for in-house call no more frequently than every third night (when
averaged over a four-week period).
ADS screenshot: As part of a program application or for the ADS Annual Update
for a program on Initial Accreditation, the program director must provide
information about the frequency of residents’ in-house call assignments.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
239
VI.F.8. At-Home call
There are a number of requirements related to at-home call:
• Time spent on patient care activities by residents on at-home call must count toward the
80-hour maximum.
• It is not subject to the every-third-night limitation, but must meet the requirement for one
day in seven off.
• It must not be so frequent that it precludes rest or reasonable personal time.
Act
ivities such as reading about the next day’s case, studying, or research activities do not
count toward the 80-hour weekly limit.
One of the most common misconceptions regarding Common Program Requirement VI.F.8. is
that residents are required to record every single minute they spend on at-home call answering
phone calls and providing documentation. This is not the expectation. However, program
directors must ensure that at-home call time is reasonable.
©2024 Accreditation Council for Graduate Medical Education (ACGME)
240
