
www.mdedge.com/jcomjournal Vol. 27, No. 1 January/February 2020 JCOM 41
Original Research
A Comparison of 4 Single-Question Measures
of Patient Satisfaction
Iris I.M. Kleiss, MD, Joost T.P. Kortlever, MD, Prithvi Karyampudi, David Ring, MD, PhD,
Laura E. Brown, PhD, Lee M. Reichel, MD, Matt D. Driscoll, MD, and Gregg A. Vagner, MD
P
atient satisfaction is an important quality metric
that is increasingly being measured, reported,
and incentivized. A qualitative study identified 7
themes influencing satisfaction among people visiting an
orthopedic surgeon’s office: trust, relatedness, expec-
tations, wait time, visit duration, communication, and
empathy.
1
However, another study found that satisfaction
and perceived empathy are not associated with wait time
or visit duration, but rather with the quality of the visit.
2
Satisfaction measures that incorporate many of these fea-
tures in relatively long questionnaires are associated with
lower response rates
3
and overlap with the factors whose
influence on satisfaction one would like to study (eg, per-
ceived empathy or communication effectiveness).
4
Single-
and multiple-question satisfaction scores are prone to a
strong right skew, with a substantial ceiling effect.
5
Ceiling
effect occurs when a considerable proportion (about half)
of participants select 1 of the top 2 scores (or the max-
imum score). An ideal scale would measure satisfaction
independent from other factors, would use 1 or just a few
questions, and would have little or no ceiling effect.
From Dell Medical School, The University of Texas at Austin,
Austin, TX.
ABSTRACT
Objective: Satisfaction measures often show substantial
ceiling effects. This randomized controlled trial tested the
null hypothesis that there is no difference in mean overall
satisfaction, ceiling and floor effect, and data distribution
between 4 different kinds of single-question scales
assessing the helpfulness of a visit. We also hypothesized
that there is no correlation between scaled satisfaction
and psychological status. Finally, we assessed how the
satisfaction scores compared with the Net Promoter
Scores (NPS).
Design: Randomized controlled trial.
Methods: We enrolled 258 adult, English-speaking new and
returning patients. Patients were randomly assigned to
1 of 4 different scale types: (1) an 11-point ordinal scale
with 5 anchor points; (2) a 5-point Likert scale; (3) a
0-100 visual analogue scale (VAS) electronic slider with 3
anchor points and visible numbers; and (4) a 0-100 VAS
with 3 anchor points and no visible numbers. Additionally,
patients completed the 2-item Pain Self-Efficacy
Questionnaire (PSEQ-2), 5-item Short Health Anxiety
Inventory scale (SHAI-5), and Patient-Reported Outcomes
Measurement Information System (PROMIS) Depression.
We assessed mean and median score, floor and ceiling
effect, and skewness and kurtosis for each scale.
Spearman correlation tests were used to test correlations
between satisfaction and psychological status.
Results: The nonnumerical 0-100 VAS with 3 anchor points and
the 5-point Likert scale had the least ceiling effect (12% and
20%, respectively). The 11-point ordinal scale had skewness
and kurtosis closest to a normal distribution (skew = –0.58
and kurtosis = 4.0). Scaled satisfaction scores had
a small but significant correlation with PSEQ-2 (r = 0.17;
P = 0.006), but not with SHAI-5 (r = –0.12; P = 0.052) or
PROMIS Depression (r = –0.12; P = 0.064). NPS were 35,
16, 67, and 20 for the scales, respectively.
Conclusion: Single-question measures of satisfaction can be
adjusted to limit the ceiling effect. Additional research in
this area is warranted.
Keywords: patient satisfaction; floor and ceiling effect;
skewness and kurtosis; quality improvement.

Measures of Patient Satisfaction
42 JCOM January/February 2020 Vol. 27, No. 1 www.mdedge.com/jcomjournal
In this randomized controlled trial, we examined whether
there were significant differences in mean and median satisfac-
tion, floor and ceiling effect, and data distribution (by looking at
skewness and kurtosis) between 4 different kinds of satisfaction
scales asking about the helpfulness of a visit. Additionally, we
hypothesized that there is no correlation between scaled sat-
isfaction and psychological status. Finally, we assessed how
the satisfaction scores compared to the Net Promoter Scores
(NPS). NPS are commonly used in the service industry to
measure customer satisfaction; we are using these scores as a
measure of patient satisfaction.
Methods
Study Design
All English-speaking new and return patients ages 18 to
89 years visiting an orthopedic surgeon in 1 of 7 clinics
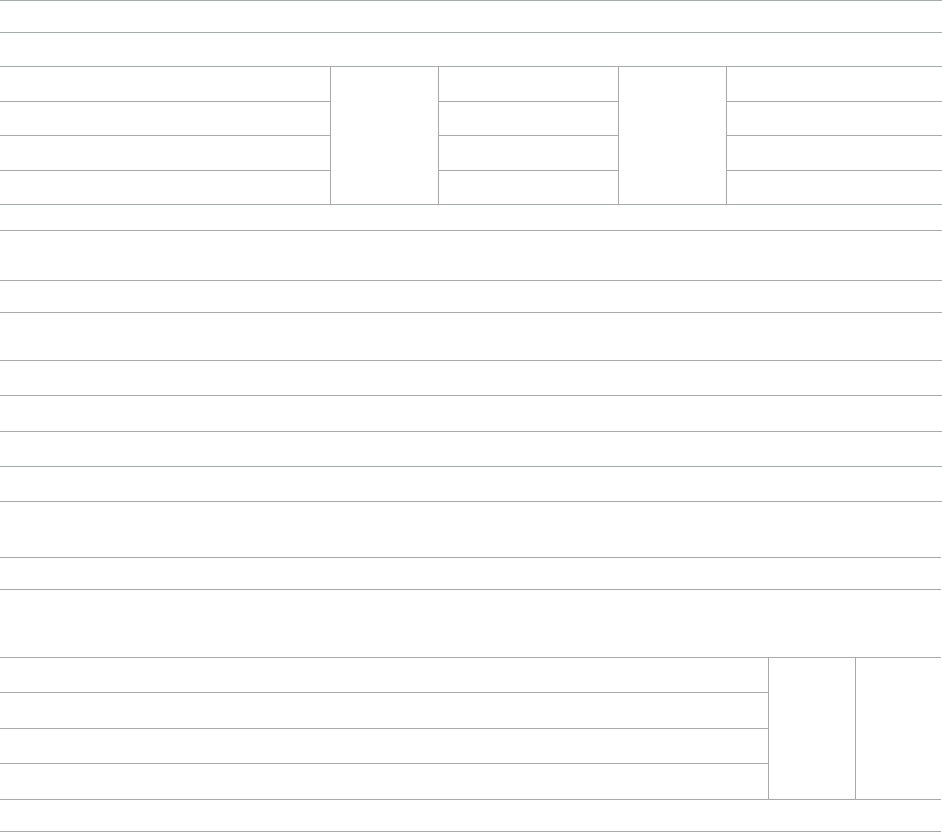
Figure 1. The 4 satisfaction scales. VAS, visual analogue scale.
Scale 4: VAS with slider, 3 anchor points, and no numbers
How helpful was this visit?
0 1 2 3 4 5 6 7 8 9 10
● ● ● ● ● ● ● ● ● ● ●
This visit was not
what I hoped
it would be
There were many
ways it could have
been better
Helpful
visit
Exceptionally
helpful visit
One of the most
helpful doctor visits
I have ever had
How helpful was this visit?
● ● ● ● ●
This visit was not
what I hoped
it would be
There were many
ways it could have
been better
Helpful
visit
Exceptionally
helpful visit
One of the most
helpful doctor visits
I have ever had
Scale 1: 11-point ordinal scale with 5 anchor points
How helpful was this visit?
How helpful was this visit?
0 50 100
Scale 2: 5-point Likert scale
Scale 3: 100-point VAS with slider and 2 anchor points
This visit was not
helpful at all
One of the most
helpful doctor visits
I have ever had
Neither useless or
helpful visit
Most helpful
visit
Least helpful
visit
Original Research
www.mdedge.com/jcomjournal Vol. 27, No. 1 January/February 2020 JCOM 43
located in a large urban area were considered eligible
for this study. Enrollment took place intermittently over
a 5-month period. We were granted a waiver of writ-
ten informed consent. Patients indicated their consent
by completing the surveys. Patients were randomly
assigned to 1 of the 4 questionnaires containing differ-
ent scale types using an Excel random-number gen-
erator. After the visit, patients were asked to complete
the survey. All questionnaires were administered on an
encrypted tablet via a HIPAA-compliant, secure web-
based application for building and managing online sur-
veys and databases (REDCap; Research Electronic Data
Capture).
6
This study was approved by our Institutional
Review Board and is registered on ClinicalTrials.gov
(NCT03686735).
7
Outcome Measures
Study participants were asked to complete questionnaires
regarding demographics (sex, age, race/ethnicity, marital
status, level of education, work status, insurance status,
comorbidities) and to rate satisfaction with their visit on the
scale that was randomly assigned to them: (1) an 11-point
Likert scale with 5 anchor points and visible numbers; (2)
a 5-point Likert scale with 5 anchor points and no visible
numbers; (3) a 0-100 VAS with 3 anchor points and visible
numbers; (4) a 0-100 VAS with 3 anchor points and no
visible numbers (Figure 1). The 4 scales should not differ
in time needed to complete them; however, we did not
explicitly measure time to completion. Participants also
completed measures of psychological aspects of illness.
The 2-item Pain Self-Efficacy Questionnaire (PSEQ-2) was
used to measure pain self-efficacy, an effective coping
strategy for pain.
8
Higher PSEQ-2 scores indicate a higher
level of pain self-efficacy. The 5-item Short Health Anxiety
Inventory scale (SHAI-5) was also administered; higher
scores on this scale indicate a greater degree of health
anxiety.
9
The Patient-Reported Outcomes Measurement
Information System (PROMIS) Depression was used to
measure symptoms of depression.
10
Finally, the diagnosis
was recorded by the surgeon (not in table).
Statistical Analysis
We reported continuous variables using mean, standard
deviation (SD), median, and interquartile range (IQR).
Categorical data are presented as frequencies and per-
centages. We calculated floor and ceiling effect and the
skewness and kurtosis of every scale. We scaled every
scale to 10 and also standardized every scale. We used
the Kruskal–Wallis test to compare differences in satis-
faction between the scales; Fisher’s exact test to com-
pare differences in floor and ceiling effect; and Spearman
correlation tests to test the correlation between scaled
satisfaction scores and psychological status.
Ceiling effects are present when patients select the
highest value on a scale rather than a value that reflects
their actual feelings about a certain topic. Floor effects
are present when patients select the lowest value in a
similar fashion. These 2 effects indicate that an indepen-
dent variable no longer influences the dependent variable
being tested. Skewness and kurtosis are rough indicators
of a normal distribution of values. Skewness (γ1) is an
index of the symmetry of a distribution, with symmetric
distributions having a skewness of 0. If skewness has a
positive value, it suggests relatively many low values, hav-
ing a long right tail. Negative skewness suggests relatively
many high values, having a long left tail. Kurtosis (γ2) is a
measure to describe tailedness of a distribution. Kurtosis
of a normal distribution is 3. Negative kurtosis represents
little peaked distribution, and positive kurtosis represents
more peaked distribution.
11,12
If skewness is 0 and kurtosis
is 3, there is a normal, or Gaussian, distribution.
Finally, we manually calculated the NPS for all scales
by subtracting the percentage of detractors (people who
scored between 0 and 6) from the percentage of promot-
ers (people who scored 9 or 10).
13
NPS are widely used in
the service industry to assess customer satisfaction, and
scores range between –100 and 100.
An a priori power analysis indicated that in order to
find a difference in satisfaction of 0.5 on a 0-10 scale,
with an effect size of 80% and alpha set at 0.05, we
needed 128 patients (64 per group). Since we wanted to
compare 4 satisfaction scales, we doubled this.
Results
Patient Characteristics
All patients invited to participate in this study agreed,
and 258 patients with various diagnoses were enrolled.
The median age of the cohort was 54 years (IQR, 40-65

Measures of Patient Satisfaction
44 JCOM January/February 2020 Vol. 27, No. 1 www.mdedge.com/jcomjournal
years); 114 (44%) were men, and 119 (42%) were new
patients (Table 1). The number of patients assigned to
scales 1, 2, 3, and 4 were 62 (24%), 70 (27%), 67 (26%),
and 59 (23%), respectively.
Difference in Distribution
Looking at the data distribution (Figure 2) and skewness
and kurtosis (Table 2) of the scales, we found that none of
the scales was normally distributed. The 11-point ordinal
scale approached the most normal data distribution, with
minimal skew (γ1, –0.58) and a normal kurtosis (γ2, 4.0).
Difference in Satisfaction Scores
Mean (SD) scaled satisfaction scores (range, 0-10) were
8.3 (1.2) for the 11-point ordinal scale, 8.3 (1.2) for the
5-point Likert scale, 8.9 (1.7) for the 0-100 numerical VAS,
and 8.3 (1.3) for the 0-100 nonnumerical VAS (Table 3
and Table 4). Because of nonnormal distributions, we
tested for a difference using median scores. We found
a difference in median scaled satisfaction scores (range,
0-10) between the 4 satisfaction scales: 11-point ordinal
scale, 8.0 (8.0-9.0); 5-point Likert scale, 8.0 (8.0-8.0);
0-100 numerical VAS, 9.5 (8.9-10); and 0-100 nonnumeri-
cal VAS, 8.4 (7.6-9.5) (P < 0.001; Table 4).
Difference in Floor and Ceiling Effect
A difference was found in ceiling effect between the dif-
ferent scales (P = 0.025), with the 0-100 numerical VAS
showing the highest ceiling effect (34%) and the 0-100
nonnumerical VAS showing the lowest ceiling effect (12%;
25
20
15
10
5
0
0 5 10
Number of patients
Satisfaction score
Satisfaction scale 1
20
15
10
5
0
0 50 100
Number of patients
Satisfaction
Satisfaction scale 3
6
4
2
0
0 50 100
Number of patients
Satisfaction
Satisfaction scale 4
50
40
30
20
0
0
1 2 3 4 5
Number of patients
Satisfaction score
Satisfaction scale 2
Figure 2. Data distribution of the 4 scales.

Original Research
www.mdedge.com/jcomjournal Vol. 27, No. 1 January/February 2020 JCOM 45
Table 2). There was no floor effect. A single patient used
the lowest score (on the Likert scale).
Correlation Between Satisfaction
and Psychological Status
Scaled satisfaction scores had a small but significant cor-
relation with PSEQ-2 (r = 0.17; P = 0.006), but not with
SHAI-5 (r = –0.12; P = 0.052) or PROMIS Depression (r =
– 0.12; P = 0.064; not in table), indicating that patients with
more self-efficacy had higher satisfaction ratings.
Net Promoter Scores
NPS were 35 for the 11-point ordinal scale; 16 for the
5-point Likert scale; 67 for the 0-100 numerical VAS; and
20 for the 0-100 nonnumerical VAS.
Discussion
Single-question measures of satisfaction can decrease
patient burden and limit overlap with measures of com-
munication effectiveness and perceived empathy. Both
long and short questionnaires addressing satisfaction
and perceived empathy show substantial ceiling effect.
We compared 4 different measures for overall scores,
floor and ceiling effect, and skewness and kurtosis, and
assessed the correlation between scaled satisfaction
and psychological status. We found that scale type
influenced the median helpfulness score. As one would
expect, scales with less ceiling effect have lower median
scores. In other words, if the goal is to collect meaning-
ful information and identify areas for improvement, there
must be a willingness to accept lower scores.
Only the nonnumerical VAS was below the threshold of
15% ceiling effect proposed by Terwee et al.
14
This scale
with 3 anchor points and no visible numbers showed the
least ceiling effect (12%) and minimal skew (–1.0), and was
closer to kurtosis consistent with a normal distribution (5.0).
However, the 11-point ordinal Likert scale with 5 anchor
points and visible numbers had the lowest skewness and
kurtosis (–0.58 and 4.0). The low ceiling effect observed
with the nonnumerical VAS (12%) might be explained by
the fact that the scale does not lead patients to a specific
description of the helpfulness of their visit, but rather asks
patients to use their own judgement in making the rat-
ing. The ordinal scale approached the most normal data
distribution, and this might be explained by the presence
of numbers on the scale. Ratings based on a 0-10 scale
are commonly used, and familiarity with the system might
have allowed people to pick a number that represents their
Table 1. Patient and Clinical Characteristics
Variables
Patients
(n = 258)
Median age, yr (IQR) 54 (40-65)
Male, no. (%) 114 (4 4)
Race, no. (%)
White 177 (69)
Latino/Hispanic 49 (19)
Other 32 (12)
Marital status, no. (%)
Married/unmarried couple 162 (63)
Single 58 (22)
Divorced/separated/widowed 38 (15)
Level of education, no. (%)
High school or less 69 (27)
2-year college 43 (17)
4-year college 78 (30)
Post-college graduate degree 68 (26)
Work status, no. (%)
Employed 162 (63)
Retired 54 (21)
Other 42 (16)
Insurance status, no. (%)
Private 139 (54)
Medicare 70 (27)
Other 49 (19)
Type of visit, no. (%)
New 109 (42)
Follow-up 149 (58)
Median PSEQ-2 score (IQR) 11 (8 -12)
Median SHAI-5 score (IQR) 9 (8 -11)
Median PROMIS Depression score (IQR) 48 (42-53)
IQR, interquartile range; PROMIS, Patient-Reported Outcomes Measurement
Information System; PSEQ-2, Pain Self-Efficacy Questionnaire short form;
SHAI-5, Short Health Anxiety Inventory short form.
Measures of Patient Satisfaction
46 JCOM January/February 2020 Vol. 27, No. 1 www.mdedge.com/jcomjournal
actual view of the visit helpfulness, rather than picking the
highest possible choice (which would have led to a ceiling
effect). Study results comparing Likert scales and VAS are
conflicting,
15
with some preferring Likert scales for their
responsiveness
16
and ease of use in practice,
17
and others
preferring VAS for their sensitivity to describe continuous,
subjective phenomenon and their high validity and reliabil-
ity.
18
Looking at our nonnumerical VAS, adding numbers to
a scale might not help avoid, and may actually increase,
the presence of ceiling effect. However, with the ordinal
scale with visible numbers, we saw a 21% ceiling effect
coupled with low skew and kurtosis (–0.58 and 4.0), which
indicate that the distribution of scores is relatively normal.
This finding is in line with other study results.
19
Our findings demonstrated that feedback concerning
self-efficacy, health anxiety, or depression had no or only
a small effect on patient satisfaction. Consistent with prior
evidence, psychological factors had limited or no correla-
tion with satisfaction.
20-24
Given the effect that priming
has on patient-reported outcome measures, the effect of
psychological factors on satisfaction could be an area of
future study.
Table 3. Characteristics of Scales
Scale
Visible
Anchors (no.)
Visible
Numbers
Possible
Range
Possible
Scaled Range
1 Yes (5) Yes 0-10 0-10
2 Yes (5) No 1-5 2-10
3 Yes (3) Yes 0-100 0 -10
4 Yes (3) No 0 -100 0-10
Table 4. Distribution of Scale Scores
Scale
Completed,
no. (%)
Mean
Score
(SD)
Median
Score (IQR) Range
Mean Scaled
Score (SD)
Median
Scaled
Score (IQR)
Mean
Scaled
Range
P Value
Scaled and
Standardized Scores
1 62 (24) 8.3 (1.2) 8.0 (8.0-9.0) 4-10 8.3 (1.2) 8.0 (8.0-9.0) 4.0-10
< 0.001 < 0.001
2 70 (27) 4.1 (0.5 9) 4.0 (4.0-4.0) 1-5 8.3 (1.2) 8.0 (8.0-8.0) 2.0 -10
3 67 (26) 89.0 (17) 95.0 (89-100) 10-100 8.9 (1.7) 9.5 (8.9 -10) 1.0-10
4 59 (23) 83.0 (13) 84.0 (76-95) 35-100 8.3 (1.3) 8.4 (7.6-9.5) 3.5 -10
IQR, interquartile range.
Table 2. Floor and Ceiling Effect and Skewness and Kurtosis of the Scales
Scale Floor Effect P Value Ceiling Effect P Value
Skewness Kurtosis
1 0 (0)
1.0
13 (21)
0.025
–0.58 4.0
2 1 (1.4) 14 (20)
–1.7 13
3 0 (0) 23 (34)
–3.0 14
4 0 (0) 7 (12)
–1.0 5.0
Note: Discrete variables reported as number (%).

Original Research
www.mdedge.com/jcomjournal Vol. 27, No. 1 January/February 2020 JCOM 47
The NPS varied substantially based on scale struc-
ture. Increasing the spread of the scores to limit the
ceiling effect will likely reduce promoters and detractors
and increase neutrals. NPS systems have been used in
the past to measure patient satisfaction with common
hand surgery techniques and with community mental
health services.
25,26
These studies suggest that NPS
could be a helpful addition to commonly used clinical
measures of satisfaction, after more research has been
done to validate it. The evidence showing that NPS are
strongly influenced by scale structure suggests that
NPS should be used and interpreted with caution.
Several caveats regarding this study should be kept
in mind. This study specifically addressed ratings of visit
helpfulness. Differently phrased questions might lead
to different results. More work is needed to determine
the essence of satisfaction with a medical visit.
1
In addi-
tion, the majority of our patient population was white,
employed, and privately insured, limiting generalizabil-
ity to other populations with different demographics.
Finally, all patients were seen by an orthopedic surgeon,
and our results might not apply to other populations or
clinical settings. However, given the scope of this study,
we suspect that the findings can be generalized to
specialty care in general and likely all medical contexts.
Conclusion
It is clear from this work that scale design can affect ceil-
ing effect. We plan to test alternative phrasings and struc-
tures of single-question measures of satisfaction with a
medical visit so that we can better study what factors
contribute to satisfaction. It is notable that this approach
runs counter to efforts to improve satisfaction scores,
because reducing the ceiling effect reduces the mean
score and may contribute to worse NPS. Further study is
needed to find the optimal measure to assess satisfaction
ratings.
Corresponding author: David Ring, MD, PhD, 1701 Trinity Street,
Austin, TX, 78712; david.ring@austin.utexas.edu.
Financial disclosures: Dr. Ring has or may receive payment or
benefits from Skeletal Dynamics; Wright Medical Group; the journal
Clinical Orthopaedics and Related Research; and universities, hos-
pitals, and lawyers not related to the submitted work.
References
1. Waters S, Edmondston SJ, Yates PJ, Gucciardi DF. Identification of
factors influencing patient satisfaction with orthopaedic outpatient
clinic consultation: A qualitative study. Man Ther. 2016;25:48-55.
2. Kortlever JTP, Ottenhoff JSE, Vagner GA, et al. Visit duration does
not correlate with perceived physician empathy. J Bone Joint Surg
Am. 2019;101:296-301.
3. Edwards P, Roberts I, Clarke M, et al. Methods to influence
response to postal questionnaires. Cochrane Database Syst Rev.
2001(3):CD003227.
4. Salisbury C, Burgess A, Lattimer V, et al. Developing a standard
short questionnaire for the assessment of patient satisfaction with
out-of-hours primary care. Fam Pract. 2005;22:560-569.
5. Ross CK, Steward CA, Sinacore JM. A comparative study of seven
measures of patient satisfaction. Med Care. 1995;33:392-406.
6. Harris PA, Taylor R, Thielke R, et al. Research electronic data
capture (REDCap)--a metadata-driven methodology and workflow
process for providing translational research informatics support. J
Biomed Inform. 2009;42:377-381.
7. Medicine USNLo. ClinicalTrials.gov. Accessed March 18, 2019.
8. Nicholas MK, McGuire BE, Asghari A. A 2-item short form of the
Pain Self-efficacy Questionnaire: development and psychometric
evaluation of PSEQ-2. J Pain. 2015;16:153-163.
9. Salkovskis PM, Rimes KA, Warwick H, Clark D. The Health Anxiety
Inventory: development and validation of scales for the mea-
surement of health anxiety and hypochondriasis. Psychol Med.
2002;32:843-853.
10. Schalet BD, Pilkonis PA, Yu L, et al. Clinical validity of PROMIS
depression, anxiety, and anger across diverse clinical samples. J
Clin Epidemiol. 2016;73:119-127.
11. Ho AD, Yu CC. Descriptive statistics for modern test score distri-
butions: skewness, kurtosis, discreteness, and ceiling effects. Educ
Psychol Meas. 2015;75:365-388.
12. Kim HY. Statistical notes for clinical researchers: assessing normal
distribution (2) using skewness and kurtosis. Restor Dent Endod.
2013;38:52-54.
13. NICE Satmetrix. What is net promoter? https://www.netpromoter.
com/know/. Accessed March 18, 2019.
14. Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were pro-
posed for measurement properties of health status questionnaires.
J Clin Epidemiol. 2007;60:34-42.
15. Hasson D, Arnetz BB. Validation and findings comparing VAS vs.
Likert scales for psychosocial measurements. Int Electronic J Health
Educ. 2005;8:178-192.
16. Vickers AJ. Comparison of an ordinal and a continuous outcome
measure of muscle soreness. Int J Technol Assess Health Care.
1999;15:709-716.
17. Jaeschke R, Singer J, Guyatt GH. A comparison of seven-point and
visual analogue scales: data from a randomized trial. Control Clin
Trials. 1990;11:43-51.
18. Voutilainen A, Pitkaaho T, Kvist T, Vehvilainen-Julkunen K. How to
ask about patient satisfaction? The visual analogue scale is less vul-
nerable to confounding factors and ceiling effect than a symmetric
Likert scale. J Adv Nurs. 2016;72:946-957.
19. Brunelli C, Zecca E, Martini C, et al. Comparison of numerical and
verbal rating scales to measure pain exacerbations in patients with
chronic cancer pain. Health Qual Life Outcomes. 2010;8:42.
20. Hageman MG, Briet JP, Bossen JK, et al. Do previsit expectations
correlate with satisfaction of new patients presenting for evaluation
with an orthopaedic surgical practice? Clin Orthop Relat Res.
2015;473:716-721.

Measures of Patient Satisfaction
48 JCOM January/February 2020 Vol. 27, No. 1 www.mdedge.com/jcomjournal
21. Keulen MHF, Teunis T, Vagner GA, et al. The effect of the content
of patient-reported outcome measures on patient perceived
empathy and satisfaction: a randomized controlled trial. J Hand
Surg Am. 2018;43:1141.e1-e9.
22. Mellema JJ, O’Connor CM, Overbeek CL, et al. The effect of
feedback regarding coping strategies and illness behavior on hand
surgery patient satisfaction and communication: a randomized
controlled trial. Hand. 2015;10:503-511.
23. Tyser AR, Gaffney CJ, Zhang C, Presson AP. The association
of patient satisfaction with pain, anxiety, and self-reported
physical function. J Bone Joint Surg Am. 2018;100:1811-1818.
24. Vranceanu AM, Ring D. Factors associated with patient satisfac-
tion. J Hand Surg Am. 2011;36:1504-1508.
25. Stirling P, Jenkins PJ, Clement ND, et al. The Net Promoter Scores
with Friends and Family Test after four hand surgery procedures.
J Hand Surg Eur. 2019;44:290-295.
26. Wilberforce M, Poll S, Langham H, et al. Measuring the patient
experience in community mental health services for older people:
A study of the Net Promoter Score using the Friends and Family
Test in England. Int J Geriatr Psychiatry. 2019;34:31-37.
JCOM is seeking submissions of original research and descriptive reports of quality improvement projects.
Original research submissions can include reports of investigations that address questions about clinical care or the
organization of health care and its impact on outcomes.
Descriptions and evaluations of quality improvement efforts will be considered
for JCOM’s “Reports from the Field” section. The section features reports on
actions being taken to improve quality of care. Such reports may include, but
are not limited to, the following items:
• Motivation for the project, including the role of research ndings
or internal or external benchmarking data
• Setting/demographics
• Intervention/implementation process
• Measurements
• Results
• Similarities to other approaches studied, limitations, applicability
in other settings, etc.
Approximate length is 4000 words. Papers submitted are sent for peer review.
Decisions about manuscripts are made within 8 weeks of receipt. Information
for authors may be found at www.mdedge.com/jcomjournal.
If you are interested in submitting a paper, contact:
Robert Litchkofski, Editor
Call for Contributions
